Abstract
Context:
Both invasive and noninvasive blood pressure (invasive arterial blood pressure [IABP] and noninvasive BP [NIBP]) monitors are used perioperatively; however, they often produce different values. The reason for this discrepancy is not clear, and it is possible that the act of cuff inflation itself might affect the IABP values, especially with the recurrent cycling of NIBP cuff.
Aim:
The aim of this study was to determine the effect of ipsilateral NIBP cuff inflation on the contralateral IABP values.
Settings and Designs:
Prospective, observational study.
Materials and Methods:
One hundred consecutive patients were studied. The NIBP device was set to cycle every 5 min for a total of 6 times. During each cuff inflation cycle, changes in IABP values from the arterial line in the contralateral arm were recorded. A total of 582 measurements were included for data analysis.
Statistical Analysis:
Chi-square, paired t-test, analysis of variance.
Results:
Mean (± standard deviation) changes in systolic BP (SBP), diastolic BP, and mean BP with cuff inflation were 6.7 ± 5.9, 2.6 ± 4.0, and 4.0 ± 3.9 mmHg, respectively. We observed an increase of 0–10 mmHg in SBP in majority (73.4%) of cuff inflations. The changes in IABP did not differ between the patients with or without hypertension or with the baseline SBP.
Conclusions:
This study showed that there is a transient reactive rise in IABP values with NIBP cuff inflation. This is important information in the perioperative and intensive care settings, where both these measurement techniques are routinely used. The exact mechanism for this effect is not known but may be attributed to the pain and discomfort from cuff inflation.
Keywords: Cuff inflation, intra-arterial blood pressure, noninvasive blood pressure
INTRODUCTION
Noninvasive blood pressure (NIBP) recording by the oscillometric method is a widely accepted standard of care for the perioperative monitoring of a patient's circulatory status. However, invasive arterial BP (IABP) measurement is considered as a standard of monitoring in patients requiring a more intense BP control and monitoring.[1,2,3,4] The two monitoring techniques often produce different values; however, the relationship between these two techniques has been poorly studied. A recent study by Wax et al. illustrated that there was a significant difference between the two monitoring techniques although it did not elucidate the reasons for these discrepancies.[5]
The effect of NIBP cuff inflation on the hemodynamics of the body is largely unknown. Previous studies have shown that cuff inflation at the arm for the BP measurement results in a transient rise in BP,[6,7] which might be due to the muscle activity or muscle compression, or to the overall anxiety of knowing that BP was being recorded.[8,9] Another potential contributing factor is that the very act of cuff inflation and the potential discomfort arising out of it may cause elevations in the arterial BP.[10] This phenomenon is known as the “alerting” response and has been studied in the outpatient, nonsurgical patient population, but data regarding the same in the perioperative setting are lacking.[11,12] This information is important in the perioperative and Intensive Care Unit (ICU) setting where both techniques are often employed and the information they produce help guide clinical interventions such as the use of vasopressors, blood transfusions, intravenous fluids, or the use of antihypertensive agents.
This study aims to elucidate the relationship between cuff inflation and the changes in IABP during the perioperative period. The objective of this study is to determine whether NIBP cuff inflation will influence the IABP readings. We hypothesize that there would be an increase in IABP readings with simultaneous NIBP cuff inflation secondary to pain and discomfort with cuff inflation.
MATERIALS AND METHODS
This study is a prospective nonrandomized observational study. After the Institutional Review Board approval and informed patient consent, 100 consecutive adult (>18 years of age) patients who were scheduled to undergo major surgical procedures from June to August 2014, where IABP monitoring was indicated for the perioperative care, were recruited for this study. Our exclusion criteria comprised patients in whom NIBP monitoring in the contralateral arm was contraindicated or not feasible, such as patients with lymphedema, previous mastectomy with axillary lymph node dissection, arteriovenous fistula, burns, skin injury, and those with poor cuff fit (body mass index >40). In addition, patients undergoing emergency surgery or those with significant cardiovascular comorbidities (heart failure, arrhythmias, and valvular heart disease) and the patients requiring inotropic support for hemodynamic instability were also excluded.
This study was conducted in the postanesthetic care unit (PACU), where patients were monitored postoperatively. All patients received general anesthesia for the surgical procedure and received standard postoperative care as per our institutional practice. The study was initiated when the patient was awake, alert (modified observer's alertness for awareness [OAA] scores) >4), comfortable (numeric rating pain score [NRS] <4) and hemodynamically stable, in the supine position.
All patients had IABP monitoring from a radial arterial cannula (20-gauge Introcan Safety®, B Braun, Melsungen, Germany), which was inserted after induction of anesthesia under strict aseptic conditions. Arterial line transducer was zeroed at the heart level, and the monitor (Cardiocap/5, Datex-Ohmeda Inc., GE Healthcare Technologies, Madison, WI, USA) was set to record the beat-to-beat measurement. Appropriate sized BP cuff was placed on the contralateral arm for the NIBP measurements. Baseline invasive and noninvasive BPs (systolic, diastolic and mean) and heart rate (HR) was recorded. The device was then set to cycle every 5 min for three times and then a rest period of 30 min followed by another set of three measurements. During each cuff inflation cycle, we recorded the changes (highest and lowest) in the arterial BP values (systolic, diastolic, and mean), the HR, NIBP and the duration of cuff inflation. We also collected the general demographic data, modified OAA scores, NRS pain scores before and after each cuff inflation.
Data were analyzed to determine the changes in the IABP (systolic, diastolic, and mean) and HR with cuff inflation by calculating the differences in the values between the baseline (prior to cuff inflation) and at the peak of cuff inflation. In addition, data were analyzed to determine the effect of successive cuff inflation on the changes in IABP and also the relationship between the IABP changes with baseline (invasive) BP and the duration of cuff inflation. Finally, we compared the changes in IABP with cuff inflation between patients who are known hypertensives and nonhypertensives.
Statistical analysis
As this was an observational study with no definite cause-effect relationship, we could not calculate a sample size. We recruited a total of 100 patients in this observational study. Data were collected and analyzed using SPSS statistical software version 16.0 (SPSS for Windows, Chicago, SPSS Inc.). All demographic data from the study were analyzed by frequency test, and the continuous data were analyzed by frequency cross tabulation and Chi-square test. Paired t-test was used to compare the arterial BP changes before cuff inflation and at maximum cuff inflation time. Two-way analysis of variance was used to test the effect of successive cuff inflation. Pearson's correlation analysis was used to test the correlation between duration of cuff inflation and change in IABP. P < 0.05 was considered statistically significant.
RESULTS
Demographics
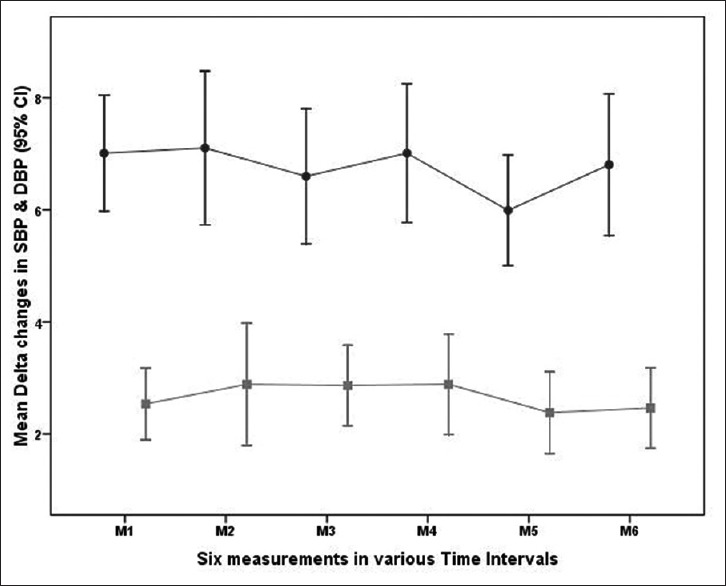
We recruited 100 patients for the study and data from three patients were excluded due to poor arterial waveforms (two) and hemodynamic instability during the study period (one). With six measurements each in 97 patients, total of 582 measurements were included in the final analysis. The demographic data are shown in Table 1. Most of our patients were in the fourth (18.6%), fifth (25.8%) or sixth (21.6%) decades of life. The mean age of the patient population was 54 years. In our study population, 48.5% of patients had hypertension, and 10.3% had diabetes. The baseline systolic BP (SBP), diastolic BP (DBP), and mean arterial BP (mean ± standard deviation [SD]) were 131 ± 18 mmHg, 78 ± 10 mmHg and 91.4 ± 13.2 mmHg, respectively. The mean (±SD) duration of BP cuff inflation is 36 ± 10 s. Modified OAA scores were similar across all patients; median (interquartile range): 5 (4–5) and there were no changes in pain scores before and after cuff inflation.
Table 1.
Demographic data
Effect of cuff inflation on invasive blood pressures
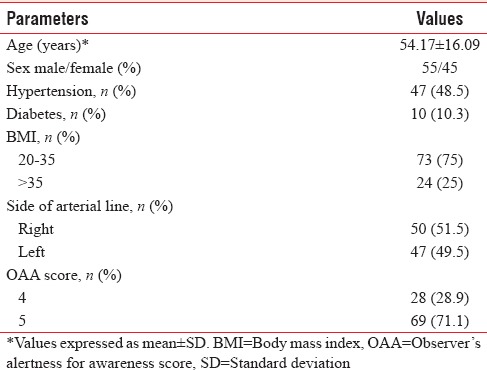
Mean changes (mean ± SD) in SBP, DBP and mean arterial BP with cuff inflation were 6.7 ± 5.9, 2.6 ± 4.0 and 4.0 ± 3.9 mmHg, respectively. We observed an increase in SBP of 0–10 mmHg in 73.4%, 11–20 mmHg in 19.2% and >20 mmHg in 1.4% of cuff inflations. In contrast, the increase in the DBP was 0–10 mmHg in the majority (85.7%) of cuff inflations and a small proportion had an increase above 11 mmHg (12.6%). A small percentage of patients also had a decrease in SBP (6%) and DBP (10.7%) with cuff inflation [Figure 1].
Figure 1.
Effect of cuff inflation on systolic and diastolic blood pressure (n = 582 readings; 97 patients with six readings each). Majority of patients had increase in systolic blood pressure (73.4%) and diastolic blood pressure (85.7%) in the range of 0–10 mmHg.
During the cuff inflation, there was statistically significant increase in the mean arterial pressure (MAP) (baseline vs. after cuff inflation: 91.40 ± 13.22 vs. 95.43 ± 13.65; mean difference: 4.03 ± 3.95; P = 0.00). Once the cuff was deflated, the MAP almost returned to the preinflation value (baseline vs. after cuff deflation: 91.40 ± 13.22 vs. 91.42 ± 13.86; mean difference: 0.01 ± 6.38; P = 0.941). This suggests that the effect of an increase in IABP to cuff inflation is very transient.
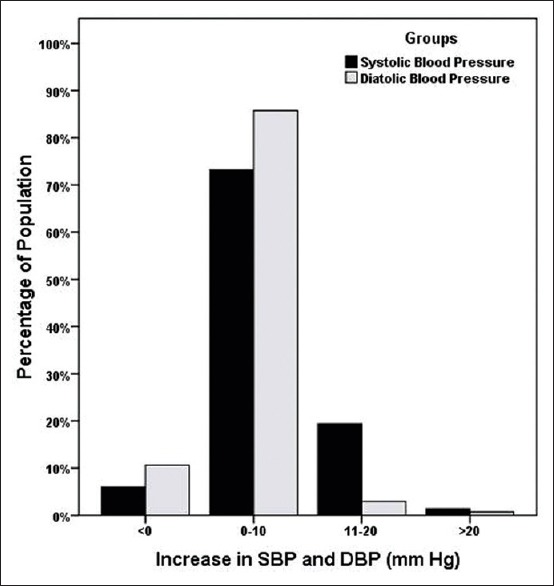
Hypertensives versus nonhypertensives
We analyzed the changes in IABP with cuff inflation in patients with or without hypertension. There was no statistically significant difference between the hypertensive and nonhypertensive patients in terms of mean rise in systolic (hypertensive vs. nonhypertensive group: 7.1 ± 6.4 vs. 6.3 ± 5.3; P = 0.114), diastolic (hypertensive vs. nonhypertensive group: 2.6 ± 4.1 vs. 2.6 ± 3.9; P = 0.979), and MAP (hypertensive vs. nonhypertensive group: 4.1 ± 4.0 vs. 3.9 ± 3.8; P = 0.441). Similarly, percentage of patients who had an increase of 0–10 mmHg in both systolic and diastolic was similar in both groups (hypertensive vs. nonhypertensive: 75.1% vs. 71.7%; P = 0.08 for SBP and 87.2% vs. 84.3%; P = 0.87 for DBP) [Figure 2].
Figure 2.
Comparison of effect of cuff inflation on systolic and diastolic blood pressure in normotensive versus hypertensive patients. Normotensive patients hypertensive patients both groups had a similar reactive rise in blood pressure with the cuff inflation. The difference between the groups was not statistically significant.
Changes in heart rate and the effect of successive cuff inflation
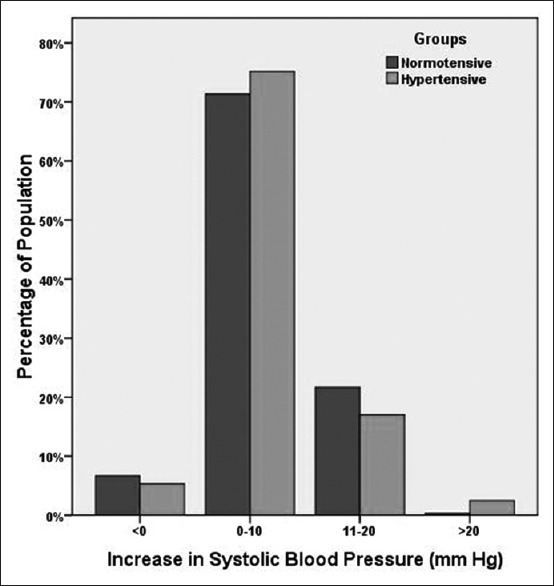
There were no significant changes in the HR from the baseline with cuff inflations (78.02 ± 17.66 vs. 77.54 ± 16.98, P = 0.73). Similarly, there were no differences in the IABP changes between the successive cuff inflations [Figure 3] and there were no significant correlations between the duration of cuff inflation and the changes in the SBP and DBP (r = 0.12 and r = 0.09, respectively).
Figure 3.
Effect of successive cuff inflation on systolic and diastolic blood pressure at various time intervals (Δsystolic blood pressure and Δdiastolic blood pressure) top–systolic blood pressure, bottom–diastolic blood pressure. There was no significant difference between the successive measurements.
Baseline systolic blood pressure and changes in invasive arterial blood pressure with cuff inflation
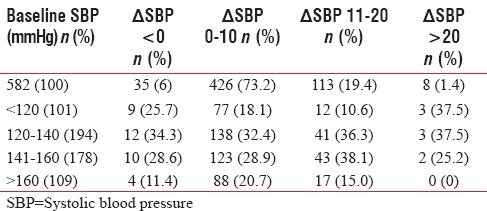
Response to cuff inflation was independent of the level of baseline SBP. The majority (73.5%) of cuff inflations resulted in an increase in SBP of less than 10 mmHg and these changes were similar across the groups with different baseline BP [Table 2]. Similarly, there was no statistical difference between high baseline SBP (>160 mmHg) and increase in SBP (P = 0.138).
Table 2.
Baseline systolic blood pressure and the reactive changes in arterial blood pressure with cuff inflation
DISCUSSION
To the best of our knowledge, with the review of literature, we did not find any studies investigating the effects of NIBP cuff inflation on the IABP recordings in the perioperative setting, but only in the clinical or ICU setting.[6,7,8,9,10,11,12,13] The importance of this study lies in the fact that both these techniques are often employed concurrently. NIBP measurement techniques utilize an oscillometric method, which calculates BP by measuring the amplitude of a series of oscillometric pulses during the cuff pressure inflation and deflation from above the SBP to DBP.[14] Although there are many factors such as NIBP cuff size, position of the cuff, quality of arterial waveform, degree of atherosclerosis, and site of measurement (central vs. peripheral) causing discrepancy between the two measurements,[15,16,17,18] the act of cuff inflation itself might affect the IABP values, especially with recurrent cycling of NIBP cuff.
The precise effect of NIBP cuff inflation on the physiology of hemodynamics is mostly unknown. Previous studies to evaluate the effect of NIBP cuff inflation were mainly done in the outpatient or office settings. Veerman et al. reported a prompt increase in SBP of about 13 and 12 mmHg in hypertensive and normotensive participants, respectively, with cuff inflation, using a noninvasive Finapress device applied to the contralateral middle finger to measure the effect of cuff inflation.[6] Other studies have also reported a similar reactive rise in BP with cuff inflation,[6,7] and have attributed this to the muscle activity or muscle compression as well as to the overall anxiety of knowing that BP was being recorded.[8,9] Another potential contributing factor is that the very act of cuff inflation and the potential discomfort arising from it may cause elevations in the IABP.[10,19]
In this study, we examined the effect of NIBP cuff inflation on the hemodynamics in the perioperative setting using an IABP measurement technique. We showed that the majority of NIBP cuff inflations (73.5%) resulted in an increase in SBP of 0–10 mmHg. We believe that the reactive rise is due to the pain and discomfort due to cuff inflation. However, there were no changes in HR with cuff inflation. This is consistent with a previous study by Skov-Madsen et al. in 56 patients in outpatient set up.[12] They reported that the discomfort caused secondary to cuff inflation during 24-h ambulatory BP monitoring did not increase the HR.
During NIBP measurement, both cuff inflation time and the maximum inflating pressure are dependent on the patient's baseline BP. Patients with hypertension may also have an exaggerated response to stress, probably due to an increased sensitivity of their sympathetic nervous system. Hence, the reactive rise in BP arising from the cuff inflation may be greater in patients with hypertension.[9,20] Charmoy et al. found that there was a significant rise in SBP with cuff inflation in hypertensive patients (P < 0.05).[21] However, they also found that there was no correlation between the baseline BP and the reactive rise in BP in both the groups. In contrast, we did not find significant differences in the reactive rise in SBP, DBP or mean arterial BP with cuff inflation between the hypertensive and nonhypertensive patients. In addition, there was no association between duration of cuff inflation and the reactive change in the BP.
Successive cuff inflations can lead to adaptation, causing the first BP values to be higher than the subsequent readings due to diminished pressor response.[11] However, in our study, there were no significant changes in the BP with successive cuff inflations.
Limitations
Our study does have limitations. First, the study was conducted in the PACU immediately after the surgery. Hence, many factors including the surgical stress response, fluid shifts and the postoperative pain management, all could have influenced the reactive changes in the BP. However, we made sure that the patients were in near normal physiological state with least discomfort before the measurements were taken. Second, our study showed that the increase in BP with NIBP cuff inflation is of small magnitude and short duration and would thus likely be of little clinical significance. Nevertheless, this is important information in the perioperative setting where both NIBP and IABP are used simultaneously, especially when tight BP control is indicated.
CONCLUSION
In summary, our study showed that NIBP cuff inflation causes a transient reactive rise in IABP. However, these changes were <10 mmHg in the majority of cuff inflations and were independent of the baseline BP. The exact mechanism for this effect is not known but may be attributed to cuff inflation and the resulting pain and discomfort.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sethi S. Correlation of invasive and non-invasive blood pressure: A must for management. Indian J Anaesth. 2010;54:581–2. doi: 10.4103/0019-5049.72658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ribezzo S, Spina E, Di Bartolomeo S, Sanson G. Noninvasive techniques for blood pressure measurement are not a reliable alternative to direct measurement: A randomized crossover trial in ICU. ScientificWorldJournal 2014. 2014 doi: 10.1155/2014/353628. 353628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holt TR, Withington DE, Mitchell E. Which pressure to believe? A comparison of direct arterial with indirect blood pressure measurement techniques in the pediatric intensive care unit. Pediatr Crit Care Med. 2011;12:e391–4. doi: 10.1097/PCC.0b013e3182230f43. [DOI] [PubMed] [Google Scholar]
- 4.Takci S, Yigit S, Korkmaz A, Yurdakök M. Comparison between oscillometric and invasive blood pressure measurements in critically ill premature infants. Acta Paediatr. 2012;101:132–5. doi: 10.1111/j.1651-2227.2011.02458.x. [DOI] [PubMed] [Google Scholar]
- 5.Wax DB, Lin HM, Leibowitz AB. Invasive and concomitant noninvasive intraoperative blood pressure monitoring: Observed differences in measurements and associated therapeutic interventions. Anesthesiology. 2011;115:973–8. doi: 10.1097/ALN.0b013e3182330286. [DOI] [PubMed] [Google Scholar]
- 6.Veerman DP, van Montfrans GA, Wieling W. Effects of cuff inflation on self-recorded blood pressure. Lancet. 1990;335:451–3. doi: 10.1016/0140-6736(90)90676-v. [DOI] [PubMed] [Google Scholar]
- 7.Kugler J, Schmitz N, Seelbach H, Rollnik J, Krüskemper GM. Rise in systolic blood pressure during sphygmomanometry depends on the maximum inflation pressure of the arm cuff. J Hypertens. 1994;12:825–9. [PubMed] [Google Scholar]
- 8.Veerman DP, van Montfrans GA, Karemaker JM, Wieling W. Inflating one's own cuff does not increase self-recorded blood pressure. J Hypertens Suppl. 1988;6:S77–8. doi: 10.1097/00004872-198812040-00020. [DOI] [PubMed] [Google Scholar]
- 9.Redman S, Dutch J. Cardiovascular responses during cuff inflation in subjects who have been sensitised to the measurement of their blood pressure. N Z Med J. 1984;97:180–2. [PubMed] [Google Scholar]
- 10.Rollnik JD, Schmitz N, Kugler J. Cardiovascular reactions induced by unpredictable, predictable, and controllable painful stimuli during sphygmomanometry. Int J Psychophysiol. 2001;40:161–5. doi: 10.1016/s0167-8760(00)00160-4. [DOI] [PubMed] [Google Scholar]
- 11.Czarkowski M, Zajac K, Rózanowski K. Can the pressor response accompanying blood pressure measurement be limited in young, normotensive women? Blood Press Monit. 2008;13:1–5. doi: 10.1097/MBP.0b013e3282f13eb8. [DOI] [PubMed] [Google Scholar]
- 12.Skov-Madsen M, Svensson M, Christensen JH. Cuff inflation during ambulatory blood pressure monitoring and heart rate. Integr Blood Press Control. 2008;1:15–9. doi: 10.2147/ibpc.s4072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin HF, Dhindsa MS, Tarumi T, Miles SC, Umpierre D, Tanaka H. Impact of blood pressure cuff inflation rates on flow-mediated dilatation and contralateral arm response. J Hum Hypertens. 2012;26:35–40. doi: 10.1038/jhh.2010.128. [DOI] [PubMed] [Google Scholar]
- 14.Alpert BS, Quinn D, Gallick D. Oscillometric blood pressure: A review for clinicians. J Am Soc Hypertens. 2014;8:930–8. doi: 10.1016/j.jash.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Jones DW, Appel LJ, Sheps SG, Roccella EJ, Lenfant C. Measuring blood pressure accurately: New and persistent challenges. JAMA. 2003;289:1027–30. doi: 10.1001/jama.289.8.1027. [DOI] [PubMed] [Google Scholar]
- 16.Chen Y, Zhu Y, Chen C, Chen X, Pan H, Chen S, et al. Relationship between noninvasive and invasive blood pressure values in end-stage renal disease patients on dialysis. Blood Press Monit. 2014;19:72–5. doi: 10.1097/MBP.0000000000000026. [DOI] [PubMed] [Google Scholar]
- 17.Tomlinson LA, Wilkinson IB. Does it matter where we measure blood pressure? Br J Clin Pharmacol. 2012;74:241–5. doi: 10.1111/j.1365-2125.2012.04203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manios E, Vemmos K, Tsivgoulis G, Barlas G, Koroboki E, Spengos K, et al. Comparison of noninvasive oscillometric and intra-arterial blood pressure measurements in hyperacute stroke. Blood Press Monit. 2007;12:149–56. doi: 10.1097/MBP.0b013e3280b083e2. [DOI] [PubMed] [Google Scholar]
- 19.Musso NR, Giacchè M, Galbariggi G, Vergassola C. Blood pressure evaluation by noninvasive and traditional methods. Consistencies and discrepancies among photoplethysmomanometry, office sphygmomanometry, and ambulatory monitoring. Effects of blood pressure measurement. Am J Hypertens. 1996;9(4 Pt 1):293–9. doi: 10.1016/0895-7061(95)00354-1. [DOI] [PubMed] [Google Scholar]
- 20.Jern S, Bergbrant A, Hedner T, Hansson L. Enhanced pressor responses to experimental and daily-life stress in borderline hypertension. J Hypertens. 1995;13:69–79. [PubMed] [Google Scholar]
- 21.Charmoy A, Würzner G, Ruffieux C, Hasler C, Cachat F, Waeber B, et al. Reactive rise in blood pressure upon cuff inflation: Cuff inflation at the arm causes a greater rise in pressure than at the wrist in hypertensive patients. Blood Press Monit. 2007;12:275–80. doi: 10.1097/MBP.0b013e3282c9ac9a. [DOI] [PubMed] [Google Scholar]


