Abstract
Background:
Intubated patients in Intensive Care Unit (ICU) are not able to take care of their mouth health, so they are at risk of bacterial colonization and dental plaques formation that can lead to systemic diseases such as pneumonia and gingivitis.
Aims:
In randomized, double-blind clinical study, the efficacy of natural herbal mouthwash containing Salvadora persica ethanol extract and Aloe vera gel was compared with chlorhexidine on gingival index (GI) of intubated patients in ICU.
Materials and Methods:
Seventy-six intubated patients (18–64 years old with mean age 40.35 ± 13.2) in ICU were admitted to this study. The patients were randomly divided into two groups: (1) Herbal mouthwash and (2) chlorhexidine solution. Before the intervention, the GIs was measured by modified GI device into two groups. The mouth was rinsed by mouthwashes every 2–3 h for 4 days. 2 h after the last intervention, GIs were determined.
Results:
Along with mechanical methods, herbal mouthwash in reducing GI was statistically significant than that of chlorhexidine (P < 0.05).
Conclusion:
The results of this study introduce a new botanical extract mouthwash with dominant healing effects on GI (1.5 ± 0.6) higher than that of synthetic mouthwash, chlorhexidine (2.31 ± 0.73).
Key words: Aloe vera gel, chlorhexidine, gingival diseases, Intensive Care Units, mouthwashes, patients
INTRODUCTION
Oral health is considered as one of the most important issues that affect on the general health of the Intensive Care Units (ICUs) admitted patients.[1] Omitting tooth brushing from dental hygiene program will cause the formation of dental plaque and consequently gingivitis.[2,3] In fact, poor oral health has been incremented as the primary cause of gingivitis.[4] Dental plaques alone can be the major cause of initiation and progression of periodontal diseases.[5,6,7] The direct correlation between dental plaques and severity of gingival inflammation or gingivitis was demonstrated.[8] Untreated gingivitis will exposed the infected patients to infection and periodontitis.[9] Untreated periodontitis is also considered as a risk factor for systemic disorders specifically bacterial pneumonia and cardiovascular diseases.[10,11,12] However, gingivitis and its related complications are readily preventable through controlling dental plaques and provision of oral and dental hygiene procedures.[13] Intubated patients in ICU are not able to take care of their mouth health, so they are at risk of bacterial colonization and dental plaques formation that can lead to systemic diseases such as pneumonia and gingivitis.[10,11,12]
Interventions for removing the dental plaques in intubated patients in ICUs include mechanical approaches and pharmaceutical approaches.[14] One of the most effective methods of controlling dental plaque is the use of mouth rinses.[15] Chlorhexidine is considered as the gold treatment for controlling the dental plaque and gingivitis due to its efficacy against different kinds of bacteria, fungi, and viruses and so far, no microbial resistance has been reported for it.[16,17] Although chlorhexidine has been introduced as the most effective anti-plaque agent,[16,17,18] but there is no sufficient evidence in regard to its efficacy and safety.[14] Some adverse effects include changing in color teeth and mucosa, mucosal desquamation, salivary stones creation, irritation, dryness of mouth, and side systemic effects as the result of swallowing were reported.[19,20] Therefore, finding the new alternative mouthwash with undesired side effects is mandatory. The World Health Organization (WHO) has recommended on finding the new natural sources such as the herbal extracts for overcoming on side effects of chemical agents.[21]
Salvadora persica is traditionally used for oral and dental health, and it was recommended by WHO for oral hygienic procedures.[22] The antibacterial activity of S. persica on cariogenic oral bacteria was confirmed.[22,23,24,25,26] Other pharmacological effects such as anti-inflammatory,[27] antioxidant,[28] antiulcer,[29,30] and sedative effects[31] were confirmed.
Aloe vera gel is the clear, jelly-like substance found in the inner part of the aloe leaf with anti-inflammatory,[32] antimicrobial,[33,34,35] antiulcer effects.[36]
Therefore, the aim of this investigation was to evaluate the efficacy of oral botanical extract mouth rinse containing S. persica ethanol extract (Miswak) and A. vera (Aloe) gel on gingival index (GI) of intubated patients of ICU and its efficacy was compared to chlorhexidine as current treatment.
MATERIALS AND METHODS
Participant
A randomized, double-blind controlled clinical trial was conducted on 76 patients under mechanical ventilation of three ICUs of Teaching Hospital, Yazd, Iran, from May to September 2014. The patients were randomly divided into two groups. The dentist measured the gingival health index of the patients before and after the intervention. The clinical design was approved by the University Committee of Ethics, and all private data of patients remained confidential. All participants provided written informed consent. This clinical study was also registered in the Iranian Clinical Trial Center under the code number 2014062418212N1. Participants with the following criteria were included all intubated patients (18–65 years old with mean age 40.35 ± 13.2) with normal teeth that had hospitalization time in ICU <24 h, participants with the following criteria were excluded hospitalized in other wards before wheeling into ICU, pregnancy, sensitivity, or anaphylaxis to herbal preparation and chlorhexidine, transfer the patient from the ICU for any reason or death before completion the study, dissatisfaction of patient's attendants, observation any damage or injury in patient's airway as a result of intratracheal intubation, or any other physical factors.
Mouthwashes
Chlorhexidine mouthwashes (0.2%) were purchased from Shahredarou company and were poured in the bottles such as the other group. Herbal solution was prepared at the formulation Unit of Medicinal Plant, Research Center of BarijEssence, Kashan, Iran. Each milliliter of product was containing 10 mg S. persica dried ethanol extract and 940 mg A. vera gel. Microbial limit test passed the criteria for oral liquid pharmaceutical products.
Study design
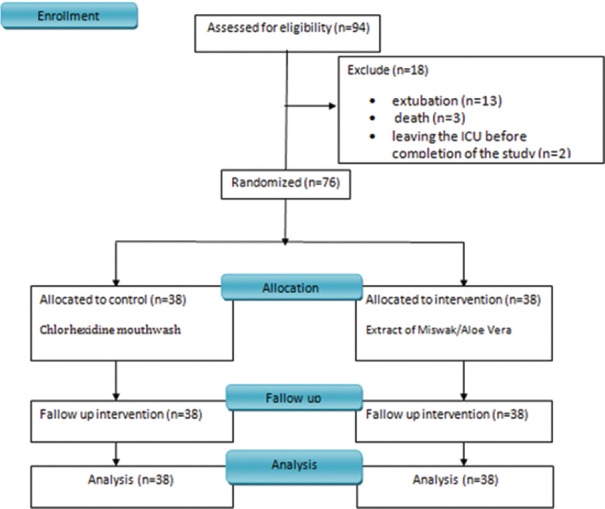
All demographic data, disease and smoking histories, cause of hospitalization, all of the medications of all intubated patients were recorded in the checklists. The GI was measured and recorded in both groups before intervention by modified GI device[37] (baseline GI). Before oral care surveillance, to ensure the suitability of obstructive pressure of the cuff, its pressure was calibrated using a special manometer (20–25 mm Hg). Then, all oral areas including the internal and external dental surfaces with rotatory movements, and gums and tongue with protrusive movements were brushed with Butler soft toothbrush (USA). Using a special syringe, each part of the mouth was irrigated with the mouthwash before and after brushing for 30 s.[38] If the patients had airway in place, it was removed, cleaned, and relocated again in place. The same method, time, and frequency of rinsing were used for both groups. Oral irrigations and secretion suctions were performed for all patients every 2–3 h using the Nursing Support Services and ward's routines, respectively. The mouthwashes were used for 4 days. 2 h after the last treatment, the GI was measured again using the same method [Figure 1].
Figure 1.
Diagram of clinical trial
Statistical analysis
All data were analyzed by SPSS version 16 (SPSS Inc., Chicago, IL, USA). Chi-square was used to examine the differences between the two groups regarding qualitative variables as gender, smoking history, and type of disease. Paired and independent t-tests were used to examine the differences between the two groups regarding quantitative variables such as breathing rate, number of teeth, systolic pressure, diastolic pressure, and pulse rate which had a normal distribution based on the Kolmogorov–Smirnov test. Mann–Whitney test was used to examine the differences between the two groups regarding quantitative variables such as temperature, number of medications, and number of antibiotics which proved to be normally distributed based on the Kolmogorov–Smirnov test.
RESULTS
Seventy-six intubated patients were completed the study. Some patients were excluded from the study due to extubation (n = 13), death (n = 3), leaving the ICU before the completion of the study (n = 2). All of the demographic data were presented in Table 1.
Table 1.
Demographic data of intubated patients of this study
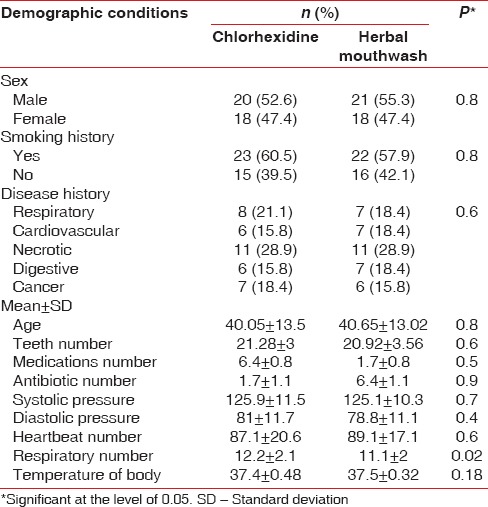
Comparison of the two groups with respect to demographic conditions showed no significant difference between the two groups at the baseline. Furthermore, the subjects in both groups were the same for age, gender, smoking, dental number, cause of disease, antibiotic number, drug number, systolic blood pressure, diastolic blood pressure, heart rate, and temperature of the body (P > 0.05). There was a difference between breathing rate that was not clinically important.
The results of the present study demonstrated that the use of chlorhexidine rinse and herbal extract mouthwash along with mechanical methods both reduced the GI in intubated patients, but this reduction in GI was more considerable in the herbal mouthwash group, and their differences were statistically significant (P < 0.05) [Table 2].
Table 2.
Gingival index for intubated patients before and after rinsing of mouthwashes
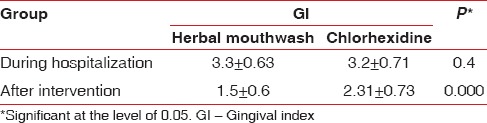
There was no significant between the means of GI of intubated patients in herbal mouthwash (3.3 ± 0.63) and chlorhexidine (3.2 ± 0.71) groups at the baseline of the study (P = 0.4).
Administration of both mouthwashes decreased the GI to 2.31 ± 0.73 and 1.5 ± 0.6 in the patients that were treated with chlorhexidine and herbal extract mouthwash, respectively. The results were shown; the herbal extract mouthwash was superior to chlorhexidine as the current treatment in reducing the GI of intubated patients in ICUs.
DISCUSSION
The results of our study exhibited the high GI for patients that were admitted to ICUs, and high GIs were not suitable for intubated hospitalized patients due to causing the systemic disorders specifically bacterial pneumonia and cardiovascular diseases.[10,11,12] Therefore, gingival disorders as silent epidemic[7] are most commonly chronic bacterial infection that affects on 60–90% of school children and nearly 100% of adults.[39,40] Furthermore, hospitalization has negative effects on oral health conditions of hospitalized patients and accelerates the accumulation of dental plaque that is associated with the destruction of mucosal membranes and increases the rate of gingivitis.[41] In addition, because the oral cares of hospitalized patients are not the right priority of nurses,[41] However, in these patients, oral problems are rapidly intensified and increased the nosocomial infections.[42,43] Therefore, oral health surveillance is one of the prominent topics of the ICU which should be performed by nurses to prevent the onset of infection.
The results of our study exhibited the prominent potency of mouthwash containing S. persica ethanol extract and A. vera gel than that of chlorhexidine in intubated hospitalized patients of ICUs.
Chlorhexidine (0.2%) as the gold standard for oral health care has been accepted.[44] Although, there are some studies that confirmed the beneficial effects of S. persica extracts[23,24,26] and A. vera gel[33,44] on oral cariogenic bacteria in vitro and in vivo conditions, separately, but our literatures survey did not show any research on the efficacy of a combination of S. persica and A. vera on GI of patients hospitalized in ICUs. In other study showed that mouthwash containing S. persica alone improves the GI as same as chlorhexidine.[45] The effectiveness of A. vera gel mouthwashes and chlorhexidine on improving GI have been demonstrated the same.[44,46]
Indeed, the higher efficacy of this natural mouthwash than that of chlorhexidine is related to the synergistic effects of S. persica and A. vera gel extracts against oral cariogenic bacteria that finally improve the GI of hospitalized patients.
Other biological activities of extracts including the anti-inflammatory effects,[27,32,35] antiulcer potency,[22,29,35] and sedative activities[31] of S. persica and A. vera and their synergic effects improve the status of oral health.
A. vera gel administration due to its efficacy in improvement of periodontal condition, nature's soothing healer property on gingiva has been recommended as a local drug delivery system in periodontal pockets.[47]
CONCLUSION
Therefore, the combination of S. persica ethanol extract and A. vera gel extract in mouthwash formula acts better than chlorhexidine in reducing the GI of intubated hospitalized patients in ICUs. Improvement in GI of hospitalized patients is one of the most important factors which can protect the patients from pathogenic microorganisms and therefore, prevent the spread of pulmonary and nosocomial pathogens in hospital and in the lungs and blood of patients.
Other larger clinical studies are required for evaluating the efficacy and safety of S. persica and A. vera mouthwash.
Financial support and sponsorship
This study was supported by Arak University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors are thankful from Arak University of Medical Sciences. The authors are extremely grateful from Dr. Mohammad Hossien Falahzade for data analysis.
REFERENCES
- 1.Jones DJ, Munro CL, Grap MJ. Natural history of dental plaque accumulation in mechanically ventilated adults: A descriptive correlational study. Intensive Crit Care Nurs. 2011;27:299–304. doi: 10.1016/j.iccn.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pennel BM, Keagle JG. Predisposing factors in the etiology of chronic inflammatory periodontal disease. J Periodontol. 1977;48:517–32. doi: 10.1902/jop.1977.48.9.517. [DOI] [PubMed] [Google Scholar]
- 3.Summers CJ, Oberman A. Association of oral disease with 12 selected variables. I. Periodontal disease. J Dent Res. 1968;47:457–62. doi: 10.1177/00220345680470031901. [DOI] [PubMed] [Google Scholar]
- 4.Carranza FA, Newman MG. Clinical Periodontology. 8th ed. Philadelphia: WB Saunders; 1996. [Google Scholar]
- 5.Berry AM, Davidson PM, Masters J, Rolls K, Ollerton R. Effects of three approaches to standardized oral hygiene to reduce bacterial colonization and ventilator associated pneumonia in mechanically ventilated patients: A randomised control trial. Int J Nurs Stud. 2011;48:681–8. doi: 10.1016/j.ijnurstu.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Haysom L, Indig D, Byun R, Moore E, van den Dolder P. Oral health and risk factors for dental disease of Australian young people in custody. J Paediatr Child Health. 2014;14:545–51. doi: 10.1111/jpc.12761. [DOI] [PubMed] [Google Scholar]
- 7.Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–20. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 8.Ames NJ. Evidence to support tooth brushing in critically ill patients. Am J Crit Care. 2011;20:242–50. doi: 10.4037/ajcc2011120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Labeau S, Blot S. Annual Update in Intensive Care and Emergency Medicine 2011. Ch. 4. Berlin Heidelberg: Springer; 2011. Research Priorities in Oral Care for Endotracheallyintubated Patients; pp. 144–155. [Google Scholar]
- 10.Chandrahas B, Jayakumar A, Naveen A, Butchibabu K, Reddy PK, Muralikrishna T. Association among oral health parameters, periodontitis, and its treatment and mortality in patients undergoing hemodialysis. J Periodontol. 2014;85:e169–78. doi: 10.1902/jop.2013.130427. [DOI] [PubMed] [Google Scholar]
- 11.Morgan JP, Minihan PM, Stark PC, Finkelman MD, Yantsides KE, Park A, et al. The oral health status of 4,732 adults with intellectual and developmental disabilities. AADE Ed J. 2012;143:838–46. doi: 10.14219/jada.archive.2012.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramírez JH, Parra B, Gutierrez S, Arce RM, Jaramillo A, Ariza Y, et al. Biomarkers of cardiovascular disease are increased in untreated chronic periodontitis: A case control study. Aust Dent J. 2014;59:29–36. doi: 10.1111/adj.12139. [DOI] [PubMed] [Google Scholar]
- 13.Sayegh A, Dini EL, Holt RD, Bedi R. Oral health, sociodemographic factors, dietary and oral hygiene practices in Jordanian children. J Dent. 2005;33:379–88. doi: 10.1016/j.jdent.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Munro CL, Grap MJ. Oral health and care in the intensive care unit: State of the science. Am J Crit Care. 2004;13:25–33. [PubMed] [Google Scholar]
- 15.Arora V, Tangade PT, Tirth A, Pal S, Tandon V. Efficacy of dental floss and chlorhexidine mouth rinse as an adjunct to toothbrushing in removing plaque and gingival inflammation – A three way cross over trial. J Clin Diagn Res. 2014;8:ZC01–4. doi: 10.7860/JCDR/2014/8807.4943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quintas V, Prada-López I, Prados-Frutos JC, Tomás I. In situ antimicrobial activity on oral biofilm: Essential oils vs 0.2% chlorhexidine. Clin Oral Investig. 2015;19:97–107. doi: 10.1007/s00784-014-1224-3. [DOI] [PubMed] [Google Scholar]
- 17.Seneviratne CJ, Leung KC, Wong CH, Lee SF, Li X, Leung PC, et al. Nanoparticle-encapsulated chlorhexidine against oral bacterial biofilms. PLoS One. 2014;9:e103234. doi: 10.1371/journal.pone.0103234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrer R, Artigas A. Clinical review: Non-antibiotic strategies for preventing ventilator-associated pneumonia. Crit Care. 2002;6:45–51. doi: 10.1186/cc1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gjermo P, Rölla G. The plaque-inhibiting effect of chlorhexidine-containing dentifrices. Scand J Dent Res. 1971;79:126–32. doi: 10.1111/j.1600-0722.1971.tb02002.x. [DOI] [PubMed] [Google Scholar]
- 20.Skoglund LA, Holst E. Desquamative mucosal reactions due to chlorhexidine gluconate. Report of 3 cases. Int J Oral Surg. 1982;11:380–2. doi: 10.1016/s0300-9785(82)80062-8. [DOI] [PubMed] [Google Scholar]
- 21.Stoeken JE, Paraskevas S, van der Weijden GA. The long-term effect of a mouthrinse containing essential oils on dental plaque and gingivitis: A systematic review. J Periodontol. 2007;78:1218–28. doi: 10.1902/jop.2007.060269. [DOI] [PubMed] [Google Scholar]
- 22.Khatak M, Khatak S, Siddqui AA, Vasudeva N, Aggarwal A, Aggarwal P. Salvadora persica. Pharmacogn Rev. 2010;4:209–14. doi: 10.4103/0973-7847.70920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Sohaibani S, Murugan K. Anti-biofilm activity of Salvadora persica on cariogenic isolates of Streptococcus mutans: In vitro and molecular docking studies. Biofouling. 2012;28:29–38. doi: 10.1080/08927014.2011.647308. [DOI] [PubMed] [Google Scholar]
- 24.Amoian B, Moghadamnia AA, Barzi S, Sheykholeslami S, Rangiani A. Salvadora persica extract chewing gum and gingival health: Improvement of gingival and probe-bleeding index. Complement Ther Clin Pract. 2010;16:121–3. doi: 10.1016/j.ctcp.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Khalessi AM, Pack AR, Thomson WM, Tompkins GR. An in vivo study of the plaque control efficacy of Persica™: A commercially available herbal mouthwash containing extracts of Salvadora persica. Int Dental J. 2004;54:279–83. doi: 10.1111/j.1875-595x.2004.tb00294.x. [DOI] [PubMed] [Google Scholar]
- 26.Sukkarwalla A, Ali SM, Lundberg P, Tanwir F. Efficacy of miswak on oral pathogens. Dent Res J (Isfahan) 2013;10:314–20. doi: 10.4103/1735-3327.115138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibrahim AY, El-Gengaihi SE, Motawea HM, Sleem AA. Anti-inflammatory activity of Salvadora persica L. against carrageenan induced paw oedema in rat relevant to inflammatory cytokines. Notulae Sci Biol. 2011;3:22–8. [Google Scholar]
- 28.Arora S, Kaushik D. Free radical scavenging activity of Salvadora persica Linn. Asian J Chem. 2007;19:4638. [Google Scholar]
- 29.Sanogo R, Monforte MT, Daquino A, Rossitto A, Maur DD, Galati EM. Antiulcer activity of Salvadora persica L.: Structural modifications. Phytomedicine. 1999;6:363–6. doi: 10.1016/s0944-7113(99)80060-9. [DOI] [PubMed] [Google Scholar]
- 30.Monforte M, Miceli N, Mondello M, Sanogo R, Rossitto A, Galati E. Antiulcer activity of Salvadora persica on experimental ASA-induced ulcer in rats: Ultrastructural modifications. Pharm Biol. 2001;39:289–92. [Google Scholar]
- 31.Monforte MT, Trovato A, Rossitto A, Forestieri AM, D'Aquino A, Miceli N, et al. Anticonvulsant and sedative effects of Salvadora persica L. stem extracts. Phytother Res. 2002;16:395–7. doi: 10.1002/ptr.977. [DOI] [PubMed] [Google Scholar]
- 32.Langmead L, Makins RJ, Rampton DS. Anti-inflammatory effects of Aloe vera gel in human colorectal mucosa in vitro. Aliment Pharmacol Ther. 2004;19:521–7. doi: 10.1111/j.1365-2036.2004.01874.x. [DOI] [PubMed] [Google Scholar]
- 33.Bazvand L, Aminozarbian MG, Farhad A, Noormohammadi H, Hasheminia SM, Mobasherizadeh S. Antibacterial effect of triantibiotic mixture, chlorhexidine gel, and two natural materials propolis and Aloe vera against Enterococcus faecalis: An ex vivo study. Dent Res J (Isfahan) 2014;11:469–74. [PMC free article] [PubMed] [Google Scholar]
- 34.Escobedo-Lozano AY, Domard A, Velázquez CA, Goycoolea FM, Argüelles-Monal WM. Physical properties and antibacterial activity of chitosan/acemannan mixed systems. Carbohydr Polym. 2015;115:707–14. doi: 10.1016/j.carbpol.2014.07.064. [DOI] [PubMed] [Google Scholar]
- 35.Sierra-García GD, Castro-Ríos R, González-Horta A, Lara-Arias J, Chávez-Montes A. Acemannan, an extracted polysaccharide from Aloe vera: A literature review. Nat Prod Commun. 2014;9:1217–21. [PubMed] [Google Scholar]
- 36.Saito H, Imanishi K, Okabe S. Effects of aloe extracts, aloctin A, on gastric secretion and on experimental gastric lesions in rats. Yakugaku Zasshi. 1989;109:335–9. doi: 10.1248/yakushi1947.109.5_335. [DOI] [PubMed] [Google Scholar]
- 37.Lobene RR, Weatherford T, Ross NM, Lamm RA, Menaker L. A modified gingival index for use in clinical trials. Clin Prev Dent. 1986;8:3–6. [PubMed] [Google Scholar]
- 38.Pearson LS. A comparison of the ability of foam swabs and toothbrushes to remove dental plaque: Implications for nursing practice. J Adv Nurs. 1996;23:62–9. doi: 10.1111/j.1365-2648.1996.tb03136.x. [DOI] [PubMed] [Google Scholar]
- 39.Lo Russo L, Fierro G, Guiglia R, Compilato D, Testa NF, Lo Muzio L, et al. Epidemiology of desquamative gingivitis: Evaluation of 125 patients and review of the literature. Int J Dermatol. 2009;48:1049–52. doi: 10.1111/j.1365-4632.2009.04142.x. [DOI] [PubMed] [Google Scholar]
- 40.Suresh L, Neiders ME. Definitive and differential diagnosis of desquamative gingivitis through direct immunofluorescence studies. J Periodontol. 2012;83:1270–8. doi: 10.1902/jop.2012.110627. [DOI] [PubMed] [Google Scholar]
- 41.Terezakis E, Needleman I, Kumar N, Moles D, Agudo E. The impact of hospitalization on oral health: A systematic review. J Clin Periodontol. 2011;38:628–36. doi: 10.1111/j.1600-051X.2011.01727.x. [DOI] [PubMed] [Google Scholar]
- 42.Bellissimo-Rodrigues WT, Menegueti MG, Gaspar GG, Nicolini EA, Auxiliadora-Martins M, Basile-Filho A, et al. Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients: A randomized clinical trial. Infect Control Hosp Epidemiol. 2014;35:1342–8. doi: 10.1086/678427. [DOI] [PubMed] [Google Scholar]
- 43.Fourrier F, Dubois D, Pronnier P, Herbecq P, Leroy O, Desmettre T, et al. Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: A double-blind placebo-controlled multicenter study. Crit Care Med. 2005;33:1728–35. doi: 10.1097/01.ccm.0000171537.03493.b0. [DOI] [PubMed] [Google Scholar]
- 44.Chandrahas B, Jayakumar A, Naveen A, Butchibabu K, Reddy PK, Muralikrishna T. A randomized, double-blind clinical study to assess the antiplaque and antigingivitis efficacy of Aloe vera mouth rinse. J Indian Soc Periodontol. 2012;16:543–8. doi: 10.4103/0972-124X.106905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rahmani ME, Radvar M. The antiplaque effects of Salvadora persica and Padina essential oil solution in comparison to chlorhexidine in human gingival disease; a randomized placebo-controlled clinical trial. Int J Pharmacol. 2005;1:311–5. [Google Scholar]
- 46.Karim B, Bhaskar DJ, Agali C, Gupta D, Gupta RK, Jain A, et al. Effect of Aloe vera mouthwash on periodontal health: Triple blind randomized control trial. Oral Health Dent Manag. 2014;13:14–9. [PubMed] [Google Scholar]
- 47.Bhat G, Kudva P, Dodwad V. Aloe vera: Nature's soothing healer to periodontal disease. J Indian Soc Periodontol. 2011;15:205–9. doi: 10.4103/0972-124X.85661. [DOI] [PMC free article] [PubMed] [Google Scholar]