Abstract
In spite of increasing prevalence of diabetes among Kenyans and evidence suggesting Kenyans with diabetes maintain poor glycemic control, no one has examined the role of cultural attitudes, beliefs, and practices in their self-management of diabetes. The purpose of this ethnographic study was to describe diabetes self-management among the Swahili of coastal Kenya, and explore factors that affect diabetes self-management within the context of Swahili culture. Thirty men and women with type 2 diabetes from Lamu town, Kenya, participated in this study. Diabetes self-management was insufficiently practiced, and participants had limited understanding of diabetes. Economic factors such as poverty and the high cost of biomedical care appear to have more influence in self-management behavior than socio-cultural and educational factors do. Economic and socio-cultural influences on diabetes self-management should not be underestimated, especially in a limited resource environment like coastal Kenya, where biomedical care is not accessible or affordable to all.
Keywords: diabetes, Africa, ethnography, self-care, health seeking, culture, illness diseases, chronic, culture / cultural competence, health behavior
Background
In the past 20 years, Kenya has seen a gradual increase in the prevalence of type 2 diabetes. Studies conducted in Kenya estimate the prevalence of type 2 diabetes to be between 2.2% and 12.2% of the sampled population (Christensen et al., 2009; Hall, Thomsen, Henrinksen, & Lohse, 2011; Hendriks, Wit, & Roos, 2012; Mathenge, Foster, & Kuper, 2010), and the International Diabetes Federation (IDF; 2015) estimates that by 2040, the rates of diabetes in this region will more than double. Kenya is witnessing increased mortality associated with diabetes complications such as diabetic ketoacidosis (Mbugua, Otieno, Kayima, Amayo, & McLigeyo, 2005) and foot ulcers (Muthuuri, 2007). Many with diabetes in Kenya are maintaining sub-optimal or poor glycemic control (Matheka, Kilonzo, Munguti, & Mwangi, 2013; Otieno, Huho, Omonge, Amayo, & Njagi, 2008; Otieno, Kariuki, & Ng’ang’a, 2003; Pastakia, Karwa, Kahn, & Nyabundi, 2011), which in tandem with poor self-care practices were among the factors attributed to the increased risk of diabetic foot ulcers, a complication of diabetes (Nyamu, Otieno, Amayo, & McLigeyo, 2003).
Mutea and Baker (2008) suggest that illiteracy, poverty, nursing shortages, lack of diabetes policies/guidelines, and inadequate medical resources impede people’s management of diabetes in Kenya. What has not been explored in Kenya is the role of cultural beliefs and practices in self-management of type 2 diabetes (e.g., healthy eating, staying active, monitoring blood glucose, taking medications, and monitoring for diabetes complications and risks). In the United States, cultural beliefs, practices, and attitudes have been demonstrated to have a vital role in diabetes self-management behavior (SMB) among African Americans, Asian Americans, and Mexican Americans. Studies among these populations have ascertained the effectiveness of tailoring self-care behavior to the cultural needs of the community in question (Joo, 2014; Kim et al. 2009; Skelly, 2011; Vincent, 2009). Among other communities in the United States, culture has been demonstrated to influence diabetes self-care by (a) promoting negative attitudes toward insulin (Lipton, Losey, Giachello, Mendez, & Girotti, 1998), (b) favoring more familiar traditional remedies (Lipton et al., 1998), (c) promoting fatalistic beliefs about diabetes (Egede & Bonadonna, 2003; Lipton et al., 1998), and (d) using spirituality to encourage diabetes self-care activities (Casarez, Engebretson, & Ostwald, 2010).
Cultural assessment is instrumental in understanding the broader cultural context in which a group or a person lives, and can provide background information to guide the design of culturally congruent health care interventions (Tripp-Reimer, Choi, Kelley, & Enslein, 2001). Among the important steps in delivering culturally competent care is understanding the knowledge, health beliefs and behaviors, and illness beliefs and practices of individuals and families (Tripp-Reimer et al., 2001). In this case, the people under study are people of Swahili ethnicity with type 2 diabetes, and who live in Lamu town on Lamu Island, Kenya. Because the Swahili have a unique set of cultural beliefs and practices that play a vital role in matters related to health, illness, and well-being (Abdulrehman & Gearhart, 2012; Gearhart & Abdulrehman, 2014), examining type 2 diabetes care in light of these cultural attitudes, values, and expressions will provide an insider’s understanding of diabetes self-management among this population. The knowledge gained through this study is foundational to health care providers in particular, who are on the frontlines of providing culturally appropriate patient care.
Conceptual Framework
In this study, we used Leininger’s (2002) sunrise model to explore factors that affect diabetes self-management using a cultural lens, which provides a comprehensive understanding of multiple factors that affect diabetes self-care. These factors include economic conditions, education, politics and law, cultural values and beliefs, kinship and society, religion and philosophy, and technology (Leininger, 2002). In the context of this study, we expect that economic conditions influence who has access to costly biomedical care. Educational status and social status influence one’s acculturation to the biomedical model. Cultural values and beliefs determine who seeks out traditional medicine. Religion provides a framework for what is considered an acceptable form of treatment for type 2 diabetes. For example, some Muslims consider insulin, which is made from pigs, to be unclean. As Muslims, Swahili who know the origins of insulin may not consider it a viable treatment for diabetes. The purpose of this study, therefore, is to explore the role of culture in self-management of type 2 diabetes among the Swahili of coastal Kenya, and explore factors that affect diabetes self-management within the context of Swahili cultural practices and beliefs.
Research Questions
Little is known in the literature about the role of the Swahili culture and its societal influences on type 2 diabetes. Using Leininger’s cultural care theory, we explore the meanings, symbols, patterns, processes, and practices of the Swahili peoples of Lamu town with type 2 diabetes. As noted by Reynolds and Leininger (1993), this type of knowledge facilitates the provision of culturally congruent care. The sunrise model (Leininger, 2002) is relevant to this study because it enables the understanding of how the Swahili cultural values and behaviors influence diabetes self-management, and we formulated research questions that explore the determinants of care expressions, and the patterns and practices that represent the building blocks of Leininger’s (1985) sunrise model.
Research Question 1: How do the Swahili of Lamu town, Kenya, manage diabetes?
Research Question 2: In what ways do demographic characteristics (e.g., age, gender, marital status, education level, socioeconomic status, and duration of diabetes) affect diabetes self-management (e.g., healthy eating, being active, monitoring glucose/complications, taking medications, problem solving, and reducing risks of complications)?
Research Question 3: How is self-management of diabetes influenced by Swahili cultural beliefs and practices?
Method
Design
This research was undertaken using ethnonursing, a type of ethnographic research used to describe, discover, and/or explore nursing care phenomena (Leininger & McFarland, 2006). This methodological approach was selected to provide the insider’s perspective on what it means to a Swahili person to have diabetes, and how the Swahili manage the disease. Instead of assessing diabetes SMB within the biomedical framework, in this study, we elected an ethnographic approach to holistically explore the cultural awareness of diabetes self-management. The ethnographic fieldwork was conducted over a period of 5 months from November 2013 to March 2014. The methods we used were participant observation, field note taking, and ethnographic interviewing, which enabled us to understand diabetes self-management within the participants’ cultural context (Silverman, 1993) and encouraged the discovery of substantive knowledge (Leininger, 1985) relating to beliefs, values, and practices associated with diabetes self-management among the Swahili peoples of Kenya.
Setting
This study was conducted in Lamu town on Lamu Island, which lies just off the northern coast of Kenya. Lamu town is known locally as Amu, has a population of 22,366 people (Kenya National Bureau of Statistics [KNBS], 2010), has been continuously inhabited for more than 700 years, and is the oldest and best preserved Swahili settlement in East Africa (Allen, 1993). As a unique amalgamation of African, Arabian, Indian, and Persian peoples and cultures, the Swahili distinguish themselves ethnically, culturally, and religiously from the majority of their Kenyan countrymen (Allen, 1993). The majority of the people in Lamu town identify themselves as Swahili, which is also true of Lamu county, which has a total population of 101,539 (KNBS, 2010) and encompasses other small communities on the mainland and on other islands in the Lamu Archipelago.
Sample
Participants in this research were selected through purposive sampling, in which the primary investigator (PI) relied on insider’s status and the knowledge of being an insider to select the most appropriate participants. The PI is a Lamu town native, who continues to visit annually and whose familiarity with the community helped in selecting research participants. During 10 years working in Lamu town as a health care provider, the PI has made contact with several individuals with diabetes. Participants were also recruited through a word of mouth advertisement to community elders and persons with type 2 diabetes. In this study, we recruited 30 Swahili male and female participants aged 18 and older, with type 2 diabetes. Confirmation of a diagnosis of diabetes was based on self-reporting, and some participants provided us with individual health records. For achieving cultural homogeneity, we used personal judgment to identify individuals of Swahili descent. Some of the ways the PI identified individuals of Swahili descent were that they spoke Swahili as a first language, used a Swahili dialect common among natives of coastal Kenya, and had family relationships and kinship connections with members of the Lamu town community.
Data Collection
In this study, data were collected using participant observation, one-on-one interviewing, and field notes. Each of the methods we used to explore diabetes self-management in Lamu town is discussed separately, below.
Participant observation
Participant observation was used to understand how participants self-manage their diabetes in the natural setting of their home environment. We used a discourse-centered approach to engage participants in the research, and to learn more about their beliefs and practices related to diabetes. Throughout the study, the PI logged notes that recorded the observations and interactions with community members. Streubert and Carpenter (2011) urged researchers to immerse themselves in the research setting to gain a contextual understanding of the phenomenon under study. The PI immersed himself through participant observation, which allowed him to learn (a) the cultural ways the Swahili express diabetes symptoms, (b) the challenges related to diabetes self-management, and (c) the implementation of various therapies used to manage diabetes (e.g., pharmaceutical drugs, herbal remedies, foods). The PI immersed himself by visiting participants in their homes, places of business, places of worship, and cultural centers, where community activities such as weddings occur. The PI observed how the society accommodates or does not accommodate the dietary needs of people with type 2 diabetes with regard to the food served at various cultural events. The PI also observed the kinds of physical activities in which people with diabetes engage during their everyday lives.
Interviews
The ethnographic interview process helped the PI better understand patterns of health-seeking behavior related to diabetes among the Swahili, and gain insights into how the Swahili talk about diabetes in their own words. According to Fetterman (2010), conducting ethnographic interviews facilitates the researcher’s ability to gain an insider’s perspective. All interviews were conducted in the Swahili language and lasted for 20 minutes to 1 hour. A follow-up phone call was made to some participants to clarify responses and to further explore emerging themes of the research. The information that was collected through participant observation helped the PI refine questions for semi-structured, ethnographic interviews about participants’ knowledge, beliefs, and practices related to diabetes. Individuals were asked to share information about how they were diagnosed with diabetes, what they knew about the disease, how they self-manage the disease, and the challenges related to management of the disease. During the interview, we collected demographic information including age, marital status, duration of diabetes, education level, mode of treatment, and family history of diabetes.
Field notes
The PI kept a diary to record thoughts, feelings, and personal experiences throughout the research period. In ethnographic research, the ethnographer becomes the research instrument (Fetterman, 2010; Streubert & Carpenter, 2011), and interpersonal skills and experiences become important elements of fieldwork (Lipson, 1989; Van Maanen, 1995). The diary also included the PI’s reflections on the personal interactions with participants and addressed the issue of reflexivity, or the tension that exists when a researcher also becomes a member of the culture under study (Streubert & Carpenter, 2011). Negotiating the roles of a Lamu town native, a health care provider, and a researcher required the PI’s ongoing reflection and self-awareness. As a native ethnographer, the PI had grown up among the participants, was familiar with the research setting, and was comfortable with the local culture, language, and health care system, which facilitated his immediate immersion in the fieldwork. Yet, there were challenges the PI had to face, including gender stratification, complex kinship networks, socioeconomic hierarchies, illiteracy, and poverty, all of which are discussed in more detail in other work (Abdulrehman, 2015).
Data were collected with the help of a female research assistant, who is a clinical officer (physician assistant) native to the Lamu community and the Swahili language. Because gender stratification is a common cultural practice among the Swahili of Lamu town, the research assistant was essential in collecting data among female participants, who were interviewed by the research assistant while the PI sat in. The research assistant also accompanied the PI on visits to participants’ homes. The research assistant did not participate in data analysis.
Data Analysis
Interviews conducted in the Swahili language were tape-recorded and then transcribed by the PI into Swahili language. Each audio-recorded interview was compared with the interview notes and the reflective journal notes to ensure the collected information provided an accurate reflection of the communication (Halcomb & Davidson, 2006). Manual content analysis of the data was used to generate common themes. Transcribed interviews were coded and then grouped into categories, which were clustered into descriptive multi-dimensional themes including self-management practices, diabetes-related treatment, diabetes-related beliefs, knowledge of diabetes, challenges related to diabetes management, and factors that affect diabetes self-management. The developed themes were further reviewed by re-listening to the audiotape recordings and reviewing transcripts to highlight examples that demonstrated the meaning of the themes from the participants’ perspectives (Halcomb & Davidson, 2006). Two interview transcripts were audited by a second researcher and reviewed together with the PI and revised before final themes were selected. To ensure accuracy of the ethnographic descriptors that were translated into English and used in this article, a forward and back translation method was used. The ethnographic descriptors that highlighted the major themes were translated into English by the PI and then back translated into Swahili by a bilingual native Swahili speaker who had no prior knowledge of the original text. The PI checked for discrepancies in meaning between the translated version and the original text.
Trustworthiness
We used Lincoln and Guba’s (1985) and Leininger’s (Leininger & McFarland, 2006) criteria for scientific rigor. To ensure credibility of the data, we used the “member checking” technique (Lincoln & Guba, 1985) as a method of validating information provided by participants with participants while collecting data and during data analysis. To ensure accuracy of information, the PI and the research assistant debriefed after every interview. Both the research assistant and the PI were members of the Lamu community, and understood the local Swahili culture and language well. Credibility was also strengthened by peer checking and debriefing of emerging categories and themes with two other researchers, one of whom is an experienced ethnographer. To improve confirmability and dependability of this study, we maintained a detailed audit trail of field notes, audiotaped recordings, data analysis records, personal notes, and synthesis products (Lincoln & Guba, 1985). To enhance transferability of this study, we included a detailed description of the study’s setting, participants, and data collection process (Lincoln & Guba, 1985). Transferability was also maintained by including appropriate participant quotations.
In addition to Lincoln and Guba’s four criteria for research evaluation, we added two additional criteria that are unique to ethnonursing research (Leininger & McFarland, 2006). These criteria are recurrent patterning and saturation. To ensure recurrent patterning, we scrutinized data for repeated patterns and themes related to diabetes self-management expressions and health-seeking behavior. To ensure saturation, we continued to interview until we got to a point where no new findings on self-management of diabetes among the Swahili of Lamu town were forthcoming (Leininger & McFarland, 2006).
Ethical Considerations
Approval for the study was obtained from Illinois State University’s Institutional Review Board and the Kenya Ministry of Higher Education, Science and Technology. Participation was voluntary, and participants’ verbal consent was obtained. We forwent obtaining written consent for two reasons. First, Harrowing, Mill, Spiers, Kulig, and Kipp (2010) argued that among populations with high illiteracy rates, the consent form itself is potentially intimidating, and they urged researchers to find other approaches to documenting informed consent. Because adult illiteracy is high in Kenya, and it is estimated that one in three Kenyan adults are illiterate (Human Development Report, 2009; United Nations Educational, Scientific and Cultural Organization [UNESCO], 2008), we obtained verbal rather than written consent from participants. Second, the formal signing of a consent form is culturally foreign among the Swahili. Kithinji and Kass (2010) pointed out that most African languages, including Swahili, are traditionally and primarily used in oral communication rather than in written form. Thus, using written consent forms among the Swahili is not the best way to inform participants of their rights. To ensure that our participants were fully and appropriately informed, we presented the study information to them orally. Confidentiality was assured among all participants by assigning each a code number and referring to participants by number rather than name during the research.
Findings
Biographical Description of the Study
Sixteen men and 14 women agreed to participate in this study. The average age and mean duration of diabetes for the 30 participants were 52.9 years and 6.2 years, respectively. A large majority of the participants were married and had a family history of diabetes. Table 1 summarizes the socio-demographic and clinical characteristics of the participants.
Table 1.
Socio-Demographic and Clinical Characteristics of Participants.
| Characteristics of Participants With Diabetes (N = 30) | Percentage or M Value |
|---|---|
| Gender | |
| Male (14) | 46.7% |
| Female (16) | 53.3% |
| Age | |
| Mean age (range) in years | 52.9 (29–80) |
| Marital status | |
| Married (23) | 76.7% |
| Divorced (2) | 6.7% |
| Widowed (4) | 13.3% |
| Single (1) | 3.3% |
| Education level | |
| Never been to secular school (16) | 53.4% |
| Completed 4th grade (2) | 6.7% |
| Completed primary school (8) | 26.7% |
| Completed secondary school (1) | 3.3% |
| College training (3) | 10% |
| Years diagnosed with Diabetes Mellitus (DM) | |
| Mean years (range) diagnosed with DM | 6.24 (6 months–35 years) |
| Literacy (able to read and write) | |
| Swahili and English (13) | 43.3% |
| Swahili (10) | 33.3% |
| Cannot read and/or write (5) | 16.7% |
| Swahili and Arabic (2) | 6.7% |
| Treatment of DM | |
| Oral anti-diabetes agents (22) | 73.3% |
| Oral agents and insulin (2) | 6.7% |
| Diet only (1) | 3.3% |
| Insulin only (1) | 3.3% |
| No therapy (4) | 13.3% |
| Herbal remedies | |
| Reported using herbal remedies (15) | 50% |
| Family history of DM | |
| 1st degree relatives with DM (19) | 63.3% |
| 2nd degree relatives with DM (4) | 13.3% |
| No family history of DM (7) | 23.3% |
The findings of this study are organized according to the themes that were generated from the research questions and participants’ narratives. Two main themes were identified including SMB and factors affecting SMB. Several subthemes that emerged from the major themes are also described below.
SMB
Understanding diabetes and self-management
Participants believed that the causes of diabetes were family history, aging, weight, and diet. Some of the local ideas about the causes of diabetes included consuming ice water, living a stressful life, the increased presence of toxic chemicals in foods such as pesticides, and vaccinations. Some participants believed that diabetes is transmitted through mosquito bites and/or sexual intercourse with their spouses. Also, there was evidence of limited understanding of the complications of diabetes. For example, nine participants were unaware of the long-term effects of diabetes, and 13 participants believed that diabetes damages internal organs. Others mentioned body weakness and death as complications of diabetes. Although diabetes complications such as limb amputation and peripheral neuropathy are uncommon in Lamu town, participants occasionally mentioned them as complications of diabetes. The following comments from the participants illustrate some of their misinformation about the causes of diabetes:
Yes, you can infect someone. Because I did not have diabetes, my husband is the one who had diabetes. Why did I then get diabetes?
One big thing that I have read in Arabic books is that ice water can cause diabetes and I have investigated and I have observed it.
Many in the Lamu community are familiar with diabetes, and refer to it as sukari, the word for sugar in Swahili. The term sukari itself promulgates dietary misconceptions about diabetes by associating diabetes with the consumption of raw sugar and thus promoting a limited application of dietary restrictions. Almost all participants associated diabetes with dietary restrictions, translated in Swahili as miko. Many of the participants associated dietary restrictions with simply avoiding foods that contain raw sugar such as sweet tea, desserts, and juices. The traditional diet in Lamu town has plenty of starch and very little protein and vegetables. In this study, we observed a lack of understanding of the food groups and how they affect diabetes. For example, one participant claimed to never consume starch while reporting to regularly eat rice and chapatti (flat bread made with wheat flour). Therefore, there is inadequate understanding of how foods that are rich in starch such as rice, maize, and breads, influence blood glucose levels. Another concern relates to controlling portion size. In this study, only two participants practiced portion control, most did not know how much of each food group should be consumed daily, and none was familiar with the notion of calorie counting.
Mode of treatment for diabetes
Most of the participants in this study were taking oral diabetes medications including Metformin and Glyburide. Figure 1 summarizes the mode of treatment for diabetes among the participants. Also, there is wide use of herbal remedies for illnesses in Lamu town; most of the participants have used herbal remedies to attempt to cure diabetes at some point, and half of the sample reported using herbal remedies on a regular basis. The herbal remedies were either prepared at home by participants or relatives, or concocted by a local herbalist. Participants used a mixture of locally grown herbs and herbs that were prepared by herbalists from neighboring tribes or countries such as Tanzania. Many in the community shared the belief that herbal remedies can cure diabetes, a notion illustrated by the following quotes from the interviews.
Figure 1.
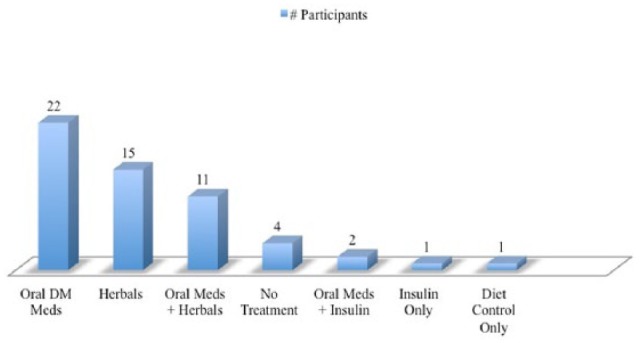
Mode of treatment for diabetes (N = 30).
There are herbals that can totally clear you of diabetes.
There is one man in Malindi, I have heard that he prepares herbs for diabetes. There are several people, like ten people, have been cured of diabetes.
Given that the effectiveness and safety of such herbal remedies have not been established in clinical trials, such practices represent potentially ineffectual self-treatment of diabetes.
Foot care
Most of the participants did not practice any form of foot care on a regular basis, including foot inspection and/or caring for sores, abrasions, or cracks. Despite widespread complaints of foot pain with numbness and tingling, and dryness of feet and cracking, only 11 participants reported regularly inspecting their feet, and none of the participants had consulted a foot specialist for their problems. Many used footwear that did not adequately protect their feet. Due to the tropical climate, fully covering the feet with shoes and socks is uncommon among the Swahili. One participant explained that heat made it impossible to wear closed shoes such as sneakers.
Disease monitoring behavior
Most of the participants monitored blood glucose on a semi-regular basis at the Lamu Center of Preventative Health, a free clinic. We observed that the health care facilities in Lamu town monitored diabetes by checking fasting blood glucose. None of the health care facilities offered the hemoglobin A1C test for monitoring diabetes. In this study, only 11 participants owned a glucometer. Those who owned glucometers used them sparingly because glucose strips are costly and not easily available in Lamu town. Participants who owned glucometers reserved them for emergency situations, such as when they are ill.
Eye care
We noticed that eye care was minimally practiced. Only four participants consulted eye specialists on a regular basis. One reason for this lack of attention is that eye specialists are not regularly available in Lamu town, and participants have to travel to Mombasa to consult an optometrist or ophthalmologist. Some participants were unaware of the connection between vision loss and diabetes, and we observed that participants were not adequately informed about the long-term effects of diabetes on eye health.
Exercise
Only five participants (one woman and four men) in this study exercised at least 3 times per week and engaged in activities such as walking, swimming, or jogging. Most of the participants characterized walking to work and/or visiting family and friends around town as their only physical activity, which is minimal, given most of Lamu town’s neighborhoods are close by. A few male participants were in a profession that demanded more physical activity, including those who operated farms that were outside Lamu town, requiring them to walk to their farms or occasionally ride donkeys. There are gender differences in physical activity; women were culturally more sedentary than men, especially women who come from families that are economically better positioned and are better able to fulfill the cultural obligation of female seclusion, also known as purdah.
Factors That Affect Diabetes Self-Management
Each of the seven factors in Leininger’s sunrise model—educational, economic, political and legal dimensions, cultural values and beliefs, kinship and social life, religious and philosophical viewpoint, and technological context—was investigated for its influence on self-management of diabetes. All of the factors appeared to have an important influence on self-management of diabetes except political, legal, and technological factors. Table 2 provides more information about these factors, including samples of ethnographic descriptors.
Table 2.
Factors That Affect Self-Management of Diabetes.
| Themes | Subthemes | Ethnographic Descriptions |
|---|---|---|
| Economic factors | Poverty | “Because of poverty, I end up eating whatever I get.” “I don’t have regular food . . . somedays I get to eat and somedays I don’t get.” “I probably stay for two days without medications.” |
| Biomedical care is costly | “[Medications at] pharmacy are costly, we cannot afford them.” “I get my medications from Mombasa, here [in Lamu town] is very expensive.” |
|
| Poor access to eye care | “[eye care] . . . I keep rescheduling my appointments because I cannot afford travelling [to Mombasa].” | |
| No access to refrigeration | “. . . I was then told that the insulin will trouble you because you do not have refrigeration, and that is why they change to pills.” | |
| Educational factors—(limited knowledge and misconceptions of DM) | DM is curable | “It is possible that you can be cured and it leaves you.” “There are herbals that can totally clear you of diabetes.” “There is one man in Malindi, I have heard that he prepares herbs for diabetes. There are several people, like ten people have been cured of diabetes.” |
| Misconceptions about causes of DM | “I was informed yesterday that diabetes is infectious.” “Yes, you can infect someone. Because I did not have diabetes, my husband is the one who had diabetes. Why did I then get diabetes?” “One big thing that I have read in Arabic books is that ice water can cause diabetes and I have investigated and I have observed it.” |
|
| Misconceptions about DM self-management (exercise, diet) | “House chores are my only exercise.” “[Describes daily chores] . . . these are not small exercise.” “I for example, sometimes these days I do not eat breakfast because I think after dinner I’m satisfied until lunch.” |
|
| Religious factors | Fasting during the holy month of Ramadan | “My fasting goes very well during Ramadan.” “Some days I fast, some days I cannot because it is difficult.” “Ramadan is more difficult than any other times . . . It gives me plenty of problems.” |
| Social factors and kinship | Family factors | “You cannot tell your wife [family] that these days do not prepare this. Because you are the only one with diabetes . . . You must be flexible…the issue of dietary restrictions is problematic.” “You cannot cook your own food, until you cook food for others in the family . . . this is what I find to be difficult.” |
| Ritual obligations (wedding and social events) | “I do not eat the food . . . I do not stress the host of the event [about my food choices] . . . I excuse myself and sit somewhere until [when the event is over] I return home . . . ” “Most likely when I attend social events is to please the hosts instead of pleasing myself . . . the reason is when people drink soda, I do not . . . in Islamic religion to attend social events when you are invited is an obligation.” |
|
| Cultural values and belief systems | Pervasive use of non-biomedical remedies | “Yes, [aloe] I use it to lower my blood sugar.” “And for local medicine, I drink boiled papaya leaves.” |
| Fear and mistrust of medications (biomedical therapies) | “I have purchased medicines that were fake . . . it is known that some make fake drugs so they can make lots of quick cash.” “When they prescribe me pharmaceutical drugs, I refuse, because I have heard that once you are used to the medicine, you have to take them everyday.” “Others have told me that I should not take pharmaceutical drugs. I should only stick with dietary restrictions.” |
|
| Defeatist belief toward diabetes | “There are several people that I have met who do not care [about diabetes]. During social events such as wedding, prayers, or funeral, you will see them over eat . . . they tell me . . . you only die once.” |
Economic factors
Economic factors manifested themselves in participants’ poverty level, which affected the affordability of oral anti-diabetic medications, food security, access to recommended foods, and access to privately owned diabetes monitoring devices (glucometer and glucose strips). None of the participants had any form of health insurance, and they depended on spouses and close relatives to help them manage diabetes. The impact of poverty or food insecurity on diet was noted in the following statements:
Because of poverty, I end up eating whatever I get.
I don’t have regular food . . . somedays I get to eat and somedays I don’t get.
Also, the high cost of biomedical care affected some participants’ access to medications and glucose monitoring devices, which in turn affected adherence to diabetes self-management. This situation is illustrated by the following comments:
[Medications at] the pharmacy are costly, we cannot afford them.
I probably stay for two days without medications.
I get my medications from Mombasa, here [in Lamu town] is very expensive.
Lack of accessibility to refrigeration was another barrier to the use of insulin, which needs to be refrigerated. As one respondent noted,
. . . I was then told that the insulin will trouble you because you do not have refrigeration, and that is why they changed to pills.
This study demonstrates the multi-faceted ways that poverty affects diabetes self-management. The prevalent use of herbal remedies, which are more affordable than oral diabetic medications, is another example of how poverty shapes diabetes self-management.
Educational factors
In this study, we observed that education level influenced diabetes knowledge. Participants who had at least completed primary school education had more understanding of causes and complications of diabetes, and more effective self-management practices. Misconceptions about the causes of diabetes were more commonly observed among those who had less than an eighth-grade education. Although beliefs that diabetes can be transmitted via sexual intercourse or from a mosquito bite were not shared by most participants in this study, they were common among those who never attended school. Five participants believed that mosquitoes could transmit diabetes, and seven participants believed sexual intercourse with their spouses brought on diabetes. Comments regarding the general infectiousness of diabetes are illustrative:
I was informed yesterday that diabetes is infectious.
In our belief, the Swahili say, if a person with diabetes enters the bathroom and urinates, and then you enter the bathroom afterwards, you can get it [diabetes].
Educational level has a unique interaction with age and gender, as suggested by the fact that of the 30 participants in the study, all five of the participants who were illiterate were women who were 47 years of age or older. The likely explanation for the gender and age effect is that women in Swahili culture were more socially constricted in terms of mobility 50 years ago. Over time, the society has become more accepting of women seeking educational opportunities.
Religious factors
Religious rituals such as fasting were reported to influence diabetes SMB. Fasting during the holy month of Ramadan is an obligatory practice reported by all participants. Fasting was described as having both positive and negative impacts on diabetes self-management. Although fasting promoted good control of diabetes and adherence to dietary restrictions during the day, it promoted a “do not care” attitude about consuming high-calorie specialty foods served during meals in the evening. The three quotes below were extracted from conversations with participants about fasting with diabetes.
My fasting goes very well during Ramadan.
Some days I fast, some days I cannot because it is difficult.
Ramadan is more difficult than any other times . . . It gives me plenty of problems.
There are deep-rooted religious and ideological beliefs in the Swahili community that fasting promotes purity, which in turn promotes wellness (Abdulrehman & Gearhart, 2012), which may explain the overall positive attitude toward fasting during Ramadan. In contrast, the lived experience among those with diabetes during fasting highlights the difficulties associated with dehydration during fasting hours, and binge eating at sundown.
Kinship and social factors
Kinship and religion influenced self-management of diabetes in terms of participants’ obligations to their families and their religion, including participating in ritual practices and upholding prescribed gender roles. In terms of family obligations, we noted that both male and female participants complained of the difficulty of changing the dietary habits of the whole family based on one person’s illness. In the Swahili cultural context, family needs are more important than individual needs. Participants also reported that making separate meals for family and self (in the case of women) was difficult due to the extra time and cost of food involved. Food preparation in the Swahili context is complex because everything is made from scratch, and ready-to-cook items are either unavailable or cost-prohibitive. The following are some of the comments made by participants about family and meal preparation:
You cannot tell your wife that these days do not prepare this. Because you are the only one with diabetes. . . . You must be flexible . . . the issue of dietary restrictions is problematic.
You cannot cook your own food until you cook food for others in the family . . . this is what I find to be difficult.
Ritual obligations observed among the Swahili of Lamu town were reported as having an undesirable influence on participants’ SMB. Attending events such as wedding feasts, which last for several days in a row, is motivated by an obligation to support the Islamic marriage ritual and to build social ties. Although participants described wedding events as detrimental to maintaining dietary restrictions, they continued to regularly attend them to fulfill their religious duty and maintain and build connections with those in attendance. In a resource-poor environment, a network of people who provide social support is necessary for getting by on a daily basis as well as during medical and other crises. The quotes below illustrate how participants explained the significance of attending social events while also expressing the feelings of social alienation associated with the inability to fully enjoy feasting, which is central to Swahili culture.
Most likely when I attend social events it is to please the hosts instead of pleasing myself . . . the reason is when people drink soda, I do not . . . in Islamic religion to attend social events when you are invited is an obligation.
I do not eat the food . . . I do not stress the host of the event [about my food choices] . . . I excuse myself and sit somewhere until [when the event is over] I return home . . .
Peer pressure at weddings was observed to have a deleterious effect on SMB because it encourages overeating. Participants explained that it is very difficult to abstain from eating certain foods at wedding feasts, where large plates of food are shared with three or four other people. Swahili men in particular are obliged to overeat at such feasts, and it is common for men to encourage each other to consume much more than they would eat at a regular meal. The Swahili believe that eating the food served at a wedding feast is a ritual obligation that sanctifies the occasion and brings blessings to the family hosting the event, especially the newlyweds.
Although female participants reported self-monitoring of blood glucose more regularly than their male counterparts did, women’s religious obligation to practice seclusion negatively affected their SMB. Although one woman reported that she regularly got together with her friends to exercise, female participants were less likely to participate in regular formal exercise compared with male participants. This is primarily because women were less likely to feel comfortable exercising in public.
Social support had a positive influence on diabetes self-management. Participants reported that support from relatives, friends, and neighbors encouraged their SMB. The family support system played an important role in terms of helping to pay for medications or facilitating with disease monitoring.
Cultural values and beliefs
Factors relating to Swahili cultural values and belief systems that affect SMB include the pervasive use of non-biomedical remedies, fear and mistrust of biomedical therapies, and a defeatist attitude toward diabetes. Herbal remedies were used independently and in conjunction with oral diabetes medications. Herbal remedies were more affordable, and some participants believed they are more effective than pharmaceutical products at lowering blood sugar.
Yes, [aloe] I use it to lower my blood sugar.
And for local medicine, I drink boiled papaya leaves.
In terms of fear and mistrust, some participants reported avoiding oral anti-diabetic medications and/or insulin due to fear of becoming dependent on them and not being able to live without them. There is also general mistrust of the Kenyan pharmaceutical industry. One participant believed that local pharmacies were producing fake medications. Although negative attitudes toward pharmaceutical drugs were not common among participants, some of their statements do suggest negative sentiment:
I have purchased medicines that were fake . . . it is known that some make fake drugs so they can make lots of quick cash.
When they prescribe me pharmaceutical drugs, I refuse, because I have heard that once you are used to the medicine, you have to take them everyday.
A defeatist attitude toward diabetes was also reported among participants, who viewed having diabetes as equivalent to being served a death warrant. For example, one participant said that her friends told her nothing can help diabetes except a grave. Below is a comment from a participant that reflects a defeatist attitude toward diabetes.
There are several people that I have met who do not care [about diabetes]. During social events such as wedding, prayers, or funeral, you will see them overeat . . . they tell me . . . you only die once.
Cultural values and beliefs greatly influence how people understand and treat diabetes. As noted in the statement above, some of these behaviors have a deleterious effect on diabetes self-management.
Discussion
This study reveals many important factors that affect self-management of diabetes among the Swahili of Lamu town, and adds new knowledge about diabetes self-care in coastal Kenya. This study’s most significant contribution is showing how culture can affect self-management of diabetes in multiple ways, including knowledge (prevalence of misconceptions and limited understanding of diabetes), beliefs (herbals can cure diabetes), treatment (medical pluralism in diabetes management), food (feasting and fasting during rituals), and values (family needs supersede individual needs).
In addition to examining the factors that affect diabetes SMB using Leininger’s sunrise model, this study’s other significant contribution is showing how poverty impedes access to health care and negatively affects diabetes self-management. This study demonstrates that among low-income participants, economic barriers are the most outstanding problem in diabetes management in coastal Kenya. Our findings support findings from other studies in Africa that demonstrate that the high cost of drugs makes it difficult for people living on low income to enjoy the full benefits of biomedical care (Aikins, 2005; Awah, Unwin, & Phillimore, 2008; BeLue et al., 2012; Hjelm & Beebwa, 2013; Hjelm & Mufunda, 2010; Popoola, 2005). Similar to our study, others conducted in sub-Saharan Africa demonstrate that economic barriers such as poverty make it difficult to afford drugs (Aikins, 2003, 2005; Popoola, 2005), disease monitoring supplies (Abdelgadir, Elbagir, Eltom, & Berne, 2006; Hjelm & Beebwa, 2013), and the recommended diet (Muchiri, Gericke, & Rheeder, 2012).
Another significant finding in our study relates to the limited understanding of diabetes and the prevalence of misconceptions related to the disease. This has been described as a barrier to diabetes self-management in several other African countries, including South Africa (Muchiri et al., 2012, Shilubane & Potgieter, 2007), Uganda (Hjelm & Beebwa, 2013; Hjelm & Nambozi, 2008), and Zimbabwe (Hjelm & Mufunda, 2010; Mufunda, Wikby, Bjorn, & Hjelm, 2012). Misconceptions documented in this study are that diabetes is curable (Aikins, 2005; Awah et al., 2008; Shilubane & Potgieter, 2007) and that diabetes can be transmitted through sexual intercourse and mosquito bites (Fezeu, Fointama, Ngufor, Mbeh, & Mbanya, 2010). Some studies have linked misconceptions and local beliefs about diabetes to social stigma and social ostracism, which has been reported in Ghana, Cameroon, and Uganda (Aikins, 2003; Awah et al., 2008; Hjelm & Beebwa, 2013). No such stigma was found in this study among the Swahili of Lamu town, Kenya, however.
This study also points to an undeniable role of medical plurality in diabetes self-management among the Swahili of Lamu town, Kenya, where biomedical therapies were used alongside herbal remedies. Fifty percent of the sample reported using local herbal remedies, a finding supported by other studies conducted in Africa that similarly document the use of herbal and traditional medicine among those with diabetes. Herbal and traditional medicine was reported among 33% of those with diabetes in Guinea (Balde et al., 2006), and among 61% of those with diabetes in Morocco (Ziyyat et al., 1997). Complementary and alternative medicine (CAM) use was reported among 46% of those with diabetes in Nigeria (Ogbera, Dada, Adeleya, & Jewo, 2010) and among 38.5% of the South Africans with diabetes (Singh, Raidoo, & Harries, 2004). Seventy-four percent of those sampled in Guinea believed in the efficacy of traditional and herbal medicine for the treatment of type 2 diabetes (Balde et al., 2006). The lesson here is that clinicians and researchers should not downplay the role of non-biomedical modalities in diabetes care, because there is enough evidence to suggest that their use in type 2 diabetes management is prevalent in Africa (Balde et al., 2006; Keter & Mutiso, 2012; Moshi, Otieno, & Weisheit, 2012; Ogbera et al., 2010; Semenya, Potgieter, & Erasmus, 2012; Singh et al., 2004; Tchacondo et al., 2012).
When discussing diabetes in the African context, it is important to consider the role of food culture. In Swahili communities in Kenya, foods are deemed to possess curative and medicinal properties (Beckerleg, 1994), and among the Swahili peoples of Lamu town, food serves an important socio-cultural role, especially at events such as weddings, where relatives and close friends share food from the same plate, an important tradition that signifies solidarity, promotes kinship ties, and provides an opportunity to build social wealth. Okoror et al.’s (2007) study on people with HIV/AIDS in South Africa described food sharing as a socio-cultural process with complex meaning and roles. In our study, we observed that the social-cultural norms associated with ritualized food consumption pose a major challenge to diabetes self-management, as diverging from these norms is extremely challenging.
Limitations
There are several limitations that are tied to investigator bias that are worth mentioning. First of all, the PI’s social status is higher than most members of the Swahili community in Lamu town because of his status as a clinician and as an educated member of the community. This is relevant because it situates the PI in a position of authority over the participants, which could affect the quality of data collected. Although this power differential cannot be erased, the PI had a brief discussion with participants about this issue, and assured them that the purpose of the interviews was not to judge them or to provide a diagnosis for any illnesses they have.
Second, the PI is also the director of the Lamu Center of Preventative Health (LCPH), a clinic that offers free health care for the Lamu community. To avoid the risk of coercion, it was important for the PI to separate the research from his work at LCPH. This was difficult because despite physically separating this research from the clinical care he provides at LCPH, the PI’s name is synonymous with LCPH. In spite of these challenges, the PI did maintain an honest dialogue with participants to explain his role as a researcher outside the clinical setting.
Third, the PI worked with a female research assistant from Lamu town, which presented another concern relating to investigator bias. A female research assistant was hired because we expected some challenges associated with gender stratification, a common cultural practice of the Swahili of Lamu town. To enhance the comfort of female participants, the female research assistant accompanied the male PI during interviews with female research participants.
In spite of these limitations, this study has several strengths. Among them is the fact that this is the first exploratory study of diabetes self-management in Kenya. This study provides foundational knowledge of diabetes self-management in the context of a limited resource environment, and it provides an important understanding of participants’ daily self-management experiences with diabetes. Most importantly, this ethnographic study provides a holistic understanding of the myriad of factors that affect diabetes self-management, not limited to individual factors, family factors, or socio-cultural factors. This study contributes to this holistic perspective on diabetes self-management, an important area for continued research.
Conclusion
This study has established that self-management activities, such as dietary restrictions, foot care, exercise, and eye care, were inadequately practiced, and that herbal remedies are a vital component to diabetes care among the Swahili of Lamu town, Kenya. The most outstanding lesson here is that economic, educational, and cultural influences play important roles in diabetes self-management in this limited resource environment, where biomedical care might be not be easily accessible and/or affordable. To improve diabetes care in this context, we need to look at this problem holistically to address each of the relevant factors in a culturally competent manner. This study paves the way for developing culturally tailored, community-centered interventions to curb diabetes and enhance self-management among Swahili patients. Situating the Swahili people of Kenya within a larger framework of diabetes-related issues in Africa provides a better understanding of how culturally tailored diabetes intervention can improve health outcomes.
Author Biographies
Munib Said Abdulrehman, PhD, FNP-BC, APN, is a 2014 graduate of Mennonite College of Nursing at Illinois State University, Normal, Illinois. He is also the executive director of the Lamu Center of Preventative Health, in Lamu, Kenya.
Wendy Woith, PhD, RN, FAAN, is an associate professor at Mennonite College of Nursing at Illinois State University, Normal, Illinois.
Sheryl Jenkins, PhD, ACNP, APN, is an associate professor at Mennonite College of Nursing at Illinois State University, Normal, Illinois.
Susan Kossman, PhD, RN, is an associate professor at Mennonite College of Nursing at Illinois State University, Normal, Illinois.
Gina Louise Hunter, PhD, is an associate professor of anthropology at Illinois State University, Normal, Illinois.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: From Illinois State University, the primary investigator (PI) received Dissertation Research Grant and Dissertation Completion Grant. Also, the PI received a grant from Sigma Theta Tau International, Xi Pi Chapter.
References
- Abdelgadir M., Elbagir M., Eltom M., Berne C. (2006). The influence of glucose self-monitoring on glycaemic control in patients with diabetes mellitus in Sudan. Diabetes Research and Clinical Practice, 74, 90–94. [DOI] [PubMed] [Google Scholar]
- Abdulrehman M. S. (2015). Reflections on native ethnography by a nurse researcher. Journal of Transcultural Nursing. Advance online publication. doi: 10.1177/1043659615620658 [DOI] [PubMed] [Google Scholar]
- Abdulrehman M. S., Gearhart R. (2012). Purity, balance and wellness among the Swahili of Lamu, Kenya. The Journal of Global Health, 2(1), 42–44. [Google Scholar]
- Aikins A. D. (2003). Living with diabetes in rural and urban Ghana: A critical social psychological examination of illness action and scope for intervention. Journal of Health Psychology, 8, 557–572. [DOI] [PubMed] [Google Scholar]
- Aikins A. D. (2005). Healer shopping in Africa: New evidence from rural-urban qualitative study of Ghanaian diabetes experiences. British Medical Journal, 331, 737–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J. V. (1993). Swahili origins: Swahili culture and the Shungwaya phenomenon. London, England: James Currey. [Google Scholar]
- Awah P., Unwin N., Phillimore P. (2008). Cure or control: Complying with biomedical regime of diabetes in Cameroon. BMC Health Services Research, 8(43), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balde N. M., Youla A., Balde M. D., Kake A., Diallo M. M., Balde M. A., Maugendre D. (2006). Herbal medicine and treatment of diabetes in Africa: An example from Guinea. Diabetes & Metabolism, 32, 171–175. [DOI] [PubMed] [Google Scholar]
- Beckerleg S. (1994). Medical pluralism and Islam in Swahili communities in Kenya. Medical Anthropology Quarterly, 8, 299–313. [Google Scholar]
- BeLue R., Diaw M., Ndao F., Okoror T., Degboe A., Abiero B. (2012). A cultural lens to understanding daily experiences with type 2 diabetes self-management among clinic patients in M’bour, Senegal. International Quarterly Of Community Health Education, 33(4), 329–347. [DOI] [PubMed] [Google Scholar]
- Casarez R. L., Engebretson J. C., Ostwald S. K. (2010). Spiritual practices in self-management of diabetes in African Americans. Holistic Nursing Practice, 24, 227–237. [DOI] [PubMed] [Google Scholar]
- Christensen D., Friis H., Mwaniki D., Kilonzo B., Tetens I., Boit M., . . . Borch-Johnsen K. (2009). Prevalence of glucose intolerance and associated risk factors in rural and urban populations of different ethnic groups in Kenya. Diabetes Research and Clinical Practice, 84, 303–310. [DOI] [PubMed] [Google Scholar]
- Egede L. E., Bonadonna R. J. (2003). Diabetes self-management in African Americans: An exploration of the role of fatalism. Diabetes Educator, 29, 105–115. [DOI] [PubMed] [Google Scholar]
- Fetterman D. M. (2010). Ethnography: Step-by-step. Los Angeles: Sage. [Google Scholar]
- Fezeu L., Fointama E., Ngufor G., Mbeh G., Mbanya J. C. (2010). Diabetes awareness in general population in Cameroon. Diabetes Research and Clinical Practice, 90, 312–318. [DOI] [PubMed] [Google Scholar]
- Gearhart R., Abdulrehman M. S. (2014). Concepts of illness among the Swahili of Lamu, Kenya. Journal of Transcultural Nursing, 25, 218–222. doi: 10.1177/1043659613515713 [DOI] [PubMed] [Google Scholar]
- Halcomb E. J., Davidson P. M. (2006). Is verbatim transcription of interview data always necessary? Applied Nursing Research, 19, 38–42. [DOI] [PubMed] [Google Scholar]
- Hall V., Thomsen R. W., Henrinksen O., Lohse N. (2011). Diabetes in Sub Saharan Africa 1999-2011: Epidemiology and public health implications: A systematic review. BMC Public Health, 11, 564–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrowing J. N., Mill J. J., Spiers J. J., Kulig J. J., Kipp W. W. (2010). Culture, context and community: Ethical considerations for global nursing research. International Nursing Review, 57, 70–77. doi: 10.1111/j.1466-7657.2009.00766.x [DOI] [PubMed] [Google Scholar]
- Hendriks M. E., Wit F. W., Roos M. T. (2012). Hypertension in sub-Saharan Africa: Cross-sectional surveys in four rural and urban communities. PLoS ONE, 7(3), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjelm K., Beebwa E. (2013). The influence of beliefs about health and illness on foot care in Ugandan persons with diabetic foot ulcers. The Open Nursing Journal, 7, 123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjelm K., Mufunda E. (2010). Zimbabwean diabetics’ beliefs about health and illness: An interview study. BMC International Health and Human Rights, 10(7), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjelm K., Nambozi G. (2008). Beliefs about health and illness: A comparison between Ugandan men and women living with diabetes mellitus. International Nursing Review, 55, 434–441. [DOI] [PubMed] [Google Scholar]
- Human Development Report. (2009). Kenya national human development report 2009. Retrieved from http://planipolis.iiep.unesco.org/upload/Kenya/KenyaNationalHumanDevelopmentReport2009.pdf
- International Diabetes Federation. (2015). Kenya. Retrieved from http://www.idf.org/membership/afr/kenya
- Joo J. Y. (2014). Effectiveness of culturally tailored diabetes interventions for Asian immigrants to the United States: A systematic review. The Diabetes Educator, 40, 605–615. doi: 10.1177/0145721714534994 [DOI] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics. (2010). The 2009 Kenya population and housing census: “Counting our people for the implementation of vision 2030.” Volume 1A-Population Distribution by Administrative Units; Retrieved from http://www.knbs.or.ke/index.php?option=com_phocadownload&view=categories&Itemid=599 [Google Scholar]
- Keter L. K., Mutiso P. C. (2012). Ethnobotanical studies of medicinal plants used by traditional health practitioners in the management of diabetes in lower eastern province, Kenya. Journal of Ethnopharmacology, 139, 74–80. [DOI] [PubMed] [Google Scholar]
- Kim M., Han H., Song H., Lee J., Kim J., Ryu J., Kim K. B. (2009). A community-based, culturally tailored behavioral intervention for Korean Americans with type 2 diabetes. Diabetes Educator, 35, 986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kithinji C., Kass N. E. (2010). Assessing the readability of non-English-language consent forms: The case of Kiswahili for research conducted in Kenya. IRB: Ethics & Human Research, 32(4), 10–15. [PMC free article] [PubMed] [Google Scholar]
- Leininger M. M. (Ed.). (1985). Qualitative research methods in nursing. Orlando, FL: Grune & Stratton. [Google Scholar]
- Leininger M. M. (2002). Culture care theory: A major contribution to advance transcultural nursing knowledge and practices. Journal of Transcultural Nursing, 13 189–192. [DOI] [PubMed] [Google Scholar]
- Leininger M. M., McFarland M. R. (Eds.). (2006). Culture care diversity and universality: A worldwide nursing theory. Sudbury, MA: Jones & Bartlett. [Google Scholar]
- Lincoln Y. S., Guba E. G. (1985). Naturalistic inquiry. Newbury Park, CA: Sage. [Google Scholar]
- Lipson J. G. (1989). The use of self in ethnographic research. In Morse J. M. (Ed.), Qualitative nursing research: A contemporary dialogue (pp. 61–75). Rockville, MD: Aspen. [Google Scholar]
- Lipton R. B., Losey L. M., Giachello A., Mendez J., Girotti M. H. (1998). Attitudes and issues in treating Latino patients with type 2 diabetes: Views of healthcare providers. Diabetes Educator, 24, 67–71. [DOI] [PubMed] [Google Scholar]
- Matheka D. M., Kilonzo J. M., Munguti C. M., Mwangi P. W. (2013). Pattern, knowledge and practices of HbA1C testing among diabetic patients in a Kenyan tertiary referral hospital. Global Health, 9(55), 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathenge W., Foster A., Kuper H. (2010). Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: A population-based survey. BMC Public Health, 10, 569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbugua P. K., Otieno C. F., Kayima J. K., Amayo A. A., McLigeyo S. O. (2005). Diabetic ketoacidosis: Clinical presentation and precipitating factors at Kenyatta national hospital, Nairobi. The East African Medical Journal, 82, 191–196. [DOI] [PubMed] [Google Scholar]
- Moshi M. J., Otieno D. F., Weisheit A. (2012). Ethnomedicine of the Kagera Region, north western Tanzania. Part 3: Plants used in traditional medicine in Kikuku village, Muleba District. Journal of Ethnobiology and Ethnomedicine, 8(1), 14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muchiri J. W., Gericke G. J., Rheeder P. (2012). Needs and preferences for nutrition education of type 2 diabetic adults in a resource-limited setting in South Africa. Health SA Gesondheid, 17(1), 1–13. [Google Scholar]
- Mufunda E., Wikby K., Bjorn A., Hjelm K. (2012). Level and determinants of diabetes knowledge in patients with diabetes in Zimbabwe: A cross-sectional study. Pan African Medical Journal, 13(78), 1–14. [PMC free article] [PubMed] [Google Scholar]
- Mutea N. K., Baker C. M. (2008). Kenyan nurses. International Journal of Nursing Practice, 14, 40–46. [DOI] [PubMed] [Google Scholar]
- Muthuuri J. M. (2007). Characteristics of patients with diabetic foot in Mombasa, Kenya. The East African Medical Journal, 84, 251–258. [DOI] [PubMed] [Google Scholar]
- Nyamu P. N., Otieno C. F., Amayo E. O., McLigeyo S. O. (2003). Risk factors and prevalence of diabetic foot ulcers at Kenyatta national hospital, Nairobi. The East African Medical Journal, 80(1), 36–43. [DOI] [PubMed] [Google Scholar]
- Ogbera A. O., Dada O., Adeleya O., Jewo P. I. (2010). Complimentary and alternative medicine use in diabetes mellitus. West African Journal of Medicine, 29, 158–162. [DOI] [PubMed] [Google Scholar]
- Okoror T. A., Airhihenbuwa C. O., Zungu M., Mokofani D., Brown D. C., Iwelunmor J. (2007). “My mother told me I must not cook anymore”—Food, culture, and the context of HIV- And AIDS-related stigma in three communities in South Africa. International Quarterly of Community Health Education, 28, 201–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otieno C. F., Huho A. N., Omonge E. O., Amayo A. A., Njagi E. (2008). Type 2 diabetes mellitus: Clinical and aetiologic types, therapy and quality of glycaemic control of ambulatory patients. East African Medical Journal, 85, 24–29. [DOI] [PubMed] [Google Scholar]
- Otieno C. F., Kariuki M. M., Ng’ang’a L. L. (2003). Quality of glycaemic control in ambulatory diabetics at the out-patient clinic of Kenyatta National Hospital, Nairobi. East African Medical Journal, 80, 406–410. [DOI] [PubMed] [Google Scholar]
- Pastakia S. D., Karwa R., Kahn C. B., Nyabundi J. S. (2011). The evolution of diabetes care in the rural, resource-constrained setting of western Kenya. The Annals of Pharmacotherapy, 45, 721–726. [DOI] [PubMed] [Google Scholar]
- Popoola M. M. (2005). Living with diabetes: The holistic experiences of Nigerians and African Americans. Holistic Nursing Practice, 19(1), 10–16. [DOI] [PubMed] [Google Scholar]
- Reynolds C. L., Leininger M. M. (1993). Madeleine Leininger: Cultural care diversity and universality theory. Newbury Park, CA: Sage. [Google Scholar]
- Semenya S., Potgieter M., Erasmus L. (2012). Ethnobotanical survey of medicinal plants used by Bapedi healers to treat diabetes mellitus in the Limpopo province, South Africa. Journal of Ethnopharmacology, 141, 440–445. [DOI] [PubMed] [Google Scholar]
- Shilubane H. N., Potgieter E. (2007). Patients’ and family members’ knowledge and views regarding diabetes mellitus and its treatment. Curationis, 30(2), 58–65. [DOI] [PubMed] [Google Scholar]
- Silverman D. (1993). Interpreting qualitative data. London: Sage. [Google Scholar]
- Singh V., Raidoo D., Harries C. (2004). The prevalence, patterns of usage and people’s attitude towards complementary and alternative medicine (CAM) among the Indian community in Chatsworth, South Africa. BMC Complementary & Alternative Medicine, 4(3), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skelly A. H. (2011). Culturally tailored intervention for African Americans with type 2 diabetes administered by a nurse case manager and community health worker reduces emergency room visits. Evidenced-Based Nursing, 13, 51–52. [DOI] [PubMed] [Google Scholar]
- Streubert H. J., Carpenter D. R. (2011). Qualitative research in nursing: Advancing the human imperative (5th Ed.). Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- Tchacondo T., Karou S. D., Agban A., Bako M., Batawila K., Bawa M. L., . . . de Souza C. (2012). Medicinal plants use in central Togo (Africa) with an emphasis on the timing. Pharmacognosy Research, 4, 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripp-Reimer T., Choi E., Kelley S., Enslein J. (2001). Cultural barriers to care: Inverting the problem. Diabetes Spectrum, 14, 13–22. [Google Scholar]
- United Nations Educational, Scientific and Cultural Organization. (2008). The development and state of art of adult learning and education: National report of Kenya. Retrieved from http://www.unesco.org/fileadmin/MULTIMEDIA/INSTITUTES/UIL/confintea/pdf/National_Reports/Africa/Africa/Kenya.pdf
- Van Maanen J. (1995). An end of innocence: Ethnography of ethnography. In Van Maanen J. (Ed.), Representation in ethnography (pp. 1–35). Thousand Oaks, CA: Sage. [Google Scholar]
- Vincent D. (2009). Culturally tailored education to promote lifestyle change in Mexican Americans with type 2 diabetes. Journal of the American Academy of Nurse Practitioners, 21, 520–527. doi: 10.1111/j.1745-7599.2009.00439.x [DOI] [PubMed] [Google Scholar]
- Ziyyat A., Legssyer A., Mekhfi H., Dassouli A., Serhrouchni M., Benjelloun W. (1997). Phytotherapy of hypertension and diabetes in oriental Morocco. Journal of Ethnopharmacology, 58, 45–54. [DOI] [PubMed] [Google Scholar]


