Abstract
This article examines lasting mortality improvements associated with availability of Medicaid at time and place of birth. Using the US Vital Statistics (1959-2010), I exploit the variation in when each of the 50 states adopted Medicaid to estimate overall infant mortality improvements that coincided with Medicaid participation. 0.23 less infant deaths per 1000 live births was associated with states' Medicaid implementation. Second, I find lasting associations between Medicaid and mortality improvements across the life-course. I build state-specific cohort life-tables and regress age-specific mortality on availability of Medicaid in their states at time of birth. Cohorts born after Medicaid adoption had lower mortality rates throughout childhood and into adulthood. Being born after Medicaid was associated with between 2.03 and 3.64 less deaths per 100,000 person-years in childhood and between 1.35 and 3.86 less deaths per 100,000 person-years in the thirties. The association between Medicaid at birth and mortality was the strongest in the oldest age group (36-40) in this study.
Keywords: United States, Medicaid, Mortality
Medicaid is often credited as one of the contributors to the rapid decline in infant mortality rates in the decade after 1965 (Corman and Grossman 1985; Mason 1991). Medicaid sought to improve infant health by increasing access to care, particularly for low income groups that had disproportionately high mortality rates. Infant mortality in the United States declined 4.5 percent per year between 1965 and 1982 (Corman and Grossman 1985). It has been fifty years since the first State began to offer Medicaid. This article examines the mortality of cohorts who were born into one of the largest policy changes in Twentieth Century.
A rise in living standards, better nutrition, public sanitation, clean water supply, and public health campaigns contributed to dramatic reductions in infant mortality rates in the United States during the first half of the Twentieth Century (Condran and Crimmins-Gardner 1978; Cutler and Miller 2005; Deaton and Paxton 2001; Elo and Preston 1996; Ewbank and Preston 1990; Fogel 2004; McKeown 1976, 1979; Meeker 1972; Preston and Haines 1991; Szreter, 1988). After several decades of experiencing significant improvements, the year-to-year decline in infant mortality stalled to 0.5 percent by 1950 (Corman and Grossman 1985). Considerable national attention was focused on how infant health improvements in the US were lagging behind other developed nations (Committee on Maternal and Child Care 1965; Falkner 1969; Lee et al. 1980; Shapiro et al. 1968). Many efforts were made to improve prenatal and neonatal medical technology as well as to make services more accessible (Corman and Grossman 1985). Medicaid, a public insurance program targeting low-income pregnant women and infants receiving assistance from Aid to Families with Dependent Children (AFDC), was created by Title XIX of the Social Security Act in 1965. The period beginning 1965 experienced twentieth century's second surge of infant mortality decline (Grossman and Jacobowitz 1981; Lee et al. 1980).
A large body of literature examining the effects of Medicaid on its recipients has emerged since the program's inception (Baldwin et al. 1998; Braveman et al. 1993; Copeland and Meier 1987; Currie and Grogger 2002; Devany et al. 1992; Goodman-Bacon 2016; Guyer 1990; Howell 2001; Lykens and Jargowsky 2002; Moss and Carver 1998; Schor et al. 2007). However, relatively few studies examine Medicaid's contribution to general population health and its longer-term consequences. In this paper, I examine states' infant, childhood, and adult mortality associated with states' Medicaid participation at time of birth. I exploit the variation in States' timing of Medicaid adoption between 1966 and 1979 to address two research questions. (1) Was Medicaid associated with reductions in infant mortality at the population level? (2) Did states' Medicaid participation at birth have lasting associations with mortality into adulthood? Macro-level views of the consequences of large-scale health care reforms are informative as the policies often influence individuals outside their immediate targeted population. And these health effects during early life may endure into adulthood. This paper follows birth cohorts over time to examine potential lasting mortality consequences associated with Medicaid.
Theory and Literature
Population-level analyses of other high-income OECD countries show significant associations between infant mortality and the country's health care system. Countries with publicly funded health care had lower infant mortality rates than similar countries whose health care services are generally private (Elola et al. 1995). National health care systems were associated with greater improvements in infant mortality after accounting for secular declines and changes in GDP (Macinko et al 2004). Between 1970 and 1996, public health care systems were associated with over 3 less infant deaths per 1000 live births as IMR fell from 16.63 to 6.20 per 1000. These publicly funded national health systems also attenuated the positive association between income inequality and infant mortality (Macinko et al 2004).
In the United States, the introduction of the public health insurance program visibly improved insurance coverage and health care utilization. Prior to 1965, only half of low-income Americans had medical-coverage (Copeland and Meier 1987) and despite having poorer health than their wealthier counterparts, low-income individuals and families used fewer medical services (Copeland and Meier 1987; Rowland et al. 1988; Wilensky and Berk 1982). In particular, 88% of upper-income women reported seeing a physician during the first trimester of pregnancy compared to 58% of lower-income pregnant women (Andersen and Andersen 1967; Copeland and Meier 1987). By the late 1970s when most states had adopted Medicaid, 24 million Americans and over a third of people in households with incomes below 125% FPL received health insurance through Medicaid (Oberg and Polich 1988; Wilensky and Berk 1982). Medicaid specifically targeted low-income pregnant women and infants and their enrollee characteristics reflected this trait (Wilensky and Berk 1982). Medicaid covered about three-quarters of low-income pregnant mothers and children under the age of 5, reducing the rate of uninsurance for these target groups to below the national average (Holahan and Zedlewski 1991). By 1980, the low-income group was utilizing medical services (hospital stays and physician visits) at an equivalent rate as the higher-income groups (Copeland and Meier 1987; Rowland et al. 1988; Wilensky and Berk 1982).
Medicaid's impact on its recipients is clear. Goodman-Bacon (2016) and Currie and Gruber (1996) find convincing evidence that Medicaid expansions in the 1980s contributed to reductions in infant mortality rates. Goodman-Bacon (2016)'s analysis exploited variations in states' timing of Medicaid adoption and differences in shares of immediately eligible children throughout the 1960s and 1970s. He finds significant reductions in infant and child mortality associated with Medicaid especially among populations that were more likely to become eligible for public assistance. Currie and Gruber (1996) examined subsequent expansions of Medicaid in the 1980s. They standardized states' Medicaid generosities by simulating the proportion of women who would be eligible from a nationally representative sample of 3,000 women from the Current Population Survey each year. Their method allowed the authors to effectively isolate the effects of States' extent of Medicaid expansions from the composition of their residents.
However, Medicaid may also have had spillover effects on women and infants who did not gain insurance coverage from the public program. Theories in diffusion suggest that as a greater proportion of women gain access to pre- and post-natal care, the health of all women would improve. Health knowledge spreads through interpersonal networks as well as institutional organizations (Backer 1991; Tarde 1962; Green et al. 2009). Interaction with peers, friends, and family as well as health care providers influence how individuals approach their health (Christakis and Fowler 2007, 2009; Glanz et al. 2008). Social network effects on health behavior are not trivial. Groups of socially connected people quit smoking in concert at different times despite the already ‘generalized knowledge’ of smoking's adverse effects on health (Christakis and Fowler 2009). Medicaid connects more women with health care providers and encourages transfer of health knowledge from physicians to the public. As more women adopt good nutrition and refrain from risky health behaviors, the more likely they are to influence other women in their social networks, even those who always had access to health care services.
Increasing health insurance coverage through Medicaid can improve health care delivery for everybody, including those who were always insured. Financial incentive for hospitals to invest in prenatal and neonatal services may have increased when more people in the community gained health insurance. Adoption of Medicare (another public insurance program for people over 65) was associated with new hospital entries, increased adoption of cardiac technology, and increased medical spending on non-Medicare patients (Finkelstein 2007). Also, improving coverage could have alleviated barriers to care reported by insured people living in communities with high rates of uninsurance: more unmet health care needs, lower access to care, and lower trusts in their physicians (Pagan and Pauly 2006, Pauly and Pagan 2007, Pagán, Balasubramanian, and Pauly 2007).
Access to prenatal and infant health care may have long-term consequences for health. As the recipients of Medicaid reach adulthood, a growing number of studies are examining the longer-term consequences of early-life insurance coverage. Boudreaux et al. (2016) show that children who were exposed to Medicaid as it rolled out across states had fewer chronic conditions in adulthood. Duration of Medicaid eligibility also matters for later life health. Two recent articles examined the longer-term consequences of expansions that increased the age to which children were eligible for Medicaid. Reduced hospitalizations, emergency department visits (Wherry et al. 2015), and disease-related mortality (Wherry and Meyer 2015) were lower among cohorts who were eligible for Medicaid longer during their childhoods.
These articles build upon a longstanding literature that connects prenatal and early-life environment to later-life health outcomes. One of the most well-known of these studies finds a positive link between ischemic health disease mortality and infant mortality rates at the place and time of birth (Barker and Osmond 1986). Their study suggests that early-life living conditions and nutrition (measured by local infant mortality rates) have long-term consequences well into adulthood even when they move to another region. Quasi-experimental studies also find poorer health outcomes among birth cohorts born during the 1918 Influenza Pandemic and the 1944 Dutch Famine relative to cohorts born immediately before or after these sudden deteriorations in living conditions (Almond 2006; Roseboom et al. 2001). The literature is strongly suggestive of initial conditions at birth having long-lasting health consequences. Medicaid explicitly aims to improve prenatal health and birth outcomes. Thus, I expect these wide-spread efforts to translate into improved health throughout the life-course.
The first research question adds to the literature by examining the overall changes in infant mortality rate—recipients and non-recipients alike—associated with States' Medicaid participation. The second part of this paper shows that cohorts who were born after their states adopted Medicaid had lower mortality in childhood and adulthood compared to cohorts born immediately prior to Medicaid.
Before delving into the analyses, I briefly describe the policy context of States' Medicaid participation during the period after 1965. The program offered federal grants to states to provide health insurance to eligible persons. During the early years, the federal government gave considerable flexibility in when or whether each state could participate in the program. States that decided to participate had to provide coverage to recipients of Aid to Families with Dependent Children (AFDC) mostly, pregnant women and infants who met income and asset requirements (Medicaid eligibility diverged from AFDC-eligibility in the 1980s). States began to participate in Medicaid quickly after the Title XIX of the Social Security Act in 1965. States in the Northeast were relatively early adopters of Medicaid. Pennsylvania and New York—the two largest states in this region—were among the first. The New England states followed in quick succession and New Jersey was the last to implement Medicaid in 1970. Infant mortality rates among the states in the Northeast in 1965 were similar to each other, ranging between 22 and 23 deaths per 1000 live births. Infant mortality among states in the Midwest and West had greater variability. Utah had the lowest IMR at around 18 deaths per 1000 and Illinois had the highest at over 25 deaths per 1000. Most of these states adopted Medicaid prior to 1968. Southern states had higher rates of infant mortality on average. Mississippi's infant mortality rates were exceptionally high at 40 deaths per 1000. The remaining states ranged between 22 and 31 deaths per 1000. The adoption of Medicaid in the South was evenly spread out across the years between 1966 and 1970.
States' timing of Medicaid implementation was different from other public policies that the Johnson administration introduced to combat poverty in the 1960s and 1970s. The Food Stamp Act of 1964 was the other major initiative targeting women and children to improve prenatal health and reduce infant mortality (Almond et al. 2011). However, the rollout of the Food Stamp Program did not coincide with states' Medicaid implementation dates. The Food Stamp Program was implemented at the county-level and its implementation stretched out between 1961 and 1976. Thirty percent of the US population already had access to food stamps by the time the first states began to offer Medicaid in January 1966. About a quarter of the population gained access to food stamps after 1970 when all but two states had joined the Medicaid program. Furthermore, states' Medicaid participation had little bearing on its counties' food stamp participation start date. Most notably, most counties in New York, Oklahoma, and Massachusetts began to offer food stamps relatively late, despite being early adopters of Medicaid. Many counties in Texas and California did not offer food stamps until after 1970. Thus, the exact timing of Medicaid implementation appears exogenous to other prenatal and infant health policy initiatives that occurred during this period. DATA
Using the US Vital Statistics micro-data, I examine mortality patterns for birth cohorts born between 1959 and 1979—the 20-year period surrounding the introduction of Medicaid in 1965. I start my analysis in 1959 when Hawaii became the last state to join the US. I use the natality micro-data for births between 1959 and 1979 to calculate the number of births by year for each state. The data does not include births to US citizens outside the United States. To derive the state-age-specific mortality rates for cohorts born between 1959 and 1979, I use the mortality micro data from 1959 to 2010. Mortality data for New Jersey is missing for the years, 1962 and 1963. Mortality data for Hawaii is incomplete for prior to 1968 and is excluded from the analyses. In 1972, the US Vital Statistics contains only a 50 percent sample of death records. I have multiplied the number of deaths in 1972 by a factor of two in my analyses.
The analyses do not differentiate race. The US Vital Statistics changed the way it categorized race several times between 1968 and 2010. Prior to 1968, people were categorized as either white or non-white. After 1968, the non-white population was classified into sub-groups and people with Latin American heritage were separated from the white classification (up until the late 1960s, they were categorized as white). The changes in how the data classifies race make it difficult to compare minority groups across the years. In addition, the number of non-whites being born and dying in some states were so small that the age-specific mortality rates quickly became unreliable.
Analytic Strategy
The main analyses exploit the variation in when States adopted Medicaid to estimate age-specific mortality improvements associated with Medicaid. Using the natality and mortality files, I create a life-table for each birth cohort in each state. These life-tables summarize the mortality experiences of cohorts born and living in each of the 50 states until age 40. I estimate changes in age-specific mortality rates associated with whether Medicaid was available in the state at time of birth. In these regression models, I control for secular declines in mortality with year fixed-effects. All regression models have panel-corrected standard errors and they also correct for heteroscedasticity. These corrections account for interdependent observations within states.
This framework takes advantage of states' variation in the timing of Medicaid start. States' baseline infant mortality in 1965 had no relation to when they joined the Medicaid program. Utah who had the lowest infant mortality rate adopted Medicaid at the same time as West Virginia who had the highest infant mortality. A low correlation coefficient across all states confirms that states' infant mortality rates in 1965 did not determine its Medicaid participation.
Systematic migration of would-be mothers of healthy babies into states offering Medicaid is unlikely. Interstate migration flows of a demographic group that would produce the healthiest babies (college-educated persons between the ages 25 to 39) have no relations to States' timing of Medicaid participation. California, an early adopter, and Florida, a late adopter, were among the top recipients of the young, college educated population in the late 1960s (Goworowska and Gardner 2012). Young, single, college-educated people consistently out-migrated from Minnesota and Alabama despite one being an early Medicaid adopter and the other, a late adopter. Furthermore, the magnitudes of these flows are small. Thirteen percent of persons aged 25 to 39 moved to a different state between 1965 and 1970. Out of the thirteen percent, less than thirty percent were college educated.
An increase in births in response to Medicaid availability may also undermine the analytical framework. While the number of births did go up during this period, the fertility rate of women aged 15 to 44 (general fertility rate) declined (Hamilton and Ventura 2006). A more thorough examination of the natality files show no statistically significant changes in births associated with the availability of Medicaid in the mothers' home states.
Results
Research Question 1: Is Medicaid associated with lower infant mortality rates?
I examine the change in infant mortality associated with States' implementation of Medicaid to address my first research question. I calculate the infant mortality rate for each state and year between 1959 and 1979 as follows.
IMRy,s = Number of deaths for infants under age one residing in state s, in year y / 1000 live births to mothers who are residents of state s, in year y
Confirming prior studies (Corman and Grossman 1985; Grossman and Jacobowitz 1981; Lee et al. 1980) the national infant mortality rate shows an accelerated decline during the period after 1965. Mortality levels varied between states and regions (Southern states had relatively higher infant mortality) but this general pattern of decline was consistent throughout the nation.
Figures 1 and 2 examine the mortality decline in relation to states' Medicaid implementation dates. The graphs align the states' infant mortality by their Medicaid start year. Figure 1 descriptively shows faster improvements in infant mortality during the years after Medicaid relative to the years before Medicaid. At the national level, the rate of IMR decline appears to be about 2.5 times greater during the seven years following Medicaid than during the seven years leading up to the program's implementation.
Figure 1. Logged ratio of infant mortality rate surrounding Medicaid start.
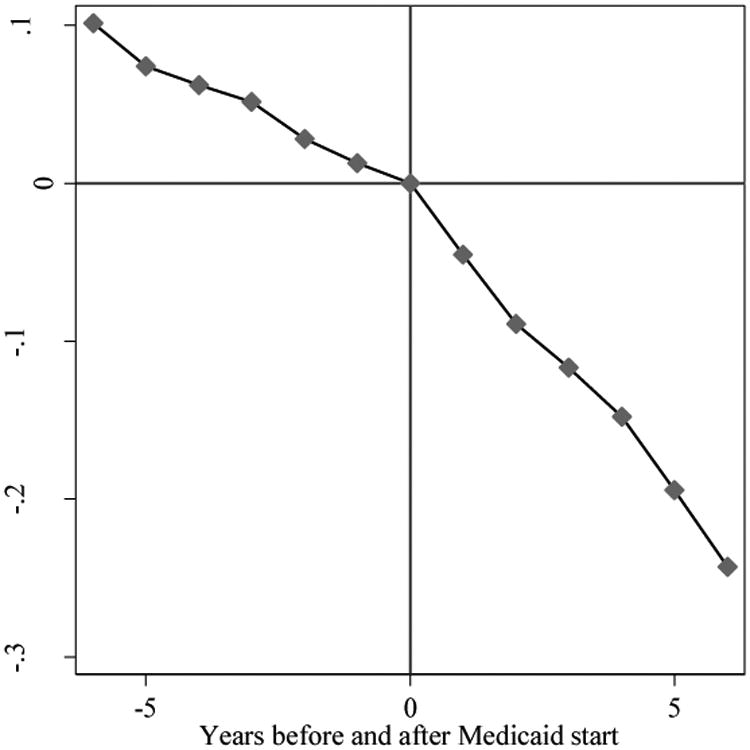
Notes: Year 0 denotes the year prior to Medicaid adoption. Values are average logged ratio of states' infant mortality rates relative to the year immediately prior to Medicaid implementation. Calculations are weighted by the number of births.
Figure 2. Regional variation in infant mortality before and after Medicaid start.
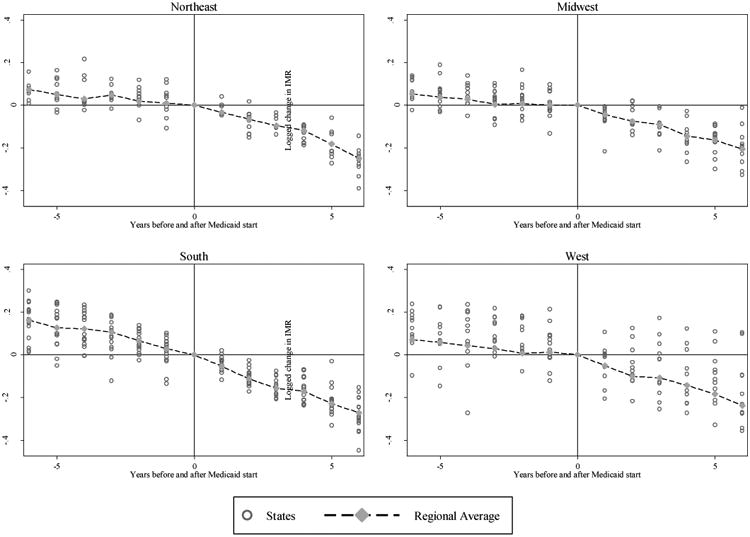
Notes: Year 0 denotes the year prior to Medicaid adoption. Values are average logged ratio of states' infant mortality rates relative to the year immediately prior to Medicaid implementation. Regional averages are weighted by the number of births.
Figure 2 shows the declines in infant mortality surrounding Medicaid for each of the four US regions. Greater change in the rate of decline after Medicaid is particularly pronounced for states in the Northeast and the Midwest.
Table 1 shows the estimated change in infant mortality associated with Medicaid. The first regression shows that states' infant mortality was on average 0.23 deaths per 1000 less after Medicaid start after controlling for the secular decline in infant mortality with year fixed-effects and accounting for interdependence within states. As expected, the magnitude of infant mortality decline associated with national public insurance in the United States is smaller than what has been observed among European countries (Macinko et al 2004). However, this change in infant mortality is not negligible. An increase in 0.23 deaths per 1000 births in 1970 (3.7 million live births) would translate into almost 1,100 more infant deaths.
Table 1. State infant mortality regressed on timing of Medicaid participation.
| Deaths per 1000 | ||
|---|---|---|
|
| ||
| mean | p-value | |
| Medicaid (0/1) | -0.225 | 0.000 |
| Birth Year | ||
| 1959 | (reference) | |
| 1960 | -0.344 | 0.000 |
| 1961 | -1.076 | 0.000 |
| 1962 | -1.079 | 0.000 |
| 1963 | -1.182 | 0.000 |
| 1964 | -1.596 | 0.000 |
| 1965 | -1.691 | 0.000 |
| 1966 | -2.585 | 0.000 |
| 1967 | -3.716 | 0.000 |
| 1968 | -4.077 | 0.000 |
| 1969 | -5.011 | 0.000 |
| 1970 | -5.816 | 0.000 |
| 1971 | -6.745 | 0.000 |
| 1972 | -7.392 | 0.000 |
| 1973 | -8.130 | 0.000 |
| 1974 | -9.123 | 0.000 |
| 1975 | -9.752 | 0.000 |
| 1976 | -10.565 | 0.000 |
| 1977 | -11.694 | 0.000 |
| 1978 | -12.020 | 0.000 |
| 1979 | -12.721 | 0.000 |
| Constant | 26.011 | |
| R-Squared | 0.886 | |
Notes: Regression models have panel-corrected standard errors and are corrected for heteroscedasticity. Estimates are weighted by the number of births in each state during a given a year. Data for New Jersey is missing for 1962 and 1963. Data for Hawaii is missing for years prior to 1968.
Research Question 2: Did the availability of Medicaid at birth have lasting consequences on mortality throughout childhood and into adulthood?
I examine changes in mortality rates in five-year age groups between cohorts born before and cohorts born after Medicaid was implemented in their states at the time of their births. The oldest age group in this analysis is the 36 to 40 age period. I calculate age-specific mortality rates from life tables of cohorts born between 1959 and 1979. I then derive the mortality rates per 100,000 person-years lived for each five-year age period from each birth cohort. 5Mx,sb= (100,000 * deaths in state, s among people born in year, b whose age was between x and x+5) / number of person-years lived in state, s by people born in year, b between ages x and x+5)
Unlike infant mortality, mortality for older age groups did not experience steady and constant declines throughout the 1960s and 70s. In fact, mortality rates appear to increase after 1970 for younger adults (Murphy et al. 2013). Mortality data ends in 2010 when the 1970 birth cohort is 40 years old. Constricted by data limitations and possible confounding effects from later mortality trends, I limit this section of the analysis to the 1959-1970 birth cohorts. All states except Arizona and Alaska had implemented Medicaid by the end of 1970.
In Table 2, I estimate the change in mortality rates (deaths per 100,000 person-years) associated with the availability of Medicaid in the state at time of birth. The regressions also include year fixed-effects with panel corrected standard errors and corrections for heteroscedasticity. Cohorts born after Medicaid implementation showed significant mortality improvements in all age groups except the 20s. Cohorts born after Medicaid adoption had lower mortality rates throughout childhood. Medicaid was associated with 2.03 less deaths per 100,000 person-years between ages 1 and 5. The mortality decline that coincided with Medicaid at birth increased to about 2.52 less per 100,000 person-years for the 11 to 15 age-period and to 3.64 less per 100,000 person-years for the 16 to 20 age-period. All of these coefficients are significant at the 0.001 level. The association between Medicaid at birth and mortality rates during the twenties is not as well defined. The regression model shows that mortality rates associated with the presence of Medicaid at birth is between -0.42 per 100,000 and 0.87 per 100,000 person-years during the 20 to 29 age-period. One explanation for these low coefficients is that the deaths from unintentional injury, homicide, and suicide are particularly high between ages 20 and 29. Mortality rates during this age-period are primarily driven by deaths from injury which may have limited connections to receiving health care in early life. The association between mortality rates and Medicaid at birth becomes stronger in the thirties. Cohorts born after Medicaid had 1.35 less deaths per 100,000 person-years in their early thirties and 3.86 less deaths per 100,000 person-years in their late thirties. HIV and cancer accounted for more deaths than homicide and suicide in the early thirties and cancer and heart disease emerged as two of the top three leading causes of death in the late thirties (CDC).The increasing association between mortality and Medicaid in older age-periods is expected. Prior studies on the consequences of poor health conditions in early life also show stronger outcomes in later adulthood (Almond 2006; Barker and Osmond 1986).
Table 2. States' mortality in five-year age groups regressed on Medicaid availability at birth.
| Age 1-5 | Age 6-10 | Age 11-15 | Age 16-20 | Age 21-25 | Age 26-30 | Age 31-35 | Age 36-40 | |
|---|---|---|---|---|---|---|---|---|
| Medicaid(0/1) | -2.03 | -2.69 | -2.52 | -3.64 | -0.42 | 0.87 | -1.35 | -3.86 |
| Birth Year | ||||||||
| 1959 | (reference) | |||||||
| 1960 | -2.96 | 1.59 | 0.08 | 0.89 | -4.89 | 3.49 | 2.94 | -7.42 |
| 1961 | -3.84 | 0.34 | -1.94 | -0.63 | -6.49 | 4.58 | 0.83 | -13.82 |
| 1962 | -2.74 | 1.45 | -2.84 | -4.55 | -7.19 | 5.80 | -5.29 | -13.11 |
| 1963 | -3.80 | -0.49 | -4.32 | -8.90 | -5.30 | 6.67 | -13.17 | -13.32 |
| 1964 | -7.61 | -0.89 | -5.65 | -12.13 | -4.75 | 7.67 | -22.77 | -13.97 |
| 1965 | -4.33 | -0.96 | -5.01 | -15.14 | 0.80 | 11.37 | -30.45 | -9.87 |
| 1966 | -8.42 | -1.51 | -6.47 | -14.21 | -2.20 | 3.84 | -37.43 | -13.94 |
| 1967 | -10.43 | -3.54 | -8.71 | -14.86 | -4.81 | -3.29 | -41.73 | -17.71 |
| 1968 | -13.58 | -4.09 | -8.88 | -11.21 | -4.59 | -8.91 | -44.00 | -23.25 |
| 1969 | -17.25 | -5.68 | -9.68 | -11.69 | -5.87 | -19.39 | -46.73 | -28.10 |
| 1970 | -20.22 | -6.69 | -10.08 | -10.94 | -7.60 | -27.74 | -49.06 | -31.85 |
| Constant | 91.09 | 39.03 | 46.82 | 116.10 | 123.40 | 131.20 | 178.00 | 209.40 |
| R-Squared | 0.632 | 0.550 | 0.572 | 0.666 | 0.594 | 0.567 | 0.615 | 0.539 |
Notes: Mortality is measured as number of deaths per 100,000 person-years lived in each five-year age range. Regression models have panel-corrected standard errors and corrections for heteroscedasticity. They are also weighted by birth cohort size. Analysis is limited to cohorts born prior to 1971. Data for New Jersey is missing for 1962 and 1963. Data for Hawaii is missing for years prior to 1968. All coefficients have p-values less than 0.001.
The population implications of these mortality declines attributed to Medicaid is not trivial. To illustrate the magnitude of these coefficients, I show how the 1970 birth cohort would look like without the mortality declines associated with Medicaid in these regression models. Table 3 presents the 1970 cohort's under-40 mortality schedule with and without the changes in mortality attributed to Medicaid in Tables 1 and 2. The number of survivors at the beginning of each age group (lx) is based on the actual number of births in the United States in 1970. I apply the age-specific mortality rates with and without the estimated decline associated with Medicaid to the 1970 birth cohort and compare the resulting number of survivors at the end of age 40 in 2010. The coefficients attributed to Medicaid in these regression models amount to 3,532 fewer people alive in 2010. 3,532 people represent a 1.7 percent increase in under-40 mortality for the 1970 cohort and 0.1 percent of all live births in the 1970.
Table 3. Predicted mortality schedules of 1970 birth cohort with and without age-specific mortality changes associated with Medicaid.
| With Medicaid | Without Medicaid | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| x | n | lx | dx | nLx | nmx | nqx | lx | dx | nLx | nmx | nqx |
| 0 | 1 | 3,716,156 | 73,476 | 3,679,418 | 0.0200 | 0.0198 | 3,716,156 | 74,297 | 3,679,008 | 0.0202 | 0.0200 |
| 1 | 5 | 3,642,680 | 12,532 | 18,182,071 | 0.0007 | 0.0034 | 3,641,859 | 12,898 | 18,177,052 | 0.0007 | 0.0035 |
| 6 | 5 | 3,630,148 | 5,397 | 18,137,247 | 0.0003 | 0.0015 | 3,628,962 | 5,883 | 18,130,101 | 0.0003 | 0.0016 |
| 11 | 5 | 3,624,751 | 6,215 | 18,108,216 | 0.0003 | 0.0017 | 3,623,079 | 6,669 | 18,098,722 | 0.0004 | 0.0018 |
| 16 | 5 | 3,618,536 | 18,343 | 18,046,819 | 0.0010 | 0.0051 | 3,616,410 | 18,987 | 18,034,583 | 0.0011 | 0.0053 |
| 21 | 5 | 3,600,192 | 20,712 | 17,949,181 | 0.0012 | 0.0058 | 3,597,423 | 20,770 | 17,935,190 | 0.0012 | 0.0058 |
| 26 | 5 | 3,579,480 | 18,611 | 17,850,874 | 0.0010 | 0.0052 | 3,576,653 | 18,442 | 17,837,159 | 0.0010 | 0.0052 |
| 31 | 5 | 3,560,869 | 22,652 | 17,747,715 | 0.0013 | 0.0064 | 3,558,211 | 22,875 | 17,733,868 | 0.0013 | 0.0064 |
| 36 | 5 | 3,538,217 | 30,616 | 17,614,544 | 0.0017 | 0.0087 | 3,535,336 | 31,268 | 17,598,512 | 0.0018 | 0.0088 |
| 41 | 3,507,601 | 3,504,068 | |||||||||
|
| |||||||||||
| Excess deaths at the end of age 40 for 1970 birth cohort (3,507,601-3,504,068) | 3,532 | ||||||||||
Notes: Life tables use actual number of births in 1970 as the radix. Mortality rates are predicted values from regression results in Tables 1 and 2. nmx for the under 1 age group is the number of deaths per life birth. All other nmx values are calculated as the number of deaths per one person-year lived during the age-period.
Limitations
The first limitation is the analyses' use of state of residence at time of death to determine whether Medicaid was available at birth. The NCHS makes place of birth available only for mortality files between 1979 and 2004 and cannot provide data to create complete life-tables for cohorts born during the key period when Medicaid was rolled out across the states.
I derive age-specific death rates using actual number of deaths by year, age, and state against the cohort's corresponding number of births in the same state. These age-specific death rates inflate from deaths of persons born out-of-state and deflate when the net-migration of people born in those states are below zero. I compare the place of birth against places of death for people who died between 1979 and 2004 to evaluate the potential effects of migration on the results. Ninety five percent of infants who died before turning age one was born in the same state that they died in. This strong relationship between place of birth and death gradually decreases in older age-periods. Over seventy-five percent of children who died in the US were born in the same state. About sixty-two percent of deaths in young adulthood occurred in the states of their birth. Nevada, Wyoming, and New Hampshire were the top three states who had the greatest proportion of deaths by people who were born outside the state. Over 70 percent of deaths between 30 and 39 were from persons born outside of Nevada (the overall percent across all age groups was 48 percent). About fifty percent of younger adults who died in Wyoming and New Hampshire were born out-of-state. Fortunately, the combined deaths from these states made up about one percent of all under-40 deaths in the United States during this period. California, New York, Illinois, Pennsylvania, Texas, and Ohio—all major contributors of under-40 deaths—all had relatively low percentage of deaths by people born out-of-state. The only problematic state was Florida. Florida contributed over five percent of under-40 deaths, thirty percent of which were from people born outside Florida. New York State was the largest state of origin. New York-born persons made up about five percent of under-40 deaths in Florida.
People who were born outside the United States also contributed to deaths in the analyses. Less than one percent of infant deaths were by foreign born infants. The percentage of deaths by foreign-born increased to 5.8 in childhood and then to11 percent in early adulthood. Mexico was the most common place of birth for foreign born people who died in the US particularly for deaths occurring between ages 16 and 30. California and New York had the largest proportion of deaths by persons born outside the 50 states at 16 and 14 percent respectively. Deaths in states other than the state of birth will likely dilute the changes in mortality associated with Medicaid at birth. It is unlikely that migration patterns coincided with the availability of Medicaid at a person's time and place of birth. Thus, the relationship between Medicaid and mortality in this paper, particularly for older age-periods, is likely to be a conservative estimate.
The analyses cannot account for all possible confounding events that occurred during the study period. Between-state differences in abortion laws and availability of family planning services may have influenced the composition of infants born each state (Scrimshaw 1978). The Family Planning Services and Population Research Act under Title X increased federal funding for family planning services through Medicaid in 1972 and in 1973 abortion became legalized after the Supreme Court's decision in Roe v. Wade. These efforts may have reduced the number of unhealthy pregnancies contributing to the decline in infant mortality after the mid-1970s.
Changes in states' economic conditions would also have influenced infant mortality during the study period. In a sensitivity analysis, I categorized the fifty states into “high income growth” and “low income growth” groups. These groups were determined by calculating the slope of each state's per capita personal income growth between 1960 and 1980 (data source: Bureau of Economic Analysis). Parallel difference-in-difference analyses stratified by income growth group confirm that the association between Medicaid and infant mortality decline holds for both low- and high- income growth states. The coefficient sizes were higher for low income growth states, however. This finding suggests that the overall effect of Medicaid may have been stronger in low income growth states where more residents were eligible for public insurance than high income growth states. The relationship between Medicaid and lowered life-course mortality also held consistently among high income growth states across all age groups but not among low income growth states suggesting that the ambiguity in the association between Medicaid at birth and mortality in the early adulthood in the main analyses is driven by the low income growth states.
This study is also limited by the length of its data. The 1970 birth cohort only reached age 40 in 2010 and mortality changes associated with Medicaid could only be examined at relatively young ages. Prior literature suggests that the effects of early-life health environment become more prominent at older ages when mortality rates increase. Similarly, the association between Medicaid availability at birth and adult mortality may become stronger in later years. In this paper, the oldest age-period (36-40) had the strongest association between Medicaid at birth and mortality.
Lastly, the analysis does not distinguish race. Medicaid would have had a greater effect on African Americans as a greater proportion of African American families were recipients of Aid to Families with Dependent Children and thus most likely to be eligible for Medicaid. The poor data quality for the non-white population in the 1950s and 1960s does not produce dependable results when the analyses are separated by race. Many states during this period had very few non-white births and even fewer deaths. Age-specific death rates quickly deteriorate into noisy trends for many smaller states. Furthermore, the NCHS changed the categorization of whites and non-whites several times during this period. Medicaid likely had a greater influence on the non-white population. A greater proportion of African Americans would have been eligible for Medicaid as more African American families were receiving AFDC. Infant mortality among non-whites during this period was also substantially higher and increasing access to medical care may have had a greater impact on infant mortality.
Discussion
Faster declines in infant mortality accompanied the advent of Medicaid in the late 1960s. These improvements that coincided with the federal public insurance program were substantial and its link to population mortality remained significant for decades after its inception. This paper shows that significant declines in infant mortality coincided with states' Medicaid adoption and cohorts who were born after Medicaid had lower mortality throughout their childhoods and adulthoods.
While Medicaid was only available to a subset of the population, changes in mortality were observed at the population level. It is likely to have directly improved the health of the neediest group and raised the average survival rate. It may also have had a positive health impact on women and infants at large by creating conduits for health knowledge to travel from researchers and physicians to the general public. As more women interacted with the medical system and changed their health beliefs and behavior, they reinforced the health knowledge of other women. Medicaid would have enhanced concurrent public health initiative and medical advance to reduce infant mortality. Combined, these factors lead to the large infant mortality improvements observed in the United States in the period after 1965.
The findings of this paper reiterate the significance of conditions in-utero and infanthood on later-life health outcomes. Being born into a state with public health insurance had strong associations with mortality long after cohorts aged out of eligibility. The results find stronger associations between Medicaid at birth and mortality at ages where natural (non-injury) deaths were the leading causes. In the future, cohorts born between 1960 and 1970 will reach older ages where more people will die from natural causes such as heart disease and cancer than from injuries. I expect the relationship between Medicaid at birth and mortality to become stronger.
References
- Almond D. Is the 1918 influenza pandemic over? Long-term effects of in utero influenza exposure in the post-1940 U.S. population. Journal of Political Economy. 2006;114:672–712. [Google Scholar]
- Almond D, Chay K, Lee D. The costs of low birth weight. Quarterly Journal of Economics. 2005;120:1031–1083. [Google Scholar]
- Almond D, Hoynes HW, Schanzenbach DW. Inside the war on poverty: the impact of food stamps on birth outcomes. The Review of Economics and Statistics. 2011;93:387–403. [Google Scholar]
- Andersen R. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen R, Andersen OW. A decade of health services: social survey trends in use and expenditure. Chicago, IL: University of Chicago Press; 1967. [Google Scholar]
- Armstrong G, Conn L, Pinner R. Trends in infectious disease mortality in the United States during the 20th century. JAMA. 1999;281:61–66. doi: 10.1001/jama.281.1.61. [DOI] [PubMed] [Google Scholar]
- Backer TE. Knowledge utilization: the third wave. Knowledge. 1991;12:255–340. [Google Scholar]
- Baldwin LM, Larson EH, Connell FA, Nordlund D, Cain KC, Cawthon ML, Byrns P, Rosenblatt RA. The effect of expanding Medicaid prenatal services on birth outcomes. American Journal of Public Health. 1998;88:1623–1629. doi: 10.2105/ajph.88.11.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJP, Osmond C. Infant mortality, childhood nutrition, and ischaemic heart disease in England and Wales. The Lancet. 1986 May 10;:1077–1081. doi: 10.1016/s0140-6736(86)91340-1. [DOI] [PubMed] [Google Scholar]
- Bisgaier J, Rhodes KV. Auditing access to specialty care for children with public insurance. New England Journal of Medicine. 2011;364:2324–2333. doi: 10.1056/NEJMsa1013285. [DOI] [PubMed] [Google Scholar]
- Boudreaux MH, Golberstein E, McAlpine DD. The long-term impacts of Medicaid exposure in early childhood: Evidence from the program's origin. Journal of Health Economics. 2016;45:161–175. doi: 10.1016/j.jhealeco.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P, Bennett T, Lewis C, Egerter S, Showstack J. Access to prenatal care following major Medicaid eligibility expansions. JAMA. 1993;269(10):1285–1289. [PubMed] [Google Scholar]
- Blumberg LJ, Dubay L, Norton S. Did the Medicaid expansions for children displace private insurance? An analysis using the SIPP. Journal of Health Economics. 2000;19:33–60. doi: 10.1016/s0167-6296(99)00020-x. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. New England Journal of Medicine. 2009;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Maternal and Child Care. Reducing infant mortality: suggested approaches. JAMA. 1965;193:310–319. [PubMed] [Google Scholar]
- Corman H, Grossman M. Determinants of neonatal mortality rates in the U.S.: A reduced form model. Journal of Health Economics. 1985;4:213–236. doi: 10.1016/0167-6296(85)90030-x. [DOI] [PubMed] [Google Scholar]
- Condran GA, Crimmins-Gardner E. Public health measures and mortality in U.S. cities in the late Nineteenth Century. Human Ecology. 1978;6:27–54. doi: 10.1007/BF00888565. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office. CBO's analysis of the major health care legislation enacted in March 2010. Statement of Douglas W Elmendorf before the Subcommittee on Health Committee on Energy and Commerce US House of Representatives 2011 [Google Scholar]
- Copeland GW, Meier KJ. Gaining ground: The impact of Medicaid and WIC on infant mortality. American Politics Research. 1987;15:254–273. doi: 10.1177/004478087015002004. [DOI] [PubMed] [Google Scholar]
- Currie J, Grogger J. Medicaid expansions and welfare contractions: offsetting effects on prenatal care and infant health? Journal of Health Economics. 2002;21:313–335. doi: 10.1016/s0167-6296(01)00125-4. [DOI] [PubMed] [Google Scholar]
- Currie J, Gruber J. Saving babies: The efficacy and cost of recent changes in the Medicaid eligibility of pregnant women. Journal of Political Economy. 1996;104:1263–1296. [Google Scholar]
- Cutler D, Lleras-Muney A, Vogl T. Socioeconomic status and health: dimensions and mechanisms. NBER Working Paper 14333 2008 [Google Scholar]
- Cutler D, Miller G. The role of public health improvements in health advances: The Twentieth-Century United States. Demography. 2005;42:1–22. doi: 10.1353/dem.2005.0002. [DOI] [PubMed] [Google Scholar]
- Daneai GD, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray C, Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David RJ, Siegel E. Decline in neonatal mortality, 1968 to 1977: Better babies or better care? Pediatrics. 1983;71:531–540. [PubMed] [Google Scholar]
- Deaton A, Paxson C. Mortality, education, income, and inequality among American cohorts. In: Wise DA, editor. Themes in the economics of aging. Chicago: University of Chicago Press; 2001. pp. 129–70. [Google Scholar]
- Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs. 2012;31:1673–1679. doi: 10.1377/hlthaff.2012.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaney B, Bilheimer L, Schore J. Medicaid costs and birth outcomes: The effects of prenatal WIC participation and the use of prenatal care. Journal of Policy Analysis and Management. 1992;11:573–592. [PubMed] [Google Scholar]
- Dubay LC, Kenney GM. The effects of Medicaid expansions on insurance coverage of children. The Future of Children. 1996;6:152–161. [PubMed] [Google Scholar]
- Elo I. Social class differentials in health and mortality: patterns and explanations in comparative perspective. Annual Review of Sociology. 2009;35:553–72. [Google Scholar]
- Elo LT, Preston SH. Educational Differentials in Mortality: United States, 1979-1985. Social Science and Medicine. 1996;42:47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Elola J, Daponte A, Navarro V. Health indicators and the organization of health care systems in Western Europe. American Journal of Public Health. 1995;85:1397–1401. doi: 10.2105/ajph.85.10.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewbank DC, Preston SH. Personal health behaviour and the decline in infant and child mortality: The United States, 1900-1930. In: Caldwell J, editor. What we know about health transition: The culture, social and behavioural determinants of health. Vol. 1. Canberra: Australian National University Printing Service; 1990. pp. 116–50. [Google Scholar]
- Falkner FT, editor. Key Issues in Reducing Infant Mortality: Report of a Conference. Washington DC: U.S. Government Printing Office; 1969. [Google Scholar]
- Fix M, Passel JS, Enchautegui ME, Zimmerman W. Immigration and immigrants: Setting the record straight. Washington DC: Urban Institute; 1994. [Google Scholar]
- Fogel RW. The Escape from Hunger and Premature Death, 1700-2100: Europe, America, and the Third World 2004 [Google Scholar]
- Glanz K, Rimer B, Viswanath K. Health behavior and health education: theory, research, and practice. Wiley; 2008. [Google Scholar]
- Goworowska J, Gardner TK. Population Division Working Paper No 94. U.S. Census Bureau; 2012. Historical migration of the young, single, and college educated: 1965 to 2000. [Google Scholar]
- Goodman-Bacon Andrew. Public insurance and mortality: Evidence from medicaid implementation. Journal of Political Economy 2016 [Google Scholar]
- Green L, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual Review of Public Health, 2009. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- Grossman M, Jacobowitz S. Variations in infant mortality rates among counties of the United States: The roles of public policies and programs. Demography. 1981;18:695–713. [PubMed] [Google Scholar]
- Gruber J. Medicaid. In: Moffitt Robert A., editor. Means-tested transfer programs in the United States. National Bureau of Economic Research; 2003. [Google Scholar]
- Guyer B. Medicaid and prenatal care: necessary but not sufficient. JAMA. 1990;264:2264–2265. [PubMed] [Google Scholar]
- Holahan J, Zedlewski S. Expanding Medicaid to cover uninsured Americans. Health Affairs. 1991;10:45–61. doi: 10.1377/hlthaff.10.1.45. [DOI] [PubMed] [Google Scholar]
- Howell EM. The impact of the Medicaid expansions for pregnant women: a synthesis of the evidence. Medical Care Research and Review. 2001;58:3–30. doi: 10.1177/107755870105800101. [DOI] [PubMed] [Google Scholar]
- Hwang A, Hwang M, Xie H, Hardy B, Skaggs B. Access to urologic care for children in California: Medicaid versus private insurance. Urology. 2005;65:170–173. doi: 10.1016/j.urology.2005.01.065. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. What is Medicaid's impact on access to care, health outcomes, and quality of care? Setting the Record Straight on the Evidence. Issue Brief 2013 [Google Scholar]
- Kenney G, Haley J. Why aren't more uninsured children enrolled in Medicaid or SCHIP? Urban Institute; 2001. Series B, No. B-35. [Google Scholar]
- Keife C, Williams D, Greenlund K, Ulene V, Gardin JM, Raczynski JM. Health care access and seven-year change in cigarette smoking: the CARDIA study. American Journal of Preventive Medicine. 1998;15:146–154. doi: 10.1016/s0749-3797(98)00044-0. [DOI] [PubMed] [Google Scholar]
- Lee KS, Paneth N, Gartner LM, Pearlman MA, Gruss L. Neonatal mortality: an analysis of the recent improvement in the United States. American Journal of Public Health. 1980;70:15–21. doi: 10.2105/ajph.70.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Lykens KA, Jargowsky PA. Medicaid matters: children's health and Medicaid eligibility expansions. Journal of Policy Analysis and Management. 2002;21:219–238. doi: 10.1002/pam.10024. [DOI] [PubMed] [Google Scholar]
- Lynch J, Smith DG, Harper S, Hillemeier M, Ross N, Kaplan GA, Wolfson M. Is income inequality a determinant of population health? Part 1. a systematic review. Milbank Quarterly. 2004;82:5–99. doi: 10.1111/j.0887-378X.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macinko JA, Shi L, Starfield B. Wage inequality, the health system, and infant mortality in wealthy industrialized countries, 1970-1996. Social Science and Medicine. 2004;58:279–292. doi: 10.1016/s0277-9536(03)00200-4. [DOI] [PubMed] [Google Scholar]
- Mason J. Reducing infant mortality in the United States through “Healthy Start”. Public Health Report. 1991;106:479–483. [PMC free article] [PubMed] [Google Scholar]
- McDonough JE. Inside National Health Reform. Berkley, CA: University of California Press; 2011. [Google Scholar]
- McKeown T. The modern rise of population. New York: Academic Press; 1976. [Google Scholar]
- McKeown T. Role of medicine: Dream, mirage, or nemesis. Princeton NJ: Princeton University Press; 1979. [Google Scholar]
- Meeker E. The improving health of the United States, 1850-1915. Explorations in Economic History. 1972;10:353–73. [PubMed] [Google Scholar]
- Merrick N, Houchens R, Tillisch S, Berlow B. Quality of hospital care of children with asthma: Medicaid versus privately insured patients. Journal of Health Care for the Poor and Underserved. 2001;12:192–207. doi: 10.1353/hpu.2010.0794. [DOI] [PubMed] [Google Scholar]
- Moss N, Carver K. The effect of WIC and Medicaid on infant mortality in the United States. American Journal of Public Health. 1998;88:1354–1361. doi: 10.2105/ajph.88.9.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Xu J, Kochanek K. National Vital Statistics Reports. US Department of Health and Human Services; 2013. Deaths: Final data for 2010. [PubMed] [Google Scholar]
- Oberg CN, Polich CL. Medicaid: entering the third decade. Health Affairs. 1988;7:83–96. doi: 10.1377/hlthaff.7.4.83. [DOI] [PubMed] [Google Scholar]
- Oreopolous P, Stabile M, Walld R, Roos LL. Short-, medium-, and long-term consequences of poor infant health: An analysis using siblings and twins. The Journal of Human Resources. 2008;43:88–138. [Google Scholar]
- Preston S, Haines M. Fatal years: Child mortality in late Nineteenth-Century America. Princeton, NJ: Princeton University Press; 1991. [Google Scholar]
- Roseboom T, van der Meulen JHP, Ravelli CJ, Osmond C, Barker DJP, Bleker OP. Effects of prenatal exposure to the Dutch famine on adult disease in late life: an overview. Molecular and Cellular Endocrinology. 2001;185:93–98. doi: 10.1016/s0303-7207(01)00721-3. [DOI] [PubMed] [Google Scholar]
- Rowland D, Lyons B, Edwards J. Medicaid: Health care for the poor in the Reagan era. Annual Review of Public Health. 1988;9:427–450. doi: 10.1146/annurev.pu.09.050188.002235. [DOI] [PubMed] [Google Scholar]
- Schor EL, Abrams M, Shea K. Medicaid: Health promotion and disease prevention for school readiness. Health Affairs. 2007:420–429. doi: 10.1377/hlthaff.26.2.420. [DOI] [PubMed] [Google Scholar]
- Scrimshaw SCM. Infant Mortality and Behavior in the Regulation of Family Size. Population and Development Review. 1978;4(3):383. [Google Scholar]
- Shapiro S. New reductions in infant mortality: The challenge of low birth weight. American Journal of Public Health. 1981;71:365–366. doi: 10.2105/ajph.71.4.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro S, Schlesinger ER, Nesbitt REL. Infant, perinatal, maternal and childhood mortality in the United States. Cambridge, MA: Harvard University Press; 1968. [Google Scholar]
- Smith JP. The impact of socioeconomic status on health over the life-course. Journal of Human Resources. 2007;4:739–764. [Google Scholar]
- Szreter S. The importance of social intervention in Britain's mortality decline c.1850-1914: A re-interpretation of the role of public health. Social History of Medicine. 1988;1:1–38. [Google Scholar]
- Tarde G. Laws of Imitation. Gloucester MA: H. Holt; 1962. [Google Scholar]
- Van den Berg GJ, Lindeboom M, Portrait F. Economic conditions early in life and individual mortality. American Economic Review. 2006;96:290–302. doi: 10.1257/000282806776157740. [DOI] [PubMed] [Google Scholar]
- Wang E, Choe M, Meara J, Koempel J. Inequality of access to surgical specialty health care: why children with government-funded insurance have less access than those with private insurance in Southern California. Pediatrics. 2004;114:584–590. doi: 10.1542/peds.2004-0210. [DOI] [PubMed] [Google Scholar]
- Wherry LR, Meyer BD. Saving Teens: Using a Policy Discontinuity to Estimate the Effects of Medicaid Eligibility. Journal of Human Resources 2015 [Google Scholar]
- Wherry L, Miller S, Kaestner R, Meyer B. NBER Working Paper Series. Cambridge, MA: 2015. Childhood Medicaid Coverage and Later Life Health Care Utilization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilensky G, Berk ML. Health care, the poor, and the role of Medicaid. Health Affairs. 1982;1:93–100. doi: 10.1377/hlthaff.1.4.93. [DOI] [PubMed] [Google Scholar]


