Abstract
Objective
We aimed to estimate risk of recurrent overdose associated with psychosocial assessment by psychiatrists during hospitalization for nonfatal overdose and prescribing patterns of psychotropic medications after discharge.
Methods
A retrospective cohort study was conducted using a nationwide claims database in Japan. We classified patients aged 19–64 years hospitalized for nonfatal overdose between October 2012 and September 2013 into two cohorts: 1) those who had consulted a psychiatrist prior to overdose (n=6,790) and 2) those who had not (n=4,950). All patients were followed up from 90 days before overdose until 365 days after discharge.
Results
Overall, 15.3% of patients with recent psychiatric treatment had a recurrent overdose within 365 days, compared with 6.0% of those without psychiatric treatment. Psychosocial assessment during hospital admission had no significant effect on subsequent overdose, irrespective of treatment by psychiatrists before overdose. There was a dose–response relationship for the association of benzodiazepine prescription after overdose with subsequent overdose in either cohort, even after accounting for average daily dosage of benzodiazepines before overdose and other confounders. In patients with recent psychiatric treatment, the cumulative proportion of recurrent overdose at 365 days was 27.7% for patients receiving excessive dosages of benzodiazepines, 22.0% for those receiving high dosages, 15.3% for those receiving normal dosages, and 7.6% for those receiving no benzodiazepines. In patients without psychiatric treatment, the cumulative proportion of recurrent overdose at 365 days was 24.3% for patients receiving excessive dosages of benzodiazepines, 18.0% for those receiving high dosages, 9.0% for those receiving normal dosages, and 4.1% for those receiving no benzodiazepines.
Conclusion
Lower dose of benzodiazepines after overdose is associated with lower risk of subsequent overdose.
Keywords: drug poisoning, self-harm, suicide attempt, repeater, consultation–liaison service, administrative database
Introduction
Admission for nonfatal overdose is a good opportunity to identify and refer patients who are at risk of suicide or drug abuse.1 Clinical practice guidelines recommend that a psychosocial assessment, including an evaluation of risk factors for current and subsequent self-harm, be offered to all patients admitted for self-harm, many of whom have overdosed themselves.2,3 Psychiatrists and/or mental health nurses typically perform these assessments.4
However, the potential benefits of these psychosocial assessments in real-world settings for patients admitted due to overdose are unknown. Some studies found a protective effect of psychosocial assessment on recurrent self-harm,5–10 but others failed to show an association.11–13 These inconsistent results may be due to the failure to evaluate effect modification by treatment by psychiatrists before overdose.
In addition, to date, little research has focused on the effect of prescribing patterns after nonfatal overdose on recurrent overdose.1 Psychotropic medications are one of the most frequently ingested substances for overdose, whereas opioid medications are rarely ingested in Japan.14–16 Among psychotropic medications, previous studies have suggested that daily dosage of benzodiazepine increased the risk of incident overdose.15,17 However, this association between prescribing patterns of psychotropic medications and recurrent overdose is unknown.
Therefore, we aimed to estimate the risk of recurrent overdose associated with psychosocial assessment by psychiatrists during hospitalization for nonfatal overdose and prescribing patterns of psychotropic medications after discharge, using two cohorts of patients in Japan stratified by treatment by psychiatrists before overdose. We also determined the effect of psychosocial assessment on the continuity of post-discharge psychiatric care. We hypothesized that psychosocial assessment during hospitalization for overdose would have a greater benefit in patients not treated by psychiatrists before admission than in those treated.
Methods
Data source
We conducted a 1-year cohort study using the National Database of Health Insurance Claim Information and Specified Medical Checkups (NDB). The study design and sample characteristics have been described elsewhere.18 The NDB includes all claims submitted electronically from 99% of hospitals in Japan,19 a country with a population of 126 million.20 The NDB captures almost all patients who received medical care services under the universal health insurance system.21 The claims include clinical and procedural information such as a patient identification number (generated from the insurance identification number, birth date, and sex), an institution identification number, sex, age, date of admission, date of discharge, drug codes, procedural codes, and diagnosis codes. Our study was reviewed and approved by the institutional review board at the Institute for Health Economics and Policy (H26-002). The ethical guideline in Japan (Ethical Guidelines for Medical and Health Research Involving Human Subjects) waives the requirement for informed consent when researchers use only anonymous data.
Patient selection
We included all overdose episodes among 19- to 64-year-old patients who were admitted to a Japanese medical facility between October 2012 and September 2013. Overdose was defined as a definitive diagnosis of drug poisoning at hospital admission (T360–T509 in the International Classification of Diseases [ICD]-10 codes). Although we intended to focus on intentional overdose rather than unintentional overdose, we included all types of overdose (ie, intentional, unintentional, and undetermined intent) as in previous studies.22–24 This was done for several reasons. First, the delineation of the intention behind overdose is often difficult and overlaps substantially.22 Second, the number of admissions for intentional overdose is much higher than that for unintentional overdose with the exception of children and elderly population.25 Third, data on external causes (ICD-10 codes: V01–Y98) were not recorded in the NDB.
To increase the likelihood that the overdose was intentional, we excluded patients who were diagnosed with overdose after hospital admissions as well as patients aged >64 years. We also excluded patients aged <19 years because adolescents are less likely to overdose on prescription drugs than adults. The initial episodes between October 2012 and September 2013 were defined as the “index episode”. An overdose episode was defined as the period from the date of admission for overdose to the date of discharge to home or the occurrence of in-hospital death. To maximize the homogeneity of suicidal risk between patients with and without psychosocial assessment, we excluded patients who were admitted to psychiatric wards, including 1) those who were transferred from the hospitals where overdose was treated to other psychiatric hospitals; 2) those who were treated for overdose in intensive care units/general wards, then transferred to psychiatric wards in the same medical facility, and discharged home without transfer to other psychiatric hospitals; and 3) those who were treated for overdose in psychiatric wards, then received treatment from psychiatrists in the same units, and discharged home. Patients who survived the index episodes were followed up from 90 days before the admission date until 365 days after the discharge date of the index episode. We created two study cohorts: one included patients who were treated by a psychiatrist at least once before the index episode (psychiatrist cohort) and the other included patients who were not treated by a psychiatrist before the index episode (no-psychiatrist cohort). The look-back period of 90 days was defined according to a previous study.15
Outcomes
The primary outcome was time to recurrent overdose within 365 days after the discharge date for the index episode. The subsequent overdose admission to an inpatient or outpatient facility was defined as the “recurrent episode”. Overdose admissions that occurred within 1 day after the discharge date were excluded to avoid counting inter-hospital transfers. Time zero was the date of discharge, and observations were censored at in-hospital death or the end of the follow-up period.
The secondary outcome was time to termination of continuous psychiatric care within 365 days after the discharge date for the index episode. Initiation of psychiatric care after overdose was defined as treatment by a psychiatrist within 28 days after the discharge date. The continuity of psychiatric care was defined as psychiatric care at least once every 28 days. To account for holidays, up to a 14-day delay between two consecutive visits was considered continuous psychiatric care. The time to psychiatric care discontinuation was the date of the last visit plus 28 days among patients who initiated and discontinued psychiatric care. The time to psychiatric care discontinuation was set to 1 day among patients who did not initiate psychiatric care. Time zero was the date of discharge, and observations were censored at recurrent overdose, in-hospital death, or the end of the follow-up period.
Primary time-invariant and time-varying variables
Psychosocial assessment conducted by psychiatrists during the index episode was the primary time-invariant variable. The psychosocial assessment group included patients who were treated for overdose in intensive care units or general wards, then received treatments from psychiatrists in the same units, and were discharged home without transfer to psychiatric wards in the same or other hospitals. Psychiatrists were supposed to carry out a comprehensive assessment of the needs and risk and arrange discharge care for patients with overdose. The no-psychosocial assessment group included patients who were treated for overdose in intensive care units or general wards, then received no treatments from psychiatrists during the index episode, and were discharged home.
Usage, including daily dosage, of psychotropic medications after the index episode was analyzed as time-varying variables. We identified all prescriptions for 97 psychotropic medications, including benzodiazepines, barbiturates, antidepressants, antipsychotics, and stabilizers (Table S1). Daily dosages for benzodiazepines, antidepressants, and antipsychotics were calculated using established conversion tables.26 Daily benzodiazepine dosage, expressed in diazepam equivalents, was categorized as none (0 mg), normal (>0 to ≤15 mg), high (>15 to ≤30 mg), and excessive (>30 mg). Daily antidepressant dosage, expressed in imipramine equivalents, was categorized as none (0 mg), normal (>0 to ≤300 mg), and high (>300 mg). Daily antipsychotic dosage, expressed in chlorpromazine equivalents, was categorized as none (0 mg), normal (>0 to ≤450 mg), and high (>450 mg). These daily dosage categorizations were based on the package inserts and previous studies.15,27 The cutoff values of normal/high dosage were defined by the maximum recommended daily dosage in the package inserts. The cutoff value of high/excessive dosage for benzodiazepines was defined by the twofold greater value of the maximum recommended daily dosage in the package inserts. Daily dosage was set to none from the first day after the discharge date of the index episode until the date of the first prescription for psychotropic medications after the overdose. To account for the delay incurred by refilling, we allowed a 7-day grace period between two consecutive prescriptions (eg, between “the date of first prescription plus number of days supplied” and “the date of the second prescription”). Daily prescription status for barbiturates and stabilizers was also assessed in the same manner.
Other variables
We obtained demographic (age and sex), clinical (number of chronic conditions and diagnostic history of borderline personality disorder, substance use disorders, and overdose), and procedural (psychotropic prescriptions before index episode and length of stay) variables before and during the index episode. These variables are listed in Table S2 and were selected as potential confounders according to evidence from previous studies.1,22,23 To assess the number of chronic conditions, we identified diagnostic history of 17 chronic conditions, such as myocardial infarction, congestive heart failure, and peripheral vascular disease, defined in the Charlson’s comorbidity index.28 We also identified diagnostic history of borderline personality disorder (ICD-10 code: F603), substance use disorders (ICD-10 codes: F10–F16 and F18–F19), and overdose (ICD-10 codes: T360–T509). We obtained data on average daily dosage of psychotropic medications within 60 days before the index episode and the length of stay during the index episode.
Statistical analyses
All analyses were conducted separately for the psychiatrist cohort and the no-psychiatrist cohort, according to the hypothesis that psychosocial assessment during hospital admission might have a different benefit depending on the treatment by psychiatrists before overdose. Descriptive statistics were calculated for the basic demographic, clinical, and procedural variables. Average daily dosage and prescription of psychotropic medications were described for the following three periods as in the previous study:1 60 days before the admission date of the index episode, days 31–90 after the discharge date of the index episode, and days 91–365 after the discharge date of the index episode. Kaplan–Meier event curves with 95% confidence intervals (CIs) for the primary and secondary outcomes were constructed by treatment patterns before and after discharge. Risk differences (RDs) were calculated by subtracting the cumulative risk of the outcomes at 365 days after discharge in the exposed group from that in the unexposed group. Cox proportional hazard models with time-varying covariates were used to assess the hazard of recurrent overdose and termination of continuous psychiatric care, expressed as hazard ratios (HRs) with 95% CIs. All variables listed in Table S3 were simultaneously entered into the models. The Cox models allowed us to adjust for a number of potential confounders, such as average daily dosage of benzodiazepines before overdose and barbiturate prescriptions before overdose. Instead of nonusers, normal-dose users were used as a reference group for daily dosages of benzodiazepines, antidepressants, and antipsychotics to demonstrate the relative effect of high-dose vs normal-dose users. Significance levels were set at 5% for all analyses. All data were analyzed using R version 3.2.2.
Results
Patients with recent psychiatric treatment
In the psychiatrist cohort, a total of 6,790 patients were eligible for analysis (Figure S1). Among this cohort, 48.1% were aged 19–34 years, 77.0% were women, 44.0% had a history of chronic conditions, 9.4% had an overdose history, and 28.7% received the psychosocial assessment (Table S2).
Before the overdose, benzodiazepines were the most frequently prescribed (93.8%) psychotropic medication, followed by antidepressants (66.9%), antipsychotics (59.5%), mood stabilizers (32.2%), and barbiturates (14.9%) (Table 1). A high or excessive dose of benzodiazepines was prescribed to 47.1% of patients before the overdose and 33.3% on days 91–365 after the overdose. Barbiturates were prescribed to 14.9% of patients before the overdose and 12.4% on days 91–365 after the overdose. A high dose of antidepressants was prescribed to <5% of patients.
Table 1.
Prescription patterns before and after initial overdose in cohorts with and without prior psychiatric treatment
| Psychotropic prescriptions | Psychiatrist cohort, n (%)
|
No-psychiatrist cohort, n (%)
|
||||
|---|---|---|---|---|---|---|
| 60 days before overdose (n=6,790) |
Days 31–90 after overdose (n=6,533) |
Days 91–365 after overdose (n=6,282) |
60 days before overdose (n=4,950) |
Days 31–90 after overdose (n=4,850) |
Days 91–365 after overdose (n=4,785) |
|
| Benzodiazepinesa | ||||||
| None (0 mg) | 419 (6.2) | 1,302 (19.9) | 1,532 (24.4) | 3,518 (71.1) | 3,247 (66.9) | 3,104 (64.9) |
| Normal (>0 to ≤15 mg) | 3,172 (46.7) | 2,647 (40.5) | 2,657 (42.3) | 1,114 (22.5) | 1,237 (25.5) | 1,362 (28.5) |
| High (>15 to ≤30 mg) | 1,807 (26.6) | 1,457 (22.3) | 1,250 (19.9) | 190 (3.8) | 225 (4.6) | 197 (4.1) |
| Excessive (>30 mg) | 1,392 (20.5) | 1,127 (17.3) | 843 (13.4) | 128 (2.6) | 141 (2.9) | 122 (2.5) |
| Barbiturates | 1,012 (14.9) | 762 (11.7) | 776 (12.4) | 136 (2.7) | 144 (3.0) | 144 (3.0) |
| Antidepressantsb | ||||||
| None (0 mg) | 2,250 (33.1) | 2,975 (45.5) | 2,892 (46.0) | 4,447 (89.8) | 4,061 (83.7) | 3,938 (82.3) |
| Normal (>0 to ≤300 mg) | 4,217 (62.1) | 3,325 (50.9) | 3,194 (50.8) | 484 (9.8) | 766 (15.8) | 827 (17.3) |
| High (>300 mg) | 323 (4.8) | 233 (3.6) | 196 (3.1) | 19 (0.4) | 23 (0.5) | 20 (0.4) |
| Antipsychoticsc | ||||||
| None (0 mg) | 2,747 (40.5) | 2,841 (43.5) | 2,684 (42.7) | 4,648 (93.9) | 4,257 (87.8) | 4,143 (86.6) |
| Normal (>0 to ≤450 mg) | 3,327 (49.0) | 3,010 (46.1) | 2,978 (47.4) | 275 (5.6) | 545 (11.2) | 591 (12.4) |
| High (>450 mg) | 716 (10.5) | 682 (10.4) | 620 (9.9) | 27 (0.5) | 48 (1.0) | 51 (1.1) |
| Stabilizers | 2,188 (32.2) | 1,898 (29.1) | 1,985 (31.6) | 272 (5.5) | 379 (7.8) | 419 (8.8) |
Notes:
Daily dosage expressed in diazepam equivalents.
Daily dosage expressed in imipramine equivalents.
Daily dosage expressed in chlorpromazine equivalents.
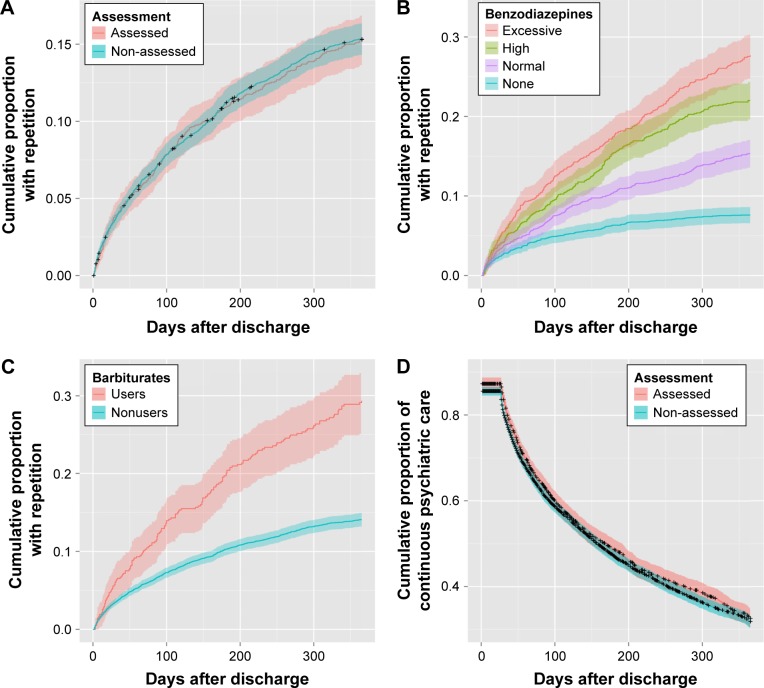
During the follow-up period of 365 days, there were 1,038 patients with recurrent overdose (15.3% [95% CI: 14.5%–16.2%]), of which 483 (46.5%) were re-admitted to the same hospital as in the index episode. Psychosocial assessment did not significantly decrease the risk of recurrent overdose (HR =0.97, 95% CI: 0.84–1.11; RD =0.0%; Table 2; Figure 1A). A dose–response relationship was found between daily dosages of benzodiazepines after overdose and recurrent overdose (Table 2; Figure 1B). The risk of recurrent overdose was lower among nonusers of benzodiazepines than in normal-dose users of benzodiazepines (HR =0.53, 95% CI: 0.42–0.66; 7.6% vs 15.3%; RD =−7.7%), and the risk was higher among high-dose users (HR =1.41, 95% CI: 1.17–1.71; 22.0% vs 15.3%; RD =6.7%) and excessive-dose users (HR =1.61, 95% CI: 1.30–2.00; 27.7% vs 15.3%; RD =12.4%). Prescription of barbiturates increased the risk of recurrent overdose (HR =1.42, 95% CI: 1.11–1.81; RD =15.2%; Table 2; Figure 1C). Patients who took a high dosage of antidepressants were more likely to have a recurrent overdose, although the estimates were unstable due to a wide CI (Table 2; Figure S2A). Prescription of antipsychotics and stabilizers did not have a significant effect on recurrent overdose (Table 2; Figure S2).
Table 2.
Cox proportional hazard models evaluating risk factors for recurrent overdose and termination of continuous psychiatric care after overdosea
| Characteristics | Psychiatrist cohort (n=6,790)
|
No-psychiatrist cohort (n= 4,950)
|
||
|---|---|---|---|---|
| HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | |
| Psychosocial assessmentb | ||||
| Assessed | 0.97 (0.84, 1.11) | 0.96 (0.89, 1.03) | 0.95 (0.73, 1.24) | 0.75 (0.71, 0.81)* |
| Non-assessed | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Benzodiazepinesc,d | ||||
| None (0 mg) | 0.53 (0.42, 0.66)* | 3.27 (2.95, 3.63)* | 0.40 (0.27, 0.61)* | 2.38 (2.03, 2.79)* |
| Normal (>0 to ≤15 mg) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| High (>15 to ≤30 mg) | 1.41 (1.17, 1.71)* | 1.13 (0.99, 1.28) | 1.75 (1.11, 2.77)* | 1.05 (0.80, 1.37) |
| Excessive (>30 mg) | 1.61 (1.30, 2.00)* | 1.00 (0.86, 1.17) | 1.75 (0.94, 3.26) | 1.13 (0.79, 1.63) |
| Barbituratesc | ||||
| Nonusers | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Users | 1.42 (1.11, 1.81)* | 0.99 (0.81, 1.21) | 1.43 (0.73, 2.80) | 1.56 (0.93, 2.64) |
| Antidepressantsc,e | ||||
| None (0 mg) | 0.99 (0.84, 1.17) | 2.45 (2.23, 2.70)* | 1.10 (0.73, 1.68) | 3.00 (2.50, 3.60)* |
| Normal (>0 to ≤300 mg) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| High (>300 mg) | 1.48 (1.05, 2.07)* | 1.00 (0.77, 1.31) | 1.36 (0.43, 4.31) | 1.55 (0.73, 3.29) |
| Antipsychoticsc,f | ||||
| None (0 mg) | 0.91 (0.76, 1.09) | 2.09 (1.88, 2.31)* | 0.81 (0.49, 1.35) | 2.04 (1.67, 2.48)* |
| Normal (>0 to ≤450 mg) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| High (>450 mg) | 1.05 (0.80, 1.36) | 0.82 (0.68, 0.98)* | 2.38 (1.28, 4.42)* | 1.00 (0.60, 1.67) |
| Stabilizersc | ||||
| Nonusers | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Users | 1.09 (0.89, 1.34) | 0.57 (0.51, 0.65)* | 1.09 (0.69, 1.71) | 0.70 (0.55, 0.89)* |
Notes:
Covariates simultaneously entered into the models: age, sex, number of chronic conditions, borderline personality disorder, substance use disorder, overdose history, psychotropic prescriptions before index episode, and length of stay.
Psychosocial assessment by psychiatrists during index episode was entered in the models as a fixed covariate.
Psychotropic prescriptions after the index episode were entered in the model as time-varying covariates.
Daily dosage expressed in diazepam equivalents.
Daily dosage expressed in imipramine equivalents.
Daily dosage expressed in chlorpromazine equivalents.
P<0.05.
Abbreviations: HR, hazard ratio; CI, confidence interval.
Figure 1.
Cumulative proportion of primary and secondary outcomes by treatment patterns before and after discharge in the psychiatrist cohort (n=6,790).
Notes: Solid line represents Kaplan–Meier event curve, and shaded area represents the 95% confidence interval. (A) Overdose repetition by psychosocial assessment, (B) overdose repetition by benzodiazepine prescription, (C) overdose repetition by barbiturate prescription, and (D) continuity of psychiatric care by psychosocial assessment.
Psychosocial assessment did not significantly decrease the risk of psychiatric care discontinuation (HR =0.96, 95% CI: 0.89–1.03; RD =−0.7%; Table 2; Figure 1D). The proportion of patients receiving psychiatric care in the assessed group decreased from 87.3% at 28 days to 32.6% at 365 days, and the range of these proportions in the non-assessed group decreased from 85.6% to 31.9% (Figure 1D).
Patients without recent psychiatric treatment
In the no-psychiatrist cohort, a total of 4,950 patients were eligible for analysis (Figure S1). The prevalence of psychotropic medication prescriptions before the index overdose was much lower in the no-psychiatrist cohort than in the psychiatrist cohort (Table 1).
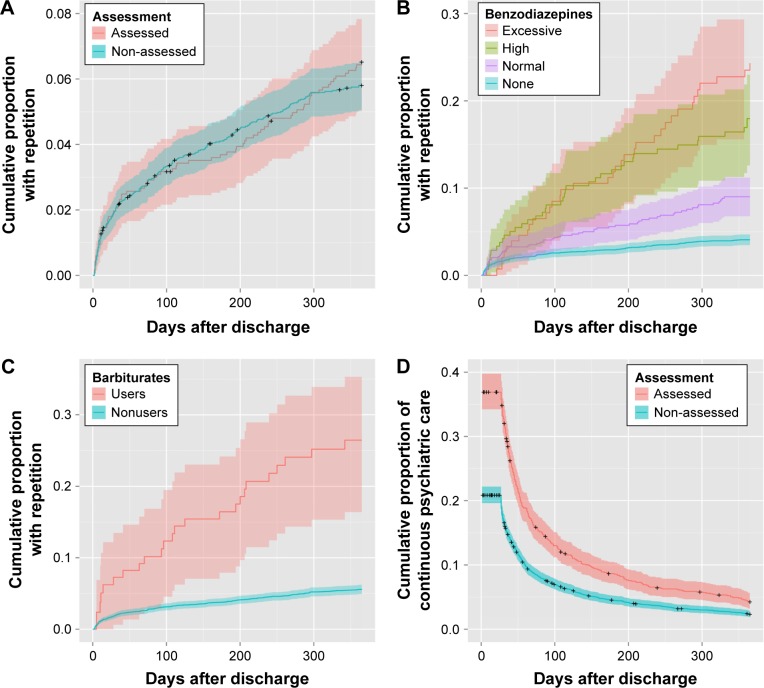
During the follow-up period of 365 days, there were 295 patients with recurrent overdose (6.0% [95% CI: 5.3%–6.6%]), of which 149 (50.5%) were re-admitted to the same hospital as in the index episode. Similar to the results from the psychiatrist cohort, psychosocial assessment did not significantly decrease the risk of recurrent overdose in the no-psychiatrist cohort (HR =0.95, 95% CI: 0.73–1.24; RD =0.7%; Table 2; Figure 2A). The risk of recurrent overdose was lower among nonusers than in normal-dose users of benzodiazepines (HR =0.40, 95% CI: 0.27–0.61; 4.1% vs 9.0%; RD =−4.9%) and higher among high-dose users (HR =1.75, 95% CI: 1.11–2.77; 18.0% vs 9.0%; RD =9.0%) and excessive-dose users (HR =1.75, 95% CI: 0.94–3.26; 24.3% vs 9.0%; RD =15.3%) (Table 2; Figure 2B). The proportion of barbiturate prescriptions was relatively small (~3% patients), resulting in an unstable estimate (HR =1.43, 95% CI: 0.73–2.80; RD =20.9%; Figure 2C).
Figure 2.
Cumulative proportion of primary and secondary outcomes by treatment patterns before and after discharge in the no-psychiatrist cohort (n=4,950).
Notes: Solid line represents Kaplan–Meier event curve, and shaded area represents the 95% confidence interval. (A) Overdose repetition by psychosocial assessment, (B) overdose repetition by benzodiazepine prescription, (C) overdose repetition by barbiturate prescription, and (D) continuity of psychiatric care by psychosocial assessment.
Unlike the findings from the psychiatrist cohort, psychosocial assessment had a significantly decreased risk of psychiatric care discontinuation in the no-psychiatrist cohort (HR =0.75, 95% CI: 0.71–0.81; RD =−1.9%; Table 2; Figure 2D). The proportion of psychiatric care in the assessed group decreased from 36.9% at 28 days to 4.2% at 365 days; however, in the non-assessed group, this number decreased from 20.9% to 2.3% (Figure 2D).
Discussion
This is the first study to evaluate the effectiveness of treatment patterns before and after discharge in patients hospitalized for nonfatal overdose. We found that there was a dose–response relationship for the association of benzodiazepine prescription after overdose with subsequent overdose, even after accounting for average daily dosage of benzodiazepines before overdose and other confounders. Our findings are consistent with those of a previous study, which detected a strong association between opioid dosage after a nonfatal opioid overdose and risk of subsequent opioid overdose.1 The present study extends the previous study by not limiting patients to those with opioid overdose.1 Because multidrug overdose is common in patients hospitalized with overdose, it makes sense to use a broader definition of overdose. Our findings also add to the literature by demonstrating that prescribing barbiturates after overdose was associated with subsequent overdose.15 These results suggest that initiation of benzodiazepine and/or barbiturate reduction strategies after overdose might have a protective effect on recurrent overdose. Patients with nonfatal overdose may benefit from the strategies such as gradual dose-tapering with structured education, written self-help instructions, and cognitive behavioral therapy.29
We found that psychosocial assessment during hospital admission had no significant effect on subsequent overdose, irrespective of treatment by psychiatrists before overdose. Although a direct comparison with previous studies is difficult because of differences in definitions of patients, exposures, and outcomes,5,7–13 our findings are inconsistent with those of Kanehara et al,6 who found that psychosocial assessment was associated with a 21% decreased risk of re-hospitalization to the same hospital using almost the same definitions of patients and exposures as in our study. One possible explanation for the discrepancy is that the outcome in the previous study may have had a low positive predictive value for overdose admission to any hospitals, which may have induced misclassification bias.6 Indeed, our analyses showed that ~50% patients were re-admitted to the same hospital as in the index episode. In addition, our findings provide evidence that psychosocial assessment was associated with a 25% decreased risk of psychiatric care discontinuation after overdose only in the cohort of patients without recent psychiatric treatment. This supports our hypothesis that psychosocial assessment has greater benefit in patients without psychiatric treatment before overdose than in those who had psychiatric treatment.
We found that most patients did not receive continuous care by psychiatrists as time passed after overdose. Even in the cohort of patients with recent psychiatric treatment, the proportion of patients receiving psychiatric care markedly decreased from 85% soon after discharge to 32% at 365 days after overdose. Previous studies reported that 43%–50% of discharged patients received follow-up psychiatric care soon after discharge.30,31 Our study extends previous findings by showing a decreasing trend across time in the proportion of patients receiving continuous psychiatric care. These results suggest the need for active outreach. Interventions that include active contact and follow-up via postcard and/or telephone may decrease the risk of recurrent overdose.32,33
Strengths and limitations
Our study had several strengths. First, we studied a large and representative sample of almost all patients hospitalized for overdose in Japan. Second, we had detailed information on prescribed psychotropic medications before and after overdose. Third, we could explicitly define time to recurrent overdose as the period between the discharge date of the index episode and the date of the subsequent overdose admission to inpatient and outpatient facilities.
Our study had several limitations. First, we cannot draw conclusion regarding the underlying mechanisms of the association between treatment patterns after discharge and subsequent overdose. Use of benzodiazepines and barbiturates may lead to behavioral disinhibition, whereas patients at sustained risk of suicide even after discharge are more likely to be prescribed a drug with more sedative effects. Second, the rate of recurrent overdose in the present study might be underestimated because of the traceability problem in the database. Namely, we could not identify those who did not continue to enroll in the same health insurance. Third, we were unable to identify patients who completed suicide by overdose without any treatments and those who attempted suicidal behaviors that were not related to drug overdose. Fourth, we were unable to distinguish unintentional overdose from intentional overdose, because we used the claims database in which data on external causes (ICD-10 codes: V01–Y98) were not recorded in Japan. Fifth, we focused only on patients hospitalized with nonfatal overdose and those who were without transfers to psychiatric wards, which may limit the generalizability of our findings to nearly lethal methods of self-harm, such as hanging and jumping. Future research should focus on patients who require transfer to psychiatric hospitals/wards to confirm the effects of psychosocial assessment.
Conclusion
Our study indicated that higher benzodiazepine dosage after nonfatal overdose had an increased risk of recurrent overdose and that the proportion of patients with psychiatric care decreased as time passed after overdose. These findings suggest that admissions for nonfatal overdose are a potential opportunity to identify patients who are at risk of subsequent overdose and who require continuous psychiatric care.
Supplementary materials
Flow diagram of patients included in both cohorts and reasons for exclusion.
Cumulative proportion of overdose repetition by treatment patterns before and after discharge.
Notes: Solid line represents Kaplan–Meier event curve, and shaded area represents the 95% confidence interval. (A) Antidepressants in psychiatrist cohort, (B) antipsychotics in psychiatrist cohort, (C) stabilizers in psychiatrist cohort, (D) antidepressants in no-psychiatrist cohort, (E) antipsychotics in no-psychiatrist cohort, and (F) stabilizers in no-psychiatrist cohort.
Table S1.
Complete list of psychotropic medications included in the covariate assessment
| Drugs | Drugs |
|---|---|
| Benzodiazepines | Antidepressants |
| Alprazolam | Maprotiline |
| Bromazepam | Mianserin |
| Brotizolam | Milnacipran |
| Chlordiazepoxide | Mirtazapine |
| Clobazam | Nortriptyline |
| Clonazepam | Paroxetine |
| Clorazepate dipotassium | Sertraline |
| Clotiazepam | Setiptiline |
| Cloxazolam | Sulpirideb |
| Diazepam | Trazodone |
| Estazolam | Trimipramine |
| Eszopiclone | Antipsychotics |
| Ethyl loflazepate | Aripiprazole |
| Etizolam | Blonanserin |
| Fludiazepam | Bromperidol |
| Flunitrazepam | Carpipramine |
| Flurazepam | Chlorpromazine |
| Flutazolam | Chlorpromazine–promethazine–phenobarbitala |
| Flutoprazepam | Clocapramine |
| Haloxazolam | Clozapine |
| Lorazepam | Fluphenazine |
| Lormetazepam | Haloperidol |
| Medazepam | Haloperidol decanoate |
| Mexazolam | Levomepromazine |
| Nimetazepam | Mosapramine |
| Nitrazepam | Nemonapride |
| Oxazolam | Olanzapine |
| Quazepam | Oxypertine |
| Rilmazafone | Paliperidone |
| Tofisopam | Paliperidone palmitate |
| Triazolam | Perospirone |
| Zolpidem | Perphenazine |
| Zopiclone | Pimozide |
| Barbiturates | Pipamperone |
| Amobarbital | Prochlorperazine |
| Barbital | Propericiazine |
| Chlorpromazine–promethazine–phenobarbitala | Quetiapine |
| Pentobarbital calcium | Reserpine |
| Phenobarbital | Risperidone |
| Phenobarbital sodium | Spiperone |
| Phenytoin–phenobarbital | Sulpirideb |
| Secobarbital sodium | Sultopride |
| Antidepressants | Tiapride |
| Amitriptyline | Timiperone |
| Amoxapine | Trifluoperazine |
| Clomipramine | Zotepine |
| Dosulepin | Stabilizers |
| Duloxetine | Carbamazepine |
| Escitalopram | Lamotrigine |
| Fluvoxamine | Lithium |
| Imipramine | Valproate |
| Lofepramine |
Notes:
Chlorpromazine–promethazine–phenobarbital combined was double-counted as both a barbiturate and an antipsychotic.
Sulpiride of <300 or ≥300 mg/day was counted as an antidepressant or an antipsychotic, respectively.
Table S2.
Characteristics of cohort that did and did not have psychiatric treatment before overdose
| Characteristics | Treatment by psychiatrists before index episode, n (%)
|
|
|---|---|---|
| Psychiatrist cohort (n=6,790) | No-psychiatrist cohort (n=4,950) | |
| Age, years | ||
| 19–34 | 3,267 (48.1) | 2,263 (45.7) |
| 35–49 | 2,561 (37.7) | 1,541 (31.1) |
| 50–64 | 962 (14.2) | 1,146 (23.2) |
| Women | 5,225 (77.0) | 3,037 (61.4) |
| Number of chronic conditions | ||
| 0 | 3,801 (56.0) | 3,253 (65.7) |
| 1 | 1,974 (29.1) | 1,050 (21.2) |
| ≥2 | 1,015 (14.9) | 647 (13.1) |
| Borderline personality disorder | 251 (3.7) | 20 (0.4) |
| Substance use disorders | 498 (7.3) | 86 (1.7) |
| Overdose history | 640 (9.4) | 131 (2.6) |
| Management during index episode | ||
| Psychosocial assessment | 1,952 (28.7) | 1,168 (23.6) |
| Length of stay of ≥4 days | 1,473 (21.7) | 1,290 (26.1) |
Table S3.
Cox proportional hazard models evaluating risk factors for overdose repetition and termination of continuous psychiatric care
| Characteristics | Psychiatrist cohort (n=6,790)
|
No-psychiatrist cohort (n =4,950)
|
||
|---|---|---|---|---|
| HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | |
| Age, years | ||||
| 19–34 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 35–49 | 0.84 (0.74, 0.96)* | 0.99 (0.92, 1.06) | 0.80 (0.62, 1.04) | 1.07 (1.01, 1.14)* |
| 50–64 | 0.55 (0.44, 0.68)* | 1.03 (0.94, 1.14) | 0.32 (0.22, 0.47)* | 1.21 (1.13, 1.30)* |
| Women | 1.75 (1.46, 2.10)* | 0.94 (0.87, 1.01) | 1.35 (1.03, 1.76)* | 0.90 (0.85, 0.95)* |
| Number of chronic conditions | ||||
| 0 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 1.11 (0.97, 1.28) | 0.97 (0.90, 1.05) | 1.48 (1.12, 1.96)* | 1.00 (0.93, 1.07) |
| ≥2 | 1.12 (0.94, 1.33) | 1.05 (0.95, 1.15) | 1.64 (1.15, 2.32)* | 1.19 (1.09, 1.29)* |
| Borderline personality disorder | 1.10 (0.85, 1.41) | 0.98 (0.83, 1.16) | 1.42 (0.56, 3.59) | 1.12 (0.82, 1.52) |
| Substance use disorders | 1.60 (1.31, 1.96)* | 1.25 (1.12, 1.40)* | 1.11 (0.53, 2.31) | 1.26 (1.08, 1.47)* |
| Overdose history | 2.07 (1.77, 2.43)* | 0.82 (0.72, 0.92)* | 2.95 (1.94, 4.49)* | 1.13 (0.96, 1.33) |
| Psychotropic prescriptions before index episode | ||||
| Benzodiazepines | ||||
| None (0 mg) | 0.74 (0.51, 1.08) | 0.84 (0.73, 0.97)* | 1.33 (0.90, 1.97) | 1.17 (1.08, 1.26)* |
| Normal (>0 to ≤15 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>15 to ≤30 mg) | 0.91 (0.76, 1.07) | 0.95 (0.87, 1.03) | 1.04 (0.61, 1.79) | 1.02 (0.87, 1.19) |
| Excessive (>30 mg) | 1.02 (0.83, 1.25) | 0.95 (0.86, 1.05) | 1.49 (0.75, 2.96) | 1.04 (0.86, 1.27) |
| Barbiturates | 0.96 (0.77, 1.20) | 1.08 (0.97, 1.21) | 1.25 (0.61, 2.54) | 1.29 (1.09, 1.53)* |
| Antidepressants | ||||
| None (0 mg) | 0.92 (0.78, 1.09) | 0.91 (0.84, 0.98)* | 1.04 (0.65, 1.68) | 1.04 (0.94, 1.16) |
| Normal (>0 to ≤300 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>300 mg) | 0.66 (0.46, 0.95)* | 0.96 (0.82, 1.14) | 0.23 (0.02, 3.09) | 1.00 (0.59, 1.68) |
| Antipsychotics | ||||
| None (0 mg) | 0.97 (0.82, 1.15) | 0.96 (0.89, 1.04) | 0.95 (0.51, 1.77) | 1.06 (0.90, 1.24) |
| Normal (>0 to ≤450 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>450 mg) | 0.81 (0.62, 1.07) | 0.88 (0.77, 1.01) | 0.52 (0.18, 1.53) | 1.04 (0.69, 1.57) |
| Stabilizers | 1.02 (0.85, 1.23) | 1.00 (0.92, 1.08) | 0.66 (0.37, 1.17) | 1.06 (0.92, 1.24) |
| Management during index episode | ||||
| Psychosocial assessment | 0.97 (0.84, 1.11) | 0.96 (0.89, 1.03) | 0.95 (0.73, 1.24) | 0.75 (0.71, 0.81)* |
| Length of stay of ≥4 days | 0.83 (0.70, 0.98)* | 1.08 (0.99, 1.17) | 1.30 (1.01, 1.69)* | 0.86 (0.81, 0.92)* |
| Psychotropic prescriptions after index episode | ||||
| Benzodiazepines | ||||
| None (0 mg) | 0.53 (0.42, 0.66)* | 3.27 (2.95, 3.63)* | 0.40 (0.27, 0.61)* | 2.38 (2.03, 2.79)* |
| Normal (>0 to ≤15 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>15 to ≤30 mg) | 1.41 (1.17, 1.71)* | 1.13 (0.99, 1.28) | 1.75 (1.11, 2.77)* | 1.05 (0.80, 1.37) |
| Excessive (>30 mg) | 1.61 (1.30, 2.00)* | 1.00 (0.86, 1.17) | 1.75 (0.94, 3.26) | 1.13 (0.79, 1.63) |
| Barbiturates | 1.42 (1.11, 1.81)* | 0.99 (0.81, 1.21) | 1.43 (0.73, 2.80) | 1.56 (0.93, 2.64) |
| Antidepressants | ||||
| None (0 mg) | 0.99 (0.84, 1.17) | 2.45 (2.23, 2.70)* | 1.10 (0.73, 1.68) | 3.00 (2.50, 3.60)* |
| Normal (>0 to ≤300 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>300 mg) | 1.48 (1.05, 2.07)* | 1.00 (0.77, 1.31) | 1.36 (0.43, 4.31) | 1.55 (0.73, 3.29) |
| Antipsychotics | ||||
| None (0 mg) | 0.91 (0.76, 1.09) | 2.09 (1.88, 2.31)* | 0.81 (0.49, 1.35) | 2.04 (1.67, 2.48)* |
| Normal (>0 to ≤450 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>450 mg) | 1.05 (0.80, 1.36) | 0.82 (0.68, 0.98)* | 2.38 (1.28, 4.42)* | 1.00 (0.60, 1.67) |
| Stabilizers | 1.09 (0.89, 1.34) | 0.57 (0.51, 0.65)* | 1.09 (0.69, 1.71) | 0.70 (0.55, 0.89)* |
Note:
P<0.05.
Abbreviations: HR, hazard ratio; CI, confidence interval.
Acknowledgments
This study was supported by grants from the Japan Society for the Promotion of Science (number: 26870914). The sponsors of the study had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The authors thank Enago (www.enago.jp) for the English language review.
Footnotes
Author contributions
YO participated in the study concept and design; acquisition, analysis, and interpretation of data; and drafting of the manuscript. DN participated in supervision of the study design, interpretation of data, and critical revision of the manuscript for important intellectual content. Both the authors contributed to and approved the final manuscript and agree to be accountable for all aspects of the work.
Disclosure
YO received research grants from the Japan Agency for Medical Research and Development, the Ministry of Health, Labour and Welfare, the Japan Society for the Promotion of Science, the Institute for Health Economics and Policy, and Mental Health and Morita Therapy. He also served as member of an advisory board for Janssen Pharmaceuticals, Inc., and as chairman of the Reporting Quality Initiative of Researchers in Clinical Epidemiology. DN has received research grants from the Japan Society for the Promotion of Science, the National Center of Neurology and Psychiatry Japan, the Ministry of Health, Labour and Welfare, and the Japan Agency for Medical Research and Development, a lecture fee from Otsuka Pharmaceutical Co., Ltd., and a manuscript fee from Sumitomo Dainippon Pharma Co., Ltd. The authors report no other conflicts of interest in this work.
References
- 1.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1–9. doi: 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 2.Royal College of Psychiatrists . Self-Harm, Suicide and Risk: Helping People Who Self-Harm. London: Author; 2010. [Google Scholar]
- 3.National Institute for Health and Clinical Excellence . Self-Harm: The Short-term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care. Manchester: Author; 2004. [PubMed] [Google Scholar]
- 4.Barr W, Leitner M, Thomas J. Psychosocial assessment of patients who attend an accident and emergency department with self-harm. J Psychiatr Ment Health Nurs. 2005;12(2):130–138. doi: 10.1111/j.1365-2850.2004.00804.x. [DOI] [PubMed] [Google Scholar]
- 5.Carroll R, Metcalfe C, Steeg S, et al. Psychosocial assessment of self-harm patients and risk of repeat presentation: an instrumental variable analysis using time of hospital presentation. PLoS One. 2016;11(2):e0149713. doi: 10.1371/journal.pone.0149713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanehara A, Yamana H, Yasunaga H, et al. Psychiatric intervention and repeated admission to emergency centres due to drug overdose. Br J Psychiatry Open. 2015;1(2):158–163. doi: 10.1192/bjpo.bp.115.002204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapur N, Steeg S, Webb R, et al. Does clinical management improve outcomes following self-harm? Results from the multicentre study of self-harm in England. PLoS One. 2013;8(8):e70434. doi: 10.1371/journal.pone.0070434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergen H, Hawton K, Waters K, Cooper J, Kapur N. Psychosocial assessment and repetition of self-harm: the significance of single and multiple repeat episode analyses. J Affect Disord. 2010;127(1–3):257–265. doi: 10.1016/j.jad.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Kapur N, House A, Dodgson K, May C, Creed F. Effect of general hospital management on repeat episodes of deliberate self poisoning: cohort study. BMJ. 2002;325(7369):866–867. doi: 10.1136/bmj.325.7369.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hickey L, Hawton K, Fagg J, Weitzel H. Deliberate self-harm patients who leave the accident and emergency department without a psychiatric assessment: a neglected population at risk of suicide. J Psychosom Res. 2001;50(2):87–93. doi: 10.1016/s0022-3999(00)00225-7. [DOI] [PubMed] [Google Scholar]
- 11.Kapur N, Murphy E, Cooper J, et al. Psychosocial assessment following self-harm: results from the multi-centre monitoring of self-harm project. J Affect Disord. 2008;106(3):285–293. doi: 10.1016/j.jad.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Kapur N, Cooper J, Hiroeh U, May C, Appleby L, House A. Emergency department management and outcome for self-poisoning: a cohort study. Gen Hosp Psychiatry. 2004;26(1):36–41. doi: 10.1016/j.genhosppsych.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Crawford MJ, Wessely S. Does initial management affect the rate of repetition of deliberate self harm? Cohort study. BMJ. 1998;317(7164):985. doi: 10.1136/bmj.317.7164.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okumura Y, Shimizu S, Ishikawa KB, Matsuda S, Fushimi K, Ito H. Comparison of emergency hospital admissions for drug poisoning and major diseases: a retrospective observational study using a nationwide administrative discharge database. BMJ Open. 2012;2(6):e001857. doi: 10.1136/bmjopen-2012-001857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okumura Y, Tachimori H, Matsumoto T, Nishi D. Exposure to psychotropic medications prior to overdose: a case-control study. Psychopharmacology (Berl) 2015;232(16):3101–3109. doi: 10.1007/s00213-015-3952-8. [DOI] [PubMed] [Google Scholar]
- 16.Ichikura K, Okumura Y, Takeuchi T. Associations of adverse clinical course and ingested substances among patients with deliberate drug poisoning: a cohort study from an Intensive Care Unit in Japan. PLoS One. 2016;11(8):e0161996. doi: 10.1371/journal.pone.0161996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shih HI, Lin MC, Lin CC, et al. Benzodiazepine therapy in psychiatric outpatients is associated with deliberate self-poisoning events at emergency departments: a population-based nested case-control study. Psychopharmacology (Berl) 2013;229(4):665–671. doi: 10.1007/s00213-013-3127-4. [DOI] [PubMed] [Google Scholar]
- 18.Okumura Y, Sakata N, Takahashi K, Nishi D, Tachimori H. Epidemiology of overdose episodes from the period prior to hospitalization for drug poisoning until discharge in Japan: an exploratory descriptive study using a nationwide claims database. J Epidemiol. doi: 10.1016/j.je.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministry of Health, Labour Welfare On the Use of the National Database of Health Insurance Claim Information and Specified Medical Checkups. 2013. [Accessed February 17, 2016]. Available from: http://www.mhlw.go.jp/stf/shingi/2r9852000002ss9z-att/2r9852000002ssfg.pdf.
- 20.Statistics Bureau [webpage on the Internet] Current Population Estimates as of October 1, 2012. 2013. [Accessed January 2, 2016]. Available from: http://www.stat.go.jp/data/jinsui/2012np/index.htm.
- 21.National Institute of Population and Social Security Research Social Security in Japan. 2014. [Accessed January 4, 2016]. Available from: http://www.ipss.go.jp/s-info/e/ssj2014/PDF/ssj2014.pdf.
- 22.Heyerdahl F, Bjornaas MA, Dahl R, et al. Repetition of acute poisoning in Oslo: 1-year prospective study. Br J Psychiatry. 2009;194(1):73–79. doi: 10.1192/bjp.bp.107.048322. [DOI] [PubMed] [Google Scholar]
- 23.Reith DM, Whyte I, Carter G. Repetition risk for adolescent self-poisoning: a multiple event survival analysis. Aust N Z J Psychiatry. 2003;37(2):212–218. doi: 10.1046/j.1440-1614.2003.01114.x. [DOI] [PubMed] [Google Scholar]
- 24.Fadum EA, Stanley B, Qin P, Diep LM, Mehlum L. Self-poisoning with medications in adolescents: a national register study of hospital admissions and readmissions. Gen Hosp Psychiatry. 2014;36(6):709–715. doi: 10.1016/j.genhosppsych.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 25.Hirata K, Matsumoto Y, Tomioka J, Kurokawa A, Matsumoto M, Murata M. Acute drug poisoning at critical care departments in Japan. Jpn J Hosp Pharm. 1998;24(4):340–348. [Google Scholar]
- 26.Inagaki A, Inada T. Dose equivalence of psychotropic drugs. Part X VIII: 2006-version (in Japanese) Jpn J Clin Pharmacol. 2006;9:1443–1447. [Google Scholar]
- 27.Okumura Y, Inada K, Matsumoto T, Shimizu S. Changes in high-dose and combined anxiolytic-hypnotic prescription in outpatient psychiatric practice after regulatory action (in Japanese) Jpn J Clin Pharmacol. 2015;18:1173–1188. [Google Scholar]
- 28.Sundararajan V, Quan H, Halfon P, et al. Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45(12):1210–1215. doi: 10.1097/MLR.0b013e3181484347. [DOI] [PubMed] [Google Scholar]
- 29.Canadian Agency for Drugs and Technologies in Health . Discontinuation Strategies for Patients with Long-term Benzodiazepine Use: A Review of Clinical Evidence and Guidelines. Ottawa, ON: Author; 2015. [PubMed] [Google Scholar]
- 30.Olfson M, Marcus SC, Bridge JA. Emergency treatment of deliberate self-harm. Arch Gen Psychiatry. 2012;69(1):80–88. doi: 10.1001/archgenpsychiatry.2011.108. [DOI] [PubMed] [Google Scholar]
- 31.Bridge JA, Marcus SC, Olfson M. Outpatient care of young people after emergency treatment of deliberate self-harm. J Am Acad Child Adolesc Psychiatry. 2012;51(2):213.e1–222.e1. doi: 10.1016/j.jaac.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Inagaki M, Kawashima Y, Kawanishi C, et al. Interventions to prevent repeat suicidal behavior in patients admitted to an emergency department for a suicide attempt: a meta-analysis. J Affect Disord. 2015;175:66–78. doi: 10.1016/j.jad.2014.12.048. [DOI] [PubMed] [Google Scholar]
- 33.Kawanishi C, Aruga T, Ishizuka N, et al. Assertive case management versus enhanced usual care for people with mental health problems who had attempted suicide and were admitted to hospital emergency departments in Japan (ACTION-J): a multicentre, randomised controlled trial. Lancet Psychiatry. 2014;1(3):193–201. doi: 10.1016/S2215-0366(14)70259-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flow diagram of patients included in both cohorts and reasons for exclusion.
Cumulative proportion of overdose repetition by treatment patterns before and after discharge.
Notes: Solid line represents Kaplan–Meier event curve, and shaded area represents the 95% confidence interval. (A) Antidepressants in psychiatrist cohort, (B) antipsychotics in psychiatrist cohort, (C) stabilizers in psychiatrist cohort, (D) antidepressants in no-psychiatrist cohort, (E) antipsychotics in no-psychiatrist cohort, and (F) stabilizers in no-psychiatrist cohort.
Table S1.
Complete list of psychotropic medications included in the covariate assessment
| Drugs | Drugs |
|---|---|
| Benzodiazepines | Antidepressants |
| Alprazolam | Maprotiline |
| Bromazepam | Mianserin |
| Brotizolam | Milnacipran |
| Chlordiazepoxide | Mirtazapine |
| Clobazam | Nortriptyline |
| Clonazepam | Paroxetine |
| Clorazepate dipotassium | Sertraline |
| Clotiazepam | Setiptiline |
| Cloxazolam | Sulpirideb |
| Diazepam | Trazodone |
| Estazolam | Trimipramine |
| Eszopiclone | Antipsychotics |
| Ethyl loflazepate | Aripiprazole |
| Etizolam | Blonanserin |
| Fludiazepam | Bromperidol |
| Flunitrazepam | Carpipramine |
| Flurazepam | Chlorpromazine |
| Flutazolam | Chlorpromazine–promethazine–phenobarbitala |
| Flutoprazepam | Clocapramine |
| Haloxazolam | Clozapine |
| Lorazepam | Fluphenazine |
| Lormetazepam | Haloperidol |
| Medazepam | Haloperidol decanoate |
| Mexazolam | Levomepromazine |
| Nimetazepam | Mosapramine |
| Nitrazepam | Nemonapride |
| Oxazolam | Olanzapine |
| Quazepam | Oxypertine |
| Rilmazafone | Paliperidone |
| Tofisopam | Paliperidone palmitate |
| Triazolam | Perospirone |
| Zolpidem | Perphenazine |
| Zopiclone | Pimozide |
| Barbiturates | Pipamperone |
| Amobarbital | Prochlorperazine |
| Barbital | Propericiazine |
| Chlorpromazine–promethazine–phenobarbitala | Quetiapine |
| Pentobarbital calcium | Reserpine |
| Phenobarbital | Risperidone |
| Phenobarbital sodium | Spiperone |
| Phenytoin–phenobarbital | Sulpirideb |
| Secobarbital sodium | Sultopride |
| Antidepressants | Tiapride |
| Amitriptyline | Timiperone |
| Amoxapine | Trifluoperazine |
| Clomipramine | Zotepine |
| Dosulepin | Stabilizers |
| Duloxetine | Carbamazepine |
| Escitalopram | Lamotrigine |
| Fluvoxamine | Lithium |
| Imipramine | Valproate |
| Lofepramine |
Notes:
Chlorpromazine–promethazine–phenobarbital combined was double-counted as both a barbiturate and an antipsychotic.
Sulpiride of <300 or ≥300 mg/day was counted as an antidepressant or an antipsychotic, respectively.
Table S2.
Characteristics of cohort that did and did not have psychiatric treatment before overdose
| Characteristics | Treatment by psychiatrists before index episode, n (%)
|
|
|---|---|---|
| Psychiatrist cohort (n=6,790) | No-psychiatrist cohort (n=4,950) | |
| Age, years | ||
| 19–34 | 3,267 (48.1) | 2,263 (45.7) |
| 35–49 | 2,561 (37.7) | 1,541 (31.1) |
| 50–64 | 962 (14.2) | 1,146 (23.2) |
| Women | 5,225 (77.0) | 3,037 (61.4) |
| Number of chronic conditions | ||
| 0 | 3,801 (56.0) | 3,253 (65.7) |
| 1 | 1,974 (29.1) | 1,050 (21.2) |
| ≥2 | 1,015 (14.9) | 647 (13.1) |
| Borderline personality disorder | 251 (3.7) | 20 (0.4) |
| Substance use disorders | 498 (7.3) | 86 (1.7) |
| Overdose history | 640 (9.4) | 131 (2.6) |
| Management during index episode | ||
| Psychosocial assessment | 1,952 (28.7) | 1,168 (23.6) |
| Length of stay of ≥4 days | 1,473 (21.7) | 1,290 (26.1) |
Table S3.
Cox proportional hazard models evaluating risk factors for overdose repetition and termination of continuous psychiatric care
| Characteristics | Psychiatrist cohort (n=6,790)
|
No-psychiatrist cohort (n =4,950)
|
||
|---|---|---|---|---|
| HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | HR (95% CI) for overdose repetition | HR (95% CI) for discontinuity of psychiatric care | |
| Age, years | ||||
| 19–34 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 35–49 | 0.84 (0.74, 0.96)* | 0.99 (0.92, 1.06) | 0.80 (0.62, 1.04) | 1.07 (1.01, 1.14)* |
| 50–64 | 0.55 (0.44, 0.68)* | 1.03 (0.94, 1.14) | 0.32 (0.22, 0.47)* | 1.21 (1.13, 1.30)* |
| Women | 1.75 (1.46, 2.10)* | 0.94 (0.87, 1.01) | 1.35 (1.03, 1.76)* | 0.90 (0.85, 0.95)* |
| Number of chronic conditions | ||||
| 0 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 1.11 (0.97, 1.28) | 0.97 (0.90, 1.05) | 1.48 (1.12, 1.96)* | 1.00 (0.93, 1.07) |
| ≥2 | 1.12 (0.94, 1.33) | 1.05 (0.95, 1.15) | 1.64 (1.15, 2.32)* | 1.19 (1.09, 1.29)* |
| Borderline personality disorder | 1.10 (0.85, 1.41) | 0.98 (0.83, 1.16) | 1.42 (0.56, 3.59) | 1.12 (0.82, 1.52) |
| Substance use disorders | 1.60 (1.31, 1.96)* | 1.25 (1.12, 1.40)* | 1.11 (0.53, 2.31) | 1.26 (1.08, 1.47)* |
| Overdose history | 2.07 (1.77, 2.43)* | 0.82 (0.72, 0.92)* | 2.95 (1.94, 4.49)* | 1.13 (0.96, 1.33) |
| Psychotropic prescriptions before index episode | ||||
| Benzodiazepines | ||||
| None (0 mg) | 0.74 (0.51, 1.08) | 0.84 (0.73, 0.97)* | 1.33 (0.90, 1.97) | 1.17 (1.08, 1.26)* |
| Normal (>0 to ≤15 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>15 to ≤30 mg) | 0.91 (0.76, 1.07) | 0.95 (0.87, 1.03) | 1.04 (0.61, 1.79) | 1.02 (0.87, 1.19) |
| Excessive (>30 mg) | 1.02 (0.83, 1.25) | 0.95 (0.86, 1.05) | 1.49 (0.75, 2.96) | 1.04 (0.86, 1.27) |
| Barbiturates | 0.96 (0.77, 1.20) | 1.08 (0.97, 1.21) | 1.25 (0.61, 2.54) | 1.29 (1.09, 1.53)* |
| Antidepressants | ||||
| None (0 mg) | 0.92 (0.78, 1.09) | 0.91 (0.84, 0.98)* | 1.04 (0.65, 1.68) | 1.04 (0.94, 1.16) |
| Normal (>0 to ≤300 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>300 mg) | 0.66 (0.46, 0.95)* | 0.96 (0.82, 1.14) | 0.23 (0.02, 3.09) | 1.00 (0.59, 1.68) |
| Antipsychotics | ||||
| None (0 mg) | 0.97 (0.82, 1.15) | 0.96 (0.89, 1.04) | 0.95 (0.51, 1.77) | 1.06 (0.90, 1.24) |
| Normal (>0 to ≤450 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>450 mg) | 0.81 (0.62, 1.07) | 0.88 (0.77, 1.01) | 0.52 (0.18, 1.53) | 1.04 (0.69, 1.57) |
| Stabilizers | 1.02 (0.85, 1.23) | 1.00 (0.92, 1.08) | 0.66 (0.37, 1.17) | 1.06 (0.92, 1.24) |
| Management during index episode | ||||
| Psychosocial assessment | 0.97 (0.84, 1.11) | 0.96 (0.89, 1.03) | 0.95 (0.73, 1.24) | 0.75 (0.71, 0.81)* |
| Length of stay of ≥4 days | 0.83 (0.70, 0.98)* | 1.08 (0.99, 1.17) | 1.30 (1.01, 1.69)* | 0.86 (0.81, 0.92)* |
| Psychotropic prescriptions after index episode | ||||
| Benzodiazepines | ||||
| None (0 mg) | 0.53 (0.42, 0.66)* | 3.27 (2.95, 3.63)* | 0.40 (0.27, 0.61)* | 2.38 (2.03, 2.79)* |
| Normal (>0 to ≤15 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>15 to ≤30 mg) | 1.41 (1.17, 1.71)* | 1.13 (0.99, 1.28) | 1.75 (1.11, 2.77)* | 1.05 (0.80, 1.37) |
| Excessive (>30 mg) | 1.61 (1.30, 2.00)* | 1.00 (0.86, 1.17) | 1.75 (0.94, 3.26) | 1.13 (0.79, 1.63) |
| Barbiturates | 1.42 (1.11, 1.81)* | 0.99 (0.81, 1.21) | 1.43 (0.73, 2.80) | 1.56 (0.93, 2.64) |
| Antidepressants | ||||
| None (0 mg) | 0.99 (0.84, 1.17) | 2.45 (2.23, 2.70)* | 1.10 (0.73, 1.68) | 3.00 (2.50, 3.60)* |
| Normal (>0 to ≤300 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>300 mg) | 1.48 (1.05, 2.07)* | 1.00 (0.77, 1.31) | 1.36 (0.43, 4.31) | 1.55 (0.73, 3.29) |
| Antipsychotics | ||||
| None (0 mg) | 0.91 (0.76, 1.09) | 2.09 (1.88, 2.31)* | 0.81 (0.49, 1.35) | 2.04 (1.67, 2.48)* |
| Normal (>0 to ≤450 mg) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| High (>450 mg) | 1.05 (0.80, 1.36) | 0.82 (0.68, 0.98)* | 2.38 (1.28, 4.42)* | 1.00 (0.60, 1.67) |
| Stabilizers | 1.09 (0.89, 1.34) | 0.57 (0.51, 0.65)* | 1.09 (0.69, 1.71) | 0.70 (0.55, 0.89)* |
Note:
P<0.05.
Abbreviations: HR, hazard ratio; CI, confidence interval.