Abstract
Aim:
The study aimed to assess the levels of awareness about the mutual relationship between diabetes and periodontitis among high-risk age group of the general population and to assess the attitude of general physicians in suggesting diabetic patients to visit a dentist.
Materials and Methods:
A structured, closed-ended questionnaire either in English or in local language (Telugu) was distributed and collected from 203 patients who were willing to participate in the study attending the Department of Periodontics, Narayana Dental College & Hospital, Nellore, AP. Data were statistically analyzed and represented in percentages and number.
Results:
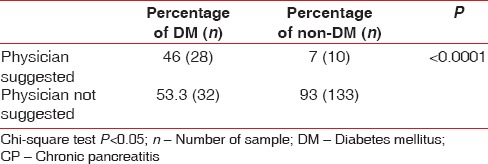
Only 49.8% of the sample population knew about the mutual relationship between diabetes and periodontitis and only 46% of the diabetic study population was suggested to visit a dentist by the physician.
Conclusion:
There is an insufficient knowledge among the diabetic population regarding the mutual relationship. Only few physicians have suggested their diabetic patients to visit a dentist. As diabetic patients tend to visit a physician earlier than a dentist, it is their responsibility to educate and motivate their patients to seek dental treatment.
Key words: Cytokines, diabetes mellitus, general physicians, hyperglycemia, periodontitis
INTRODUCTION
Periodontitis is a common local inflammatory disease of tooth-supporting tissues initiated by microorganisms present in the dental plaque. As the disease progresses, there is periodontal pocket formation with increased attachment loss, alveolar bone destruction, and increased tooth mobility that ultimately result in the loss of teeth. Association between various systemic diseases and periodontitis has long been established and it is the focus of most researches in the recent past. Diabetes mellitus (DM) is a commonly prevalent systemic disease and has been proved to have a bidirectional relationship with periodontitis.[1]
Diabetes is characterized by hyperglycemia (elevated blood glucose) that results from defects in the secretion of the hormone insulin or from impaired insulin action or both. Alterations in lipid and protein metabolism are also seen. Chronic hyperglycemia is associated with long-term dysfunction and damage to numerous end-organs, with marked effects on the eyes, kidneys, heart, nerves, and blood vessels.[2]
Although periodontitis is a recognized complication of diabetes, people with well-controlled diabetes, having good oral hygiene, are not at an increased risk of periodontitis. However, their susceptibility to periodontitis is significantly increased when their diabetes is poorly controlled, particularly smokers.
National diabetes fact sheet, 2011, presented by the Centres for Disease Control and Prevention (CDC) reported that adults aged 45 years or older with poorly controlled diabetes were 2.9 times more likely to develop severe periodontitis than nondiabetics.[3] In the successful treatment and prevention of both these commonly prevalent diseases, knowledge about their mutual influence among the dentists, general practitioners, and patients plays a critical role.
In addition, general practitioners and health-care providers for diabetic patients should also possess basic dental knowledge to find out the signs and symptoms of dental diseases to provide appropriate treatment or advice to visit a dentist.
Hence, the present study aimed to assess the levels of awareness about the relationship between diabetes and periodontitis among high-risk age group of the general population of Nellore. In addition, the attitude of general physicians in suggesting the diabetic patients to visit a dentist has also been assessed.
MATERIALS AND METHODS
A structured, closed-ended questionnaire was prepared in English and in the local language (Telugu) for evaluating the main aim of the study. The study was designed and conducted at the Department of Periodontics, Narayana Dental College & Hospital, Nellore, AP. The questionnaire was distributed among patients attending the outpatient unit of the department and satisfying the following selection criteria: Patients of age 40–55 years; patients without any condition that limits their ability to brush their teeth; patients with not <20 teeth; and patients who can read and write either in English or in the local language (Telugu).
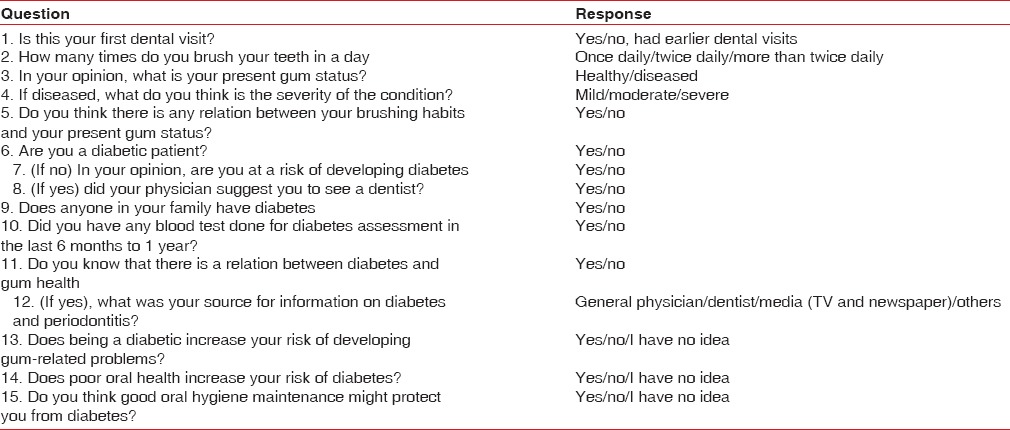
Patients who readily agreed to participate in the study were provided with the self-constructed questionnaire [Table 1].[4] Prior to study, a questionnaire was pretested and validated. The questionnaire was validated for construct and content validity, reliability, and ease of use. Content and construct validity shows no significant changes. Questionnaire showed high degree (0.89) of agreement during test-retest of questionnaire. Demographic data such as age, sex, educational status, and occupation have been recorded and documented. Two hundred and three participants were included in the study and the completed questionnaire forms from the participants were collected and analyzed. The collected data were imported into the Statistical Package for Social Sciences version 21 (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) for statistical analysis. Data were represented in frequency, percentages, and graphs. Chi-square test was used for assessing the association between diabetic population and knowledge about the mutual relationship.
Table 1.
Questionnaire
RESULTS
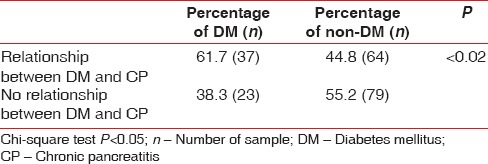
Demographic data of the study population including response to questionnaire were represented in Table 2. Out of the 203 patients questioned, 123 were males and 80 were females. Nearly, 4.4% were from health-related professions such as pharmacy, nursing, and paramedical. A composition of 30% of the studied population were reportedly first-time visitors to a dentist. Nearly, 29.6% of the studied population were diabetic and 44.8% had a family history of diabetes, of which, 37.1% are nondiabetic but having a family history of diabetic. In spite of being at a high risk (based on age ≥40 years) for diabetes, 37.9% of the studied population did not undergo any blood test for screening DM in the past 6 months and 13.79% had not undergone any blood test knowing the family history of diabetes. Only 49.8% of the sample population knew about the mutual relationship between diabetes and periodontitis and the percentage of knowledge about mutual relationship between diabetic and nondiabetic population is shown in Table 3 and the source of information regarding mutual relationship is shown in Graph 1. General physicians have suggested only 46% of their diabetic patients to visit a dentist [Table 4]. Nearly, 21.2% of the studied population had no idea that diabetes would cause periodontal problems, 60% of the diabetic population agreed that their current oral status is related to diabetes, and 46.66% felt that they had periodontal problems.
Table 2.
Response to questionnaire
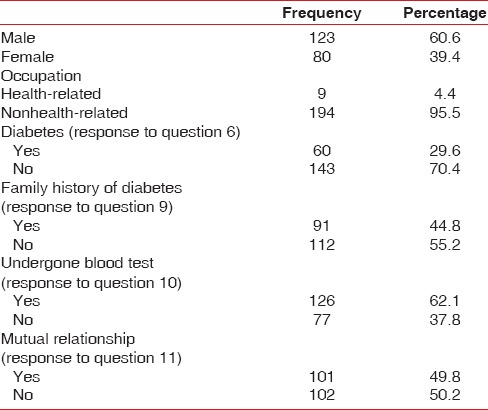
Table 3.
Percentage of diabetic and nondiabetic population knowledge about mutual relationship
Graph 1.
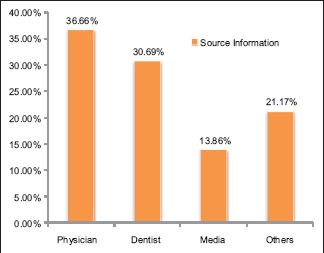
Source of information regarding mutual relationship
Table 4.
Percentage of physician suggesting study population to visit a dentist
DISCUSSION
Both periodontitis and DM are frequent chronic diseases and generate enormous costs for the public health-care system. Numerous studies, review articles,[5,6] and meta-analyses[1] indicated a mutual influence between periodontitis and DM.
Grossi and Genco in 1998 proposed that the relation between periodontitis and diabetes is bi-directional,[7] this was further supported by Taylor.[8]
Various factors have been reported that deter patients with DM from seeking dental care, including financial factors, the fear of dental treatment, and lack of knowledge of the need for dental check-up. Type 2 DM patients were 2.8 times more likely to have destructive periodontal disease[9] and 4.2 times more likely to have alveolar bone loss progression.[10] Mealey and Oates in 2006[5] have shown the prevalence of periodontitis in diabetic subjects that is estimated to be double or even triple the number in the normal population.
The World Dental Federation and International Diabetes Federation have pointed out that the key for the prevention of periodontitis in patients with DM lies in close collaboration between dentists and physicians.
However, in the present study, an attempt has been made to estimate the knowledge about the established bi-directional relationship between diabetes and periodontitis by questionnaire study. We limited the age group to be between 40 and 55 years based on the National diabetes fact sheet, 2011, by CDC. Education qualification of minimum of 10th class was set as a limit so that participants can read and write either English or local language (Telugu). No data regarding higher education were collected.
Occupation of the participants was categorized as health-related and nonhealth-related professions. Number of participants related to health profession was insignificant, i.e., 4.4%, which has a negligible impact on the study.
According to a study by Aggarwal and Panat,[11] only 10.8% of the patients with DM visit a dentist for regular check-ups and Indians with type 2 diabetes reported suboptimal oral hygiene behavior.
Weinspach et al.[3] reported that a total of 56% of the participants of their study had an insufficient knowledge about the mutual influence between diabetes and periodontitis, which correlates with the current study (50.2%). Among the diabetic study population, 38.3% had no idea about mutual relationship (P < 0.02).
Lin et al.[12] stated that endocrinologists and dentists are not equally equipped with the knowledge about the relationship between DM and periodontitis. In our study, only 46% (P < 0.0001) of the general physicians suggested their patients to visit a dentist. There is a wide gap between their practice and the current evidence.
These findings suggest that there is a significant need for increased knowledge of mutual relationship and adoption of preventive oral hygiene behaviors that would improve oral health among diabetics.
Limitations and future considerations
Smaller sample size too early to generalize the results
Stratification of education levels was not done in the study. Higher level of education may influence the knowledge about relationship
Further studies with larger sample size and inclusion of level of education might potentiate the study.
CONCLUSION
There is an insufficient knowledge among the high-risk age group individuals about the mutual relationship between diabetes and periodontitis. To promote proper oral health and to reduce the risk of oral diseases, health professionals in both the dental and medical fields need to take responsibility for educating the public about the oral manifestations of diabetes and its complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chávarry NG, Vettore MV, Sansone C, Sheiham A. The relationship between diabetes mellitus and destructive periodontal disease: A meta-analysis. Oral Health Prev Dent. 2009;7:107–27. [PubMed] [Google Scholar]
- 2.Mealey BL, Moritz AJ. Hormonal influences: Effects of diabetes mellitus and endogenous female sex steroid hormones on the periodontium. Periodontol 2000. 2003;32:59–81. doi: 10.1046/j.0906-6713.2002.03206.x. [DOI] [PubMed] [Google Scholar]
- 3.Weinspach K, Staufenbiel I, Memenga-Nicksch S, Ernst S, Geurtsen W, Günay H. Level of information about the relationship between diabetes mellitus and periodontitis – Results from a nationwide diabetes information program. Eur J Med Res. 2013;18:6. doi: 10.1186/2047-783X-18-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eldarrat AH. Awareness and attitude of diabetic patients about their increased risk for oral diseases. Oral Health Prev Dent. 2011;9:235–41. [PubMed] [Google Scholar]
- 5.Mealey BL, Oates TW. American Academy of Periodontology. Diabetes mellitus and periodontal diseases. J Periodontol. 2006;77:1289–303. doi: 10.1902/jop.2006.050459. [DOI] [PubMed] [Google Scholar]
- 6.Casanova L, Hughes FJ, Preshaw PM. Diabetes and periodontal disease: A two-way relationship. Br Dent J. 2014;217:433–7. doi: 10.1038/sj.bdj.2014.907. [DOI] [PubMed] [Google Scholar]
- 7.Grossi SG, Genco RJ. Periodontal disease and diabetes mellitus: A two-way relationship. Ann Periodontol. 1998;3:51–61. doi: 10.1902/annals.1998.3.1.51. [DOI] [PubMed] [Google Scholar]
- 8.Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: An epidemiologic perspective. Ann Periodontol. 2001;6:99–112. doi: 10.1902/annals.2001.6.1.99. [DOI] [PubMed] [Google Scholar]
- 9.Emrich LJ, Shlossman M, Genco RJ. Periodontal disease in non-insulin-dependent diabetes mellitus. J Periodontol. 1991;62:123–31. doi: 10.1902/jop.1991.62.2.123. [DOI] [PubMed] [Google Scholar]
- 10.Taylor GW, Burt BA, Becker MP, Genco RJ, Shlossman M. Glycemic control and alveolar bone loss progression in type 2 diabetes. Ann Periodontol. 1998;3:30–9. doi: 10.1902/annals.1998.3.1.30. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal A, Panat SR. Oral health behavior and HbA1c in Indian adults with type 2 diabetes. J Oral Sci. 2012;54:293–301. doi: 10.2334/josnusd.54.293. [DOI] [PubMed] [Google Scholar]
- 12.Lin H, Zhang H, Yan Y, Liu D, Zhang R, Liu Y, et al. Knowledge, awareness, and behaviors of endocrinologists and dentists for the relationship between diabetes and periodontitis. Diabetes Res Clin Pract. 2014;106:428–34. doi: 10.1016/j.diabres.2014.09.008. [DOI] [PubMed] [Google Scholar]


