Abstract
Background:
Many factors contribute to uneventful and healthy postoperative healing. Hence, closure of periodontal flap postsurgery for the attainment of primary union between flap margins is of utmost importance. Isoamyl 2-cyanoacrylate is a tissue adhesive, which can be used for the closure of elevated flaps to overcome the problems associated with conventional suture material like silk.
Aim:
This study aims to compare healing after periodontal flap surgery using isoamyl 2-cyanoacrylate (bioadhesive material) and silk sutures.
Materials and Methods:
The study was carried out on twenty patients who needed flap surgical procedure for pocket therapy.
Statistical Analysis Used:
Results were subjected to statistical analysis. Paired t-test was used for intragroup postprocedure improvement in each parameter, and independent sample t-test was used for intergroup comparison.
Results:
Early healing was seen with isoamyl 2-cyanoacrylate during the 1st week when compared with silk. However, no significant difference was seen in the 2nd week when both the materials were compared.
Conclusions:
It can be concluded that cyanoacrylate aids in early initial healing.
Key words: Conventional flap surgery, cyanoacrylate, sutures, tissue healing
INTRODUCTION
Several techniques have been employed for the treatment of periodontal pockets. Flap surgery for periodontal reattachment, demands close postoperative adaptation for the mature, gingival connective tissue onto the prepared tooth surface.[1,2,3]
Braided silk has a phenomenon of “wicking,” making it a site for secondary infection.[4,5] Furthermore, it has the maximum amount of inflammatory tissue response (Postlethwaite 1974). Hence, a need for an alternative to sutures is felt.
Cyanoacrylates are tissue adhesives that were synthesized in 1959 by Coover et al. The present study was carried out to evaluate healing after periodontal flap surgery using isoamyl 2-cyanoacrylate and silk sutures.
MATERIALS AND METHODS
In total, twenty patients were selected. Patients having moderate to severe periodontitis as assessed by clinical criteria (i.e., probing depth of ≥5 mm and bone loss on radiograph ≥50%) in consecutive three teeth in at least in two quadrants, between 20 and 50 years of age of both the sexes and demonstrating acceptable oral hygiene before surgical therapy were included in the study. Patients having any known systemic diseases and/or drug therapy which may interfere with wound healing, drug allergies to any of medications used in the study, habit of smoking, tobacco chewing, or any other habit that might influence the disease or the treatment and pregnant or lactating mother were excluded from this study. Informed written consent was obtained from all the subjects. The protocol was approved by the institutional review committee for human subjects, and the study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013.
Phase1 therapy and oral hygiene instructions were carried out for all the subjects. On completion of phase 1 therapy, subjects were called at 4 weeks for baseline measurements [Figures 1 and 2] and patients where inflammation had subsided were taken up for surgery.
Figure 1.

Baseline (4 weeks after completion of phase 1 therapy)
Figure 2.
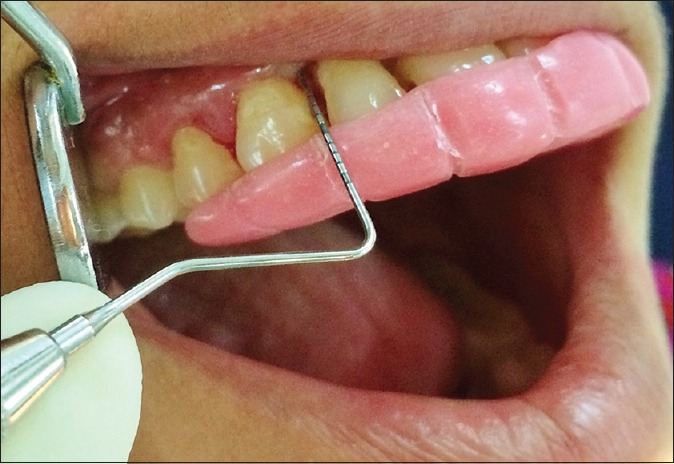
Pocket depth at baseline
On the day of the surgery, before surgical procedure a short case history including specific clinical parameters such as plaque index (Turesky–Gilmore–Glickman modification of the Quigley-Hein index), Sulcus bleeding index (Muhlemann and Sons), and periodontal probing depth was recorded.
Sulcus bleeding index and periodontal probing depth were assessed again 6 weeks and 3 months after surgery, plaque index at 1 week, 6 weeks, and 3 months postsurgery and early healing index (Watchtel et al.) was assessed after 1 and 2 weeks postsurgery.
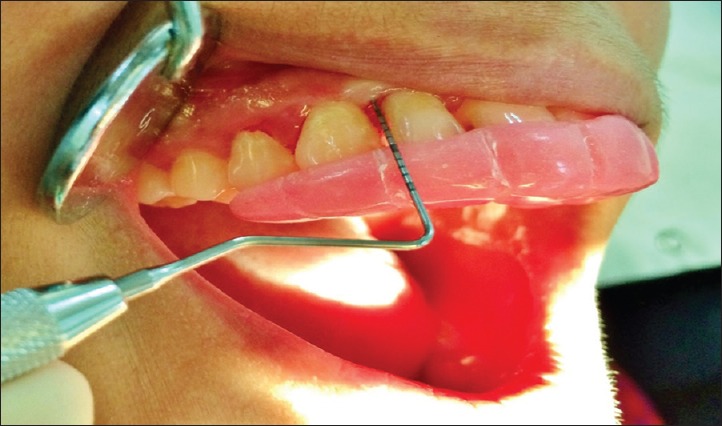
The surgical procedure was performed using routine local anesthesia (2% lignocaine with epinephrine 1:100,000) sulcular incision was made for all teeth. The conventional nondisplaced mucoperiosteal flap was then raised on the buccal and lingual/palatal aspects of teeth. Thorough debridement was carried by removing local irritants and diseased granulation tissue. After debridement, the flap was trimmed and repositioned to accomplish as much complete interproximal closure as possible [Figure 3].
Figure 3.

Flap reflection
The surgical area to be treated was randomly selected into two areas as Group A and Group B.
Group A: Sites where flap was secured with sutures (3-0 silk) after surgery.
Group B: Sites where flap was secured with isoamyl 2-cyanoacrylate after surgery [Figure 4].
Figure 4.

Immediate postoperative with sutures one site (11, 12, 13) and isoamyl 2-cyanoacrylate on the other site (21, 22, 23)
In one area, the flap was then sutured with surgical silk material using interrupted sutures as necessary. No periodontal pack was used.
Closure on the cyanoacrylate site was done with isoamyl 2-cyanoacrylate [Figure 5]. Isoamyl 2-cyanoacrylate was placed in a dropwise manner on the flap margins, which were held in place. The application was done till a thin film of set cyanoacrylate formed. No periodontal pack was used [Figure 6].
Figure 5.

Isoamyl 2-cyanoacrylate
Figure 6.

Application of isoamyl 2-cyanoacrylate
Postsurgical instructions were given. Sutures were removed after 1 week [Figure 7].
Figure 7.

Postoperative at 1 week, after suture removal
Objective (redness, crater formation, materia alba, presence of sutures) and subjective criteria (pain/discomfort, esthetic acceptance, burning sensation/itching) were noted. Subjects were recalled for a further checkup after 2 weeks, 6 weeks, and 3 months [Figures 8 and 9] postoperatively. All the postoperative parameter were checked and recorded in both sites.
Figure 8.
Postoperative pocket depth at 3 months
Figure 9.

Postoperative photograph taken at 3 months
The statistical analysis was performed using t-test.
RESULTS
The mean value of plaque index in Group A and Group B was almost similar at the baseline. The percentage improvement in plaque index for Group A and Group B at the 3 months in relation to baseline plaque index is 53.90% (Group A) and 56.00% (Group B) with P = 0.486. At 3 months approximately, a similar improvement in plaque index is evident in both groups. Thus, the relative improvement in plaque index is not significantly different between Group A and Group B [Figure 10].
Figure 10.
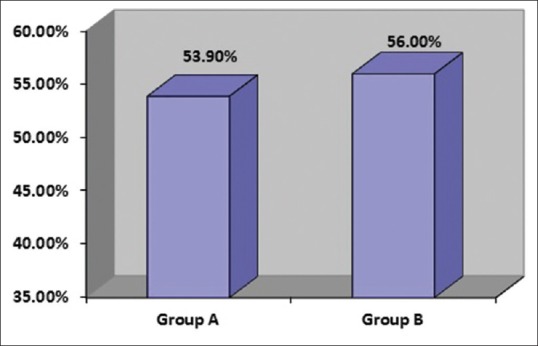
The comparison of percentage improvement in plaque index between two groups
The mean value of early healing index seen in Group A and Group B at 1 week was significantly different (P < 0.001). The mean value of early healing index at 2nd week was not significantly different between Groups A and B with P = 0.109. Similar levels of early healing index are evident in both groups in the 2nd week. Thus, early healing index is not significantly different between Group A and Group B in the 2nd week [Figure 11].
Figure 11.
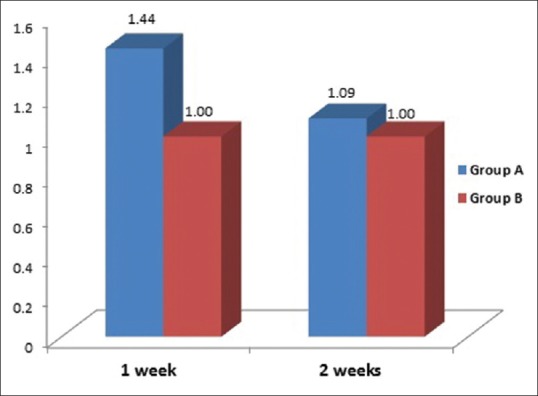
The comparison between Group A and Group B of early healing index at 1 week and 2 weeks follow-ups
The mean value of bleeding index in Group A and Group B was almost similar at the baseline. The improvement in the percentage of bleeding index for Group A and Group B at 3 months in comparison to baseline bleeding index is 99.20% (Group A) and 100.00% (Group B) with P = 0.324. At 3 months approximately, a similar improvement in bleeding index is evident in both groups. Thus, there is no significant difference in bleeding index is Group A and Group B [Figure 12].
Figure 12.
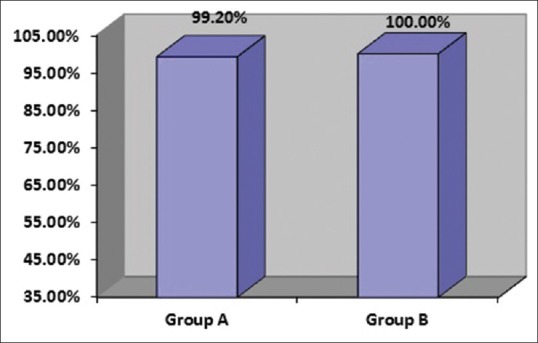
The comparison between Group A and Group B of percentage improvement in bleeding index between baseline and 3 months
The mean value of probing depth in Group A and Group B was almost similar at the baseline. The improvement in percentage seen in probing depth for Group A and Group B at 3 months in comparison to baseline probing depth is 68.90% (Group A) and 71.10% (Group B) with P = 0.240. At approximately, 3 months similar improvement in probing depth index is observed in both groups. Thus, there is no statistically significant difference in improvement in probing depth between Group A and Group B [Figure 13].
Figure 13.
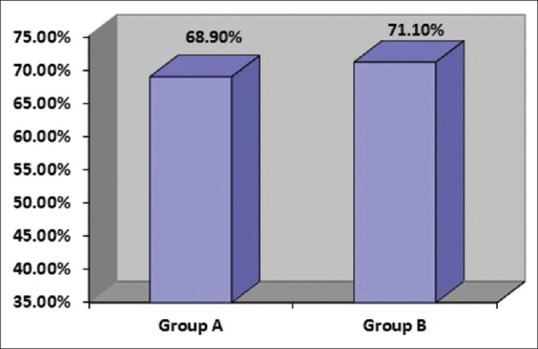
The comparison between Group A and Group B of percentage improvement in probing depth between baseline and 3 months
The incidence of pain/discomfort is significantly higher in Group A compared to Group B, the difference being statistically significant with P = 0.001. It is important to note that none of the cases from Group A and Group B had burning/itching sensation. All cases of Group B showed esthetical acceptability compared to Group A, the difference being statistically significant with P = 0.001. Thus, after 1 week absence of pain/discomfort or burning/itching was seen in Group B and also everyone from Group B showed esthetical acceptability [Figure 14].
Figure 14.
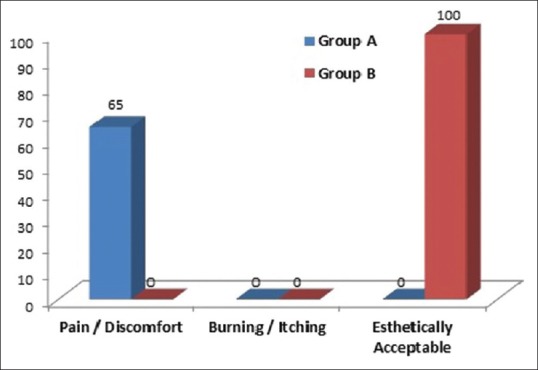
The comparison of subjective parameters between Group A and Group B after 1 week posttreatment
The incidence of redness did not differ significantly between Group A and Group B with P = 0.147. It is important to note that absence of crater formation at the tip of papillae and absence of loss of sutures was seen in Group A and Group B. All cases of Group A showed the presence of materia alba/debris whereas all cases of Group B showed absence of materia alba/debris the difference being statistically significant with P = 0.001. Thus, after 1 week redness, crater formation at the tip of papillae, materia alba/debris was absent in Group B [Figure 15].
Figure 15.
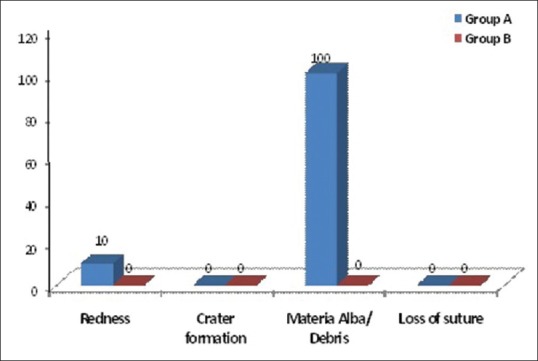
The comparison of objective parameters between Group A and Group B after 1 week posttreatment
DISCUSSION
Statistically significant reduction of plaque index was seen in Group B compared to Group A from baseline to 1 week. After 6 weeks and 3 months, no significant difference was seen in plaque index when both groups were compared. Similar observations were seen in a study carried by Padhye and Pol.[6]
Statistically significant reduction in early healing index was seen in Group B compared to Group A after 1 week. No significant difference was seen in healing after 2 weeks when both groups were compared. The finding was in conjunction with study done by Vastani and Maria.[7]
Statistically significant reduction of sulcus bleeding index was seen in Group B as compared to Group A from baseline to 6 weeks and 3 months. A similar result was seen by Padhye and Pol.[6]
Statistically significant reduction of periodontal probing depth was seen in Group B as compared to Group A from baseline to 6 weeks and 3 months.
Statistical significant difference was seen when pain/discomfort, burning/itching, and esthetics was assessed between the sutured site and the site where isoamyl 2-cyanoacrylate was applied. Isoamyl 2-cyanoacrylate showed the absence of pain/discomfort, absence of burning/itching and was found to be esthetically acceptable by all subjects. Results were in conjunction with study done by Giray et al.[8]
Statistically significant difference was seen when redness, crater formation at tip of papillae, loss of suture, and accumulation of materia alba were assessed after 1 week between the sutured site and the site where isoamyl 2-cyanoacrylate was applied. The absence of redness, absence of crater formation at the tip of papilla and absence of materia alba were seen in the site where isoamyl 2-cyanoacrylate was applied.
Padhye and Pol[6] stated that cyanoacrylate has an added advantage with respect to time and methodology of diminishing the two-step procedure of suturing followed by dressing to just one step of application of the material.
Time taken during surgical procedures using cyanoacrylate is crucial because it:
Lessens trauma to the patient
Lessens fatigue to the surgeon
Reduces postoperative swelling and operating time
Easier to apply than suture
More comfortable to the patient.
Other advantages are, in cyanoacrylate tissue adaptation is better, and healing is faster. Forrest[9] reported that the tissue adaptation is better as it provides fixation of the flap to the whole surface, while sutures provide only marginal fixation. Miller et al.[10] have shown similar findings.[6]
Moreover, cyanoacrylate also saves cost of preparing, sterilization, and storing instruments at the time of suture removal.
Advantages of cyanoacrylate from subjects point of view:
At times, removal of sutures is annoying/painful for some patients
There is less discomfort on sutureless site in the days after surgery.
From the result of our study, it is clear that the healing after 1 week was better in the site where isoamyl 2-cyanoacrylate was applied compared to the sutured site, though healing after 2nd week is similar in both groups.
Similarly, isoamyl 2-cyanoacrylate was found to be better when plaque index was considered as compared to sutured site after 1 week, though no significant difference was seen after 6 weeks and 3 months when both groups were compared.
Isoamyl 2-cyanoacrylate is also found to be better as compared to sutures as it has advantages such as immediate hemostasis, easy application, no technical skill is required, patient acceptance, esthetically more acceptable, noninvasive, less chair side time, absence of postsurgical pain or infection, easy maintenance, and no food lodgment. Moreover, the biologic sealant is well accepted by the oral tissues and shows good acceptability with no side effects by all the subjects in the study.
Thus, looking at these aspects isoamyl 2-cyanoacrylate can be easily, routinely, and conveniently used for closure after periodontal flap surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carranza FA. General principles of periodontal surgery. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, editors. Carranza's Clinical Periodontology. 10th ed. Philadelphia: W.B. Saunders and Company; 2007. pp. 887–901. [Google Scholar]
- 2.Levin MP. Periodontal suture materials and surgical dressings. Dent Clin North Am. 1980;24:767–81. [PubMed] [Google Scholar]
- 3.Ramfjord SP. Surgical pocket therapy. Int Dent J. 1977;27:263–9. [PubMed] [Google Scholar]
- 4.Macht SD, Krizek TJ. Sutures and suturing – Current concepts. J Oral Surg. 1978;36:710–2. [PubMed] [Google Scholar]
- 5.Kulkarni S, Dodwad V, Chava V. Healing of periodontal flaps when closed with silk sutures and N-butyl cyanoacrylate: A clinical and histological study. Indian J Dent Res. 2007;18:72–7. doi: 10.4103/0970-9290.32424. [DOI] [PubMed] [Google Scholar]
- 6.Padhye A, Pol DG. Clinical evaluation of the efficacy of N-butyl 2-cyanoacrylate as bioadhesive material in comparison to conventional silk sutures in modified widman flap surgery in anterior region. JIDA. 2011;5:899–904. [Google Scholar]
- 7.Vastani A, Maria A. Healing of intraoral wounds closed using silk sutures and isoamyl 2-cyanoacrylate glue: A comparative clinical and histologic study. J Oral Maxillofac Surg. 2013;71:241–8. doi: 10.1016/j.joms.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 8.Giray CB, Atasever A, Durgun B, Araz K. Clinical and electron microscope comparison of silk sutures and n-butyl-2-cyanoacrylate in human mucosa. Aust Dent J. 1997;42:255–8. doi: 10.1111/j.1834-7819.1997.tb00130.x. [DOI] [PubMed] [Google Scholar]
- 9.Forrest JO. The use of cyanoacrylates in periodontal surgery. J Periodontol. 1974;45:225–9. doi: 10.1902/jop.1974.45.4.225. [DOI] [PubMed] [Google Scholar]
- 10.Miller GM, Dannenbaum R, Cohen DW. A preliminary histologic study of the wound healing of mucogingival flaps when secured with the cyanoacrylate tissue adhesives. J Periodontol. 1974;45:608–18. doi: 10.1902/jop.1974.45.8.2.608. [DOI] [PubMed] [Google Scholar]


