Abstract
Pseudopolyps are a well described entity in the literature and even though the exact pathogenesis of their formation is not completely understood, they are considered non-neoplastic lesions originating from the mucosa after repeated periods of inflammation and ulceration associated with excessive healing processes. Their occurrence is less common in Crohn's disease than in ulcerative colitis, and their overall prevalence ranges from 4% to 74%; moreover, they are found more often in colon but have been detected in other parts of the gastrointestinal tract as well. When their size exceeds the arbitrary point of 1.5 cm, they are classified as giant pseudopolyps. Clinical evaluation should differentiate the pseudopolyps from other polypoid lesions, such as the dysplasia-associated mass or lesion, but this situation represents an ongoing clinical challenge. Pseudopolyps can provoke complications such as bleeding or obstruction, and their management includes medical therapy, endoscopy and surgery; however, no consensus exists about the optimal treatment approach. Patients with pseudopolyps are considered at intermediate risk for colorectal cancer and regular endoscopic monitoring is recommended. Through a review of the literature, we provide here a proposed classification of the characteristics of pseudopolyps.
Keywords: Pseudopolyps, Inflammatory polyps, Post-inflammatory polyps, Giant pseudopolyps, Ulcerative colitis, Inflammatory bowel disease, Crohn's disease, Classification, Dysplasia-associated mass or lesion
Core tip: In inflammatory bowel disease patients, pseudopolyps are formed at the bowel wall during the inflammatory process. Published reports have begun to elucidate the mechanism of pseudopolyp formation and prevalence; however, the clinical challenge in distinguishing these entities from other dysplastic lesions remains and there is scarce data about their complications and management. In this review, we aimed to condense the published reports about their prevalence and to present a classification of their distinct characteristics based on endoscoping and histologic criteria, in order to facilitate their recognition. Moreover, available methods for confronting their complications and long-term management are presented.
INTRODUCTION
The word pseudopolyp (PP) derives from the compound pseudo, a prefix with Greek origin meaning "fake", and a second compound, polyp, which means "any projection into the intestinal lumen above the layer of mucosa"[1]. The precise pathogenesis of these "fake" polyps is not entirely understood, even though a respectable number of reports exist in the current medical literature. PPs have been described in association with ulcerative colitis (UC) as far back as 1926, although the modern identifier terminology was not used at that time[2]. Their name originated as an effort to separate them from the true neoplastic polyps, namely adenomas[3].
This review focuses on the description of the distinct characteristics of PPs, emphasizing their management and differentiation from dysplasia-associated lesion or mass (DALM) encountered in inflammatory bowel disease (IBD) patients.
LITERATURE RESEARCH
To conduct this review, a search of the medical literature of the PubMed database was carried out to identify articles published up to January of 2016. Topically relevant articles were identified using the terms "pseudopolyps", "inflammatory polyps", "inflammatory pseudopolyps", "giant pseudopolyps"," post inflammatory pseudopolyps", "inflammatory bowel disease", "ulcerative colitis", "Crohn's disease", and "colonic polyps". Bibliographies of the relevant articles were manually searched to identify potentially topical supplementary references, which were retrieved and reviewed. The images provided in this review represent cases managed in our clinical division.
DEFINITIONS AND MECHANISMS OF FORMATION
PPs are formed as a consequence of alternating cycles of inflammation and regeneration of the ulcerated epithelium[4]. The terms pseudopolyps[5], inflammatory polyps[6], post-inflammatory polyps[7] or inflammatory pseudopolyps[8] are often applied interchangeably in the literature, creating confusion. The term pseudopolyps, however, has been applied to the characterization of surviving islets of mucosa between ulcers during a severe attack, which create the impression of a polyp[9], and of loose mucosal tags, which are formed because of severe ulceration undermining the integrity of the muscularis mucosa. In conjunction with the inflammation process and cellular infiltration of the submucosa, granulation tissue is formed, which is more intense in some focal areas, thereby producing inflammatory polyps[10]. During the healing process, which features re-epithelization and excessive regeneration, post-inflammatory polyps are formed[11], taking their shape from the elongation of mucosal tags related to the bowel's peristaltic contractions and the stream of feces[12]. From this perspective, the post-inflammatory polyps can be separated into the following categories: (1) pseudopolyps; (2) inflammatory polyps; and (3) post-inflammatory polyps.
HISTOLOGY
Histology reveals the various aspects of inflammation-acute and chronic-that occur in bowel wall, often simultaneously and parallel in neighboring areas of the colon. The first type is composed only from mucosa, which can be relatively intact or edematous, representing mucosal remnants between zones of ulceration and which, for most authors, are considered the "true'' PPs[10] (Figure 1A).
Figure 1.
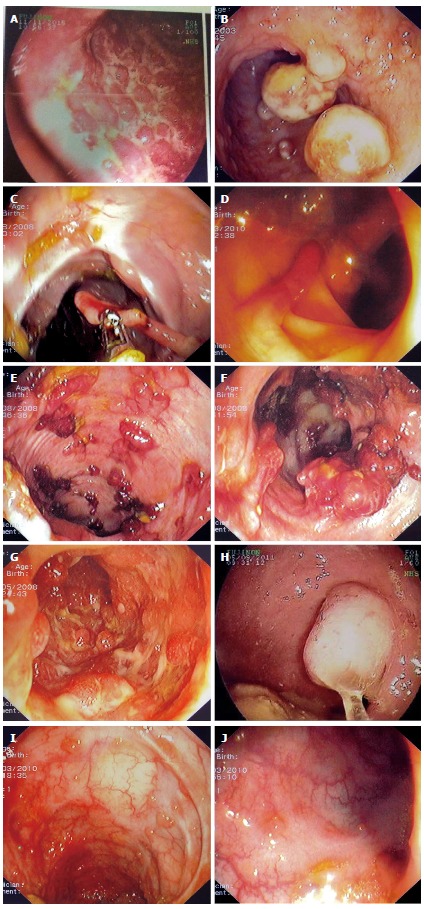
Examples of various types of pseudopolyps in different patients with inflammatory bowel disease. A: Endoscopic picture of deep ulcers and residual islets of surviving mucosa, the "true" pseudopolyps; B: Localized pseudopolyps of varying size up to 1.6 cm with discrete borders, pale surface, exudates on surface and varying forms. Biopsy of the polyps revealed inflammatory infiltration of lymphocytes, distortion and branching of the crypts compatible with post inflammatory pseudopolyps; C: Long filiform pseudopolyp located in the transverse colon captured with biopsy forceps; D: Localized filiform pseudopolyposis located in sigmoid colon; E: Post-inflammatory generalized pseudopolyposis; F: Cluster of pseudopolyps in sigmoid colon with 2.5 cm size, creating a giant localized pseudopolyp. Multiple biopsies of the polyp showed lined epithelium with a core of connective tissue and vessels with inflammatory infiltration which confirmed the diagnosis of pseudopolyp; G: Multiple pseudopolyps stubble the sigmoid colon. In this case, surveillance for dysplasia-associated lesion or mass can be challenging because of the intense inflammation and the multiple pseudopolyps; H: Pseudopolyp or adenoma-like mass? Solitary polyp with 1.5 cm size and broad-based with discrete borders but without exudates, amenable to endoscopic removal and having a pale surface. Histology after removal of the polyp with electrocautery showed villous adenoma with mild dysplasia, and without dysplasia in the surrounding mucosa or elsewhere in the colon, compatible with adenoma-like mass; I: Localized post-inflammatory pseudopolyps; J: Localized pseudopolyps of 0.3 cm maximum size, located in sigmoid colon with discrete borders and pale, glistering surface. Endoscopic characteristics were adequate for recognition of pseudopolyps without the need for biopsies or further intervention.
Inflammatory polyps consist of compact, non-epithelialized granulation tissue, representing a dense mixture of lymphocytes, plasma cells and mast cells predominantly but also includes neutrophils and eosinophils, all of which are detected as infiltrating the proper lamina of ulcerated epithelium. Post-inflammatory pseudopolyps are composed of a layer of normal or slightly-hyperplastic glandular epithelium, mucosa muscularis and a submucosa core of fibrovascular tissue. However, at the bowel wall, mixed forms of these types are frequently found; for example, remnant mucosa infiltrating granulation tissue or granulation tissue at the free ends of post-inflammatory polyps have been detected. The latter is due to secondary ulceration or inflammatory infiltration at the base of PPs[13].
Kelly et al[6] divided PP types into polypoid mucosal tags and mature inflammatory polyps, encompassing essentially all the previous forms, and proposed the term inflammatory polyp as the most appropriate for general use. Histology of the giant pseudopolyp (GPP) type of PIP is composed of multiple bands of the same elements[5].
MORPHOLOGY AND DISTINCT FORMS OF PP
PPs exist in a variety of forms, including sessile, frond-like and pedunculated, and they can occur as solitary or multiple, or as diffuse or localized in distribution[9]. They also vary in size, but are usually short. When a PP exceeds 1.5 cm in size (Figure 1B), the term giant pseudopolyp has prevailed for their characterization[5], with this description first appearing in the literature in 1965[9].
A distinct form of the post-inflammatory polyps is the filiform polyps. These appear as slender, finger-like or worm-like projections of the mucosa and sub-mucosa, and look like a polyp stalk without a head and often with branching[14] (Figure 1C and D). They often create a cluster, and as such are termed as localized giant pseudopolyposis[15] (Figure 1E and F). In the literature, the term filiform polyposis often accounts for GPPs[7]. Another distinct form of the post-inflammatory polyps is the bridged PP, representing a mucosal bridge that formed from a long filiform polyp connecting to the opposite end of the lumen[16].
LOCATION AND DISTRIBUTION OF PPS
PPs are more commonly encountered in large intestine, likely due to this tissue being affected in both UC and Crohn's disease (CD). The most common site is transverse colon and, thereafter, descending and sigmoid colon, with rectum being the least common site; moreover, PP in the rectum are usually found at the upper third region[17]. The GPPs show similar topographic occurrence[7]. However, as CD can involve the entire gastrointestinal tract, the PPs can be present throughout but have been detected less often in extra-colonic regions. There is an exception to this distribution pattern for UC patients with backwash ileitis, wherein PPs have also been found at the terminal ileum[18]. There are also reports of PPs located at the esophagus[19], stomach[20], and different parts of the small bowel[21], with ileum presentation predominating in the latter[22]. There is one case report of a CD patient with pansinusitis location of PP, which regressed with medical therapy[23], and another case report of a patient with refractory pouchitis who presented with a large PP located in an affected pouch[24].
PREVALENCE OF PP IN IBD
PPs are a common finding in IBD[13]. They are found more often in UC than in CD, and some authors have reported a double prevalence in UC as compared with colonic CD[25]. The reported prevalence rates vary from 4% to 74%[26,27], but most of the data supporting these findings was obtained from older studies that considered only UC. The most commonly reported incidence rates in UC fall within the range of 10%-20%[28]. This variation in reported prevalence can be ascribed to miscellaneous diagnostic criteria and different populations studied[6,9-11,17,19,21,26,29-50] (Table 1). For the prevalence of GPP, in particular, a review of 53 colectomised patients with GPPs found that 66.6% had CD and 33.7% had UC[12]; however, a more recent review of 78 patients with IBDs and GPPs found a prevalence of 53.8% in UC patients, which was slightly higher than that found in CD patients (46.2%)[7].
Table 1.
Prevalence of pseudopolyps in inflammatory bowel disease
| Ref. | Year of publication | IBD diagnosis | Prevalence of pseudopolyps | Special characteristics |
| Bargen et al[29] | 1929 | UC (n = 693) | 10.0% | |
| Baars et al[30] | 2012 | UC (n = 171) | 30.0% | 44% of UC patients and 30% of CD patients with unknown status for PP |
| CD (n = 77) | 38.0% | |||
| Baars et al[31] | 2012 | UC, CD (n = 152) | 20.0% | |
| Bacon et al[32] | 1956 | UC (n = 84) | 57.1% | Colectomy specimens |
| Bockus et al[27] | 1956 | UC (n = 125) | 74.0% | Hospitalized patients |
| Chang et al[21] | 2007 | CD (n = 23) | 22.0% | Examined only small intestine |
| Chawla et al[26] | 1990 | UC (n = 50) | 4.0% | |
| Chuttani et al[33] | 1967 | UC (n = 46) | 15.0% | |
| De Dombal et al[17] | 1966 | UC (n = 465) | 12.5% | |
| De Felice et al[19] | 2015 | CD (n = 24) | 4.0% | Location esophagus |
| Dukes et al[11] | 1954 | UC (n = 120) | 10.0% | Colectomy specimens |
| Edwards et al[34] | 1964 | UC (n = 624) | 14.9% | |
| Geboes et al[39] | 1975 | CD (n = 43) | 16.0% | |
| Jalan et al[10] | 1969 | UC (n = 399) | 18.7% | |
| Kelly et al[6] | 1987 | UC, CD (n = 86) | UC: 36% | Colectomy specimens |
| CD: 17% | ||||
| GPP: 4.6% | ||||
| Lescut et al[35] | 1993 | CD (n = 20) | 10.0% | Only small intestine examined as location |
| Luo et al[36] | 2009 | UC, CD (n = 34) | 29.0% | Pediatric population |
| Maroo et al[37] | 1974 | UC (n = 122) | 8.0% | |
| Modigliani et al[50] | 1990 | CD (n = 142) | 41.0% | Active colonic or ileocolonic CD |
| Ray et al[38] | 2011 | UC (n = 40) | 27.0% | |
| Rutter et al[44] | 2004 | UC (n = 136) | 39.0% | Control population without CRC Population with CRC |
| Tandon et al[40] | 1965 | UC (n = 69) | 17.6% | |
| Teague et al[41] | 1975 | UC (n = 150) | 17.0% | |
| Teh et al[42] | 1987 | UC (n = 61) | 21.3% | |
| Velayos et al[43] | 2006 | UC (n = 188) | 42.0% | Control population without CRC Population with CRC |
| UC (n = 188) | 56.0% | |||
| Wang et al[45] | 2007 | UC (n = 2726) | 22.0% | Active UC |
| Watts et al[46] | 1966 | UC (n = 169) | 47.0% | Surgical specimens |
| Waugh et al[47] | 1964 | UC (n = 205) | 5.9% | Surgical specimens |
| Wright et al[48] | 1965 | UC (n = 269) | 10.0% | |
| Zheng et al[49] | 2007 | CD (n = 27) | 48.0% |
CD: Crohn's disease; CRC: Colorectal cancer; IBD: Inflammatory bowel disease; UC: Ulcerative colitis.
There is similar prevalence of PPs in both sexes, and the peak overall incidence is at the ages between 20-40 years. There is no trend in increasing prevalence with extended period of history of the IBD. Specifically, Jalan et al[10] reported that 33% of patients with PP had a < 5-mo history of UC and De Dombal et al[17] reported that among 204 patients with UC, 8.8% had PP on the first flare. For cases of GPPs, Ooi et al[51] reported appearance with a median disease history of 5 years after diagnosis for UC and 6 years after diagnosis for CD; however, there was a broad variation in the times of appearance, ranging from 1 mo to 20 years for UC and from 3 mo to 37 years for CD.
CLINICAL SIGNIFICANCE
The presence of PPs in a patient with IBD can be an indirect marker of previous episodes of severe inflammation, and their incidence rises with more extensive colitis. Although there are not any clear prognostic criteria predicting their formation, it is a common belief that intense flares and hyperplastic healing predispose to PP formation. A cornerstone study by De Dombal et al[17], involving 465 patients with UC, has shown that 19.5% of patients with total colitis had PPs and 38% of the patients with PPs had suffered at least one episode of severe flare; in addition, 57.1% of the patients who underwent colectomy to address fulminant UC in 1956 had PP. This high prevalence can be attributable to severe active disease[32]. Teague et al[41] expressed a similar opinion, citing a PP prevalence of 41% in 48 patients with total colitis, and Jalan et al[10] reported that 31% of patients with severe UC had PP.
In regards to predicting PP formation, Babic et al[52] proposed that elevation in two of the three following parameters-C-reactive protein, C4 and procollagen III peptide-accompany formation of PP in UC, calculating the positive predictive value and accuracy to be as high as 90% and 93%, respectively. The existence of PP has also been linked with the occurrence of extra-intestinal symptoms, specifically arthropathy[10]. Their presence in general, however, does not characterize any specific phase of IBD, as they can be found in both active and quiescent disease states, with the exception of the first form (i.e., the mucosal remnants) which are only found in active IBD[53].
PP AND RISK FOR COLORECTAL CANCER
Patients with PP are considered to be at intermediate risk for colorectal cancer (CRC). United Kingdom guidelines suggest surveillance colonoscopy be performed at a 3-year interval[54], European Crohn's and Colitis Organization guidelines suggest colonoscopy at 2- or 3-year intervals[55] and the American Society for Gastrointestinal Endoscopy suggests between 1- and 3-year intervals[56]. Three studies, performed by Rutter et al[44], Velayos et al[43] and Baars et al[57], have shown a near 2-fold increased risk of CRC in patients with previous or present PP in endoscopy (Table 2). In much older reports, there was a debate about the possibility of PP malignant transformation, with advocates representing both sides. Among these, Goldgraber et al[9] reported a case series of several forms of PP with some showing premalignant changes, but later analysis proved these were benign lesions, regardless of size[10,34].
Table 2.
Pseudopolyps and increased incidence of colorectal cancer
| Ref. | Year of publication | IBD diagnosis | Format of study | Cancer risk |
| Rutter et al[44] | 2004 | UC with CRC (n = 68) | Case-control study 1:2, documentation of PP | OR = 2.29; 95%CI: 1.28-4.11 |
| Velayos et al[43] | 2006 | UC with CRC (n = 188) | Case-control study 1:1, history of PP | OR = 2.5; 95%CI: 1.4-4.6 |
| Baars et al[57] | 2011 | UC (n = 113) | Case-control study 1:2 | RR = 1.92; 95%CI: 1.28 -2.88 |
| CD (n = 58) | ||||
| IC (n = 2) |
CD: Crohn's disease; CRC: Colorectal cancer; IBD: Inflammatory bowel disease; IC: Intermediate colitis; OR: Odds ratio; PP: Pseudopolyp; RR: Relative risk; UC: Ulcerative colitis.
Nowadays, malignant transformation of PP is considered an extremely rare event, with only two reports of GPP harboring carcinoma or dysplasia features[11,58]. Another case report from Klarskov et al[59] presented a carcinoma in rectum stump that had arose from serrated adenoma with a filiform form. The authors speculated that the serrated adenoma had derived from transformation of preexisting PP. A possible mechanism has been implicated by Jawad et al[60], who reported that PP can be the source of premalignant mutations, following their analysis of DNA taken from 30 PP samples and which showed four identifiable mutations. However, more studies are needed to confirm the doubt in their benign nature.
A possible explanation about the relationship between PP and increased risk of CRC lies in the facts that they are considered markers of episodes of previous severe inflammation and that their incidence of appearance rises with the increased extent of colitis[17], which is in turn linked to CRC. Another possible explanation is that their presence, especially if they are numerous, can obscure the capability of finding dysplastic lesions in endoscopic surveillance[43] (Figure 1G).
LONG-TERM MANAGEMENT
Questions remain about the optimal management or follow-up strategies for PP, especially for cases with multiple PP, because no large trials have been published regarding these issues. A great matter of concern involves distinguishing them from adenoma-like DALM and non-adenoma-like DALM (Figure 1H). The main characteristics and differences between these entities are summarized in Table 3, and include features such as location and endoscopic appearance[61-64]. Even though some diagnostic endoscopic criteria may be used for recognizing PP, they are not completely reliable[65]. There can be good inter-observer agreement for identifying PP during endoscopy in general[66], but when it comes to distinguishing PP from other dysplastic lesions, the efficiency falls. Farraye et al[63] performed an internet-based study and found that gastroenterologists with non-IBD-specialized expertise had lower capability of distinguishing different forms of lesions in IBD patients.
Table 3.
Characteristics for differential diagnosis between pseudopolyps, adenoma-like DALM and non-adenoma-like DALM
| Pseudopolyps | Adenoma-like DALM | Non-adenoma-like DALM | |
| Number | Often multiple | Can be multiple, usually solitary | Usually solitary |
| Location | Located in area inside colitis | Located in area inside and outside colitis | Located in area inside colitis |
| Endoscopic appearance | Smooth surface, can have exudate, definite borders, pale surface | Well circumscribed, definite borders, smooth surface sessile or pedunculated | Not amenable to endoscopic removal, irregular borders, often ulcerated or necrotic material |
| Management | No necessity for removal or biopsies except doubt | Endoscopic removal and endoscopic surveillance if dysplasia not recognized in adjacent mucosa or in other area of colitis | Proctocolectomy when HDG in lesion or multifocal LGD in area of colitis |
DALM: Dysplasia-associated lesion or mass; HGD: High-grade dysplasia; LGD: Low-grade dysplasia.
There is a general acceptance that if PP are adequately recognized using endoscopic criteria and do not provoke any complications, no removal is considered obligatory[63] (Figure 1I and J). However, it is considered mandatory that the surface of any PP be surveyed adequately during endoscopy. In older reports, especially of cases with large PP, surgical intervention was frequently performed for the removal, due to confusion with CRC or villous adenoma and related to the more common use of radiological approaches, such as barium enema, for diagnosis and monitoring[67]. Nowadays, however, endoscopic surveillance is more effective than surgical intervention[51].
Chromo-endoscopy might aid in differential diagnosis, since PPs (as non-neoplastic polyps) show Kudo's pattern classification of type II[68]. In another study by Koinuma et al[69], magnifying endoscopy was demonstrated as a useful tool for distinguishing neoplastic from non-neoplastic lesions, reducing the amount of biopsies needed; however, the efficacy of this technique for studying the underlying inflammatory process was shown to be limited by the presence of multiple PPs[65]. In another study, 165 patients with long-standing UC were divided and randomized for endoscopic surveillance by means of either conventional endoscopy (with biopsies every 10 cm) or chromo-endoscopy (with 0.1% methylene blue); there were two false-negative results that were not identified by the chromo-endoscopy procedure, for which non-targeted biopsies from colons with multiple PP proved to contain dysplasia[70].
Nevertheless, in cases where there is either doubt about the diagnosis of PP, suspicion of DALM or large-size PP, or presence of multiple PP wherein endoscopic surveillance is compromised, multiple biopsies should be obtained in repeated examinations[56,71] or proceeding the endoscopic or surgical removal, with surrounding tissue examination by biopsy as well[72].
In the same context, the discovery of PP in a patient with IBD, without evidence of suspicious lesions in endoscopy and in which the presence of PP does not obstruct adequate endoscopic surveillance of the mucosa, should not urge gastroenterologists towards more intense endoscopic follow-up. Neither should it discourage them from the use of chromo-endoscopy for surveillance in any manner other than those proposed in the various guidelines (with an approximate 3-year interval), and certainly not in a different way than would be performed in patients without PPs[54-56]. As mentioned before, CRC derived from PP is a rare event and occurrence of PP has not been linked with early CRC[30]. Therefore, screening for CRC in all patients with PP is not recommended before 8-10 years after onset of symptoms[54-56].
COMPLICATIONS
In rare instances, PP can provoke serious complications, and physicians should be aware of these. Many reports have appeared regarding this issue for cases of GPP. Maggs et al[7] reviewed 78 patients with GPP, among which 15% were complicated with obstruction and sub-obstruction and 3% with intussusception of mechanical etiology due to the large size. In patients with CD, obstruction can occur in the small intestine with PP. In addition, GPPs can produce symptoms similar to IBD, such as bloating, diarrhea and abdominal pain. In that same review, from among the total of 25 patients with inactive disease, 11 had symptoms that regressed after removal of the GPP. Yet, it is important to emphasize that, even in cases of PP, the onset or persistence of symptoms cannot always be attributed to flare or activity of IBD.
There are reports of patients with generalized PP suffering from protein-losing enteropathy and pulmonary embolism, with the possible mechanism being extreme gastrointestinal losses due to the extensive inflamed surface area[73]; other complications include bleeding[74], iron deficiency anemia[75] and dysphagia[76].
TREATMENT
Treatment can be categorized as medical, endoscopic and surgical. Most reports dealing with complications have presented the use of interventional methods, but the majority of these are case reports. Medical treatment has been used for PP and shown to induce regression. Choi et al[71] reported regression of GPP in patients with IBD upon administration of mesalazine and azathioprine. Infliximab has also been shown to induce regression of PP in CD[77]. Topical enema with budenoside use was also reported to induce remission and control of minor bleeding of PP in sigmoid colon[78].
Endoscopic procedures such as argon plasma coagulation[79], endoscopic loop polypectomy[80], and ablation with yttrium aluminium garnet (commonly referred to as YAG) laser have been reported for control of bleeding provoked by ulcerated PP[81]. Endoscopic resection with electrocautery is another effective means reported for removing either symptomatic PPs or PPs of which their benign nature was not able to be established only with endoscopic criteria and which need further histological evaluation[82].
Surgical methods are used when endoscopic therapy fails to manage complicated PP, for example in lower gastrointestinal bleeding or when obstructing phenomena, such as luminal obliteration or intussusception, occur[67]. The various surgical procedures range from segmental dissection to hemicolectomy[83], depending on the cause. However, with the recent advances in endoscopic treatment, the need for a surgical approach has lessened over time.
CONCLUSION
We have reviewed the main aspects regarding PPs and their pathogenesis, management and differentiation from DALM in IBD. Further research can focus on prognostic factors related to their formation. Another interesting subject for clarification is the relationship and comparison between different medical treatments and the possibility of reducing PP prevalence with the additional aim of changing the natural history of IBD.
A key question that remains is: Is the presence of PP a marker of more aggressive IBD with more flares? Theoretically, the answer is positive, accepting the fact that PPs are a result of severe attack. However, that answer leaves open the next question as to whether these patients are indeed suffering from more flares. In addition, it remains unknown whether the newer biological agents and intensified medical therapy, which potentially reduce PP formation, correspond to a decline in CRC risk. We believe that in order to facilitate the management of patients with PP and promote future research on this clinical topic, better documentation of characteristics of pseudopolyps in patients with PP is needed. To this end, Table 4 summarizes the information on descriptions of the characteristics of PPs, which we recommend should be documented when a patient with PPs is encountered.
Table 4.
Summary of characteristics of pseudopolyps and other polypoid lesions in inflammatory bowel disease
| Pseudopolyps and polypoid manifestation | Characterization |
| Location | Upper gastrointestinal tract |
| Small bowel | |
| Large bowel | |
| Both small and large intestine | |
| Special location (pouch) | |
| Size | < 1.5 cm |
| > 1.5 (giant) | |
| Number | < 10 |
| > 10 multiple | |
| Pattern of distribution | Congested |
| Scarce | |
| Years since disease onset | < 1 yr |
| 1-5 yr | |
| > 5 yr | |
| Bowel background mucosa | Relapsed |
| Remission | |
| Endoscopic appearance | Obstructing |
| Bridging (mural bridging lesions) | |
| Penduculated | |
| Filiform (digitiform or fingerlike) | |
| Flat | |
| Mixed type (> 2 types of previous categories) | |
| Long, glistering, with or without exudate | |
| Resectable or not | |
| Definite borders, not stricturing | |
| Histology | Inflammatory |
| Adenomatous | |
| Dysplastic low-grade (DALM) | |
| Dysplastic high-grade (DALM) | |
| Serrated | |
| IBD type | Ulcerative colitis |
| Crohn's disease | |
| Indeterminate colitis | |
| Follow-up | Reduction in number |
| Reduction in size | |
| Increase in number | |
| Increase in size |
DALM: Dysplasia-associated lesion or mass; IBD: Inflammatory bowel disease.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: All authors declare no potential conflicts of interest.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 13, 2016
First decision: December 19, 2016
Article in press: February 17, 2017
P- Reviewer: Owczarek d, Sperti C S- Editor: Ma YJ L- Editor: A E- Editor: Liu WX
References
- 1.Lawrence JC. Gastrointestinal polyps: Statistical study of malignancy incidence. Am J Surg. 1936;31:499–536. [Google Scholar]
- 2.De WI, Wheeler C. Multiple polypi of the colon. Br J Surg. 1926;14:58–66. [Google Scholar]
- 3.Kovalcik PJ, Szydlowski TR. Localized giant pseudopolyposis of the colon in ulcerative colitis. Dis Colon Rectum. 1980;23:268–270. doi: 10.1007/BF02587098. [DOI] [PubMed] [Google Scholar]
- 4.Lumb G. Pathology of ulcerative colitis. Gastroenterology. 1961;40:290–298. [PubMed] [Google Scholar]
- 5.Hinrichs HR, Goldman H. Localized giant pseudopolyps of the colon. JAMA. 1968;205:248–249. [PubMed] [Google Scholar]
- 6.Kelly JK, Gabos S. The pathogenesis of inflammatory polyps. Dis Colon Rectum. 1987;30:251–254. doi: 10.1007/BF02556166. [DOI] [PubMed] [Google Scholar]
- 7.Maggs JR, Browning LC, Warren BF, Travis SP. Obstructing giant post-inflammatory polyposis in ulcerative colitis: Case report and review of the literature. J Crohns Colitis. 2008;2:170–180. doi: 10.1016/j.crohns.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Riddell RH, Goldman H, Ransohoff DF, Appelman HD, Fenoglio CM, Haggitt RC, Ahren C, Correa P, Hamilton SR, Morson BC. Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Hum Pathol. 1983;14:931–968. doi: 10.1016/s0046-8177(83)80175-0. [DOI] [PubMed] [Google Scholar]
- 9.Goldgraber MB. Pseudopolyps in ulcerative colitis. Dis Colon Rectum. 1965;8:355–363. doi: 10.1007/BF02627260. [DOI] [PubMed] [Google Scholar]
- 10.Jalan KN, Walker RJ, Sircus W, McManus JP, Prescott RJ, Card WI. Pseudopolyposis in ulcerative colitis. Lancet. 1969;2:555–559. doi: 10.1016/s0140-6736(69)90260-8. [DOI] [PubMed] [Google Scholar]
- 11.Dukes CE. The surgical pathology of ulcerative colitis. Ann R Coll Surg Engl. 1954;14:389–400. [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly JK, Langevin JM, Price LM, Hershfield NB, Share S, Blustein P. Giant and symptomatic inflammatory polyps of the colon in idiopathic inflammatory bowel disease. Am J Surg Pathol. 1986;10:420–428. doi: 10.1097/00000478-198606000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Buck JL, Dachman AH, Sobin LH. Polypoid and pseudopolypoid manifestations of inflammatory bowel disease. Radiographics. 1991;11:293–304. doi: 10.1148/radiographics.11.2.2028064. [DOI] [PubMed] [Google Scholar]
- 14.Lim YJ, Choi JH, Yang CH. What is the Clinical Relevance of Filiform Polyposis? Gut Liver. 2012;6:524–526. doi: 10.5009/gnl.2012.6.4.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah SM, Rogers HL, Nagai N. Localized giant pseudopolyposis in Crohn's disease: colonoscopic findings. Dis Colon Rectum. 1978;21:104–106. doi: 10.1007/BF02586449. [DOI] [PubMed] [Google Scholar]
- 16.Van Moerkercke W, Deboever G, Lambrecht G, Hertveldt K. Severe bridging fibrosis of the colon in a man with inflammatory bowel disease. Endoscopy. 2007;39 Suppl 1:E294. doi: 10.1055/s-2007-966418. [DOI] [PubMed] [Google Scholar]
- 17.De Dombal FT, Watts JM, Watkinson G, Goligher JC. Local complications of ulcerative colitis: stricture, pseudopolyposis, and carcinoma of colon and rectum. Br Med J. 1966;1:1442–1447. doi: 10.1136/bmj.1.5501.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gardiner GA. "Backwash ileitis" with pseudopolyposis. AJR Am J Roentgenol. 1977;129:506–507. doi: 10.2214/ajr.129.3.506. [DOI] [PubMed] [Google Scholar]
- 19.De Felice KM, Katzka DA, Raffals LE. Crohn's Disease of the Esophagus: Clinical Features and Treatment Outcomes in the Biologic Era. Inflamm Bowel Dis. 2015;21:2106–2113. doi: 10.1097/MIB.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 20.Zegel HG, Laufer I. Filiform polyposis. Radiology. 1978;127:615–619. doi: 10.1148/127.3.615. [DOI] [PubMed] [Google Scholar]
- 21.Chang DK, Kim JJ, Choi H, Eun CS, Han DS, Byeon JS, Kim JO. Double balloon endoscopy in small intestinal Crohn's disease and other inflammatory diseases such as cryptogenic multifocal ulcerous stenosing enteritis (CMUSE) Gastrointest Endosc. 2007;66:S96–S98. doi: 10.1016/j.gie.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Kahn E, Daum F. Pseudopolyps of the small intestine in Crohn's disease. Hum Pathol. 1984;15:84–86. doi: 10.1016/s0046-8177(84)80335-4. [DOI] [PubMed] [Google Scholar]
- 23.Ernst A, Preyer S, Plauth M, Jenss H. Polypoid pansinusitis in an unusual, extra-intestinal manifestation of Crohn disease. HNO. 1993;41:33–36. [PubMed] [Google Scholar]
- 24.Shen B, Fazio VW, Remzi FH, Delaney CP, Bennett AE, Achkar JP, Brzezinski A, Khandwala F, Liu W, Bambrick ML, et al. Comprehensive evaluation of inflammatory and noninflammatory sequelae of ileal pouch-anal anastomoses. Am J Gastroenterol. 2005;100:93–101. doi: 10.1111/j.1572-0241.2005.40778.x. [DOI] [PubMed] [Google Scholar]
- 25.Margulis AR, Goldberg HI, Lawson TL, Montgomery CK, Rambo ON, Noonan CD, Amberg JR. The overlapping spectrum of ulcerative and granulomatous colitis: a roentgenographic-pathologic study. Am J Roentgenol Radium Ther Nucl Med. 1971;113:325–334. doi: 10.2214/ajr.113.2.325. [DOI] [PubMed] [Google Scholar]
- 26.Chawla LS, Chinna JS, Dilawari JB, Sood A. Course and prognosis of ulcerative colitis. J Indian Med Assoc. 1990;88:159–160. [PubMed] [Google Scholar]
- 27.Bockus HL, Roth JL, Buchman E, Kalser M, Staub WR, Finkelstein A, Valdes-Dapena A. Life history of nonspecific ulcerative colitis: relation of prognosis to anatomical and clinical varieties. Gastroenterologia. 1956;86:549–581. doi: 10.1159/000200623. [DOI] [PubMed] [Google Scholar]
- 28.Sheikholeslami MR, Schaefer RF, Mukunyadzi P. Diffuse giant inflammatory polyposis: a challenging clinicopathologic diagnosis. Arch Pathol Lab Med. 2004;128:1286–1288. doi: 10.5858/2004-128-1286-DGIPAC. [DOI] [PubMed] [Google Scholar]
- 29.Bargen JA. Complications and Sequelae of Chronic Ulcerative Colitis. Ann Intern Med. 1929;3:335–352. [Google Scholar]
- 30.Baars JE, Kuipers EJ, van Haastert M, Nicolaï JJ, Poen AC, van der Woude CJ. Age at diagnosis of inflammatory bowel disease influences early development of colorectal cancer in inflammatory bowel disease patients: a nationwide, long-term survey. J Gastroenterol. 2012;47:1308–1322. doi: 10.1007/s00535-012-0603-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baars JE, Nuij VJ, Oldenburg B, Kuipers EJ, van der Woude CJ. Majority of patients with inflammatory bowel disease in clinical remission have mucosal inflammation. Inflamm Bowel Dis. 2012;18:1634–1640. doi: 10.1002/ibd.21925. [DOI] [PubMed] [Google Scholar]
- 32.Bacon HE, Carroll PT, Cates BA, Mcgregor RA, Ouyang LM, Villalba G. Non-specific ulcerative colitis, with reference to mortality, morbidity, complications and long-term survivals following colectomy. Am J Surg. 1956;92:688–695. doi: 10.1016/s0002-9610(56)80140-2. [DOI] [PubMed] [Google Scholar]
- 33.Chuttani HK, Nigam SP, Sama SK, Dhanda PC, Gupta PS. Ulcerative colitis in the tropics. Br Med J. 1967;4:204–207. doi: 10.1136/bmj.4.5573.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edwards FC, Truelove SC. Course and prognosis of ulcerative colitis: Part IV Carcinoma of the colon. Gut. 1964;5:15–22. doi: 10.1136/gut.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lescut D, Vanco D, Bonnière P, Lecomte-Houcke M, Quandalle P, Wurtz A, Colombel JF, Delmotte JS, Paris JC, Cortot A. Perioperative endoscopy of the whole small bowel in Crohn's disease. Gut. 1993;34:647–649. doi: 10.1136/gut.34.5.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo YY, Chen J. Clinical and colonoscopic characteristics of pediatric inflammatory bowel disease. Zhonghua Erke Zazhi. 2009;47:129–133. [PubMed] [Google Scholar]
- 37.Maroo MK, Nag NK, Sortur SV, Patil RS. Ulcerative colitis in Southern Maharashtra. J Indian Med Assoc. 1974;63:350–354. [PubMed] [Google Scholar]
- 38.Ray G. Inflammatory bowel disease in India--changing paradigms. Int J Colorectal Dis. 2011;26:635–644. doi: 10.1007/s00384-010-1084-5. [DOI] [PubMed] [Google Scholar]
- 39.Geboes K, Vantrappen G. The value of colonoscopy in the diagnosis of Crohn's disease. Gastrointest Endosc. 1975;22:18–23. doi: 10.1016/s0016-5107(75)73675-1. [DOI] [PubMed] [Google Scholar]
- 40.Tandon BN, Mathur AK, Mohapatra LN, Tandon HD, Wig KL. A study of the prevalence and clinical pattern of non-specific ulcerative colitis in northern India. Gut. 1965;6:448–453. doi: 10.1136/gut.6.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teague RH, Read AE. Polyposis in ulcerative colitis. Gut. 1975;16:792–795. doi: 10.1136/gut.16.10.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teh LB, Koh D, Ng HS, Kwok KC, Lim TC, Ho MS, Seah CS. Ulcerative colitis in Singapore: a clinical study of sixty-one patients. Ann Acad Med Singapore. 1987;16:474–479. [PubMed] [Google Scholar]
- 43.Velayos FS, Loftus EV, Jess T, Harmsen WS, Bida J, Zinsmeister AR, Tremaine WJ, Sandborn WJ. Predictive and protective factors associated with colorectal cancer in ulcerative colitis: A case-control study. Gastroenterology. 2006;130:1941–1949. doi: 10.1053/j.gastro.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 44.Rutter MD, Saunders BP, Wilkinson KH, Rumbles S, Schofield G, Kamm MA, Williams CB, Price AB, Talbot IC, Forbes A. Cancer surveillance in longstanding ulcerative colitis: endoscopic appearances help predict cancer risk. Gut. 2004;53:1813–1816. doi: 10.1136/gut.2003.038505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang Y, Ouyang Q. Ulcerative colitis in China: retrospective analysis of 3100 hospitalized patients. J Gastroenterol Hepatol. 2007;22:1450–1455. doi: 10.1111/j.1440-1746.2007.04873.x. [DOI] [PubMed] [Google Scholar]
- 46.Watts JM, de Dombal FT, Goligher JC. Early results of surgery for ulcerative colitis. Br J Surg. 1966;53:1005–1014. doi: 10.1002/bjs.1800531202. [DOI] [PubMed] [Google Scholar]
- 47.Waugh JM, Peck DA, Beahrs OH, Sauer WG. Surgical Management of Chronic Ulcerative Colitis. Arch Surg. 1964;88:556–569. doi: 10.1001/archsurg.1964.01310220046009. [DOI] [PubMed] [Google Scholar]
- 48.Wright V, Watkinson G. The Arthritis of Ulcerative Colitis. Br Med J. 1965;2:670–675. doi: 10.1136/bmj.2.5463.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zheng JJ, Cu XQ, Shi XH, Wang YM, Jia LM, Zhou XL, Wang FM. Colonoscopic and histologic features of colonic Crohn's disease in Chinese patients. J Dig Dis. 2007;8:35–41. doi: 10.1111/j.1443-9573.2007.00281.x. [DOI] [PubMed] [Google Scholar]
- 50.Modigliani R, Mary JY, Simon JF, Cortot A, Soule JC, Gendre JP, Rene E. Clinical, biological, and endoscopic picture of attacks of Crohn's disease. Evolution on prednisolone. Groupe d'Etude Thérapeutique des Affections Inflammatoires Digestives. Gastroenterology. 1990;98:811–818. doi: 10.1016/0016-5085(90)90002-i. [DOI] [PubMed] [Google Scholar]
- 51.Ooi BS, Tjandra JJ, Pedersen JS, Bhathal PS. Giant pseudopolyposis in inflammatory bowel disease. Aust N Z J Surg. 2000;70:389–393. doi: 10.1046/j.1440-1622.2000.01826.x. [DOI] [PubMed] [Google Scholar]
- 52.Babic Z, Jagić V, Petrović Z, Bilić A, Dinko K, Kubat G, Troskot R, Vukelić M. Elevated serum values of procollagen III peptide (PIIIP) in patients with ulcerative colitis who will develop pseudopolyps. World J Gastroenterol. 2003;9:619–621. doi: 10.3748/wjg.v9.i3.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keating JW, Mindell HJ. Localized giant pseudopolyposis in ulcerative colitis. AJR Am J Roentgenol. 1976;126:1178–1180. doi: 10.2214/ajr.126.6.1178. [DOI] [PubMed] [Google Scholar]
- 54.Cairns SR, Scholefield JH, Steele RJ, Dunlop MG, Thomas HJ, Evans GD, Eaden JA, Rutter MD, Atkin WP, Saunders BP, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002) Gut. 2010;59:666–689. doi: 10.1136/gut.2009.179804. [DOI] [PubMed] [Google Scholar]
- 55.Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982–1018. doi: 10.1016/j.crohns.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 56.American Society for Gastrointestinal Endoscopy Standards of Practice Committee. Shergill AK, Lightdale JR, Bruining DH, Acosta RD, Chandrasekhara V, Chathadi KV, Decker GA, Early DS, Evans JA, Fanelli RD, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101–1121.e1-13. doi: 10.1016/j.gie.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 57.Baars JE, Looman CW, Steyerberg EW, Beukers R, Tan AC, Weusten BL, Kuipers EJ, van der Woude CJ. The risk of inflammatory bowel disease-related colorectal carcinoma is limited: results from a nationwide nested case-control study. Am J Gastroenterol. 2011;106:319–328. doi: 10.1038/ajg.2010.428. [DOI] [PubMed] [Google Scholar]
- 58.Kusunoki M, Nishigami T, Yanagi H, Okamoto T, Shoji Y, Sakanoue Y, Yamamura T, Utsunomiya J. Occult cancer in localized giant pseudopolyposis. Am J Gastroenterol. 1992;87:379–381. [PubMed] [Google Scholar]
- 59.Klarskov L, Mogensen AM, Jespersen N, Ingeholm P, Holck S. Filiform serrated adenomatous polyposis arising in a diverted rectum of an inflammatory bowel disease patient. APMIS. 2011;119:393–398. doi: 10.1111/j.1600-0463.2011.02717.x. [DOI] [PubMed] [Google Scholar]
- 60.Jawad N, Graham T, Novelli M, Rodriguez-Justo M, Feakins R, Silver A, Wright N, McDonald S. PTU-124 Are pseudopolyps the source of tumorigenic mutations in ulcerative colitis? Gut. 2012;61(Suppl 2):A236. [Google Scholar]
- 61.Rubin PH, Friedman S, Harpaz N, Goldstein E, Weiser J, Schiller J, Waye JD, Present DH. Colonoscopic polypectomy in chronic colitis: conservative management after endoscopic resection of dysplastic polyps. Gastroenterology. 1999;117:1295–1300. doi: 10.1016/s0016-5085(99)70279-9. [DOI] [PubMed] [Google Scholar]
- 62.Farraye FA, Odze RD, Eaden J, Itzkowitz SH, McCabe RP, Dassopoulos T, Lewis JD, Ullman TA, James T, McLeod R, et al. AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138:738–745. doi: 10.1053/j.gastro.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 63.Farraye FA, Waye JD, Moscandrew M, Heeren TC, Odze RD. Variability in the diagnosis and management of adenoma-like and non-adenoma-like dysplasia-associated lesions or masses in inflammatory bowel disease: an Internet-based study. Gastrointest Endosc. 2007;66:519–529. doi: 10.1016/j.gie.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 64.Friedman S. Endoscopic evaluation of polypoid lesions in patients with inflammatory bowel disease. Tech Gastrointest Endosc. 2004;6:175–181. [Google Scholar]
- 65.Bernstein CN. The color of dysplasia in ulcerative colitis. Gastroenterology. 2003;124:1135–1138. doi: 10.1053/gast.2003.50180. [DOI] [PubMed] [Google Scholar]
- 66.Thia KT, Loftus EV, Pardi DS, Kane SV, Faubion WA, Tremaine WJ, Schroeder KW, Harmsen SW, Zinsmeister AR, Sandborn WJ. Measurement of disease activity in ulcerative colitis: interobserver agreement and predictors of severity. Inflamm Bowel Dis. 2011;17:1257–1264. doi: 10.1002/ibd.21480. [DOI] [PubMed] [Google Scholar]
- 67.Biondi A, Persiani R, Paliani G, Mattana C, Vecchio FM, D'Ugo D. Giant inflammatory polyposis as the first manifestation of inflammatory bowel disease. Am J Gastroenterol. 2009;104:2359–2360. doi: 10.1038/ajg.2009.245. [DOI] [PubMed] [Google Scholar]
- 68.Kudo S, Tamura S, Nakajima T, Yamano H, Kusaka H, Watanabe H. Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc. 1996;44:8–14. doi: 10.1016/s0016-5107(96)70222-5. [DOI] [PubMed] [Google Scholar]
- 69.Koinuma K, Togashi K, Konishi F, Kirii Y, Horie H, Okada M, Nagai H. Localized giant inflammatory polyposis of the cecum associated with distal ulcerative colitis. J Gastroenterol. 2003;38:880–883. doi: 10.1007/s00535-002-1164-6. [DOI] [PubMed] [Google Scholar]
- 70.Kiesslich R, Fritsch J, Holtmann M, Koehler HH, Stolte M, Kanzler S, Nafe B, Jung M, Galle PR, Neurath MF. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880–888. doi: 10.1053/gast.2003.50146. [DOI] [PubMed] [Google Scholar]
- 71.Choi YS, Suh JP, Lee IT, Kim JK, Lee SH, Cho KR, Park HJ, Kim DS, Lee DH. Regression of giant pseudopolyps in inflammatory bowel disease. J Crohns Colitis. 2012;6:240–243. doi: 10.1016/j.crohns.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 72.Itzkowitz SH, Harpaz N. Diagnosis and management of dysplasia in patients with inflammatory bowel diseases. Gastroenterology. 2004;126:1634–1648. doi: 10.1053/j.gastro.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 73.Anderson R, Kaariainen IT, Hanauer SB. Protein-losing enteropathy and massive pulmonary embolism in a patient with giant inflammatory polyposis and quiescent ulcerative colitis. Am J Med. 1996;101:323–325. doi: 10.1016/S0002-9343(96)00201-X. [DOI] [PubMed] [Google Scholar]
- 74.Marks RD, Roberts-Thomson IC. Gastrointestinal: colonic pseudopolyposis. J Gastroenterol Hepatol. 2000;15:213. doi: 10.1046/j.1440-1746.2000.02085.x. [DOI] [PubMed] [Google Scholar]
- 75.Manning RJ, Lewis C. Inflammatory ileal polyps in Crohn's disease presenting as refractory iron deficiency anemia. Gastrointest Endosc. 1986;32:122. doi: 10.1016/s0016-5107(86)71780-x. [DOI] [PubMed] [Google Scholar]
- 76.Gheorghe C, Aposteanu G, Popescu C, Gheorghe L, Oproiu A, Popescu I. Long esophageal stricture in Crohn's disease: a case report. Hepatogastroenterology. 1998;45:738–741. [PubMed] [Google Scholar]
- 77.Liatsos C, Kyriakos N, Panagou E, Karagiannis S, Salemis N, Mavrogiannis C. Inflammatory polypoid mass treated with Infliximab in a Crohn's disease patient. J Crohns Colitis. 2010;4:707–708. doi: 10.1016/j.crohns.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 78.Pilichos C, Preza A, Demonakou M, Kapatsoris D, Bouras C. Topical budesonide for treating giant rectal pseudopolyposis. Anticancer Res. 2005;25:2961–2964. [PubMed] [Google Scholar]
- 79.Attar A, Bon C, Sebbagh V, Béjou B, Bénamouzig R. Endoscopic argon plasma coagulation for the treatment of hemorrhagic pseudopolyps in colonic Crohn's disease. Endoscopy. 2007;39 Suppl 1:E249. doi: 10.1055/s-2007-967011. [DOI] [PubMed] [Google Scholar]
- 80.Rutter M, Saunders B, Emmanuel A, Price A. Endoscopic snare polypectomy for bleeding postinflammatory polyps. Endoscopy. 2003;35:788–790. doi: 10.1055/s-2003-41582. [DOI] [PubMed] [Google Scholar]
- 81.Forde KA, Green PH. Laser ablation of symptomatic rectal pseudopolyps. Gastrointest Endosc. 1989;35:135. doi: 10.1016/s0016-5107(89)72737-1. [DOI] [PubMed] [Google Scholar]
- 82.Corless JK, Tedesco FJ, Griffin JW, Panish JK. Giant ileal inflammatory polyps in Crohn's disease. Gastrointest Endosc. 1984;30:352–354. doi: 10.1016/s0016-5107(84)72453-9. [DOI] [PubMed] [Google Scholar]
- 83.Atten MJ, Attar BM, Mahkri MA, Del Pino A, Orsay CP. Giant pseudopolyps presenting as colocolic intussusception in Crohn's colitis. Am J Gastroenterol. 1998;93:1591–1592. doi: 10.1111/j.1572-0241.1998.00491.x. [DOI] [PubMed] [Google Scholar]


