Abstract
Nurses seek to understand better what practicing with wisdom means and how to apply wisdom to practice; however, the experience of wisdom in nursing has not been well defined or researched. This study was designed to understand how emergency department (ED) nurses construct the meaning of wisdom within the culture of clinical nursing practice. Using Charmaz’s constructivist grounded theory methodology, we developed a preliminary theory capturing the experience of wisdom in practice. The core theoretical model focuses on two juxtaposed processes, technical and affective, and is grounded in expertise. Significant findings were the recognition of affective categories, such as emotional intelligence, required to practice using wisdom. Results reinforce and extend the current wisdom literature and provide a new perspective on wisdom in practice in a nursing context.
Keywords: emergency care, grounded theory, nursing community, qualitative analysis
Human beings seek to comprehend wisdom better and to apply it in daily life. Two types of wisdom are described in the psychology literature, general and personal (Staudinger & Glück, 2011). General wisdom is directed toward other individuals from a third-person perspective as a trait manifested by caring for others. In contrast, personal wisdom is individual, focused on advice and judgment based on insight gained from experience (Mickler & Staudinger, 2008). Personal wisdom is about one’s own life and problems seen from a first-person perspective.
Wisdom gained attention in nursing when the concept was added to the definition of nursing informatics (NI) in the 2008 edition of the American Nurses Association’s (ANA) Nursing Informatics: Scope and Standards of Practice. Early definitions of NI outlined data, information, and knowledge as foundational concepts for the specialty. Building on early work in the fields of information science, wisdom was added to the NI definition, aligning it with the data, information, knowledge, wisdom (DIKW) framework. The most current NI scope and standards indicate that nursing informaticists support the development of wisdom for all types of nurses (ANA, 2015a). Wisdom is typically defined as use of knowledge, but from foundational literature, wisdom has many aspects beyond a cognitive/knowledge sphere. Because all nurses have a desire to be wise within their own clinical practice, it is imperative that they understand what the concept of wisdom represents in the context of clinical nursing practice.
Neither the current ANA (2015b) Nursing Scope and Standards of Practice nor the Code for Ethics (ANA, 2015a) discusses the concept of wisdom. Few scholars have explored or modeled the concept of wisdom in a nursing context. A comprehensive literature search revealed characteristics of wisdom being described as cognitive, ethical, intuitive, and emotional processes. Cognitive attributes of wisdom include expertise, proficiency, and knowledge (Benner, 1999, 2000; Matney, Brewster, Sward, Cloyes, & Staggers, 2011). Having these traits requires nurses to understand the problem at hand, make distinctions between alternatives, and think creatively about the solution (Nelson, 2002). Wisdom concerns ethics and involves values and the desire to achieve a common good (Haggerty & Grace, 2008; Uhrenfeldt & Hall, 2007). Finally, the concept encompasses intuition and emotion (Edmondson & Pearce, 2007). These attributes link wisdom to human acts or behavior, leading one to believe that wisdom is a label that one might choose to apply to certain actions (Haggerty & Grace, 2008; Litchfield, 1999).
This article describes the second arm of the development of a theory of wisdom-in-action (WIA) for nursing. In the first arm, a construct illustrating WIA was developed using derivation and synthesis (Matney, Avant, & Staggers, 2016). For this arm of the research, we were interested in an insider perspective of what wisdom means to nurses, and how those experiences are represented through categories and processes grounded in the data. Therefore, the aim of this study was to understand how emergency department (ED) nurses construct the meaning of wisdom in the ED setting within the culture of clinical nursing practice. The research questions were as follows:
Research Question 1: What does wisdom mean to emergency room nurses?
Research Question 2: What central processes are used to practice wisely and gain knowledge through practice?
Research Question 3: What key concepts are involved in the processes?
Research Question 4: How are the processes related to each other?
Method
Design and Approach
Wisdom is intrinsically a social-cultural shared construct or experience, something perceived and difficult to define. Thus, we examined the actions, perceptions, decision making, and human interactions of clinical ED nurses using a constructivist grounded theory (CGT) approach. CGT is a logically consistent, inductive research approach used for generating formal mid-range theory of human behavior in a social context (Charmaz, 2006; Jeon, 2004; Morse et al., 2009). Contemporary grounded theory (GT), on the other hand, draws on strategies from early approaches to GT, such as coding, mePmo writing, and theoretical statements, but shifts its epistemological foundations to an interpretive/constructivist paradigm (Charmaz, 2006, 2014). The main reason we chose CGT was because we already had involvement and interactions with this research topic and CGT acknowledges this subjectivist stance. Charmaz (2014) stated that the researcher should not be theoretically innocent but rather should be theoretically agnostic, a stance consistent with our knowledge of the topic.
The theoretical perspectives of CGT are symbolic interactionism (SI) and interpretivism. SI supports and informs the research methodology of CGT because actions are performed in the environment, or culture, based on meanings (Oliver, 2011). In SI, the focus is on how one interprets the situation and chooses one type of action. Interpretivism is the study of social life and aligns with CGT, which aims toward an understanding of an individual’s actions and the meaning of those actions (Charmaz, 2006; Crotty, 1998). The epistemology that informs both theoretical perspectives is constructivism; wherein human beings construct meanings as they interact with the world they are interpreting.
Sample and Setting
After we obtained institutional review board approval from the study setting, practicing ED nurses were recruited through a flyer sent to their work email and posted in the department. The inclusion criteria for nurse participants were (a) employed within the ED setting within the previous 5 years, and (b) a registered nurse, at any level of education, with at least 5 years of nursing experience. Including ED nurses was a theoretical sampling choice, as these nurses frequently deal with stressful or uncertain situations in a fast-paced environment, are required to possess a high degree of knowledge across myriad patient conditions, and have the autonomy to make decisions and perform interventions during critical situations (Laxmisan et al., 2007). The nurses practiced in a 452-bed tertiary center with a Level-1 trauma center in an urban setting in the western United States. The trauma center had more than 82,000 ED visits in 2013 (U.S. News & World Report, 2013).
With the theoretical sampling frame selected, a convenience sample of nurses was recruited. Convenience sampling allowed us to recruit nurses who were easily accessible and added theoretically meaningful insights relevant to the tentative analytic categories previously identified in the derived theory (Tweed & Charmaz, 2012). The sample consisted of 10 nurses (seven women, three men), with an age range of 22 to 59 years. On average, they had 11.1 years of experience (range = 5–35 years). Participants included associate degree (n = 4), baccalaureate degree (n = 5), and master’s degree (n = 1) nurses. All 10 of the nurses were currently working in the field of nursing although one of them no longer worked in the ED. Each participant signed an informed consent for participation before the interview. To protect confidentiality, digitized interviews were transcribed and then destroyed. After transcription, all names (people, places, care providers, etc.) were changed to pseudonyms in the transcripts. The stories within the interviews were given identifiers, and a master list that linked the nurses’ names to the stories was kept in a locked file within the school of nursing.
Data Collection Methods
We chose to obtain stories regarding nurses’ practice because daily situations yield a certain kind of story readily analyzable using a grounded theory methodology and stories would be easy for nurses to recall accurately (Lai, 2010). After obtaining informed consent for study participation, each nurse was asked the initial open-ended interview question, “Tell me about a clinical situation in which you or someone else demonstrated wisdom in a clinical situation.” The specific question guiding the interview was chosen because previous psychology researchers used this question to investigate social and nonverbal behaviors people display when using wisdom in life matters (Kunzmann & Baltes, 2005). Nurses were allowed to tell their story from beginning to end without interruption.
The next step used “deepening” questions or probes to understand the situation and the process of decision making. This went beyond the facts and explored the nurses’ thought processes during the clinical story. Deepening probe questions in response to stories of clinical wisdom included the following: What information did you use to make a decision? What made this situation difficult? What did you learn from this situation? How did this influence your future practice? What haunts you?
The final question focused on defining wisdom, “Describe the characteristics, or attributes, of the wisest nurse you have ever worked with.” We solicited as many stories as the nurses wanted to give. Each nurse provided one description of a wise nurse (totaling 10) and three to four stories describing stressful situations (totaling 30). The audio-recorded face-to-face, interviews generally lasted an hour.
Data analysis
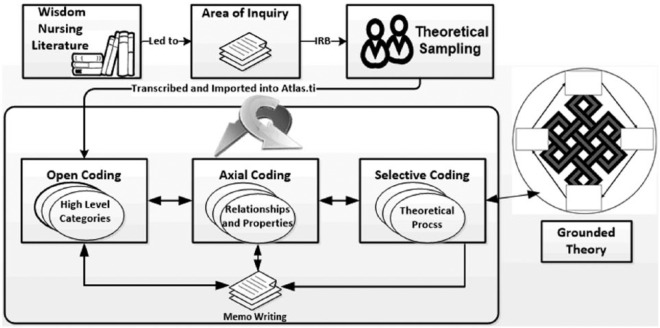
Analysis methods were consistent with Charmaz’s (2014) recommendations for CGT and included three coding phases: open coding, axial coding, and selective coding. Coding was inductive/deductive, comparative, interactive, and iterative. We wrote memos throughout the analysis process. The goal of analysis was to immerse ourselves fully in the data by studying and restudying the data (Charmaz, 1996). Figure 1 pictorially displays the CGT process. Each step is described and discussed below.
Figure 1.
Representation of constructivist grounded theory analysis process.
Note. IRB = institutional review board.
The goal of open coding was to produce as many codes as possible to describe the meaning of the story, using line-by-line and action-by-action coding (Lieblich, Tuval-Mashiach, & Zilber, 1998). Consistent with a focus on the social process of WIA, we used gerunds and other code words or phrases to index segments of transcripts that answered our analytic questions, such as “What action is happening here?” What is the person actually saying? What do these statements and actions imply? What is the participant’s understanding of the situation? What social processes are occurring in the context of the data? What category do these data indicate? (Charmaz, 2014; Saldaña, 2009).
We made several passes through the data during open coding until the initial concepts were identified (Corbin & Strauss, 2008). The properties, dimensions, and relationships to each other were determined in the axial coding phase. At this phase, the theory’s interpretive and illustrative framework began to emerge (Mills, Bonner, & Francis, 2006). We used constant data comparison to determine new categories and to refine all categories for interpretation (Charmaz, 1996).
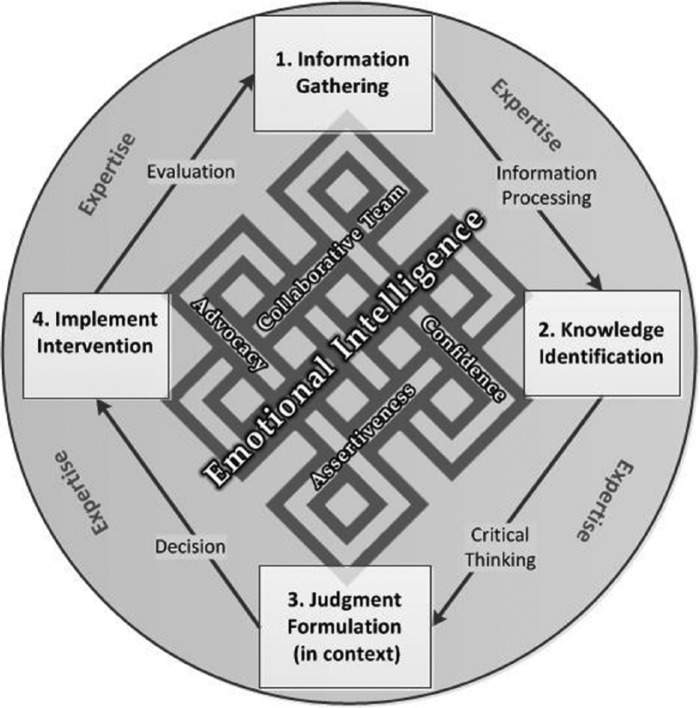
We used an iterative process for open coding and axial coding. Cluster and network diagramming assisted in analyzing the codes. Open codes were grouped into code families for consideration as categories and to visualize co-occurring codes using network diagramming. After the categories began to emerge, cluster diagramming aided in understanding the relationships between categories (see Figure 2). Charmaz (2014) described clustering as linked wheels with spokes. We found that clustering represented interesting groups of ideas in linked categories and illustrated the axial codes or relationships among the codes within the categories.
Figure 2.
The process of practicing with wisdom.
During selective coding, we interpreted the theoretical process from the data and defined high-level categories and subcategories central to the process (Tweed & Charmaz, 2012). Concurrently, we wrote memos throughout the analysis process (Charmaz, 2014; Lempert, 2007). After identifying all categories, subcategories, and relationships, we reviewed the nursing and wisdom literature to refine the properties and relationship(s) for each concept (Charmaz, 1996). This phase of the research process developed theoretical sensitivity by highlighting similarities between the findings of this study and previous theoretical constructs and concept analyses in the literature (threaded within the results and further described in the discussion). We also considered the potential transferability of the phenomenon of WIA aligned with similar situations in health care (Chiovitti & Piran, 2003). WIA might be transferrable to clinical decision making in other settings beyond the ED. The grounded theory of WIA infuses the nursing process with technical and affective wisdom processes congruent with wise practice across a range of practice settings. Although each category achieved data saturation in this study, and the theory as a whole achieved theoretical saturation, establishing transferability of the theory of WIA across health care practice settings was not the goal of this study.
We diagrammed the theory as concepts and relationships emerged (Lempert, 2007). Diagrams assisted in understanding the meaning of the phenomenon by providing a visual display of what was known. Diagramming also allowed us to identify gaps where concepts were lost or not yet known. For example, during one of our early theory-diagramming sessions, we noticed that knowledge was missing. We went back to the data and reevaluated knowledge as a key category. Concepts and properties were further refined, and actual data were included to illustrate how the analysis is grounded in lived experience.
Findings
The nurses’ stories varied widely in a number of ways. The patient ages in the stories ranged from a premature newborn to the elderly, and clinical scenarios included behavioral, trauma, medical, and obstetrical patients. Some stories pertained to an individual and others pertained to families. Typical clinical stories of WIA were non-routine, challenging events or situations that dealt with uncertainty.
As we studied the data, we identified thoughts and actions performed when nurses felt they had “made a difference.” We recognized two different juxtaposed processes in the data: a technical care-delivery process and an affective process, with expertise underpinning both processes. These processes were not sequential or mutually exclusive. The technical care-delivery process (the outside ring in Figure 2) included actions related to the science of nursing and aligned closely with the nursing process. The affective process consisted of emotion and human-interaction characteristics woven through the entire situation. The affective categories co-occurred so frequently that they were almost inextricable from one another; therefore, relationships between them could not be clearly identified. The affective categories are visualized within a Celtic knot, which, by its interconnectedness, is a symbol for the union of wisdom and method. This might represent the art of nursing. From the data, the process of using wisdom in practice, henceforth called wisdom-in-action (WIA), can occur only when both processes exist. In the next section, the theory categories and subcategories are discussed. Table 1 illustrates the categories and subcategories discussed next.
Table 1.
A Grounded Theory of Wisdom in Emergency Nursing.
| Categories | Subprocesses | Linking Concepts |
|---|---|---|
| Expertise | ||
| Technical wisdom process | ||
| Information gathering | Obtaining patient history | Information processing |
| Assessing | ||
| Obtaining pertinent information | ||
| Knowledge identification | Explicit knowledge | Critical thinking |
| Intuitive knowledge | ||
| Judgment formulation | Decision making | |
| Intervention implementation | Evaluation | |
| Affective wisdom process | ||
| Emotional intelligence | Self-awareness | |
| Motivation | ||
| Self-regulation | ||
| Empathy | ||
| Advocacy | ||
| Assertiveness | ||
| Confidence | ||
| Team collaboration | ||
Expertise
We coded all 30 stories and 10 descriptions of a “wise nurse” having expertise where expertise is having an expert level of knowledge, tenure, and experience. A foundation of expertise underlies and influences both the technical and affective wisdom processes. The expert nurse has an intuitive grasp of clinical situations with highly proficient performance. How nurses handle emergencies and use available systems is a learned skill that demonstrates proficiency or expertise (Benner, 1984, 2000). As one participant shared, “I think that wisdom can really only be obtained through experience and the book learning, and everything is important and a great foundation.” Another nurse explained the rationale for performing an intervention as, “I was drawing from experience.”
Technical Process Wisdom Categories
The technical care process portion of the model illustrates the scientific process of care. This process consists of four high-level categories: information gathering, knowledge identification, judgment formulation, and intervention implementation; and four linking concepts: information processing, critical thinking, decision making, and evaluation (see Figure 2).
Information gathering
Information gathering occurs as soon as the patient enters the ED and reoccurs after interventions. During this process, nurses obtain information about the patient and the situation. The three sub processes are types of information gathering: obtaining patient history, assessing the patient, and obtaining pertinent information from the care record. Information is data structured within the context of care and was always obtained prior to the action of using knowledge or applying a judgment (Matney, Maddox, & Staggers, 2014).
Assessing the patient
The first type of information gathering occurred during assessment. When one patient was being wheeled into the ED, the nurse stated that she “immediately looked at the monitor and there was just a totally disorganized rhythm.” She then gathered further information: “We analyzed the rhythm, and she was in VFib [ventricular fibrillation].”
Assessing patient history
Often, the patient’s history was being taken by the nurse at the same time as the assessment was being made. This information came from the patient, the patient’s family, or the ambulance crew.
Obtaining pertinent information
Nurses also gathered pertinent information including information such as laboratory values, medications, and vital signs. The nurse continued, “We reviewed the cardiac profile.”
Information processing
Nurses described the information they gathered and described the problem. This implied that the cognitive processing of information occurred in their minds. During information processing, relationships in the information are formalized and synthesized. The linkage between information gathering and knowledge identification is information processing.
Knowledge identification
Two types of knowledge, explicit and intuitive, were demonstrated within the stories.
Explicit knowledge
Explicit knowledge was coded when the nurses described pattern matching in their stories or described scenarios seen previously that they used to generate knowledge. One nurse described pattern matching when speaking about a patient: “She probably had anoxic brain as well. . . . I had previous experience where I saw a lot of people that were anoxic brain injuries, and she looked just like that.” Explicit knowledge was manifested when the nurse described the rationale for interventions: “One thing that that patient needed immediately was IV [intravenous] access. That is really the lifeline for any patient—especially a sick patient.”
Intuitive knowledge
Intuition was coded when the nurses made clinical decisions with no concrete information available to explain their actions (Berragan, 1998; Rew & Barrow, 1987). The nurses described this as a “gut feeling” or “hunch” about something that did not have concrete facts to support it. This feeling motivated the nurse to perform some type of intervention. One nurse said, “Something was just very wrong.” She sat close to the patient’s room because of her feeling, and soon after, the patient began projectile vomiting blood.
Critical thinking
In the stories, nurses used critical thinking to define and understand a problem (physical or mental) and to establish a desired goal. The nurses determined the problem in the context of the situation. Critical thinking is the link between knowledge identification and judgment formulation, and is the act of cognitively analyzing, reasoning, predicting, and transforming knowledge (Scheffer & Rubenfeld, 2000).
Judgment formulation
Judgment was coded when knowledge regarding the situation motivated some type of intervention. Judgment was also coded when the explanation was given as to why an intervention was performed. One nurse stated, “There was a totally disorganized rhythm on the monitor, so we defibrillated him.” In this situation, the nurse used knowledge to determine a plan of action; this included identifying the problem, goal(s), and interventions.
Decision making
Decision making is the linkage between judgment and intervention. During this time, the nurse in the ED made a determination as to what the right care options were for this patient (in context): “We got the crash cart there, and we got her patched up with the defibrillator patches. . . . We made the decision that she needed to be defibrillated.”
Intervention implementation
After the nurses made a decision, they performed an action (an intervention). The intervention for the patient above was, “We charged the defibrillator and defibrillated her.” Within the stories, the types of interventions included medication or oxygen administration, providing support or education, and performing a procedure such as monitoring the patient or starting an IV.
Evaluation
The final link in the care process was evaluation. Evaluation determines the results of procedures or interventions and leads back into information gathering where the process begins again. Types of evaluations were reviewing laboratory findings and evaluating vital signs or equipment. After the above patient was defibrillated, the nurse stated, “She did not suffer any real negative consequences because of that early recognition and defibrillation of VFib.”
Affective Process Categories (The Celtic Knot of Nursing Care)
From the data, we identified the importance of concepts related to mood, feelings, and attitudes in the process of providing care. These concepts were coded and grouped into affective process categories. The stories indicated that these nontechnical categories were as essential as the technical categories.
Emotional intelligence
Emotional intelligence encompasses four subcategories: self-awareness, self-regulation, motivation, and empathy (Codier, 2015; Kooker, Shoultz, & Codier, 2007). Because this concept represents four subcategories, the font is the larger within the Celtic Knot of Nursing Care (see Figure 2).
Self-awareness
We coded self-awareness when the nurses recognized their own strengths and abilities. One nurse had previous experience as an IV nurse so he felt he was the best one to try to insert an IV on a premature baby:
I guess point is . . . with the a 27-seven-week infant . . . having the skills and the confidence and the ability to place an IV line in such a small little child was something that was necessary and gave me a great feeling.
Managing negative emotions
Nurses had a desire to recognize negative emotions and learn to overcome them. Nurses often discussed negative emotions when the patient was under the influence of drugs or alcohol or was a psychiatric patient. In the following story, the nurse was describing an intoxicated patient who fell off a porch and injured himself. She recognized the negative emotions and overcame them by staying calm and talking with the patient:
He was drunk, but he just would not comply with anything. He was ripping his gown off . . . throwing. . . . We put him in one of the behavior rooms. . . . He was trying to rip the rails off the bed. Any time you came into the room he would be very aggressive; he would want to lunge at you and stuff. Dealing with this patient, you felt like you couldn’t really do anything for this patient because he was being so aggressive and so abusive. I think that is really high stress.
So what did the nurse do to calm him down?
Just talking to him and sitting down and keeping my distance but just talking and letting him vent and letting him know that “I’m not going to hurt you. I’m not going to do anything without telling you” and stuff. I think that really helped defuse that situation. I think it does with a lot of patients.
Self-regulation
The nurses described many emotions they felt during patient interactions of various kinds. They portrayed self-regulation by managing their negative emotions, such as anger or anxiety. Open codes for this subcategory included “feeling stressed,” “feeling uncomfortable,” “feeling frustrated,” and “feeling angry.”
Empathy
Empathy was evident when the nurses thought about each person as an individual and treated even the most minor injury as important to that specific person. Sometimes, we had “reading between the lines” to understand what the person was saying. This category included compassion that occurred when a nurse witnessed suffering, entered that person’s or family’s experience, was motivated to help, and/or shared the burden with them (Goetz, Keltner, & Simon-Thomas, 2010; Von Dietze & Orb, 2000). The following is an example of empathy from the nurses’ stories:
I think about how everyone needs mothering. You have to listen to their story. You have to think it through. He didn’t even know what he needed. . . . There is a bigger picture than what is going on in the room. . . . I couldn’t have gone on with my life until I helped him figure it out.
Advocacy
Advocacy was treating every person with dignity and equality, and alleviating suffering. When one nurse questioned a physician regarding the wrong dose on an order, she was being an advocate. In another story, a patient came in and admitted to his nurse that he was an alcoholic. The nurse stated, “I told him that if he was serious we could really get him help and that he was very brave, and that I was so proud that he could admit that today.” The nurse described the ethical dimension of WIA by pointing to advocacy as an element of wise practice, and the ANA (2015b) addressed the importance of advocacy in its Code of Ethics.
Assertiveness
Several stories had cases in which the nurse had to take control of the situation. In one instance, the provider was an intern and the patient started “exorcist projectile vomiting blood.” The intern “freaked out and left the room,” so the nurse assertively stepped up to manage the situation. In another scenario, a physician was not in the room, but the patient needed to be defibrillated. The nurse stated, “I knew I had to do it but that was the first time I had ever defibrillated without a physician at the bedside.”
Nurses demonstrated assertiveness when nurses suggested different types of interventions, such as laboratory tests, to the providers. Assertiveness is the ability to stand up for oneself or one’s patients by expressing thoughts, feelings, opinions, or needs without being aggressive or hurting others (Hodgetts, 2011). Confidence co-occurred in all reported cases of assertiveness. The data indicate that confidence needs to exist for the nurses to be assertive.
Confidence
The nurses discussed gaining and practicing with confidence. Nurses gained confidence when they were successful in performing a skill: “It made me more confident in the future that I had the knowledge of what I needed to do . . . when the ‘shit hit the fan.’” Nurses illustrated practicing with confidence through self-assurance and the realization of their own knowledge and ability: “I had the skills and the confidence and the ability to place an IV line in such a small little child.” Confidence requires the capacity to believe in oneself.
Collaborative team
Team collaboration was present when nurses, physicians, and all ancillary members were working cooperatively together, sharing problems and making decisions to carry out a plan for the patient. Collaboration requires social skills and the ability to communicate effectively with others. In a stressful situation, team collaboration is crucial. One nurse said,
If you have it in your mind that this is for the good of the patient and that I am working with this physician as a team to have the best outcome that we can have . . .
The findings from this study, grounded in the data, illustrate that expertise and both technical and nontechnical skills are required to practice nursing within the emergency room with wisdom. The ability to perform patient care technical tasks will certainly affect nurses’ success in practice; however, how nurses work with others, advocate for the patient, and incorporate self-awareness might play an even larger part than nursing skills. Nurses must possess the ability to communicate with health care team members and emotionally connect to their patients.
Discussion
The use of storytelling as a way to understand nursing practice led to valuable insights about the complexities of contemporary practice and nursing wisdom in an ED setting. By telling stories about a few meaningful experiences, nurses had the opportunity to reflect on wisdom within their own practice and to realize they practiced using wisdom (Lieblich et al., 1998). One nurse stated at the end of a session, “I feel like I just had a therapy session where the therapist validated that I was a good nurse.” Participating in qualitative research can be transformative for some research participants.
We examined similarities between the findings of this study and previous theoretical constructs and concept analyses in the literature. Specifically, the wisdom theory from this study was compared to Benner’s (1984) novice to expert framework, Carper’s (1978) patterns of knowing, and the DIKW framework (ANA, 2015b).
The foundation of practicing with wisdom is expertise. Benner (1984) defined five levels of nursing experience: novice, advanced beginner, competent, proficient, and expert. Each level is attained through years of clinical experience, education, and training. Our study found that practicing with wisdom first requires expertise for a specific situation and includes evaluating information, identifying a problem, and creating and modifying plans as needed to provide care. This skill set requires, at the minimum, a proficient nurse who perceives and understands the whole situation.
Carper (1978) described four types of knowing: (a) empirics, (b) esthetics, (c) personal knowledge, and (d) ethics. These types of knowing were present providing validation for the wisdom theory. Empirics are the science or cognitive aspect of nursing. This aligns with the technical care process in this study. Nurses look at the facts (information gathering) to systematically determine the problem, make a decision, and perform an intervention. Carper describes esthetics as the art of nursing and describes it as a tacit process where the nurse “perceives” what is happening to the patient. This pattern aligns with the affective process (the Celtic knot) in the middle of the grounded theory but because of this study, the attributes of esthetics can be further defined; emotional intelligence includes empathy and understanding and the ability to deal with the emotional aspects of the patient and family. Carpers’ described ethics as the moral component. Ethics aligns with judgment formulation and decision making. Wisdom and ethics share similar attributes and are closely related.
Practicing with wisdom requires information and knowledge. Therefore, there is good alignment between the grounded theory from this study and the DIKW framework (ANA, 2015b). Data are not included because practice requires contextual data, which by definition equals information (Matney, Brewster, Sward, Cloyes, & Staggers, 2011; Matney, Avant, Staggers, 2013). Wise practice involves the synthesis of information (information processing) to uncover knowledge (knowledge identification). Having knowledge supports decision making regarding the science of nursing.
This study adds to the research by providing specific insights about practicing wisdom in emergency nursing. Wisdom includes expertise, technical, and affective categories. All affective categories identified in this study were previously mentioned in the literature, but they were never grouped as a whole, as illustrated in the Celtic knot model of practicing nursing with wisdom. The separate affective categories might have been under-valued in their contributions to wisdom. By grouping them together, their importance is more apparent. These categories are important to the patient, and in practice, education, and leadership settings.
The theory developed using CGT provides evidence for the categories needed to be a wise nurse. The theory could represent a consciousness-raising for nurses; they can visualize the characteristics and actions required to perform wise practice and recognize the importance wisdom plays in practice. This is significant for nursing education because it provides the possibility of quantifying nurses’ skill levels and monitoring the changes over time for each affective characteristic. Some tools are already developed that measure these categories, such as the Perceived Self-Confidence Scale (White, 2014), but further tool development is needed. Knowing how these characteristics of wise nurses make a difference in care could lead to changes in nursing curricula to emphasize the categories of wisdom and characteristics of wise nurses. The ultimate significance is that the increased skill level intrinsic to wisdom-in-practice might improve the quality of care.
The theory of wisdom is important and significant for patients and their families. Human’s want and need to be cared for by nurses who consider their specific human values, have a high level of scientific knowledge, and have advanced technical skill. All of these characteristics are included in the theory of WIA.
Research about wisdom in nursing is still in its infancy. Clinical questions pertaining to the profession should be developed with a focus on personal qualities of relevance to practicing with wisdom. In our reflecting on the memos, stories, and literature review, additional research questions emerged. Suggestions for questions to be addressed in future studies include the following: What is the theory and research related to knowledge processing? What is the relationship between cognition and emotions in nursing? How are the categories in the Celtic knot different from and similar to the emotional intelligence domains? If all categories in the Celtic knot have measurement tools, can these be a measure of WIA? Are there unique sets of wisdom categories that are optimal for different practice settings and levels of leadership responsibilities?
Conclusion
Practicing nursing with wisdom is a complex process. Wisdom categories clearly emerged from ED nurses’ stories about their practice. Understanding these categories can be used both to help nurses demonstrate wisdom as they provide nursing care and to teach new nurses the process of becoming wise in nursing practice. It was humbling to see the art and the science of nursing threaded through the care given by ED nurses.
Author Biographies
Susan A. Matney, RN, PhD, FAAN, is a senior medical informaticist at Intermountain Healthcare in Salt Lake City, UT, USA.
Nancy Staggers, RN, PhD, FAAN, is a health informatics consultant and adjunct professor, Informatics, Biomedical Informatics and College of Nursing, at the University of Utah, Salt Lake City, Utah, USA.
Lauren Clark, RN, PhD, FAAN, is a professor and chair of the Division of Health Systems and Community-Based Care at the University of Utah College of Nursing in Salt Lake City, Utah, USA.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- American Nurses Association. (2008). Nursing informatics: Scope and standards of practice. Silver Spring, MD: Author. [Google Scholar]
- American Nurses Association. (2015a). Nursing informatics: Scope and standards of practice ( 2nd ed.). Silver Spring, MD: Author. [Google Scholar]
- American Nurses Association. (2015b). Code of ethics for nurses with interpretive statements. Washington, DC: Author. [Google Scholar]
- Benner P. (1984). From novice to expert: Excellence and power in clinical nursing practice. Menlo Park, CA: Addison-Wesley. [Google Scholar]
- Benner P. (1999). Nursing leadership for the new millennium. Claiming the wisdom & worth of clinical practice. Nursing and Health Care Perspectives, 20, 312–319. [PubMed] [Google Scholar]
- Benner P. (2000). The wisdom of our practice. American Journal of Nursing, 100(10), 99–105. doi: 10.2307/3522335 [DOI] [PubMed] [Google Scholar]
- Berragan L. (1998). Nursing practice draws upon several different ways of knowing. Journal of Clinical Nursing, 7, 209–217. doi: 10.1046/j.1365-2702.1998.00146.x [DOI] [PubMed] [Google Scholar]
- Carper B. (1978). Fundamental patterns of knowing in nursing. Advances in Nursing Science, 1(1), 13–23. doi: 10.1097/00012272-197810000-00004 [DOI] [PubMed] [Google Scholar]
- Charmaz K. (1996). Grounded theory. In Smith J. A., Harre R., Van Langenhove L. (Eds.), Rethinking methods in psychology (pp. 27–49). London: Sage. [Google Scholar]
- Charmaz K. (2006). Constructing grounded theory: A practical guide through qualitative analysis. Thousand Oaks, CA: Sage. [Google Scholar]
- Charmaz K. (2014). Constructing grounded theory (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Chiovitti R. F., Piran N. (2003). Rigour and grounded theory research. Journal of Advanced Nursing, 44, 427–435. doi: 10.1046/j.0309-2402.2003.02822.x [DOI] [PubMed] [Google Scholar]
- Codier E. (2015). Emotional intelligence: Enhancing value-based practice and compassionate care in nursing. Evidence Based Nursing, 18(1), 8. doi: 10.1136/eb-2014-101733 [DOI] [PubMed] [Google Scholar]
- Corbin J. M., Strauss A. (2008). Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage. [Google Scholar]
- Crotty M. (1998). The foundations of social research: Meaning and perspective in the research process. London: Sage. [Google Scholar]
- Edmondson R., Pearce J. (2007). The practice of health care: Wisdom as a model. Medicine, Healthcare and Philosophy, 10, 233–244. doi: 10.1007/s11019-006-9033-3 [DOI] [PubMed] [Google Scholar]
- Goetz J. L., Keltner D., Simon-Thomas E. (2010). Compassion: An evolutionary analysis and empirical review. Psychological Bulletin, 136, 351–374. doi: 10.1037/a0018807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty L. A., Grace P. (2008). Clinical wisdom: The essential foundation of “good” nursing care. Journal of Professional Nursing, 24, 235–240. doi: 10.1016/j.profnurs.2007.06.010 [DOI] [PubMed] [Google Scholar]
- Hodgetts S. (2011). Being assertive benefits everyone. Nursing Times, 107(47), 41. [PubMed] [Google Scholar]
- Jeon Y. H. (2004). The application of grounded theory and symbolic interactionism. Scandinavian Journal of Caring Sciences, 18, 249–256. doi: 10.1111/j.1471-6712.2004.00287.x [DOI] [PubMed] [Google Scholar]
- Kooker B. M., Shoultz J., Codier E. E. (2007). Identifying emotional intelligence in professional nursing practice. Journal of Professional Nursing, 23(1), 30–36. doi: 10.1016/j.profnurs.2006.12.004 [DOI] [PubMed] [Google Scholar]
- Kunzmann U., Baltes P. (2005). The psychology of wisdom. In Sternberg R. J., Jordan J. (Eds.), A handbook of wisdom: Psychological perspectives (pp. 110–135). New York: Cambridge University Press. [Google Scholar]
- Lai C. K. Y. (2010). Narrative and narrative enquiry in health and social sciences. Nurse Researcher, 17(3), 72–84. [DOI] [PubMed] [Google Scholar]
- Laxmisan A., Hakimzada F., Sayan O. R., Green R. A., Zhang J., Patel V. L. (2007). The multitasking clinician: Decision-making and cognitive demand during and after team handoffs in emergency care. International Journal of Medical Informatics, 76, 801–811. doi: 10.1016/j.ijmedinf.2006.09.019 [DOI] [PubMed] [Google Scholar]
- Lempert L. B. (Ed.). (2007). Asking questions of the data: Memo writing in the grounded theory tradition. London: Sage. [Google Scholar]
- Lieblich A., Tuval-Mashiach R., Zilber T. (1998). Narrative research: Reading, analysis, and interpretation. Thousand Oaks, CA: Sage. [Google Scholar]
- Litchfield M. (1999). Practice wisdom. Advances in Nursing Science, 22(2), 62–73. doi: 10.1097/00012272-199912000-00007 [DOI] [PubMed] [Google Scholar]
- Matney S. A., Avant K. C., Staggers N. (2013). The construct of wisdom-in-action for clinical nursing. Poster presented at the American Nursing Informatics Association, San Antonio, TX. [Google Scholar]
- Matney S. A., Avant K. C., Staggers N. (2016). Toward an understanding of wisdom in nursing. The Online Journal of Issues in Nursing, 21(1). [DOI] [PubMed] [Google Scholar]
- Matney S. A., Brewster P. J., Sward K. A., Cloyes K. G., Staggers N. (2011). Philosophical approaches to the nursing informatics data-information-knowledge-wisdom framework. Advances in Nursing Science, 34, 6–18. doi: 10.1097/ANS.0b013e3182071813 [DOI] [PubMed] [Google Scholar]
- Matney S. A., Maddox L. J., Staggers N. (2014). Nurses as knowledge workers: Is there evidence of knowledge in patient handoffs? Western Journal of Nursing Research, 36, 171–190. doi: 10.1177/0193945913497111 [DOI] [PubMed] [Google Scholar]
- Mickler C., Staudinger U. M. (2008). Personal wisdom: Validation and age-related differences of a performance measure. Psychology and Aging, 23, 787–799. doi: 10.1037/a0013928 [DOI] [PubMed] [Google Scholar]
- Mills J., Bonner A., Francis K. (2006). Adopting a constructivist approach to grounded theory: Implications for research design. International Journal of Nursing Practice, 12, 8–13. doi: 10.1111/j.1440-172X.2006.00543.x [DOI] [PubMed] [Google Scholar]
- Morse J. M., Stern P. N., Corbin J. M., Bowers B., Clarke A. E., Charmaz K. (2009). Developing grounded theory: The second generation. Walnut Creek, CA: Left Coast Press. [Google Scholar]
- Nelson R. (2002). Major theories supporting health care informatics. In Englebardt S., Nelson R. (Eds.), Health care informatics: An interdisciplinary approach (pp. 3–27). St. Louis, MO: Mosby. [Google Scholar]
- Oliver C. (2011). The relationship between symbolic interactionism and interpretive description. Qualitative Health Research, 22, 409–415. doi: 10.1177/1049732311421177 [DOI] [PubMed] [Google Scholar]
- Rew L., Barrow E. M. (1987). Intuition: A neglected hallmark of nursing knowledge. Advances in Nursing Science, 10(1), 49–62. doi: 10.1097/00012272-198710000-00010 [DOI] [PubMed] [Google Scholar]
- Saldaña J. (2009). The coding manual for qualitative researchers. Thousand Oaks, CA: Sage. [Google Scholar]
- Scheffer B. K., Rubenfeld M. G. (2000). A consensus statement on critical thinking in nursing. Journal of Nursing Education, 39, 352–359. [DOI] [PubMed] [Google Scholar]
- Staudinger U. M., Glück J. (2011). Psychological wisdom research: Commonalities and differences in a growing field. Annual Review of Psychology, 62, 215–241. [DOI] [PubMed] [Google Scholar]
- Tweed A., Charmaz K. (2012). Grounded theory methods for mental health practitioners. In Harper D., Thompson A. R. (Eds.), Qualitative research methods in mental health and psychotherapy: A guide for students and practitioners (pp. 131–146).West Sussex, UK: John Wiley. [Google Scholar]
- Uhrenfeldt L., Hall E. O. (2007). Clinical wisdom among proficient nurses. Nursing Ethics, 14, 387–398. doi: 10.1177/0969733007075886 [DOI] [PubMed] [Google Scholar]
- U.S. News & World Report. (2013). Best hospitals: Intermountain Medical Center. Retrieved from http://health.usnews.com/best-hospitals/area/ut/intermountain-medical-center-6870141
- Von Dietze E., Orb A. (2000). Compassionate care: A moral dimension of nursing. Nursing Inquiry, 7, 166–174. doi: 10.1046/j.1440-1800.2000.00065.x [DOI] [Google Scholar]
- White K. A. (2014). Development and validation of a tool to measure self-confidence and anxiety in nursing students during clinical decision making. Journal of Nursing Education, 53(1), 14–22. doi: 10.3928/01484834-20131118-05 [DOI] [PubMed] [Google Scholar]