Abstract
Six evidential sources are examined to investigate how Edwards and Steptoe applied ethical standards to their research leading to the birth of Louise Brown: (i) Their own contemporary writings from 1970 onwards. (ii) Archival evidence from the British Medical Association (BMA), the British Association for the Advancement of Science (BAAS), and correspondence between Edwards and the Ford Foundation. (iii) Minutes of Oldham General Hospital (OGH) Ethics Committee. (iv) Letters by Edwards to prospective patients. (v) oral evidence from interviews with a patient and colleagues. (vi) Evidence from their clinical case management of patients. Taken together these sources suggest that Edwards and Steptoe demonstrated a strong awareness of the ethical issues involved, and offer evidence of honesty to patients about the realistic prospects of success and ethical practice. Nonetheless, decisive evidence that ethical aspirations were put into practice is not available.
Keywords: Edwards and Steptoe, ethics, history, Oldham, test-tube baby
Introduction
Louise Joy Brown was the first child born of an IVF procedure on 25 July 1978 (Steptoe and Edwards, 1978). The recent discovery of research notes from this period amongst the papers of Edwards and at Bourn Hall Clinic has now enabled us to undertake an objective archival-based account of the work that led up to this birth. Our accompanying papers (Elder and Johnson, in 2015-a, Elder and Johnson, in 2015-b, Elder and Johnson, in 2015-c) describe our archival research on the clinical and scientific aspects of the work. In those papers, we show that the numbers of patients and treatment cycles involved was higher than had been known before (Elder and Johnson, 2015b), and we document the evidence underlying the approaches used to try to resolve the many problems encountered (Elder and Johnson, 2015c). Here we describe our research into the ethical aspects of that work which are exclusively the ethics concerning the patients being treated or, at least initially, serving as experimental subjects. Interestingly, at that time, the ethics of researching on human embryos did not feature much, only coming to the fore in the 1980s (Johnson and Theodosiou, 2012, Johnson et al., 2010).
Materials and methods
The data were abstracted from notebooks and loose paper sheets and scraps, anonymised and analysed as described in Elder and Johnson (2015a), which also describes the archival sources used. Briefly, these include archives at the British Medical Association (BMA) and at the National Archive (NA) plus papers among the possessions of the late Edwards and his late wife, Ruth Fowler Edwards, which have been kindly made available to us by his family (RGE). In-text references are indicated by the archive initials plus a reference number and date, and the details for each reference are recorded in the reference list. In addition, scientific papers and the volume A Matter of Life (Edwards and Steptoe, 1980) have been consulted, as described in Elder and Johnson (2015a).
We have interviewed patient Grace McDonald [GM], who volunteered to be interviewed (for transcript see Suppl. Material 1 in Elder and Johnson, 2015b). We felt constrained from approaching other patients by issues of sensitivity and confidentiality; indirect soundings elicited concerns about public exposure, and were therefore not pursued. We have also interviewed three members of staff who were associated with the research in Oldham. We jointly interviewed in person John Webster [JW] and Noni Fallows [NF], and one of us [MHJ] interviewed Sandra Corbett [SC] by telephone (Fig. 1). Edited transcripts of these interviews are available (Supplementary Material 1, Supplementary Material 2), and are referenced by the initials JW, NF or SC followed by the page number(s) referred to. Each of these interviewees has consented to the use in this paper of all information that refers to their transcripts.
Figure 1.
Nursing staff with Patrick Steptoe at Oldham General Hospital, July 1978: (left to right, front row) Edith Astall, Sandra Corbett, Noni Fallows, Sandra Marr, Marjorie Travis, Muriel Harris; (back row) Lorna Jones, Jennifer Thompson, Olga Brewster (Copyright John Fallows Collection, reproduced with permission).
Results and discussion
The data in Elder and Johnson (2015b) make it clear that up to 282 patients were exposed to 457 laparoscopic cycles to produce two live healthy babies. The Medical Research Council (MRC), in declining to fund this work in 1971, cited ethical concerns as major reasons for their decision, in particular the need for more animal and primate research, and concerns about the use of women for “purely experimental purposes” (Johnson et al., 2010). Here we review the evidence that bears on the question: how did Edwards and Steptoe attempt to address the ethical issues confronting them? We have examined six sources of evidence in an attempt to address this question.
Publications by Edwards and Steptoe
Relatively few primary papers from Steptoe and Edwards discuss consent procedures (as was the norm in that period; see Beecher, 1966), but some do. For example, Steptoe and Edwards (1970, p.683) state that they “insisted that all of them [“the volunteer patients”] were referred to us in the normal way through normal medical channels”, and confirmatory evidence of referral by a range of doctors is found in the correspondence in Edwards’ papers (RGE1, 1970–76) and from the interviews (JW, p. 19; SC, p.3). Steptoe and Edwards (1970) also state: “The object of the investigations was fully discussed with the patients, including the possible clinical applications to relieve their infertility” (see later). Perhaps, however, the most useful paper is Edwards’ (1974) discourse entitled ‘Fertilization of Human Eggs in Vitro: Morals, Ethics and the Law’. In this paper, he admits that the MRC had at least a case, saying (p.8): “An immediate issue with new clinical methods concerns the ethics of human experimentation, for if patients are to benefit, new methods have to be perfected, often with the collaboration of people unlikely to gain from the research.”, and later on the same page: “Volunteers who have had a chance of ultimately benefiting from the work have been involved while the methods were being developed.” This section is particularly pertinent given our finding in the dataset we examined that the first 159 laparoscopic cycles (on 97 patients) involved no embryo transfers (Elder and Johnson, 2015b). He then goes on (p.810) to set out the ethical context in which such research should be approached, using for comparison other forms of then novel clinical intervention (e.g. organ transplants, contraceptive and thalidomide use, and ovulation induction). Thus, he first discusses the risks inherent in their work to the “patient volunteers” and concludes that in respect of IVF they are proportionate. He then discusses what research on animal models (including non-human primates) has told us about risks, and concludes that the animal models are reassuring, but that our understanding of human reproduction so outstrips that about other primates, as to render work on the latter unhelpful clinically. There then follows a section on how any pregnancy established by IVF would be monitored for its normality, together with a justification for the research in terms of the enhanced knowledge that would accrue to all aspects of gynaecology.
After this general ethical discourse, Edwards (1974) goes to the nub of the issue: the infertile patients. He discusses, inter alia (p. 1012) the incidence and impact of infertility, the ethical and legal issues and socio-medical outcomes relating to non-IVF treatment approaches (including use of donor eggs, surrogacy, acceptance of infertility, adoption) for various classes of infertility. The most significant part of this section is on page 11: “Patients seeking treatments must be kept fully informed about the methods contemplated and the probability of success,” followed by a discussion about what would now be called autonomy, voluntariness and the capacity of patients to understand the information and to give effective consent to enter experimental research treatment. The infertile patient is returned to on page 19 in a discussion about the ethics of translational research, in which the value of research ethics committees is considered. Overall, this discourse is remarkable for 1974 coming from a scientist, and certainly betrays a great deal of thought by Edwards about the ethical issues raised by medical research. Indeed, it is legitimate to ask whether the MRC response of 1971 was beneficial in stimulating this deep ethical deliberation, which thereafter became a continuing feature of his published work. Thus, 9 out of 56 (16%) of his papers between 1971 (when the first ethico-legal paper was published; Edwards and Sharpe, 1971) and 1978 (the year of Louise Brown’s birth), addressed primarily ethico-legal issues (Gardner and Johnson, 2011), a high proportion for a practicing scientist even today.
However, evidence of ethical interest and understanding is not evidence of ethical practice. Is there evidence that bears on this question? Decisive independent corroborative evidence on this question is difficult to come by, but a wealth of circumstantial evidence bears on this question.
Documentary evidence from the BMA and the Ford Foundation
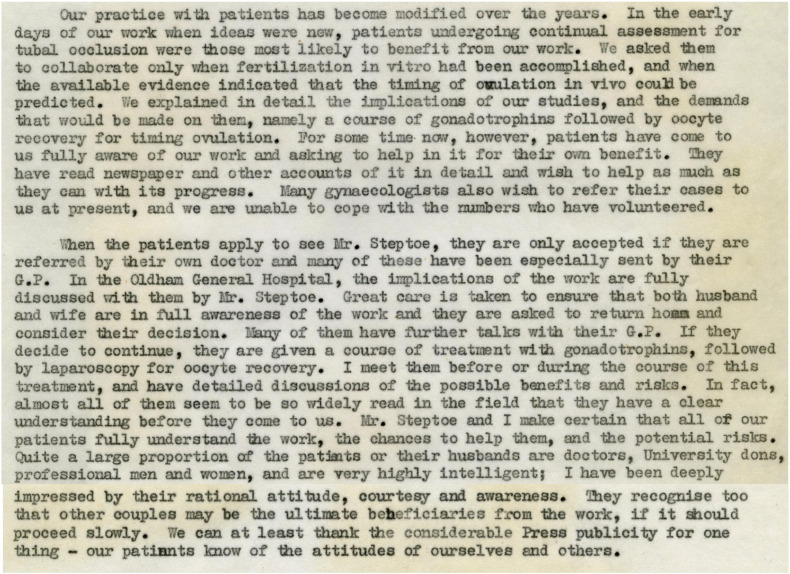
Several documentary sources provide evidence for ‘consistency of story’. Thus, a letter dated 26 May 1972 from Edwards to Richard Mahoney at the Ford Foundation in New York sets out their ethical approach to patients in detail (extract shown in Figure 2; RGE2, 1972). This letter fleshes out the statements made in Steptoe and Edwards (1970, p.7649). Later in this letter, Edwards writes: “we have given evidence to a committee in Professional Standards appointed by the B.M.A. [British Medical Association] … and our work was accepted and approved by them.”
Figure 2.
Extract from a letter dated 26 May 1972 from Edwards to Richard Mahoney at the Ford Foundation in New York (RGE2, 1972).
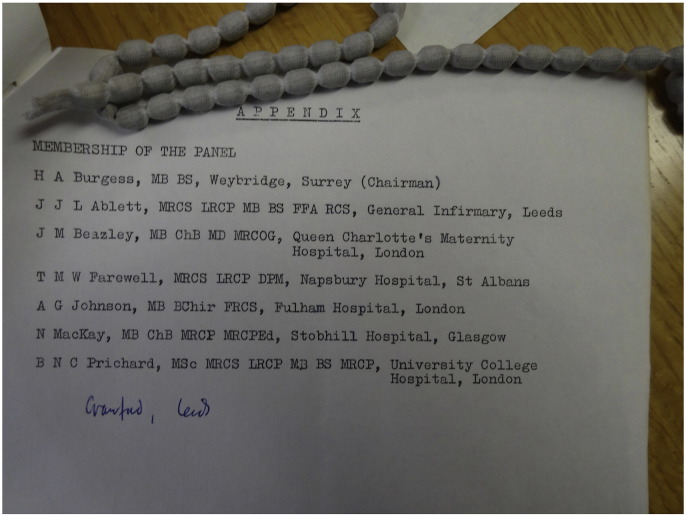
The archives of the BMA reveal that this committee was a ‘Special Panel appointed by the Board of Science and Education’ in April 1970. It was composed of ‘younger doctors’ and charged with identifying ‘areas of anxiety and conscience in medical practice.’ (BMA1, 1972, p.1; membership listed in Figure 3). It held circa-monthly meetings for which Agendas and Minutes are available from 13 October 1970 until 24 June 1971 (but which are missing thereafter), and took evidence on a number of the more controversial areas of medical practice. After each meeting, a draft statement was included with the Minutes, and the final published statement (dated March 1972) contains a section headed ‘In Vitro Fertilisation’ that is broadly supportive of IVF ‘experimental’ research involving patients.
In Vitro Fertilisation
34. Co-operation from patients with problems of infertility will allow clinical experimental research to be undertaken which is designed to help with problems of infertility and also present a deeper understanding of the processes of conception. It is most important that such patients be given detailed explanations of the full procedure and implications before any experimentation involving in vitro fertilization is undertaken. An undertaking should be given to use only the husband’s spermatozoa in the fertilisation of the ova obtained by laparoscopy, and until more information is available the Panel considers that it would be unethical to use a foster [surrogate] uterus.
[Paras. 35–37 go on to express broad approval for preimplantation genetic diagnosis, suggest that the field be kept under review, and propose that the BMA prepares guidelines in the absence of any legislation].
BMA1, 1972, p.9-10, paras 34–37
Figure 3.
Members of the Special Panel appointed by the Board of Science and Education of the British Medical Association in April 1970.
However, this final report differs from earlier drafts, which are far less enthusiastic. Thus, the agenda for the third meeting on the 22 January 1970 included a draft containing the following:
In Vitro Fertilisation: It was felt that a line of research which had dangerous potential was not acceptable and might be unethical. It was not premature to study in vitro fertilisation, but it was thought premature to implant in the human uterus without first having undertaken the experiment in animals and followed through the pregnancy to discover whether defects occurred. Furthermore, it was thought it would be unethical to use a foster uterus, or to put fertilised ova in deep storage. Experimental research of maintaining an embryo in culture was thought to be unacceptable, particularly beyond the stage where organs developed
The general tone was less supportive and did not change substantially in further drafts on the 25 February, 18 March, and 14 April 1971. So what led to the change of both tone and content in the final report a year later (dated March 1972)? The Minutes of the last meeting of the special panel found in the archive are dated the 24 June, 1971, and record:
Resolved; That the SECRETARY enquire into the possibility of the following attending a future meeting of the Panel to discuss the interim statement:-
……
Mr R G Edwards and Mr P C Steptoe (Manchester)
(In Vitro Fertilisation)
No further records are found in the BMA archives, but Edwards’ papers do contain some informative letters (RGE3, 1971). Thus, on 30 June 1971, a letter was sent to Edwards from the committee secretary, Walther Hedgcock, asking if he would be prepared to meet the panel, and saying that Steptoe had also been invited. Edwards replied to say that he was willing but would not be free until November that year. After several exchanges of letters, it seems that the meeting did take place some time in December 1971, as a letter from Hedgcock dated 17 January 1972 was received in response to a complaint from Edwards about the form of the draft Minutes of the meeting. In the absence of any further documentation, one must presume that it was the evidence given by Edwards and Steptoe that swayed the panel members, as suggested by Edwards himself in his letter to Mahoney (see above and RGE2, 1972).
An indication of the form that this evidence might have taken can be gleaned from a set of Minutes of the Working Party set up by the British Association for the Advancement of Science in 1971 to ‘study the scientific, social, ethical and legal implications of recent advances in genetics and biology’. This working group met eight times between the beginning of 1972 and November 1973 and its report was published in 1974 (Jones and Bodmer, 1974). According to the draft Minutes of the meeting on 12 May 1972 (RGE4, 1972), Patrick Steptoe gave evidence orally and (p.6) “outlined what he told patients at the outset of his study of their infertility. He emphasized to them that he cannot guarantee them a baby but the research work carried out might in the future be an indirect benefit to the patient.” This latter reference presumably refers to the fact that many of the women were young and thus might later have children by IVF treatment; indeed we know that women from the Oldham programme were contacted later, in 1980, by John Webster and the administrative secretary at Bourn Hall (JW, p. 29–30), and some of them were treated successfully there (GM, p.24; SC, p. 6). On p.7 (RGE4, 1972), it is recorded “Mr Steptoe emphasised that the patients must be fully informed of the objects of the research being carried out, the methods and the outcome. The patients must also be told of the risks of implantation – in particular … Also the chances of the baby being abnormal must be put to the parents.” Thus, the documentary evidence, although incomplete, is consistent.
Evidence from the records of the Ethics Committee at Oldham General Hospital
Only fragmentary evidence has been found relating to ethical review at Oldham General Hospital over the period 1969–1978. The Area Medical Committee [AMC] Minutes of 23 July 1974 record as Item 6: Research and Ethical Committee – terms of reference and membership.
AGREED to form a Research Committee (Sub-Committee of the AMC) whose remit would include the ethics of research.
Members: 1) Chairman of AMC -Mr PC Steptoe 2) Vice Chairman of AMC -Dr J Wilkinson 3) General Practitioner -Dr EA Creswell 4) Hospital Consultant -Dr G Garrett 5) Area Medical Officer -Dr B Gilbert 6) Lay member -To request AHA [Area Health Authority] for nomination – preferably a solicitor Noted – that where discussions of this committee involve any member, he shall be represented by a deputy.
Dr Janus AGREED to be Mr Steptoe’s deputy. (RGE5, 1974)
Some Minutes of this committee have been found. Thus, on 1 June 1976 Dr G Garrett (Chairman), Dr EA Creswell, Dr B Gilbert, Mr RH Jackson, Mr PC Steptoe, Dr J Wilkinson are reported as being present.
Project No 2
Submitted by:- Mr PC Steptoe, Consultant Obstetrician/Gynaecologist
A request had been received from two research centres in Oxford and Cambridge for collaboration with Oldham for the assessment of human oocytes and embryos. This involved the recovery of oocytes from voluntary patients undergoing laparoscopic sterilisation, as well as those already taking part in the established research programme.
APPROVED (RGE4, 1972)
Likewise on 29 March 1977, when Dr G Garrett (Chairman), Dr EA Creswell, Dr B Gilbert, Mr PC Steptoe, Dr J Wilkinson were present with an apology from Mr RH Jackson.
Project No 2
Submitted by:- Mr PC Steptoe, Consultant Obstetrician/Gynaecologist.
Proposal to explore the storage and re-implantation of Embryos in order to overcome the problem of implantation
Embryos to be obtained after in vitro fertilisation of oocytes with patients with absent or hopelessly diseased tubes.
High failure rate of bringing about successful implantation in the recovery cycle indicates we should store the embryos and implant them following a normal cycle.
The embryo will be handled with strict regard to the ethical considerations and transfers from one patient to another will not be involved.
AGREED subject to the following:-
- (i)
that an independent witness checks the embryos, and
- (ii)
that the case notes should be kept longer than the statutory period: these cases would require longer follow up. [‘5 years’ added by hand with an arrow from statutory period] (RGE5, 1974).
This Minute may refer to the plans to try and freeze embryos in order to overcome the problems encountered when implanting them in a stimulated cycle (see Elder and Johnson, 2015c). Freezing was attempted in June and July of 1977, but never really took off. There are two points to make here, both relating to the farsightedness of Edwards and Steptoe. Thus, it is, to our knowledge, (i) the first time this issue was ever debated, (and it is pertinent to contemporary discussions in clinical IVF; Cohen and Alikani, 2013), as is (ii) the need for witnessing.
Finally, on the 10 October 1977, when Dr G Garrett (Chairman), Mr A Adler, Mr PC Steptoe, Dr J Wilkinson were present with apologies from Dr EA Creswell, Dr B Gilbert
Project No 2
Submitted by:- Mr PC Steptoe, Consultant Obstetrician/Gynaecologist
Work is being carried out on oocyte recovery, in vitro fertilisation and embryo transfer. A number of patients have such serious pathology in the pelvis following previous inflammatory disease, that it is not possible to recover oocytes even though the ovaries are functioning satisfactorily.
It is therefore proposed to carry out transfer of an oocyte from a volunteer donor fertilized by the recipient’s husband’s spermatozoa. This technique is used widely in veterinary practice with great success. Genetically it would be the equivalent [of] artificial insemination by donor of spermatozoa. Genetically the child would have half chromosomes from the donor and half from the husband, but the woman would have the pleasure of pregnancy and delivery.
Ethically there would appear to be no different problem from that of artificial insemination of donor semen which is widely accepted and practised.
AGREED subject to the following:-
- (i)
Genetic screening;
- (ii)
Prospective parents should agree to consider the child as their own;
- (iii)
Medico-legal approval. [‘?’ Added in hand writing] (RGE5, 1974)
As far as we can see from the records available to us, donor oocytes were never used in Oldham. For none of these Minutes is it recorded that Steptoe actually left while his request was being discussed, beyond the record of setting up the committee stating ‘Noted – that where discussions of this committee involve any member, he shall be represented by a deputy”. However, it may be pertinent to record that, although appointed chair of the committee at its foundation meeting, he is not recorded as chairing any of the sessions at which his own work was discussed.
The establishment and use of research ethics committees in the UK only gained currency from 1967 onwards, when it was suggested, but not mandated, that every hospital authority should ensure that all clinical investigations carried out within it are ethical, as ascertained by prior approval from a committee of doctors “including those experienced in clinical investigation” (Hedgecoe, 2009). However, full implementation of even the modest proposals of the Royal College of Physicians was slow, and by the beginning of 1972 only about 70% of non-teaching hospitals (such as Oldham District General Hospital, [ODGH]) had ethics committees, of which only about 20% included a lay member (Hedgecoe, 2009, p. 348–349). Thus, ODGH was part of this changing ethical landscape, albeit towards the tail end, and, when the ethics committee was formed, it did include a lay member and did place conditions on the projects of the clinician/scientist. Moreover, before the ethics committee was formed, it is suggested (JW, p.33) that the hospital board may have functioned as such. In fact, it seems likely to have been the Area Medical Committee, given that the rubric found at beginning of that committee’s Minutes (RGE5, 1974) says “AGREED to form a Research Committee (Sub-Committee of the AMC) whose remit would include the ethics of research”. Indeed, in a copy of page 1 from the Bourn Hall ethics committee dated 26 November 1982 found in the papers of the late Rev Dr Tim Appleton, it is stated that “approval was given by the whole Committee of the Oldham and District Area Health Authority and the Manchester Region Research Committee in 1968 for basic studies on human oocytes … Later, in 1968/69 the committee had accepted that such oocytes could be fertilised in vitro from donor semen, with further assessment for the normality of the resulting embryos.” (MHJ, personal communication).
Letters written by Edwards to prospective patients
In the Edwards archive are carbon copies of over one hundred letters sent by Edwards to people from all continents who had evidently written to him enquiring about treatment (RGE1, 1970–76). Most letters are drafted individually and hand-signed (except when Edwards was away on sabbatical leave from August 1977 and several months thereafter, when his secretary signed them), displaying an extraordinary compassion and care for those receiving them. A feature common to each of these replies is explicit caution against expecting too much, thus: “at present our work is highly experimental… and it is very difficult for us to forecast research work of this nature.”(11September 1970); “I must stress, however, that our work is highly experimental at the moment and it maybe [sic] some time before we are in a position to offer help…” (13 November 1970); “We are still working to try and help people to have their own children and, although we are much closer to success than we were in 1968, there is still some way to go …” (26 January 1973); “Our work must still be considered exploratory …” (15 October 1975); “I must stress that our work is still experimental at present and we can make no promises…” (23 August 1976). These letters do provide strong evidence that patients were informed.
Interview evidence
An interview with Grace MacDonald (formerly Montgomery and mother of Alastair, the second baby born as a result of the Oldham work), is reproduced extensively below to give a feel for the general tone (Suppl. Material 1, Elder and Johnson, 2015b: GM, pp. 11–14):
| MHJ | And did he [PS] explain to you what the programme involved at that point or later? |
| GM | He had explained it very, very clearly the time before, when we’d come down in October to his rooms and he explained the implications that there was no, up till then, had been no success. He was, he was brutally honest. |
| MHJ | He took you through the procedures and so on, did he? |
| GM | Yes. Mm-hmm. |
| MHJ | Yes, and you were happy with all that? |
| GM | Oh, absolutely. |
| MHJ | And the lack of certainty? |
| GM | I’m a great believer in looking on the positive. |
| MHJ | Did you ask him how many people he’d tried to help? |
| GM | No, I didn’t, actually; I just… |
| MHJ | Did he, did he say that? |
| GM | No, he didn’t. I think, he just said that there were other girls on the, on the programme; I’d probably meet some of them and I don’t think, I don't think I even thought to ask. I think, I was just single-mindedly thinking that, you know, it was, this was my chance and that if, you know, if I could, at least, be given this chance, then along with other people, we’d all, you know, we would all be successful. But, I didn’t, actually, think at the time, oh, I wonder how many others? I had, in my own naïve way at that time, I had, kind of, assumed that eventually it would be very successful and there would be lots of, you know, other women trying this and being successful. But we were also told at the time that it would be very, very secret. You know, for the, for the children’s sake. So, I accepted that at face-value that there may be loads of others out there and that we would never know – naïve, or what? |
| KE | No, no. For those days, you were quite right, yes. |
| MHJ | And they explained why they kept it secret, didn’t they? |
| GM | Well, I think, because of that, all the adverse publicity, which was horrible, I mean, how many innovative things have there been in history and nowadays we’ll look back on them and think, what on earth were…? And the same has happened with IVF, hasn’t it, now? How many people are there…? |
| MHJ | But you were aware of the negative… |
| GM | Press, yes. |
| MHJ | Did that cause you any concern? |
| GM | No. Not at all, because I believed totally in… I had met Patrick by that time and I saw what a really nice ethical person he was – very honest, and I trusted him, trusted him implicitly. So, I knew that there wouldn’t be a question of… |
| KE | I know what you mean; you could see that he was a man of integrity. |
| GM | That’s it. Mm-hmm. And then, of course, when I met Bob, that was it. I just realised straight away, what a wonderful person and… |
| MHJ | So, when did you meet Bob? |
| GM | When did I meet Bob? Did I put that down? Right, it would have been ‘15th February 1977’. |
| ………. | |
| MHJ | So that was when you saw Bob, again, at Oldham. Is this at Oldham General, all of this, or…? |
| GM | No, this was, by this time it was - I had the big operation at Oldham General and what also gave me a lot of encouragement was because it was Christmas time, they closed Kershaw’s down, so some of the girls who were at Kershaw’s came into the ward with me, and I, and I’m still in touch with one of the girls; we’re very close friends. And she never did have a baby. But she, they were still at the tail end of the, kind of, month’s cycle to see, you know, they had had the implant done at Kershaw’s, but they were moved up to the main hospital. But, unfortunately, P234 and P233 who were on either side of me… and I didn’t like to ask them; you could see they didn’t want to talk about it, but eventually I went over and said to P233, excuse me asking, but, you know, are you, have you, by any chance, been on a special kind of study with Mr Steptoe and they, kind of, looked and I said, why I’m asking is, I’m now being told that I think I’m going to be accepted on it. So that was all right. So they told… |
| MHJ | And so they took the secrecy thing very seriously? |
| GM | Oh, very, very, uh-huh, and then the funny thing was, P234, who was in the bed next to me, she was back in the next time when I went in and, in February. |
| MHJ | So, February, you met Bob and that was to go in for the first attempt, was it? |
| GM | That was the first attempt. |
| MHJ | Okay, you said that once you met Bob, all your fears disappeared. |
| GM | Oh, totally. |
| MHJ | What was the first meeting like? |
| GM | Well, he was just, he was just so gentle and, again, just so down to earth about it and just explained what was going to be happening; I wasn’t to worry. I would be coming, well, you know, in, coming in, for the blood tests and the carrying round the… |
| KE | The urine samples. |
| GM | Sample bottles, and orange bottles. Plastic orange bottle; and he explained exactly what, you know, what was going to be happening and, but he was just so kind and just, as I said, down to earth about it. Not, you know, he didn’t talk in technical jargon and… |
| KE | Yes, so he wouldn’t talk down to you, would he? |
| GM | Oh, not at all. |
| KE | Never, yes. |
| GM | No, he was, he was just wonderful. |
| MHJ | He just talked conversationally? |
| GM | Yes, just Bob, really. |
| MHJ | And did he explain to you about the chances of success and so on, or…? |
| GM | No, I don't think he really did. He just said that there were quite a few, well, there were quite a few other girls on the programme by this time. There weren’t going to be as many and they did explain that, that time, but he hoped I’d be fine and I know, he was, he said, I know you’re away from home, and then we started talking about Edinburgh, because he’d been up there … |
Further evidence from patients comes from the account published by Lesley and John Brown (Brown and Brown, 1979), in which Lesley recalls (p. 106) after their first consultation that she did not remember “Mr Steptoe saying his method of producing babies had ever worked, and I certainly didn’t ask. I just imagined hundreds of children had already been born through being conceived outside their mothers’ wombs.”, and later on the same page “I wouldn’t have believed it if Mr. Steptoe had told me straight out that, after years of trying, no one had ever had a baby from an implant. My mind was made up. ‘I’ll soon be pregnant now’, I told myself on the train home.” This section, together with later evidence of denial (“You said hundreds of women had had babies like yours” “I made a mistake … I’m the first one”, p.158) in the face of contrary information given by another patient (“Didn’t you hear the nurses say it hadn’t worked on anyone before”, p.111) and a nurse (“Mr Steptoe hasn’t had one success so far”, p.112), illustrates one of the problems confronting Edwards and Steptoe. Thus, the absence of any workable treatment for infertility meant that many patients frequently heard what they wanted to. Indeed Webster said of Lesley Brown: “No, Lesley was a nice lady, but she was… you know, sometimes you were talking to her and you wondered whether it was all going in.” and “Patrick could have said something to her that she just didn’t take on board”. (JW, p.24). However, evidence that they were at least alert to this danger is found in Edwards (1974, p.11), where he says: “It is obviously hard to assess how much some patients understand: in follow-up studies after genetic counseling, one-half of the patients had fully grasped the nature of their problems, and their level of education was a significant factor in comprehension but not in their decision to limit their family…”.
The interview with Noni Fallows (nurse from 1969) and John Webster (doctor from 1974) expands on some of the points raised earlier (Suppl. Material 1). Thus, on patient recruitment (NF/JW, p. 19):
| JW | Via … through Oldham and District, through the Infertility Clinic in Oldham and District General Hospital. He already had a list of infertility patients had there and after he’d met up with Bob and realised there was a chance of this working, he kept a list of patients whom he considered suitable for treatment and whenever Bob decided he would come up to Oldham, usually in the vacations, Patrick’s secretary would pull out these patients’ notes. He’d go through them and she would contact those whom he’d selected. Some of course wanted to come through..... others had given up any idea of becoming pregnant and I suppose some of them had become too old. So that’s how they were recruited. |
| MJ | So they generally tended to be local or were they…? |
| JW | Oh, not at all. No. He used to get people coming from all over. |
| MJ | So they would write to Patrick and he’d put them on the waiting list at Oldham General, would he? |
| JW | Yes. After he’d seen… these are patients he’d seen before. They didn’t just come on the waiting list to have IVF. They were patients he’d personally looked after. |
On counselling and information-giving, neither was able to be very informative. Clearly this was an area that Steptoe handled himself, for example:
| JW | Well, I’m sure Patrick had done that. I mean, I think there was very little said, really, apart from that was an experimental project and we didn’t know… there were no successes. It was sort of, you know, take your chance. (JW, p. 19) |
| and | |
| I think people realised that it was just… the chap was just trying his best and they were grateful to be involved in the programme. I’m sure he explained that, you know, it was… the outcome was probably going to be poor in the majority of cases. And he had no figures to give them, of course, did he? (JW, p. 20) |
A similar response was given by SC (p.36), who nonetheless did say, in response to the question: “they had been told that this was an experimental treatment. You’re sure about that?”, (p. 5): “Yes. Everything was explained to them… [by] Mr. Steptoe. As regards the scientific side Bob Edwards would speak to them” and later, in response to the question (p.6): “what did the patients think in the very early days before replacements were occurring where they were just really trying to perfect the egg recovery technique and get the fertilization and development working, because those patients didn’t have any chance of pregnancy, did they?“, she said, on the basis of having discussed explicitly these issues with patients “They did know that, yes. … I think they were hoping that they would be the one that would be successful.”
These general sentiments echoed those of Noni Fallows (NF, p.23). “They were all just glad to be there, glad that we were there trying to help them.”
It is clear, however, that, typically for that time, no written patient information was provided (NF/JW, p.32), although (NF/JW, p.33): “They would sign a consent form for the laparoscopy procedure, but I don’t think it was detailed information as regards what would happen to… that an oocyte might not be collected or if it was, it was going to be fertilised in vitro.” However the hospital consent forms, along with patient notes appear to have been destroyed (NF/JW, pp. 34–35). Indeed, John Fallows, who up until March 2006 was Head of Medical Illustration at Oldham General Hospital remembers “a memo instructing all heads of departments to destroy any medical records [photographs in his case] that are over 20 [or perhaps 25] years old and are not in current use.” This instruction was presumably a consequence of the Data Protection Act 1998, as similar instructions were issued at other local hospitals.
Evidence from clinical management
It is clear from the notebooks that patient management was approached very cautiously. Thus, we have found no evidence of ovarian hyperstimulation syndrome (OHSS), despite that fact that, as JW said (p.23):
We’d never had any problems with hyperstimulation as far as I’m aware.
and it was an unknown territory because, you know, up to that time HMG [human menopausal gonadotropin] had only been used in anovulatory patients, not in patients who’d been ovulating, so we didn’t really know where we were in terms of dosage.
Likewise, the maximum number of embryos replaced was two (Elder and Johnson, 2015b) such was their concern to avoid multiple pregnancies, a danger which had been foreseen previously by Edwards (1965). In fact, none of the staff can recall any morbidity during their time working there (SC, p.7; JW, p.23).
However, two areas of their clinical practice do give grounds for ethical concern. First, the early experience of an ectopic pregnancy in 1974 meant that all women to be admitted to the programme had to have irreversibly damaged oviducts, and so, to ensure that no other tubal pregnancies occurred, all agreed for safety reasons to having their cornua sealed (JW, p.5):
| JW | where the tubes were hopelessly damaged, we used to seal the cornual ends.… because of Patient 38 in the days in Oldham, who had had an ectopic pregnancy following embryo replacement. She’d had both tubes removed previously, but had a little knob of tube remaining on either side, and unfortunately the embryo gravitated into the cornua |
Whilst understandably in the patients’ interests, this procedure did make some of the nursing staff uncomfortable (NF, p.30–31).
Second, although no paper evidence has come to light, evidence from a filmed interview with Steptoe screened in 1980 (Williams, 1980) reveals that he asked for an assurance from all patients undergoing IVF and embryo transfer that they would permit an amniocentesis on any pregnancy and would agree to a termination if an abnormality was found. That this practice occurred was confirmed by GM in a post-interview follow up.
General discussion
This account is the first to review objectively the ethical evidence concerning the clinical work leading to Louise Brown’s birth. A number of ethical issues are raised by our research, amongst which is the application of 495 potential laparoscopic cycles to 282 patients to produce two live healthy babies, three lost established pregnancies, and perhaps 11 lost early pregnancies (although the evidence for most of these is slim; Elder and Johnson, in 2015-a, Elder and Johnson, in 2015-b, Elder and Johnson, in 2015-c). When, in 1971, the MRC had declined to fund this work, ethical concerns were cited as major reasons for their decision, in particular the need for more animal and primate research, and concern about the use of women for “purely experimental purposes” (Johnson et al., 2010). In this general discussion, we consider the evidence bearing on the ethics of the work in the context of the time.
It is important when reviewing historical events to capture the ethical framework at the time – because ethical values are culturally and temporally located (Ferber, 2013, p.103–105). The early 1970s sit at the cusp of major changes in ethical thinking and practice. Thus, bioethics as a distinct discipline was born in the USA around 1970 (Reich, 1994) and the first institutions devoted to its study (e.g. the Hastings Center and the Kennedy Institute) (Callahan, 1999) were formed in the late 1960s, with the first journals of bioethics appearing in the mid -1970s (RGE6, 1974–75). Only in 1967 in the UK were Ethical Review Committees (ERC) recommended by the Committee on the Ethical Supervision of Clinical Investigations in Institutions (RCP, 1967), cautiously endorsed by the Ministry of Health (MoH, 1968) the following May, suggesting that the primary ethical responsibility lay with the doctor and that the research ethics committees should function more as informal advisory bodies (Hedgecoe, 2009). In the USA, recommendations in favour of Institutional Review Boards (IRB) came even later (NCPHSBBR, 1973). This ‘emergence of bioethics’ as a distinctive element derived from increasing concern amongst the Government, the medical profession and the general public about medical practice and traditional medical ethics, and was aimed initially at protecting the profession by strengthening its ethical backbone (Johnson, in press). These concerns included challenges to medical paternalism and inward-looking professional self-regulation, and an increasingly influential role in medical practice for lay-persons, especially patients (later ‘consumers’) and pressure groups, especially feminist and religious groups. Additional challenges arose from the public exposure of several medical scandals in various parts of the English-speaking world (see Beecher, 1966, Ferber, 2013, Pappworth, 1967, Wilson, 2014). Moreover, the MRC itself did not have a dedicated ethics committee as such, using instead its Clinical Research Board, which lacked lay and non-medico-scientific members (Johnson et al., 2010). Thus, Edwards and Steptoe were sailing in relatively uncharted, if turbulent, ethical waters. However, Edwards read and thought deeply about the ethical implications of their work and, as his many contemporary and subsequent publications show, he became something of a bioethical expert himself. Within this general framework, what can be concluded from the evidence available?
First, it is important to dissect out the two classes of patient involved. Initially patients did not benefit directly from the research. Thus, from 1969 to December 1971, before embryo transfers were attempted and when egg recovery, fertilization and in-vitro culture were being perfected, 169/520 (32%) of the recorded procedures and 106/282 (38%) of the identified patients were included. However, only 97 (34%) of these patients were actually scheduled for and underwent laparoscopy, and so they were ‘experimental subjects’, as the MRC had claimed. Moreover, 76 of them (27%) did not subsequently undergo embryo transfer attempts in Oldham up to 1978. Edwards (1974) admits this point, but, unlike the MRC, did not see this as a necessary impediment to patient involvement, as long as criteria relating to information, voluntariness and consent were met. It would have been open to the MRC to fund the work, placing ethical conditions on Edwards and Steptoe. Indeed, the initial decision of the MRC in 1970 to offer positions to both of them at the MRC Clinical Research Centre at Northwick Park (Johnson et al., 2010, p.2162), suggests that such a route may have been contemplated initially. The remainder and majority of the patients, for whom transfers were intended, were ‘undergoing experimental treatment’. However, the low priority accorded to infertility compared with that given to the ‘population problem’ by the referees of their subsequent grant application effectively sunk this possibility: IVF did not appear to offer to these sceptics a credible solution to a real enough problem as to be justified ethically. So one is forced to examine the evidence regarding how Edwards and Steptoe assessed the relative risks and benefits of the research, as they were then perceived.
The MRC had suggested that research on animals, and in particular on primates, was required before the risk of applying the technology to humans could be justified (Johnson et al., 2010, p.2167). In a contemporary report on a CIBA foundation meeting examining inter alia legal aspects of embryo transfer, Mclaren and Parkes (1973) state: “Thousands of transfers of fertilized eggs from one female mammal to another … have failed to demonstrate adverse effects on the progeny.”, and go on to say that biologically, there are few grounds for concern about egg transfer in humans. Edwards himself (1974, p.4), based on his considerable experience of the impact of ‘aberrant’ genetic make-up of early animal embryos on live birth outcomes (Johnson, 2011, p.248–9), expressed firm, but cautious, optimism about Nature’s facility at filtering out early errors. It may also appear puzzling from our present ethical perspective that the MRC suggested use of primates in research. However, at that time the same level of ethical concern about their use did not exist as it does now. Thus their use in the UK was governed by the 1876 Cruelty to Animals Act until 1986 when the Animals (Scientific Procedures) Act came into effect (Radford, 2001). The 1876 Act did not mention primates; indeed the genesis of the Act was stimulated more by concern about the welfare of cats, dogs and horses than monkeys. The MRC’s suggestion was also ill-advised for several reasons, all of which were advanced by Edwards and Steptoe in their response to the MRC rejection. They drew attention to the lack of general agreement among experts on the value of primates as human models, as well as on what a good ‘primate model’ might be, supporting their view by the relative absence of research on primates prior to human trials in other areas of medicine. They also pointed out how little was known about primate early pregnancy compared with that in humans, and that primate size and anatomy rendered laparoscopic oocyte recovery and trans-cervical embryo transfer impossible (Edwards, 1974, NA1, 1971). Nonetheless, and possibly in response to the MRC suggestion, Edwards did evidently attempt in 1972 to achieve IVF and embryo transfer in super-ovulated rhesus monkeys in collaboration with John Marston, but without success (RGE7, 1972). Thus, both the evidence and the informed contemporary view did not support this line of risk attribution taken by the MRC.
Perhaps more serious was the other major risk raised, namely the potential damage to patients caused by laparoscopic egg recovery. However, we have found no evidence of any mortality or serious physical morbidity from laparoscopic egg recovery and embryo transfer performed by Steptoe over the period 1969 to 1978. Indeed, the approach taken clinically was very cautious, in respect of both avoidance of OHSS and of multiple pregnancy. Thus for both the major ethical risks raised by the MRC, the risk:benefit ratio does not seem to have favoured risks over benefits at the time, regardless of the benefits in the longer term.
It is useful to contextualise IVF by considering ethical discourses surrounding other experimental treatments being developed at or shortly before that time, of which kidney and heart transplants are perhaps the best studied. Both involved patients who were approaching death, and in whom desperation was even more extreme than those who could not conceive. In 1970, the Eighth Human Kidney Transplant Register is quoted in Fox and Swazey (1974, p.76) as reporting that of 3645 patients who had received kidney transplants (of which 40% had been performed within the previous 12 years), only 52% of those receiving cadaveric kidneys were alive after 1 year and 41% after 2 years, with equivalent figures for consanguinous donors of 78% and 75%, respectively. Moreover, only 66% of those surviving after 1 year were rated ‘completely normal’ in their renal functions. This situation was the case in 1970 when 150 centres were performing kidney transplants (p. 74), some 20 years after the first had been attempted (p.7071). By any stretch of the imagination this procedure was still experimental, or, as Fox and Swazey (p.75) describe it, post-experimental/pre-therapeutic. Whilst for heart transplants, which had first been attempted only in 1967, the National Heart Institute’s summary for 1970 (p.77) records only 22/165 survivors, of which only 2 had survived more than 2 years, and half had not survived longer than 18 months. Fox and Swazey (p.83) conclude that heart transplants constitute “scientific investigation” but not accepted therapy, and that ‘guidelines’ be recommended on the proper treatment of donors and recipients. These discussions were occurring concurrent with those in which Edwards and Steptoe were engaging, and of which the two of them were certainly aware from their involvement in the Working Party set up by the British Association for the Advancement of Science in 1971 (Jones and Bodmer, 1974). They give a useful comparative perspective that may have suggested to the two IVF pioneers that they were behaving ethically by the standards of the time.
So can we reach any firm conclusions about how ethically Edwards and Steptoe approached their research between 1969 and 1978? Ferber (2013, p.127130), in her discussion on how to interpret historically the ethical aspects of human experimentation, lists a number of ways of assessing the ethicality of research. She starts by asserting that the very nature of modern medicine demands a risk-benefit analysis, and then goes on to analyse those conditions historically that have led to the elevation of risk or benefit respectively. We will use these conditions as a useful template for our final analysis, starting with those she associates with benefit elevation and then with the elevation of risk.
She asserts that ethical behavior is encouraged by openness, by the exposure of research work in the medical and mainstream literature, as well as by the introduction of guidelines and review processes, both professionally and by the state. Edwards and Steptoe published their results in great detail in a range of highly accessible medical and scientific journals (Elder and Johnson, in 2015-c, Gardner and Johnson, 2011). Moreover, Edwards was criticized widely from the mid 1960s for his use of the media to discuss his research publicly (Johnson et al., 2010, p.2166) and rarely shrank from engaging in any professional or public debates (Edwards and Sharpe, 1971, Johnson et al., 2010). Both Edwards and Steptoe also, as we have seen, engaged with both the BMA and the BAAS with supportive outcomes. Their attempts to engage the MRC in dialogue were closed down by the MRC itself, thereby depriving the MRC of the chance to engage actively in the ethics of MRC for at least 10 years (Johnson et al., 2010). Thus, Ferber’s historical conditions for elevating benefit seem to have been met by the two IVF pioneers as far as society allowed.
What about the conditions that elevated risk historically? First, Ferber asserts that rarely is the doctor found to be acting consciously in a malign or evil way: there is no evidence that either of these attributes applied to Edwards and Steptoe. Second, her analysis suggests that the prevailing culture encouraged or permitted unethical behaviour: there is little evidence to support this applying nationally to Edwards and Steptoe, and much against it (Johnson et al., 2010). However, there is some evidence of a possible micro-culture of permission within the ambit of Oldham General Hospital, where Steptoe clearly wielded considerable influence and authority as the senior consultant, and was perceived as being ‘very charismatic’ (NF, p.5). This charisma does raise an issue related to authority that could compromise patient autonomy, namely trust. Thus, any relationship between doctor and patient must be based on trust and, paradoxically, the more trustworthy the patient’s perception of the doctor, the greater will his or her authority be over the patient. It is clear from such evidence that we have that Steptoe was perceived as being very trustworthy (e.g. GM, p.12). We have little evidence that he abused that trust, other than perhaps his insistence on an amniocentesis and a termination if the fetus was abnormal. Such an agreement, presumably, was put in place primarily to protect the programme’s reputation rather than the patients’ interests, but was legally unenforceable. Whether Steptoe’s combination of authority, charisma and trust-worthiness was sufficient to offset the massive ethical scrutiny and criticism to which their work was being subjected elsewhere, together with the wide-spread prejudice against fertility restoration at that time, must be considered doubtful. Indeed, we have oral evidence that he was well aware of the need to remain within ethical bounds (NF in respect of ethics, p.32): “was always referring to the medical research council – how we had to be very careful as funding had been refused”. Moreover, although initially at least he chaired the ethics committee (in 1974) by 1976 Steptoe was not in the chair, and, moreover, the committee did impose restrictive conditions when giving permissions on at least two occasions (29 March 1977, 10 October 1977).
Third, Ferber lists the possibility of ‘getting away’ with the work because its subjects were so vulnerable. Vulnerable the patient volunteers certainly were – not just because many of them, as remains the case today (Everywoman, 2013), were described as being ‘desperate’ (see NF, p.9. “Yes. They had desperation in their eyes, didn’t they, John?”), and had been turned away ‘empty wombed’ by other specialists, but also because for many of them their infertility and attempts at treatment were a secret, kept from even their families. Moreover, Steptoe did insist that they kept their treatment at the clinic secret (Suppl. Info 1, Elder and Johnson, 2015b: GM p.13; Brown and Brown, 1979) – not for any malign purpose but to prevent them from being hounded by the press (as he explained in 1971 in his evidence to the BAAS committee: RGE4, 1972; see also Steptoe, 1978). However, Steptoe would only take patients referred by another doctor, and we have no evidence to suggest that any were pressured into treatment: hence, Noni Fallows’ perception (NF, p.23) “They were all just glad to be there, glad that we were there trying to help them.” and Sandra Corbett’s similar response.
The issue of whether consent can truly be given freely and informed when patients are ‘desperate’ is much discussed (see Archard, 2008, Scott, in press, Scott et al., 2012). It is reasonable to conclude, from empirical evidence presented by Scott albeit in the related context of egg sharing, that most of the patients who volunteered to undergo ‘experimental IVF’ did so primarily in the hope of becoming pregnant but secondarily with an altruistic aim of ‘advancing knowledge and thereby helping others’ (see also Suppl. Info 1, Elder and Johnson, 2015b: GM pp.30–31). So, the question is, given that there was no relevant statute law in place at the time, did the women on the programme consent to their treatment validly under the common law requirements of capacity, information as to nature and purpose, and voluntariness? We have little direct evidence on this question, as we are constrained by confidentiality from contacting any of the patients identified in the records. However, it seems unlikely that capacity was an issue, and we have written and, albeit very limited, oral evidence of information being given. The common-law position on voluntariness derives from case law concerning ‘a patient’s will being overborne in some way’ (Scott, in press). In the main case law on this matter, the Court of Appeal ‘explored the notion of undue influence and the way it might negate voluntariness, analysing the effect of influence with reference to three factors: namely, the strength of will of the patient (for instance if tired or in pain s/he may be less able to resist); the relationship between the persuader and the patient; and the types of arguments used.’ (Scott, in press). The overall conclusion from this and one other example from case law is that it ‘is not easy to prove that voluntariness is negated by undue influence in the treatment context,’ (Scott, in press). Moreover, both these key cases occurred in 1992 and 2002, long after the period in question. Finally, were some IVF patients to have perceived themselves to have been pressured by Steptoe or Edwards (and we have no evidence that any of them did have such perceptions), was it likely to have been due to misunderstanding of, or to malign intent on the part of, Steptoe and Edwards? We cannot answer this question, as we do not have the evidence to do so.
A fourth condition suggested by Ferber was the hope of making money or getting grants: palpably not applicable in this case (Johnson and Elder, in 2015-a, Johnson and Elder, in 2015-b, Johnson et al., 2010). A fifth condition was the desire for professional advancement and recognition. This condition certainly has a ring of truth for Steptoe, who felt keenly his lack of recognition as a clinician and pioneer of laparoscopy (Edwards, 1996). However, for Edwards, who already had a Cambridge University position and an internationally distinguished reputation, which even the MRC had admitted (Johnson et al., 2010), his very work on IVF had put this reputation at considerable risk (Johnson, 2011).
The final condition that historically was identified by Ferber as contributing to unethical practice was ‘the attraction of having done good as one perceives it’ leading to ‘over enthusiasm’. It is certainly the case that both Edwards and Steptoe were deeply committed to helping the infertile: the latter since many years (Edwards, 1996) and the former, not only in his foresighted Lancet paper of 1965 (Edwards, 1965), but also as part of his larger liberal vision, as articulated frequently from as early as 1971 (Edwards and Sharpe, 1971, p.90): “The lobbyists for reform in the laws of drug and alcohol addiction, abortion, and sexual behaviour have achieved much public approval in their areas of concern”. Thus there is no doubting their mutual enthusiasm and commitment to helping the infertile. The question is: did that lead them to go to too far or too fast, as was indeed suspected by some of their peers at the time (Johnson et al., 2010)? The evidence suggests that they did at least strive to act ethically.
The following are the supplementary data related to this article.
Edited transcript of interview with Noni Fallows and John Webster conducted at Bourn Hall on 19 May 2014.
Edited transcript of interview with Sandra Corbett conducted by phone on 26 June 2014.
Acknowledgement
The research was supported by grants from the Wellcome Trust (088708, 094985 and 100606), which otherwise had no involvement in the research or its publication. We thank Rosamund Scott and members of the Cambridge ReproSoc group for their helpful comments on a draft of this paper, and John Fallows for allowing us to quote him and for permission to use one of his photographs.
Biography
Martin H Johnson FRCOG, FMedSci, FRS is Emeritus University Professor of Reproductive Sciences and fellow of Christ’s College, Cambridge, and Honorary Academic Fellow of St Paul's College, Sydney University. In 2014 he was awarded the Marshall medal by the Society for Reproduction and Fertility, and was elected an Honorary Member of the Physiological Society. He is author of Essential Reproduction (seventh edition, Wiley Blackwell, January 2013), co-editor of Sexuality Repositioned (2004), Death Rites and Rights (2007) and Birth Rites and Rights (2011), and has authored over 300 papers on reproductive and developmental science, history, ethics, law and medical education.
Contributor Information
Martin H. Johnson, Email: mhj21@cam.ac.uk.
Kay Elder, Email: kay.elder@bourn-hall.com.
References
- Archard D. Informed Consent: Autonomy and Self-Ownership. J. Appl. Philos. 2008;25:19–34. [Google Scholar]
- Beecher H.K. Ethics and Clinical Research. N. Engl. J. Med. 1966;274:1354–1360. doi: 10.1056/NEJM196606162742405. [DOI] [PubMed] [Google Scholar]
- BMA1 . 1972. Professional Standards: A statement prepared by a Special Panel appointed by the Board of Science and Education of the British Medical Association. (B/35/3/38) [Google Scholar]
- BMA2 . 1970. Agenda for 3rd meeting Pr. St. (BS) 11. Item 9 “Consider: Draft memorandum on Professional Standards for submission to the Board of Science and Education (Doc. Pr. St. (BS) 12 - herewith)”. (22 January 1970) [Google Scholar]
- BMA3 . 1971. Minutes (PrSt (BS) 25 1970–71) (Minute 63, page 2) (24th June 1971). [Google Scholar]
- Brown L., Brown J. The Leisure Circle, Ltd.; Wembley, UK: 1979. Our miracle called Louise. A parents’ story. [Google Scholar]
- Callahan D. The Hastings Centre and the early years of bioethics. Kennedy Inst. Ethics J. 1999;9(1):25–51. doi: 10.1353/ken.1999.0001. [DOI] [PubMed] [Google Scholar]
- Cohen J., Alikani M. The time has come to radically rethink assisted reproduction. Reprod. BioMed. Online. 2013;27:323–324. doi: 10.1016/j.rbmo.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Edwards R.G. Maturation in vitro of human ovarian oocytes. Lancet. 1965;ii:926. doi: 10.1016/s0140-6736(65)92903-x. [DOI] [PubMed] [Google Scholar]
- Edwards R.G. Fertilization of Human Eggs in Vitro: Morals, Ethics and the Law. Q. Rev. Biol. 1974;49:3-26.s. doi: 10.1086/407901. [DOI] [PubMed] [Google Scholar]
- Edwards R.G. Patrick Christopher Steptoe, C. B. E. 9 June 1913–22 March 1988. Biogr. Mem. Fellows R. Soc. 1996;42:434–452. [PubMed] [Google Scholar]
- Edwards R.G., Sharpe D.J. Social values and research in human embryology. Nature. 1971;231:87–91. doi: 10.1038/231087a0. [DOI] [PubMed] [Google Scholar]
- Edwards R.G., Steptoe P.C. Hutchinson; London: 1980. A Matter of Life. The Story of IVF - a Medical Breakthrough. [Google Scholar]
- Elder K., Johnson M.H. The Oldham Notebooks: an analysis of the development of IVF 1969–1978. I. Introduction, Materials and Methods. Reproductive BioMedicine and Society Online. 2015;1:3–8. doi: 10.1016/j.rbms.2015.04.001. (in this issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder K., Johnson M.H. The Oldham Notebooks: an analysis of the development of IVF 1969–1978. I!. The treatment cycles and their outcomes. Reproductive BioMedicine and Society Online. 2015;1:9–18. doi: 10.1016/j.rbms.2015.04.003. (in this issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder K., Johnson M.H. The Oldham Notebooks: an analysis of the development of IVF 1969–1978. I!I. Variations in procedures. Reproductive BioMedicine and Society Online. 2015;1:19–33. doi: 10.1016/j.rbms.2015.04.004. (in this issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everywoman J. Cassandra’s prophecy: why we need to tell the women of the future about age-related fertility decline and ‘delayed’ childbearing. Reprod. BioMed. Online. 2013;27:4–10. doi: 10.1016/j.rbmo.2013.03.023. [DOI] [PubMed] [Google Scholar]
- Ferber S. Palgrave MacMillan; UK: 2013. Bioethics in historical perspective. [Google Scholar]
- Fox R.C., Swazey J.P. University of Chicago Press; London and Chicago: 1974. The courage to fail. [Google Scholar]
- Gardner R.L., Johnson M.H. Bob Edwards and the first decade of Reproductive BioMedicine Online. Reprod. BioMed. Online. 2011;22:106–124. doi: 10.1016/j.rbmo.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Hedgecoe A. A form of practical machinery: The origins of research ethics committees in the UK, 1967–1972. Med. Hist. 2009;53:331–350. doi: 10.1017/s0025727300000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H. Robert Edwards: the path to IVF. Reprod. BioMed. Online. 2011;23:245–262. doi: 10.1016/j.rbmo.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H. Regulating reproduction: Custom and Law in the 19th and 20th Centuries. In: Hopwood N., Flemming R., Kassell L., editors. Cultures of reproduction from antiquity to the present day. Cambridge University Press; 2015. (in press) [Google Scholar]
- Johnson M.H., Elder K. The Oldham Notebooks: an analysis of the development of IVF 1969–1978. V. The role of Jean Purdy reassessed. Reproductive BioMedicine and Society Online. 2015;1:46–57. doi: 10.1016/j.rbms.2015.04.005. (in this issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Elder K. The Oldham Notebooks: an analysis of the development of IVF 1969–1978. VI. Sources of support for, and expenditure on, the work. Reproductive BioMedicine and Society Online. 2015;1:58–70. doi: 10.1016/j.rbms.2015.04.006. (in this issue) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M.H., Theodosiou A.A. PGD and the making of the ‘genetic embryo’ as a political tool: A historical analysis. In: McLean Sheila., editor. Regulating PGD: A Comparative and Theoretical Analysis. Routledge; 2012. pp. 39–70. [Google Scholar]
- Johnson M.H., Franklin S.B., Cottingham M., Hopwood N. Why the Medical Research Council refused Robert Edwards and Patrick Steptoe support for research on human conception in 1971. Hum. Reprod. 2010;25:2157–2174. doi: 10.1093/humrep/deq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A., Bodmer W.F. Oxford University Press; Oxford: 1974. Our future inheritance: choice or chance? [Google Scholar]
- McLaren A., Parkes A.S. Legal and other aspects of artificial insemination by donor. J. Biosoc. Sci. 1973;5:205–208. doi: 10.1017/s0021932000009135. [DOI] [PubMed] [Google Scholar]
- MoH . 1968. Ministry of Health, Supervision of the ethics of clinical investigations, 1968, HM68(33) [Google Scholar]
- NA1 . 1971. Letter from Edwards and Steptoe to MRC, 11 June 1971: NA FD 10/161. [Google Scholar]
- NCPHSBBR . National Research Act, § 202(a)(2) 1973. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. [Google Scholar]
- Pappworth M.H. Routledge and Kegan Paul; London: 1967. Human Guinea-Pigs. [Google Scholar]
- Radford M. Oxford University Press; Oxford: 2001. Animal Welfare Law in Britain: Regulation and responsibility. (Chapter 3) [Google Scholar]
- RCP . RCP; London: 1967. Royal College of Physicians of London, Report of the Committee on the supervision of the ethics of clinical investigations in institutions; p. 4. [Google Scholar]
- Reich W.T. The word “bioethics”: its birth and the legacy of those who shaped it. Kennedy Inst. Ethics J. 1994;4(4):319–350. doi: 10.1353/ken.0.0126. [DOI] [PubMed] [Google Scholar]
- RGE1 . Patient Matters Box 1. 1970–76. Carbon copies of letters to Doctors and Patients. [Google Scholar]
- RGE2 . 1972. Letter dated 26th May 1972 from Edwards to Richard Mahoney at the Ford Foundation in New York. Copy supplied personally to MHJ by Professor Edwards from his private papers in 2012, but no longer available for transfer to the archive. [Google Scholar]
- RGE3 . Vol. 16. 1971. Letters concerning evidence to BMA committee and an associated lecture. (Data, journals and papers Folder). [Google Scholar]
- RGE4 . Vol. 10. 1972. Draft minutes for May 12th 1972 of the Working Party of the British Association for the Advancement of Science. (Data, journals and papers Folder). [Google Scholar]
- RGE5 . 1974. Minutes of the ODGH ethical review committee dated 23rd July 1974, 1st June 1976, 29 March 1977, and 10th October 1977. (Acc 1601 Box 3) [Google Scholar]
- RGE6 . Vol. 18. 1974–75. Letters (dated 1974/5) concerning the foundation of a new ethics journal between RGE and Excerpta Medica North Holland; did not go ahead as was preempted by BMA’s Journal of Medical Ethics in 1975. (Data, journals and papers Folder). [Google Scholar]
- RGE7 . Vol. 13. 1972. Data sent to RGE by John Marston on 14th January 1972 on rhesus monkeys. (Data, journals and papers Folder). [Google Scholar]
- Scott R. Egg-sharing, Motivation and consent: ethical, legal and policy issues. In: Golombok S., Scott R., Wilkinson S., Richards M., Appleby J., editors. Regulating Reproductive Donation. Cambridge University Press; 2015. (in press) [Google Scholar]
- Scott R., Wiliams C., Ehrich K., Farsides B. Donation of ‘spare’ fresh or frozen embryos to research: who decides that an embryo is ‘spare’ and how can we enhance the quality and protect the validity of consent? Med. Law Rev. 2012;20:255–303. doi: 10.1093/medlaw/fws013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe P.C. Medicine and the media. BMJ. 1978:565. doi: 10.1136/bmj.2.6136.565-b. (19th August 1978) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G. Laparoscopic recovery of preovulatory human oocytes after priming of ovaries with gonadotrophins. Lancet. 1970;i:683–689. doi: 10.1016/s0140-6736(70)90923-2. [DOI] [PubMed] [Google Scholar]
- Steptoe P.C., Edwards R.G. Birth after the reimplantation of a human embryo. Lancet. 1978;ii:366. doi: 10.1016/s0140-6736(78)92957-4. [DOI] [PubMed] [Google Scholar]
- Williams P. 1980. To Mrs. Brown a daughter. A film made for Thames television by Peter Williams TV: The Studio, Boughton, Faversham, UK. [Google Scholar]
- Wilson D. Manchester University Press.; 2014. The history of British Bioethics. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Edited transcript of interview with Noni Fallows and John Webster conducted at Bourn Hall on 19 May 2014.
Edited transcript of interview with Sandra Corbett conducted by phone on 26 June 2014.