Abstract
Background:
Decision-making in periodontal therapeutics is critical and is influenced by accurate diagnosis of osseous defects, especially furcation involvement. Commonly used diagnostic methods such as clinical probing and conventional radiography have their own limitations. Hence, this study was planned to evaluate the dimensions of furcation defects clinically (pre- and post-surgery), intra-surgically, and by cone beam computed tomography (CBCT) (pre- and post-surgery).
Materials and Methods:
The study comprised a total of 200 Grade II furcation defects in forty patients, with a mean age of 38.05 ± 4.77 years diagnosed with chronic periodontitis which were evaluated clinically (pre- and post-surgically), by CBCT (pre- and post-surgically), and intrasurgically after flap reflection (40 defects in each). After the presurgical clinical and CBCT measurements, demineralized freeze-dried bone allograft was placed in the furcation defect and the flaps were sutured back. Six months later, these defects were evaluated by recording measurements clinically, i.e., postsurgery clinical measurements and also postsurgery CBCT measurements (40 defects each).
Results:
Presurgery clinical measurements (vertical 6.15 ± 1.71 mm and horizontal 3.05 ± 0.84 mm) and CBCT measurements (vertical 7.69 ± 1.67 mm and horizontal 4.62 ± 0.77 mm) underestimated intrasurgery measurements (vertical 8.025 ± 1.67 mm and horizontal 4.82 ± 0.67 mm) in both vertical and horizontal aspects, and the difference was statistically not significant (vertical P = 1.000, 95% confidence interval [CI], horizontal P = 0.867, 95% CI). Further, postsurgery clinical measurements (vertical 2.9 ± 0.74 mm and horizontal 1.52 ± 0.59 mm) underestimated CBCT measurements (vertical 3.67 ± 1.17 mm and horizontal 2.45 ± 0.48 mm). There was statistically significant difference between presurgery clinical–presurgery CBCT (P < 0.0001, 95% CI) versus postsurgery clinical–postsurgery CBCT (P < 0.0001, 95% CI) values in both vertical and horizontal aspects.
Conclusion:
The use of CBCT appears to be prudent for accurate diagnosis of furcation defects in advanced periodontal diseases. Presurgical and postsurgical three-dimensional imaging enable the clinician to optimize treatment decisions and assess the quantum of healing more definitively.
Key words: Cone-beam computed tomography, furcation defects, periodontal disease
INTRODUCTION
Chronic periodontal diseases are inflammatory conditions affecting the periodontium and are currently considered as one of the most prevalent oral diseases affecting the adult population.[1] Periodontal disease leads to attachment loss, alveolar bone destruction, and subsequently loosening of teeth. The teeth more commonly involved are the molars. Proper diagnosis is extremely crucial to determine the prognosis and adopt an adequate treatment strategy. Diagnosis of furcation involvement is based on many methods such as probing pocket depth (PPD), determining clinical attachment level (CAL), probing of furcation entrance, and periapical radiographs.[2]
However, the current diagnostic methods lack consistency and have many limitations. Accurate clinical analysis of the furcation is not possible most of the times due to limited access to the depths of the furcations, morphologic variations, and measurement errors. Intraoral radiographs (IRs) are also used to assess the bone loss in furcation involved teeth, but they also have limitations in correctly diagnosing the case. Intraoral periapical (IOPA) radiographs give only a two-dimensional (2D) information of a three-dimensional (3D) structure.[3] Gradually, the introduction of tuned aperture computed tomography (CT) has crossed the boundaries of 2D imaging. 3D image analysis was possible using this modality but with an erroneously high radiation exposure to the patient.
Therefore, surgical exposure was the only method to accurately detect the extent and type of bone destruction as well as to determine the amount of bone gain after regenerative therapy. However, 6–12 months re-entry procedure may be too early because of the continued maturation of the osseous graft.[4] Research has demonstrated that osteoid may be incompletely formed within 8 months and the maturation process of bone may take up to 2 years.[4,5] Another hindrance in utilizing re-entry for analysis of the results is the ethical issue, which restricts the operator for re-entry surgeries, making it difficult to accurately assess the results. More recently, cone beam CT (CBCT) has been introduced to assess the head and neck structures. This method is useful in assessing images three-dimensionally with the advantage of high accuracy, high resolution, and low cost as compared to CT.[6]
Ross and Thompson noticed furcation involvement in only 22% of cases with conventional radiographs.[7] Walter et al. reported that CBCT and intrasurgical evaluation of maxillary molar furcation involvement were found to be in substantial agreement and that CBCT enables a precise estimation and categorization of furcation involvement, as well as visualization of the root morphologies with root proximities or root fusions.[8] CBCT seems to be more accurate in diagnosing such conditions. Current literature reveals paucity of information concerning estimation and comparison of treatment results in furcation areas. The study was aimed to evaluate and compare dimensions of furcation defects clinically (pre- and post-surgery), intrasurgically, and by CBCT (pre- and post-surgery).
MATERIALS AND METHODS
A total of forty patients (21 females and 19 males) among those visiting the outpatient Department of Periodontics and Implantology, with an average age of 38.05 ± 4.77 years and who were diagnosed with generalized chronic periodontitis were recruited in the study. Inclusion criteria for the study were patients with at least 30% of the sites involved and exhibited PPD ≥5 mm, CAL ≥5 mm with at least one molar with Grade II furcation involvement.
Patients having furcation caries, pregnant and lactating women, metal crowns in CBCT irradiation area were excluded from the study. The study protocol was approved by the Institutional Ethics Committee and was in accordance to the Helsinki criteria. The study design was explained and informed consent was obtained from all the patients. All patients underwent Phase I periodontal therapy, involving oral hygiene instructions and scaling and root planing. All the clinical measurements were performed by a single examiner (RK), and all the CBCT measurements were performed by a second examiner (NP). These examiners were calibrated to determine the intraexaminer consistency for the vertical and the horizontal measurements. The particular quadrant with Grade II furcation involvement was identified. Custom-made occlusal acrylic stents were made to standardize the probe angulations and position. Occlusal stents were fabricated with cold cure acrylic resin on a cast model obtained from an alginate impression. A groove was made in stent in relation to each involved tooth. After this, the measurements were made as follows.
Presurgery cone beam computed tomography measurements
After a period of 4–6 weeks of Phase I therapy, the patient was recalled. Before any clinical measurement, CBCT of the site to be operated was obtained (KODAK 9000C and KODAK 9000C 3D Extraoral Imaging System, Carestream Health, Inc., France). The vertical component measurements were done as follows in the sagittal view [Figure 1c]:
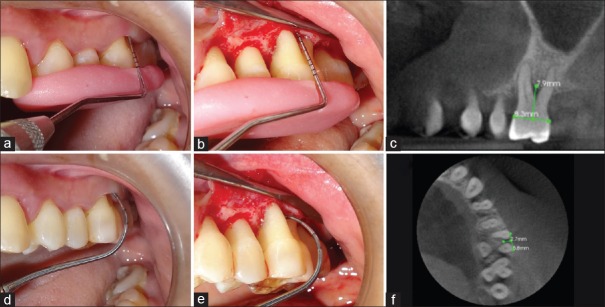
Figure 1.
Presurgery, intrasurgery, and cone beam computed tomography measurements of furcation defects. (a) Presurgical clinical measurement of vertical component; (b) Intrasurgical measurement of vertical component; (c) Presurgery cone beam computed tomography measurement of vertical component; (d) Presurgical clinical measurement of horizontal component; (e) Intrasurgical measurement of horizontal component; (f) Presurgery cone beam computed tomography measurement of horizontal component
First, cementoenamel junction (CEJ) was identified and a horizontal line joining the CEJ was made from mesial to the distal side of the tooth
A perpendicular line to the first line was made in such a way that it runs from the middle of the tooth to the middle of the furcation till the alveolar crest
This distance between the alveolar crest and the point where this line meets the first line was measured.
The horizontal component measurements were done as follows in axial view [Figure 1f]:
A line was drawn from the most buccal end of one root to the other as shown
Later, a perpendicular line is drawn to first line from the center of first line till the bone trabeculae starts, i.e., crest.
Presurgery clinical measurements
After presurgery CBCT measurements had been recorded, presurgery clinical measurements were performed as follows:
Patient was given local anesthesia in the region to be treated
Williams graduated periodontal probe (Hu-Friedy, Chicago, IL, USA) was used to measure vertical component measurements and Nabers probe (Hu-Friedy, Chicago, IL, USA) was used for horizontal component measurements
Vertical component was measured from CEJ till resistance was felt in midbuccal area after placing stent [Figure 1a]
Horizontal component was measured with Nabers probe. Probe was penetrated till resistance was felt [Figure 1d].
Intrasurgical measurements
After presurgical measurements had been performed, mucoperiosteal flap was reflected and thorough debridement was carried out. The intrasurgical measurements were done as follows:
After placing stent, vertical component was measured with Williams probe from CEJ to the crest of alveolar bone [Figure 1b]
Horizontal component was measured with Nabers probe [Figure 1e].
For the comparison between these three measurements, i.e., presurgery, intrasurgery, and CBCT, intrasurgery can be considered as the gold standard, i.e., most accurate measurements. After thorough debridement and the necessary measurements demineralized freeze-dried, bone allograft was placed in the furcation defects. The flaps were then sutured and periodontal dressing was placed. The patients were prescribed with antibiotics and analgesics for a period of 1 week postsurgically. Sutures and periodontal dressing were removed after 1 week.
Postsurgery clinical and cone beam computed tomography measurements
After a period of 6 months postsurgery, clinical [Figure 2a and c] and CBCT [Figure 2b and d] measurements were repeated in the same manner as described above.
Figure 2.
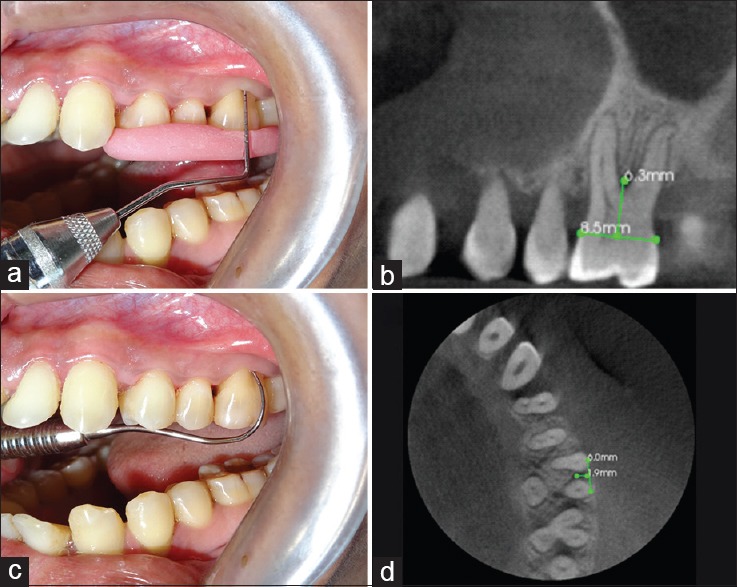
Postsurgery clinical and cone beam computed tomography measurements of furcation defects. (a) Postsurgical clinical measurement of vertical component; (b) Postsurgery cone beam computed tomography measurement of vertical component; (c) Postsurgical clinical measurement of horizontal component; (d) Postsurgery cone beam computed tomography measurement of horizontal component
Statistical analysis
The data were analyzed using the STATA Version 13.0 (StataCorp.2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). P value was taken as statistically significant when <0.05. The variables were presented as mean ± standard deviation. The comparison between the clinical and CBCT pre- and post-surgery measurements was done using one-way ANOVA.*
RESULTS
A total of 200 Grade II furcation defects in forty patients diagnosed with chronic periodontitis were evaluated clinically (pre- and post-surgically), by CBCT (pre- and post-surgically), and intrasurgically after flap reflection (40 defects in each).
The Cronbach's alpha statistics was used to describe the reliability of repeated measures. Based on the evaluation, the alpha values for the vertical and horizontal measurements were 0.95 and 0.90, respectively.
Results of this study are discussed below.
The mean ± SD of vertical and horizontal component measurements of pre- and post-surgery clinical, intra-surgery and pre- and post-surgery cone beam computed tomography are shown in [Table 1].
Table 1.
Vertical and horizontal component measurements of pre- and post-surgery clinical, intra-surgery and pre- and post-surgery cone beam computed tomography
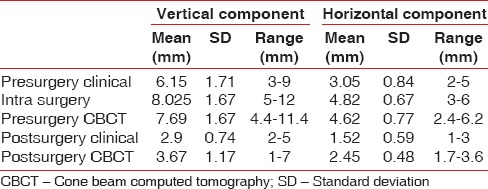
Vertical component
The mean difference when comparing presurgery clinical versus intrasurgery measurements was 1.87 mm, and this difference between the two was statistically significant (P < 0.0001), indicating underestimation of presurgical measurements when compared to intrasurgical measurements. Similarly, the presurgery clinical measurements underestimated presurgery CBCT measurements and the difference was statistically significant (P < 0.0001), whereas there was a mean difference of 0.332 mm between intrasurgery versus presurgery CBCT measurements, indicating CBCT underestimation of intrasurgical measurements [Table 2]. This means that CBCT and intrasurgical measurements of furcation defect yielded similar results. In addition, there was an underestimation of postsurgery clinical measurements when compared to postsurgery CBCT measurements and the difference reached statistical significance (P < 0.0001).
Table 2.
Comparison of vertical and horizontal component measurements of presurgery clinical, intrasurgery, postsurgery clinical and pre- and post-surgery cone beam computed tomography*
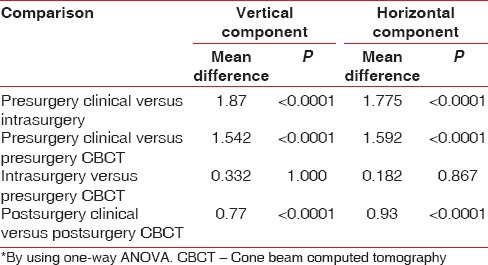
Mean difference between presurgery clinical–presurgery CBCT versus postsurgery clinical–postsurgery CBCT values was 0.772 mm which was statistically significant indicating lesser postsurgical values as compared to presurgical values.
Horizontal component
The mean difference when comparing presurgery clinical versus intrasurgery measurements was 1.775 mm, and this difference was statistically significant (P < 0.0001). This indicated that presurgical measurements underestimated intrasurgical measurements. There was statistically significant difference in presurgery clinical versus presurgery CBCT measurements, depicting that presurgical clinical measurement underestimated presurgery CBCT measurements (P < 0.0001) whereas there was no significant difference between intrasurgery versus presurgery CBCT measurements. Presurgery CBCT measurements underestimated intrasurgery clinical measurements in horizontal component too, but the differences were not statistically significant. Mean difference between postsurgery clinical versus postsurgery CBCT measurements was 0.93 mm which was statistically highly significant (P < 0.0001), indicating underestimation of postsurgery clinical measurements compared to postsurgery CBCT measurements [Table 2].
Mean difference between presurgery clinical–presurgery CBCT versus postsurgery clinical–postsurgery CBCT values was 0.66 mm which was statistically significant, indicating lesser postsurgical values as compared to presurgical values.
DISCUSSION
There is a plenty of literature stating that there is a higher risk of periodontal breakdown in molar furcation area, resulting in less favorable treatment outcomes of periodontal lesions adjacent to furcation involvement and greater risk of tooth loss.[9] In addition, molars in the mandible and buccal furcations in the maxilla, the correct diagnosis of furcation involvement with Class II seems especially important because at these sites a regenerative surgical procedure might be a possible treatment of choice.[10,11,12] Hence, accurate diagnosis is a necessity for appropriate treatment to be carried out and to achieve optimum clinical results. Furcation involvement diagnosis includes the amount of horizontal and vertical bone loss in the furcation area and evaluation of root morphology, length of root trunk, and the angle of root separation.[13] Clinical diagnosis seems to be difficult at times or error some due to lack of proper knowledge and interexaminer related bias. Furthermore, other methods such as IOPA radiographs have its own limitations of reflecting only 2D structures. CBCT has set a new avenue for the accurate diagnosis of furcation involvement and has proved to be better as compared to conventional imaging modalities.[14]
Despite the robust amount of studies that have been carried out, there is still need to add more data to the literature to make a decision regarding the method that should be followed for accurate diagnosis of furcation defects and to evaluate postsurgical results. Hence, the study was aimed to compare measurements of furcation involvement before surgery-, during surgery-, and after surgery-clinically and by CBCT.
A total of 200 Grade II furcation defects were evaluated in forty patients clinically (presurgery (40) and postsurgery (40)), by CBCT (presurgery (40) and postsurgery (40)), and intrasurgically (40 defects). After 6 months, these defects were evaluated clinically, i.e., postsurgery clinical measurements were taken and also postsurgery CBCT measurements were taken (40 defects in each). The results of our study connote that both presurgical clinical and presurgical CBCT measurements underestimated intrasurgical measurements. However, there was no statistically significant difference between CBCT measurements when compared to intrasurgical measurements. On the other hand, there was statistically significant difference between presurgical and intrasurgical measurements. Results obtained indicate that postsurgery clinical measurements underestimate postsurgery CBCT measurements.
Misch et al.,[6] in 2006, carried out a study in which artificial osseous defects on mandible were generated in dry skulls, and it was shown that CBCT measurements were similarly accurate as direct measurements using a periodontal probe in buccal and lingual defects. Fuhrmann et al.,[15] in 1995, collated and compared images of dental radiographs with CT images for the valuation of horizontal and vertical bone loss. With the help of dental radiographs, 60% of infraosseous defects could be spotted. The vertical defect was underrated by a mean of 2.2 mm whereas CT scan could uncover 100% of the defects. The outcome of the above two studies is homogeneous to our study. In addition, Banodkar et al.,[16] in 2015, evaluated the accuracy of CBCT measurements of alveolar bone defect caused due to periodontal disease, by comparing it with actual surgical measurements which is the gold standard. The authors concluded that CBCT is highly accurate in measurement of periodontal defects and proves to be a very useful tool in periodontal diagnosis and treatment assessment.
The presurgery CBCT measurements underestimated the intrasurgical measurements in this study, but the difference was not statistically significant. The logic to this could be that during debridement of osseous defect the bone at the base to the defect is removed resulting in deeper defect during surgical measurements. Further, the defect base is more cancellous, so there is likelihood that the probe penetrates more during intrasurgical measurements. Further, the accuracy of both measurements is different. CBCT measurements are made in points like 0.01 mm whereas measurements with probe are done with 1 mm distance. Results obtained by Qiao et al.,[17] in 2014, are similar to our study and the authors inferred that CBCT was a highly accurate method of demonstrating loss of periodontal tissue, especially in furcation defects and also root morphologies in maxillary molars. In this study, 15 patients with 20 defects were studied. Feijo et al.,[18] in 2012, confirmed the accuracy of CBCT in measurements of horizontal periodontal bone defects. Six patients with 8 maxillary molars were evaluated. The authors concluded that there was no difference between CBCT and clinical measurements. However, CBCT overestimated clinical measurements by 0.4 mm. In the present study also, there was no significant difference between CBCT and intrasurgical measurements, but CBCT underestimated intrasurgical measurements. Grimard et al.[19] in 2009 compared the measurements from digital IR and cone beam volumetric tomography (CBVT) images to direct surgical measurements for the evaluation of regenerative treatment outcomes. The authors have concluded that compared to direct surgical measurements CBVT was significantly more precise and accurate than IRs. Our study defers from this study as in this study IR are not taken.
In addition, presurgical measurements underestimated intrasurgical measurements. The logic to this might be that in case of horizontal component measurement with Nabers probe the position of the gingival margin hinders the exact measurements of furcation defect depth.
During both vertical and horizontal measurements, the mean of postsurgery clinical–postsurgery CBCT was less as compared to mean of presurgery clinical–presurgery CBCT measurements, which may be attributed to the regeneration that took place within 6 months.
CONCLUSION
The use of CBCT in advanced periodontal disease diagnosis appears to be more informative and prudent. A comprehensive assessment of furcation involvement is possible with CBCT and further to optimize treatment decisions. Although it may seem that the results indicate towards a better insight of details in Grade II furcation defects, the same can be applied to other types of periodontal defects, which may be evaluated and confirmed in additional investigations in future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
One-way ANOVA.
REFERENCES
- 1.Scaf G, Morihisa O, Loffredo Lde C. Comparison between inverted and unprocessed digitized radiographic imaging in periodontal bone loss measurements. J Appl Oral Sci. 2007;15:492–4. doi: 10.1590/S1678-77572007000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pihlstrom BL. Periodontal risk assessment, diagnosis and treatment planning. Periodontol 2000. 2001;25:37–58. doi: 10.1034/j.1600-0757.2001.22250104.x. [DOI] [PubMed] [Google Scholar]
- 3.Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48. doi: 10.1046/j.0906-6713.2003.003423.x. [DOI] [PubMed] [Google Scholar]
- 4.Mellonig JT. Autogenous and allogeneic bone grafts in periodontal therapy. Crit Rev Oral Biol Med. 1992;3:333–52. doi: 10.1177/10454411920030040201. [DOI] [PubMed] [Google Scholar]
- 5.Dragoo MR, Sullivan HC. A clinical and histological evaluation of autogenous iliac bone grafts in humans. I. Wound healing 2 to 8 months. J Periodontol. 1973;44:599–613. doi: 10.1902/jop.1973.44.10.599. [DOI] [PubMed] [Google Scholar]
- 6.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 7.Ross IF, Thompson RH., Jr Furcation involvement in maxillary and mandibular molars. J Periodontol. 1980;51:450–4. doi: 10.1902/jop.1980.51.8.450. [DOI] [PubMed] [Google Scholar]
- 8.Walter C, Weiger R, Zitzmann NU. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol. 2010;37:436–41. doi: 10.1111/j.1600-051X.2010.01556.x. [DOI] [PubMed] [Google Scholar]
- 9.Pretzl B, Kaltschmitt J, Kim TS, Reitmeir P, Eickholz P. Tooth loss after active periodontal therapy 2: Tooth-related factors. J Clin Periodontol. 2008;35:175–82. doi: 10.1111/j.1600-051X.2007.01182.x. [DOI] [PubMed] [Google Scholar]
- 10.Jepsen S, Heinz B, Jepsen K, Arjomand M, Hoffmann T, Richter S, et al. A randomized clinical trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part I: Study design and results for primary outcomes. J Periodontol. 2004;75:1150–60. doi: 10.1902/jop.2004.75.8.1150. [DOI] [PubMed] [Google Scholar]
- 11.Bowers GM, Schallhorn RG, McClain PK, Morrison GM, Morgan R, Reynolds MA. Factors influencing the outcome of regenerative therapy in mandibular class II furcations: Part I. J Periodontol. 2003;74:1255–68. doi: 10.1902/jop.2003.74.9.1255. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann T, Richter S, Meyle J, Gonzales JR, Heinz B, Arjomand M, et al. A randomized clinical multicentre trial comparing enamel matrix derivative and membrane treatment of buccal class II furcation involvement in mandibular molars. Part III: Patient factors and treatment outcome. J Clin Periodontol. 2006;33:575–83. doi: 10.1111/j.1600-051X.2006.00947.x. [DOI] [PubMed] [Google Scholar]
- 13.Walter C, Weiger R, Zitzmann NU. Periodontal surgery in furcation-involved maxillary molars revisited – An introduction of guidelines for comprehensive treatment. Clin Oral Investig. 2011;15:9–20. doi: 10.1007/s00784-010-0431-9. [DOI] [PubMed] [Google Scholar]
- 14.Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: Caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am. 2008;52:825–41, vii. doi: 10.1016/j.cden.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Fuhrmann RA, Bücker A, Diedrich PR. Assessment of alveolar bone loss with high resolution computed tomography. J Periodontal Res. 1995;30:258–63. doi: 10.1111/j.1600-0765.1995.tb02131.x. [DOI] [PubMed] [Google Scholar]
- 16.Banodkar AB, Gaikwad RP, Gunjikar TU, Lobo TA. Evaluation of accuracy of cone beam computed tomography for measurement of periodontal defects: A clinical study. J Indian Soc Periodontol. 2015;19:285–9. doi: 10.4103/0972-124X.154176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Qiao J, Wang S, Duan J, Zhang Y, Qiu Y, Sun C, et al. The accuracy of cone-beam computed tomography in assessing maxillary molar furcation involvement. J Clin Periodontol. 2014;41:269–74. doi: 10.1111/jcpe.12150. [DOI] [PubMed] [Google Scholar]
- 18.Feijo CV, Lucena JG, Kurita LM, Pereira SL. Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: An in vivo study. Int J Periodontics Restorative Dent. 2012;32:e162–8. [PubMed] [Google Scholar]
- 19.Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol. 2009;80:48–55. doi: 10.1902/jop.2009.080289. [DOI] [PubMed] [Google Scholar]