Abstract
It took years of epidemiological and molecular research to demonstrate that Aristolochia, a widely used herbal remedy, causes cancer and kidney failure. This and similar lessons should inspire more global efforts to properly investigate the safety and efficacy of all herbal treatments.

Subject Categories: Molecular Biology of Disease; S&S: Health & Disease; S&S: Politics, Policy & Law
“The desire to take medicine is perhaps the greatest feature which distinguishes man from animals.”—Sir William Osler
We know from written and archeological records that humans have been using herbs for millennia to both prevent and treat disease. Today, herbal medicines remain widely popular, fueled by cultural factors, centuries‐old tradition, and a burgeoning industry that claims that herbs (i) are gentle, safe, effective, and natural alternatives to pharmaceuticals; (ii) possess unique properties that are not found in drugs; and (iii) are less toxic and more effective when used in combination, a cardinal principle of traditional Chinese medicine (TCM).
Yet, the history of herbal use also shows that not all herbs are benign and sometimes are deadly. Moreover, we cannot know whether all herbal medicines are safe because only a few have been tested systematically for toxicity or carcinogenicity. As an example, the potent toxic effects associated with the use of Aristolochia species—which came to light only after recent epidemiologic studies vividly demonstrated the health risks of this widely used family of medicinal herbs. This previously unknown toxicity provides a strong argument for more effective regulation of herbal medicine use in developed and developing countries to prevent similar dangers to public health. We will discuss the cultural, commercial, and political forces that restrict governments and public health authorities from instituting stronger regulatory measures for herbal use. We also will propose actions, which, if implemented, would help protect users of herbal remedies and promote global public health.
The recognition of Aristolochia's profound toxicity and carcinogenicity in humans began in the early 1990s, when about 100 otherwise healthy Belgian women developed a rapidly progressing chronic kidney disease that ultimately required dialysis or renal transplantation. An investigation of this disease cluster revealed that all of these women had been placed on a weight‐loss regimen that included a mixture of compounds, including Aristolochia fangchi, an herb used in TCM. In total, 1,800 women ingested A. fangchi daily over a period of 20 months. Although most women reported no adverse effects, a significant fraction of the subset with so‐called Chinese herbs nephropathy (CHN) subsequently developed urothelial carcinomas of the upper urothelial tract (UTUC) 1. Earlier, Jean‐Pierre Cosyns, a Belgian pathologist at the Catholic University in Brussels, highlighted the unique renal histopathology associated with CHN and noted the striking clinical similarities between CHN and another chronic kidney disease of unknown etiology known as Balkan endemic nephropathy (BEN), which also is closely associated with UTUC.
BEN occurs in certain farming villages located along tributaries of the Danube River in Bulgaria, Romania, Serbia, Croatia, and Bosnia‐Herzegovina. Its geographic has remained constant since the disease was first recognized in the 1950s. Various hypotheses have been proposed to explain the development of BEN and its association with UTUC, but all failed to account for the unique epidemiologic and pathophysiologic features of this disease; thus, BEN remained a medical mystery disease for more than 50 years.
Important clues to the etiology of BEN include the detection of aristolactam (AL)‐DNA adducts in renal tissues of the Belgian women diagnosed with CHN 1; also, incidental observations by Ivic, a Serbian microbiologist, that traditional methods used in the Balkan region for harvesting and milling of wheat to prepare homemade bread involved the co‐mingling of Aristolochia clematitis seeds with wheat grains. One of us (Arthur Grollman) therefore hypothesized that dietary ingestion of aristolochic acids (AA), in conjunction with individual genetic susceptibility, could account fully for the particular epidemiologic, clinical, and pathophysiologic features of BEN and UTUC. This theory then led to testable predictions, namely that chronic dietary exposure to AA‐contaminated bread would result in the accumulation of AL‐DNA adducts in target tissues and that DNA synthesis past those AL‐DNA adducts would lead to mutations in the TP53 tumor suppressor gene.
Grollman, Bojan Jelakovic, and their colleagues then conducted a molecular epidemiologic study to test these predictions on a cohort of patients with BEN/UTUC, who resided in the endemic regions of Croatia, Serbia, and Bosnia. They detected high levels of AL‐DNA adducts in the renal cortex of most of these patients but not among comparable patients from non‐endemic areas, a result that is consistent with environmental/dietary exposure to AA. Moreover, the mutational spectrum of the TP53 tumor suppressor gene was dominated by A:T to T:A transversions located almost exclusively on the non‐transcribed DNA strand. In conjunction with characteristic mutational “hot spots”, this finding was consistent with the mutational spectrum associated with AL‐DNA adducts in cell culture, while readily distinguishable from among 27,000 tumor mutations listed in a multinational TP53 database. These observations established AA as the mutagen responsible for initiating UTUC 2, and the terms BEN and CHN were replaced in the literature by “aristolochic acid nephropathy” (AAN). UTUC remains an integral part of the disease entity.
These studies in the Balkans paved the way for molecular epidemiologic investigations of UTUC and, subsequently, of other cancers in Asian countries where Aristolochia herbs have been used in the practice of traditional medicine. The biomarkers developed in our studies of BEN/UTUC were used to investigate potential causes of UTUC in Taiwan, where the prevalence of this cancer, and also of end‐stage renal disease, is among the highest in the world. Data from Taiwan's national health insurance database revealed that, between 1997 and 2003, at least one‐third of the population of Taiwan was prescribed herbal medicines containing AA, with the incidence of UTUC increasing proportionally with the amount of AA ingested. The TP53 mutational spectrum observed in Taiwanese patients with UTUC was identical to that reported for BEN/UTUC, with >60% of all mutations involving A:T transversions located on the non‐transcribed strand. AL‐DNA adducts were detected in 84% of patients with A:T to T:A mutations in TP53 3. Remarkably, although Taiwanese patients were exposed only intermittently to relatively high doses of AA, the mutational spectrum was almost identical to patients in the Balkans who were exposed daily to low doses of the toxin 3. We conclude from these studies that AA, an intrinsic component of all Aristolochia herbal remedies, contributes significantly to the overall incidence of UTUC and chronic kidney disease in Taiwan. These findings have major implications for global public health, especially in China, where millions of people are estimated to be at risk of developing AAN/UTUC because of the widespread use of Aristolochia herbs 4.
Mutational patterns of the TP53 gene have been used not only to identify AA‐induced UTUC, but also to identify environmental mutagens associated with other human cancers, such as aflatoxin in hepatocellular carcinoma and ultraviolet light in non‐melanoma cancers of the skin. Next‐generation sequencing technology made it feasible to extend the analysis beyond individual genes to search for genomewide mutation patterns in AA‐induced UTUC 5. Our studies revealed that key elements of the genomewide mutational signature for AA are similar to those observed in TP53, including the predominance of A:T to T:A transversions with a marked bias for the non‐transcribed strand. Additional characteristics include an excess of splice acceptor‐site mutations and a high mutational load. Recently, a similar signature was found in whole‐exome sequence data from patients with hepatocellular carcinoma, renal cell carcinoma, intrahepatic cholangiocarcinoma, and bladder cancer, which suggests that AA‐induced mutations might also contribute to the initiation and/or progression of these cancers.
The Aristolochia family of herbaceous plants occupies a prominent place in the history of medicine. Theophrastus (371–287 BC), a student of Aristotle, first described Aristolochia clematitis, popularly known as birthwort, and its use in treating snakebite, head wounds, insomnia, constipation, uterine problems, and generalized edema (Fig 1). Around 70 AD, Dioscorides compiled De Materia Medica, arguably the most influential medical work of classical antiquity. His detailed description of the pharmaceutical properties of A. clematitis was subsequently translated into Arabic and medieval Latin and later appeared in the first printed books (herbals) of the Renaissance, in the first London Pharmacopoeia (1618), and, eventually, in relevant pharmacopoeias. These materia medica document the continuous use of Aristolochia‐based herbal medicines in Europe, North and South America, and the Middle East during the past 2,500 years 6.
Figure 1. Aristolochia clematitis (birthwort) has been used as an herbal remedy for 2,500 years (Dawson, 1927).
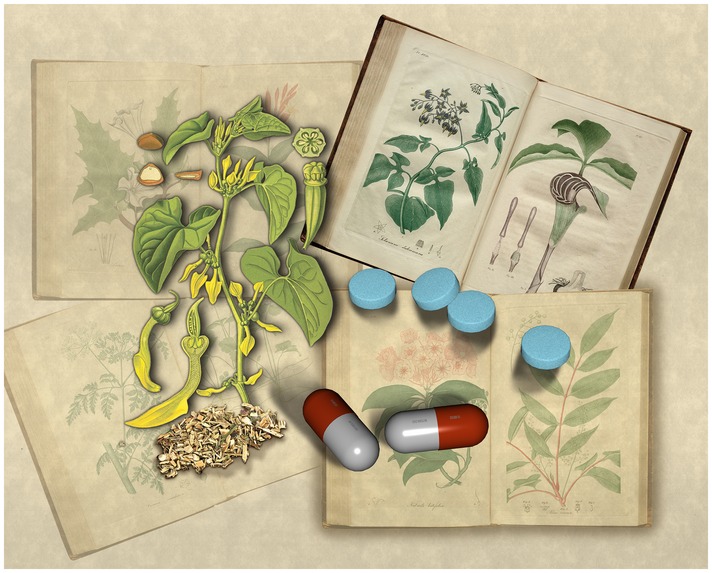
The Bencao Gangmu, compiled by Li Shizhen in the late 16th century and the principal source of information for TCM until today, includes several species of Aristolochia. The Carakasamhita, dating from ca 400 AD, constitutes one of the earliest Ayurvedic medical treatises. In this classic text, scholars identified several species of Aristolochia that are still being used in Ayurveda. Both as a single herb and as a component of multi‐herb mixtures, the Aristolochia family of medicinal plants has been a fixture in traditional medicine throughout Asia, the South‐East Asian subcontinent, and Western Europe.
Despite their long and widespread usage, the intrinsic toxicities of Aristolochia herbs were not recognized, owing, in large part, to the latency period between exposure and the onset of symptomatic disease, and in part, to genetic determinants that confer susceptibility to only ~5% of those exposed to these herbs. Thus, the use of Aristolochia in both Western medicine and TCM for more than two millennia raises the question about whether its potential toxicity in humans should have been recognized before the late 20th century, based on published observations. It is important to remember that almost all carcinogens (and many toxins) require a long latency period before symptoms become apparent, making it very difficult for lay persons and medical professionals to identify the causative actions of a drug taken months or years earlier.
Indeed, the literature on Aristolochia contains a number of relevant reports 6. In 1851, the French chemist Mathieu Orfila, the founder of modern quantitative toxicology, described lethal effects of A. clematitis in short‐term experiments performed on dogs. More than a century ago, the nephrotoxic effects of partially purified Aristolochia extracts were clearly shown in rodents. In the Balkans, horses ingesting hay contaminated with A. clematitis were observed to develop renal failure. Moreover, Aristolochia was found to be effective in the treatment of gout, reported first in ancient times and again in the 18th century, when birthwort (A. clematitis) was introduced as a component of Portland's powders. In both cases, the herb was administered daily for 2 years at an estimated dose now known to produce irreversible renal toxicity and/or urothelial cancer. For more than 80 years, “The Powders” enjoyed great popularity, despite the pronouncement by William Cullen, a leading physician of the time, in The Practice of Physic: Materia Medica (1789) that, “In every instance I have known, the persons who had taken (Portland Powders) for the time prescribed for gout afterwards were free from any inflammation of the joints; and, after finishing this course of the medicine, have been attacked with apoplexy, asthma or dropsy, which proved fatal”. Despite this evidence, the potent toxicities associated with the medicinal use of Aristolochia herbs in humans were not fully appreciated until the first cases of CHN/AAN were reported in Belgium in 1993. Moreover, Aristolochia is just one of several widely used herbs that later proved to have serious, chronic toxicities—other examples include comfrey tea that is highly toxic to the liver and sassafras and other herbs that contain chemical carcinogens.
Aristolochic acid‐I, a nitrophenanthrene compound found in all Aristolochia species, is responsible for both the nephrotoxic and carcinogenic properties associated with this family of herbs. It is actively reabsorbed in the proximal tubule and results in acute cytotoxicity. AA‐I also is associated with tubulointerstitial fibrosis, leading to chronic kidney disease, progressing over time to renal insufficiency, and end‐stage kidney failure. Some isomers of AA are both nephrotoxic and genotoxic, while others, such as AA‐II, lack nephrotoxic potential. Our current model for the mechanism of nephrotoxicity of AA‐I postulates cytotoxic effects on the renal proximal tubule mediated by interactions with a protein target rather than DNA.
In AAN, renal cortical fibrosis develops slowly over a long period before symptoms of renal dysfunction appear. An even longer delay, sometimes as long as 20–30 years, occurs between exposure to AA and the appearance of symptoms of UTUC. In Western medicine, physicians routinely analyze renal function by determining the level of creatinine in the blood, which helps to diagnose kidney malfunction at an early stage. This analysis is rarely done in the practice of traditional medicine where diagnosis and treatment are guided by principles of a complex, ancient healing system based on the principles of yin and yang, elements linked to organ systems of the body, the emotions, the climates, the seasons, and tastes. Latency in the appearance of symptoms is likely to temporarily obscure chronic kidney disease and/or carcinogenicity associated with other TCM herbs. Thus, we conclude that a long history of usage is insufficient to assure the safety of herbal remedies.
This raises another important question: How widespread are the adverse effects of medicinal herbs in general? Plants are not just benign sources of food or medicines; digoxin, atropine, morphine, nicotine, and ricin are just a few of the many, highly toxic compounds that plants produce, presumably to kill pathogens, parasites, and herbivores. It is therefore prudent to assume that many herbs may contain toxic or carcinogenic substances that can cause subsequent health problems for humans.
…a long history of usage is insufficient to assure the safety of herbal remedies
For example, ephedra, long used in TCM, was approved in the United States to treat symptoms of mild bronchoconstriction. Later, when this herb was marketed as a dietary supplement to promote weight loss, it was shown to cause elevated blood pressure, myocardial damage and strokes. One such product, Metabolife 356, generated 19,000 reports of adverse effects. Ephedra was frequently blended with herbs containing caffeine and used to enhance athletic performance in young, otherwise healthy people, and caused numerous adverse cardiovascular effects. Nine years of persistent efforts by physicians, consumer activists and several US senators were required before the FDA belatedly banned this herb from the marketplace. Even then, ephedra was replaced by extracts of Citrus aurantium, which contains synephrine, a structural analog of ephedrine, the active principal of ephedra. And so, a multi‐billion dollar market was quickly and inexpensively restored. Predictably, adverse cardiovascular effects caused by synephrine, similar to those reported for ephedra, soon followed.
…the history of medical treatment prior to the era of scientific medicine is largely the history of the placebo effect
Many herbs commonly injure the liver, accounting for 20% of reported hospitalization for drug‐related hepatotoxicity 7. Liver injury from chemicals develops slowly, manifesting signs between 1 week and 1 month after exposure. Symptoms are generally non‐specific and often are difficult to attribute to a specific herb. Hepatotoxicity may be idiosyncratic, as in the case of kava, or intrinsic and dose dependent, as with the pyrrolizidine alkaloids (PA), components of herbs that affect not only humans but also livestock and wildlife. PAs are found in 3% of the world's flowering plants, many of which have been incorporated into TCM. PAs can be detected in blood and are associated with an unusual hepatic sinusoidal obstruction. The foregoing are just a few examples taken from the growing body of literature describing toxic effects of herbal remedies on the kidney, heart, and liver.
Of course, the perception of therapeutic effectiveness is responsible for the popularity of herbal remedies. However, this perception is created, in large part, by the self‐limited nature of most symptomatic illness and by the remarkable power of the placebo effect, which has been shown to account for 30–50% of the perceived efficacy of many therapeutic agents. Indeed, the history of medical treatment prior to the era of scientific medicine is largely the history of the placebo effect 8. The importance of placebo controls, first recognized in the 1950s by Beecher and others, led to the current FDA requirement to use randomized double‐blind, placebo‐controlled trials for evaluating the efficacy of drugs. Such recent applications of statistics stand, alongside the discovery of antibiotics and anesthetics, as one of the most important developments in medicine in the past 1,000 years.
Recently, several of the most popular herbal remedies in the USA were subjected to standard randomized, placebo‐controlled, clinical trials: gingko biloba, used to prevent decline in memory and onset of dementia, St John's wort for treating minor or moderate depression, garlic to reduce hypercholesterolemia, saw palmetto for symptoms of prostatic enlargement, and Echinacea to prevent or treat the common cold. Improvements observed in these studies were attributed entirely to the placebo effect, as opposed to the intrinsic properties of the herb under study 9. It would be highly informative, therefore, to subject other popular herbal mixtures used in TCM and Ayurveda to blinded, placebo‐controlled trials.
… recent applications of statistics stand alongside the discovery of antibiotics and anesthetics as one of the most important developments in medicine in the past 1,000 years
This does not mean that herbs or their active components are not biologically active. By the end of the 19th century, the therapeutic benefits of a number of herbs were recognized, and, in some cases, their active principles were extracted and purified and marketed. However, considering the large number of herbs in use at that time, the list of demonstrable active and effective herbs is remarkably short: ma huang (ephedrine), Digitalis purpura (digoxin), Cinchona bark (quinine), Ipecacuanha (emetine), Opium poppy (morphine), Colchicum (colchicine), and Belladonna (atropine). Using large collections and sophisticated screening techniques, pharmaceutical companies have long sought to isolate active principles from herbs used in traditional medicine but, to date, few novel compounds have been found. Pharmaceutical companies also have screened extracts of thousands of plants explicitly for their cytotoxic effects to identify novel compounds for cancer chemotherapy. Although costly and inefficient, this approach resulted in the discovery of a number of anti‐tumor agents, including Taxol, camptothecin and vincristine. In 1965, aristolochic acid emerged from such a random screen as the most potent anti‐tumor compound identified at that time. Not surprisingly, severe renal toxicity was observed in the Phase I study that followed and further development of AA as an anti‐tumor agent was abandoned.
Related to this subject is the isolation of the anti‐malaria drug artemisinin from the Chinese herb, Quinghau (Artemisia annua), a component of herbal mixtures used to reduce fever in TCM. This significant achievement, recognized by the award of the Nobel Prize in Medicine in 2015, was the result of Project 523, conducted secretly by Chinese scientists at the height of the Cultural Revolution with approval and support from Mao Zedong. It involved screening 808 herbal mixtures, some of which contained Quinghau or other species of Artemisia herbs for anti‐parasitic activity in mouse models. Standard phytochemical procedures showed that artemisinin could be extracted efficiently from Artemisia with ethyl ether, but not by the methods used in TCM, which partially inactivate this compound. Subsequent structural studies by a large team of organic chemists led to the development of synthetic methods for artemisinin. Thus, the discovery and development of artemisinin owes its success less to TCM than to the application of strategies used by Western pharmaceutical companies to facilitate the discovery of anti‐tumor drugs.
… an editorial in the New York Times presciently referred to DSHEA as “The Snake Oil Protection Act”
From a pharmacological standpoint, detailed knowledge of the composition, biological activity, and bioavailability of a medication is essential to ensure its safe and effective use. Plant extracts contain hundreds of chemical compounds, their active principles are mostly unknown, and extracts rarely can be standardized for pharmacologic activity. In addition to their intrinsic toxicities, certain herbs modify the pharmacokinetics of life‐saving drugs. We need structures, rules, and regulations to ensure the quality, safety, and efficacy of botanical products. We and others already have expressed serious concerns about the lack of quality control in the processing of medicinal herbs, the accidental, or deliberate inclusion of toxic chemicals, including heavy metals, and the rampant adulteration of commercial herbal products with pharmacologically active compounds and prescription drugs, all problems that urgently need to be addressed.
The USA, the UK, and other Western countries have been in the grips of an herbal medicine renaissance, sparked initially by individuals and groups who promote “natural” healing, commercial interests in advertising and sales of herbal products, and then further influenced by the counterculture of the 1960s and broad dissatisfaction with contemporary healthcare systems. Germany, France, and other Western European countries were less affected by this trend. In the UK, an important legal change took place when the Ministry of Health chose to accept documented statements that a particular herb had been used for an extended period of time without adverse effects as proof of safety and efficacy. Aristolochia, of course, would easily pass such a test. In the United States, Congress passed the Dietary Supplement and Health Education Act (DSHEA) in 1994, which, by classifying botanicals as dietary supplements, relieved manufacturers from providing evidence, prior to marketing that their product was of high quality and safe. At the time, an editorial in the New York Times presciently referred to DSHEA as “The Snake Oil Protection Act”.
… scientists and health organizations should hold the WHO accountable for its failure to recognize the silent epidemic of AAN and the growing evidence of botanical hazards worldwide
Twenty years later, more than 75,000 non‐vitamin, non‐mineral supplements (including herbals) are marketed in the United States and abroad, generating annual revenues of more than U$30 billion. Major deficiencies in the regulation of herbal supplements under DSHEA include the lack of standardization to insure a consistent level of the (presumed) active ingredients; absence of pre‐market testing for safety, as required for all prescription and OTC drugs; lack of adequate labeling to inform consumers about all ingredients in these products; and failure to require prompt reporting of all adverse effects to the FDA.
… empirical knowledge based on tradition should not be permitted to “trump” the scientific method in matters of public health
In the EU, more than 1,300 traditional herbal medical products have been registered by the health regulatory authorities of the 28 EU member states. The EU is now debating regulatory guidelines for herbal remedies, which would consider efficacy as well as quality and safety. This legislative approach combines scientific evaluation with data collected from many years of herbal medicine use. Harmonizing the process for evaluating and authorizing traditional herbal medicines among EU countries will be difficult and fraught with compromises, such as the “herbalist exception” in the UK, which pleased herbalists and the public, but diminished regulatory effectiveness. It will be even more difficult to extend this approach to parts of the world where the philosophies of TCM and Ayurveda prevail.
Indeed, botanicals and their extracts are often used as first‐line treatments in countries where access to conventional medical care is limited and a strong culture of traditional healing exists. The true frequency of acute and chronic illness caused by botanical remedies is unknown, especially in developing countries, owing to limited awareness of the problem and the lack of organized surveillance. Our concern is heightened by recent announcements from the governments of several African and Asian countries to invest in expanding the production, sales, and exports of traditional remedies. Discussions of the hazards of herbal remedies touch on sensitive economic and cultural issues, including the pride taken by many nations in their heritage of traditional healing and issues of sovereignty. There also is strong resistance from practitioners of traditional medicine and manufacturers of botanicals. We emphasize that our primary issue is the prevention of toxicities associated with herbal medicine and not a categorical rejection of traditional healing practices.
The World Health Organization (WHO) would be the logical organization to address these problems on a global level. Unfortunately, its recent monograph, WHO Traditional Medicine Strategy, 2014–2023, follows the premise that traditional medicine is of proven quality 10. The publication offers “to promote the safe and effective use of traditional and complementary medicine through the regulation of products, practices and practitioners”, but it is highly unlikely that the randomized controlled trials required for these purposes will be undertaken. Indeed, there is very little discussion regarding the almost complete lack of scientific evidence supporting the efficacy of herbal remedies or their demonstrated hazards, notwithstanding the more than 300 publications related to the toxic effects of Aristolochia alone. The WHO monograph, financed in part by traditional/herbal medicine groups of several nations, appears to have been created by advocates for traditional medicine with little input from the biomedical community.
Several factors contribute to the current problem: a virtually complete lack of communication between the biomedical community and organizations representing traditional healers in countries that have a strong culture of traditional medicine; a lack of epidemiologic data concerning herbal toxicity in areas where a preponderance of healthcare is provided by traditional healers; and, alarmingly, the failure of the WHO to recognize and deal with this aspect of herbal medicine use. Prevention of disease is a moral and ethical obligation, and, in the absence of leadership from established organizations, the global health community must take steps to prevent further suffering and loss of life. Scientists should help to develop educational programs concerning the clinical pharmacology of botanicals and could provide technical assistance in creating regional laboratories and epidemiologic units. Importantly, interested scientists and health organizations should hold the WHO accountable for its failure to recognize the silent epidemic of AAN and the growing evidence of botanical hazards worldwide.
Basic and clinical studies designed to test safety of botanicals should begin at once, especially in China, where problems in the processing of herbs have been documented, and where significant governmental resources have recently been allocated to research Chinese herbal medicine. The usefulness of applying molecular epidemiologic approaches and using interdisciplinary research to explore mechanisms of herbal toxicity are illustrated by what was learned from our research on Aristolochia. Asian scientists are well positioned to explore the intrinsic toxicities of herbs currently used in TCM, including their potential for carcinogenicity, and to conduct the randomized, double‐blind, placebo‐controlled clinical studies required for establishing efficacy and safety. In the United States, where a branch of the National Institutes of Health has been established to support research on alternative and complementary medicine, more resources should be devoted to basic and clinical studies of the toxicities of herbs, as their usage in Western countries differs significantly from those in TCM.
In conclusion, empirical knowledge based on tradition should not be permitted to “trump” the scientific method in matters of public health. Basic and clinical scientists, as well as public health officials, have a moral and legislated responsibility to take actions that will evaluate both long‐ and short‐term safety, as well as the efficacy of botanical products in widespread use. The carcinogenic and nephrotoxic effects of Aristolochia would have gone unnoticed without the application of scientific methods and the mortality and morbidity associated with AAN and UTUC would have been considerably greater.
Conflict of interest
The authors declare that they have no conflict of interest.
Sidebar A:Further reading.
Aristolochia
Dawson WR (1927) A study of the progress of medical botany through twenty‐two centuries. Pharm J Pharmacist 396–397: 427–430
Ivic M (1969) The problem of etiology of endemic nephropathy. Lijec Vjesn 91: 1273–1281
Vanherweghem JL et al (1993) Rapidly progressive interstitial renal fibrosis in young women, association with slimming regimen, including Chinese herbs. Lancet 341: 387–391
Kabat GC (2016) Deadly remedy; how a mysterious disease led to the recognition of a worldwide public health threat. In Getting Risk Right: Understanding the Science of elusive Health Risks. New York: Columbia University Press
Artemisinin
Jianfang Z (Ed.) (2013) A Detailed Chronological Record of Project 523 and the Discovery and Development of Qinghaosu (Artemisinin). Houston, TX: Strategic Book Publishing and Rights Co.
Regulation of herbal supplements
Dietary Supplement Health and Education Act (DSHEA) (1994) Public Law 103–417, 25 October 1994; Codified at 42 USC 287C–11.
Marcus DM, Grollman AP (2012) The consequences of ineffective regulation of dietary supplements. Arch Int Med 172: 1035–1036
Cohen PA (2011) Hazards of hindsight – monitoring the safety of nutritional supplements. N Engl J Med 370: 1277–1280
Bloom BR (2011) WHO needs change. Nature 473: 143–45
Acknowledgements
We acknowledge the contributions of our many colleagues and collaborating medical scientists in Croatia and Taiwan whose research established the causal role of aristolochic acid in Balkan endemic nephropathy and upper urothelial cancer. We thank Annette Oestreicher Grollman for knowledgable commentary and expert editing. Research on aristolochic acid was generously supported by a grant from Henry and Marsha Laufer.
References
- 1. Nortier JL, Martinez MC, Schmeiser HH, Arlt VM, Bieler CA, Petein M, Depierreux MF, De Pauw L, Abramowicz D, Vereerstraeten P et al (2000) Urothelial carcinoma associated with the use of a Chinese herb (Aristolochia fangchi). N Engl J Med 342: 1686–1692 [DOI] [PubMed] [Google Scholar]
- 2. Grollman AP, Shibutani S, Moriya M, Miller F, Wu L, Moll U, Suzuki N, Fernandes A, Rosenquist T, Medverec Z et al (2007) Aristolochic acid and the etiology of endemic (Balkan) nephropathy. Proc Natl Acad Sci USA 104: 12129–12134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen CH, Dickman KG, Moriya M, Zavadil J, Sidorenko VS, Edwards KL, Gnatenko DV, Wu L, Turesky RJ, Wu XR et al (2012) Aristolochic acid‐associated urothelial cancer in Taiwan. Proc Natl Acad Sci USA 109: 8241–8246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grollman AP (2013) Aristolochic acid nephropathy: Harbinger of a global iatrogenic disease. Environ Mol Mutagen 54: 1–7 [DOI] [PubMed] [Google Scholar]
- 5. Hoang ML, Chen CH, Sidorenko VS, He J, Dickman KG, Yun BH, Moriya M, Niknafs N, Douville C, Karchin R et al (2013) Mutational signature of aristolochic acid exposure as revealed by whole‐exome sequencing. Sci Transl Med 5: 197ra102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grollman AP, Scarborough J, Jelaković B (2009) Aristolochic acid nephropathy: an environmental and iatrogenic disease In Advances in Molecular Toxicology, Fishbein JC. (ed.), Vol. 3, pp 211–222. Amsterdam, the Netherlands: Elsevier; [Google Scholar]
- 7. Teschke R, Eickhoff A (2015) Herbal hepatotoxicity in traditional and modern medicine: actual key issues and new encouraging steps. Front Pharmacol 6: 1–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shapiro AK, Shapiro E (1997) The Powerful Placebo: From Ancient Priest to Modern Physician. Baltimore, MD: The Johns Hopkins Press; [Google Scholar]
- 9. Offit PA (2012) Studying complementary and alternative therapies. JAMA 307: 1803–1804 [DOI] [PubMed] [Google Scholar]
- 10. WHO (2013) Traditional Medicine Strategy 2014–2023. Geneva, Switzerland: World Health Organization; [Google Scholar]


