Abstract
Hepatitis C virus (HCV) infection has been a global health problem for decades, due to the high number of infected people and to the lack of effective and well-tolerated therapies. In the last 3 years, the approval of new direct acting antivirals characterized by high rates of virological clearance and excellent tolerability has dramatically improved HCV infection curability, especially for patients with advanced liver disease and for liver transplant recipients. Long-term data about the impact of the new direct acting antivirals on liver fibrosis and liver disease-related outcomes are not yet available, due to their recent introduction. However, previously published data deriving from the use of pegylated-interferon and ribavirin lead to hypothesizing that we are going to observe, in the future, a reduction in mortality and in the incidence of hepatocellular carcinoma, as well as a regression of fibrosis for people previously affected by hepatitis C. In the liver transplant setting, clinical improvement has already been described after treatment with the new direct acting antivirals, which has often led to patients delisting. In the future, this may hopefully reduce the gap between liver organ request and availability, probably expanding liver transplant indications to other clinical conditions. Therefore, these new drugs are going to change the natural history of HCV-related liver disease and the epidemiology of HCV infection worldwide. However, the global consequences will depend on treatment accessibility and on the number of countries that could afford the use of the new direct acting antivirals.
Keywords: Direct acting antivirals, Hepatitis C, Liver transplantation, Liver fibrosis, Cirrhosis, Hepatocellular carcinoma
Core tip: The approval of new direct acting antivirals with high rates of virological clearance and excellent tolerability has dramatically improved hepatitis C virus (HCV) infection curability, especially for patients with advanced liver disease and for liver transplant recipients. The aim of this review is to draw the possible future scenery in HCV-related liver disease, focusing our attention on the impact of second generation direct acting antivirals on liver fibrosis, hepatocellular carcinoma and liver transplantation.
INTRODUCTION
Since its discovery, hepatitis C virus (HCV) has been a constant burden for global health, with 3 to 4 million new infections each year and an overall number of 130-170 million infected people in the world[1]. The prevalence of HCV infection has a large geographical variability, ranging from less than 1% to more than 10% in different regions[2,3]. In particular, 2.3 million of the chronically infected subjects have been estimated to reside in the United States, 1.5 in Japan and 11.5-19 in Europe[4].
HCV infection becomes chronic in up to 50%-80% of cases, establishing a damage that may lead to cirrhosis and its complications [e.g., hepatocellular carcinoma (HCC), portal hypertension, liver decompensation and insufficiency] in approximately 10%-20% of patients[5,6]. Nevertheless, chronic HCV infection may be associated with extrahepatic manifestations, such as cryoglobulinemia and non-Hodgkin lymphoma, mainly caused by the continuous stimulation of the immune system[7,8].
Non-pegylated interferon (IFN) or pegylated IFN (PEG-IFN) in combination with ribavirin (RBV) have been the main pharmacological agents for the treatment of HCV infection. However, only 30%-40% of subjects with genotype 1 HCV and 70%-90% of those with genotype 2 and 3 treated with PEG-IFN in association with RBV were able to reach a sustained virological response (SVR), defined as the absence of detectable levels of HCV-RNA 24 wk after the end of treatment[9-14]. In 2011 the association of the first-generation direct acting antivirals (DAAs) boceprevir and telaprevir with PEG-IFN and RBV increased the overall SVR rates to 68%-75% for naive patients and to 59%-88% for treatment-experienced patients, even if these regimens were dedicated just to the treatment of genotype 1 HCV infection[12,14,15]. However, the suboptimal response rates, the long duration of treatment (24-48 wk) and the scarce tolerability of boceprevir and telaprevir, especially by cirrhotic patients, has heavily affected their clinical use and has led to search for new drugs[16].
SECOND-GENERATION DAAs
The second-generation DAAs are characterized by elevated SVR rates, good safety profiles, and more comfortable types of administration. They can be used or not in combination with RBV, depending on virological and disease-associated characteristics[17]. Sofosbuvir (SOF) has been the first new agent approved by the Food and Drug Administration (FDA) in December 2013 (Table 1 and Figure 1)[18].
Table 1.
Main features of antiviral targets and clinical indications of second-generation direct acting antivirals[17]
| Molecule | Class | Target | Genotype | Associations |
| Sofosbuvir | Nucleotide polymerase inhibitor | NS5B RNA-dependent RNA polymerase | Pangenotypic | Ledipasvir |
| Daclatasvir | ||||
| Simeprevir | ||||
| Velpatasvir | ||||
| Dasabuvir | Non-nucleoside polymerase inhibitor | NS5B RNA-dependent RNA polymerase | Genotype 1 | Ombitasvir + paritaprevir + ritonavir |
| Ombitasvir | NS5A | Genotype 1, 4 | Paritaprevir + ritonavir with or without dasabuvir | |
| Daclatasvir | NS5A | Genotype 1, 2, 3 | Sofosbuvir | |
| Ledipasvir | NS5A | Genotype 1, 4 | Sofosbuvir | |
| Velpatasvir | NS5A | Pangenotypic | Sofosbuvir | |
| Elbasvir | NS5A | Genotype 1, 4 | Grazoprevir | |
| Paritaprevir | NS3/4A protease | Genotype 1, 4 | Ombitasvir + ritonavir with or without dasabuvir | |
| Simeprevir | NS3/4A protease | Genotype 1, 4 | Sofosbuvir | |
| Grazoprevir | NS3/4A protease | Genotype 1, 4 | Elbasvir |
Figure 1.
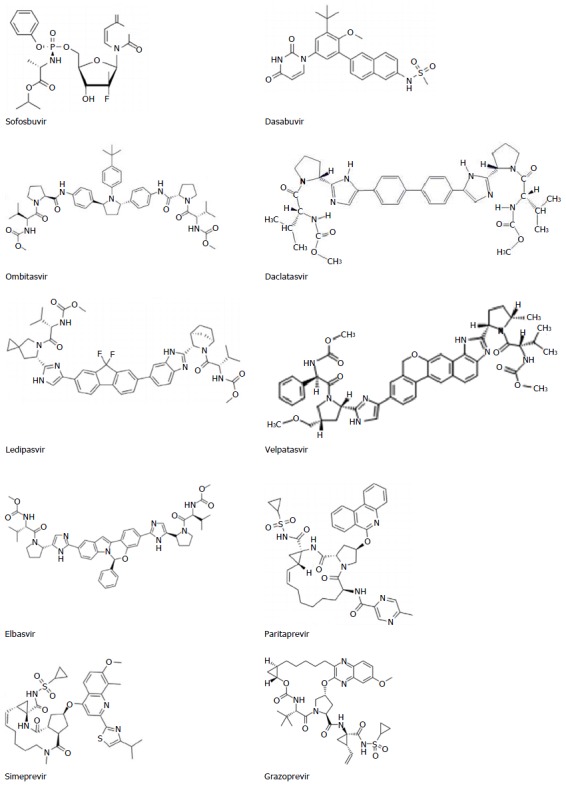
Second-generation direct acting antivirals molecules.
SOF targets HCV-RNA replication with a pangenotypic efficacy since it blocks the nucleotide polymerase NS5B, which is highly preserved among different HCV genotypes[19]. Treatment with SOF, either in combination with PEG-IFN plus RBV or with RBV alone has shown SVR rates above 85% at 12 wk after the end of treatment (SVR12)[20]. Successively, new DAAs for the treatment of HCV infection in association with SOF have been approved: Simeprevir (SMV, a NS3/4A protease inhibitor) and ledipasvir (LDV, a NS5A inhibitor) for genotype 1, and daclatasvir (DCV, a NS5A inhibitor) for genotype 3, reporting SVR12 rates > 90%[21-24]. More recently, the pangenotypic NS5A inhibitor velpatasvir has also been approved for HCV treatment in combination with SOF[25,26].
The first antiviral regimen SOF-free was approved in July 2015 and includes paritaprevir (a NS3/4A protease inhibitor), ritonavir (a CYP3A inhibitor, used as a pharmacologic booster) and ombitasvir (a NS5A inhibitor), in association with dasabuvir (a non-nucleoside NS5B polymerase inhibitor), and is indicated for the treatment of genotype 1 (with dasabuvir) and 4 (without dasabuvir) HCV infection[27,28]. Successively, the FDA has approved another SOF-free antiviral regimen including elbasvir and grazoprevir[29], and new drugs with pangenotypic efficacy are in final phase of study and will soon be available[30].
The main advantage of the new DAAs-based antiviral regimens is the achievement of high SVR rates for all HCV genotypes within a short treatment period, together with the infrequent occurrence of side effects, usually of mild grade. Resistance-associated variants (RAVs) of the virus may exist prior to treatment, may persist for years after treatment and affect most frequently the NS3/5A viral protein; RAVs are associated with (but do not inevitably result in) treatment failure, which may occur in about 10%-15% of patients[31,32].
The most ambitious result we might expect from the use of DAAs would be the reduction of liver cirrhosis-related complications, such as HCC development, and in the long-term period a decreased progression towards end-stage liver disease and a decreased need for liver transplant (LT), as well as the prevention of post-LT HCV infection recurrence[33]. Indeed, according to the latest data published by the World Health Organization in 2013, 5%-7% of infected subjects died from a disease related to HCV[34], with an estimated risk of liver failure of 10.4% and 26.5% in patients with F3 and F4 fibrosis, respectively[35]. HCV-associated liver disease represents the most common indication for LT and, in developed countries, is the most common etiological factor of HCC, which is the third leading cause of cancer death worldwide[36-40].
However, due to the relatively recent introduction of these new drugs, data about their impact on liver disease progression, complications and liver-related mortality are scarce. Therefore, previously published data about the impact of SVR achieved with PEG-IFN-based regimens are the only available reference to evaluate the future positive effects that DAAs might produce on liver disease outcomes.
IMPACT OF VIRAL ERADICATION ON LIVER CIRRHOSIS-ASSOCIATED MORBIDITY AND MORTALITY
Published data have demonstrated a correlation between the achievement of SVR and the reduction of HCV-related complications, liver disease severity and mortality (Table 2).
Table 2.
Main studies highlighting the effects of hepatitis C virus antiviral therapy on patients’ mortality, fibrosis regression and risk of hepatocellular carcinoma
| Ref. | HCV genotype | Fibrosis stage | Treatment | SVR rate | Mortality (n, pts) | Survival | Other outcomes |
| Veldt et al[47], 2007 | G1: 280/474 (59%) | Ishak score 4: 120 (25%) | Duration of treatment, 26 wk (21-48) | 142/280 (50.7%) | SVR: 2/280 (0.7%) | - | SVR associated with reduction in the hazard of events (adjusted HR = 0.21, 95%CI: 0.07-0.58; P < 0.003) |
| Ishak score 5: 94 (20%) | IFN: 131 (27%) | Non-SVR: 24/280 (8.6%) | |||||
| Ishak score 6: 265 (55%) | IFN + RBV: 130 (27%) | ||||||
| PEG-IFN: 10 (2.1%) | |||||||
| PEG-IFN + RBV: 208 (43%) | |||||||
| Yoshida et al[64], 1999 | G1: 1177/2400 (49%) | F0: 45 (1.9%) | IFN-α: 84% | 789/2400 (32.8%) | - | - | Risk of HCC for IFN therapy: Adjusted risk ratio = 0.516, 95%CI: 0.358-0.742 (P < 0.001); risk of HCC for SVR pts: risk ratio = 0.197, 95%CI: 0.099-0.392 (P < 0.002) |
| G2: 496/2400 (20.6%) | F1: 665 (27.7%) | IFN-β: 14% | |||||
| F2: 896 (37.7%) | Combination of IFN-α and IFN-β: 2% | ||||||
| F3: 564 (23.5%) | |||||||
| F4: 230 (9.6%) | |||||||
| Veldt et al[41], 2004 | SVR | SVR: | Recombinant IFN α2a, α2b, or natural IFN monotherapy for 39 wk | 286 | SVR | SVR group: Comparable with the general population | 29% regression and 5% progression of fibrosis in SVR group |
| G1: 112/286 (39.2%) | F4: 15 (5.2%) | 6/286 (2.1%) | |||||
| Not specified: 174/286 (60.8%) | Non-SVR: | 3/50 (6%) | |||||
| Non-SVR | F4: 11 (22%) | ||||||
| G1: 21/50 (42%) | |||||||
| Not specified: 29/50 (58%) | |||||||
| Maruoka et al[42], 2012 | Treated (577): | Treated: | IFN (not specified) | 221/577 (38.3%) | Untreated: 37/144 (25.7%) | - | Risk ratio of overall death and liver-related death reduced to 0.173 (95%CI: 0.075-0.402) |
| G1: 383/577 (66.2%) | F0: 15 (2.6%) | Non-SVR | |||||
| G2: 144/577 (24.8%) | F1: 290 (503%) | 74/356 (20.8%) | |||||
| Untreated (144) | F2: 132 (22.9%) | SVR 10/221 (4.5%) | |||||
| F3: 82 (12.2%) | |||||||
| F4: 58 (10.1%) | |||||||
| Untreated: | |||||||
| F0: 2 (1.4%) | |||||||
| F1: 64 (44.4%) | |||||||
| F2: 32 (22.2%) | |||||||
| F3: 18 (12.5%) | |||||||
| Bruno et al[49], 2016 | G1: 88/181 (48.6%) | F4: 100% | IFN mono-therapy or IFN (pegylated or not) + RBV | 181 | 18/181 (9.9%) | - | - |
| CPT A5: 154/181 (85.1%) | |||||||
| CPT A6: 27/181 (14.9%) | |||||||
| Cardoso et al[44], 2010 | G1: 60% | F4: 54% | PEG-IFN + RBV: 252 (82%), PEG-IFN: 22 (7%), IFN ± RBV: 33 (11%) | 103/307 (33.5%) | 21/307 (6.8%) | - | - |
| G2: 8% | |||||||
| G3: 16% | |||||||
| G4: 13% | |||||||
| Tada et al[46], 2016 | G1: 1476/2743 (53.8%) | - | IFN (not specified) | 587/2267 (25.9%) | 137/2267 (6%) | - | - |
| G2: 789/2743 (28.3%) | |||||||
| Unknown: 478/2743 (17.4%) | |||||||
| Van der Meer et al[48], 2012 | G1: 340/498 (68.3%) | Ishak 4: 143/498 (27%) | IFN: 175 (33%) | 192/498 (38.5%) | SVR: 13 | - | SVR reduced all-cause mortality (HR = 0.265, 95%CI: 0.14-0.49; P < 0.001) |
| G2: 48/498 (9.6%) | Ishak 5: 101/498 (19%) | IFN + RBV: 148 (28%) | Non-SVR: 100 | ||||
| G3: 88/498 (17.7%) | Ishak 6: 22/498 (4%) | PEG-INF: 176 (33%) | |||||
| G4: 22/498 (4.4%) | PEG-IFN + RBV: 176 (33%) | ||||||
| D’Ambrosio et al[52], 2012 | G1: 11/38 (28.9%) | Only cirrhotic patients | IFN + RBV: 10/38 (26.3%) | - | - | - | SVR reduced area of fibrosis by 2.3% (P < 0.0001), with a median individual decrease of 71.8% |
| G2: 24/38 (63.2%) | PEG-IFN + RBV: | ||||||
| G3: 3/38 (7.9%) | 28/38 (73.6%) | ||||||
| Duration of treatment 24 mo (24-48) | |||||||
| Mallet et al[53], 2008 | G1: 51/96 (53.1%) | F4: 100% | IFN or PEG-IFN, with or without RBV | 39/96 (40.6%) | SVR: 4 (10.2%) | - | Regression of fibrosis (according to METAVIR score): Stage 4: 69 (71.9%); stage 3: 9 (9.4%); stage 2: 10 (10.4%); stage 1: 7 (7.3%); stage 0: 1 (1%) |
| Non-SVR: 17 (29.8%) | |||||||
| Reichard et al[56], 1999 | G1: 41/100 (41%) | F0-3: 22 | IFN alpha2b: 73 | 27/100 (27%) | - | - | Reduction of portal inflammation (P < 0.0002), piecemeal necrosis (P < 0.0004), lobular necrosis (P < 0.0005), fibrosis (P < 0.0008) after SVR |
| G2: 27/100 (27%) | F4: 4 | Human leucocyte IFN alpha: 42 | |||||
| G3: 23/100 (23%) | |||||||
| Mixed: 9/100 (9%) | |||||||
| Arif et al[57], 2003 | Naive (52): | Naive | IFN alpha2b | Naive | - | - | Reduction in fibrosis score in both groups: responders = -0.91 (P = 0.038), non-responders = -0.48 (P = 0.021) |
| G1a: 64% | 21/52 (40.4%) | ||||||
| G1b: 19% | Fibrosis score: 2.91 ± 1.64 | Duration of treatment: | |||||
| G2: 6% | 12-24 wk: 10 | Experienced | |||||
| G3: 10% | 24 wk: 56 | 18/79 (22.8%) | |||||
| G4: 1% | 36 wk: 8 | ||||||
| 48 wk: 30 | |||||||
| Experienced (79): | |||||||
| G1a: 55% | |||||||
| G1b: 26% | |||||||
| G2: 7% | |||||||
| G3: 10% | |||||||
| G4: 2% | Fibrosis score: 2.83 ± 1.62 | ||||||
| George et al[58], 2009 | G1: 75/141 (53%) | Fibrosis stage ≥ 2: 116 | IFN alpha2b + RBV: 146 (97%) | 100% | - | 1 | 39/49 (79.6%) reduction in fibrosis stage (according to Ishak score) 16/49 (32.6%) pts had 2 point or greater decrease in stage |
| G2: 49/141 (35%) | Fibrosis stage = 4: 16 | PEG-IFN alpha2a + RBV: | |||||
| G3: 14/141 (10%) | 4 (3%) | ||||||
| G4: 3/141 (2%) | According to Scheuer | ||||||
| Poynard et al[59], 2002 | - | Standard: | Standard: | Standard: | - | - | Decrease in fibrosis index score in SVR group compared with non-responders: From 0.33 ± 0.06 at baseline to 0.18 ± 0.06 at 72 wk vs from 0.41 ± 0.03 at baseline to 0.44 ± 0.03 at 72 wk (P < 0.001) |
| F0: 12 (15%) | IFN alpha2a 3 MU | 3/78 (3.8%) | |||||
| F1: 42 (54%) | TIW for 24 wk | ||||||
| F3: 24 (31%) | Reinforced: IFN alpha2a 6 MU daily for 12 d followed by thrice weekly for 22 wk, then 3 MU thrice weekly for 24 wk | Reinforced: | |||||
| F4: 0 (0%) | 14/87 (16%) | ||||||
| Reinforced: | |||||||
| F0: 16 (18%) | |||||||
| F1: 41 (47%) | |||||||
| F3: 30 (35%) | |||||||
| F4: 0 | |||||||
| Shiratori et al[60], 2000 | - | SVR: | IFN alpha2a or | 183/487 (37.6%) | - | - | SVR group: Rate of fibrosis progression -0.28 ± 0.03 unit/year (regression) |
| F0: 3 (2%) | IFN alpha2b or | ||||||
| F1: 42 (23%) | Natural IFN alpha weekly for 3 to 6 mo | ||||||
| F2: 69 (37%) | Non-SVR group: Rate of fibrosis progression: 0.02 ± 0.02 unit/year | ||||||
| F3: 45 (25%) | IFN alpha 6-7 times per wk for 8 wk | ||||||
| F4: 24 (13%) | |||||||
| Non-SVR: | P < 0.001 | ||||||
| F0: 3 (1%) | |||||||
| F1: 95 (31%) | |||||||
| F2: 109 (36%) | |||||||
| F3: 67 (22%) | |||||||
| F4: 30 (10%) | |||||||
| Maylin et al[62], 2008 | G1: 21/210 (39%) | F0-1: 121 (38%) | IFN alpha: 3 (1%) | 100% | - | - | Fibrosis stage improved in 56%, stable in 32%, deteriorated in 12%; regression of cirrhosis observed in 9 of 14 (64%) |
| G2: 55/210 (18%) | F2: 111 (35%) | IFN-lymphoblastoid: 5 (1%) | |||||
| G3: 101/210 (32%) | F3: 56 (17%) | IFN-hybrid: 9 (3%) | |||||
| G4-5: 33/210 (11%) | F4: 31 (10%) | IFN alpha2a: 18 (5%) | |||||
| IFN alpha2a + RBV: 5 (2%) | |||||||
| PEG-IFN alpha2a + RBV: 27 (8%) | |||||||
| IFN alpha2b: 22 (6%) | |||||||
| IFN alpha2b + RBV: 41 (12%) | |||||||
| PEG-IFN alpha2b + RBV: 214 (62%) |
Pts: Patients; IFN: Interferon; PEG: Pegylated; SVR: Sustained virological response; HCC: Hepatocellular carcinoma; RBV: Ribavirin.
Veldt et al[41] reported that among 286 subjects who achieved SVR and were followed-up for 5 years, only 1% experienced liver failure, with a survival similar to that of the general population. Another study including 721 patients with chronic hepatitis C reported a significantly lower annual mortality rate in subjects who had previously achieved SVR after IFN therapy compared to those who had not (0.44%/year, 1.98%/year and 3.19%/year for SVR, non-SVR and untreated patients, respectively; P < 0.0001). The study also showed that viral clearance was able to reduce the hazard ratio for total deaths by 0.173[42].
A meta-analysis including 129 trials for a total amount of 15067 patients has demonstrated that SVR achievement reduces the risk of LT requirement by 90%, and the risk of death by 60%-84%[43]. Nevertheless, viral clearance leads to a lower incidence of liver-related morbidity and death (0.62 and 0.61 among SVR patients, respectively, and 4.16 and 3.76 among non-SVR patients, respectively; P < 0.001)[44]. Recent data further confirmed that HCV infection resolution allows reduction in the incidence of liver decompensation[45], all-cause mortality[46,47] and annual deaths rate (8.9% in SVR patients vs 26.0% in non-SVR patients; P < 0.001)[48]. This evidence was confirmed by an extensive review by Szabo et al[34]; moreover, survival rates comparable to general population have been reported after the achievement of SVR even in patients with well-compensated cirrhosis[49]. Although useful to figure out the long-term benefits expected from DAAs, the interpretation of data emerging from the use of IFN- or PEG-IFN-based regimens is limited by the selection of patients, since those affected by comorbidities were usually not suitable for treatment and were not included in outcomes analyses; moreover, the lack of homogeneous design and patients’ stratification make it difficult to deduce general conclusions.
IMPACT OF VIRAL ERADICATION ON LIVER FIBROSIS
Despite the positive impact of HCV infection eradication on patients’ prognosis, few data about liver cirrhosis/fibrosis regression are available.
Regression of liver fibrosis as a result of viral clearance is supported by the reduction of inflammatory mediators that leads to apoptosis of myofibroblasts, and occurs by the inactivation of stellate cells. The downregulation of inflammation, as well as microvascular remodelling, degradation of extracellular matrix and hepatocyte repopulation leads to the generation of new hepatic tissue[50,51].
Cirrhosis regression has been reported in about 61% of cases after a median time of 3 years from the achievement of SVR (Table 2)[52]. Mallet et al[53] observed the evolution of liver fibrosis in 96 patients treated with IFN or PEG-IFN with or without RBV, for a median follow-up of 118 mo. Although statistical significance was not reached, 18 subjects obtained a regression of fibrosis from METAVIR stage 4 to stage ≤ 2. In another study, among 153 cirrhotic patients treated with IFN or PEG-IFN in combination or not with RBV for 24 or 48 wk, 75 (49%) had a regression of fibrosis after a mean time of 21 ± 4 mo. In addition to SVR, factors independently associated with histology improvement were age < 40 years (P < 0.001) and body mass index < 27 kg/m2 (P < 0.001)[54].
Other small studies reported variable rates of fibrosis regression after different time periods from viral clearance[55-62].
However, the neo-formed parenchyma derived from the generation of new liver tissue is different from the healthy one and is characterized by architectural and structural alterations[63]. At present, little is known about its functionality.
IMPACT OF VIRAL ERADICATION ON THE DEVELOPMENT OF HCC
In HCV-infected subjects, the development of liver cirrhosis is the main oncogenic trigger for HCC[5,64,65], though not the only one. Indeed, direct and indirect viral-related mechanisms may contribute to the growth of cancer cells, including the expression of viral proteins with oncogenic effect from infected cells, messy proliferation of non-infected hepatocytes responsive to the apoptotic boost and the oxidative stress caused by inflammation[66].
The first study documenting the importance of viral clearance in reducing the risk of HCC development was published in 1995. Ninety HCV-infected subjects, half of whom had undergone antiviral therapy with IFN, were followed-up for 5 years; seventeen of the untreated subjects developed HCC, compared with only 2 of those treated[67]. A subsequent study also reported a significant difference in HCC occurrence between SVR and non-SVR patients (5.1% and 21.8%, respectively; P < 0.001)[48]. A recent meta-analysis including 31528 patients with a median follow-up ranging from 3 years to 8 years demonstrated that SVR is a key factor in reducing the risk of HCC development, since among responders only 1.5% developed tumour lesions compared to 6.2% of non-SVR patients[68]. Moreover, considering only those subjects with advanced fibrosis (F3-F4 according to METAVIR score), the incidence of HCC was 17.9% among non-responders, four times greater than the 4.2% rate reported among responders (P < 0.001).
HCV eradication may also reduce the risk of HCC recurrence after surgical treatment. A 63.4% cumulative recurrence rate has been reported in non-treated patients, compared to 63.2% in treated patients who did not achieve SVR and to 41.7% in the SVR group (non-treated vs SVR, P = 0.008; SVR vs treated without SVR, P = 0.035)[69]. Mazzaferro et al[70] also found SVR as the only factor significantly reducing HCC late recurrence in HCV-pure (hepatitis B anticore antibody negative) patients. A subsequent meta-analysis also reported a reduced rate of early recurrence in 51 patients undergoing surgical resection or percutaneous ablation, reporting a 30% reduction in HCC recurrence rate[71]. In addition, IFN therapy seems to exert beneficial effects, even when started before HCC curative treatments[72].
Although based on heterogeneous studies, these data have raised the issue of the favourable properties of IFN in the prevention of HCC development and recurrence. IFN seems to combine antiviral and antiproliferative effects, such as inhibition of angiogenesis, enhancing of antitumoral immunity and induction of pro-apoptotic boost[70,73]. Recent data have highlighted that IFN may prevent postoperative recurrence of HCC expressing metastatic tumour antigen 1, having 1-year recurrence rate as high as 7% in IFN-treated patients vs 24% in the control group (P < 0.05)[74].
DAAs may likely modulate the expression of genes involved in the production of endogenous IFN. In patients treated with SOF in association with RBV a reduction in types I and II IFN in liver tissue and an increase of IFN-alpha2 have been observed[75]. Conversely, other authors have reported a loss of intrahepatic immune activation by IFN-gamma, associated with normalization of the natural killer cells phenotype and function, consequent to DAAs treatment[76]. How these findings may be associated with DAAs treatment outcome still needs to be further elucidated.
Although the risk of HCC development is significantly reduced by viral clearance it is not completely eliminated, especially in cases of persistence of other cofactors promoting carcinogenesis. Toyoda et al[77] reported that 18/522 patients who achieved SVR after IFN treatment developed HCC after a median follow-up of about 7.2 years (1.0-22.9 years), with an incidence of 1.2% and 4.3% at 5 years and 10 years, respectively. In the analysis, the presence of diabetes mellitus and advanced fibrosis (FIB-4 index ≥ 2) at 24 wk after SVR were correlated to an increased risk of developing HCC. Other data identified type 2 diabetes mellitus and total alcohol intake as independent risk factors for HCC development (HR = 2.77, 95%CI: 2.13-3.60, P < 0.001 and HR= 2.13, 95%CI: 1.74-2.61, P < 0.001, respectively)[78]. In another study, among 232 SVR patients who underwent liver biopsy between 1992 and 2009, the development of HCC was definitively lower in the group with low-intermediate grade fibrosis (F0-F2 according to Metavir) than in that with F3-F4 grade (1.6% and 8%, respectively)[79].
Data about the impact of DAAs treatment on HCC recurrence in previously treated patients and on the development of new HCC nodules have been recently published. It seems to be clear that these new antivirals are not able to modify the natural history of HCC in cirrhotic patients, and it has also been postulated that they may act as promoters, although other studies have not supported this hypothesis[80-87]. Probably, an investigation focused on the immunologic changes and the microenvironmental hepatic tissue alterations consequent to DAAs treatment may be worthwhile to quell this debate[88].
DAAs AND LT
HCV infection-associated cirrhosis and HCC account for 40% of all cases on the LT waiting list in the United States and for about 1/3 of LTs in cirrhotic patients[39,40]. HCV infection recurrence of the graft is universal and leads to cirrhosis in up to 20%-30% of recipients, being one of the most important causes of death and retransplantation[89,90]. The time course of post-LT HCV reinfection is faster than among immunocompetent individuals; cirrhosis can be histologically documented within 5 years after LT, and from that point on the first episode of decompensation may occur within less than 1 year[91].
After HCV infection eradication, a 62%-84% decrease in 5-year mortality as well as a reduction by 90% of the risk of receiving LT have been reported[43]. This improvement in survival was observed in both sustained virological responders and relapsers[92]. The new available DAAs account for response rates higher than 90% and are better tolerated than either IFN and PEG-IFN, allowing for treatment of patients for whom the previous antivirals were contraindicated and who had low chances of response due to unfavourable virological or clinical conditions[93]. As patients who achieve SVR have a reduced risk of progression to cirrhosis and of developing its complications, the widespread use of the new DAAs will probably change the scenario of LT, potentially reducing the need for liver organs.
DAAs treatment before LT
The aim of antiviral treatment in patients on the waiting list is to prevent the recurrence of HCV infection after LT. To reduce the risk of post-LT recurrence, the achievement of at least 30 d of HCV-RNA negativity before LT has been suggested[94,95]. However, whether it is necessary to continue antiviral therapy after LT in patients who received a very short course of therapy before transplantation is not yet clear[96].
Furthermore, achieving SVR in waiting-list patients may directly impact the severity of liver disease, with possible delisting after treatment. A recent real-life multicentre study[97] including 103 decompensated cirrhotic patients listed for LT and treated with second-generation DAAs reported HCV eradication rates of 16% at 24 wk and of 35% at 48 wk after the beginning of treatment (Table 3). This was associated with delisting of 20% of patients at 48 wk from the end of treatment. The evidence of a significant improvement of liver function also comes from the SOLAR-1 study cohort A[98], including cirrhotic patients with decompensated disease treated with LDV and SOF plus RBV. For this study, similar SVR rates (from 86% to 89%) were reported for Child-Pugh class B and C patients regardless of treatment duration, and this was associated with the improvement of model for end-stage liver disease (MELD) and Child-Pugh scores.
Table 3.
Main studies evaluating the effects of direct acting antivirals in patients with advanced cirrhosis and/or listed for liver transplantation
| Ref. | HCV genotype | Fibrosis stage | Treatment | SVR rate | Observed improvement |
| Charlton et al[98], 2015 | Cohort A | Child A: 1/108 (1%) | LDV/SOF + RBV 12 or 24 wk | Child B: | - |
| G1a: 74/108 (68.5%) | Child B: 65/108 (60.2%) | -12 wk 26/30 (87%) | |||
| G1b: 31/108 (28.7%) | Child C: 42/108 (38.9%) | -24 wk 24/27 (89%) | |||
| G4: 3/108 (2.8%) | |||||
| Child C: | |||||
| -12 wk 19/22 (86%) | |||||
| -24 wk 20/23 (87%) | |||||
| Belli et al[97], 2016 | G1a: 20/103 (19.4%) | Child A: 0 | SOF/RBV: 52/103 (50.4%) | SOF/RBV (24-48 wk): RVR 61% | MELD: - 3.4 points |
| G1b: 40/103 (38.8%) | Child B: 46/103 (44.7%) | SOF/LDV ± RBV: 9/103 (8.7%) | EVR 98% | ||
| G2: 3/103 (3%) | Child C: 57/103 (55.3%) | SOF/DCV ± RBV: 35/103 (33.9%) | Child: -2 points | ||
| G3: 20/103 (19.4%) | SOF/SMV ± RBV: 7/103 (6.8%) | SOF + 2nd DAA (12-24 wk): | |||
| G4: 20/103 (19.4%) | RVR 67% | Delisting: 20% | |||
| EVR 98% | |||||
| Improvement in refractory ascites that became treatable with diuretics | |||||
| Munoz et al[107], 2015 | - | Only cirrhosis | SOF/LDV + RBV (12-24 wk): 230 | SVR 84% | MELD: -2.9 + - 0.1 |
| DCV/SOF + RBV (12 wk): 56 | Child B to Child A: 35% | ||||
| GRZ/ELB (12 wk): 27 | Child C to Child B: 48% | ||||
| SOF/LDV/DCV ± RBV (12 wk): 220 | |||||
| Manns et al[101], 2016 | G1a: 50/107 (46.7%) | Child A: 2/107 (2%) | LED/SOF + RBV 12 or 24 wk | genotype 1 | MELD improvement in 72% |
| G1b: 47/107 (43.9%) | Child B: 60/107 (56%) | Child B: 12 wk 20/23 (87%); 24 wk 22/23 (96%) | Child B to Child A: 28% | ||
| G4: 10/107 (9.4%) | Child C: 45/107 (42%) | Child C: 12 wk 17/20 (85%); 24 wk 18/23 (78%), 1/2 (50%) | Child C to Child B: 68% | ||
| Genotype 4 | |||||
| Child B: 12 wk 2/3 (67%); 24 wk 100% | |||||
| Child C: 12 wk 0% | |||||
| 24 wk | |||||
| Poordad et al[100], 2016 | G1a: 34/60 (56.7%) | Child A: 12/60 (20%) | DCV/SOF + RBV 12 or 24 wk | Child A: 11/12 (92%) | MELD improvement in 47% of pts |
| G1b: 11/60 (18.3%) | Child B: 32/60 (53.3%) | Child B: 30/32 (94%) | Child improvement in 60% of pts | ||
| G2: 5/60 (8.3%) | Child C: 16/60 (27.7%) | Child C: 9/16 (56%) | |||
| G3: 6/60 (10%) | |||||
| G4: 4/60 (6.7%) | |||||
| Jacobson et al[99], 2015 | Part 1 | Only Child B cirrhosis | GRZ/ELB 12 wk | SVR 27/30 (90%) | MELD improvement in 11/30 (36.7%) pts |
| G1a: 27/30 (90%) | |||||
| G1b: 3/30 (10%) | |||||
| Curry et al[26], 2015 | G1a: 159/267 (59.6%) | Child A: 16/267 (6%) | SOF/VEL 12 or 24 wk | SOF/VEL 12 wk: 75/90 (83%) | MELD improvement in 51% of pts |
| G1b: 48/267 (18%) | Child B: 240/267 (89.9%) | SOF/VEL + RBV 12 wk | SOF/VEL + RBV 12 wk: 82/87 (94%) | Child improvement in 47% of pts | |
| G2: 12/267 (4.5%) | Child C: 11/267 (4.1%) | SOF/VEL 24 wk: 77/90 (86%) | |||
| G3: 39/267 (14.6%) | |||||
| G4: 8/267 (3%) | |||||
| G6: 1/267 (0.3%) | |||||
| Gray et al[106], 2016 | G1a: 29/101 (28.7%) | Child A: 15/101 (14.8%) | SOF/LDV ± RBV 12 wk | 74.3% | No significant differences from baseline |
| G1b: 19/101 (18.8%) | Child B: 67/101 (66.3%) | Mortality rate 7.9% (6% Child B, 21% Child C) | |||
| G1 (no subtype): 27/101 (26.7%) | Child C: 19/101 (18.8%) | ||||
| G2: 0 | |||||
| G3: 24/101 (23.8%) | |||||
| G4: 1/101 (1%) | |||||
| Mixed: 1/101 (1%) | |||||
| Aquel et al[103], 2015 | G1a: 82/119 (69%) | Child A: 84/119 (70%) | SMV/SOF ± RBV 12 wk | RVR: 82/119 (69%) | MELD improvement in 61/92 (66.4%) pts that achieved SVR 12 |
| G1b: 24/119 (20%) | Child B: 34/119 (29%) | SVR 12: 92/118 (78%; Child A: 83%, Child B: 68%) (1 pts died after achieving SVR4) | |||
| G1 (no subtype): G13/119 (11%) | Child C: 1/119 (1%) | ||||
| Saxena et al[104], 2015 | 1a: 98/160 (62%) | Child A: 101/160 (65%) | SMV/SOF ± RBV 12 wk | Child A (37% with RBV): 91% | No significant differences from baseline |
| 1b: 62/160 (38%) | Child B: 49/160 (31%) | Child B/C (35% with RBV): 73% | |||
| Child C: 6/160 (4%) |
Pts: Patients; LDV: Ledipasvir; SOF: Sofosbuvir; RBV: Ribavirin; DCV: Daclatasvir; SMV: Simeprevir; RVR: Rapid virological response (HCV-RNA < 15 UI after 4 wk of treatment); EVR: Early virological response (HCV-RNA < 15 UI after 12 wk of treatment); GRZ: Grazoprevir; ELB: Elbasvir; VEL: Velpatasvir; FCH: Fibrosing cholestatic hepatitis.
Other studies confirmed liver function amelioration after viral eradication in decompensated cirrhotic patients[26,98-104]; although in cases with more advanced liver impairment (Child-Pugh C, albumin lower than 3.5 g/dL, MELD > 20) and in the elderly worsening of liver function has also been reported[105,106].
Delisting due to clinical improvement may therefore become frequent in the era of DAAs, making it possible to reserve LT only to patients who do not show significant benefit. Munoz[107] estimated that DAAs-induced reduction in MELD score down to the threshold of LT benefit may occur in 592-993 listed patients/year during the first year after treatment, and that approximately 213-515 donated livers/year may become available for redistribution to other patients.
The future impact of DAAs on indications for LT and on organ allocation policy may depend not only on the decreased number of HCV-infected recipients but also on the potential use of anti-HCV positive donors[108]. Indeed, DAAs might introduce a new era, in which anti-HCV positive donors could be reconsidered as a potential source of liver grafts. Moreover, in case of HCV infection transmission from anti-HCV positive donors during LT, it may be easily cured[108]. Recent data suggest that LT outcomes for recipients who accept HCV-positive allografts could be comparable with those of recipients who received HCV-negative allografts[109,110]. Probably, in the future, histological evaluation may become crucial in the choice and the allocation of liver grafts from anti-HCV positive donors, overcoming the issue of previous or active HCV infection. However, these considerations are based on the universal adoption of screening policies for HCV infection, as well as on the widespread use of DAAs for HCV infection treatment, which is still limited by restricted accessibility.
DAAs treatment after LT
DAAs have demonstrated unprecedented results in the treatment of LT recipients (Table 4).
Table 4.
Studies evaluating the effects of direct acting antivirals in liver transplant recipients
| Ref. | HCV genotype | Fibrosis stage | Treatment | SVR12 rate | Observed improvement |
| Charlton et al[98], 2015 | Cohort B | No cirrhosis: 111/229 (48.5%) | LDV/SOF + RBV 12 or 24 wk | No cirrhosis: | - |
| G1a: 164/229 (71.6%) | Child A: 51/229 (22.3%) | 12 wk 53/55 (96) 24 wk 55/56 (98) | |||
| G1b: 63/229 (27.5%) | Child B: 52/229 (22.7%) | Child A: | |||
| G4: 2/229 (0.9%) | Child C: 9/229 (3.9%) | 12 wk 25/26 (96%) | |||
| FCH: 6/229 (2.6%) | 24 wk 24/25 (96%) | ||||
| Child B: | |||||
| 12 wk 22/26 (85%) | |||||
| 24 wk 23/26 (88%) | |||||
| Child C: | |||||
| 12 wk 3/5 (60%) | |||||
| 24 wk 3/4 (75%) | |||||
| FCH: | |||||
| 12 and 24 wk 100% | |||||
| Manns et al[101], 2016 | Cohort B | No cirrhosis: 101/226 (44.7%) | LDV/SOF + RBV 12 or 24 wk | Genotype 1: | MELD improved in 58% |
| G1a: 113/226 (50%) | Child A: 71/226 (31.4%) | No cirrhosis: 12 wk: 42/45 (93%) | |||
| G1b: 86/226 (38%) | Child B: 40/226 (17.7%) | 24 wk: 44/44 (100%) | Child B to A: 52% | ||
| G4: 27/226 (12%) | Child C: 9/226 (4%) | Child A: | Child C to B: 60% | ||
| FCH: 5/226 (2.2%) | 12 wk: 30/30 (100%) | ||||
| 24 wk: 27/28 (96%) | |||||
| Child B: | |||||
| 12 wk: 19/20 (95%) | |||||
| 24 wk: 20/20 (100%) | |||||
| Child C: | |||||
| 12 wk: 1/2 (50%) | |||||
| 24 wk: 4/5 (80%) | |||||
| FCH: | |||||
| 12 and 24 wk: 100% | |||||
| Genotype 4: | |||||
| No cirrhosis: | |||||
| 12 and 24 wk 100% | |||||
| Child A: | |||||
| 12 wk 3/4 (75%) | |||||
| 24 wk 100% | |||||
| Child B: | |||||
| 12 and 24 wk 100% | |||||
| Child C: | |||||
| 12 wk 0% | |||||
| Poordad et al[100], 2016 | G1a: 31/53 (58.5%) | F0: 6 | DCV/SOF + RBV 12 and 24 wk | 50/53 (94%) | - |
| G1b: 10/53 (18.9%) | F1: 10 | ||||
| G2: 0 | F2: 7 | ||||
| G3: 11/53 (20.7%) | F3: 13 | ||||
| G4: 0 | F4: 16 | ||||
| G6: 1/53 (1.9%) | ND: 1 | ||||
| Brown et al[111], 2016 | G1a: 87/151 (57.6%) | Cirrhosis: 97/151 (64.2%) | SMV/SOF ± RBV | 133/151 (88%) | - |
| G1b: 42/151 (27.8%) | SMV/SOF 105/119 (88%) | ||||
| G1 (unspecified): 22/151 (14.6%) | SMV/SOF + RBV 28/32 (88%) |
LDV: Ledipasvir; SOF: Sofosbuvir; RBV: Ribavirin; DCV: Daclatasvir; SMV: Simeprevir; RVR: Rapid virological response (HCV-RNA < 15 UI after 4 wk of treatment); EVR: Early virological response (HCV-RNA < 15 UI after 12 wk of treatment); GRZ: Grazoprevir; ELB: Elbasvir; VEL: Velpatasvir; FCH: Fibrosing cholestatic hepatitis; HCV: Hepatitis C virus.
The SOLAR-1 study, cohort B[98], explored the efficacy of LDV and SOF plus RBV in the treatment of LT recipients without cirrhosis (group 3), with compensated cirrhosis (group 4), and with Child-Pugh B (group 5) and C cirrhosis (group 6). In groups 3 and 4 the SVR rates ranged from 96% to 98% independent of treatment duration; in group 5, SVR was achieved by 86% of patients who received 12 wk of treatment and by 88% of those who received 24 wk of treatment, and group 6, instead, had lower rates of SVR, being 60% and 75% in patients receiving 12 wk and 24 wk of treatment, respectively.
Another study with a similar design, the SOLAR-2, also reported excellent SVR rates in LT recipients with decompensated cirrhosis and genotype 1 or 4 HCV infection treated with LDV and SOF plus RBV for 12 wk or 24 wk[101].
The ALLY-1 and the HCV-TARGET study confirmed good outcomes also for the combination regimens including SMV plus SOF with or without RBV and DCV plus SOF with RBV[100,111].
Although these data may highlight that the achievement of SVR is more difficult in LT cirrhotic patients with more advanced liver impairment, the SOLAR-1 and -2 studies also reported an improvement in MELD and Child-Pugh scores in treated patients[98,101]. This was confirmed by a prospective, multicentre study in patients with post-LT hepatitis C recurrence treated with LDV and SOF plus RBV; the response rate was 96% in Child-Pugh A patients compared to 85% and 65% in Child-Pugh class B and C ones, respectively. However, an improvement in Child-Pugh class and MELD scores was observed in patients with decompensated cirrhosis who achieved SVR12[112].
Therefore, liver function improvement consequent to antiviral treatment will hopefully reduce the need for retransplantation and the morbidity and mortality related to liver dysfunction and liver cirrhosis complications.
HCV INFECTION AND DISEASE-RELATED COMPLICATIONS IN THE FUTURE
The future trend of HCV-related morbidity and mortality in the era of IFN-free antiviral regimens is difficult to predict, although encouraging prospects can be inferred by recent data and projections.
Sievert et al[113] recently analysed the future effects of the increase in SVR rates in the Australian population, taking into account three different models: Without increasing (first scenario) or increasing (second scenario) the number of treated patients and, finally, considering treatment prescription restricted to patients with fibrosis ≥ F3 only (third scenario).
Applying the model of restricted prescription in the time period between 2015 and 2017, an estimated reduction by 51% of HCC development and by 56% and 54% of compensated and decompensated cirrhosis could be expected in 2030, respectively, as well as a 56% decrease in mortality rates. The cumulative costs of HCV infection were reduced by 26% from the base case. If the time span was extended to all years, a 90% decrease in compensated and decompensated liver cirrhotic patients was expected by 2030, with a reduction of HCC by 84%. In absence of eligibility restriction, chronically infected people were estimated to reduce by 60% in 2030, with a slightly lower decrease of cases of cirrhosis and HCC and comparable cumulative costs reduction.
A similar study conducted on the French population analysed the reduction in the need for LT associated with HCV infection treatment. Based on two main scenarios constructed by estimating the number of LT candidates between 2013-2022, the authors demonstrated that antiviral treatments will avoid 4425 transplants, reducing by 45% and by 88% the gap between liver organs request and availability for patients with decompensated cirrhosis and HCC, respectively. This will allow for satisfaction of the LT demand for patients affected by HCC within 2022, although (probably) the same results cannot be achieved for decompensated cirrhotic patients[114].
Finally, Kabiri et al[115] published a transition model analysis to predict the effect of HCV therapies in the United States. Compared to a scenario including new therapies but with limited treatment capacities and risk-based or birth-cohort screening, a scenario with universal screening and absence of treatment limitations was able to prevent 91000 cases of HCC, 128800 cases of decompensated cirrhosis, 153200 liver-related deaths, and 13400 LT. The authors concluded that HCV might be destined to become a rare disease within 2036.
Although the major limitation of these studies is represented by the correct estimation of treatment response rates, as well as by the quantification of treatment costs, which are in constant evolution, they may provide a useful projection of the evolution of HCV-related health and economic burden in the near future.
CONCLUSION
The discovery of DAAs has radically changed the world scene of hepatitis C infection and its associated morbidity and mortality.
The current evolution and revolution of HCV antiviral treatment has increased the number of patients achieving viral eradication and, therefore, is going to reduce the incidence of cirrhosis, the rate of liver decompensation and HCC development, as well as patients’ mortality. This will probably lead to a decrease in the need for LT, providing an adequate supply for nearly all patients with HCC and part of those with decompensated cirrhosis. The future widespread use of these new antivirals might also influence the policy of donor selection, leading to the expansion of the pool of available liver organs, since HCV infection may represent no more a contraindication for the use of liver grafts.
Although DAAs have made it possible to envisage a bright future in the fight against HCV-related liver disease, only long-term follow-up studies will allow for accurate quantification of the benefit obtained. The assessment of less evident effects of the new antivirals, such as microenvironmental and immunologic changes in the liver, is also mandatory to predict and avoid the occurrence of possible unexpected consequences.
Finally, the disparity in the use of DAAs throughout the world caused by the high costs and the restricted availability makes it difficult to draw definitive conclusions about the future epidemiology and evolution of HCV-related liver disease worldwide.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors have no conflict of interest to declare.
Peer-review started: September 3, 2016
First decision: October 20, 2016
Article in press: December 2, 2016
P- Reviewer: Bock T, Bourgoin SG, Pekgoz M, Wang K, Wang L, Yang SS S- Editor: Qi Y L- Editor: Filipodia E- Editor: Li D
References
- 1.European Association for Study of Liver. EASL Recommendations on Treatment of Hepatitis C 2015. J Hepatol. 2015;63:199–236. doi: 10.1016/j.jhep.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden Of Hepatitis C Working Group. Global burden of disease (GBD) for hepatitis C. J Clin Pharmacol. 2004;44:20–29. doi: 10.1177/0091270003258669. [DOI] [PubMed] [Google Scholar]
- 3.Lavanchy D. The global burden of hepatitis C. Liver Int. 2009;29 Suppl 1:74–81. doi: 10.1111/j.1478-3231.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–714. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hoshida Y, Fuchs BC, Bardeesy N, Baumert TF, Chung RT. Pathogenesis and prevention of hepatitis C virus-induced hepatocellular carcinoma. J Hepatol. 2014;61:S79–S90. doi: 10.1016/j.jhep.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58–S68. doi: 10.1016/j.jhep.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Ferri C, Ramos-Casals M, Zignego AL, Arcaini L, Roccatello D, Antonelli A, Saadoun D, Desbois AC, Sebastiani M, Casato M, et al. International diagnostic guidelines for patients with HCV-related extrahepatic manifestations. A multidisciplinary expert statement. Autoimmun Rev. 2016;15:1145–1160. doi: 10.1016/j.autrev.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Younossi Z, Park H, Henry L, Adeyemi A, Stepanova M. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology. 2016;150:1599–1608. doi: 10.1053/j.gastro.2016.02.039. [DOI] [PubMed] [Google Scholar]
- 9.Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Gonçales FL, Häussinger D, Diago M, Carosi G, Dhumeaux D, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975–982. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 10.Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, Goodman ZD, Koury K, Ling M, Albrecht JK. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet. 2001;358:958–965. doi: 10.1016/s0140-6736(01)06102-5. [DOI] [PubMed] [Google Scholar]
- 11.Hadziyannis SJ, Sette H, Morgan TR, Balan V, Diago M, Marcellin P, Ramadori G, Bodenheimer H, Bernstein D, Rizzetto M, et al. Peginterferon-alpha2a and ribavirin combination therapy in chronic hepatitis C: a randomized study of treatment duration and ribavirin dose. Ann Intern Med. 2004;140:346–355. doi: 10.7326/0003-4819-140-5-200403020-00010. [DOI] [PubMed] [Google Scholar]
- 12.Bacon BR, Gordon SC, Lawitz E, Marcellin P, Vierling JM, Zeuzem S, Poordad F, Goodman ZD, Sings HL, Boparai N, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1207–1217. doi: 10.1056/NEJMoa1009482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherman KE, Flamm SL, Afdhal NH, Nelson DR, Sulkowski MS, Everson GT, Fried MW, Adler M, Reesink HW, Martin M, et al. Response-guided telaprevir combination treatment for hepatitis C virus infection. N Engl J Med. 2011;365:1014–1024. doi: 10.1056/NEJMoa1014463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobson IM, McHutchison JG, Dusheiko G, Di Bisceglie AM, Reddy KR, Bzowej NH, Marcellin P, Muir AJ, Ferenci P, Flisiak R, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405–2416. doi: 10.1056/NEJMoa1012912. [DOI] [PubMed] [Google Scholar]
- 15.Poordad F, McCone J, Bacon BR, Bruno S, Manns MP, Sulkowski MS, Jacobson IM, Reddy KR, Goodman ZD, Boparai N, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195–1206. doi: 10.1056/NEJMoa1010494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hézode C, Fontaine H, Dorival C, Zoulim F, Larrey D, Canva V, De Ledinghen V, Poynard T, Samuel D, Bourliere M, et al. Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132–142.e4. doi: 10.1053/j.gastro.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 17.HCV Guidance: Recommendations for Testing, Managing, and Treating Hepatitis C. Available from: http://www.hcvguidelines.org.
- 18.FDA approves Sovaldi for chronic hepatitis C. FDA news release US food and Drug administration, December 6, 2013.
- 19.Sofia MJ, Bao D, Chang W, Du J, Nagarathnam D, Rachakonda S, Reddy PG, Ross BS, Wang P, Zhang HR, et al. Discovery of a β-d-2’-deoxy-2’-α-fluoro-2’-β-C-methyluridine nucleotide prodrug (PSI-7977) for the treatment of hepatitis C virus. J Med Chem. 2010;53:7202–7218. doi: 10.1021/jm100863x. [DOI] [PubMed] [Google Scholar]
- 20.Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, Schultz M, Davis MN, Kayali Z, Reddy KR, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878–1887. doi: 10.1056/NEJMoa1214853. [DOI] [PubMed] [Google Scholar]
- 21.Lawitz E, Sulkowski MS, Ghalib R, Rodriguez-Torres M, Younossi ZM, Corregidor A, DeJesus E, Pearlman B, Rabinovitz M, Gitlin N, et al. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756–1765. doi: 10.1016/S0140-6736(14)61036-9. [DOI] [PubMed] [Google Scholar]
- 22.Afdhal N, Reddy KR, Nelson DR, Lawitz E, Gordon SC, Schiff E, Nahass R, Ghalib R, Gitlin N, Herring R, et al. Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N Engl J Med. 2014;370:1483–1493. doi: 10.1056/NEJMoa1316366. [DOI] [PubMed] [Google Scholar]
- 23.Kowdley KV, Gordon SC, Reddy KR, Rossaro L, Bernstein DE, Lawitz E, Shiffman ML, Schiff E, Ghalib R, Ryan M, et al. Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N Engl J Med. 2014;370:1879–1888. doi: 10.1056/NEJMoa1402355. [DOI] [PubMed] [Google Scholar]
- 24.Sulkowski MS, Gardiner DF, Rodriguez-Torres M, Reddy KR, Hassanein T, Jacobson I, Lawitz E, Lok AS, Hinestrosa F, Thuluvath PJ, et al. Daclatasvir plus sofosbuvir for previously treated or untreated chronic HCV infection. N Engl J Med. 2014;370:211–221. doi: 10.1056/NEJMoa1306218. [DOI] [PubMed] [Google Scholar]
- 25.Foster GR, Afdhal N, Roberts SK, Bräu N, Gane EJ, Pianko S, Lawitz E, Thompson A, Shiffman ML, Cooper C, et al. Sofosbuvir and Velpatasvir for HCV Genotype 2 and 3 Infection. N Engl J Med. 2015;373:2608–2617. doi: 10.1056/NEJMoa1512612. [DOI] [PubMed] [Google Scholar]
- 26.Curry MP, O’Leary JG, Bzowej N, Muir AJ, Korenblat KM, Fenkel JM, Reddy KR, Lawitz E, Flamm SL, Schiano T, et al. Sofosbuvir and Velpatasvir for HCV in Patients with Decompensated Cirrhosis. N Engl J Med. 2015;373:2618–2628. doi: 10.1056/NEJMoa1512614. [DOI] [PubMed] [Google Scholar]
- 27.Poordad F, Hezode C, Trinh R, Kowdley KV, Zeuzem S, Agarwal K, Shiffman ML, Wedemeyer H, Berg T, Yoshida EM, et al. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N Engl J Med. 2014;370:1973–1982. doi: 10.1056/NEJMoa1402869. [DOI] [PubMed] [Google Scholar]
- 28.Zeuzem S, Jacobson IM, Baykal T, Marinho RT, Poordad F, Bourlière M, Sulkowski MS, Wedemeyer H, Tam E, Desmond P, et al. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N Engl J Med. 2014;370:1604–1614. doi: 10.1056/NEJMoa1401561. [DOI] [PubMed] [Google Scholar]
- 29.Lawitz E, Gane E, Pearlman B, Tam E, Ghesquiere W, Guyader D, Alric L, Bronowicki JP, Lester L, Sievert W, et al. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1075–1086. doi: 10.1016/S0140-6736(14)61795-5. [DOI] [PubMed] [Google Scholar]
- 30.Gentile I, Scotto R, Zappulo E, Buonomo AR, Pinchera B, Borgia G. Investigational direct-acting antivirals in hepatitis C treatment: the latest drugs in clinical development. Expert Opin Investig Drugs. 2016;25:557–572. doi: 10.1517/13543784.2016.1161023. [DOI] [PubMed] [Google Scholar]
- 31.Forton DM. How much of a problem is resistance in treating hepatitis C? Curr Opin Infect Dis. 2016;29:625–631. doi: 10.1097/QCO.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 32.Jiménez-Pérez M, González-Grande R, España Contreras P, Pinazo Martínez I, de la Cruz Lombardo J, Olmedo Martín R. Treatment of chronic hepatitis C with direct-acting antivirals: The role of resistance. World J Gastroenterol. 2016;22:6573–6581. doi: 10.3748/wjg.v22.i29.6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Righi E, Londero A, Carnelutti A, Baccarani U, Bassetti M. Impact of new treatment options for hepatitis C virus infection in liver transplantation. World J Gastroenterol. 2015;21:10760–10775. doi: 10.3748/wjg.v21.i38.10760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Szabo SM, Samp JC, Walker DR, Lane S, Cline SK, Gooch KL, Jimenez-Mendez R, Levy AR. Liver-specific case fatality due to chronic hepatitis C virus infection: a systematic review. Ann Hepatol. 2015;14:618–630. [PubMed] [Google Scholar]
- 35.Xu F, Moorman AC, Tong X, Gordon SC, Rupp LB, Lu M, Teshale EH, Spradling PR, Boscarino JA, Trinacty CM, et al. All-Cause Mortality and Progression Risks to Hepatic Decompensation and Hepatocellular Carcinoma in Patients Infected With Hepatitis C Virus. Clin Infect Dis. 2016;62:289–297. doi: 10.1093/cid/civ860. [DOI] [PubMed] [Google Scholar]
- 36.El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999;340:745–750. doi: 10.1056/NEJM199903113401001. [DOI] [PubMed] [Google Scholar]
- 37.Kao JH, Chen DS. Changing disease burden of hepatocellular carcinoma in the Far East and Southeast Asia. Liver Int. 2005;25:696–703. doi: 10.1111/j.1478-3231.2005.01139.x. [DOI] [PubMed] [Google Scholar]
- 38.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szabó E, Lotz G, Páska C, Kiss A, Schaff Z. Viral hepatitis: new data on hepatitis C infection. Pathol Oncol Res. 2003;9:215–221. doi: 10.1007/BF02893380. [DOI] [PubMed] [Google Scholar]
- 40.Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR) J Hepatol. 2012;57:675–688. doi: 10.1016/j.jhep.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 41.Veldt BJ, Saracco G, Boyer N, Cammà C, Bellobuono A, Hopf U, Castillo I, Weiland O, Nevens F, Hansen BE, et al. Long term clinical outcome of chronic hepatitis C patients with sustained virological response to interferon monotherapy. Gut. 2004;53:1504–1508. doi: 10.1136/gut.2003.038257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maruoka D, Imazeki F, Arai M, Kanda T, Fujiwara K, Yokosuka O. Long-term cohort study of chronic hepatitis C according to interferon efficacy. J Gastroenterol Hepatol. 2012;27:291–299. doi: 10.1111/j.1440-1746.2011.06871.x. [DOI] [PubMed] [Google Scholar]
- 43.Hill A. Effects of Sustained Virological Response on the risk of liver transplant, hepatocellular carcinoma, death and re-infection: meta-analysis of 129 studies in 34563 patients with Hepatitis C infection. 65th Annual Meeting of the American Association for the Study of Liver Diseases AASLD. Boston, MA, USA, 2014 Nov 7-11 [Google Scholar]
- 44.Cardoso AC, Moucari R, Figueiredo-Mendes C, Ripault MP, Giuily N, Castelnau C, Boyer N, Asselah T, Martinot-Peignoux M, Maylin S, et al. Impact of peginterferon and ribavirin therapy on hepatocellular carcinoma: incidence and survival in hepatitis C patients with advanced fibrosis. J Hepatol. 2010;52:652–657. doi: 10.1016/j.jhep.2009.12.028. [DOI] [PubMed] [Google Scholar]
- 45.Iacobellis A, Siciliano M, Perri F, Annicchiarico BE, Leandro G, Caruso N, Accadia L, Bombardieri G, Andriulli A. Peginterferon alfa-2b and ribavirin in patients with hepatitis C virus and decompensated cirrhosis: a controlled study. J Hepatol. 2007;46:206–212. doi: 10.1016/j.jhep.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 46.Tada T, Kumada T, Toyoda H, Kiriyama S, Tanikawa M, Hisanaga Y, Kanamori A, Kitabatake S, Yama T, Tanaka J. Viral eradication reduces all-cause mortality in patients with chronic hepatitis C virus infection: a propensity score analysis. Liver Int. 2016;36:817–826. doi: 10.1111/liv.13071. [DOI] [PubMed] [Google Scholar]
- 47.Veldt BJ, Heathcote EJ, Wedemeyer H, Reichen J, Hofmann WP, Zeuzem S, Manns MP, Hansen BE, Schalm SW, Janssen HL. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med. 2007;147:677–684. doi: 10.7326/0003-4819-147-10-200711200-00003. [DOI] [PubMed] [Google Scholar]
- 48.van der Meer AJ, Veldt BJ, Feld JJ, Wedemeyer H, Dufour JF, Lammert F, Duarte-Rojo A, Heathcote EJ, Manns MP, Kuske L, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584–2593. doi: 10.1001/jama.2012.144878. [DOI] [PubMed] [Google Scholar]
- 49.Bruno S, Di Marco V, Iavarone M, Roffi L, Crosignani A, Calvaruso V, Aghemo A, Cabibbo G, Viganò M, Boccaccio V, et al. Survival of patients with HCV cirrhosis and sustained virologic response is similar to the general population. J Hepatol. 2016;64:1217–1223. doi: 10.1016/j.jhep.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 50.Sun M, Kisseleva T. Reversibility of liver fibrosis. Clin Res Hepatol Gastroenterol. 2015;39 Suppl 1:S60–S63. doi: 10.1016/j.clinre.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Iredale JP. Hepatic stellate cell behavior during resolution of liver injury. Semin Liver Dis. 2001;21:427–436. doi: 10.1055/s-2001-17557. [DOI] [PubMed] [Google Scholar]
- 52.D’Ambrosio R, Aghemo A, Rumi MG, Ronchi G, Donato MF, Paradis V, Colombo M, Bedossa P. A morphometric and immunohistochemical study to assess the benefit of a sustained virological response in hepatitis C virus patients with cirrhosis. Hepatology. 2012;56:532–543. doi: 10.1002/hep.25606. [DOI] [PubMed] [Google Scholar]
- 53.Mallet V, Gilgenkrantz H, Serpaggi J, Verkarre V, Vallet-Pichard A, Fontaine H, Pol S. Brief communication: the relationship of regression of cirrhosis to outcome in chronic hepatitis C. Ann Intern Med. 2008;149:399–403. doi: 10.7326/0003-4819-149-6-200809160-00006. [DOI] [PubMed] [Google Scholar]
- 54.Poynard T, McHutchison J, Manns M, Trepo C, Lindsay K, Goodman Z, Ling MH, Albrecht J. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303–1313. doi: 10.1053/gast.2002.33023. [DOI] [PubMed] [Google Scholar]
- 55.Bruno S, Boccaccio V, Russo ML, Maisonneuve P. Is the benefit of treating patients with cirrhosis proven? Liver Int. 2016;36 Suppl 1:21–27. doi: 10.1111/liv.13013. [DOI] [PubMed] [Google Scholar]
- 56.Reichard O, Glaumann H, Frydén A, Norkrans G, Wejstål R, Weiland O. Long-term follow-up of chronic hepatitis C patients with sustained virological response to alpha-interferon. J Hepatol. 1999;30:783–787. doi: 10.1016/s0168-8278(99)80129-9. [DOI] [PubMed] [Google Scholar]
- 57.Arif A, Levine RA, Sanderson SO, Bank L, Velu RP, Shah A, Mahl TC, Gregory DH. Regression of fibrosis in chronic hepatitis C after therapy with interferon and ribavirin. Dig Dis Sci. 2003;48:1425–1430. doi: 10.1023/a:1024196201684. [DOI] [PubMed] [Google Scholar]
- 58.George SL, Bacon BR, Brunt EM, Mihindukulasuriya KL, Hoffmann J, Di Bisceglie AM. Clinical, virologic, histologic, and biochemical outcomes after successful HCV therapy: a 5-year follow-up of 150 patients. Hepatology. 2009;49:729–738. doi: 10.1002/hep.22694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Poynard T, Imbert-Bismut F, Ratziu V, Chevret S, Jardel C, Moussalli J, Messous D, Degos F. Biochemical markers of liver fibrosis in patients infected by hepatitis C virus: longitudinal validation in a randomized trial. J Viral Hepat. 2002;9:128–133. doi: 10.1046/j.1365-2893.2002.00341.x. [DOI] [PubMed] [Google Scholar]
- 60.Shiratori Y, Imazeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, Kuroki T, Nishiguchi S, Sata M, Yamada G, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517–524. doi: 10.7326/0003-4819-132-7-200004040-00002. [DOI] [PubMed] [Google Scholar]
- 61.Pol S, Carnot F, Nalpas B, Lagneau JL, Fontaine H, Serpaggi J, Serfaty L, Bedossa P, Bréchot C. Reversibility of hepatitis C virus-related cirrhosis. Hum Pathol. 2004;35:107–112. doi: 10.1016/j.humpath.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 62.Maylin S, Martinot-Peignoux M, Moucari R, Boyer N, Ripault MP, Cazals-Hatem D, Giuily N, Castelnau C, Cardoso AC, Asselah T, et al. Eradication of hepatitis C virus in patients successfully treated for chronic hepatitis C. Gastroenterology. 2008;135:821–829. doi: 10.1053/j.gastro.2008.05.044. [DOI] [PubMed] [Google Scholar]
- 63.Wanless IR, Nakashima E, Sherman M. Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis. Arch Pathol Lab Med. 2000;124:1599–1607. doi: 10.5858/2000-124-1599-ROHC. [DOI] [PubMed] [Google Scholar]
- 64.Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, Inoue O, Yano M, Tanaka M, Fujiyama S, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med. 1999;131:174–181. doi: 10.7326/0003-4819-131-3-199908030-00003. [DOI] [PubMed] [Google Scholar]
- 65.Yang JD, Roberts LR. Hepatocellular carcinoma: A global view. Nat Rev Gastroenterol Hepatol. 2010;7:448–458. doi: 10.1038/nrgastro.2010.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lemon SM, McGivern DR. Is hepatitis C virus carcinogenic? Gastroenterology. 2012;142:1274–1278. doi: 10.1053/j.gastro.2012.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nishiguchi S, Kuroki T, Nakatani S, Morimoto H, Takeda T, Nakajima S, Shiomi S, Seki S, Kobayashi K, Otani S. Randomised trial of effects of interferon-alpha on incidence of hepatocellular carcinoma in chronic active hepatitis C with cirrhosis. Lancet. 1995;346:1051–1055. doi: 10.1016/s0140-6736(95)91739-x. [DOI] [PubMed] [Google Scholar]
- 68.Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329–337. doi: 10.7326/0003-4819-158-5-201303050-00005. [DOI] [PubMed] [Google Scholar]
- 69.Kanogawa N, Ogasawara S, Chiba T, Saito T, Motoyama T, Suzuki E, Ooka Y, Tawada A, Kanda T, Mikami S, et al. Sustained virologic response achieved after curative treatment of hepatitis C virus-related hepatocellular carcinoma as an independent prognostic factor. J Gastroenterol Hepatol. 2015;30:1197–1204. doi: 10.1111/jgh.12925. [DOI] [PubMed] [Google Scholar]
- 70.Mazzaferro V, Romito R, Schiavo M, Mariani L, Camerini T, Bhoori S, Capussotti L, Calise F, Pellicci R, Belli G, et al. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology. 2006;44:1543–1554. doi: 10.1002/hep.21415. [DOI] [PubMed] [Google Scholar]
- 71.Zhang W, Song TQ, Zhang T, Wu Q, Kong DL, Li Q, Sun HC. Adjuvant interferon for early or late recurrence of hepatocellular carcinoma and mortality from hepatocellular carcinoma following curative treatment: A meta-analysis with comparison of different types of hepatitis. Mol Clin Oncol. 2014;2:1125–1134. doi: 10.3892/mco.2014.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Saito T, Chiba T, Suzuki E, Shinozaki M, Goto N, Kanogawa N, Motoyama T, Ogasawara S, Ooka Y, Tawada A, et al. Effect of previous interferon-based therapy on recurrence after curative treatment of hepatitis C virus-related hepatocellular carcinoma. Int J Med Sci. 2014;11:707–712. doi: 10.7150/ijms.8764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.George PM, Badiger R, Alazawi W, Foster GR, Mitchell JA. Pharmacology and therapeutic potential of interferons. Pharmacol Ther. 2012;135:44–53. doi: 10.1016/j.pharmthera.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 74.Lee D, Chung YH, Kim JA, Park WH, Jin YJ, Shim JH, Ryu SH, Jang MK, Yu E, Lee YJ. Safety and efficacy of adjuvant pegylated interferon therapy for metastatic tumor antigen 1-positive hepatocellular carcinoma. Cancer. 2013;119:2239–2246. doi: 10.1002/cncr.28082. [DOI] [PubMed] [Google Scholar]
- 75.Meissner EG, Wu D, Osinusi A, Bon D, Virtaneva K, Sturdevant D, Porcella S, Wang H, Herrmann E, McHutchison J, et al. Endogenous intrahepatic IFNs and association with IFN-free HCV treatment outcome. J Clin Invest. 2014;124:3352–3363. doi: 10.1172/JCI75938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Serti E, Chepa-Lotrea X, Kim YJ, Keane M, Fryzek N, Liang TJ, Ghany M, Rehermann B. Successful Interferon-Free Therapy of Chronic Hepatitis C Virus Infection Normalizes Natural Killer Cell Function. Gastroenterology. 2015;149:190–200.e2. doi: 10.1053/j.gastro.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toyoda H, Kumada T, Tada T, Kiriyama S, Tanikawa M, Hisanaga Y, Kanamori A, Kitabatake S, Ito T. Risk factors of hepatocellular carcinoma development in non-cirrhotic patients with sustained virologic response for chronic hepatitis C virus infection. J Gastroenterol Hepatol. 2015;30:1183–1189. doi: 10.1111/jgh.12915. [DOI] [PubMed] [Google Scholar]
- 78.Arase Y, Kobayashi M, Suzuki F, Suzuki Y, Kawamura Y, Akuta N, Kobayashi M, Sezaki H, Saito S, Hosaka T, et al. Effect of type 2 diabetes on risk for malignancies includes hepatocellular carcinoma in chronic hepatitis C. Hepatology. 2013;57:964–973. doi: 10.1002/hep.26087. [DOI] [PubMed] [Google Scholar]
- 79.Matsumura H, Nirei K, Nakamura H, Higuchi T, Arakawa Y, Ogawa M, Tanaka N, Moriyama M. Histopathology of type C liver disease for determining hepatocellular carcinoma risk factors. World J Gastroenterol. 2013;19:4887–4896. doi: 10.3748/wjg.v19.i30.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Reig M, Mariño Z, Perelló C, Iñarrairaegui M, Ribeiro A, Lens S, Díaz A, Vilana R, Darnell A, Varela M, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol. 2016;65:719–726. doi: 10.1016/j.jhep.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 81.Conti F, Buonfiglioli F, Scuteri A, Crespi C, Bolondi L, Caraceni P, Foschi FG, Lenzi M, Mazzella G, Verucchi G, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol. 2016;65:727–733. doi: 10.1016/j.jhep.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 82.Yang JD, Aqel BA, Pungpapong S, Gores GJ, Roberts LR, Leise MD. Direct acting antiviral therapy and tumor recurrence after liver transplantation for hepatitis C-associated hepatocellular carcinoma. J Hepatol. 2016;65:859–860. doi: 10.1016/j.jhep.2016.06.023. [DOI] [PubMed] [Google Scholar]
- 83.ANRS collaborative study group on hepatocellular carcinoma (ANRS CO22 HEPATHER, CO12 CirVir and CO23 CUPILT cohorts) Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: Data from three ANRS cohorts. J Hepatol. 2016;65:734–740. doi: 10.1016/j.jhep.2016.05.045. [DOI] [PubMed] [Google Scholar]
- 84.Cheung MC, Walker AJ, Hudson BE, Verma S, McLauchlan J, Mutimer DJ, Brown A, Gelson WT, MacDonald DC, Agarwal K, et al. Outcomes after successful direct-acting antiviral therapy for patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;65:741–747. doi: 10.1016/j.jhep.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 85.Yang JD, Larson JJ, Watt KD, Allen AM, Wiesner RH, Gores GJ, Roberts LR, Heimbach JA, Leise MD. Hepatocellular Carcinoma is the Most Common Indication for Liver Transplantation and Placement on the Waitlist in the United States. Clin Gastroenterol Hepatol. 2016 doi: 10.1016/j.cgh.2016.11.034. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kozbial K, Moser S, Schwarzer R, Laferl H, Al-Zoairy R, Stauber R, Stättermayer AF, Beinhardt S, Graziadei I, Freissmuth C, et al. Unexpected high incidence of hepatocellular carcinoma in cirrhotic patients with sustained virologic response following interferon-free direct-acting antiviral treatment. J Hepatol. 2016;65:856–858. doi: 10.1016/j.jhep.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 87.Cardoso H, Vale AM, Rodrigues S, Gonçalves R, Albuquerque A, Pereira P, Lopes S, Silva M, Andrade P, Morais R, et al. High incidence of hepatocellular carcinoma following successful interferon-free antiviral therapy for hepatitis C associated cirrhosis. J Hepatol. 2016;65:1070–1071. doi: 10.1016/j.jhep.2016.07.027. [DOI] [PubMed] [Google Scholar]
- 88.Llovet JM, Villanueva A. Liver cancer: Effect of HCV clearance with direct-acting antiviral agents on HCC. Nat Rev Gastroenterol Hepatol. 2016;13:561–562. doi: 10.1038/nrgastro.2016.140. [DOI] [PubMed] [Google Scholar]
- 89.Berenguer M. Natural history of recurrent hepatitis C. Liver Transpl. 2002;8:S14–S18. doi: 10.1053/jlts.2002.35781. [DOI] [PubMed] [Google Scholar]
- 90.Berenguer M, Prieto M, San Juan F, Rayón JM, Martinez F, Carrasco D, Moya A, Orbis F, Mir J, Berenguer J. Contribution of donor age to the recent decrease in patient survival among HCV-infected liver transplant recipients. Hepatology. 2002;36:202–210. doi: 10.1053/jhep.2002.33993. [DOI] [PubMed] [Google Scholar]
- 91.Ponziani FR, Gasbarrini A, Pompili M, Burra P, Fagiuoli S. Management of hepatitis C virus infection recurrence after liver transplantation: an overview. Transplant Proc. 2011;43:291–295. doi: 10.1016/j.transproceed.2010.09.102. [DOI] [PubMed] [Google Scholar]
- 92.Ponziani FR, Milani A, Gasbarrini A, Zaccaria R, Viganò R, Iemmolo RM, Donato MF, Rendina M, Toniutto P, Pasulo L, et al. AISF RECOLT C- Group. Treatment of genotype-1 hepatitis C recurrence after liver transplant improves surivival in both sustained responders and relapsers. Transplant Int. 2013;26:281–289. doi: 10.1111/tri.12027. [DOI] [PubMed] [Google Scholar]
- 93.Hüsing A, Kabar I, Schmidt HH, Heinzow HS. Hepatitis C in Special Patient Cohorts: New Opportunities in Decompensated Liver Cirrhosis, End-Stage Renal Disease and Transplant Medicine. Int J Mol Sci. 2015;16:18033–18053. doi: 10.3390/ijms160818033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen T, Terrault NA. Perspectives on treating hepatitis C infection in the liver transplantation setting. Curr Opin Organ Transplant. 2016;21:111–119. doi: 10.1097/MOT.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 95.Curry MP, Forns X, Chung RT, Terrault NA, Brown R, Fenkel JM, Gordon F, O’Leary J, Kuo A, Schiano T, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: an open-label study. Gastroenterology. 2015;148:100–107.e1. doi: 10.1053/j.gastro.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 96.Donato MF, Monico S, Malinverno F, Aghemo A, Maggioni M, Reggiani P, Colombo M. Bridging all oral DAA therapy from wait time to post-liver transplant to improve HCV eradication? Liver Int. 2015;35:1–4. doi: 10.1111/liv.12646. [DOI] [PubMed] [Google Scholar]
- 97.Belli LS, Berenguer M, Cortesi PA, Strazzabosco M, Rockenschaub SR, Martini S, Morelli C, Donato F, Volpes R, Pageaux GP, et al. Delisting of liver transplant candidates with chronic hepatitis C after viral eradication: A European study. J Hepatol. 2016;65:524–531. doi: 10.1016/j.jhep.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 98.Charlton M, Everson GT, Flamm SL, Kumar P, Landis C, Brown RS, Fried MW, Terrault NA, O’Leary JG, Vargas HE, et al. Ledipasvir and Sofosbuvir Plus Ribavirin for Treatment of HCV Infection in Patients With Advanced Liver Disease. Gastroenterology. 2015;149:649–659. doi: 10.1053/j.gastro.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 99.Jacobson I. Efficacy and safety of grazoprevir and elbasvir in hepatitis C genotype 1-infected patients with Child-Pugh class B cirrhosis (CSALT part A) J Hepatol. 2015;62(Suppl 2):S193–S194. [Google Scholar]
- 100.Poordad F, Schiff ER, Vierling JM, Landis C, Fontana RJ, Yang R, McPhee F, Hughes EA, Noviello S, Swenson ES. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology. 2016;63:1493–1505. doi: 10.1002/hep.28446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Manns M, Samuel D, Gane EJ, Mutimer D, McCaughan G, Buti M, Prieto M, Calleja JL, Peck-Radosavljevic M, Müllhaupt B, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis. 2016;16:685–697. doi: 10.1016/S1473-3099(16)00052-9. [DOI] [PubMed] [Google Scholar]
- 102.Lawitz E. SVR12 results from the Phase II, open-label IMPACT study of simeprevir in combination with daclatasvir and sofosbuvir in treatment- naıve and -experienced patients with chronic HCV genotype 1/4 infection and decompensated liver disease. J Hepatol. 2015;62(Suppl 1):227A. [Google Scholar]
- 103.Aquel BA, Pungpapong S, Leise M, Werner KT, Chervenak AE, Watt KD, Murphy JL, Ryland K, Keaveny AP, McLemore R, et al. Multicenter experience using simeprevir and sofosbuvir with or without ribavirin to treat hepatitis C genotype 1 in patients with cirrhosis. Hepatology. 2015;62:1004–1012. doi: 10.1002/hep.27937. [DOI] [PubMed] [Google Scholar]
- 104.Saxena V, Nyberg L, Pauly M, Dasgupta A, Nyberg A, Piasecki B, Winston B, Redd J, Ready J, Terrault NA. Safety and efficacy of simeprevir/sofosbuvir in hepatitis C- infected patients with compesansated and decompensated cirrhosis. Hepatology. 2015;62:715–725. doi: 10.1002/hep.27922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.McCaughan G. The TOSCAR study: sofosbuvir and daclatasvir therapy for decompensated HCV cirrhosis with MELD scores ≥15: what is the point of no return? J Hepatol. 2015;62(Suppl 1):738A. [Google Scholar]
- 106.Gray E, O’Leary A, Stewart S, Bergin C, Cannon M, Courtney G, Crosbie O, De Gascun CF, Fanning LJ, Feeney E, et al. High mortality during direct acting antiviral therapy for hepatitis C patients with Child’s C cirrhosis: Results of the Irish Early Access Programme. J Hepatol. 2016;65:446–448. doi: 10.1016/j.jhep.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 107.Munoz S. Curing decompensated wait-listed HCV patients with the new DAAs: Potential Significant impact on liver transplant wait list and organ allocation. 66th Annual Meeting of the American Association for the Study of Liver Diseases AASLD. San Francisco, USA, 2015 Nov 13-17 [Google Scholar]
- 108.Coilly A, Samuel D. Pros and Cons: Usage of organs from donors infected with hepatitis C virus - Revision in the direct-acting antiviral era. J Hepatol. 2016;64:226–231. doi: 10.1016/j.jhep.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 109.Perumpail RB, Hahambis TA, Aggarwal A, Younossi ZM, Ahmed A. Treatment strategies for chronic hepatitis C prior to and following liver transplantation. World J Hepatol. 2016;8:69–73. doi: 10.4254/wjh.v8.i1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Patwardhan VR, Curry MP. Reappraisal of the hepatitis C virus-positive donor in solid organ transplantation. Curr Opin Organ Transplant. 2015;20:267–275. doi: 10.1097/MOT.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 111.Brown RS, O’Leary JG, Reddy KR, Kuo A, Morelli GJ, Burton JR, Stravitz RT, Durand C, Di Bisceglie AM, Kwo P, et al. Interferon-free therapy for genotype 1 hepatitis C in liver transplant recipients: Real-world experience from the hepatitis C therapeutic registry and research network. Liver Transpl. 2016;22:24–33. doi: 10.1002/lt.24366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Reddy KR. Ledipasvir/Sofosbuvir With Ribavirin for the Treatment of HCV in Patients With Post- Transplant Recurrence: Preliminary Results of a Prospective, Multicenter Study. 65th Annual Meeting of the American Association for the Study of Liver Disease AASLD. Boston, MA, USA, 2014 Nov 7-11 [Google Scholar]
- 113.Sievert W, Razavi H, Estes C, Thompson AJ, Zekry A, Roberts SK, Dore GJ. Enhanced antiviral treatment efficacy and uptake in preventing the rising burden of hepatitis C-related liver disease and costs in Australia. J Gastroenterol Hepatol. 2014;29 Suppl 1:1–9. doi: 10.1111/jgh.12677. [DOI] [PubMed] [Google Scholar]
- 114.Deuffic-Burban S, Mathurin P, Rosa I, Bouvier AM, Cannesson A, Mourad A, Canva V, Louvet A, Deltenre P, Boleslawski E, et al. Impact of emerging hepatitis C virus treatments on future needs for liver transplantation in France: a modelling approach. Dig Liver Dis. 2014;46:157–163. doi: 10.1016/j.dld.2013.08.137. [DOI] [PubMed] [Google Scholar]
- 115.Kabiri M, Jazwinski AB, Roberts MS, Schaefer AJ, Chhatwal J. The changing burden of hepatitis C virus infection in the United States: model-based predictions. Ann Intern Med. 2014;161:170–180. doi: 10.7326/M14-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]


