Abstract
Patient: Male, 74
Final Diagnosis: Giant intradiverticular bladder tumor with metastasis
Symptoms: Hematuria
Medication:—
Clinical Procedure: —
Specialty: Urology
Objective:
Rare disease
Background:
Intradiverticular bladder tumors are rare. This renders diagnosis of an intradiverticular bladder tumor difficult. Imaging plays a vital role in achieving the diagnosis, and subsequently staging of the disease.
Case Report:
A 74-year-old male presented to our center with a few months history of constitutional symptoms. Upon further history, he reported hematuria two months prior to presentation, which stopped temporarily, only to recur a few days prior to coming to the hospital. The patient admitted to having lower urinary tract symptoms. However, there was no dysuria, no sandy urine, and no fever. Palpation of his abdomen revealed a vague mass at the suprapubic region, which was non tender. In view of his history and the clinical examination findings, an ultrasound of the abdomen and computed tomography (CT) was arranged. These investigations revealed a giant tumor that seemed to be arising from a bladder diverticulum, with a mass effect and hydronephrosis. He later underwent operative intervention.
Conclusions:
Intradiverticular bladder tumors may present a challenge to the treating physician in an atypical presentation; thus requiring a high index of suspicion and knowledge of tumor pathophysiology. As illustrated in our case, CT with its wide availability and multiplanar imaging capabilities offers a useful means for diagnosis, disease staging, operative planning, and follow-up.
MeSH Keywords: Diverticulum, Multidetector Computed Tomography, Urinary Bladder Neoplasms
Background
Primary bladder neoplasms make up 2–6% of all tumors in the United States, typically affecting men aged 50–70 years [1]. Intradiverticular bladder tumors account for approximately 1% of all urinary bladder tumors [2]. This renders diagnosis of an intradiverticular bladder tumor difficult. Bladder diverticula are a result of herniation of the interlacing muscle fibers, and are most commonly associated with chronic bladder outlet obstruction. Due to the lack of muscle layer within the diverticulum, urinary stasis, recurrent infection, and irritation of the wall with metaplasia increases the risk of neoplastic change [3]. Cystoscopy is a reliable method for diagnosing this disease, but in cases where the orifice is inaccessible, diagnosis may be missed. Imaging plays a vital role in achieving the diagnosis, and subsequently staging of the disease. We report a case of a 74-year-old male who presented to our center with gross hematuria and constitutional symptoms, and was eventually found to have a giant transitional cell carcinoma (TCC) of the bladder diverticulum observed on computed tomography (CT), followed by histopathological examination.
Case Report
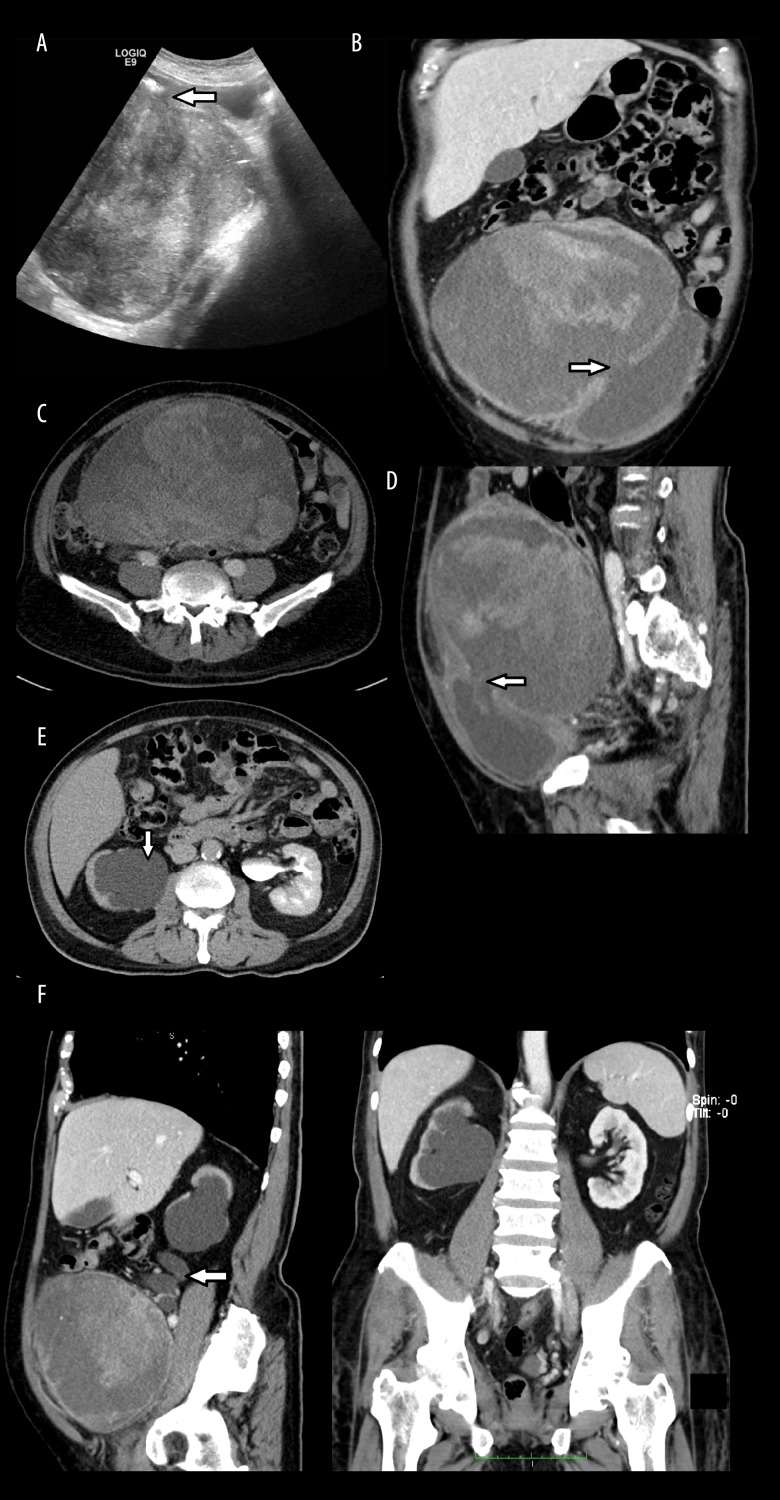
A 74-year-old male with underlying hypertension presented to our center with a few months history of loss of appetite and loss of weight. Upon further history evaluation, he reported passing bloody urine two months prior to his presentation, which stopped temporarily, only to recur a few days prior to coming to the hospital. The patient admitted to having lower urinary tract symptoms. However, there was no dysuria, no sandy urine, and no fever. Upon examination, he looked pale and lethargic. Palpation of the abdomen revealed a vague mass at the suprapubic region, which was non tender. Digital rectal examination showed an enlarged prostate gland. Blood investigations revealed a hemoglobin level of 11.5 g/dL, a white cell count of 14.5×109/L, and a platelet count of 402×109/L. Other blood parameters were unremarkable. In view of the patient’s history and clinical examination findings, supplemented by the blood results, imaging investigations were carried out. An ultrasound (Figure 1A) of the abdomen showed a heterogeneous mass arising within the bladder diverticulum, with demonstration of the diverticulum neck. The CT pre- and post-contrast enhancement through different planes demonstrated a giant intradiverticular bladder tumor, occupying the entirety of the abdominal cavity, with mass effect and right hydronephrosis (Figure 1B–1F). A cystoscopy done early during the workup showed the urinary bladder deviated to the left hemipelvis. There was poor visibility inside the urinary bladder, and the bladder neck could not be located. The procedure was then abandoned. In light of these findings, the patient was then scheduled for operative intervention. A radical cysto-prostatectomy, right radical nephrectomy, left end ureterostomy, and retroperitoneal lymph node dissection were performed. Intraoperatively, a huge bladder diverticulum weighing approximately 14 kg and bulging upon entry into the peritoneal cavity was found, with gross bilateral hydronephrosis (more on the right kidney) and multiple lymph node metastases. However, the patient developed hospital acquired pneumonia and succumbed to sepsis post-operatively; and unfortunately passed away.
Figure 1.
Ultrasound and CT images. (A) Ultrasound images in sagittal view demonstrating the heterogeneous appearance of the intradiverticular bladder tumor. The neck of the diverticulum is noted (arrow). (B–D) Non-contrasted CT images on coronal (B), axial (C), and sagittal (D) views showing heterogeneity and huge size of the intradiverticular bladder tumor. The neck of the diverticulum is clearly shown on the coronal (B) and sagittal (D) views (arrow). (E) Contrasted CT image on axial view, during the excretory phase showing right hydronephrosis with absence of contrast excretion (arrow). (F) Contrasted CT images on sagittal and coronal views demonstrating right hydronephrosis. The right ureter is noted to be tortuous (arrow).
Discussion
Of the various neoplasms affecting the urinary tract, urinary bladder is the most common site. The presence of a bladder diverticulum increases the likelihood of neoplastic changes. One study reported that when a diverticulum was present, the likelihood of neoplastic changes relative to that of a normal bladder was increased by 0.8–10% [4]. It is postulated that diverticula, due to the lack of a muscular layer, act as foci of urinary stasis, resulting in chronic inflammation, recurrent infection, development of dysplasia and metaplastic change [5].
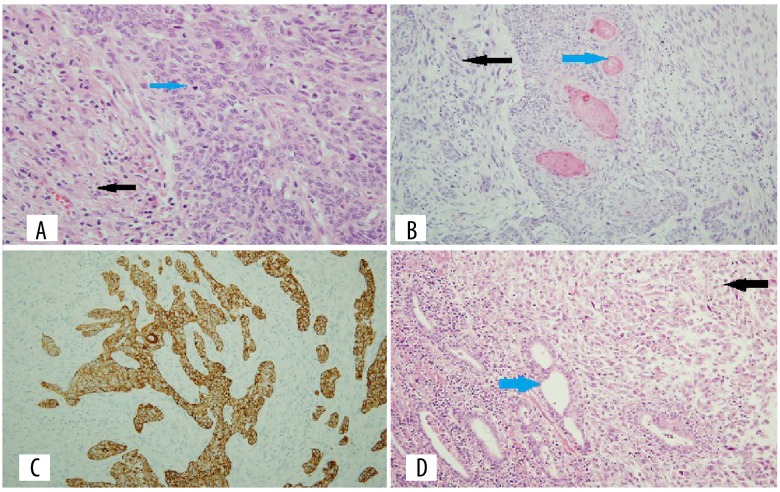
There are a few histological subtypes of urinary bladder carcinoma, the most common being of epithelial origin. These include TCC, also known as urothelial carcinoma (approximately 78%) (Figure 2A–2D), squamous cell carcinoma (17%), combination of transitional and squamous cell types (2%), and adenocarcinoma (2%) [6]. However, irrespective of the histological subtype, an intradiverticular bladder neoplasm poses a greater challenge due to its early transmural spread and invasion, a trait favored by a lack of muscular layer.
Figure 2.
Histopathological images. (A) Slide showing side by side a urothelial carcinoma component (blue arrow) and adjacent sarcomatoid change (black arrow) (×40). (B) Urothelial carcinoma component with squamous differentiation (blue arrow) and adjacent sarcomatoid change (black arrow) (×40). (C) The urothelial carcinoma component is positive with the epithelial marker CK5/6 immunostaining (×20). (D) The prostate gland is involved with tumor infiltration (black arrow) with adjacent benign prostate glands (blue arrow) (×40).
The approach to treatment varies; and whether a conservative or a more radical approach is taken depends on various factors. Garzotto and colleagues showed in their study that bladder tumors that are confined to diverticula and treated conservatively should be treated with a multimodal approach rather than a solitary surgical approach regardless of the tumor stage [7]. The authors found an 89% 4-year disease free period while avoiding a cystectomy. In our case, an operative approach was favored.
There are previous reports describing the occurrence of intradiverticular bladder tumors in the literature [8,9], but none as huge as demonstrated in our case. Therefore, achieving the diagnosis may present a challenge to treating physicians. The importance of radiological studies in aiding diagnosis cannot be undermined. Conventional radiography and ultrasound may be of limited use. Cystoscopy, as has been demonstrated above, frequently fails to reveal a tumor especially when met with a narrow orifice for which the cystoscope cannot enter.
Typically on CT, TCC appears either as an intraluminal papillary or nodular mass, or focal wall thickening. In an inadequately distended bladder, small or flat lesions tend to be missed. In 5% of cases, these lesions have calcifications; which typically encrust the tumor surface and may be nodular or arched [10]. They display early enhancement, approximately 60 seconds from injection. Intradiverticular tumors have a tendency towards early perivesical fat invasion, owing to the lack of muscle layer in their wall [1]. One case series of 20 patients reported a 100% detection of tumors [11]. These signs were not readily seen in our case, which proved to be a challenge. CT is relatively widely available and has multiplanar imaging capabilities. However, CT imaging modality provides a solution to the limitations of the aforementioned imaging studies.
Due to the atypical clinical presentation and often advanced stage of disease when eventually diagnosed, intradiverticular bladder tumors cause various complications. These complications may be related to facilitated tumor invasion owing to the relative lack of muscle fibers [12], or may be related to involvement of the surrounding structures and mass effect. These tumors have relatively poor prognosis. Currently, pathologic staging appears to be the most important prognostic factor [13].
Conclusions
Intradiverticular bladder tumors may present a challenge to the treating physician in an atypical presentation; this requires a high index of suspicion and knowledge of tumor pathophysiology. As illustrated in our case, CT scan, which is readily available and offers imaging through different planes with post processing capabilities, can play a pivotal role in diagnosis, disease staging, operative planning, and follow-up.
References:
- 1.Wong JJ, Woodward PJ, Manning MA, Sesterhenn IA. Neoplasms of the urinary bladder: Radiologicpathologic correlation. Radiographics. 2006;26:553–80. doi: 10.1148/rg.262055172. [DOI] [PubMed] [Google Scholar]
- 2.Walker NF, Gan C, Olsburgh J, Khan MS. Diagnosis and management of intradiverticular bladder tumors. Nat Rev Urol. 2014;11:383–90. doi: 10.1038/nrurol.2014.131. [DOI] [PubMed] [Google Scholar]
- 3.Raheem OA, Besharatian B, Hickey DP. Surgical management of bladder transitional cell carcinoma in a vesicular diverticulum: case report. Can Urol Assoc J. 2011;5(4):e60–64. doi: 10.5489/cuaj.10094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eksioglu AS. Transitional cell carcinoma within a bladder diverticulum: CT findings and pathologic correlation. Gazi Medical Journal. 2009;20(3):131–34. [Google Scholar]
- 5.Di Paolo PL, Vargas HA, Karlo CA, et al. Intra-diverticular bladder cancer: CT imaging features and their association with clinical outcomes. Clin Imaging. 2015;39(1):94–98. doi: 10.1016/j.clinimag.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dondalski M, White ME, Ghahremani, Patel SK. Carcinoma arising in urinary bladder diverticula: imaging findings in six patients. Am J Roentgenol. 1993;161(4):817–20. doi: 10.2214/ajr.161.4.8372767. [DOI] [PubMed] [Google Scholar]
- 7.Garzotto MG, Tewari A, Wajsman Z. Multimodal therapy for neoplasms arising from a vesical diverticulum. J Surg Oncol. 1996;62:46–48. doi: 10.1002/(SICI)1096-9098(199605)62:1<46::AID-JSO10>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 8.Golijanin D, Yossepowitch O, Beck SD, et al. Carcinoma in a bladder diverticulum: Presentation and treatment outcome. J Urol. 2003;170:1761–64. doi: 10.1097/01.ju.0000091800.15071.52. [DOI] [PubMed] [Google Scholar]
- 9.Matta EJ, Kenney AJ, Barre GM, Vanlangendonck RM. Intradiverticular bladder carcinoma. Radiographics. 2005;25:1397–403. doi: 10.1148/rg.255045205. [DOI] [PubMed] [Google Scholar]
- 10.Moon WK, Kim SH, Cho JM, Han MC. Calcified bladder tumors: CT features. Acta Radiol. 1992;33:440–43. [PubMed] [Google Scholar]
- 11.Kim JK, Park SY, Ahn HJ, et al. Bladder cancer: Analysis of multi-detector row helical CT enhancement pattern and accuracy in tumor detection and perivesical staging. Radiology. 2004;231:725–31. doi: 10.1148/radiol.2313021253. [DOI] [PubMed] [Google Scholar]
- 12.Das CJ, Debnath J, Thulkar SP, et al. Transitional cell carcinoma in a herniated vesical diverticulum. Br J Radiol. 2007;80(957):e227–29. doi: 10.1259/bjr/68501519. [DOI] [PubMed] [Google Scholar]
- 13.Humphrey PA, Moch H, Cubilla AL, et al. The 2016 classification of tumors of the urinary system and male genital organs – Part B: Prostate and bladder tumors. Eur Urol. 2016;70:106–19. doi: 10.1016/j.eururo.2016.02.028. [DOI] [PubMed] [Google Scholar]