Abstract
This brief history of topographical anatomy begins with Egyptian medical papyri and the works known collectively as the Greco‐Arabian canon, the time line then moves on to the excitement of discovery that characterised the Renaissance, the increasing regulatory and legislative frameworks introduced in the 18th and 19th centuries, and ends with a consideration of the impact of technology that epitomises the period from the late 19th century to the present day. This paper is based on a lecture I gave at the Winter Meeting of the Anatomical Society in Cambridge in December 2015, when I was awarded the Anatomical Society Medal.
Keywords: Galen, Vesalius, dissection, Renaissance, Harvey, legislation, technology
It would be a conceit to attempt to cover such a vast topic in a brief paper. Mindful of John of Salisbury's comments in the Metalogicon (1159), I therefore intend to stand on the shoulders of some of the giants of our discipline and apologise for omitting many others who also have a legitimate claim to the status of ‘giant’. This paper is based on a lecture I gave at the Winter Meeting of the Anatomical Society in Cambridge in December 2015, when I was awarded the Anatomical Society Medal: I hope that it will be of particular interest and use to young anatomists just starting in the field.
This brief history of topographical anatomy begins with Egyptian medical papyri and the works known collectively as the Greco‐Arabian canon, the time line then moves on to the excitement of discovery that characterised the Renaissance, the increasing regulatory and legislative frameworks introduced in the 18th and 19th centuries, and ends with a consideration of the impact of technology that epitomizes the period from the late 19th century to the present day.
Medical papyri
Some of the first written evidence of the use of anatomical terms and anatomico‐physiological concepts that survives in the West is contained in rolls of Egyptian medical papyri, notably the (Edwin) Smith papyrus, the (Georg) Ebers Papyrus, and the (Heinrich) Brugsch Papyrus, also known as the Greater Berlin Papyrus (Acierno, 1994; Willerson & Teaff, 1996). The Smith Papyrus dates from around 1600 BCE and is believed to be an incomplete copy of a much older document, written around 3000–2500 BCE. It is regarded as the earliest known recorded group of rational observations in natural science (Stiefel et al. 2006), offering insights into the state of clinical knowledge in ancient Egypt. It consists of 48 cases, of which 27 deal with head trauma, and contains the first descriptions of the cranial sutures, meninges, external surface of the brain (like ripples that happen in copper through smelting) and the cerebrospinal fluid; together with clinical observations concerning the neurological sequelae of injuries to the brain and the cervical spine; what may be the first description linking the heartbeat and pulse; and the concept of clinical ‘triage’, often considered to have arisen at the time of the Napoleonic Wars. The hieroglyph for the brain appears for the first time in this papyrus and is translatable as ‘skull offal’ (Wickens, 2015), a derogatory term that may explain why the brain was not considered worth preserving during mummification. The Ebers papyrus contains a treatise on the heart and great vessels and the Brugsch papyrus contains a description of the heart similar to that found in the Ebers papyrus (Willerson & Teaff, 1996).
This was a time when internal anatomy could only be viewed vicariously. Skeletal remains might be uncovered when burial sites were disturbed. Thoraco‐abdominal viscera would be exposed during the preparation of bodies for mummification or when entrails were scrutinised by those practising anthropomancy (rare), and might be glimpsed serendipitously in the living, through gaping wounds. However, the deliberate opening of a human body in order to examine its contents violated all culturally acceptable and legal boundaries and was strictly forbidden. There is no evidence that the type of ‘dissection’ performed during the rituals associated with mummification or anthropomancy led to any appreciation of systematised, topographical anatomy: …only in the context of a culture pattern oriented towards a kind of ‘science’ do dissections furnish anatomical knowledge… (Benedict, 1934).
The Greco‐Arabic canon
Some thousand years after the Egyptian medical papyri were written, medical schools had been established in Croton, Kos, Cnidus and Alexandria. At various times, Alcmaeon, Hippocrates, Herophilus, Erasistratus, Galen and Aretaeus studied and may also have taught at these schools.
Alcmaeon of Croton
Alcmaeon of Croton was a pre‐Socratic physician and philosopher living in the latter half of the 6th century BCE. He has been described as the first truly experimental biologist and even as the ‘father of anatomy’ (Chalcidius, 1876). Although his books about medicine and natural sciences, including De Natura, are now lost, we know of his work through secondary and tertiary sources, principally Theophrastus (ca. 370–286 BCE, a pupil of Aristotle). De Natura is said to have influenced others, including Hippocrates, Herophilus, Plato and Galen. Alcmaeon …seems to have been the first practitioner of [nonhuman] anatomic dissection as a tool of intellectual inquiry… (Gross, 1995), although this is disputed (Mavrodi & Paraskevas, 2014). His most detailed dissections concerned the special senses; he described what we now recognise as the optic nerves as two channels leading from the back of the eye to the brain … The eyes see by means of the wateriness about them, but it is evident that the eye contains fire, for a blow on the eye produces flashes… We hear with the ears because there is an empty space in them; this space resounds. Sound is produced by the cavity… We distinguish tastes with the tongue… We smell through the nostrils by drawing up the air to the brain during inspiration… (Debernardi et al. 2010). Alcmaeon advocated an empirical approach to observations of natural phenomena (Celesia, 2012). He sought to improve his clinical practice by deepening his understanding of anatomy, a concept familiar to modern medical educators. His clinical observations of the altered cognitive states that frequently followed brain injury or head trauma were distilled into his proposal that the brain housed the mind and the soul, thought, memory and intelligence, prefiguring by well over a thousand years Thomas Willis's proposal that the higher cognitive function of the human brain was a product of the convolutions of the cerebral cortex (Molnár, 2004).
Hippocrates
Hippocrates (ca. 460–370 BCE) is commonly regarded as the ‘father of (rational) medicine’ and the forefather of neurology. His principal methods of patient examination, inspection, palpation and auscultation, remain part of a modern clinical examination and he too recognised that a knowledge of anatomy was a fundamental part of clinical practice, since it was …the basis of medical discourse. He described the brain as being in two halves divided by a thin vertical membrane (as it was in other animals), supplied by two stout channels coming from the liver and spleen. He developed Alcmaeon's ideas about the brain as the analyst or interpreter of the external world … It ought to be generally known that since the source of our pleasure, merriment and amusement, as of our grief, pain, anxiety and tears, is none other than the brain. It is especially the organ which enables us to think, see and hear… (Wickens, 2015). Hippocrates was aware that blood vessels started from the heart, but did not distinguish between arteries and veins. From his wide clinical experience, he recognised that compression caused tingling and pallor or lividity of the extremities and that a lesion of the carotid artery would evoke contralateral hemiplegia (for further reading, see Breitenfeld et al. 2014). In the Hippocratic corpus (only some of which was written by Hippocrates), the body is considered in terms of viscera and orifices (including eyes, ears and genitals), linked by hollow tubes and channels that included phlebes (generic term for any type of blood vessel), solid threads or neura (a polysemic term used indiscriminately to describe sinews, ligaments, tendons, arteries and veins, see Swanson, 2014) and hollow neura such as poroi that might open up to convey an excess of fluid. In The Nature of Bones, Hippocrates is perhaps describing the vagus nerves when he writes of two ‘stout cords’ (tonoi) that run from the brain and pass down on either side of the windpipe. (Although outwith the remit of this paper, the interested reader should consult Craik, 2009 for a discussion of the parallels between Hippocratic channels and similar concepts in Chinese traditional medicine.) The extent to which the anatomy that is described in the Hippocratic corpus is based on dissection/autopsy is unclear in the literature, but it is assumed that some of it is so based.
The Alexandrian physicians
Herophilius of Chalcedon (325–255 BCE) and Erasistratus of Chios (310–250 BCE) both worked in the great medical school in Alexandria during the period when human cadaveric dissection was briefly permitted, possibly as a consequence of the patronage of the Ptolomeic pharaohs, Ptolemy Soter and Ptolemy Philadelphius (von Staden, 1992). Pliny records that the pharaohs visited Herophilus and might have participated in anatomical dissection (Durant, 1939). Human dissection may have taken place earlier in Babylon and in the Achaemenian dynasty (558 or 559–330 BCE) (Shoja & Tubbs, 2007), but the weight of evidence suggests that it was usually forbidden in the ancient world. Almost all that was then ‘known’ about human anatomy was therefore extrapolated from animal dissection and vivisection: the distinction between human and non‐human animal anatomy was probably not regarded as significant.
Herophilius, also hailed as a ‘father of anatomy’ or the ‘Vesalius of antiquity’ (Wiltse & Pait, 1998; Bay & Bay, 2010), is noted especially for his writings about the nervous system, prompting the bold claim that he provided …possibly the single most profound insight into the workings of the body ever made by an individual… (Wickens, 2015). A physician as well as an anatomist, he recognized that thread‐like structures, neura, originated in the brain and spinal cord and not in the heart, contrary to Aristotelean cardiocentric views: …the neura that make voluntary motion possible have their origin in the cerebrum (enkephalos) and spinal marrow (Pearce, 2008). His dissections allowed him to distinguish between vessels and nerves and to confirm Alcmaeon's earlier finding that the walls of arteries were thicker than the walls of veins. As with so many of the very early anatomists, his writings have not survived; what is attributed to him comes to us filtered through secondary sources, with the potential for post hoc embellishment and alteration. According to Rufus of Ephesus (a Greek physician who lived in the second half of the 1st century BCE), Herophilus distinguished between soft or porous sensory fibres and hard or solid motor fibres that made muscles move. According to Galen, Herophilus described seven pairs of nerves arising from the brain. He also described the eponymous torcular; the eye (identifying the iris, choroid, cornea, retina, ciliary body and vitreous humour); the alimentary canal, including the pancreas, liver and duodenum (dodekadaktylon, literally 12 fingers long); the male and female reproductive organs (including the prostate); and the arteries and veins (for more comprehensive descriptions of the many anatomical ‘discoveries’ attributed to Herophilus, see Wiltse & Pait, 1998).
Erasistratus was also a practising physician, but his writings and biological views have a physiological rather than an anatomical bias (Dobson, 1927). His efforts to explain physiological principles mechanistically rather than by hidden forces were not popular and attracted ridicule from later authorities including Galen. Like Herophilus, he distinguished between (hard) motor and (soft) sensory nerves, indeed some have credited the younger man with being the first to make this distinction. Erasistratus described four ventricles in the brain, noting that the fourth ventricle under the cerebellum communicated with the third, whereas Herophilus seems not to have noticed the third ventricle: this may have been the first description of the cerebral aqueduct (Tsuchiya et al. 2015). He likened the cerebral gyri to the coils of the small intestine and, long before Thomas Willis (1664), he suggested that the extensive cortical surface of the human brain was in some way related to intelligence, …since man greatly surpasses other beings in intelligence, his brain is greatly convoluted. He considered that each organ was supplied by a network of fine tubes (woven triplets), wherein veins carried blood, arteries carried vital pneuma and hollow nerves carried psychic pneuma from the ventricles in the brain (for further reading on the doctrine of pneuma in Western scientific tradition, see Frixione, 2013). Frederick Ruysch popularised a very similar view in 1696, proposing that tissues were composed of vascular networks (he had perfected a method of injecting vessels with wax, a technique that became known as the ‘Ruyschian Art’) (Haviland & Parish, 1970).
Erasistratus described the heart valves and recognised that the heart functioned as a pump, likening it to a blacksmith's bellows. He considered the heart to be the source of the arteries and veins, recalling a similar description in the treatise on the heart in the Ebers papyrus. He knew that the anatomical ends of the arteries were the beginnings of the veins, but was convinced that the blood remained within the veins and at no point normally encroached on the breath‐vessels (arteries), calling the potential connections between them synanastomoses: Galen later demonstrated that arteries also contain blood (Sternbach et al. 2011). Some writers have suggested that Erasistratus came close to discovering the circulation of the blood because he believed that pneuma, like blood, could only flow one way, directed by valves within the heart (Dobson, 1927; Pasipoularides, 2013); others regard this as an unfounded and extravagant claim.
Both Herophilus and Eristratus were accused of vivisecting human criminals as well as dissecting human cadavers, but this has proved a contentious point: …there appears to be no mention of vivisection having been performed by these two men in any of the fragments of writing that are available from the time of their deaths until Celsus [working in 20 CE]… (Wiltse & Pait, 1998). Galen makes no reference to such distasteful activity despite being familiar with (and sometimes criticising) the work of Herophilus and Eristratus: modern writers have suggested that defamatory rumours about human vivisection were spread by opponents of cadaveric dissection, including Christian polemicists, to discredit the ancient Greeks. The charge of ‘anatomist as (human) vivisector’, effectively that of ‘anatomist as executioner’, continued into the early modern period, but has always been denied (Sawday, 1995).
Galen
Claudius Galen was born in Pergamum (now Bergama, Turkey), probably in 129 CE. He became one of the most celebrated anatomists and physicians of all time, hailed as the founder of experimental physiology and embryology. He studied anatomy in Smyrna, Corinth and Alexandria, where he examined a human skeleton, and was well versed in the work of many of his predecessors (the ‘ancients’) at an early age. Galen practised as a physician in the Roman Empire for 50 years, during which time he was appointed as a surgeon to the gladiators (probably for his renowned skill in treating wounds) and he served as physician to Marcus Aurelius (161–180 CE). He recognised that a physician was more likely to maim or kill his patients if he was unaware of the relevant anatomy and exhorted his students to remember this important maxim. In his quest for anatomical and physiological knowledge, he dissected or vivisected large numbers of animals, including monkeys, fish, cats, dogs, snakes, pigs, ostriches, cranes, cattle, goat fetuses in utero and at least one war elephant, purchased from the Circus Maximus: he considered Barbary macaques to be most similar to humans (Mattern, 2013). In bloody vivisections that were often undertaken in public, he demonstrated the muscles and nerves that mediate phonation and the movements of respiration; that lesions of the spinal cord produced loss of movement and sensation below the level of the cut; that urine was formed in the kidney (and not, as was then thought, in the bladder); and that arteries contained blood not pneuma (here he contradicted Erasistratus). He challenged his onlookers to match his surgical dexterity, as when he transiently ligated the recursive (recurrent laryngeal) nerves of a pig to demonstrate their role in generating the pig's squeal. HIs work on the recurrent laryngeal nerve is remembered in the eponymous ansa Galeni, the nervous loop between the posterior branch of the recurrent laryngeal nerve and the internal branch of the superior laryngeal nerve (Kruse et al. 2006). (For further reading on Galen's experiments on the nervous system, see Wickens, 2015.) Galen's deductions were not always correct: his experiments with arterial cannulation led him to believe erroneously that the pulse was carried in the walls of the arteries (again contradicting Eristratus, who had considered the heart to be a pump), while his extrapolations from animal dissections convinced him that the human heart consisted of two chambers and that blood passed from the right to the left side of the heart via tiny pores in the intervening septum; that blood was formed in the liver; and that the uterus was bicornuate. Galenic physiology recognised natural, vital and animal spirits, which were contained respectively in veins (associated with the liver), arteries (associated with the heart) and nerves (associated with the brain). His explanations were sometimes confusing and he often referred to other works that he expected his reader to consult for clarification.
Galen was a prolific author, producing …over 500 papers, books, and treatises, totalling more than four million words, only a fraction (˜120) of his works could be saved from a fire in the Temple of Peace in 191CE… (Shoja et al. 2015): what remained represents some 10% of extant ancient Greek writing. It seems likely that his words were often transcribed verbatim by scribes as he delivered his lectures and demonstrations. His writing on anatomy and physiology, contained in the 17 books that make up De usu partium corporis humani (On the Usefulness of the Parts of the Human Body), is a distillation of these observations. (‘Usefulness’ in this context incorporated the teleological view that ‘usefulness’ or ‘utility’ was the result of a purposeful design.) The constraints of Roman law meant that Galen never dissected humans. He apparently declined an invitation to accompany Marcus Aurelius to the German war, where he would have had the opportunity to dissect slain ‘barbarians’ (Mattern, 2013); indeed he wrote scathingly about the surgeons who went, saying that because they had not first honed their dissecting skills on animals, they would learn nothing more than what butchers knew (Savage‐Smith, 1995). He considered that treating the wounds of severely injured gladiators gave him a window into the body: this experience, together with his familiarity with the works of Herophilus and Erasistratus, who almost certainly had dissected humans, and his familiarity with human bones, suggests that he possessed some knowledge of human anatomy. However, despite its title, the anatomy set out in De usu partium corporis humani contains numerous errors that betray its reliance on non‐human anatomy. Galen was aware of this limitation: … In the second chapter of the first book of De Anatomicis Administrationibus [Galen] advises the student to study human material if in any way possible, especially bones, but failing this, not to give up, study an animal. Thus he will acquire a background which can be used to advantage even in work with human patients. … Galen could not dissect human subjects. He chooses an ape, therefore, because it is most like man, definitely second best, but better than nothing, and in many places he calls attention to both likenesses and differences between ape and man if he thinks they are important… (Goss, 1958). Such caveats notwithstanding, Galen's authority was almost universally regarded as sacrosanct until his anatomical writing was challenged by Renaissance anatomists: earlier refutations of some of his claims published by Persian scholars such as Rhazes and Ibn al‐Nafis did not diminish his reputation.
Aretaeus of Cappadocia
Aretaeus of Cappadocia is thought to have lived in the 2nd century CE. Although he was probably a contemporary of Galen, the latter apparently did not mention him in his writing. Aretaeus is now acknowledged as one of the greatest medical scholars of Greco‐Roman antiquity after Hippocrates (Tekiner, 2015): his treatise entitled On the Causes, Symptoms and Cure of Acute and Chronic Diseases is the only extant work by a member of the Pneumatic School (Pearce, 2013). His explanation of a neurological conundrum that had exercised others before him concurs with a similar conclusion reached by Hippocrates (in On the Injuries of the Head), and predates Domenico Mistichelli's description of the pyramidal decussation in 1709 by many centuries. Apoplexy is a paralysis, but a paralysis of the whole body, of sensation, of understanding, and of movement. But if the head be primarily affected on the right side, the left side of the body will be paralysed. If on the left side, the right… The cause of this is the interchange in the origins of the nerves … each of them passes over to the other side from that of its origin, decussating each other in the form of a letter X. Herophilus, Erasistratus, Galen and Aretaeus all appreciated that motor and sensory functions were mediated by separate neural pathways, and they all wrote of the concept of ‘sympathy’, i.e. that parts not visibly connected might nevertheless be functionally related.
The move to the east
The fall of the Western Roman Empire in the 5th century CE signified the start of the Early Medieval Period, an era that previously was somewhat disparagingly, but tellingly, referred to as the Dark Ages. During this time, scholarship and learning in Western Europe were dominated by the stultifying, infallible authority of the Christian Church: productive scientific enquiry of the kind that had so energised the Greek physicians and scholars in previous centuries stagnated for the next thousand years. Manuscripts and books that had not been destroyed by conflagration now migrated further to the East, where they were translated into Farsi, Syriac and Arabic, and then copied and distributed in Southern Italy, Byzantium and throughout the Islamic world during the Islamic Golden Age (Middle Age) of medicine (approximately 7th to 13th century CE) (Abdel‐Halim, 2001). The Bayt al‐Hikmah (House of Wisdom), founded in Baghdad in 830 CE by the Abbasid Caliph Al‐Ma'mun (786–833 CE), was the intellectual hub of Islamic scholarship, where many of the newly imported documents were translated: ‘ownership’ of ancient Greek medical and anatomical knowledge passed to Arabic physicians.
Galen's manuscripts were translated by numerous scholars in the years immediately after his death (Mattern, 2013). Some six centuries later, Hunain (Hunayn) ibn Ishāq (809–873 CE), a Nestorian Christian physician and meticulous translator of Greek medical, philosophical and scientific texts into Arabic, translated over 100 of Galen's books and papers, including his major work on anatomy and dissection, On Anatomical Procedures, as well as smaller anatomical works such as On Bones for Beginners, On Disagreements that Occur Regarding Dissection/Anatomy, On the Anatomy of the Vocal Organs, On the Anatomy of the Eye, On the Movement of the Chest and Lungs, and On the Voice. Hunain, known as Johahnnitius in Latinised versions of his Arabic translations (Dalfardi et al. 2014), travelled from Baghdad to Egypt, Syria and Palestine in search of ancient texts to be translated and also published on his own account, including works on ophthalmology (Ten Treatises of the Eye contained the first detailed anatomical illustration of the eye) and dentistry.
Persian anatomists and physicians upheld some of the misconceptions of their ancient Greek sources, such as the Aristotelian view that there were three ventricles in the heart; developed new ideas, such as Avicenna's re‐interpretation of the Cell Doctrine/ventricular theory (linking the ventricles of the brain to mental function) (Green, 2003); and refuted others. Rhazes (Abῡ Bakr Muhammad bin Zakariyā ar‐Rāzī, 865–925 CE), whose books were based largely on the work of Hippocrates, Galen and Oribasius, was one of the first to express his doubts about some of Galen's conclusions in Kitāb shukῡk ‘alā jālīnῡs (The Book of Doubts about Galen), long before the challenges of European Renaissance anatomists (Compier, 2010). The earliest representation of the cerebral ventricles as four small circles occurs in Rhazes, almost lost within the lines of the text [Kitāb al‐Mansῡrī (The Book of Mansur or Liber Al Mansuri) (de Koning, 1903; Russell, 2013). Novel anatomico‐physiological descriptions, for example by Avicenna (Ibn Sina, 980–1037 CE) and Ibn al‐Nafis (1210–1288 CE), tantalisingly predated much later European ‘discoveries’ of the circle of Willis, the circulation of the blood and the (small) pulmonary and coronary circulations (Cattermole, 1997; Loukas et al. 2008; Bosmia et al. 2013; Karimi et al. 2013). The extent to which Persian anatomists dissected human cadavers is not clear: it is unlikely that human dissection was a widespread practice, if it happened at all under Islamic law (Savage‐Smith, 1995). Scholars such as Mesue (Ibn Masawaih, 777–857 CE) dissected apes for their anatomical studies and teaching, adhering to the Galenic precept of the perceived similarity between the tail‐less apes and humans.
Renaissance anatomy, pre‐Vesalius
By the end of the 12th century, a revivalist movement in the natural sciences was starting in Western Europe that would reach its zenith in the 15th and 16th centuries. Arabic translations of ancient Greek scientific texts were now translated into medieval Latin, particularly in the Toledo School of Translators in the 12th–13th centuries (Arráez‐Aybar et al. 2015a), and were circulated progressively more widely across Europe: Gerald of Cremona translated Avicenna's Canon in Toledo between 1150 and 1187 (Lemay, 1978). Salerno, Bologna, Montpelier and Paris were the first major centres of medical teaching in Europe. Their curricula were based on translations of Galen and Avicenna and were primarily, if not exclusively, text‐based: medieval scholasticism endorsed by the Church ensured a stout defence of Galenic dogma that brooked no dissent. The practice of dissection was introduced in Salerno, albeit using pigs (Anatomia Porci of Copho), on the by now familiar grounds that the internal organs of the pig were similar to those of a man. Frederick II (1194–1250), the Holy Roman Emperor, known as stupor mundi (wonder of the world) ruled that a human body should be dissected at Salerno at least once in 5 years in the presence of the assembled physicians and surgeons of the kingdom, and that no surgeon should be admitted to practice unless he could show that he was …learned in the anatomy of human bodies, and had become perfect in that part of medicine without which neither incisions could safely be made or fractures cured (Pilcher, 1906; Persaud, 1984).
Dismembering and eviscerating cadavers was a widespread practice …as part of a belief system common throughout Europe [as exemplified by] the practice of ‘dispersal burial’ by the nobility, and the veneration accorded the remains of saints (Sawday, 2015). Toward the end of the 13th century, opening human cadavers was occasionally permitted for forensic purposes: the first such dissection is thought to have taken place in 1286 in Cremona, in an attempt to establish the possible cause of an epidemic (Prioreschi, 2001). Several other judicial autopsies were recorded in or near Bologna around the transition of the 13th into the 14th century: for example, in 1302, Bartolomeo da Varignana and four other physicians and surgeons undertook an autopsy on Azzolino degli Onesti. Given the fragmentary knowledge of normal human anatomy at the time, the criteria for identifying ‘abnormalities’ must have been tenuous, but forensic examinations helped to determine mysterious causes of death, and were thought to benefit the public good (Park, 1994). In so doing, they played a significant role in ‘normalising’ dissection as a legitimate means of scientific endeavour at a time when the practice was variously described as cruel, repugnant and ultimately useless, because it could never discover ‘unknowable’ divine design.
Mundinus and Berengario
One of the great milestones for anatomists must be the first public, pedagogical dissection (of an executed woman) by Mondino de Luzzi of Bologna (Mundinus) in 1315. Mundinus was an Italian physician, anatomist and professor of surgery in Bologna and is often called the ‘restorer of anatomy’. He produced what was probably the first book devoted entirely to anatomy, Anatomia Corporis Humani or Anathomia mundini (see Crivellato & Ribatti, 2006 for a selection of passages). Essentially a dissection manual, the folio of 22 leaves was completed in 1316, but not published until 1478 in Padua (Pilcher, 1903), not long after the introduction of metal movable‐type printing in Europe. The book was reprinted frequently thereafter and disseminated widely throughout Europe until its final edition was issued in Venice in 1580: over 40 editions, printings and translations are known. Despite the fact that Mundinus used Latin and Arabic terminologies indiscriminately, making the book what would now be called a ‘difficult read’, it remained the basis of anatomical lectures at the University of Padua into the second half of the 17th century (Olry, 1997). The text was heavily reliant upon the anatomy of Galen and Avicenna and other ancient sources. Its credentials as the ‘first modern anatomy text’ have been queried on the grounds that it perpetuated Galenic and Aristotelian inaccuracies (Infusino et al. 1995). An alternative, less harsh, view is that, though flawed, the Anatomia added to the cumulative empirical experience on which modern topographical anatomy is built. At times, Mundinus appeared to have struggled to reconcile his findings with Galenic dogma; for example, he wrote that the lobes of the liver (five, according to Galen) had not yet fully separated in his specimen. He also offered what could only be dissection‐based observations, for example, he described ‘amigdalae’ (what we now recognise as the thyroid glands), situated under the longitudinal muscles of the neck, below the larynx: this appears to be a novel anatomical finding (Lamberg, 2001). Despite admitting that he had dissected two females in 1315, Mundinus described a seven‐chambered uterus, betraying a lingering belief in the medieval view that the human uterus contained seven chambers or cells (three on the right, three on the left, and one in the middle): this unusual, non‐Galenic, view of the uterus, which is often attributed to Michael Scot (1180–1250), astrologer in the court of Emperor Frederich II (Reichman, 2010), and adopted by the anatomists in Salerno, is apparently a much earlier concept (Kudlien, 1965). Mundinus stated explicitly that he dissected the bodies of criminals: … [To begin a dissection] put the cadaver of the decapitated or hanged person in the supine position … and … The study of these muscles is better done in the desiccated cadaver than in the cadaver of the recently hanged… (Prioreschi, 2001).
Originally without illustration, later copies, including text published within the Fasciculuo de medicina (an Italian version of de Ketham's earlier Fasciculus medicinae) in 1493, contain the oft repeated image of a Late Medieval public dissection, La lezione di anatomia: the highest point in the figure is the seated lector, quoting from a text (usually based on Galen or Avicenna), physically separated from an ostensor standing below him who indicates features that the barber surgeon, incisor or sector, has revealed in the abdominal cavity of a corpse lying on a trestle table (Fig. 1). Most of the ‘audience’ show little or no interest in the proceedings, and the lector looks ahead, not at the corpse: the implication that there is little to be learned from the physical exploration happening in front of them is clear. Other contemporary images of public dissections reinforce the authority of the written word rather than the physical deed in anatomical training at that time: ‘seeing what was believed’ was of far greater importance than ‘believing what was seen’, when the ‘real’ anatomy was at odds with the ‘virtual’, i.e. textual anatomy. Guido da Vigevano (1280–1349) an anatomist, engineer and practising physician, who is thought to have been a student of Mondino de Liuzzi at the University of Bologna, pioneered the use of simple drawings to illustrate his anatomical descriptions in Anathomia, an atlas of anatomy dedicated to Philip VI in 1345. Eighteen of the original 24 plates are extant, of which six refer to neuroanatomical structures and the technique of trephination described (but not illustrated) by the ancient Greeks (Rengachary et al. 2009). By 1347, some of the Italian medical schools required that students attend a dissection. At the medical school in Montpelier, biannual public dissections occurred from 1340 and became annual events from 1378; the corpses were provided by Louis, Duke of Anjou. In 1348, Pope Clement VI allowed his physician to examine the corpses of plague victims in order to try to determine the cause of the disease.
Figure 1.
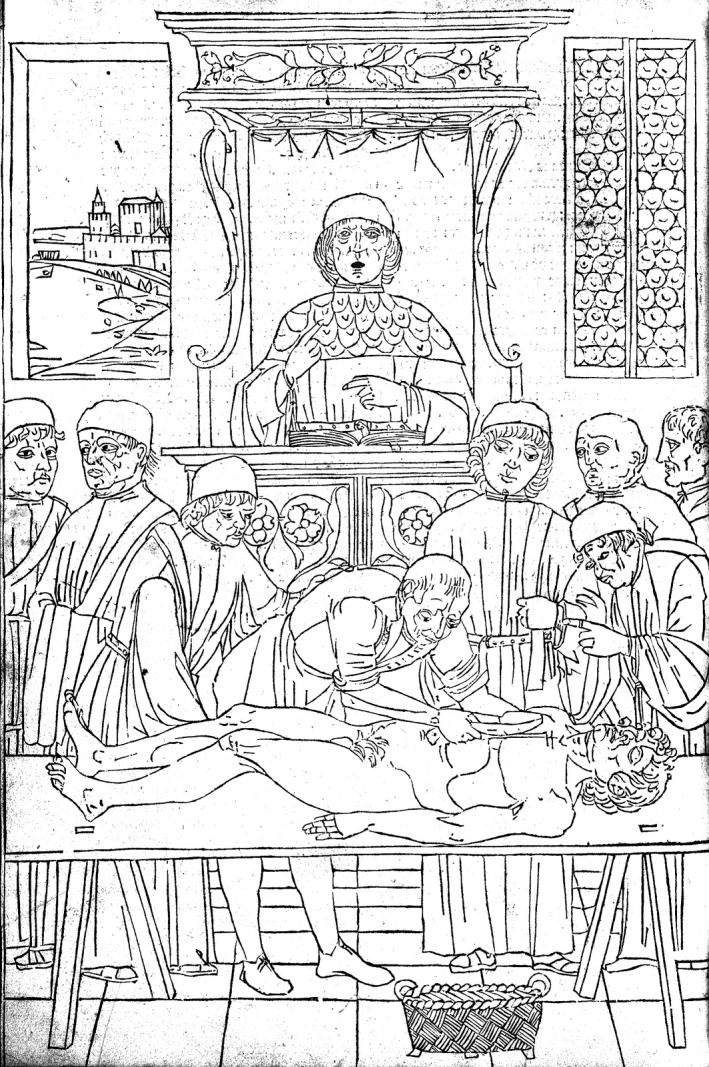
An academic dissection scene where the lector, seated in his high chair, reads the text, an ostensor demonstrates the anatomy and a barber‐surgeon (sector) carries out the dissection. From The Fasciculus Medicinae of Johannes de Ketham. Facsimile of the first, Venetian, edition of 1491. With introduction by Karl Sudhoff, translated and adapted by Charles Singer. R Lier & Co. Milan, 1924. Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
The earliest anatomical diagrams were stylised representations of the texts of the Greco‐Arabic canon. Intended as aids for memorising the text, the pedagogic value of pictures that helped understanding of complexity did not begin to gain traction until Vesalius published the Fabrica in the mid‐16th century. A series of five schematic drawings, named the Fünfbilderserie by Karl Sudhoff, of a human figure in squatting, frog‐like positions, and depicting Galenic anatomical systems (bones, muscles, veins, arteries and nerves), have been found loose‐leaf in 12th and 13th century manuscripts in various sites in Europe and in the Far East and in 14th century Arabic and Persian manuscripts. It has been suggested that the original drawings might have been prepared centuries earlier in Alexandria, presumably during the brief time when human dissection was permitted in the medical school (Sudhoff, 1908; Gurunluoglu et al. 2013).
Jacopo Berengario da Carpi (1460–1530) a surgeon and a member of the faculty of medicine at Bologna from 1502 to 1526, is regarded as the first anatomist who used anatomical drawings that intentionally illustrated the text. HIs massive work, Commentaria cum amplissimis additionibus super anatomiam Mundini (1521), was clearly based on Mondino's Anatomia corporis humani (1493). A shorter, more accessible, version, Isagogae breves, was published in 1522, and contained additional illustrations of the heart and brain. Like Mundinus, Berengario's anatomical descriptions followed the classical stages of dissection (reflecting the varying rates of putrefaction of an unfixed cadaver), namely abdomen chest, brain, muscles, and bones. [Thomas Vicary's graphic explanation of a 16th century dissection will suffice to explain the rationale: The partes contained in the bellie can in no wyse longe continue or endure whcn ye lyfe is once disseveryd from the bodie withoute stynke or noysome savours … that none may approache thereunto to make demonstracion thereof … then the thorax, the head and neck, and lastly the extremities (Copeman, 1963)]. Unlike Mundinus, Berengario had completed as many as 100 cadaveric dissections and so wrote with greater authority, even challenging Galen's description of the existence of a rete mirabile in man (see later). His illustrations were not based on precedents from medieval manuscripts but showed signs of the influence of contemporary artists (Laurenza, 2012). The drawings of the cerebral ventricles in situ in the second edition of Isagogae breves were clearly based on dissected specimens (Fig. 2), and were probably the first to abandon the visual metaphor of three, five or even nine circles previously used to illustrate the Cell Doctrine. [The first detailed drawings of a Galenic dissection of the brain appeared in 1535 in Anatomiae pars prior by Johannes Eichmann (Dryander) of Marburg (Hanigan et al. 1990)].
Figure 2.
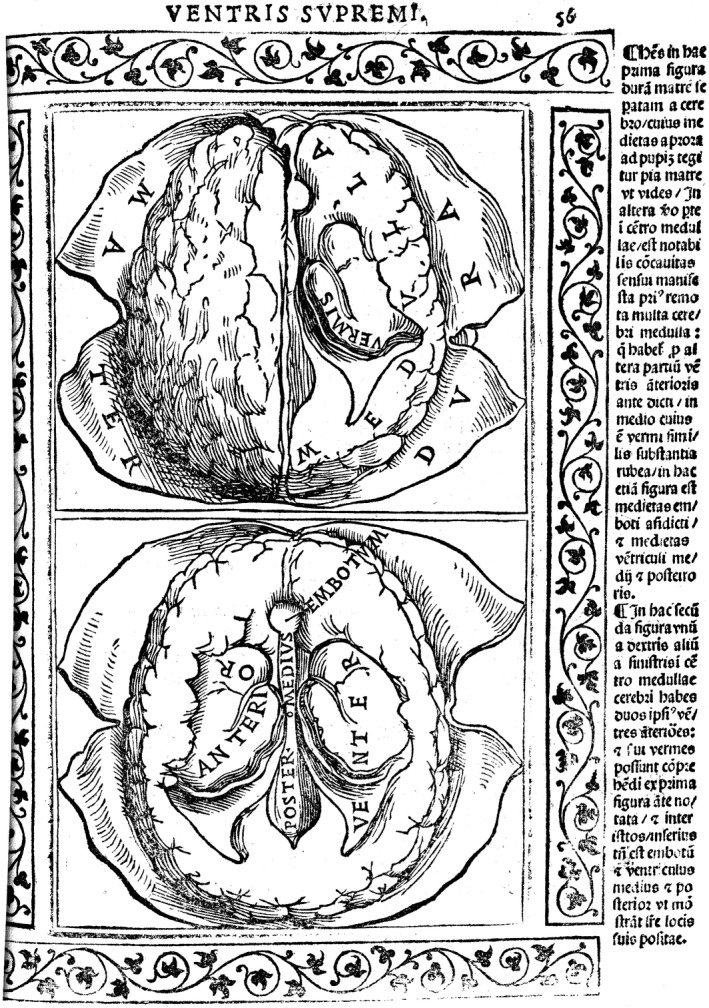
Brain dissected to reveal the ventricles at two levels, from Isagogae breves perlucide ac uberime in Anatomiam humani Corpori (Jacopo Berengario da Carpi, 1523). Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Berengario vivisected animals but recognised the limitations of the practice. Like many other scholars in the 16th century, he was interested in the differences between living and dead bodies: he believed that dissection allowed him to see structures that were not accessible in the living. He dismissed the notion that death caused the vapours or spirits thought to surround the brain and heart to condense into liquid, regarding the fluid that accumulated around the heart postmortem to be a natural consequence of death (Shotwell, 2013). His experiments with injections of water to reveal communications between vessels may have been the earliest use of this technique (Degueurce & Adds, 2010).
The development of (more) accurate representation
The visual language of anatomy changed during the Renaissance. The intellectual tradition that produced the frog‐like figures of the Fünfbilderserie, the gravida figures exemplifying the symbolism of ‘sacred anatomy’ in de Ketham's Fasciculus Medicinae (Sawday, 1995) (Fig. 3), and astrological figures such as the Zodiac men, where man was a microcosm reflecting the macrocosm of the Ptolemaic universe, slowly disappeared: the journey towards the ‘style‐less style’ of modern anatomical images (Kemp, 2010) had begun. A significant first step on that journey was Alberti's (1435/1972) codification of linear geometric perspective in Della Pittura (1435), enabling artists to draw a three‐dimensional solid on a two‐dimensional surface (Blunt, 1978). Of equal significance for anatomists, Renaissance art all'antica was inspired by the style of the ancient Roman and Greek sculptors: as it was based on the human form, artists and sculptors needed to understand how the body was constructed. Ghiberti (1378–1455) explained that … It is necessary for the artist to have seen anatomy in order that the sculptor … wanting to compose the statua virile knows how many bones are in the human body and in a like manner knows all the muscles and … nerves in the body of man… (Mayor, 1964). Although Ghiberti exhorted artists to watch, but not necessarily to perform, a dissection (haver veduto notomia), some artists and sculptors dissected, or at least flayed, corpses to gain the musculoskeletal information they sought. Vasari (1550) wrote that Antonio Pollaiuolo, whose print of the Battle of the Ten Naked Men (Battle of the Nude Men) was the earliest large copperplate engraving (1465) (Fig. 4), …skinned many human bodies to study the anatomy and was the first who thus investigated the action of the muscles in order to draw them correctly. Leonardo da Vinci dissected more than 10 cadavers and made detailed drawings of his preparations: the experience enabled him to criticise his contemporaries for the anatomical implausibility of their finished work: …a good painter must know what muscles swell for any given action, and must emphasise the bulging of those muscles only and not the rest, as some painters do who think that they are showing off their skill when they draw nudes that are knotty and graceless – mere sacks of nuts.
Figure 3.
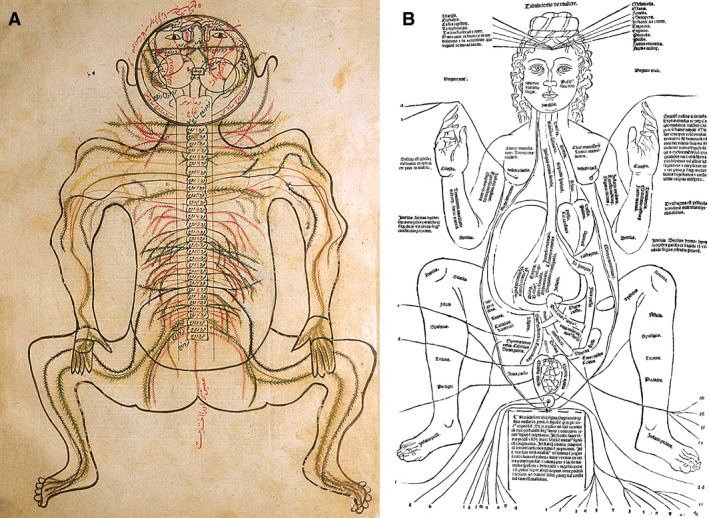
(A) Drawing of the nervous system from Mansur's text. Reproduced with permission from: Shoja MM, Tubbs RS (2007) The history of anatomy in Persia. J Anat 210, 359–378. (B) A pregnant woman. From The Fasciculus Medicinae of Johannes de Ketham. Facsimile of the first, Venetian, edition of 1491. With introduction by Karl Sudhoff, translated and adapted by Charles Singer. R Lier & Co Milan, 1924. Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Figure 4.
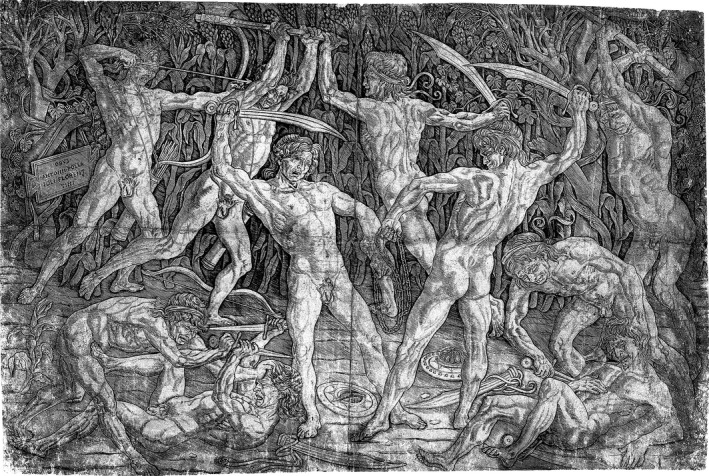
The Battle of the Nude Men, Antonio Pollaiuolo, Florence ca. 1470. Reproduced by kind permission of The Metropolitan Museum of Art, New York.
Artists collaborated with anatomists in the preparation of anatomical drawings for publication, but very few were true ‘artist‐anatomists’. The remarkable drawings prepared by Leonardo da Vinci that speak so eloquently of his anatomical knowledge elicited the following comments from William Hunter in a letter to Albrecht von Haller in 1774: … [da Vinci] was by far the best Anatomist and physiologist of his time … and … certainly the first man we know of who introduced the practice of making anatomical drawings. However, da Vinci's anatomical studies were little known in the 15th and 16th centuries and so will not be considered further here (but see Clayton & Philo, 2012).
The birth of modern human anatomy: Vesalius
Andreas Vesalii (Vesalius, 1514–1564), the ‘father of modern human anatomy’, mapped the human body at a time when other cartographers mapped the heavens (Frisius) and the earth (Mercator, Ortelius). His most famous book, De Humani Corporis Fabrica, was published in the same year as Copernicus’ iconoclastic theory, De Revolutionibus Orbium Coelestium (1543).
The son of the apothecary to Charles V, the Holy Roman Emperor, Vesalius first studied medicine and anatomy in Paris, where he complained that his teaching consisted of …the casual and superficial demonstration of a few organs presented to me and to my fellow students in one or two public dissections by unskilled barbers (O'Malley, 1964). By the early 16th century, Renaissance physicians and anatomists had realised that the ‘barbarous Latin’ of some of the early medieval translators was misleading and often incomprehensible, and sought new translations of the original sources: Johan Guenther von Andrenach (Johannes Guinter), one of Vesalius's tutors, translated Galen's original Greek texts De anatomicis administrationibus and De usu partium. The young Vesalius helped Guenther to prepare dissections for a medical text for students that summarised Galen's anatomy, Institutionum Anatomicarum, Secundum Galeni Sententiam.
The outbreak of war between Henry II of France and Charles V forced Vesalius to leave Paris in 1536, before graduating. He returned to Louvain to continue his medical studies and received the degree of bachelor of medicine in 1537. He then travelled to Italy, enrolling in the medical school of the University of Padua in the autumn of 1537 (Porzionato et al. 2012). He received the degree of doctor of medicine magna cum laude on 5 December 1537 and on the following day accepted an appointment as explicator chirurgiae, charged with lecturing on anatomy and surgery. An enthusiastic and popular teacher, Vesalius created permanent records of his dissections that would be available to study long after putrefaction had destroyed his handiwork. He published six anatomical tables (Tabulae Anatomicae Sex), as so‐called ‘fugitive sheets’ for his students: these very large woodcuts surely rank as some of the earliest, and certainly the most spectacular, student ‘hand outs’ ever produced. Three of the sheets showed the portal, caval and arterial systems and were based on charts drawn by Vesalius while he was teaching; the others show anterior, lateral, and posterior views of a skeleton standing on the ground in life‐like poses and were drawn by Jan Stefan van Calcar from a human skeleton that had been articulated by Vesalius. The anatomy illustrated in the Tabulae is quite clearly Galenic anatomy: for example, the chart of the arterial system included the rete mirabile and the liver was five‐lobed. Vesalius had access to a relatively plentiful supply of cadavers, possibly supplemented by grave robbing, but mainly reflecting his good working relationship with Marcantonio Contarini, a sympathetic judge in the criminal court who apparently arranged the time of executions according to the anatomist's needs. Vesalius was reported as telling his students that … After dinner … I shall demonstrate the remaining inner muscles of the thigh and perhaps also of the leg with the foot to complete the whole anatomy of the muscles of the body. For tomorrow we shall have another body – I believe they will hang another man upon which I shall demonstrate to you all the veins, arteries and nerves … for this subject is now too dryed and wrinkled… (Sawday, 1990). In 1546, he reminisced that … I shall no longer bother to petition the judges to delay an execution to a time suitable for dissection.
As he worked, Vesalius accumulated empirical evidence of ‘discrepancies’ between the anatomy he saw in the human cadaver and the anatomy that he read in Galen's notes. In his ‘Letter on the China root’, Vesalius wrote that he had lectured in Padua on Galen's book On the Bones three times …before I dared call attention to his mistakes… (O'Malley, 1964). He had scrutinised Galen's writing for a new edition of Guenther's student textbook, and so was well versed in the errors it perpetuated. Presumably he was also aware of Berengario da Carpi's criticisms of Galen's anatomy. Vesalius began to voice his doubts in public. In January 1540, he was invited by the students at the University of Bologna to perform a public dissection. In front of an audience of some 200 spectators in the Church of San Francesco, he openly challenged Galen's anatomical descriptions, angering the orthodox Galenic anatomist Matthaus Curtius (Matteo Corte) who was lecturing with him [the combination of lecturer and dissector was a common practice in public demonstrations (Klestinec, 2011)].
During the period 1539–1543, Vesalius prepared the book for which he is remembered, De Humani Corporis Fabrica Librorum Septem, seven books in which he challenged the belief that Galen had described human cadaveric anatomy, using over 200 illustrations of his own dissections with …a likeness that could deceive the eye. The title‐page of the Fabrica abandoned the previous conventional depiction of lector, ostensor and sector and showed Vesalius assuming all three roles as he dissected a female corpse in a crowded theatre (Fig. 5) (see Sawday, 1995, for an analysis of the complex messages conveyed on the title‐page). The detailed drawings within the Fabrica surpassed any previous depictions of the dissected human body. The 14 Vesalian ‘muscle men’ in Book 2 (Fig. 6) are …arguably the most important of all illustrations in the history of medical science… Whoever was responsible for the consummate artistry of the muscle‐men … the process of their planning, design, delineation and execution represents one of the most remarkable achievements in the history of anatomical art and in the art of anatomical illustration (Kemp, 1970). Illustrations were no longer simply aides‐mémoires to learning, they now facilitated understanding. The identity of the artists and woodcutters is uncertain; speculative attributions to Titian or van Calcar have not been substantiated. The woodcuts were transported over the Alps to Basel, where they were printed and published by Johannes Oporinus (Johann Herbst), one of the most important printers of the 16th century. Two hundred of the woodblocks apparently survived until World War II, but were destroyed in the Allied bombing of Munich (Scatliff & Johnston, 2014). There were probably several reasons why Vesalius chose not to have the book published locally in Italy. Not only had Basel overtaken Venice as the publishing centre of Europe, but Oporinus's former partner Robert Winter had published the second edition of Vesalius's pamphlet on Rhazes as well as his Venesection Letter of 1539. Possibly Vesalius thought that his Latin text would be printed accurately because Oporinus was a scholar of both Latin and Greek. He may also have feared that his Galenist opponents based in Padua would seek to delay publication of the Fabrica in Italy. The choice of woodcuts is interesting, given that Pollaiuolo had used copperplate engraving almost a century earlier in 1465, and likely reflects local preference: publishers north of the Alps continued to use woodcuts for their books and atlases, whereas their Italian counterparts preferred engraving (Campbell, 1987). Vesalius was concerned that his work would be plagiarised. In his letter of instruction to Oporinus, he bemoans …the fate of my Tabulae anatomicae, originally published three years ago in Venice and afterward hideously plagiarised everywhere even while it was being dressed up in more pretentious titles. His concern was justified: the figures in both the Fabrica and the Epitome (a shorter version of the Fabrica) were plagiarised by many anatomists throughout Europe well into the next century. Figures appeared in books by anatomists including Thomas Lambrit (Thomas Geminus, a Huguenot printer and unqualified surgeon, 1545), Juan Valverde de Hamusco (1556), Ambroise Paré (1575) and Helkiah Crooke (1615) (Lanska & Lanska, 2013). The text of the Fabrica is rarely remarked upon with the enthusiasm that continues to be afforded to the figures, indeed it has been described as …one of the most famous, visually familiar, of all unread books… (Nutton, 2012). Moreover, the Fabrica was too expensive for most potential readers to purchase. Did he but realise it, extensive plagiarism, although exceedingly irksome at the time, played a significant role in disseminating Vesalius's illustrations and his view of post‐Galenist anatomy throughout Europe.
Figure 5.
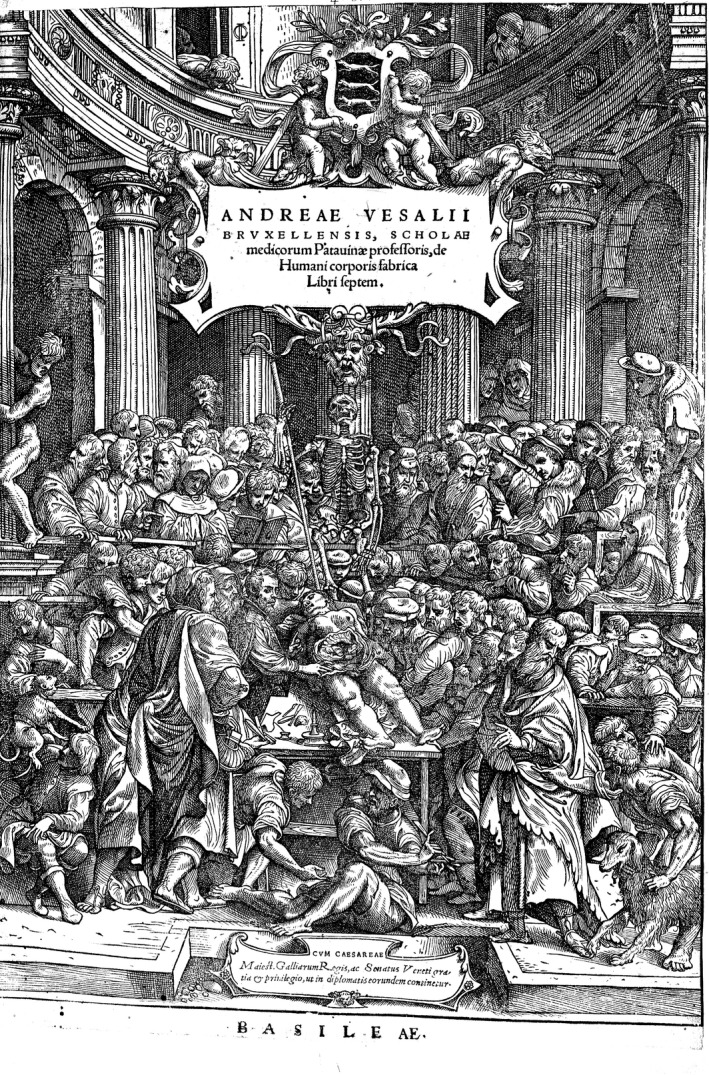
Title page. De humani corporis fabrica, Andreas Vesalius, Basel (1543). Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Figure 6.
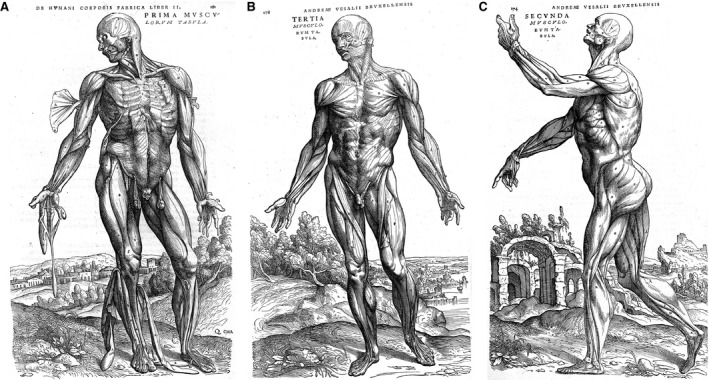
Three of the series of ‘muscle men’ from De humani corporis fabrica, Andreas Vesalius (1543). Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Much of the description of the brain and its functions in the Fabrica is very similar to that in Galen's De Usu Partium. Vesalius continued the Galenic practice of ordinal numbering of cranial nerves, listing seven, slightly altered, pairs of cranial nerves, including the trochlear nerve (Shaw, 1992). He famously disagreed with Galen about the rete mirabile (wondrous net). This meshwork of small branches of the internal carotid artery is found at the base of the brain in ungulates but not in man: it had been described by Herophilus, prompting the speculation that he had not dissected human cadavers, or at least had not dissected human brains. Galen had considered it to be the site where the vital spirits were converted into the animal spirits (psychic pneuma), a transformation that he regarded as a requirement for reasoning and movement. Galen described the rete as looking …as if you had taken several fisherman's nets and superimposed them. Berengario was probably the first to deny its existence in man and criticised others for their belief in Galen, in the manner of the little boy addressing the crowd in the story of the Emperor's New Clothes. Having dissected at least 100 heads, Berengario confidently stated that … I believe that Galen has imagined the rete mirabile and he never saw it and I believe that other men after Galen believe in the rete mirabile more because of the opinion of Galen than because of fact… (Berengario, Isogoga Breves, 1522). Vesalius initially hedged his bets, retaining the rete mirabile in Tabula III of the Tabula Anatomica Sex. However, he found no evidence of a rete mirabile when dissecting human brains, and removed it from drawings of the arterial system in the Fabrica. Instead, two small drawings comparing the rete as described by Galen in De usu partium and as Vesalius saw it in a dissected ovine brain, are accompanied by these self‐reproachful words … I myself cannot wonder enough at my own stupidity and too great trust in the writings of Galen and other anatomists; yes, I who so much laboured in my love for Galen that I never undertook to dissect a human head in public without that of a lamb or ox at hand, so as to supply what I could in no way find in that of man, and to impress it on the spectators, lest I be charged with failure to find that plexus so universally familiar by name. For the soporial [internal carotid] arteries quite fail to produce such a ‘plexus reticularis’ as that which Galen recounts. Despite Vesalius's denials, the rete mirabile appeared in human anatomy texts until the end of the 18th century, often accompanied by caveats such as Veslingius's admission that …it could be seen more clearly in unreasoning animals than in humans… (Pranghofer, 2009; Ghosh, 2014). [For further reading on Vesalian neuroanatomy, see Catani & Sandrone, 2015].
Vesalius was not the first to advocate that anatomy was best learned by dissecting cadavers rather than reading texts or watching others dissect: pre‐Vesalian anatomists similarly exhorted their students, although most were of necessity referring to animal anatomy, whereas Vesalius was concerned with what would now be regarded as ‘evidence‐based’ human anatomy. Like his predecessors, Vesalius also performed vivisections, and at the end of the Fabrica he echoed Galen's words … Through dissection of the dead we gain accurate knowledge of the number, position, shape, special substance, and composition of each part of the body; and from dissection of a living animal learn about the function [functionem] of each part, or at least gain information that may lead us to deduce that function… (Richardson & Carman, 2009). He repeated Galen's demonstrations on the role of the recursive nerve in phonation, but most of his experiments on animals focused on the nature of the arteries. Unlike Berengario, Vesalius sought to explore the ‘function’ of various structures using dissection as a research tool and was much less concerned with the anatomical consequences of post‐mortem change (Shotwell, 2013). He deliberately included animal anatomy in the Fabrica, for example, by adding muscles only found in dogs or baboons, but which Galen had described as human, or, out of necessity, illustrating a canine hyoid bone because the human counterpart had been damaged during judicial strangulation.
Supporters of Galen were understandably outraged by the claims made in the Fabrica and launched vituperative attacks on Vesalius, railing against his perceived disloyalty to Galen. Jacobus Sylvius, Vesalius's old teacher in Paris, condemned him, justifying the continued use of Galen's texts on the grounds that the human body had clearly changed in the years since Galen. He wrote that the Fabrica contained error‐ridden filth and that it had been published by …an insolent and ignorant slanderer who has treasonably attacked his teachers with violent mendacity. Vesalius burned his manuscripts and made no further contributions to anatomical thinking other than making corrections for the second edition of the Fabrica in 1555.
Anatomical thinking did not change immediately after publication of the Fabrica, but the gauntlet had been thrown down. Vesalius had shown that the body, not ancient texts, was the source of accurate information. Galen's authority had been challenged and would ultimately disappear over the next hundred years. The era of the modern ‘scientist‐anatomist’ had begun.
Four 17th century anatomists
Thomas Willis
Thomas Willis (1621–1675), is regarded as the founder of modern clinical neuroscience and comparative neuroanatomy (Molnár, 2004; Arráez‐Aybar et al. 2015b). A chemist and clinician (albeit after an unconventionally brief formal medical education), Willis was initially interested in chemistry and its application to medicine and there is little to suggest an early interest in neuroanatomy before his appointment as Sedleian Professor of Natural Philosophy at the University of Oxford in 1660. As holder of this post, Willis would have been expected to deliver a traditional lecture course, based on Aristotle's natural philosophy. In preparing his lectures, he appears to have become dissatisfied with the …received opinions of others [and] the suspicions and guesses of my own mind…, and wrote that henceforth he intended …to believe nature and ocular demonstrations. His motivation to learn more about the anatomy of the brain, using a scalpel rather than a pen to …unlock the secret places of Man's Mind [in order] to look into the living and breathing Chapel of the Deity, may in part have reflected his devout Anglicanism: was he hoping that detailed exploration of the brain would reveal the location of the rational human soul, which he believed to act on the brain (O'Connor, 2003; Caron, 2015)? The results of Willis's scepticism, prompted no doubt by his unconventional medical education, which had spared him prolonged exposure to the teachings of Aristotle, Hippocrates, Galen and Avicenna, were seminal publications that collectively and quite intentionally presented the …first systematic attempt to integrate anatomical observations into a broader philosophical argument about human nature (Caron, 2015). Willis intimated the nature of this grand design at the end of the Cerebri Anatome: … A superstructure may indeed be promised to be laid upon this foundation laid…. Thus the first book, Cerebri Anatome cui Accessit Nervorum Descriptio et Usus (Anatomy of the brain and the descriptions and use of the nerves), laid the anatomical foundation for his subsequent books on neuropathology (Pathologiae Cerebri et Nervosi Generis Specimen and the second part of De Anima Brutorum Quae Hominis Vitalis ac Sensitiva Est) and on physiology (the first part of De Anima Brutorum) (Molnár, 2004). He was under no illusions as to the immensity of the task he had set himself …to explicate the uses of the Brain, seems as difficult a task as to paint the Soul, of which it is commonly said, That it understands all things but itself…
Cerebri Anatome, published in 1664, is regarded as the first great neuroanatomical text: it influenced the way the brain was perceived for almost 200 years. Willis was assisted by members of the Oxford Experimental Philosophy Club (The Invisible College) who met every Thursday to perform experiments and discuss their findings. The group included Christopher Wren, Savilian Professor of Astronomy, who drew many of the fine illustrations (copperplate) (Fig. 7) (Cavalcanti et al. 2009); Richard Lower, who undertook most of the dissections, particularly of the peripheral nervous system; Thomas Millington, a physician who succeeded Willis as Sedelian Professor of Natural Philosophy; and Robert Boyle, who developed ways of preserving and hardening brains in ‘spirits of wine’ that preserved structures at the base of the brain and facilitated detailed dissection (the usual way of examining unfixed brains had been to slice them in situ) (Scatliff & Johnston, 2014). The Cerebri Anatome contains many new neuroanatomical terms, including anterior commissure, cerebellar peduncles, corpus striatum, and the word ‘neurology’ (which first appeared in Samuel Pordage's translation of the Cerebri from Latin into English in 1681). Like others before him, Willis chose names that had no connection with any putative function (as none was yet known) but referred to some characteristic feature such as colour, shape or location; thus the corpus striatum was a ‘striped body’ and the vagus nerve ‘wandered’. Interestingly, although Willis is credited with naming the vagus nerve, Caspar Bartholin the Elder (1585–1629) is said to have introduced the term nervus vagus in 1611 in the Institutiones Anatomicae (Porzionato et al. 2013).
Figure 7.
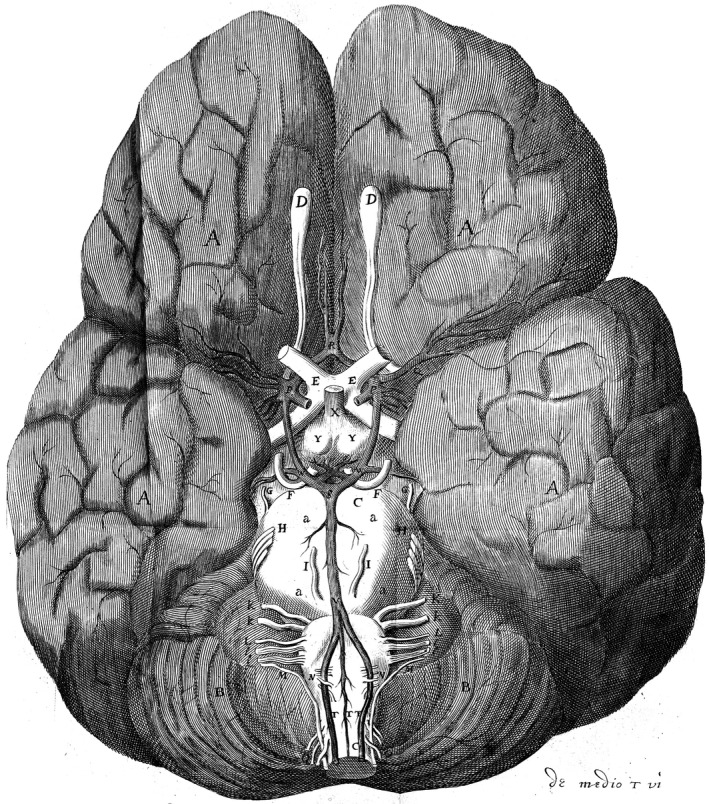
The base of a human brain (the first figure in Cerebri Anatome): the circle of Willis is illustrated. Nicolaus Steno (1638–1686) commented that …the best figures of the brain up to the present are those presented to us by Willis. Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Willis divided the brain into three functional regions, cerebri (cerebral cortex), cerebel (cerebellum) and corpus striatum, whereas previously the brain had been subdivided into cerebri and cerebel. The elevated status of the corpus striatum reflected Willis's belief that it behaved as a ‘neural crossroads’ where all the senses merged and where instructions (animal spirits) were received from the overlying cerebri and reflected back to the periphery. He demoted the function of the cerebral ventricles as posited in the various versions of the Cell Doctrine theory, regarding them as ‘mere sinks’ to collect detritus, proposing instead that the grey regions of the cerebri were the seat of higher human cognitive functions and that the corpus callosum allowed animal spirits to travel between the two sides of the brain. He considered that automated movements were produced in the cerebel, whereas the cerebrum was the …primary seat of the rational soul in man, and of the sensitive soul in animals. It is the source of movements and ideas. Willis reclassified and renumbered the cranial nerves into nine pairs (Galen and Vesalius had only identified seven pairs). The first six nerves were numbered as we know them today; the auditory and facial nerves were combined as the seventh nerve; the glossopharyngeal, vagus and accessory nerves were grouped together as the eighth nerve, and the hypoglossal became the ninth cranial nerve (Shaw, 1992; Davis et al. 2014). Willis did not dismiss the existence of a rete mirabile entirely in man, but, like Veslingius, he argued that it was only found in …those sort of man … being of a slender wit or unmoved disposition, being otherwise confined to lesser animals. He proposed a mechanistic role for the rete in animal brains, principally in regulating the pressure of the blood flow into the brain (Pranghofer, 2009).
Willis is remembered mainly because of the eponymous arterial circle, but he never claimed this honour for himself and his name was only associated with the circle over a century later by Albrecht von Haller as the circulum qui dicitur Willisii in his Bibliotheca anatomica (1774) (Meyer & Hierons, 1962). Portions of the vascular anastomosis at the base of the brain had already been described by others including Berengario da Carpi, Vesalius, Falloppius, Casserius, Veslingius (the first to describe the posterior communicating arteries bilaterally) and Wepfer (probably the first to describe the complete circle textually; Lo & Ellis, 2010). Other anatomists had ignored it, perhaps because they were unable to differentiate arteries from veins or had assumed it to be a variant of the rete mirabile. Willis was interested in the blood supply of the brain and to that end he developed experimental injection protocols with his colleagues. Working with Lower, he had found that after injecting an inky liquor into one of the carotid arteries …vessels got revealed in every secret place of the brain and cerebellum by filling with the same colour. From a clinical perspective, he wondered how what he termed the ‘four chariots’, namely the two internal carotid arteries and the two vertebral arteries, could maintain a cerebral blood supply so that …if by chance one or two should be stopt, there might easily be found another passage instead of them. Richard Lower explained how this problem was examined and ultimately resolved in a letter to Robert Boyle: …we took a young spaniel, and tied both carotid arteries in the neck very fast and close with silk, and the dog was not at all altered by it, but continued very lively and brisk, and was so far from taking unkindly what was done to him, that within a quarter of an hour after, he got loose and followed the doctor into the town… In this pleasant humour he continued two or three days, and then we opened his head, and found all the vessels of the brain as full of blood as usually they are in other dogs, who do not suffer the same experiment. But this I might have told you in a shorter time; for if one artery be syringed with any tinctured licquor, all the parts of the brain will be equally filled with it at the same time, as several times we have tried. Apparently the Royal Society arranged for Dr Walter Charleton to confirm these observations, and when he found differences between human and animal brains, it was suggested that these discrepancies should be communicated discretely to Willis, since he had already presented the Society with a copy of the quarto edition of Cerebri Anatome (Compston, 2011).
Willis sometimes followed his patients for years and tried to relate their clinical histories with anatomical changes he found at autopsy (often performed by Lower). His sound dissection‐based knowledge of normal anatomy allowed him to recognise achalasia of the cardia, unilateral degeneration of the cerebral peduncle in a case of long‐standing unilateral paralysis, and morphological abnormalities of the brain in cases of congenital mental retardation, among other cases, long before the underlying pathological mechanisms had been established.
Raymond de Vieussens
Willis was not the only neuroanatomist of note at this time, although his name is probably the best remembered. Raymond de Vieussens, a French anatomist and physician, wrote the Neurographia Universalis, Hoc est, omnium corporis humani nervorum, simul et cerebri, medullaeque spinalis descriptio anatomica (1684), regarded as one of the most complete, accurate and well‐illustrated descriptions of the brain, spinal cord and peripheral nerves to be published in the 17th century. Neurographia Universalis contains descriptions of the white matter of the centrum ovale and the continuity of the white matter fibres that carried ‘animal spirits’ from the centrum ovale to the brainstem. Based on his dissections, Vieussens clarified the relationship between the optic nerve and the lateral geniculate nucleus of the dorsal thalamus, and is credited with providing the first descriptions of the dentate nuclei, the pyramids and the olivary bodies. His pioneering work on the heterogeneity of white matter tracts laid the basis for many future studies that culminated in modern hodology (Vergani et al. 2012). Vieussens did not confine his research to the nervous system: he later published Nouvelles Découvertes sur le Coeur, in which he presented the detailed anatomy of the lymphatics and blood vessels of the heart (Loukas et al. 2007).
Humphrey Ridley
Humphrey Ridley is remembered by the cognoscenti for the eponymous circular sinus, but rarely, if ever, cited in the context of his pioneering work on skull base venous anatomy, then a region of almost uncharted territory and now the fiefdom of skull base surgeons. The title of his book, published in English in 1695, makes clear that he intended to provide his readers with a description of The Anatomy of the Brain Containing its Mechanisms and Physiology: Together with Some New Discoveries and Corrections of Ancient and Modern Authors upon that Subject. Whenever possible, he worked on bodies freshly taken down from the gallows so that the veins of the skull base were still engorged. He injected tinged warmed wax or quicksilver into the vessels: the warmed wax solidified on cooling, emphasising the vascular anatomy and facilitating dissection. (Leonardo da Vinci had used a similar technique to examine the three‐dimensional anatomy of the cerebral ventricles, but his work had yet to be rediscovered.) Using this technique, Ridley made a number of original findings that are only now being recognised. He demonstrated the intercavernous venous sinuses and the draining veins of the corpus striatum (Compston, 2012; Thakur et al. 2012) and pointed out that Willis had failed to show the origin of meningeal arteries from the intracranial internal carotid artery. He may have been the first to describe the ophthalmic artery, although this discovery is usually attributed to Zinn and to Albrecht von Haller, much later in the 18th century.
Until the 17th century, the brain was thought to have only two coverings, the dura mater and the pia mater. Gerard Blaes, a Dutch anatomist, had discovered and named the arachnoid membrane in 1664 (Sanan & van Loveren, 1999). Further descriptions of the arachnoid are usually attributed to Andreas Ottomar Goelicke (1697) and Frederick Ruysch (1699), but Ridley had demonstrated a retiform membrane that spanned the cortical gyri, and that ‘…may be called after the same name of that membrane investing the crystalline Humor of the eye, Arachnoeides… in 1695: according to Goodrich (2000) this was the first thorough description of the arachnoid membrane. Ridley also described the subarachnoid cisterns (now called cerebellomedullary, quadrigeminal and olfactory cisterns), predating the findings of Bichat and Magendie in the 19th century (Thakur et al. 2012). Some 300 years later, the subarachnoid cisterns and the arachnoid membranes provide the natural corridors and planes for atraumatic dissection during brain surgery (Lü, 2015). Other ‘firsts’ attributed to Ridley are the experimental demonstration that cerebral arteries did not open into the cranial venous sinuses and the first accurate description of the trigeminal ganglion and its three branches (Vieussens had described only two branches). Like Willis, Ridley wanted to know how a circulation to the brain was maintained in his patients …if even three of the four great arteries, which furnish this part with blood were totally obstructed, there would yet be a way left for a competent supply from the other unobstructed fourth. These I call the communicant branches (Ridley, 1695): his description of the arterial circle included the posterior cerebral and superior cerebellar arteries with the oculomotor nerve between them, whereas Willis did not mention these arteries (Veith et al. 2015).
William Harvey
William Harvey (1578–1657) took his first degree at Gonville and Caius College, Cambridge, and then travelled to Padua to study medicine, where he was a pupil of Fabricius. In 1615, Harvey was elected Lumleian Lecturer of the Royal College of Physicians, a role he fulfilled on alternate years for the next 30 years. In 1628, after much deliberation, he published his seminal work on the circulation of the blood Exercitatio anatomica de motu cordis et sanguinis in animalibus (Concerning the Motion of the Heart and Blood), considered by some to be the finest achievement of renaissance anatomy (McKechnie & Robertson, 2002). De motu cordis was published in Latin in Frankfurt when Harvey was 50 years old: the first English translation did not appear until two decades later.
Ibn Nafis (mid‐13th century) and Servetus (1553) had both suggested that blood flowed from the right side of the heart to the left side via the lungs rather than through pores in the interventricular wall (as Galen had suggested) (Bestetti et al. 2014). In De Re Anatomica, Libri XV (1559), Realdo Colombo, a Paduan anatomist and assistant to Vesalius, described the pulmonary loop and the contraction and relaxation phases of the heart, and showed that pulmonary veins contained blood not air: Harvey referred repeatedly to Colombo's findings in De motu cordis. Andrea Cesalpino (1571) also described the pulmonary loop and demonstrated experimentally in animals that a ligated artery bulged on the cardiac side, implying blood flow toward the periphery, whereas a ligated vein bulged on the peripheral side, implying flow toward the heart (Pasipoularides, 2013). Fabricius described venous valves in 1603, but he concluded that they functioned to prevent overdistension of the veins and retard blood flow in the systemic loop. Harvey incorporated all of these findings, together with the results of his own experiments on cold‐ and warm‐blooded animals, into his theory. He proposed that the blood circulated in one direction around the body, driven by the mechanical pumping action of the heart; that auricular contraction preceded ventricular contraction; and that the arterial pulse was the shockwave of the beating heart and not the intrinsic pulsatility of the arterial walls as previously believed (the clinical relevance of the pulse implied by this finding was not immediately appreciated by physicians, including Harvey himself). Harvey's theory replaced Galen's open‐ended system in which blood ebbed and flowed (Aird, 2011). He assumed, but could not prove, a physical connection between arteries and veins: the demonstration of capillary circulation by Malpighi in 1661 in De Pulmonibus provided the missing link.
Viewing the body: public and private spectacles
In Northern Europe, in the high and later Middle Ages, a recently dead body was rarely opened, other than for the purpose of ‘division of the corpse (Mos Teutonicus)’, a practice favoured by northern European royalty and aristocracy. Consequently, documented references to autopsies and dissections are virtually unknown in Germany, England and France before the 15th century. It has been suggested that this geographical dichotomy reflected very different cultural sensitivities towards the status of a corpse. Italians believed that death involved the rapid separation of body and soul, after which a corpse was seen as an inert, insensitive vessel, whereas northern Europeans regarded death as a protracted process that continued until only the bony skeleton remained, from which it could be inferred that a recently dead corpse was somehow still ‘sensitive’ or ‘semi‐animate’ (Park, 1995).
During the 14th century, the dual practices of dissection (opening and dismembering a corpse as part of an anatomical demonstration) and autopsy or postmortem (examining the viscera of a corpse in order to determine the possible cause of death) spread rapidly among the cities of northern and central Italy. Autopsies were often requested by families and undertaken domestically in the home of the deceased, whereas dissections were public events attended by students and the fashionable elite. Berengario recalled in his Commentaria (1521) that he had displayed the placenta of a woman who had been executed …before almost five hundred students of our University of Bologna and also many citizens… (Ferrari, 1987). The curricula of the new medical schools offered relatively few opportunities to observe a dissection, although students studying at the Universities of Perugia, Padua or Florence were expected to attend at least one dissection before graduating. Corpses of executed criminals or paupers who died in charitable hospitals were used, but with the proviso that …only unknown and ignoble bodies [could] be sought for dissection, from distant regions without injury to neighbours and relatives… (Benedetti, 1497, quoted in Park, 1995), a stipulation that significantly reduced the number of available corpses, but ensured that the audience was unlikely to recognise the corpse.
By the 15th century, Italian anatomists needed more corpses to dissect than the law allowed. To obtain more bodies, physicians might suggest that a postmortem be undertaken even when the cause of death was known, and students might be asked to pay for and attend the funerals of those they had dissected, in the hope that a free funeral would encourage families to offer their deceased relatives for dissection. Grave robbing and plundering rotting corpses in charnel houses increased the number of corpses and body parts available for study, and concomitantly fuelled a public suspicion of anatomists’ activities that was to last for centuries. Vesalius was probably describing the behaviour of many similarly enthusiastic anatomy students when he recalled picking over corpses in the charnel house by the public gallows at Montfaucon and at the Cemetery of Innocents while he was a student in Paris, and disarticulating a dried skeleton found by the roadside when he was a student in Louvain (Saunders & O'Malley, 1950). He later described the efforts of his own students to avoid prosecution. …At Padua the students snatched from the tomb and brought to the public dissection the body of a lovely dame of ill repute, the mistress of a monk of St. Anthony … they took great care to remove all the skin from the cadaver so that she could not be identified by the monk, who joined the harlot's parents in laying complaint before the city prefect over its removal from the tomb (Vesalius, 2007).
Anatomy theatres in Europe date from the latter half of the 15th century. Initially they were temporary structures made of wood that could be erected and dismantled as needed for public dissections (a dissection undertaken in front of an audience, composed mainly of students but also including representatives of the university and worthy citizens). As the popularity of public ‘anatomies’ increased, purpose‐built anatomy theatres were erected in various Universities, including Padua (1594), Bologna (1595), Leiden (1596) and Paris (1604). Seats were allocated according to rank, a task entrusted to a praefectus, while custodes kept the importunam plebem away and two quaestores collected money to cover expenses (Ferrari, 1987). From the 16th till the early 18th century, public anatomy lessons in the Italian theatres were held either at Christmas or during the carnival. The occasions could become boisterous: Vesalius recorded that huge crowds attended his dissections of the genital organs.
The motto carved in the anatomy theatre in Padua, Hic locus est ubi mors gaudet succurrere vitae (This is a place where the dead are pleased to help the living), explicitly stated the intended purpose of the theatre: the same sentiment, albeit expressed slightly differently, still greets medical students in many dissecting rooms around the world. English travellers returning from their ‘Grand Tour’ of the European continent expressed disappointment at the lack of local opportunities to attend public dissections in ornate, bespoke theatres such as those they had seen abroad (Sawday, 1995). Anatomy clearly fascinated Renaissance audiences, just as exhibitions of plastinated prosections such as BodyWorlds™, today draw vast crowds of sightseers to be ‘edutained’ (Moore & Brown, 2004; Walter, 2004; Jones, 2016).
Sourcing cadavers in England: 16th to 19th centuries
In the centuries before regulatory legislation and modern body donation schemes, obtaining cadavers to dissect was not easy in England. The Guild or Fellowship of Surgeons and the Barber's Company both claimed the right to practise surgery in London during the 15th century. An Act of Parliament in 1540 brought these two often disputatious groups together as the Company of Barbers and Surgeons of London: the Act decreed that no surgeon was to perform the tasks of a barber, and vice versa, excepting only the drawing of teeth. The union is commemorated in a Holbein painting showing Henry VIII handing the Charter with its Great Seal to Thomas Vicary: an inscription in Latin in the upper left quadrant of the painting, …and by thy counsel men study the monuments of Galen… reminds the viewer of the persisting potency of the ancient Greek polymath. (The Charter and Seal are both artistic licence, because the union was established by Act of Parliament.)
Convicted murderers could be dissected by anatomists after they were hanged: ‘opening of the body’ was a fate reminiscent of the medieval practice of hanging, drawing and quartering of traitors and was an additional punishment inflicted upon the corpse. The newly formed Barber Surgeons were charged with providing technical and theoretical education to surgical apprentices and were permitted to dissect four bodies annually in the Barber Surgeons’ Hall in Monkwell Street, London, located close to Newgate Prison. Samuel Pepys famously described a visit to Chyrurgeon's [sic] Hall on 27 February 1662/1663 for a lecture on the kidneys and ureters, after which he had …a fine dinner and good learned company, later returning to the Hall alone to see the cadaver: the body was of …a lusty fellow, a seaman, that was hanged for a robbery. I did touch the dead body with my bare hand: it felt cold, but methought it was a very unpleasant sight… (http://www.pepysdiary.com/diary/1663/02/27/). Collecting the permitted corpses from the gallows usually involved scuffles between agents of the Barber Surgeons and the relatives and friends of the executed felon: the lifeless corpse might be taken down and sold more profitably to a private anatomy school during the melee. The beadles found their task more and more difficult and the scenes at Tyburn became a scandal. Fights were frequent and sometimes the beadles had to return empty‐handed, while on other occasions they were pursued, intercepted and the body was taken from them … sometimes with the assistance of constables and others they succeeded in regaining it after an unseemly struggle (Lett, 1943). At least one of the four permitted dissections was to be held in public each year and tickets were issued to watch the dissection. John Caius (1510–1573), an English physician who graduated from Cambridge and who had studied in Padua with Vesalius and Montana, is generally credited with introducing the study of practical anatomy by human dissection into England: he performed annual dissections before the Barber Surgeons for almost 20 years (Nutton, 1979). The Barber Surgeons prohibited their members from conducting private ‘anatomies’ unless permitted to do so by the Company's officer, but this proscription was frequently ignored. In 1564–1565, Henry VIII's daughter, Elizabeth I, granted the Royal College of Physicians of London a charter permitting the College to obtain the bodies of four criminals for public dissection each year (Forbes, 1974).
By the middle of the 17th century, the idea that dissection‐based anatomy was relevant to the study of medicine, for example in the interpretation of clinical case histories, was gaining ground. The supply of bodies from the gallows could not satisfy the demands for corpses for education and research. Legal measures such as increasing the number of crimes punishable by hanging proved ineffective. Public attitudes to dissection remained largely negative: as anatomisation was the antithesis of the belief that all bodies should be buried intact, its implementation provoked widespread disquiet. In his Essay Towards the Improvement of Physick (1714), John Bellars wrote that …it is not easy for the students to get a body to dissect at Oxford, for the mob being so mutinous to prevent their having one (Hurren, 2008).
Eighteenth century anatomy wore public and private faces. It had a dark side: many anatomists and surgeons were dependent upon and complicit in criminal activity to obtain cadavers for dissection. It was also a time when training in anatomy became a sine qua non for a career as a professional surgeon; when remarkable wax anatomical models were produced in Italy and spread throughout Europe (Ballestriero 2010); when the importance of anatomy in midwifery and pathology (the idea that diseases were anatomically based) was increasingly appreciated; and when the accuracy (greater visual truth) of published anatomical drawings was enhanced by techniques such as the camera obscura, used by Chesleden in Osteographia (Neher, 2010), and squares and diopters, used by Albinus in Tabulae sceleti et musculorum (Huisman, 1992). Despite the macabre undertones, the Enlightenment was a time when the discipline of anatomy flourished as never before (Cunningham, 2010).
Public anatomy, ‘entrepreneurial’ anatomy, was offered to a predominantly non‐medical, well‐educated audience who paid to be instructed but also entertained at a single event or a series of lectures delivered over days or weeks: in the age of Enlightenment, some familiarity with anatomy was considered essential in a liberal education. Public anatomists …aimed to entertain, to enlighten, to bedazzle, and to offer moral edification (Guerrini, 2004). The lectures, in commercial or domestic settings, were delivered by practising surgeons, who probably also worked in the growing number of private anatomy schools or local charitable hospitals (Billing, 2004). As the institutions and the entrepreneurs both needed a regular supply of corpses, their relationship was often fraught. The young William Chesleden, a member of the Company of Barber Surgeons, who would later become the leading surgeon in England, challenged the Company's right to control dissection in London by giving 35 lectures on the ‘anatomic parts of the human body’ at his house in Cheapside in 1713–1714 without permission. These lectures formed the basis of The Anatomy of the Humane Body, which ran to 15 editions in English and one in German; three editions were published in America (1795, 1796 and 1806). The Barber Surgeons censured Chesleden for his ‘ill practices’ and ordered him not to hold his demonstrations at the same time as the Company held its lectures in the Company's Hall (Sanders, 1999). Some 35 years later, Chesleden wrote witheringly about this censure: … And the rulers of the barber surgeons company at the same time contrived a by‐law to prevent the knowledge of anatomy from spreading: cunningly forseeing that the younger surgeons, by that knowledge, would advance too fast upon them. They made it a penalty of ten pounds to dissect a body out of the hall without their leave, which was scarce to be obtained, and if anyone offended (as they called it) they were sure to be prosecuted. The improvements in anatomy and surgery, since these restraints have been removed, will sufficiently convince the world of the unfitness of them… (Gelfand, 1972).
Public demonstrations usually included elements of comparative anatomy and animal vivisection as well as human cadaveric anatomy, a format that would have been familiar to Renaissance audiences. As well as the opportunity to see a ‘fresh’ human cadaver, audiences might be able to handle permanent, dried anatomical preparations in which vessels had occasionally been enhanced by injections of coloured wax or mercury. Animals, particularly dogs, were cheap and accessible and could be opened while still alive to demonstrate ‘function’. An advertisement for Chesleden's new course, posted in 1721 in the Daily Courant, gives a flavour of what contemporary audiences might expect to receive for their money: A course of Anatomy: In which will be shewn all the known Mechanisms of the Human Body; together with the Comparative Anatomy of Birds, Beasts and Fishes … The whole to be illustrated by Mechanical Experiments, there being a new Apparatus made for this Purpose. To be performed by William Chesleden, F.R.S and Fra. Hucaksbee, at his house in Crane‐Court, Fleet‐Street, where Subscriptions are taken in… (Guerrini, 2004). Chesleden subsequently played a leading role in the disjoinder of the Barber Surgeons and the Company of Surgeons (later to become the Royal College of Surgeons); his stance was possibly coloured by his earlier dispute with the Barbers. The Act of Separation received the Royal Assent on 2 May 1745, ending the Barber‐Surgeons’ near monopoly on the legal use of corpses in anatomical teaching.
The next year, in September 1746, William Hunter, anatomist, midwife and surgeon, advertised a course of anatomical lectures with the additional, and novel, opportunity to learn the art of dissection …in the same manner as at Paris. Hunter had studied in Paris, where he had seen that students actively participated in dissection, and he recognised that young surgical apprentices in England also needed to acquire hands‐on experience of anatomy through cadaveric dissection before operating on their patients. The demand for cadavers increased further as more students took Hunter's courses, from 20 students in 1748 to 100 in 1756, and as other private medical and anatomy schools followed the market trend and offered the opportunity to dissect to their students. The fact that the London anatomists of the mid‐1740s styled their teaching as being ‘Parisian’ or ‘French’ indicates the degree to which London teaching was perceived – rightly or wrongly – as indebted to pre‐existing continental practices… (Chaplin, 2009). By 1760, it was the norm that students dissected for themselves in private anatomy schools. There was no state‐regulated training for medical practice in 18th century England, but applicants for licences to practise from the College of Surgeons were obliged to attend two full courses of anatomy and these included dissection.
Resurrectionists and the first Anatomy Act, 1832
The Murder Act was enacted in 1752 and mandated the dissection or gibbeting of a murderer's body after execution …for better preventing the horrid crime of murder that some further terror … be added to the punishment… (‘Dissection’ in this context usually meant that a small incision was made in the skin of the chest or upper arm of the corpse at the place of execution, and the body was then dispatched to be dissected ‘properly’ elsewhere). From 1752 until 1800, the bodies of some 80 criminals convicted under the Murder Act of 1752 and executed in the cities of London and Westminster were delivered to the Surgeons’ Hall at the Old Bailey: the bodies were ‘dissected and anatomized’ and their bodies exposed to the public (Chaplin, 2009).
The number of executed criminals actually declined in the 18th century (Mitchell et al. 2011). Market forces inevitably commodified the corpses of the disenfranchised poor (Richardson, 2001) and a nefarious, highly lucrative, trade in supplying bodies and body parts to anatomists and surgeons burgeoned. Medical students who had flouted the law to obtain material for their personal study were now replaced by Resurrectionists (Cole, 1964) or ‘sack‐em‐up men’, gangs of grave robbers who earned more in a night's work selling freshly exhumed corpses and body parts to anatomists and surgeons than law abiding citizens might earn in many months. They operated in the form of unlicensed guilds in London, Edinburgh, Glasgow and Dublin, each gang having an extensive territorial ‘reach’: in Lambeth in 1795, a professional gang of 15, working only in the winter, could supply eight surgeons of repute from 30 burial grounds (churchyards, private cemeteries and public burial fields, particularly the paupers’ grounds on the outskirts of London). Corpses might also be sold by or stolen from undertakers, asylum‐keepers, workhouse superintendents or hospital porters. No corpse was immune from being plucked from its coffin and shroud under cover of darkness unless stringent measures were taken to deter the thieves. Sir Astley Cooper remarked in 1828 that … There was no man in England whatever might be his rank or consequence whose body he could not obtain after his death if he had a mind to dissect it… (Anonymous 1829). In 1795, a child's body cost 6 shillings for the first foot (0.3 m) and 9 pence for each extra inch (25 mm). Within 25 years, the cost of a standard corpse had risen ten times; ‘freaks’ cost considerably more (Magee, 2001).
Public outrage at the activity of the Resurrectionists and especially the behaviour of Burke and Hare, two Irishmen who murdered 16 victims and sold their bodies for dissection to the Medical School in Edinburgh, coupled with revulsion at the anatomisation of executed felons, often erupted into disturbances of the peace. When a dog unearthed human remains in the grounds of an anatomy school in Aberdeen, the building was set on fire by an angry mob (estimated to be some 20 000 strong). The attending fire engine was denied access to the site and it was deemed advisable that a party of soldiers who had been marched out from the nearby 79th Regiment to put down the riot should not interfere (The Sydney Monitor NSW, 1828–1838).
London‐based Resurrectionists sometimes shipped bodies out of London. In 1826, three casks were found on Georges’ Dock, Liverpool, labelled ‘Bitter Salts,’ which were consigned for shipment to Edinburgh. They remained there overnight and the following morning, the stench attracted attention. The police … found eleven dead bodies contained therein, salted and pickled (Lassek, 1958). Mindful of the twin needs of maintaining public order and establishing whether continued cadaveric dissection was justified for medical education and research, a Parliamentary Select Committee on Anatomy was convened in 1828 following representations by medical luminaries such as John Abernethy, Charles Bell, Everard and Benjamin Home, Benjamin Brodie and Astley Cooper. It is instructive to read the robust responses of Sir Astley Cooper (a regular employer of Resurrectionists) to two questions asked of him when he appeared before the Committee. Q. Can the young practitioner be expected to possess the necessary courage in performing a difficult operation on the living if he has not already been taught to perform a similar operation upon a dead body? A. He must be a blockhead if he made the attempt; and the practice of the most sensible and most expert surgeons in London has been to visit the receptacles for the dead, for the purposes of performing the operations which they were about to execute upon the living, if the operations were in the least novel. Q. Can a student know where to cut with freedom, when with caution, and when not at all, if he has not an intimate knowledge of every part of the human body? A. I would not remain in a room with a man who attempted to perform an operation in surgery, who was unacquainted with anatomy, unless he would be directed by others; he must mangle the living, if he has not operated on the dead (Lancet, 1827–1828, volume II, page 75).
The chairman of the Parliamentary Select Committee, Henry Warburton, drafted a staunchly Benthamite report, which he presented to the House of Commons on 22 July 1828. The statistics revealed that at least 800 students were attending 12 anatomy schools in London at the time [eight independent (private) schools and four hospital‐based schools]. Five hundred students were dissecting 475 bodies, most of which were acquired illegally. The Committee credited William Hunter with …opening a regular school for dissection… (Gelfand, 1972). Warburton obtained leave to bring in his Anatomy Bill in 1829, arguing that, despite the public distaste for the use of the corpses of paupers for dissection, there was no other way to advance the vitally important medical science of anatomy: the Bill was defeated in the House of Lords. He reintroduced a simplified bill, entitled ‘A Bill for Regulating Schools of Anatomy’ in December 1831. After robust opposition, the Bill passed through Parliament and was eventually given Royal Assent on 1st August 1832 (Farrell, 2009). In essence, the Act allowed medical schools to accept an unclaimed corpse from the mortuaries of a workhouse or a charitable hospital if the deceased had not formally registered their dissent to being dissected and if their body had not been claimed for burial by relatives within 48 h. It repealed the law that the bodies of executed murderers should be dissected and created a supervisory board of inspectors (Anonymous, 1832). Significantly, the Act did not concern itself with incomplete bodies, which meant that medical schools did not need to account to the newly constituted Anatomy Inspectorate for body parts that had been procured by ‘undocumented’ means (MacDonald, 2009).
Anatomists were apparently enthusiastic … The most opportune occurrence for medical science in this country is the passing of the anatomical act. It is a lever of which we can scarcely estimate the power… (Anonymous, 1833). Elsewhere, there was less optimism. Once anatomy laws allowed for the use of unclaimed bodies, cadavers were less illicit but still in the category of found objects, unclaimed, somehow less than human (Dyer & Thorndike, 2000). Despite Warburton's good intentions, not only did the Act not solve the problem of the inadequacy of the supply of cadavers, it helped to turn the Victorian workhouse into a feared and hated institution: bodies were still diverted from the workhouse to the dissecting table (Mitchell et al. 2011; Ghosh, 2015). The exponential growth of burial insurance in the early nineteenth century, and its cultural importance in poor communities until well into the second half of the twentieth century reflect the very long‐term impact of the anatomy legislation… (Richardson, 2008). Plus ça change: apparently bequeathal is again seen as a way of defraying the burden of funeral costs … It is important that bequeathal is not viewed as an option to address funeral poverty although for some individuals it is unquestionably used in this manner (Professor Sue Black, Dundee, quoted in the Daily Telegraph, 8 January 2016). (For further reading about the consequences of the Anatomy Act, Poor Law Amendment Act and Medical Act, see Richardson, 2001; Hurren, 2012).
Private anatomy schools
Approximately 60 practitioners, mostly surgeons, advertised private courses of lectures in anatomy, surgery or midwifery in London in the latter half of the 18th century: most worked from private premises for personal profit (Chaplin, 2008; citing Lawrence, 1996). Independent anatomy schools in London and elsewhere still flourished in the early years of the 19th century and were often close to the great hospitals. In 1826, the larger private schools included Grainger's school in Webb Street near St Thomas's and Guy's, Terrel's School in Aldersgate near St Bartholomew's, and Hunter's school in Great Windmill Street near the Middlesex. Joshua Brooke's school in Great Marlborough Street was particularly popular because it was open all year round: he had been one of the pioneers of an early form of embalming, using his own secret formulation to enable dissection to continue in the summer as well as during the cold winter months. However, by 1871 almost all the private schools had disappeared: the last was probably Cooke's London School of Anatomy in Handel Street (then called Henrietta Street), Brunswick Square, which opened in 1870 and closed in the early part of the 20th century (Morton, 1991). The schools sold their collections of specimens to the interested general public and to the new medical schools that opened in London, where they formed the nuclei of teaching collections: the specimens were the products of a ‘profession’ that was, by the standards of the time, far from genteel (Chaplin, 2008). One of the most famous Enlightenment collections of anatomical specimens had been amassed by John Hunter, William Hunter's more famous younger brother, who is often referred to as the ‘father of scientific surgery’ (Ellis,2001). When he died in 1793, his extraordinary collection was thought to contain over 17 000 objects, including preparations of human and animal anatomy and pathology, collections of fossils, shells and other objects of natural history, paintings, prints and drawings. It was purchased posthumously by Act of Parliament in 1799, and ultimately placed into the care of the Company (later the Royal College) of Surgeons in London. Bombing in World War II not only claimed the Vesalian woodcuts in Munich, it also depleted the greater part of John Hunter's collection when the Royal College of Surgeons sustained severe bomb damage on the night of 10 May 1941. (Discussion of the development of anatomy museums in England and elsewhere, with themes of public accessibility and utility; and of the methods of preserving, collecting and displaying dissected body parts in those museums, is beyond the remit of this review: for further reading, see Bates, 2008; Chaplin, 2008; Mitchell, 2012; Alberti & Hallam, 2013).
In 1858, the Medical Act changed the relationship between state, public and medical practitioners in England. The Act was designed to regulate the qualifications of practitioners in medicine and surgery: henceforth qualified practitioners would be registered by the General Council of Medical Education and Registration of the United Kingdom (General Medical Council, GMC). As medical education became university‐based within Medical Schools, cadaveric dissection disappeared from the public gaze behind the closed doors of purpose‐built dissecting rooms.
Anatomy text books in English—catching up with Europe in the 18th century
David Edwarde's De indiciis et praecognitionibus (1532) is thought to contain the first printed references to anatomical dissection (of the abdominal viscera) to be published by an English author in England. The Anatomie of the Bodie of Man, attributed to Thomas Vicary, but published many years after his death by the surgeons at St Bartholomew's Hospital (1577), is often described as the first English anatomy book, but is mostly a shortened version of a 14th century manuscript (Thomas, 2006). Ten editions bearing Vicary's name were published over the next hundred years: the pre‐Vesalian anatomy it contained did not change in all that time! Of the nine anatomy books published in England between 1500 and 1600, only four were written by native authors (Furdell, 2002). Helikah Crooke's Microcosmographia (1615) was probably the first since John Banester's Historie of Man (1578) and drew heavily on the writing and illustrations of European anatomists, being …collected and translated out of all the best authors of anatomy….
Most anatomy textbooks were imported from France and Italy until the beginning of the 19th century, when Jones Quain's Elements of Descriptive and Practical Anatomy, first published in 1828, quickly became the standard work for English‐speaking students. The literary reviews of Quain and of Grainger's notes and Knox's translation of Cloquet, all contain criticisms of the state of anatomical instruction in England at the start of the 19th century and lament the lack of contemporary anatomical texts in English …hitherto our students have generally been driven to … having to search the systems of France and Germany for instruction which they ought to have found at home (Anonymous, 1830). However, a palpable change was in the air and it seemed that at last English anatomy was about to catch up with the rest of Europe …a new era is dawning in medical education in this country. Within these few years a revolution has taken place in our schools… It is especially in the teaching of anatomy that we anticipate great changes… Anatomy will be taught from the body and the profession will no longer be scandalised by seeing crowds of young men just learn enough from plates and the diagram board, to get through the examination of the College of Surgeons (Anonymous, 1833). In 1858, Henry Gray and Henry vanDyke Carter published Gray's Anatomy. Gray's preface to the first edition caught the essence of the new thinking, emphasising that, for medical practitioners, anatomy was a science with a clinical application … This Work is intended to furnish the Student and Practitioner with an accurate view of the Anatomy of the Human Body, and more especially the application of this science to Practical Surgery (Gray 1858). In the latter part of the 19th century, as developments in antisepsis (Lister, 1867), anaesthesia (1846) (Robinson & Toledo, 2012) and haemostasis ushered in the previously unimaginable prospect of pain‐free, elective surgery, and successful operations reflected a surgeon's skill rather than his speed, the importance of anatomical knowledge in minimising intra‐operative iatrogenic injuries became a reality: … In order that the observer, by examining [the drawings], may avoid mistakes on the living body… The exact position and relations of the structures which must be divided or avoided in the course of an operation are indicated… (Braune, 1877). This self‐evident truth had been expressed by almost every author of an anatomical text since the ancient Greeks, but until now opportunities for its enactment had been relatively limited.
The transparent body—‘outside‐in’ becomes ‘inside‐out’
For centuries, anatomists and surgeons approached the interior of the body from the outside; the only way to see under the skin was to incise it and develop and reflect the flaps so created. That started to change in the late 19th century, as technological innovations rendered visible the previously invisible (van Dijck, 2005), stimulating anatomical research and radically altering clinical practice. Thomas Edison's invention of a long‐lasting incandescent lamp (1879) solved a problem that had confounded all previous attempts to shine a light into dark spaces and Wilhelm Röntgen devised a way of seeing beneath the skin. Three‐dimensional anatomical knowledge was essential for interpreting the new views of the body revealed by endoscopes, X‐rays, computed tomography (CT), magnetic resonance imaging (MRI) and ultrasound. Although topographical anatomy had not suddenly altered, the new ‘inside‐out perspective’ meant that anatomists and clinicians had to re‐interpret an internal landscape with which they had thought they were familiar. By the end of the 20th century, the old adage ‘big surgeon, big incision’ had lost its currency: in the future, the small incisions of multiple portal laparoscopic surgery may be replaced by single incision laparoscopic surgery (SILS) and in some cases by natural orifice transluminal endoscopic surgery (NOTES), which leaves no external scar (Moris et al. 2012; Antoniou et al. 2015; Porzionato et al. 2015).
Endoscopy
Using natural orifices to look inside the body was never going to be easy in the pre‐technological era. Overcoming the obstacles that anatomy places in the way of rigid or flexible tubes without damaging surrounding tissues, and devising means of safely illuminating dark internal spaces and reflecting a clear, magnified image of the target structure back to the observer's eye proved daunting tasks. Hippocrates described using a speculum to examine the rectum; Eristratus used ‘catheters’ with the correct anatomical curvature; Avicenna stood behind his patients and used reflected sunlight and polished glass mirrors to examine the vulva; Albukasim (Albukasis, 936–1013 CE) is credited with inventing devices to examine the ear and urethra, and to remove foreign bodies from the throat. Little more happened over the next 800 years, although ingenious ways of using sunlight were occasionally reported, for example, Giulio Aranzio's use of a hole in a closed wooden window shutter to direct sunbeams exclusively into his patient's nasal cavity while removing nasal polyps (Gurunluoglu et al. 2011). Archibald Cleland (1729) used biconvex lenses placed in front of a wax candle to magnify and redirect the light in order to examine the nasal cavity. Samuel Vogel (1780s) obtained what is thought to be the first view of the eardrum in a living patient using a small plane mirror to reflect sunlight into the external acoustic meatus. Philip Bozzini (1806), often called the father of modern endoscopy, is credited with solving the problem of reflecting images back to the eye using his Lichtleiter, an instrument in which concave mirrors reflected candlelight from a candle inside a metal chimney through an open tube via variously shaped attachments into the oesophagus, bladder or rectum (Bush et al. 1974). His invention was dismissed as a ‘mere toy’ by the Vienna Medical Faculty (Morgenstern, 2005) but not by others, who recognised the potential of his design.
The introduction of electric technology was a game changer. There have been many ‘firsts’ in the post‐Edison era, in terms of instrumentation and surgical approach, including the development of the first gastroscope by Mikulicz‐Radecki (1880) and Howard Kelly's first use of a rigid sigmoidoscope (1895); the first attempt to examine the peritoneal cavity endoscopically by ‘celioscopy’ (1901); the first use of an endoscope in the cerebellopontine angle for a trigeminal neurectomy via a retrosigmoid craniotomy (Doyen, 1917); the first use of fibre optic endoscopy (1954); the first laparoscopic appendicectomy (1982) and the first laparoscopic cholecystectomy (1987) (Spaner & Warnock, 1997; Vilardell, 2005). Equally important were the numerous cadaveric dissection studies designed to identify and evaluate the key anatomical landmarks, anatomical ‘safe zones’ and danger spots to be encountered or avoided during endoscopic and laparoscopic procedures (e.g. Tanriover et al. 2004; Campero et al. 2006; Shimizu et al. 2006; Iaconetta et al. 2007; Apaydin et al. 2010; Ignjatovic et al. 2010; Hosemann & Draf, 2013; Hosemann & Schroeder, 2015; Weber & Hosemann, 2015). Structures previously considered ‘small print’, such as the vidian artery (Kassam et al. 2008) or the anterior fornix (Venkataramana et al. 2009), became microsurgical landmarks. In describing transnasal endoscopic surgical approaches to the clivus (an approach that would have been unthinkable a few decades ago) Stamm et al. comment that …success of this type of surgery depends on perfect knowledge of the anatomy [and] intense endoscopic surgery training… (Stamm et al. 2006). Applications were not exclusively clinical: endoscopic and videofluoroscopic evaluation of normal subjects has increased understanding of the anatomical bases of activities such as swallowing (Curtis et al. 2015) and phonation.
Imaging—are radiologists the contemporary anatomists?
The noise of war's alarm should not distract attention from the marvellous triumph of science which is reported from Vienna … Professor Routgen [sic] … has discovered a light which for the purpose of photography will penetrate wood, flesh, cloth, and most other organic substances. The Professor has succeeded in photographing … a man's hand which showed only the bones, the flesh being invisible. This news, cabled from the London Standard on 6 January 1896, appears to be the first account in English of Wilhelm Röntgen's momentous discovery of X‐rays some months earlier in November 1985, for which he was awarded the first Nobel Prize in 1901 (Glasser, 1995). The clinical potential of X‐rays to look inside the body was recognised very quickly, as this quote from the New York Sun makes clear … Never in the history of science has a great discovery received such prompt recognition and has been so quickly utilized in a practical way as the new photography which Professor Roentgen gave to the world only three weeks ago. Already it has been used successfully by European surgeons in locating bullets and other foreign substances in human hands, arms and legs and in diagnosing diseases of the bones in various parts of the body… (Spiegel, 1995). Techniques exploiting X‐rays during the first half of the 20th century included fluoroscopy, mammography, angiography (the use of intravenous contrast media recalling much earlier cadaveric studies using warmed wax and coloured liquids to explore vascular anatomy), urography and nuclear medicine (Bradley, 2008). Interpreting the images produced by each new protocol required a thorough knowledge of cadaveric anatomy and surface (living) anatomy. In the early 1970s, CT scanning and MRI revealed levels of anatomical detail acquired non‐invasively that had previously been seen only on the pages of atlases of frozen, sectioned cadavers (Braune, 1867–1872, 1877; Lichterman, 2008). Today, those details can be inspected in varying projections in multiplanar reformations (MPRs), maximum intensity projections (MIP), and volume‐rendered images acquired from multidetector CT (MDCT) scans (e.g. Ramachandran et al. 2009; Sussmann & Ko, 2010; Ugurel et al. 2010). Interpretation of these images requires sound anatomical knowledge: As radiology becomes ever more central to clinical pathways and clinical decision‐making, an understanding of radiological and cross‐sectional anatomy is essential to the doctors of tomorrow (Pathiraja et al. 2014).
During the 1960s, ultrasound evolved from being a …medical curiosity to a recognized clinical procedure, capable of providing unique diagnostic information (Goldberg et al. 1993). Today, ultrasound is one of the most widely used modalities in medical imaging, providing high resolution images of dynamic anatomy in real time in cardiology, gynaecology, gastroenterology, etc. In obstetrics, routine 3D‐US scanning at 18–20 weeks (obstetric staging) is used to confirm the delivery date, assess the position of the placenta and evaluate selected fetal anatomical landmarks in order to detect the presence of fetal anomalies such as myelomeningocele and orofacial clefts (Sepulveda et al. 2012). The use of non‐diagnostic ultrasound imaging in guiding interventional procedures such as regional nerve blocks, central venous catheterisation, and cutting‐needle and fine needle aspiration biopsies, has significantly reduced the risk of iatrogenic injury (e.g. Shah et al. 2013). As with the other imaging modalities, an understanding of detailed three‐dimensional anatomy is essential for interpretation of the images on the screen.
Modern imaging has played a major role in deepening our understanding of the structure and function of the brain, enabling the detection of pathological abnormalities and significantly enhancing neurosurgical practice. There have been surprises: functional MRI revealed the default mode network, a previously unsuspected system active in the supposedly ‘resting’ brain but deactivated whenever conscious attention to a task is required (Raichle & Snyder, 2007; Griffiths, 2015; Sandrone, 2016). The brain is invisible in an X‐ray image of the head, whereas MRI reveals its structure with a detail commensurate with that seen in a freshly sectioned postmortem brain. Additional techniques, such as MR angiography, including ‘time of flight’ MRI; functional MRI, including BOLD (blood oxygen level dependent) imaging; and diffusion tensor imaging (DTI), all extend the range and nature of the information that can be acquired from MR‐based datasets and complement morphological and physiological studies. Interpreting and validating these images introduced the work of Josef Klingler to a new audience and reinforced the importance of remaining grounded in ‘real’ anatomy. Klingler's dissections of the brain, undertaken in the 1930s and 1940s, became …the basis for the anatomic maps underpinning stereotactic neurosurgery and profoundly influenced the correlation of neurological function and anatomy to neurosurgery (Klingler, 1935; Agrawal et al. 2011). Although DTI‐based tractography considers a single direction of diffusion per voxel and therefore likely oversimplifies tract anatomy (Zemmoura et al. 2014), images from DTI‐based tractography (effectively proxies for white matter tracts in vivo), reciprocally enhance dissections of the same tracts prepared according to Klingler's protocol (Ludwig & Klingler, 1956), …fiber‐dissection and diffusion‐tensor magnetic resonance imaging techniques are reciprocally enriched not only in their application to the study of the complex intrinsic architecture of the brain, but also in their practical use for diagnosis and surgical planning (Fernández‐Miranda et al. 2008).
The 21st century dissecting room—same locus, different focus
Medical students in the 21st century may learn topographical anatomy using prosected ‘wet’ specimens, plastinated specimens or plastic specimens: unlike their counterparts of a century ago, they may never see the inside of a dissecting room; indeed, where their Medical Dean believes that …teaching by dissection is an old‐fashioned, traditional technique inappropriate for today's generation of students (Moxham & Plaisant, 2014), their medical school may no longer possess such a facility. That said, and despite the universally diminished presence of topographical anatomy in undergraduate curricula (Drake et al. 2009), many other students are still required to dissect all or part of a body and increasingly may also practise clinical procedures on the cadavers they dissect (e.g. Nutt et al. 2012; Benninger et al. 2104). Embalming protocols have changed to meet the needs of the end‐users. Cadavers used for student dissection are still more likely to be embalmed in formaldehyde or phenol, but those used for clinical workshops, biomechanical investigations or surgical training (for example to study ultrasound‐guided regional anaesthesia, Kessler et al. 2014), are now usually either ‘soft’, Thiel‐embalmed (Balta et al. 2015; Hammer et al. 2015; Healy et al. 2015) or unembalmed, frozen‐thawed (e.g. Mitchell et al. 2012), to better simulate the visual and haptic properties of living tissues. Cadaveric dissection is always an educational, evidence‐based experience, but a cadaver is not ‘simply’ an extraordinarily valuable teaching resource. Cadaveric anatomical research continues to change clinical practice, exemplified for example by the impact of the demonstrations of bronchopulmonary segmentation on thoracic surgery and of intrahepatic portal venous anatomy on liver surgery; the concept of the angiosome on optimal flap design in reconstructive surgery …the single greatest anatomical advance over the past 100 years (Eizenberg, 2015); and the importance of a detailed knowledge of sulcal anatomy in neurosurgery. Surgical problems are often the impetus for cadaveric dissection studies, stimulating what Shane Tubbs has termed ‘reverse translational research in anatomy’ (i.e. from the bed to the bench and back) (Tubbs, 2016).
Bronchopulmonary segments
The anatomy of the bronchial tree had been explored using ‘wax corrosion’ casts and wax‐injected dried dissections by Swammerdam in the 17th century, and using metal casts by Bidloo in the 18th century: no functional significance had been attached to the arrangement of the bronchi seen in these studies beyond their obvious role as conduits. The modern concept of segmental anatomy is attributed to William Ewart (1848–1929) a pathologist at the Brompton Hospital in London, who is generally regarded as the ‘father of segmental anatomy’. Ewart believed that the …present deficiencies in our anatomical knowledge… probably contributed to the slow progress in pulmonary surgery (Ewart, 1889). From an analysis of corrosion casts of lungs prepared using a low melting point alloy, he proposed that the lung consisted of anatomically and functionally separate components which he called ‘respiratory units’. These were subsequently renamed as ‘bronchopulmonary segments’ (Kramer & Glass, 1932). The successful surgical resection of individual segments (Churchill and Belsey, 1939), heralded …a new era of thoracic surgery … ushered in by developments in anatomy (Tompsett, 1965). Understanding and interpreting the three‐dimensional anatomy of the respiratory tree soon became integral to clinical management of pulmonary disease: …the technically perfect film and the brilliant bronchoscopic field are of little avail if there is uncertainty in the conception of the anatomy of the bronchial tree (Neil et al. 1939).
Functional hepatic segments
The modern concept of segmental liver anatomy was initially developed by Claude Couinaud. Using detailed dissection studies and analyses of corrosion casts of explanted livers, he divided the liver into eight functional segments based on the distribution of the intrahepatic branches of the portal vein (Couinaud, 1957; Sutherland & Harris, 2002; Bismuth, 2013). His descriptions, although since modified (Lodge, 2016), formed the basis for subsequent advances in surgical techniques and interventional and diagnostic imaging: the complexity of hepatic interventions now performed underlines the importance of recognising and understanding normal, frequently variant, portal vein anatomy (Schmidt et al. 2008; Ugurel et al. 2010).
Angiosome concept
Seven years before Röntgen's momentous announcement, Carl Manchot had published Die Hautarterien des menschlichen Körpers (Manchot, 1889). Using a recipe that has long since been lost, he had injected and dissected the arterial system in numerous cadavers, describing the cutaneous perforators and their source vessels in 40 different cutaneous vascular territories, excluding the head, neck, hands and feet (Fig. 8). In so doing, he laid the foundation for what would become a revolution in skin flap design and vascularised tissue transfer almost a century later. His work was extended by Michel Salmon's (1936) radiographic studies of cadavers injected with a mixture containing lead oxide. Both of these meticulous anatomical studies remained largely unknown to the English‐speaking world for decades.
Figure 8.
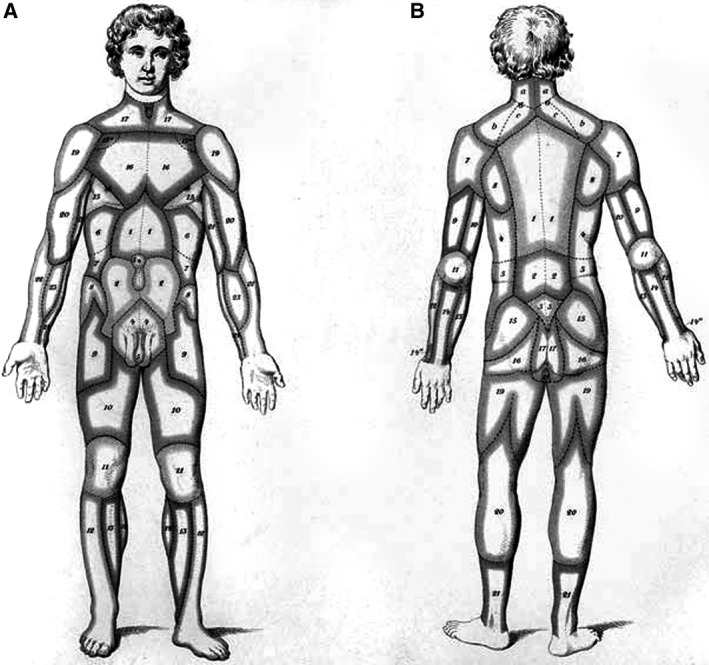
Carl Manchot's vascular territories of the human integument (From Manchot C. Die Hautarterien des menschlichen Körpers. Leipzig: FCW Vogel; 1889). (A) Cutaneous vascular territories, ventral surface. (B) Cutaneous vascular territories, dorsal surface. Reproduced with permission from: Morris SF, Taylor GI (2012). Vascular territories. In: Plastic Surgery (ed. Neligan PC). Volume 1. Principles. Chapter 23, pp. 479–511. Saunders.
An ‘anatomic revolution’ in reconstructive surgery began in the 1970s (Morris & Taylor, 2012). It had become clear that flap survival depended on a precise knowledge of the vascular supply of the donor tissue being transferred to a host site, whether the flap was based on a known axial blood supply or on random vessels. In the search for new donor sites for tissue transfer, surgeons returned to the dissection room (Morris & Taylor, 2012). Fast forward to 1987, and a landmark paper by Ian Taylor and John Palmer introduced the angiosome, an anatomical concept with clinical implications (Taylor & Palmer, 1987). On the basis of ink injection studies, dissection, perforator mapping and radiographic analyses of fresh cadavers and isolated limbs, Taylor's group conceptualised angiosomes as three‐dimensional vascular territories (consisting of skin, subcutaneous tissue, fascia, muscle, tendon and bone) fed by a source artery and drained by specific veins (Fig. 9). The principles of three‐dimensional vascular anatomy revealed by their meticulous studies determine the choice of appropriate perforator flap, whether musculocutaneous (indirect) or septocutaneous (direct), used to reconstruct soft tissue defects (see Inoue & Taylor, 1996; Houseman et al. 2000; Taylor et al. 2011, 2012; Griffin et al. 2014; Jordan et al. 2014).
Figure 9.
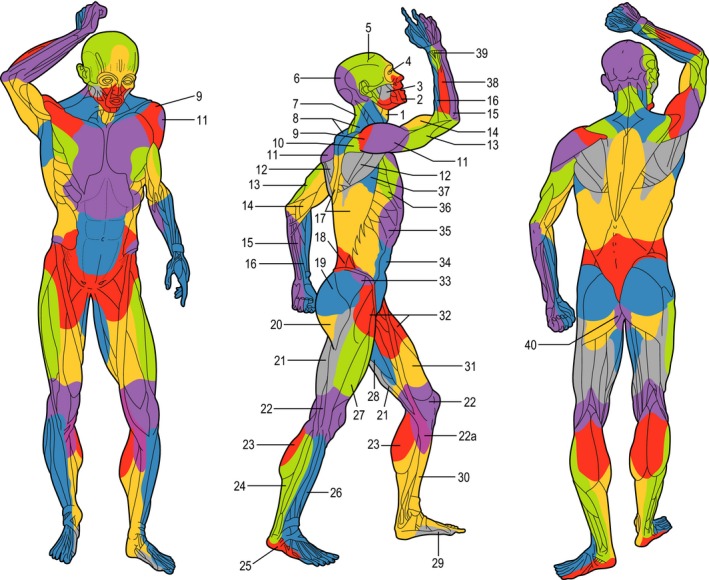
The angiosomes of the source arteries of the body. The angiosomes are: (1) thyroid; (2) facial; (3) buccal (internal maxillary); (4) ophthalmic; (5) superficial temporal; (6) occipital; (7) deep cervical; (8) transverse cervical; (9) acromiothoracic; (10) suprascapular; (11) posterior circumflex humeral; (12) circumflex scapular; (13) profunda brachii; (14) brachial; (15) ulnar; (16) radial; (17) posterior intercostals; (18) lumbar; (19) superior gluteal; (20) inferior gluteal; (21) profunda femoris; (22) popliteal; (22a) descending genicular (saphenous); (23) sural; (24) peroneal; (25) lateral plantar; (26) anterior tibial; (27) lateral femoral circumflex; (28) adductor (profunda); (29) medial plantar; (30) posterior tibial; (31) superficial femoral; (32) common femoral; (33) deep circumflex iliac; (34) deep inferior epigastric; (35) internal thoracic; (36) lateral thoracic; (37) thoracodorsal; (38) posterior interosseous; (39) anterior interosseous; and (40) internal pudendal. Reproduced with permission from: Morris SF, Taylor GI (2012). Vascular territories. In: Plastic Surgery (ed. Neligan PC). Volume 1. Principles. Chapter 23, pp. 479–511. Saunders.
Trans‐sulcal approaches in neurosurgery
The gyri and sulci of the cerebral cortex were initially described as looking like ripples of smelted copper in the Edwin Smith papyrus, or like loops of small bowel by anatomists such as Galen, Vesalius and Casserius. Relatively little importance was attributed to the cerebral cortex, which was regarded as a mere ‘mantle’ that protected the more important internal white matter and ventricles. The realisation that the major convolutions, fissures and sulci that contour the cortical surface were not randomly distributed is a relatively new concept.
Charles d'Estienne illustrated the cerebellar folia as a series of irregular fine lines, and in so doing pictorially differentiated the cerebellum from an almost featureless cerebral cortex, in a figure in De dissectione partium corporis humani libri tres (a book completed in 1539 but not published until 1545) (Rifkin et al. 2011). Franciscus de la Böe Sylvius, working in Leyden in the mid‐17th century, described for the first time a deep lateral fissure that …divides the cerebrum into an upper, larger part and a lower, smaller part (Sylvius, 1663). However, it was not until the 19th century that the reasonably consistent arrangement of the main gyri and sulci was appreciated, independently, by Luigi Rolando, Achille Louis Foville and Louis Pierre Gratiolet. Rolando described the cerebral convolutions, which he considered could be …reduced to regular and specific shapes and positions…, including the central sulcus (fissure of Rolando) in Della Strutura degli Emisferi Cerebrali (1829) (apparently the central fissure had been noted earlier by the Danish anatomist Casper Bartholin (1585–1629), but the eponym was awarded to Rolando). Foville's detailed atlas of the anatomy of the central nervous system was illustrated with dissections produced using a technique that he had learned in Gall's laboratory (Foville, 1844): the book represents …one of the greatest efforts up to that time of providing the basis for mastering the anatomical substrate of mental functions and neurological and psychiatric disorder… (Brogna et al. & Fiengo, 2012) (Fig. 10). It was published 10 years before Gratiolet's (1854) detailed study of the brains of human and nonhuman primates in which he adopted Arnold's suggested division of each cerebral hemisphere into five lobes (frontal, parietal, occipital, temporal, insular); provided the first accurate descriptions of the cerebral lobes and cerebral fissures; and introduced the term plis de passage for the connections between adjacent gyri (Parent, 2014). Within 50 years, the physical map of the cortical surface had been joined by cytoarchitectonic and myeloarchitectonic maps of cortical architecture and connectivity, published by Campbell, Brodmann and others (Campbell, 1905; Eadie, 2003; Zilles & Amunts, 2010; Loukas et al. 2011; Macmillan, 2014). Some of these topographical maps sought to correlate cortical areas with specific functions: contrary to popular opinion, Korbinian Brodmann, whose map is probably the most famous of all of the cortical maps produced in the first half of the 20th century, was careful to point out that his …studies of localization are based on purely anatomic considerations and were initially conceived to resolve only anatomic problems (Garey, 1999).
Figure 10.
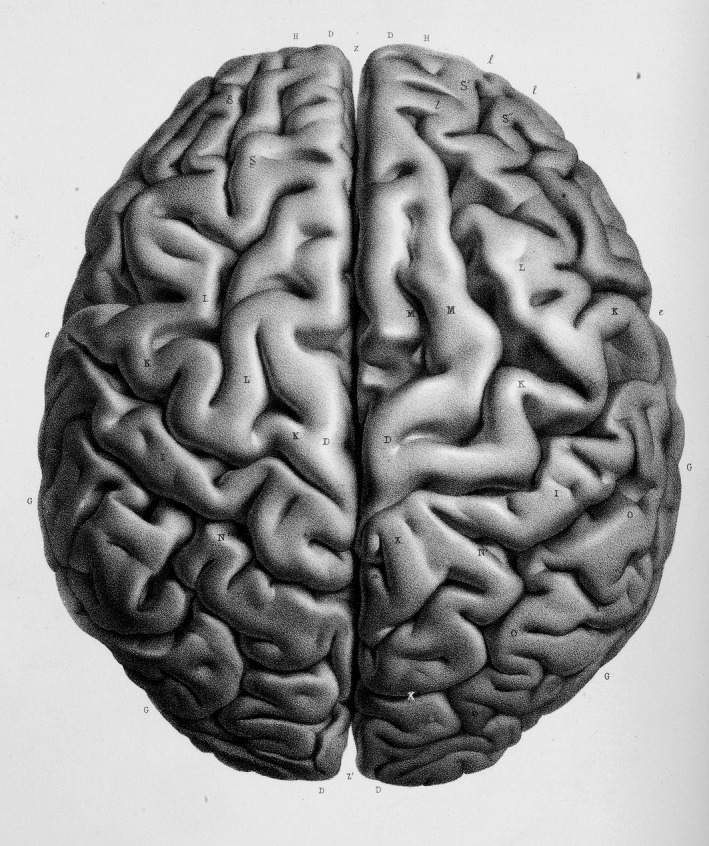
Superior view of the cerebral hemispheres with an accurate representation of the gyri and sulci, including variations in the precentral and postcentral gyri. Plate 11 in A.L Foville's Atlas published with Traité complet de l'anatomie, de la physiologie et de la pathologie du système nerveux cérébro‐spinal (1844). Reproduced by kind permission of the President and Council of The Royal College of Surgeons of England.
Today, a detailed knowledge of the anatomy of the cerebral sulci and gyri is part of a neurosurgeon's armamentarium: localising a craniotomy procedure, recognising eloquent areas of the brain (complemented by intraoperative neurophysiological testing), and accessing deep areas of the brain, all depend on identifying appropriate anatomical cues. An extensive literature of detailed cadaveric dissection studies now documents the sulci used as anatomical landmarks or microsurgical corridors in transcisternal, transfissural and transsulcal approaches (Ribas et al. 2006; Afif & Mertens, 2010; Ribas, 2010; Campero et al. 2014): in neurosurgery, as in so many other surgical specialisms, surgeons have returned to the dissecting room with the aim of enhancing their clinical practice.
What now?
Two narrative threads interweave in this short history of topographical anatomy. The first is the story of how the interior spaces of the human body were accessed and their contents described. The second is the story of the application and integration of that anatomical knowledge in clinical practice, whether directly in clinic, operating theatre or imaging suite, or indirectly in the dissecting room, whether teaching or undertaking research.
‘Work in progress’ describes areas where anatomical knowledge remains incomplete and/or controversial and includes acquiring a more detailed understanding of the anatomy of the extremes of age; resolving or refining disputed descriptions of regional anatomy, such as the pelvic floor (unifying the differing perspectives of colorectal and urological surgeons, obstetricians and radiologists) and the cervical deep fascia; updating anatomical terminology with reference to consensus papers produced by surgical groups and attitudinally correct cardiac terminology; acknowledging that textbooks tend to describe the youthful anatomical average, embracing evidence‐based anatomy and undertaking meta‐analyses of anatomical databases (Cornwall, 2013; Roy et al. 2015); recognising the ranges of normal anatomical variation, e.g. in assessing dermatome distribution in the lower limb (Lee et al. 2008) or the prevalence of vascular variations (Schmidt et al. 2008).
Cadaveric dissection has played a central role in both stories. An extensive contemporary literature makes an eloquent case for its retention in postgraduate research and training. In contrast, dissection has proved vulnerable to pedagogic fashion and economic reality in undergraduate medical education (Winkelmann, 2007; Bergman et al. 2014): the aptly named ‘Millennial anatomy lab’ offers one way forwards (Benninger et al. 2014).
References
- Abdel‐Halim RE (2001) Experimental medicine 1000 years ago. Urol Ann 3, 55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno LJ (1994) The History of Cardiology. London: The Parthenon Publishing Group; [Cited in Willerson JT, Teaff R (1996) Egyptian contributions to cardiovascular medicine. Tex Heart Inst J 23, 191–200]. [PMC free article] [PubMed] [Google Scholar]
- Afif A, Mertens P (2010) Description of sulcal organization of the insular cortex. Surg Radiol Anat 32, 491–498. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Kapfhammer JP, Kress A, et al. (2011) Josef Klingler's models of white matter tracts: influences on neuroanatomy, neurosurgery, and neuroimaging. Neurosurgery 69, 238–252. [DOI] [PubMed] [Google Scholar]
- Aird WC (2011) Discovery of the cardiovascular system: from Galen to William Harvey. J Thromb Haemost 9(Suppl. 1), 118–129. [DOI] [PubMed] [Google Scholar]
- Alberti LB (1435/1972) On Painting (C. Grayson, translated). London: Penguin; [Cited in Russell G (2013) Vesalius and the emergence of veridical representation in Renaissance anatomy. Prog Brain Res 203, 3–32]. [DOI] [PubMed] [Google Scholar]
- Alberti SJMM, Hallam E. (eds.) 2013) Medical Museums Past, Present; Future. London: Royal College of Surgeons of England. [Google Scholar]
- Anonymous (1829) Address to the Community on the Necessity of Legalizing the Study of Anatomy. By order of the Massachusetts Medical Society, pp. 34–41 Boston: Perkins and Marvin; American Annuals of Education. New Series Volume 1, XLII. [Google Scholar]
- Anonymous (1830) The Medico‐Chirurgical Review and Journal of Medical Science. [Google Scholar]
- Anonymous (1832) An Act for Regulating Schools of Anatomy, Anno Secundo & Tertio. [Google Scholar]
- Anonymous (1833) The Medico‐Chirurgical Review and Journal of Practical Medicine. [Google Scholar]
- Antoniou SA, Antoniou GA, Antoniou AI, et al. (2015) Past, present, and future of minimally invasive abdominal surgery. JSLS 19, e2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apaydin N, Tubbs RS, Loukas M, et al. (2010) Review of the surgical anatomy of the axillary nerve and the anatomic basis of its iatrogenic and traumatic injury. Surg Radiol Anat 32, 193–201. [DOI] [PubMed] [Google Scholar]
- Arráez‐Aybar LA, Bueno‐López JL, Raio N (2015a) Toledo School of Translators and their influence on anatomical terminology. Ann Anat 198, 21–33. [DOI] [PubMed] [Google Scholar]
- Arráez‐Aybar LA, Navia‐Álvarez P, Fuentes‐Redondo T, et al. (2015b) Thomas Willis, a pioneer in translational research in anatomy (on the 350th anniversary of Cerebri anatome). J Anat 226, 289–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balta JY, Lamb C, Soames RW (2015) A pilot study comparing the use of Thiel‐ and formalin‐embalmed cadavers in the teaching of human anatomy. Anat Sci Educ 8, 86–91. [DOI] [PubMed] [Google Scholar]
- Ballestriero R (2010) Anatomical models and wax Venuses: art masterpieces or scientific craft works? J Anat 216, 223–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates AW (2008) ‘Indecent and demoralising representations’: public anatomy museums in mid‐Victorian England. Med Hist 52, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bay NS, Bay BH (2010) Greek anatomist Herophilus: the father of anatomy. Anat Cell Biol 43, 280–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedict R (1934) Patterns of Culture. New York: Houghton Mifflin. [Google Scholar]
- Benninger B, Matsler N, Delamarter T (2014) Classic versus millennial medical lab anatomy. Clin Anat 27, 988–993. [DOI] [PubMed] [Google Scholar]
- Bergman EM, Verheijen IW, Scherpbier AJ, et al. (2014) Influences on anatomical knowledge: the complete arguments. Clin Anat 27, 296–303. [DOI] [PubMed] [Google Scholar]
- Bestetti RB, Restini CB, Couto LB (2014) Development of anatomophysiologic knowledge regarding the cardiovascular system: from Egyptians to Harvey. Arq Bras Cardiol 103, 538–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billing C (2004) Modelling the anatomy theatre and the indoor hall theatre: dissection on the stages of early modern London. EMLS, Special Issue 13, 1–17. [Google Scholar]
- Bismuth H (2013) Revisiting liver anatomy and terminology of hepatectomies. Ann Surg 257, 383–386. [DOI] [PubMed] [Google Scholar]
- Blunt A (1978) Artistic Theory in Italy 1450–1660. Fourth Impression. Norfolk, VA: The Thetford Press. [Google Scholar]
- Bosmia A, Watanabe K, Shoja MM, et al. (2013) Michael Servetus (1511–1553): physician and heretic who described the pulmonary circulation. Int J Cardiol 167, 318–321. [DOI] [PubMed] [Google Scholar]
- Bradley WG (2008) History of medical imaging. Proc Am Philos Soc 152, 349–361. [PubMed] [Google Scholar]
- Braune W (1867–1872) Topographisch‐Anatomischer Atlas: Nach Durchschnitten an Gefrornen Cadavern. Leipzig: Verlag von Veit & Comp. [Google Scholar]
- Braune W (1877) An Atlas of Topographical Anatomy after Plane Sections of Frozen Bodies. Philadelphia: Lindsay and Blakiston. Translated by Edward Bellamy [English translation]. [Google Scholar]
- Breitenfeld T, Jurasic MJ, Breitenfeld D (2014) Hippocrates: the forefather of neurology. Neurol Sci 35, 1349–1352. [DOI] [PubMed] [Google Scholar]
- Brogna C, Fiengo L, Türe U (2012) Achille Louis Foville's atlas of brain anatomy and the Defoville syndrome. Neurosurgery 70, 1265–1273. [DOI] [PubMed] [Google Scholar]
- Bush RB, Leonhardt H, Bush IV, et al. (1974) Dr. Bozzini's Lichtleiter. A translation of his original article (1806). Urology 3, 119–123. [DOI] [PubMed] [Google Scholar]
- Campbell A (1905) Histological Studies on the Localisation of Cerebral Function. Cambridge: Cambridge University Press. [Google Scholar]
- Campbell T (1987) The Earliest Printed Maps 1472–1500. London: The British Library. [Google Scholar]
- Campero A, Tróccoli G, Martins C, et al. (2006) Microsurgical approaches to the medial temporal region: an anatomical study. Neurosurgery 59(Suppl. 2), ONS279–ONS307. [DOI] [PubMed] [Google Scholar]
- Campero A, Ajler P, Emmerich J, et al. (2014) Brain sulci and gyri: a practical anatomical review. J Clin Neurosci 21, 2219–2225. [DOI] [PubMed] [Google Scholar]
- Caron L (2015) Thomas Willis, the restoration and the first works of neurology. Med Hist 59, 525–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catani M, Sandrone S (2015) Brain Renaissance. From Vesalius to Modern Neuroscience. Oxford: Oxford Universty Press. [Google Scholar]
- Cattermole GN (1997) Michael Servetus: physician, Socinian and victim. J R Soc Med 90, 640–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavalcanti DD, Feindel W, Goodrich JT, et al. (2009) Anatomy, technology, art, and culture: toward a realistic perspective of the brain. Neurosurg Focus 27, E2. [DOI] [PubMed] [Google Scholar]
- Celesia GG (2012) Alcmaeon of Croton's observations on health, brain, mind, and soul. J Hist Neurosci 21, 409–426. [DOI] [PubMed] [Google Scholar]
- Chalcidius (1876) Platonis Timaeus Interprete Chalcidio cum Ejusdem Commentario. Lipsiae (Leipzig): B.G. Teubner; [Cited in Celesia GG (2012) Alcmaeon of Croton's observations on health, brain, mind, and soul. J Hist Neurosci 21, 409–426]. [DOI] [PubMed] [Google Scholar]
- Chaplin S (2008) Nature dissected, or dissection naturalized? The case of John Hunter's museum. Mus Soc 6, 135–151. [Google Scholar]
- Chaplin SDJ (2009) John Hunter and the ‘museum oeconomy’, 1750–1800. PhD thesis, University of London.
- Churchill ED, Belsey R (1939) Segmental pneumonectomy in bronchiectasis. Ann Surg 109, 481–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clayton M, Philo R (2012) Leonardo da Vinci Anatomist. London: Royal Collection Publications. [Google Scholar]
- Cole H (1964) Things for the Surgeon: A History of the Resurrection Men. London: Heinemann. [Google Scholar]
- Compier AH (2012) Rhazes in the renaissance of Andreas Vesalius. Med Hist 56, 3–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compston A (2011) Here there are lions. Brain 134, 3127–3134. [Google Scholar]
- Compston A (2012) Editorial. Brain 135, 645–647. [DOI] [PubMed] [Google Scholar]
- Copeman WS (1963) The evolution of anatomy and surgery under the Tudors. Ann R Coll Surg Engl 32, 1–21. [PMC free article] [PubMed] [Google Scholar]
- Cornwall J (2013) Perhaps we don't know what we thought we knew: why clinicians need to re‐visit and re‐engage with clinical anatomy. AMJ 6, 339–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couinaud C (1957) Le Foie; Études Anatomiques et Chirurgicales. Paris: Masson. [Google Scholar]
- Craik EM (2009) Hippocratic bodily ‘channels’ and oriental parallels. Med Hist 53, 105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crivellato E, Ribatti D (2006) Mondino de’ Liuzzi and his Anothomia: a milestone in the development of modern anatomy. Clin Anat 19, 581–587. [DOI] [PubMed] [Google Scholar]
- Cunningham A (2010) The Anatomist Anatomis'd: An Experimental Discipline in Enlightenment Europe. Farnham: Ashgate. [Google Scholar]
- Curtis JA, Laus J, Yung KC, et al. (2015) Static endoscopic evaluation of swallowing: transoral endoscopy during clinical swallow evaluations. Laryngoscope doi:10.1002/lary.25828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalfardi B, Daneshfard B, Nezhad GS (2014) Johannitius (809–873 AD), a medieval physician, translator and author. J Med Biogr 2014 Jun 9. pii: 0967772014532890 [DOI] [PubMed] [Google Scholar]
- Davis MC, Griessenauer CJ, Bosmia AN, et al. (2014) The naming of the cranial nerves: a historical review. Clin Anat 27, 14–19. [DOI] [PubMed] [Google Scholar]
- Debernardi A, Sala E, D'Aliberti G, et al. (2010) Alcmaeon of Croton. Neurosurgery 66, 247–252. [DOI] [PubMed] [Google Scholar]
- Degueurce C, Adds P (2010) The celebrated écorchés of Honoré Fragonard, part 1: the classical techniques of preparation of dry anatomical specimens in the 18th century. Clin Anat 23, 249–257. [DOI] [PubMed] [Google Scholar]
- Dobson JF (1927) Erasistratus. Proc R Soc Med 20, 825–832. [PMC free article] [PubMed] [Google Scholar]
- Doyen E (1917) Surgical Therapeutics and Operative Techniques, vol. I, pp. 599–602. London: Balliere, Tindall, and Cox. [Google Scholar]
- Drake RL, McBride MJ, Lachman N, et al. (2009) Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ 2, 253–259. [DOI] [PubMed] [Google Scholar]
- Durant W (1939) Pliny, Gauis Secundus (the elder) Historia Naturalus In: The Story of Civilization, The Life of Greece, Part II (ed. Durant W.), pp. 524–537. New York: Simon and Schuster; [Cited in Wiltse LL, Pait GT (1998) Herophilus of Alexandria (325–255 B.C.): the father of anatomy. Spine 23, 1904–1914]. [DOI] [PubMed] [Google Scholar]
- Dyer GS, Thorndike ME (2000) Quidne mortui vivos docent? The evolving purpose of human dissection in medical education. Acad Med 75, 969–979. [DOI] [PubMed] [Google Scholar]
- Eadie MJ (2003) Alfred Walter Campbell (1868–1937). J Neurol 250, 249–250. [DOI] [PubMed] [Google Scholar]
- Eizenberg N (2015) Anatomy and its impact on medicine: will it continue? Australas Med J 8, 373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis H (2001) A History of Surgery. London: Greenwich Medical Media Ltd. [Google Scholar]
- Ewart W (1889) The Bronchi and Pulmonary Blood Vessels. London: Bailliere, Tindall and Cox; [Cited in Tompsett DH (1965) The bronchopulmonary segments. Med Hist 9, 177–181]. [Google Scholar]
- Farrell S (2009) Warburton, Henry (1784–1858), of 45 Cadogan Place, Mdx In: The History of Parliament: The House of Commons 1820–1832 (ed. Fisher DR.). Cambridge: Cambridge University Press; http://www.historyofparliamentonline.org/volume/1820-1832/member/warburton-henry-1784-1858 [Google Scholar]
- Fernández‐Miranda JC, Rhoton AL Jr, Alvarez‐Linera J, et al. (2008) Three‐dimensional microsurgical and tractographic anatomy of the white matter of the human brain. Neurosurgery 62(Suppl. 3), 989–1026. [DOI] [PubMed] [Google Scholar]
- Ferrari G (1987) Public anatomy lessons and the carnival: the anatomy theatre of Bologna. Past & Present 117, 50–106. [DOI] [PubMed] [Google Scholar]
- Forbes TR (1974) A note on the procurement of bodies for dissection at the Royal College of Physicians of London in 1694 and 1710. J Hist Med Allied Sci 29, 332–334. [DOI] [PubMed] [Google Scholar]
- Foville AL (1844) Atlas: Traité Complet de L'anatomie, de la Physiologie et de la Pathologie du Système Nerveux Cérébro‐Spinal. Paris: Fortin, Masson et Cie. [Google Scholar]
- Frixione E (2013) Pneuma‐fire interactions in Hippocratic physiology. J Hist Med Allied Sci 68, 505–528. [DOI] [PubMed] [Google Scholar]
- Furdell EL (2002) Publishing and Medicine in Early Modern England. Rochester: University of Rochester Press. [Google Scholar]
- Garey LJ (1999) Brodmann's ‘Localization in the Cerebral Cortex’. London: Imperial College Press; [Cited in Loukas M, Pennell C, Groat C, Tubbs RS, Cohen‐Gadol AA (2011) Korbinian Brodmann (1868–1918) and his contributions to mapping the cerebral cortex. Neurosurgery 68, 6–11]. [DOI] [PubMed] [Google Scholar]
- Gelfand T (1972) The ‘Paris manner’ of dissection: student anatomical dissection in early eighteenth‐century Paris. Bull Hist Med 46, 99–130. [PubMed] [Google Scholar]
- Ghosh SK (2014) Johann Vesling (1598–1649): seventeenth century anatomist of Padua and his Syntagma Anatomicum. Clin Anat 27, 1122–1127. [DOI] [PubMed] [Google Scholar]
- Ghosh SK (2015) Human cadaveric dissection: a historical account from ancient Greece to the modern era. Anat Cell Biol 48, 153–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser O (1995) W. C. Roentgen and the discovery of the Roentgen rays. AJR Am J Roentgenol 165, 1033–1040. [DOI] [PubMed] [Google Scholar]
- Goldberg BB, Gramiak R, Freimanis AK (1993) Early history of diagnostic ultrasound: the role of American radiologists. AJR Am J Roentgenol 160, 189–194. [DOI] [PubMed] [Google Scholar]
- Goodrich JT (2000) A millennium review of skull base surgery. Child's Nerv Syst 16, 669–685. [DOI] [PubMed] [Google Scholar]
- Goss CM (1958) Book review on: Galen on anatomical procedures (De anatomicis administrationibus). Translation of the surviving books with introduction and notes by Charles Singer. Anat Rec 131, 253–257. [Google Scholar]
- Gratiolet LP (1854) Memoire Sur Les Plis Cerébraux de L'homme et des Primates. Paris: Bertrand; [Cited in Ribas GC (2010) The cerebral sulci and gyri. Neurosurg Focus 28(2), E2]. [DOI] [PubMed] [Google Scholar]
- Gray H (1858) Anatomy Descriptive and Surgical. London: J W Parker & Son. [Google Scholar]
- Green CD (2003) Where did the ventricular localization of mental faculties come from? J Hist Behav Sci 39, 131–142. [DOI] [PubMed] [Google Scholar]
- Griffin M, Hindocha S, Malahias M, et al. (2014) Flap decisions and options in soft tissue coverage of the upper limb. Open Orthop J 8, 409–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths D (2015) Neural control of micturition in humans: a working model. Nat Rev Urol 12, 695–705. [DOI] [PubMed] [Google Scholar]
- Gross CG (1995) Aristotle on the brain. Neuroscientist 1, 245–250. [Google Scholar]
- Guerrini A (2004) Anatomists and entrepreneurs in eighteenth‐century London. J Hist Med Allied Sci 59, 219–239. [DOI] [PubMed] [Google Scholar]
- Gurunluoglu R, Shafighi M, Gurunluoglu A, et al. (2011) Giulio Cesare Aranzio (Arantius) (1530–89) in the pageant of anatomy and surgery. J Med Biogr 19, 63–69. [DOI] [PubMed] [Google Scholar]
- Gurunluoglu R, Gurunluoglu A, Williams SA, et al. (2013) The history and illustration of anatomy in the Middle Ages. J Med Biogr 21, 219–229. [DOI] [PubMed] [Google Scholar]
- Hammer N, Löffler S, Bechmann I, et al. (2015) Comparison of modified Thiel embalming and ethanol‐glycerin fixation in an anatomy environment: potentials and limitations of two complementary techniques. Anat Sci Educ 8, 74–85. [DOI] [PubMed] [Google Scholar]
- Hanigan WC, Ragen W, Foster R (1990) Dryander of Marburg and the first textbook of neuroanatomy. Neurosurgery 26, 489–498. [DOI] [PubMed] [Google Scholar]
- Haviland TN, Parish LC (1970) A brief account of the use of wax models in the study of medicine. J Hist Med Allied Sci 25, 52–75. [DOI] [PubMed] [Google Scholar]
- Healy SE, Rai BP, Biyani CS, et al. (2015) Thiel embalming method for cadaver preservation: a review of new training model for urologic skills training. Urology 85, 499–504. [DOI] [PubMed] [Google Scholar]
- Hippocrates Hippocrates Loc Hom = Places in Man 460–370 BC.
- Hosemann W, Draf C (2013) Danger points, complications and medico‐legal aspects in endoscopic sinus surgery. GMS Curr Top Otorhinolaryngol Head Neck Surg 12, Doc06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosemann W, Schroeder HW (2015) Comprehensive review on rhino‐neurosurgery. GMS Curr Top Otorhinolaryngol Head Neck Surg doi:10.3205/cto000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houseman ND, Taylor GI, Pan WR (2000) The angiosomes of the head and neck: anatomic study and clinical applications. Plast Reconstr Surg 105, 2287–2313. [DOI] [PubMed] [Google Scholar]
- Huisman T (1992) Squares and diopters: the drawing system of a famous anatomical atlas. Tractrix 4, 1–11. [PubMed] [Google Scholar]
- Hurren E (2008) Whose body is it anyway? Trading the dead poor, coroner's disputes, and the business of anatomy at Oxford University, 1885–1929. Bull Hist Med 82, 775–818. [DOI] [PubMed] [Google Scholar]
- Hurren ET (2012) ‘Abnormalities and deformities’: the dissection and interment of the insane poor, 1832–1929. Hist Psychiatry 23(Pt 1), 65–77. [DOI] [PubMed] [Google Scholar]
- Iaconetta G, Fusco M, Cavallo LM, et al. (2007) The abducens nerve: microanatomic and endoscopic study. Neurosurgery 61(Suppl. 3), 7–14. [DOI] [PubMed] [Google Scholar]
- Ignjatovic D, Spasojevic M, Stimec B (2010) Can the gastrocolic trunk of Henle serve as an anatomical landmark in laparoscopic right colectomy? A postmortem anatomical study. Am J Surg 199, 249–254. [DOI] [PubMed] [Google Scholar]
- Infusino MH, Win D, O'Neill YV (1995) Mondino's book and the human body. Vesalius 1, 71–76. [PubMed] [Google Scholar]
- Inoue Y, Taylor GI (1996) The angiosomes of the forearm: anatomic study and clinical implications. Plast Reconstr Surg 98, 195–210. [DOI] [PubMed] [Google Scholar]
- Jones DG (2016) The public display of plastinates as a challenge to the integrity of anatomy. Clin Anat 29, 46–54. [DOI] [PubMed] [Google Scholar]
- Jordan DJ, Malahias M, Hindocha S, et al. (2014) Flap decisions and options in soft tissue coverage of the lower limb. Open Orthop J 8, 423–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimi A, Zargaran A, Borhani‐Haghighi A (2013) Avicenna's description of Willis circle. Int J Cardiol 168, 3041. [DOI] [PubMed] [Google Scholar]
- Kassam AB, Vescan AD, Carrau RL, et al. (2008) Expanded endonasal approach: vidian canal as a landmark to the petrous internal carotid artery. J Neurosurg 108, 177–183. [DOI] [PubMed] [Google Scholar]
- Kemp M (1970) A drawing for the Fabrica; and some thoughts upon the Vesalius muscle‐men. Med Hist 14, 277–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp M (2010) Style and non‐style in anatomical illustration: from Renaissance Humanism to Henry Gray. J Anat 216, 192–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler J, Moriggl B, Grau T (2014) The use of ultrasound improves the accuracy of epidural needle placement in cadavers. Surg Radiol Anat 36, 695–703. [DOI] [PubMed] [Google Scholar]
- Klestinec C (2011) Theatres of Anatomy: Students, Teachers, and Traditions of Dissection in Renaissance Venice. Baltimore: The Johns Hopkins University Press. [Google Scholar]
- Klingler J (1935) Erleichterung der makroskopischen Praeparation des Gehirns durch den Gefrierprozess Schweiz. Arch Neurol Psychiatr 36, 247–256. [Google Scholar]
- de Koning P (1903) Trois Traite′s D'anatomie Arabes par Muhammad ibn, ‘Ali Zakariyyā al‐Rāzī’Ali ibn al‐’Abbās et ‘Ali ibn Sīnā. Leiden: Brill; [Cited Russell G (2013) Vesalius and the emergence of veridical representation in Renaissance anatomy. Prog Brain Res 203, 3–32]. [DOI] [PubMed] [Google Scholar]
- Kramer R, Glass A (1932) Bronchoscopic localization of lung abscess. Annals Otol Rhinol Laryngol 41, 1210–1220. [Google Scholar]
- Kruse E, Olthoff A, Schiel R (2006) Functional anatomy of the recurrent and superior laryngeal nerve. Langenbecks Arch Surg 391, 4–8. [DOI] [PubMed] [Google Scholar]
- Kudlien F (1965) The seven cells of the uterus: the doctrine and its roots. Bull Hist Med 39, 415–423. [PubMed] [Google Scholar]
- Lamberg BA (2001) The thyroid gland in Anothomia Mundini (1316). Dan Medicinhist Arbog 2001, 142–147 [article in Danish]. [PubMed] [Google Scholar]
- Lanska DJ, Lanska JR (2013) Medieval and Renaissance anatomists: the printing and unauthorized copying of illustrations, and the dissemination of ideas. Prog Brain Res 203, 33–74. [DOI] [PubMed] [Google Scholar]
- Lassek AM (1958) Human Dissection; Its Drama and Struggle. Springfield: Thomas. [Google Scholar]
- Laurenza D (2012) Art and Anatomy in Renaissance Italy Images from a Scientific Revolution. The Metropolitan Museum of Art New York. New Haven: Yale University Press. [Google Scholar]
- Lee MW, McPhee RW, Stringer MD (2008) An evidence‐based approach to human dermatomes. Clin Anat 21, 363–373. [DOI] [PubMed] [Google Scholar]
- Lemay R (1978) Gerard of Cremona In: Dictionary of Scientific Biography, vol. 15 (ed. Gillispie ChC.), pp. 173–192. New York, NY: Charles Scribner's Sons. [Cited in Arráez‐Aybar et al. (2015)]. [Google Scholar]
- Lett H (1943) Anatomy at the Barber‐Surgeons’ Hall. Br J Surg 31, 101–111. [Google Scholar]
- Lichterman B (2008) Medical classics: Ica anatomy by Nikolai Pirogov. First published 1851–1859. BMJ 336, 725. [Google Scholar]
- Lister J (1867) On the antiseptic principle in the practice of surgery. Br Med J 2, 246–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo WB, Ellis H (2010) The circle before Willis: a historical account of the intracranial anastomosis. Neurosurgery 66, 7–18. [DOI] [PubMed] [Google Scholar]
- Lodge JPA (2016) Liver In: Gray's Anatomy. 41st edn (Editor‐in‐Chief: Standring S.), Chapter 67, pp. 1160–1173. London: Elsevier. [Google Scholar]
- Loukas M, Clarke P, Tubbs RS, et al. (2007) Raymond de Vieussens. Anat Sci Int 82, 233–236. [DOI] [PubMed] [Google Scholar]
- Loukas M, Lam R, Tubbs RS, et al. (2008) Ibn al‐Nafis (1210–1288): the first description of the pulmonary circulation. Am Surg 74, 440–442. [PubMed] [Google Scholar]
- Loukas M, Pennell C, Groat C, et al. (2011) Korbinian Brodmann (1868–1918) and his contributions to mapping the cerebral cortex. Neurosurgery 68, 6–11. [DOI] [PubMed] [Google Scholar]
- Lü J (2015) Arachnoid membrane: the first and probably the last piece of the roadmap. Surg Radiol Anat 37, 127–138. [DOI] [PubMed] [Google Scholar]
- Ludwig E, Klingler L (1956) Atlas Cerebri Humani. Basel: S. Karger AG. [Google Scholar]
- MacDonald H (2009) Procuring corpses: the English anatomy inspectorate, 1842 to 1858. Med Hist 53, 379–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmillan M (2014) Alfred Walter Campbell and the visual functions of the occipital cortex. Cortex 56, 157–181. [DOI] [PubMed] [Google Scholar]
- Magee R (2001) Art macabre: resurrectionists and anatomists. ANZ J Surg 71, 377–380. [PubMed] [Google Scholar]
- Manchot C (1889) Die Hautarterien des Menschlichen Körpers. Liepzig: FCW Vogel. [Google Scholar]
- Mattern SP (2013) The Prince of Medicine. Galen in the Roman Empire. Oxford: Oxford University Press. [Google Scholar]
- Mavrodi A, Paraskevas G (2014) Morphology of the heart associated with its function as conceived by ancient Greeks. Int J Cardiol 172, 23–28. [DOI] [PubMed] [Google Scholar]
- Mayor AH (1964) Artists as anatomists. Metropol Mus Art Bull 22, 201–210. [Google Scholar]
- McKechnie MDJ, Robertson C (2002) The resuscitation greats. William Harvey. Resuscitation 55, 133–136. [DOI] [PubMed] [Google Scholar]
- Meyer A, Hierons R (1962) Observations on the history of the ‘circle of Willis’. Med Hist 6, 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell PD (2012) There's more to dissection than Burke and Hare: unknowns in the teaching of anatomy and pathology from the Enlightenment to the early 20th century in England In: Anatomical Dissection in Enlightenment England and Beyond: Autopsy, Pathology and Display, vol. Cj 1 (ed. Mitchell PD.), pp. 1–11. Farnham: Ashgate. [Google Scholar]
- Mitchell PD, Boston C, Chamberlain AT, et al. (2011) The study of anatomy in England from 1700 to the early 20th century. J Anat 219, 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell EL, Sevdalis N, Arora S, et al. (2012) A fresh cadaver laboratory to conceptualize troublesome anatomic relationships in vascular surgery. J Vasc Surg 55, 1187–1194. [DOI] [PubMed] [Google Scholar]
- Molnár Z (2004) Thomas Willis (1621–1675), the founder of clinical neuroscience. Nat Rev Neurosci 5, 329–335. [DOI] [PubMed] [Google Scholar]
- Moore CM, Brown CM (2004) Gunther von Hagens and Body Worlds Part 1: the anatomist as prosektor and proplastiker. Anat Rec B New Anat 276, 8–14. [DOI] [PubMed] [Google Scholar]
- Morgenstern L (2005) The 200th anniversary of the first endoscope: Philipp Bozzini (1773–1809). Surg Innov 12, 105–106. [DOI] [PubMed] [Google Scholar]
- Moris DN, Bramis KJ, Mantonakis EI, et al. (2012) Surgery via natural orifices in human beings: yesterday, today, tomorrow. Am J Surg 204, 93–102. [DOI] [PubMed] [Google Scholar]
- Morris SF, Taylor GI (2012) Vascular territories In: Plastic Surgery, vol. 1 (ed. Neligan PC.), Principles: Chapter 23, pp. 479–511. Philadelphia: Saunders. [Google Scholar]
- Morton LT (1991) London's last private medical school. J R Soc Med 84, 682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moxham BJ, Plaisant O (2014) The history of the teaching of gross anatomy—how we got to where we are!. Eur J Anat 18, 219–244. [Google Scholar]
- Neher A (2010) The truth about our bones: William Cheselden's Osteographia. Med Hist 54, 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil JH, Gilmour W, Gwynne FJ (1939) The anatomy of the bronchial tree. BMJ 1, 495–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt J, Mehdian R, Parkin I, et al. (2012) Cadaveric surgery: a novel approach to teaching clinical anatomy. Clin Teach 9, 148–151. [DOI] [PubMed] [Google Scholar]
- Nutton V (1979) John Caius and the Linacre tradition. Med Hist 23, 373–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutton V (2012) Vesalius revisited: his annotations to the 1555 Fabrica. Med Hist 56, 415–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor JP (2003) Thomas Willis and the background to Cerebri Anatome. J R Soc Med 96, 139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olry R (1997) Medieval neuroanatomy: the text of Mondino dei Luzzi and the plates of Guido da Vigevano. J Hist Neurosci 6, 113–123. [DOI] [PubMed] [Google Scholar]
- O'Malley CD (1964) Andreas Vesalius of Brussels, 1514–1564. Berkeley: University of California Press. [Google Scholar]
- Parent A (2014) Louis Pierre Gratiolet (1815–1865) and his contribution to the study of cerebral convolutions in primates. Neurosci Med 5, 1–8. [Google Scholar]
- Park K (1994) The criminal and the saintly body: autopsy and dissection in Renaissance Italy. Renaiss Q 47, 1–33. [PubMed] [Google Scholar]
- Park K (1995) The life of the corpse: division and dissection in late medieval Europe. J Hist Med Allied Sci 50, 111–132. [DOI] [PubMed] [Google Scholar]
- Pasipoularides A (2013) Historical Perspective: Harvey's epoch‐making discovery of the circulation, its historical antecedents, and some initial consequences on medical practice. J Appl Physiol (1985) 114, 1493–1503. [DOI] [PubMed] [Google Scholar]
- Pathiraja F, Little D, Denison AR (2014) Are radiologists the contemporary anatomists? Clin Radiol 69, 458–461. [DOI] [PubMed] [Google Scholar]
- Pearce JM (2008) The development of spinal cord anatomy. Eur Neurol 59, 286–291. [DOI] [PubMed] [Google Scholar]
- Pearce JM (2013) The neurology of Aretaeus: radix pedis neurologia. Eur Neurol 70, 106–112. [DOI] [PubMed] [Google Scholar]
- Persaud TV (1984) Early History of Human Anatomy: From Antiquity to the Beginning of the Modern era. Springfield: Charles C Thomas. [Google Scholar]
- Pilcher LS (1903) Jacobus Berengarius Carpensi and his Commentaries on Mundinus. Med Library Hist J 1, 1–8. [PMC free article] [PubMed] [Google Scholar]
- Pilcher LS (1906) The Mondino myth. Med Library Hist J 4, 311–331. [PMC free article] [PubMed] [Google Scholar]
- Porzionato A, Macchi V, Stecco C, et al. (2012) The anatomical school of Padua. Anat Rec (Hoboken) 295, 902–916. [DOI] [PubMed] [Google Scholar]
- Porzionato A, Macchi V, De Caro R (2013) The role of Caspar Bartholin the Elder in the evolution of the terminology of the cranial nerves. Ann Anat 195, 28–31. [DOI] [PubMed] [Google Scholar]
- Porzionato A, Polese L, Lezoche E, et al. (2015) On the suitability of Thiel cadavers for natural orifice transluminal endoscopic surgery (NOTES): surgical training, feasibility studies, and anatomical education. Surg Endosc 29, 737–746. [DOI] [PubMed] [Google Scholar]
- Pranghofer S (2009) ‘It could be seen more clearly in unreasonable animals than in humans’: the representation of the rete mirabile in early modern anatomy. Med Hist 53, 561–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prioreschi P (2001) Determinants of the revival of dissection of the human body in the Middle Ages. Med Hypotheses 56, 229–234. [DOI] [PubMed] [Google Scholar]
- Raichle ME, Snyder AZ (2007) A default mode of brain function: a brief history of an evolving idea. NeuroImage 37, 1083–1090. [DOI] [PubMed] [Google Scholar]
- Ramachandran I, Rodgers P, Elabassy M, et al. (2009) Multidetector computed tomography of the mesocolon: review of anatomy and pathology. Curr Probl Diagn Radiol 38, 84–90. [DOI] [PubMed] [Google Scholar]
- Reichman E (2010) Anatomy and the doctrine of the seven‐chamber uterus in rabbinic literature. Hakirah 10, 245–265. [Google Scholar]
- Rengachary S, Colen C, Dass K, et al. (2009) Development of anatomic science in the late middle ages: the roles played by Mondino de Liuzzi and Guido da Vigevano. Neurosurgery 65, 787–793. [DOI] [PubMed] [Google Scholar]
- Ribas GC (2010) The cerebral sulci and gyri. Neurosurg Focus 28, E2. [DOI] [PubMed] [Google Scholar]
- Ribas GC, Yasuda A, Ribas EC, et al. (2006) Surgical anatomy of microneurosurgical sulcal key points. Neurosurgery 59(Suppl. 2), ONS177–ONS210. [DOI] [PubMed] [Google Scholar]
- Richardson R (2001) Death, Dissection and the Destitute. Chicago: University of Chicago Press. [Google Scholar]
- Richardson R (2008) The Making of Mr Gray's Anatomy. Bodies, Books, Fortune, Fame. Oxford: Oxford University Press. [Google Scholar]
- Richardson WF, Carman JB (2009) Translation of ‘De Humani Corporis Libri Septem’. Novato: Norman Publishing. [Cited in Shotwell AR (2013)]. [Google Scholar]
- Rifkin BA, Ackerman MJ, Folkenberg J (2011) Human Anatomy Depicting the Body from the Renaissance to Today. London: Thames and Hudson. [Google Scholar]
- Robinson DH, Toledo AH (2012) Historical development of modern anesthesia. J Invest Surg 25, 141–149. [DOI] [PubMed] [Google Scholar]
- Roy J, Henry BM, Pękala PA, et al. (2015) Median and ulnar nerve anastomoses in the upper limb: a meta‐analysis. Muscle Nerve doi:10.1002/mus.24993. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Russell G (2013) Vesalius and the emergence of veridical representation in Renaissance anatomy. Prog Brain Res 203, 3–32. [DOI] [PubMed] [Google Scholar]
- Sanan A, van Loveren HR (1999) The arachnoid and the myth of Arachne. Neurosurgery 45, 152–155. [DOI] [PubMed] [Google Scholar]
- Sanders MA (1999) William Cheselden: anatomist, surgeon, and medical illustrator. Spine (Phila Pa 1976) 24, 2282–2289. [DOI] [PubMed] [Google Scholar]
- Sandrone S (2016) The resting human brain and the predictive potential of the default mode network Commentary 3.1. In: Gray's Anatomy. 41st edn (Editor‐in‐Chief: Standring S.). London: Elsevier. [Google Scholar]
- Saunders JBDCM, O'Malley CD (1950) The Illustrations from the Works of Andreas Vesalius of Brussels a Discussion of the Plates and a Biographical Sketch of Vesalius. New York: Dover Publications. [Google Scholar]
- Savage‐Smith E (1995) Attitudes toward dissection in medieval Islam. J Hist Med Allied Sci 50, 67–110. [DOI] [PubMed] [Google Scholar]
- Sawday J (1990) The fate of Marsyas dissecting the renaissance body In: Renaissance Bodies: The Human Figure in English Culture, C. 1540–1660 (eds. Gent L, Llewellyn N.), pp. 111–135. London: Reaktion Books. [Google Scholar]
- Sawday J (1995) The Body Emblazoned. Dissection and the Body in Renaissance Culture. Oxford: Routledge. [Google Scholar]
- Scatliff JH, Johnston S (2014) Andreas Vesalius and Thomas Willis: their anatomic brain illustrations and illustrators. AJNR Am J Neuroradiol 35, 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt S, Demartines N, Soler L, et al. (2008) Portal vein normal anatomy and variants: implication for liver surgery and portal vein embolization. Semin Intervent Radiol 25, 86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepulveda W, Ximenes R, Wong AE, et al. (2012) Fetal magnetic resonance imaging and three‐dimensional ultrasound in clinical practice: applications in prenatal diagnosis. Best Pract Res Clin Obstet Gynaecol 26, 593–624. [DOI] [PubMed] [Google Scholar]
- Shah A, Smith A, Panchatsharam S (2013) Ultrasound‐guided subclavian venous catheterisation – is this the way forward? A narrative review. Int J Clin Pract 67, 726–732. [DOI] [PubMed] [Google Scholar]
- Shaw JP (1992) A history of the enumeration of the cranial nerves by European and British anatomists from the time of Galen to 1895, with comments on nomenclature. Clin Anat 5, 466–484. [Google Scholar]
- Shimizu S, Tanaka R, Rhoton AL Jr, et al. (2006) Anatomic dissection and classic three‐dimensional documentation: a unit of education for neurosurgical anatomy revisited. Neurosurgery 58, E1000. [DOI] [PubMed] [Google Scholar]
- Shoja MM, Tubbs RS (2007) The history of anatomy in Persia. J Anat 210, 359–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoja MM, Tubbs RS, Ghabili K, et al. (2015) The Roman Empire legacy of Galen (129–200 AD). Childs Nerv Syst 31, 1–5. [DOI] [PubMed] [Google Scholar]
- Shotwell AR (2013) The revival of vivisection in the sixteenth century. J Hist Biol 46, 171–197. [DOI] [PubMed] [Google Scholar]
- Spaner SJ, Warnock GL (1997) A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech A 7, 369–373. [DOI] [PubMed] [Google Scholar]
- Spiegel PK (1995) The first clinical X‐ray made in America–100 years. AJR Am J Roentgenol 164, 241–243. [DOI] [PubMed] [Google Scholar]
- von Staden H (1992) The discovery of the body: human dissection and its cultural contexts in ancient Greece. Yale J Biol Med 65, 223–241. [PMC free article] [PubMed] [Google Scholar]
- Stamm AC, Pignatari SS, Vellutini E (2006) Transnasal endoscopic surgical approaches to the clivus. Otolaryngol Clin North Am 39, 639.xi–656.xi. [DOI] [PubMed] [Google Scholar]
- Sternbach GL, Varon J, Fromm RE, et al. (2011) Galen and the origins of artificial ventilation, the arteries and the pulse. Resuscitation 49, 119–122. [DOI] [PubMed] [Google Scholar]
- Stiefel M, Shaner A, Schaefer SD (2006) The Edwin Smith Papyrus: the birth of analytical thinking in medicine and otolaryngology. Laryngoscope 116, 182–188. [DOI] [PubMed] [Google Scholar]
- Sudhoff K (1908)Ein Provenzalischer Anatomischer Traktat aus dem 13. Jahrhundert, in Ein Betrag zur Geschichte der Anatomie im Mittelalter Speziell der Anatomischen Graphik Nach Handschriften des 9. bis 15. Jahrhunderts. Studien zur Geschichte der Medizin. Leipzig: J.A. Barth, Facsimile reprint Hildesheim: Georg Olms, 1964. [Cited in Cavalcanti and Wickens]. [Google Scholar]
- Sussmann AR, Ko JP (2010) Understanding chest radiographic anatomy with MDCT reformations. Clin Radiol 65, 155–166. [DOI] [PubMed] [Google Scholar]
- Sutherland F, Harris J (2002) Claude Couinaud: a passion for the liver. Arch Surg 137, 1305–1310. [DOI] [PubMed] [Google Scholar]
- Swanson L (2014) Neuroanatomical Terminology: A Lexicon of Classical Origins and Historical Foundations. Oxford: Oxford University Press. [Google Scholar]
- Sylvius F (1663) Disputationes Medicarum. Amstelodami: J. van den Bergh; [Cited in Parent A (2014) Louis Pierre Gratiolet (1815–1865) and his contribution to the study of cerebral convolutions in primates. Neurosci Med 5, 1–8]. [Google Scholar]
- Tanriover N, Rhoton AL Jr, Kawashima M, et al. (2004) Microsurgical anatomy of the insula and the sylvian fissure. J Neurosurg 100, 891–922. [DOI] [PubMed] [Google Scholar]
- Taylor GI, Palmer JH (1987) The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg 40, 113–141. [DOI] [PubMed] [Google Scholar]
- Taylor GI, Corlett RJ, Dhar SC, et al. (2011) The anatomical (angiosome) and clinical territories of cutaneous perforating arteries: development of the concept and designing safe flaps. Plast Reconstr Surg 127, 1447–1459. [DOI] [PubMed] [Google Scholar]
- Taylor GI, Rozen WM, Whitaker IS (2012) Establishing a perforator flap nomenclature based on anatomical principles. Plast Reconstr Surg 129, 877e–879e. [DOI] [PubMed] [Google Scholar]
- Tekiner H (2015) Aretaeus of Cappadocia and his treatises on diseases. Turk Neurosurg 25, 508–512. [DOI] [PubMed] [Google Scholar]
- Thakur JD, Sonig A, Chittiboina P, et al. (2012) Humphrey Ridley (1653–1708): 17th century evolution in neuroanatomy and selective cerebrovascular injections for cadaver dissection. Neurosurg Focus 33, E3. [DOI] [PubMed] [Google Scholar]
- The Sydney Monitor NSW (1828–1838) From the Aberdeen Journal. http://trove.nla.gov.au/ndp/del/article/32141608
- Thomas DP (2006) Thomas Vicary and the anatomie of mans body. Med Hist 50, 235–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tompsett DH (1965) The bronchopulmonary segments. Med Hist 9, 177–181. [Google Scholar]
- Tsuchiya R, Kuroki T, Eguchi S (2015) The pancreas from Aristotle to Galen. Pancreatology 15, 2–7. [DOI] [PubMed] [Google Scholar]
- Tubbs RS (2016) The continuing relevance of anatomy in current surgical practice and research. Preface commentary In: Gray's Anatomy. 41st edn (Editor‐in‐Chief: Standring S.). London: Elsevier. [Google Scholar]
- Ugurel MS, Battal B, Bozlar U, et al. (2010) Anatomical variations of hepatic arterial system, coeliac trunk and renal arteries: an analysis with multidetector CT angiography. Br J Radiol 83, 661–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dijck J (2005) The Transparent Body. A Cultural Analysis of Medical Imaging. Seattle and London: University of Washington Press. [Google Scholar]
- Vasari G (1550) Le Vite de’ più Eccellenti Pittori, Scultori, ed Architettori (Lives of the Most Eminent Painters, Sculptors and Architects). Volume III: Filarete and Simone to Mantegna Florence: Torrentino. [Google Scholar]
- Veith P, Watanabe K, Shoja MM, et al. (2015) Humphrey Ridley (1653–1708): forgotten neuroanatomist and neurophysiologist. Clin Anat 28, 12–15. [DOI] [PubMed] [Google Scholar]
- Venkataramana NK, Rao SAV, Naik AL (2009) Endoscopic third ventriculostomy. J Pediatr Neurosci 4, 108–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergani F, Morris CM, Mitchell P, et al. (2012) Raymond de Vieussens and his contribution to the study of white matter anatomy: historical vignette. J Neurosurg 117, 1070–1075. [DOI] [PubMed] [Google Scholar]
- Vesalius A (2007) On the Fabric of the Human Body. A translation of De Humani Corporis Fabrica Libri Septem. Andreas Vesalius. Book V The Organs of Nutrition and Generation Translated by Richardson WF, in collaboration with Carman JB. Novato: Norman Publishing. [Google Scholar]
- Vilardell F (2005) Digestive Endoscopy in the Second Millennium. From the Lichtleiter to Echoendoscopy. Stuttgart: Thieme. [Google Scholar]
- Walter T (2004) Body Worlds: clinical detachment and anatomical awe. Sociol Health Illn 26, 464–488. [DOI] [PubMed] [Google Scholar]
- Weber RK, Hosemann W (2015) Comprehensive review on endonasal endoscopic sinus surgery. GMS Curr Top Otorhinolaryngol Head Neck Surg doi:10.3205/cto000123. eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickens A (2015) A History of the Brain. London: Psychology Press. [Google Scholar]
- Willerson JT, Teaff R (1996) Egyptian contributions to cardiovascular medicine. Tex Heart Inst J 23, 191–200. [PMC free article] [PubMed] [Google Scholar]
- Wiltse LL, Pait GT (1998) Herophilus of Alexandria (325–255 B.C.): the father of anatomy. Spine 23, 1904–1914. [DOI] [PubMed] [Google Scholar]
- Winkelmann A (2007) Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ 41, 15–22. [DOI] [PubMed] [Google Scholar]
- Zemmoura I, Serres B, Andersson F, et al. (2014) FIBRASCAN: a novel method for 3D white matter tract reconstruction in MR space from cadaveric dissection. NeuroImage 103, 106–118. [DOI] [PubMed] [Google Scholar]
- Zilles K, Amunts K (2010) Centenary of Brodmann's map – conception and fate. Nat Rev Neurosci 11, 139–145. [DOI] [PubMed] [Google Scholar]


