Abstract
Most individuals who develop Major Depressive Disorder (MDD) will experience a recurrent depressive episode; we know little, however, about cognitive mechanisms that increase the likelihood of recurrence. In the current study we examined whether negatively biased self-referential processing, negative life events, baseline depressive symptoms, and psychotropic medication use predicted the onset of a subsequent depressive episode in a longitudinal study of women with a history of recurrent MDD. Higher levels of depressive symptoms at baseline predicted experiencing a greater number of negative life events which, in turn, tended to predict recurrence of depression. Importantly, after accounting for other associations, negatively biased self-referential processing contributed unique variance to the likelihood of experiencing a depressive episode over the next three years. Thus, negatively biased self-referential processing appears to be a significant risk factor for the recurrence of depressive episodes and may be an important target for interventions aimed at preventing future episodes.
Keywords: self-referent encoding, depression, recurrence, cognitive processes
Major Depressive Disorder (MDD) is highly recurrent. At least half of individuals with a history of MDD will experience another episode of depression within a few years of recovery from the original episode (Keller et al., 1992). Moreover, recurrence rates are as high as 70% for individuals who have already experienced two depressive episodes (Solomon et al., 2000). Given these alarming statistics and the enormous costs of MDD (World Health Organization, 2012), it is critical that we identify predictors of recurrence in individuals with a history of MDD, and ultimately intervene to alter the underlying pathophysiological mechanisms. In the current study, we aimed to examine whether negatively biased self-referential processing increases the risk for recurrence after accounting for demographic and clinical variables that are known to influence recurrence, including baseline depressive symptoms, psychotropic medication use, and stressful life events.
Cognitive theories of depression (Beck, 1967; Teasdale, 1988) emphasize that negative biases in the cognitive processing of emotional information play a critical role in the onset, maintenance, and recurrence of depressive episodes. For example, Beck (1967) posited that negative cognitive schemas are a salient risk factor for depression; they are conceptualized as negatively biased representations of self-referential cognition that influence the way in which individuals attend to, interpret, and recall emotional information. Moreover, in his differential activation hypothesis, Teasdale (1988) proposed that patterns of information processing become established during initial depressive episodes and then influence cognition when individuals experience a dysphoric mood state. Specifically, dysphoric mood negatively biases information processing, thereby increasing negative interpretations of events, making negative self-referential constructs more accessible and, ultimately, increasing the likelihood of recurrence.
Historically, research examining cognitive predictors of recurrence has relied exclusively on self-report measures of cognition (e.g., Alloy et al., 2006; Segal et al., 2006; see Lau, Segal, & Williams, 2004, for a review). However, there are drawbacks to this approach. Self-report measures are limited by individual differences in participants’ level of insight and self-awareness. They are also subject to recall, demand, and reference biases. Moreover, because of the use of Likert scales, self-report measures are subject to response bias and diminished sensitivity. It is for these and other reasons that information-processing tasks have increasingly been used to elucidate the nature of cognitive biases in other domains of depression research. Indeed, information-processing tasks have been central in advancing our understanding of individuals who are currently depressed. There is now a wealth of evidence from studies of performance on information-processing tasks demonstrating that currently depressed individuals are characterized by negative biases in attention, memory, and interpretation (Beevers, 2005; Gotlib & Joormann, 2010; Mathews & MacLeod, 2005). Moreover, researchers using information-processing tasks have found that formerly depressed individuals also show biases in attention and memory (see Joormann & Arditte, 2015, for a review). In fact, there is growing evidence that, compared to participants without a history of depression, formerly depressed participants exhibit negatively biased self-referential processing when they are in a negative mood state (Fritzsche et al., 2010; Kircanski, Mazur, & Gotlib, 2013). Biased self-referential processing reflects participants’ underlying negative cognitive schemas (Beck, 1967) and, thus, might be an important marker of vulnerability to depression. To date, however, investigators have used exclusively self-report measures to examine cognitive predictors of episode recurrence in depression. Thus, we do not know whether performance on a self-referential processing task can predict the onset of future depressive episodes.
This study is the first to examine whether performance on an information-processing task predicts the onset of a subsequent depressive episode. We recruited women who were currently not depressed but who had experienced two or more depressive episodes, both to increase the homogeneity of our sample and because this population is at high risk for recurrence (Mueller et al., 1999; Solomon et al., 2000). At baseline, we assessed self-referential processing using the self-referential encoding task (SRET; Derry & Kuiper, 1981). Importantly, following recovery from a depressive episode, cognitive biases can remain latent until they are activated by a negative mood induction (Teasdale, 1988). Therefore, before participants completed the SRET, we induced a negative mood state (see also Taylor & Ingram, 1999, and Joormann, Talbot, & Gotlib, 2007). Moreover, given the evidence demonstrating that risk for recurrence is influenced by baseline depressive symptoms, psychotropic medication use, and stressful life events (Judd et al., 1998; Hammen, 2005), we included these variables as predictors in our model of depression recurrence in order to assess the unique contribution of self-referential processing after accounting for these variables. Because baseline depressive symptoms have been found to influence the experience of subsequent negative life events (Hammen, 2005), we hypothesized that more severe depressive symptoms at baseline would predict a higher number of negative life events, which in turn would predict future episodes of depression. We also hypothesized that more negatively biased self-referential processing would predict recurrence above and beyond associations with other variables included in the model.
Method
Participants
Participants were 100 women diagnosed with Major Depressive Disorder, Recurrent, in Full Remission, defined as having at least two past depressive episodes but not having experienced a major depressive episode (MDE) for the past two months. Women were recruited from the community and screened for initial inclusion/exclusion criteria via a telephone interview; potentially eligible participants came to the laboratory for an in-person diagnostic interview (the Structured Clinical Interview for DSM IV Axis I Disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 2002) to assess current and past psychopathology. Interviews were conducted by post-baccalaureate research assistants who received extensive training on DSM-IV-TR diagnostic criteria and on administration of the SCID-I. Inter-rater reliability was excellent (K = .93). Individuals were excluded if they had experienced severe head trauma, were not fluent in English, had learning disabilities, bipolar disorder, or psychotic symptoms, or met Diagnostic and Statistical Manual of Mental Disorders (4th ed; DSM-IV-TR; American Psychiatric Association, 2000) criteria for alcohol or substance abuse within the past six months.
Baseline Assessment
Mood induction
We induced a negative mood state by having participants watch one of three randomly-assigned, six-minute film clips (Dead Poets Society, Weir, 1989; My Girl, Zieff, 1991; Stepmom, Columbus, 1998). While viewing the film clip and for an additional two minutes following the clip, participants imagined being in the situation and the feelings they would experience in the situation (see Westermann, Spies, Stahl, and Hesse, 1996). Participants rated their mood before and after the mood induction on a 5-point Likert scale ranging from 1 = very sad to 5 = very happy.
Self-referential encoding task
The SRET consisted of 40 adjectives: 20 positive (e.g., happy, interesting) and 20 negative (e.g., boring lazy; see supplement). To construct the SRET, we compiled a larger list of adjectives from previous studies of information processing in depression. Five psychology graduate students then rated each word in the list as having a positive or a negative valence; adjectives were retained only if agreement was unanimous. The final positive and negative word lists did not differ in word length, familiarity, or level of arousal (all ps > .05).
The SRET was presented using e-prime software Version 1.1. Participants were seated in front of a computer and were instructed to place their right index finger on a key labeled ‘yes’ and their left index finger on a key labeled ‘no.’ Each trial began with the phrase ‘Describes me?’ presented in the middle of the screen for 500 ms. After 250 ms, participants were presented with one of the adjectives in random order and were instructed to indicate whether the word described them by pressing the corresponding key. Participants’ responses were recorded on each trial. Lastly, a 1,000 ms fixation cross was presented. Participants completed several practice trials, followed by the experimental trials, during which the experimenter was outside of the room.
Participants then worked for 3 minutes on a distractor task, the digit-symbol task of the WAIS-R (Wechsler, 1981). The experimenter then returned to administer an incidental recall task. Participants were given a sheet of paper and were asked to recall as many words as possible from the SRET, regardless of whether they had endorsed the words as self-descriptive. There was no time limit.
We calculated four dependent variables from the SRET task: number of positive and of negative words endorsed as self-referential, and number of positive and of negative words recalled. To be consistent with recent research (e.g., Fritzsche et al., 2010; Kircanski et al., 2013), and to control for individual differences in rates of overall endorsement and recall, we computed recall of endorsed positive and negative words as proportions of the total number of words endorsed and recalled. Because these proportions sum to 1, and analyses of positive and negative words produce identical coefficients with the opposite sign, we present recall results only for negative words. Although some researchers have also examined participants’ reaction time to assess the self-relevance of each word, we did not use this approach in the current study because our version of the SRET did not instruct participants regarding response time. Consequently, numerous factors (e.g., lapses in concentration, unexpected distractions) could confound interpretation of reaction-time data. Therefore, consistent with recent research (e.g., Kircanski et al., 2013), we analyzed the number of positive and of negative words endorsed as self-referential.
Self-report measures
Participants completed the Beck Depression Inventory-II (BDI; Beck, Steer, & Brown, 1996), a 21-item measure of depressive symptoms. They also completed the Shipley Institute of Living Scale (Shipley, 1940), a vocabulary test that provides a reliable estimate of verbal intelligence and that is frequently used to ensure the observed group differences on cognitive tasks are not due to differences in verbal ability (Weiss & Schell, 1991).
Follow-up Assessments
Subsequent MDE
We followed participants for three years after their Time 1 visit or until they experienced a recurrent depressive episode. During this time, participants were asked to return to the laboratory approximately every 18 months to complete the SCID-I and self-report questionnaires. Of the original 100 participants, 19 were lost to attrition and 22 returned to the laboratory but did not complete the SCID-I during the follow-up assessment, typically due to time constraints. The current study was part of a larger longitudinal investigation examining girls at risk for depression based on their mothers’ history of the disorder; therefore, when time was constrained, assessments related to the daughters were prioritized. For the remaining 59 participants, interviewers used the SCID-I to assess whether participants experienced an MDE since their last assessment. If a participant did not attend her 18-month follow-up visit (Time 2), we assessed the presence of a depressive episode since her initial Time 1 visit at the 3-year visit (Time 3). Of the 59 participants, 29 (49.15%) experienced an MDE within three years of their baseline assessment. Missing data resulting from participant attrition were unrelated to participants’ age, ethnicity, marital status, household income, education, baseline depressive symptoms, psychotropic medication use, Shipley test scores, or SRET performance, ps > .05.
Negative Life Events
Following the SCID, participants reported on the life events that they had experienced since the previous assessment using the Life Events Survey (LES; Sarason, Johnson, & Siegel, 1978). Participants reported on the presence of a total of 50 life events (e.g., death of a family member, end of a romantic relationship). A total negative life events score was computed by calculating the average number of negative life events that were endorsed per month since the last assessment. Thus, a negative life events score of 1.0 would indicate that a participant had experienced, on average, one negative life event per month since her last assessment. Negative life event scores were examined for the period immediately prior to the recurrent depressive episode for those participants who experienced a recurrence, or for the matched follow-up assessment period for those participants who did not experience a recurrence. For example, if a participant experienced a recurrence of depression at the first follow-up assessment, we examined negative life event scores reported at the first follow-up assessment both for that participant and for the matched participant who did not experience a recurrence of depression.
Procedure
Within one week of their diagnostic evaluation, eligible participants were scheduled for their baseline assessment (Time 1), where they completed a measure of mood and a negative mood induction. They then completed a second mood measure followed by the SRET. To assess the occurrence of another depressive episode within three years of the baseline assessment, participants returned to the laboratory approximately every 18 months for three years or until they experienced a recurrent depressive episode. During these follow-up assessments, participants were administered the SCID and reported on negative life events experienced since their last assessment.
Planned Analyses
In order to test simultaneous predictors of recurrence while also accounting for hypothesized interrelations among the predictors, we used Mplus version 7.0 statistical software (Muthén & Muthén, 2012) to conduct structural equation modeling (SEM) analyses. SEM has advantages over other analytic approaches, including the ability to handle missing data without the need for listwise deletion or imputation (Asparouov & Muthén, 2010). Our model consisted of two parts: (1) a measurement model that consisted of factor loadings for the observed SRET variables (number of negative and of positive words endorsed as self-relevant and proportion of negative words recalled) that indexed the latent factor of self-referential processing (‘SRET’); and (2) a structural model that consisted of path and correlation coefficients that connected the latent and observed variables in a model predicting recurrence of a depressive episode within three years. Our structural model was developed based on a priori expectations of predictors of depression recurrence, which was treated as a categorical variable. We used weighted least squares mean variance (WLSMV) as is recommended for categorical variables (Muthén, du Toit, & Spisic, 1997).
Results
Participant Characteristics
Demographic and clinical characteristics of participants are presented in Table 1. Participants who experienced a recurrence of depression (REC) and those who did not (NREC) did not differ significantly in age, t(57) = 1.34, ethnicity, χ2(4, N = 58) = 7.49, marital status, χ2(2, N = 59) = 0.93, household income, χ2(4, N = 53) = 2.76, education, χ2(6, N = 59) = 6.72, Shipley test scores, t(56) = 1.54, number of previous depressive episodes t(40) = 0.62, p = .537, baseline BDI scores, t(57) = 1.68, or proportion taking psychotropic medication, χ2(1, N = 59) = 2.05, all ps = ns. We also examined group differences in SRET performance at baseline. Compared to participants in the NREC group, participants in the REC group endorsed significantly fewer positive words, t(43) = 2.80, p = .008, and recalled a higher proportion of negative words that were endorsed, t(43) = −2.12, p = .032; the two groups did not differ in the number of negative words endorsed, t(43) = −1.36, p = .179. Participants’ SRET performance was not related to their number of previous depressive episodes, |rs|(63) < .08, ps > .521.
Table 1.
Participant Characteristics
| Variable | Non-Recurrence (N = 30) | Recurrence (N = 29) |
|---|---|---|
| Baseline age, M(SD) | 42.59 (6.00) | 44.76 (6.44) |
| Ethnicity | ||
| Caucasian, % | 83.33% | 75.00% |
| African American, % | 6.67% | 0.00% |
| Latina, % | 0.00% | 14.29% |
| Asian, % | 10.00% | 7.14% |
| Other, % | 0.00% | 3.57% |
| Married, % | 63.33% | 62.07% |
| Household income<$100k, % | 42.86% | 60.00% |
| College education, % | 73.33% | 82.76% |
| Shipley | 59.43 (7.17) | 56.61 (6.77) |
| Previous Depressive Episodes | 5.71 (5.03) | 6.61 (4.08) |
| Baseline BDI, M(SD) | 11.40 (10.05) | 15.55 (8.87) |
| Psychotropic medication, % | 60.00% | 41.38% |
| SRET | ||
| Positive Words Endorsed | 14.41 (3.92) | 11.22 (3.73) |
| Negative Words Endorsed | 5.77 (3.34) | 7.13 (3.32) |
| Proportion Negative Words Endorsed and Recalled | 23.10% (19.50%) | 34.75% (16.51%) |
| Negative Life Events Scores | 0.26 (0.20) | 0.40 (0.26) |
Note. BDI = Beck Depression Inventory; SRET = Self-Referential Encoding Task
Mood Induction
To examine the effectiveness of the mood induction, we conducted a group (REC, NREC) by time (baseline, post-film) repeated-measures analysis of variance (ANOVA) on self-reported mood. As expected, this analysis yielded a significant main effect of time, F(1, 54) = 84.69, p < .001, η2 = 0.61, 95% CI (0.43, 0.71). Participants’ mood significantly declined from before (M = 3.86, SD = 0.52) to after (M = 2.70, SD = 0.93) watching the video clip. Neither the main effect of group nor the interaction of group and time was significant, Fs(1, 54) < 2.24, ps > .14, η2s < .04. Thus, mood at the time of the SRET would not explain observed group effects.
Predicting Depression Recurrence
Model fit
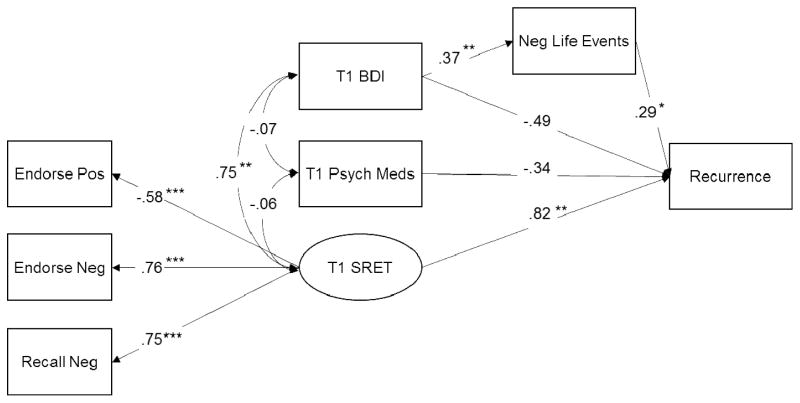
Results indicated that the a priori model was a strong fit to the data: Comparative Fit Index (CFI) = 0.997, Tucker Lewis Index (TLI) = 0.993, and Root Mean Square Error of Approximation (RMSEA) = 0.015 (see Figure 1). No modification indices greater than 10.0 were suggested.
Figure 1.
Standardized parameter estimates from the SEM model predicting recurrence of a major depressive episode within three years. ***p < .001, **p < .05, *p < .10. BDI = Beck Depression Inventory; SRET = Self-Referential Encoding Task
Parameter estimates
As can be seen in Figure 1, all three of the SRET variables loaded significantly on the SRET latent variable. As expected, number of positive words endorsed loaded negatively on the SRET latent variable, β = −0.58, p < .001, 95% CI (−1.10, −0.06), and both number of negative words endorsed, β = 0.76, p < .001, 95% CI (0.23, 1.29), and proportion of negative words recalled, β = 0.75, p < .001, 95% CI (0.22, 1.27), loaded positively on the SRET latent variable. Thus, higher scores on the SRET latent variable represent more negatively biased self-referential processing.
Recurrence of major depression within three years
Within the larger structural model, the baseline variables (BDI scores, psychotropic medication use, and SRET performance) were allowed to correlate. Not surprisingly, higher baseline BDI scores were correlated with more negative biases on the SRET, r = .75, p < .001, 95% CI (0.61, 0.84); no other correlations were significant. Neither BDI scores nor psychotropic medication use directly contributed to recurrence, IβsI < 0.48, ps > .10. As hypothesized, however, higher baseline BDI scores predicted higher subsequent negative life event scores, β = 0.37, p = .004, 95% CI (−0.14, 0.88); in turn, higher negative life event scores tended to predict recurrence, β = 0.29, p = .095, 95% CI (−0.22, 0.80); the indirect path between baseline BDI scores and recurrence was not significant, β = 0.11, p = .150, 95% CI (−0.40, 0.62). Importantly, after accounting for the concurrent and predictive relations among all other variables included in the model, the SRET latent variable contributed unique and significant variance to the likelihood of recurrence, β = 0.82, p = .032, 95% CI (0.29, 1.35), which is considered a “large” effect (Kline, 2005). Specifically, more negative self-referential processing at baseline significantly increased the likelihood that formerly depressed individuals would experience a recurrent MDE over the next three years.
Discussion
This study is the first to examine whether performance on an information-processing task predicts the onset of a subsequent depressive episode in adults with a history of MDD. Consistent with previously reported rates of recurrence (Keller et al., 1992), 49% of the women in the current study experienced a recurrent depressive episode within three years of their baseline assessment. Path analyses indicated that higher levels of depressive symptoms at baseline predicted higher subsequent negative life event scores, which, in turn, tended to predict recurrence. Importantly, after accounting for concurrent and prospective associations among other variables included in the model, negatively biased self-referential processing contributed unique variance to the likelihood of experiencing a recurrent depressive episode within the next three years. Specifically, compared to participants who did not subsequently experience a recurrent episode of depression, participants who experienced a recurrent episode endorsed, at baseline, 15% fewer positive words and 7.5% more negative words, and recalled 10% more negative words that they endorsed. Compared to remitted depressed individuals in other investigations (e.g., Fritzsche et al., 2010; Kircanski et al., 2013), participants in the current study who experienced a subsequent depressive episode endorsed and recalled slightly fewer positive and more negative words, whereas participants who did not experience a subsequent depressive episode endorsed and recalled slightly more positive and fewer negative words. Both groups, however, endorsed and recalled fewer positive and more negative self-referential adjectives than did healthy controls in other studies (e.g., Fritzsche et al., 2010; Kircanski et al., 2013).
These data represent the first support using an experimental task for the long-held assertion that negatively biased self-referential processing is a risk factor for recurrent depressive episodes (Beck, 1967). Our findings are consistent with recent studies conducted in community samples of children and adolescents showing that negative biases in self-referential processing predict subsequent increases in depressive symptoms (Black & Possel, 2013; Connolly, Abramson, & Alloy, in press; Goldstein, Hayden, & Klein, in press), and they extend this research to the prediction of a diagnosable recurrent depressive episodes in adult women. Previous research on predictors of depression recurrence has focused on demographic, clinical, or environmental variables (e.g., Mueller et al., 1999; Solomon et al., 2000), which are difficult, if not impossible, to alter. In contrast, cognitive predictors of recurrence can be directly targeted and altered (e.g., Hollon et al., 2006). Our findings support cognitive interventions that modify negative self-schemas and biases in self-referential processing. In particular, there are several cognitive bias modification (CBM) paradigms that could be effective in altering negative biases in self-referential processing. For example, Lang, Blackwell, Harmer, Davison, and Holmes (2011) used a CBM task designed to change negative thinking styles through the use of mental imagery. This approach might be readily adapted to target more specifically negative self-referential thinking. Alternatively, a version of the Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998) could be used in which words that are related to the self (e.g., me, self, I) are disproportionately paired with positive self-referential adjectives. Regardless of the specific intervention, the current findings indicate that such treatment may be effective in reducing rates of recurrence of depression in women with a history of MDD.
It is important to note three limitations of the current study. First, we used a self-report measure of stressful life events, which is subject to subjective-reporting biases and is likely to be less sensitive in capturing the clinical impact of stressful life events than are interview-based assessments. Second, we included only females, which limits the generalizability of our findings. Although this increased the homogeneity of our sample and minimized the influence of confounding variables that disproportionately affect women (e.g., information-processing biases or risk for recurrence; Mueller et al., 1999; Teachman, 2005), it will be important in future research to include males to examine possible gender differences in cognitive risk factors for recurrence. Finally, despite our best effort to retain participants, 19 of the original 100 were lost to attrition and 22 returned to the laboratory but did not complete the SCID-I during their follow-up assessment, typically due to time constraints. Future research should consider alternative methods to increase participant retention. Future research might also examine whether negatively biased self-referential processing increases risk for the first onset of a depressive episode.
Despite these limitations, this study advances our understanding of cognitive risk factors for depression recurrence by using an information-processing task to test, for the first time, the hypothesis that negatively biased self-referential processing predicts a recurrent depressive episode above and beyond depressive symptoms at baseline, psychotropic medication, and negative life events. Identifying negative biases in self-referential processing as a risk factor for recurrence has important implications for intervention efforts. By altering the negative self-schemas that underlie biases in self-referential processing, we may be able to reduce the high rates of episode recurrence in MDD. We are hopeful that the current study will also advance our understanding of cognitive risk factors that predict the recurrence of depression by encouraging a larger methodological shift in research toward using information-processing tasks to assess cognitive predictors of recurrence.
Figure 2.
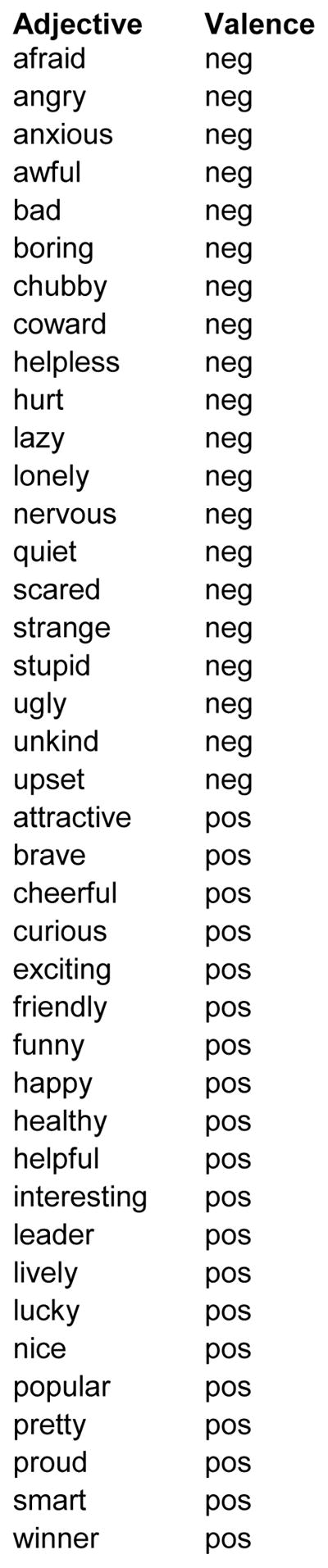
Positive and Negative Adjectives Presented in the Self-Referential Encoding Task (SRET)
Acknowledgments
This research was supported by National Institute of Mental Health (NIMH) Grants F32-MH102013 (JL), F32-MH096385 (KK), and R01-MH59259 (IHG) and the Brain & Behavior Research Foundation (Young Investigator Award 22337 to JL and Distinguished Investigator Award to IHG). KK is now at the Emotion and Development Branch, NIMH.
References
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2006;115(1):145–156. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR) American Psychiatric Association; 2000. [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. Hoeber Medical Division; New York: 1967. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beevers CG. Cognitive vulnerability to depression: A dual process model. Clinical Psychology Review. 2005;25(7):975–1002. doi: 10.1016/j.cpr.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Black SW, Pössel P. The combined effects of self-referent information processing and ruminative responses on adolescent depression. Journal of Youth and Adolescence. 2013;42(8):1145–1154. doi: 10.1007/s10964-012-9827-y. [DOI] [PubMed] [Google Scholar]
- Columbus C., Director . Stepmom [Motion picture] United States: Columbia Pictures; 1998. [Google Scholar]
- Connolly SL, Abramson LY, Alloy LB. Information processing biases concurrently and prospectively predict depressive symptoms in adolescents: Evidence from a self-referent encoding task. Cognition and Emotion. doi: 10.1080/02699931.2015.1010488. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derry PA, Kuiper NA. Schematic processing and self-reference in clinical depression. Journal of abnormal psychology. 1981;90(4):286–297. doi: 10.1037//0021-843x.90.4.286. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. 2002. SCID-I/P. [Google Scholar]
- Fritzsche A, Dahme B, Gotlib IH, Joormann J, Magnussen H, … von Leupoldt A. Specificity of cognitive biases in patients with current depression and remitted depression and in patients with asthma. Psychological Medicine. 2010;40(05):815–826. doi: 10.1017/S0033291709990948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein BL, Hayden EP, Klein DN. Stability of self-referent encoding task performance and associations with change in depressive symptoms from early to middle childhood. Cognition and Emotion. doi: 10.1080/02699931.2014.990358. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annual review of Clinical Psychology. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: the implicit association test. Journal of Personality and Social Psychology. 1998;74(6):1464. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Clinical Psychology. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Joormann J, Arditte KA. Cognitive Aspects of Depression. In: Gotlib IH, Hammen C, editors. Handbook of depression. New York, NY: Guilford Press; 2015. pp. 298–321. [Google Scholar]
- Joormann J, Talbot L, Gotlib IH. Biased processing of emotional information in girls at risk for depression. Journal of abnormal psychology. 2007;116(1):135. doi: 10.1037/0021-843X.116.1.135. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, … Keller MB. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. Journal of Affective Disorders. 1998;50(2):97–108. doi: 10.1016/s0165-0327(98)00138-4. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Mueller TI, Endicott J, Coryell W, Hirschfeld RM, et al. Time to recovery, chronicity, and levels of psychopathology in major depression: A 5-year prospective follow-up of 431 subjects. Archives of General Psychiatry. 1992;49:809–816. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- Kircanski K, Mazur H, Gotlib IH. Behavioral activation system moderates self-referent processing following recovery from depression. Psychological Medicine. 2013;43(09):1909–1919. doi: 10.1017/S0033291712002851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling: Second Edition. New York, NY: Guilford Press; 2005. [Google Scholar]
- Lang TJ, Blackwell SE, Harmer CJ, Davison P, Holmes EA. Cognitive bias modification using mental imagery for depression: developing a novel computerized intervention to change negative thinking styles. European Journal of Personality. 2012;26(2):145–157. doi: 10.1002/per.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau MA, Segal ZV, Williams JMG. Teasdale’s differential activation hypothesis: implications for mechanisms of depressive relapse and suicidal behaviour. Behaviour Research and Therapy. 2004;42(9):1001–1017. doi: 10.1016/j.brat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annu Rev Clin Psychol. 2005;1:167–195. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- Mueller TI, Leon AC, Keller MB, Solomon DA, Endicott J, Coryell W, … Maser JD. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. American Journal of Psychiatry. 1999;156(7):1000–1006. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- Muthén B, Du Toit SH, Spisic D. Robust inference using weighted least squares and quadratic estimating equations in latent variable modeling with categorical and continuous outcomes. Psychometrika. 1997;75:1–45. [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. Journal of consulting and clinical psychology. 1978;46(5):932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry. 2006;63(7):749–755. doi: 10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Shipley WC. A self-administering scale for measuring intellectual impairment and deterioration. The Journal of Psychology. 1940;9(2):371–377. [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea MT, … Endicott J. Multiple recurrences of major depressive disorder. American Journal of Psychiatry. 2000;157(2):229–233. doi: 10.1176/appi.ajp.157.2.229. [DOI] [PubMed] [Google Scholar]
- Taylor L, Ingram RE. Cognitive reactivity and depressotypic information processing in children of depressed mothers. Journal of abnormal psychology. 1999;108(2):202. doi: 10.1037//0021-843x.108.2.202. [DOI] [PubMed] [Google Scholar]
- Teachman BA. Information processing and anxiety sensitivity: Cognitive vulnerability to panic reflected in interpretation and memory biases. Cognitive Therapy and Research. 2005;29(4):479–499. [Google Scholar]
- Teasdale JD. Cognitive vulnerability to persistent depression. Cognition & Emotion. 1988;2(3):247–274. [Google Scholar]
- Wechsler D. WAIS-R. Psychological Corporation; 1981. [Google Scholar]
- Weir P., Director . Dead poets society [Motion picture] United States: Touchstone Pictures; 1998. [Google Scholar]
- Weiss JL, Schell RE. Estimating WAIS-R IQ from the shipley institute of living scale: A replication. Journal of Clinical Psychology. 1991;47(4):558–562. doi: 10.1002/1097-4679(199107)47:4<558::aid-jclp2270470414>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Westermann R, Spies K, Stahl G, Hesse FW. Relative effectiveness and validity of mood induction procedures: A metaanalysis. European Journal of Social Psychology. 1996;26:557–580. [Google Scholar]
- World Health Organization. Depression: Fact sheet N°369. 2012 Oct; Retrieved February 6, 2013, from http://www.who.int/mediacentre/factsheets/fs369/en/index.html.
- Zieff H., Director . My girl [Motion picture] United States: Columbia Pictures; 1991. [Google Scholar]