Abstract
Although focus groups are commonly used in health research to explore the perspectives of patients or health care professionals, few studies consider methodological aspects in this specific context. For this reason, we interviewed nine researchers who had conducted focus groups in the context of a project devoted to the development of an electronic personal health record. We performed qualitative content analysis on the interview data relating to recruitment, communication between the focus group participants, and appraisal of the focus group method. The interview data revealed aspects of the focus group method that are particularly relevant for health research and that should be considered in that context. They include, for example, the preferability of face-to-face recruitment, the necessity to allow participants in patient groups sufficient time to introduce themselves, and the use of methods such as participant-generated cards and prioritization.
Keywords: cancer, content analysis, focus groups, health care administration, electronic personal health record, research, qualitative, technology
Focus groups have been widely used in health research in recent years to explore the perspectives of patients and other groups in the health care system (e.g., Carr et al., 2003; Côté-Arsenault & Morrison-Beedy, 2005; Kitzinger, 2006). They are often included in mixed-methods studies to gain more information on how to construct questionnaires or interpret results (Creswell & Plano Clark, 2007; Kroll, Neri, & Miller, 2005).
The fact that the group process helps people to identify and clarify their views is considered to be an important advantage of focus groups compared with individual interviews (Kitzinger, 1995). The group functions as a promoter of synergy and spontaneity by encouraging the participants to comment, explain, disagree, and share their views. Thus, experiences are shared and opinions voiced that might not surface during individual interviews (Carey, 1994; Stewart, Shamdasani, & Rook, 2007). Although focus groups allow participants to respond in their own words and to choose discussion topics themselves, they are not completely unstructured. Questions relating to the research topic are designed by the researchers and are used to guide the discussion (Stewart et al., 2007). The degree of structure of the focus group depends on the openness of the research question(s). Hence, although it takes more time and effort to organize focus groups, and they cause greater logistical problems than individual interviews do, they might generate more ideas about, and yield deeper insights into, the problem under investigation (Coenen, Stamm, Stucki, & Cieza, 2012; Kingry, Tiedje, & Friedman, 1990; Morgan, 2009).
Historically, focus groups were used mainly for market research before the method was adopted for application in qualitative research in the social sciences (Morgan, 1996). The use of focus groups in health care research is even more recent. For this reason, methodological recommendations on using focus groups in the health care context are quite rare, and researchers rely mainly on general advice from the social sciences (e.g., Krueger, 1988; Morgan, 1993; Morgan & Krueger, 1998; Stewart et al., 2007). Even though focus groups have been used in a great variety of health research fields, such as patients’ treatments and perceptions in the context of specific illnesses (rheumatoid arthritis: for example, Feldthusen, Björk, Forsblad-d’Elia, & Mannerkorpi, 2013; cancer: for example, Gerber, Hamann, Rasco, Woodruff, & Lee, 2012; diabetes: for example, Nafees, Lloyd, Kennedy-Martin, & Hynd, 2006; heart failure: for example, Rasmusson et al., 2014), community health research (e.g., Daley et al., 2010; Rhodes, Hergenrather, Wilkin, Alegría-Ortega, & Montaño, 2006), or invention of new diagnostic or therapeutic methods (e.g., Vincent, Clark, Marquez Zimmer, & Sanchez, 2006), the method and its particular use in health research is rarely reflected. Methodological articles about the focus group method in health care journals mainly summarize general advice from the social sciences (e.g., Kingry et al., 1990; Kitzinger, 1995, 2006), while field-specific aspects of the target groups (patients, doctors, other medical staff) and the research questions (not only sociological but often also medical or technical) are seldom addressed. Reports on participant recruitment and methods of conducting the focus groups are primarily episodic in nature (e.g., Coenen et al., 2012; Côté-Arsenault & Morrison-Beedy, 2005) and often focus on very specific aspects of the method (communication: for example, Lehoux, Poland, & Daudelin, 2006; activating methods: for example, Colucci, 2007) or aim at a comparison between face-to-face focus groups and other methods (individual interviews: for example, Coenen et al., 2012; telephone groups: for example, Frazier et al., 2010; Internet groups: for example, Nicholas et al., 2010). Thus, systematic reviews of factors influencing the results of focus groups as well as advantages, disadvantages, and pitfalls are missing. One consequence is that researchers might find it difficult to recruit enough participants or might be surprised by the communication styles of the target groups. Furthermore, in the tradition of classical clinical research, the group discussions might result in a question-and-answer situation or “resemble individual interviews done in group settings” (Colucci, 2007, p. 1,424), thereby missing out on the opportunity to use the group setting to activate all participants and to encourage a deeper elaboration of their ideas. Colucci, for example, proposed the use of exercises (e.g., activity-oriented questions) to focus the attention of the group on the core topic and to facilitate subsequent analyses.
Recommendations from the social sciences on using the focus group method can be subsumed under the following headings: subjects (target groups, composition of groups, recruitment), communication in the groups (discussion guide, moderator, moderating techniques), and analysis of focus groups (e.g., Morgan, 1993; Morgan & Krueger, 1998; Stewart et al., 2007). Specific requirements for health research can be identified in all three thematic fields: Recruitment might be facilitated by using registers of quality circles to recruit physicians or pharmacists, or by recruiting patients in outpatients departments. It might be hampered by heavy burdens on target groups—be they time burdens (e.g., clinical schedules, time-consuming therapy) or health constraints (e.g., physical fitness). With regard to communication in focus groups, finding suitable locations, identifying optimal group sizes, planning a good time line, as well as selecting suitable moderators (e.g., persons who are capable of translating medical terms into everyday language) might pose a challenge. The analysis of focus groups in health care research might also require special procedures because the focus group method is used to answer not only sociological research questions (e.g., related to the reconstruction of the perspectives of target groups) but also more specific research questions, such as user requirements with regard to written information or technical innovations.
The aim of our study was to gather more systematic methodological information for conducting focus groups in the context of health research in general and in the more specific context of the implementation of a technical innovation. To this end, we conducted interviews with focus group moderators about their experiences when planning and moderating focus groups. The groups in question were part of a research program aimed at developing and evaluating an electronic personal health record. We chose this program for several reasons: First, because it consisted of several subprojects devoted to different research topics related to the development of a personal electronic health record, it offered a variety of research content (cf. next section). Second, the focus groups were conducted to answer research questions of varying breadth, which can be regarded as typical of research in health care. Third, the focus groups comprised a variety of target groups—not only patients but also different types of health care professionals (general practitioners, independent specialists with different areas of specialization, hospital doctors, pharmacists, medical assistants, nursing staff).
In this article, we report the findings of these interviews in relation to the following questions: (a) What challenges associated with the characteristics of the target groups of health research (patients, physicians, other health care professionals) might be considered during the recruitment process? How should the specific research question relating to a technical innovation be taken into account during the recruitment process? (b) Should specific aspects of the communication styles of target groups be taken into account when planning and moderating focus groups in health care? Can additional challenges be identified in relation to the technical research question? and (c) How was the method appraised by the interviewees in their own research context?
Method
Research Program and Description of Focus Groups
The “Information Technology for Patient-Centered Health Care” (INFOPAT) research program (www.infopat.eu) addresses the fact that, because patients with chronic conditions (e.g., colorectal cancer, type 2 diabetes) have complex health care needs, many personal health data are collected in different health care settings. The aim of the program is to develop and evaluate an electronic personal health record aimed at improving regional health care for chronically ill people and strengthening patients’ participation in their health care process. Subprojects are devoted, for example, to developing the personal electronic health record (Project Cluster 1), a medication platform (Project Cluster 2), and a case management system for chronically ill patients (Project Cluster 3). In the first, qualitative, phase, the researchers explored patients’ and health care professionals’ experiences with cross-sectoral health care and patient self-management, and their expectations regarding the advantages and disadvantages of a personal electronic health record. The information gathered in this phase of the program served as a basis for constructing a personal electronic health record prototype. This prototype was implemented as an intervention in a second, quantitative, phase dedicated to investigating the impact of such a record on a range of health care variables (e.g., self-management, health status, patient–doctor relationship, compliance). The University Hospital Heidelberg Ethics Committee approved the studies of the INFOPAT research program. All participants gave their written informed consent, and the participants’ anonymity and confidentiality were ensured throughout the studies according to the ethical standards of German Sociological Association.1
Twenty-one focus groups were conducted during the qualitative phase of the program. Three groups consisted of colorectal cancer patients, four comprised type 2 diabetes patients, four were made up of physicians, three comprised physicians and pharmacists, four consisted of physicians and other health care professionals, and three consisted of other health care professionals (for more detailed information, see Tausch & Menold, 2015). Participants were recruited from urban and rural districts of the Rhine-Neckar region in Germany. Patients were approached in clinics, by their local general practitioners, or in self-help groups. Health care professionals were recruited in clinics, cooperating medical practices, and professional networks.
The focus groups took place at several locations at the National Center of Tumor Diseases (NCT) in Heidelberg, Germany, and the University of Heidelberg. The groups consisted of between four and seven participants and lasted between 1.5 and 2 hours. All focus groups were conducted by two researchers—a moderator and a co-moderator; a third researcher took notes. Semistructured discussion guides were used, and the groups were video- and audio recorded (cf., for example, Baudendistel et al., 2015; Kamradt et al., 2015). The researchers performed content analysis on the transcripts; the schema of categories was oriented toward the research questions. The focus groups addressed research questions of varying breadth, including, for example, individual health care experiences (comparatively broad), the expected impact of the record on the patient–doctor relationship (medium breadth), and technical requirements for such a personal health record (comparatively narrow). The variety of the research questions was important for our study because it proved to be of relevance for the interviewees’ appraisal of the usefulness of the focus group method.
Interviews With the Focus Group Moderators
We conducted qualitative interviews with nine of the 10 focus group moderators in the INFOPAT program (one moderator moved to a different department shortly after the completion of data collection and was not available for interview). The interviewees were aged between 30 and 54 years (M age = 36 years; SD = 8.3 years). Their professions were health scientist, pharmacist, general practitioner, or medical ethicist. Their professional experience ranged from one to 23 years (M = 7.1 years, SD = 7.7 years), and they had little or no previous experience of organizing and conducting focus groups. The moderators were interviewed in groups of one to three persons according to their project assignment (cf. Table 1).
Table 1.
Overview of Interviews and Interviewees.
| Interview | Project Clustera | Interviewees |
|---|---|---|
| 1 | 1 | Moderators 1, 2, and 3 |
| 2 | 1 | Moderators 4, 5, and 6 |
| 3 | 2 | Moderators 7 and 8 |
| 4 | 3 | Moderator 9 |
A description of the cluster research questions is given in the text.
The interviews lasted approximately 1 hour, and the interview questions were guided by the chronological order in which a focus group is organized and conducted (recruitment, preparation, moderation, methods) and by the utilization and usefulness of the results. We tape recorded the interviews, transcribed them verbatim, and performed qualitative content analysis on the transcripts (Elo & Kyngäs, 2008; Mayring, 2015) with the help of the program MAXQDA 10.0.
The final system of categories2 (Tausch & Menold, 2015) consisted of two types of codes: All relevant text passages were coded with respect to the content of the statement. In addition, a second type of code was required if the statement related to a specific group of participants (e.g., patients, hospital doctors, men, women).
Results
On the basis of the research questions, the contents of interview statements were classified into the three superordinate thematic categories: recruitment, communication in the focus groups, and appraisal of the focus group method. Consequently, the reporting of the results is structured according to three main topics.
Recruitment
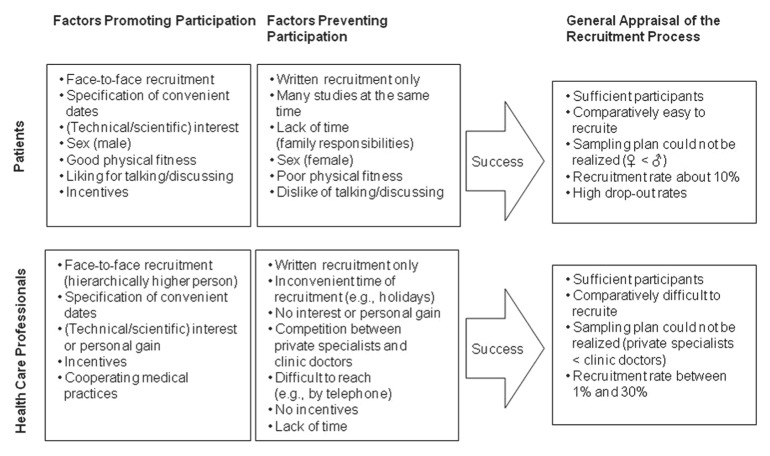
Statements relating to the recruitment of the participants were sorted into the main categories “factors promoting participation”, “factors preventing participation”, and “general appraisal of the recruitment process”. Figure 1 shows the subcategories that were identified under these main categories. Because many of the statements referred only to patients or only to health care professionals (physicians, other health care professionals), the subcodes shown in Figure 1 are sorted by these two types of participants.
Figure 1.
Factors relating to the recruitment process.
Factors relevant for all target groups
As the following interviewee statement shows, addressing potential participants face-to-face (rather than in writing) proved crucial for the success of recruitment in all target groups:
Well, a really good tip when recruiting patients is . . . to address the people yourself. Not to get someone else to do it who . . . has nothing to do with [the project], because ultimately you really do have to explain a lot of things, also directly to the patient. And then it’s always good if the person [who does the recruiting] is actually involved in the project.3
In the case of the clinicians, being addressed by a superior was even more effective for their willingness to participate: “And then top down. If the nursing director asks me, then it’s not so easy to say no.”
Furthermore, a positive response was more often achieved if the groups were scheduled at convenient times for the addressees, and they only had to choose between several alternatives. Patients welcomed times contiguous with their therapies: “And many [of the patients] said: ‘Yes, maybe we can do it after my chemotherapy, on that day when I’m in the clinic anyway?’” Whereas medical assistants were given the opportunity to take part in the groups during working hours, general practitioners preferred evening appointments on less busy weekdays (e.g., Wednesdays and Fridays):
Well, what I found quite good was to suggest a day and a time. And we concentrated on the fact that practices are often closed on Wednesday afternoons. So that’s a relatively convenient day. And then evenings for the pharmacists from seven-thirty onwards.
Interest in the topic of the discussion, or at least in research in general, was an important variable for participation. Together with lack of time, it turned out to be the main reason why sampling plans could not be realized. Among patients, men were much more interested in discussing a technical innovation such as an electronic personal health record, while women—besides their lesser interest—often declined because of family responsibilities: “Well, I’d say a higher proportion of women said: ‘I have a lot to do at home, housework and with the children, therefore I can’t do it.’”
Family physicians, physicians from cooperating medical practices, and hospital doctors showed more interest in discussing an electronic personal health record than did medical specialists in private practice, who often saw no personal gain in such an innovation. For example, one interviewee stated,
Family physicians generally have a greater willingness [to engage with] this [health] record topic. They see . . . also a personal benefit for themselves. . . . or they simply think it might be of relevance to them or they are interested in the topic for other reasons. Some of them even approached us themselves and said, “Oh, that interests me and I’d like to take part.”
In addition, because of heavy workload, private practitioners were difficult to reach (e.g., by telephone). This also lowered the participation of this target group on the focus groups.
Factors relevant only for patients
Two other variables that influenced patients’ willingness to participate were mentioned in the interviews. First, because this target group consisted of cancer patients and diabetes patients with multimorbidity, poor physical fitness also prevented several addressees from participating in the groups. The inability to climb stairs, or the general inability to leave the house, made it impossible for them to reach the location where the groups took place: “[They] immediately replied: ‘Well, no, . . . that’s really too much for me,’ and unfortunately they could not, therefore, be included in the groups.” Furthermore, unstable physical fitness often led to high drop-out rates. The moderators of the focus groups therefore proposed that up to twice as many participants as required should be recruited: “And depending on the severity of the illness, you have to expect a drop-out rate of up to fifty percent. So, if you want to have four people, you should invite eight.”
Second, moderators reported that patients’ liking for, or dislike of, talking and discussing influenced their tendency to join the groups. Participating patients were generally described as talkative. For example: “And with patients, all in all, I had the feeling that those who agreed [to participate] were all people who liked talking, because those who did not like talking refused out of hand.” Patients who refused to participate often argued that they felt uncomfortable speaking in front of a group: “And the men, when they declined they often said: ‘No, group discussion is not for me! I don’t like talking in front of a group.’”
Success
The researchers eventually succeeded in recruiting sufficient participants. However, they were not able to realize the sampling plans according to a certain proportion of male and female patients or types of physicians. “Well, we finally managed to fill up our groups, but only as many [participants] as necessary.” Comparing the different target groups, recruiting patients was described as easier than recruiting physicians: “And that was much easier insofar as you just had to go to the clinic and each day there were five or six patients whom you could address.” However, only 10% of the patients who were addressed agreed to participate. In the health care professional group, the recruitment rates ranged between 0% and 30%, depending on the subgroup. This can be demonstrated by the following interviewee utterance:
And in the private practitioner sector it was rather . . . . Well, we tried to recruit specialists in private practice, in other words internists, gastroenterologists, and oncologists. The success [rate proved to be] extremely poor. . . . Well, on the whole, the willingness to take part, the interest, is not there. Or, well they don’t give the reasons, but they say they don’t want to take part. So that was difficult and, yes, it didn’t go too well.
Communication in the Focus Groups
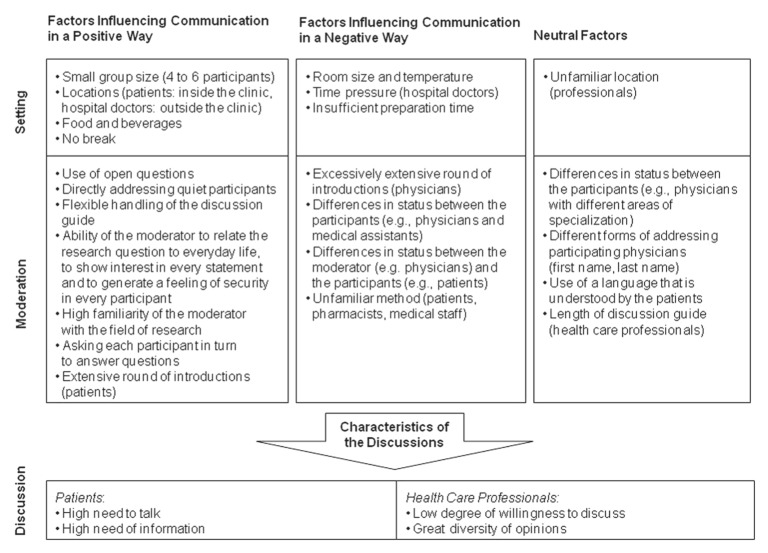
With regard to the communication in the focus groups, the moderators identified factors that influenced communication in a positive or negative way. In addition, we discussed a number of factors with them that are often described in the social science literature as problematic when conducting focus groups. However, the interviewees considered that some of these factors had not influenced communication in the focus groups conducted within the framework of the INFOPAT program. In our system of categories, we also coded whether the factors in question were related to (a) the setting or (b) the moderation of the focus groups (cf. Figure 2).
Figure 2.
Influences on and characteristics of the focus group discussion.
Factors relating to the setting
As Figure 2 shows, communication was reported to be positively influenced by small group size, location, provision of food and beverages, and conducting the focus group without a break. In contrast to general recommendations on focus groups in the context of sociological research, the moderators in the INFOPAT program considered a smaller group size of between four and six participants to be ideal. With regard to location, the interviewees reported that, depending on the target group, different places were perceived as positive. Patients preferred locations inside the clinic because they were easy to reach and caused no additional effort. Furthermore, because these locations were familiar to them, they facilitated an atmosphere of security and ease, which was seen as an important prerequisite for an open and honest discussion. This is clear from the following quotation:
Well, the patient focus groups were all located at the clinic. We chose this location on purpose to make it easier for them, because they come to the clinic anyway for their therapy. And they know the place and they feel comfortable and in good hands.
By contrast, the clinician groups benefited from being located outside the clinic. In contrast to other common addressees of focus groups, these professionals were not only accustomed to participating in groups outside their familiar surroundings but also this location helped them to distance themselves from their professional duties and to engage more deeply in the discussion, as shown by the following quotation:
Yes, one was located at the O-Center. We chose this location on purpose so that the clinicians had to leave the hospital. It’s not too far, only a few yards away. But we wanted them to leave the clinic, and not to run back to the ward when they were called. And, well, I liked this location.
Food and beverages were welcome in all the groups and also helped to create a positive and trusting atmosphere. And finally, the interviewees found that it was better to omit the break, thereby avoiding the interruption of the ongoing discussion. This is reasonable considering the comparatively short duration of the focus group session (between 1.5 and 2 hours). Statements relating to a break might have been different in the case of longer focus group durations.
The interviewees reported that the size and temperature of the room and time pressure on the participants or the moderator had a negative impact on communication. Some of the focus groups in the project took place in midsummer and had to be held in rooms without blinds or air conditioning. The moderators of these groups had to work hard to maintain the participants’ (and their own) attention and concentration. Time pressure on the participants (e.g., the clinicians) led to an unwillingness to engage in active discussion and created a question-and-answer situation, as shown by the following statement:
And in one group of physicians . . . we never reached the point where they joined in fully. During the whole discussion they never completely arrived. And they had already cut the time short in advance. They were under so much time pressure that they were not able to discuss in an open manner.
Moderators reported that they, too, had experienced time pressure—namely, in situations where they did not have enough time to prepare the room and the recording devices. This had caused them to be nervous and stressed at the beginning of the discussion, which had negatively affected the mood of the participants, thereby rendering an honest and open discussion particularly difficult.
Factors relating to the moderation
Many of the positive factors reported by the interviewees have already been described for focus groups in general—for example, using open questions, directly addressing quiet participants, and handling the discussion guide in a flexible way. Furthermore, by showing interest in every statement, and by generating a feeling of security in every participant, moderators fostered a fruitful discussion:
I believe that another important point is that you are calm yourself. That you give the people the feeling “you can feel safe with me, you don’t have to worry that I will make fun of you . . . or that I won’t take you seriously.”
Interviewees also considered that building a bridge between the technical innovation under discussion (a web-based electronic personal health record) and everyday life (e.g., online banking) was an important factor in getting all participants to contribute to the discussion. As one interviewee noted,
We tried to anchor it in their everyday lives. And . . . the example that always worked was when we said: “Think of it as if it were a kind of online banking.” Everyone understands what online banking is. It’s about important data on the internet; they’re safe there somehow. I have my password. And people understood that. Well, it’s important to anchor it in their reality . . . because otherwise the topic is simply far too abstract.
In this context, the fact that the groups were moderated by the researchers themselves proved very helpful because they were able to answer all questions relating to the research topic. As the following quote shows, this was an important prerequisite for opinion formation on the part of participants:
Well, I think that a really important quality criterion . . . is that you have completely penetrated [the topic]. If you only know the process from the outside . . . and you then conduct the focus group about it. . . . Somewhere, at some stage, [one discussion] narrowly missed the point. . . . You simply have to be totally immersed in the topic, well, I believe that [someone who is totally immersed in the topic] is the ideal person for the job. And in our case the thinking was, okay, so I’m a doctor, but on balance it’s more important that both [moderators] are absolutely well informed because it’s a complex topic.
The more specific the research question was, the more useful the moderating strategy of inviting one participant after the other to express their opinion appeared to be. By using this strategy, the moderators ensured that every participant contributed to the discussion.
A point that was strongly emphasized by the interviewees was the duration of the round of introductions at the beginning of the focus group session. In the patient groups, introductions took much more time than the researchers had expected. Patients had a high need to express themselves and to tell the others about their illness and their experiences with the health system. Although this left less time to work through the topics in the discussion guide, the researchers came to realize that there were several good reasons not to limit these contributions: First, the introductions round proved important for helping the participants to “arrive” at the focus group, for creating a basis of trust, and for building up a sense of community among the participants. Second, the interviewees reported that, because many topics in the discussion guide (e.g., participants’ experiences with coordinating visits to different medical specialists) had already been brought up in the round of introductions, they did not have to be discussed further at a later stage:
And that is the crux of this general exchange of experiences at the beginning. Sure, it costs you a lot of time, but I almost think that if you don’t give them that time, you won’t get what you want from them, in the sense that you say: “I want to hear your frank opinion or attitude.” You don’t want them to simply answer you because they think that’s what you want to hear. You have to create an atmosphere in which they really forget where they are. I’m relatively convinced that you wouldn’t achieve that without such [a round of introductions].
The moderators’ experience in the physician groups was different. These groups benefited from having a rather short round of introductions. Giving participants too much time to introduce themselves meant that they presented their expertise rather than reporting their experiences. In contrast to the patient groups, this did not substantially contribute to the discussion of the research topics.
Depending on the context, status differences between the moderators and the participants, or among the participants, were appraised differently by interviewees. In one group comprising physicians and medical assistants, the moderators observed that status differences had a negative influence on communication. Very young female medical assistants, in particular, did not feel free to express their opinions in the presence of their superiors. By contrast, presumed differences in status between family doctors, hospital doctors, and medical specialists in private practice did not have any negative impact on communication. Nor did different forms of address (some participants in these groups were addressed by their first name and some by their last name, depending on the relationship between the moderator and the participants). Status differences between moderators (if medical doctors) and participants (patients) had an impact on communication when patients regarded doctors as an important source of information (e.g., about the meaning of their blood values) or as representatives of the health care system to whom complaints about the system should be addressed. The latter case was the subject of the following interview statement by a moderator who is a physician by profession:
And a lot [was said about] the kind of experiences they had had here at the NCT. And of course, when the patients have been treated here for many years—or even for not so many [years], but they have had many experiences—they sometimes reported at length. And I had the feeling that this had a bit of a feedback function, quite generally, for the NCT. Also the somehow frustrating experiences they had had, or a lot of things that had not gone that well in conversational exchanges [with the staff]. There was a relatively large amount of feedback that didn’t have a lot to do with the topic because I was, of course, involved as a senior physician and I am not an external researcher, but rather someone who is also seen as being jointly responsible, or at least as someone who can channel criticism.
Finally, because most of the moderators were not medical professionals, they did not experience the translation of medical or technical terms into everyday language as problematic. Rather, they automatically used terms that were also familiar to the participants.
Characteristics of the discussion
The factors described above resulted in focus group discussions that might be interpreted as characteristic of health research. The patient focus groups were characterized by a strong need to talk and a high need for information. In the health care professional focus groups, researchers experienced a greater variety of communication styles. Because of a lack of time, or because they falsely expected a question-and-answer situation, some groups demonstrated a low degree of willingness to engage in discussion:
Although, I believe that was partly due . . . well there was one [woman] who was very demanding; she wanted to know straight away: “Yes, what’s the issue here? What do I have to say to you?” Well, the three who came from the one practice, I think they really had the feeling that we would ask them questions and they would bravely answer them and then they could go home again. So, for them this principle that they were supposed to engage in a discussion, for them that was somehow a bit, I don’t know . . . disconcerting. . . . They really thought: “Okay, well we want to know now what this is all about. And they’ll ask us the questions and then we’ll say yes, no, don’t know, maybe. And then we’ll go home again.” Well, at least that was my impression.
Other groups, especially those consisting of different types of health care professionals (e.g., physicians with different areas of specialization, or physicians and pharmacists), were characterized by lively discussion and a great variety of opinions.
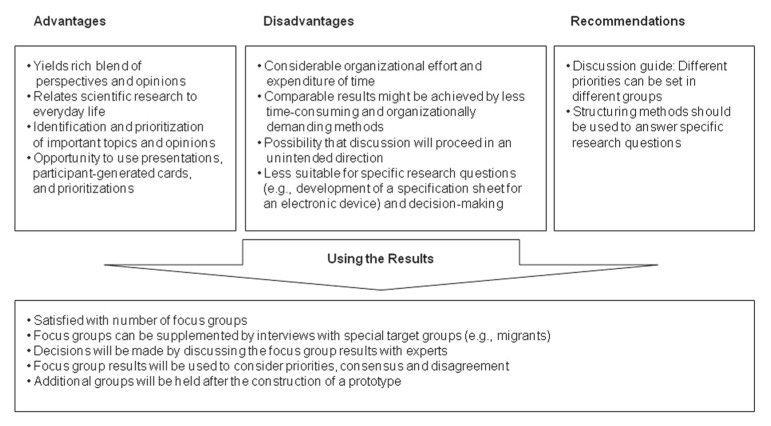
Appraisal of the Focus Group Method
We classified moderators’ statements relating to the appraisal of the focus group method into four main categories: “advantages of the method”, “disadvantages of the method”, “recommendations for other researchers in related research areas”, and “statements on how they used the results” (cf. Figure 3).
Figure 3.
Appraisal of the focus group method.
Advantages
The researchers reported that the focus group method yielded a rich blend of perspectives and opinions, brought forth, in particular, by the interaction between the participants:
But for this question and the topic, and for our lack of knowledge, that was . . . a lot of new information . . . and very many good ideas and critical remarks that you naturally read in the literature from time to time. But, let’s say, because of the complexity of the participants’ reactions and the weight they attached to things, it’s different than reading in a literature review that [this or that] could be taken into account.
The results of the focus groups further enriched the researchers’ work by relating it to everyday life: “Well, what was nice was that the topic was related to the participants’ lives. That people said: ‘Now the topic is important for me.’” Furthermore, the method yielded information about which aspects were most important and how the variety of opinions should be prioritized. This was achieved, in particular, by using participant-generated cards:
And with regard to prioritization, we incorporated it using participant-generated cards. We said: “Look: If you could develop this record now, what would be the three most important things that must absolutely be taken into consideration, from your point of view, no matter what they relate to.” And they wrote them down on the cards. And after that they were asked to carry out their own prioritization—that is, what was most important to them personally. One person wrote “data protection” first, while another [wrote] “sharing with my wife.” . . . That was good. . . . That helped a lot because it was simply clear once again what things were important to them.
In cases where concrete questions had to be answered or decisions had to be made, the interviewees also welcomed the opportunity to use structuring methods such as presentations, flip-charts, and participant-generated cards to obtain the relevant information:
. . . Well, the aim was that at the end we [would] have a set of requirements for the engineering [people]. And the engineering [people] don’t so much want to know about experiences and desires and barriers, but rather they want to know should the button be green or red and can you click on it. And that’s why I thought at the beginning it will be difficult with a focus group and an open discussion. Now, if you say that one can also interpret a focus group the way we did, partly with very specific questions and these participant-generated cards, then I think it is indeed possible to answer such questions as well.
Disadvantages
The main disadvantages of the focus group method were seen in the considerable organizational effort and expenditure of time involved. A question raised by some of the interviewees was whether comparable results could have been achieved using less time-consuming and organizationally demanding methods.
It’s true to say that you lose time. Well, you could implement [the innovation] straight away and see whether it’s better. Maybe, in this case you’re wrong and you just think it’s better or in any case not worse than before. You basically lose a year on this whole focus groups thing.
Moreover, in some cases, the discussion went in an unwanted direction and the moderators never fully succeeded in bringing the group back to the intended topics.
Furthermore, like many other medical research projects, INFOPAT included quite specific research questions. In this connection, the moderators emphasized that open focus group discussions would not have succeeded in answering those questions. Only by using methods such as participant-generated cards and prioritization was it possible to answer at least some of them. Nonetheless, some interviewees did not consider the focus group method to be really suitable for this type of research questions:
Of course we also have our engineers as counterparts who . . . need very specific requirements at some point. The question is whether such a focus group . . . . [It] can’t answer that in detail in this first stage. It’s simply not practicable.
Recommendations
As described under the “Communication in the Focus Groups” section above, the round of introductions in the patient groups lasted much longer than planned, thereby shortening the time available for other topics in the discussion guide. As a result, the moderators decided to choose a different thematic focus in each group so that every topic was discussed more deeply in at least one group.
What we usually did was to consider what hadn’t been addressed that much in the previous focus group. That [topic] was given more room in the next focus group because the guide, well it was quite a lot. You could have easily gone on discussing for another hour or two.
Using the results
On the whole, the researchers were satisfied with the number of groups that were conducted and the results that they yielded. They did not agree that more groups would have led to better, or different, results—with one possible exception, namely, in the case of specific target groups (e.g., migrants). Only one group had been composed of patients with a migrant background, and, as one interviewee stated, “I just thought, the patients with a migrant background . . . now that was [only] one group, it by no means covers the whole range.”
In cases where the results of the focus groups were perceived as not being concrete enough to proceed to the next research step (e.g., formulating a specification sheet for the construction of the electronic personal health record), the researchers planned to bring experts together in a roundtable format to make decisions on the basis of the priorities, agreements, and disagreements that had emerged from the focus groups. Following the construction of a prototype, they intended to conduct further focus groups to validate or adapt the usability of the electronic personal health record system.
Discussion
Our analysis of interviews with focus group moderators yielded considerable insights into methodological aspects of conducting focus groups in health research. Our first research question related to characteristics of the target groups that should be considered during the recruitment process. We identified face-to-face contact as an important factor promoting focus group participation. The interviewees considered this type of contact to be better suited to answering target persons’ questions and explaining the method and aims of the focus groups. Moreover, they felt that addressees might find it more difficult to decline a face-to-face invitation than a written one. With regard to health care professionals, an invitation issued by a hierarchically higher person was most effective, even though ethical aspects should be considered in this case, and voluntary participation should nevertheless be ensured. Otherwise, the order to participate might prevent an atmosphere of open communication and might lead to a lower quantity or to more negative statements.
Furthermore, whereas physicians are usually accustomed to discussing topics with others, an important characteristic that influenced willingness to participate on the part of members of other target groups (other health care professionals, patients) was a liking for, or a dislike of, talking. Researchers might take account of this fact by explaining the method in more detail, by developing arguments to overcome fears, or, as suggested, for example, by Colucci (2007), by convincing the addressees with other activities implemented in the focus groups. Other relevant personal characteristics—be they related to the research topic (e.g., technical interest in the case of an electronic innovation) or to the specific target group (e.g., physical fitness on the part of patients or lack of time on the part of health care professionals)—should be anticipated when planning recruitment. These characteristics might be taken into account by preparing arguments, providing incentives, giving thought to favorable dates and times, and choosing easily accessible locations. An interesting finding was that, depending on the target group, different locations were considered to have a positive influence on the discussion. Whereas locations inside the clinic were preferred in the case of the patient focus groups because of familiarity and easy accessibility, hospital doctors were more engaged in the discussion when the focus group site was located at least some yards away from their workplace.
Finally, the experience of our researchers that up to 50% of the patients had to cancel at short notice because of health problems does not appear to be uncommon in this research context. That overrecruitment is an effective strategy—particularly in health care research—has been reported by other authors (e.g., Coenen et al., 2012).
With our second research question, we focused on aspects of communication in the focus groups. The interviews revealed several factors specific to research topics and addressees of health care studies that influenced the discussions. Consequently, in addition to considering general recommendations regarding the organization and moderation of focus groups (e.g., choosing adequate rooms with a pleasant atmosphere, serving food and beverages, using open questions, showing interest in all contributions, and directly addressing quiet participants), these health care specific aspects should be taken into account. Relevant factors that should be addressed when moderating focus groups in this context are (a) the strong need to talk and the high need for information in the patient groups, (b) status differences between the participants or between the moderators and the participants, (c) the size of the focus group, and (d) the specificity of the topic of discussion. The interview data revealed that these factors influenced the discussions and thus the results achieved with the groups. In addition, the following four possibilities of addressing these factors were identified:
First, the moderators had to devote more time to the round of introductions in the patient groups, which served as a warm-up, created an atmosphere of fellowship and openness, and accommodated this target group’s strong need to talk. Second, with respect to status differences between the moderator and the participants, no definite recommendations can be derived from the interviews. The interviewees found that it was less favorable when the moderator was perceived not only in that role but also in other roles (e.g., physician), because this might hamper a goal-oriented discussion. However, they considered deep insight into the research topic on the part of the moderators to be beneficial, at least for certain research topics. Thus, one should carefully weigh up whether it is more advantageous or more disadvantageous when the group moderator is a physician. Interviewees considered status differences between participants to be disadvantageous only in one case, where—because of organizational constraints—medical assistants and their superiors joined the same focus group, which gave rise to some reticence on the part of the young assistants. Similar problems have been reported by other authors, for example, Côté-Arsenault and Morrison-Beedy (2005; see also Hollander, 2004). However, interviewees did not experience as problematic status differences between physicians with different areas of specialization.
Third, with respect to group size, interviewees found comparatively small focus groups appropriate to give all participants enough time to tell their stories. In contrast to social science research, where groups of between eight and 20 participants are recommended, our interviewees considered groups of between four and six persons to be optimal. This is in line with Côté-Arsenault and Morrison-Beedy (2005), who recommended small groups for health research, especially when sensitive topics are discussed. Our interview data revealed that this recommendation might also be useful for other health research topics.
Fourth, with regard to the topic of the discussion, interviewees found it helpful to structure different phases of the discussion in different ways, depending on the specificity of the research questions. In contrast to social science research, certain types of research questions in health research require comparatively specific answers. Some of the focus groups in our study were aimed at collecting participants’ expectations regarding an electronic personal health record or—even more specifically—at developing a product specifications document. Conducting focus groups during the development of a technical innovation is a method that is being increasingly used in health care research. Hence, the experiences of the interviewees with regard to these aspects of their research might be relevant for many other research programs. For this type of research questions, it proved useful to include more structured parts in the discussion, for example, having certain questions answered by each participant in turn, or using methods such as participant-generated cards and prioritization. This made it easier to obtain the opinion of each participant and to cover as many concerns and expectations as possible. This finding is in line with recommendations by Colucci (2007), who proposed the use of activity-oriented questions for health research topics as an enrichment of data collection and a means of making it easier to talk about sensitive and complex topics.
All the moderators found that their discussion guides contained too many questions and too many topics. This might have been due, at least partly, to a desire to determine all relevant aspects in advance—a tendency that might be typical of health research. However, Morgan (1995) also addressed this phenomenon in relation to social research in general: “A common error in focus group question guidelines is too much emphasis on what is of interest to the researcher and not enough emphasis on what is of interest to the participants” (p. 520).
With our third research question, we addressed the appraisal of the focus group method in the interviewees’ research context. Our results show that one should think carefully before using focus groups in the field of health research. The impression that they are quick and easy to conduct might be a misconception, especially in this research context. In fact, the appraisal of the method by the moderators revealed both advantages and disadvantages. The main advantages were the rich blend of perspectives and opinions obtained and the opportunity to have them prioritized by the target groups. For their research topics, the interviewees saw a further important advantage in the fact that they were able to relate their scientific research to everyday life, a point that might be of general importance for a number of research questions in health research, especially those that refer to new medical diagnostics or technical innovations.
The interviewees considered that the main disadvantages of focus groups were the substantial organizational effort and expenditure of time they required. They raised the question whether comparable results could have been achieved using less costly methods. Fortunately, we conducted our interviews with researchers from a research program aimed at answering research questions of different degrees of specificity. As a result, the moderators were able to compare the usefulness of focus groups for different types of research questions. Their statements revealed that they were satisfied with the results relating to more open research questions such as experiences with cross-sectoral health care. For more specific research questions, the interviewees valued the possibility of organizing the discussions in a more structured way and using methods that activated all participants (e.g., participant-generated cards, prioritizations). Nonetheless, they considered meetings of experts to be a necessary intermediate step, for example, on the way to a product specifications document. We recommend that, depending on the specificity of the results that are projected, consideration should be given to including such intermediate steps in the planning stage.
Limitations of the Study
Our analysis of the interviews with the focus group moderators revealed a number of methodological problems that typically occur when focus groups are used in a health research context and yielded recommendations on using such groups in this context. However, some limitations of the present study should also be discussed: First, we conducted our research with focus group moderators, all of whom worked in the same research program. Even though the INFOPAT program consists of several subprojects, they all deal to a greater or lesser extent with the advantages and disadvantages of an electronic support system (electronic personal health record). Furthermore, the moderators were mainly health scientists and had little or no experience with conducting focus groups. This might also have been specific for the research program in which our study was conducted. In other health care programs, focus groups might be moderated mainly by physicists or lay persons (e.g., in participatory health research). Consequently, had we also conducted interviews with focus group moderators from other research areas or included moderators with other professions or more focus group experience, this might have led to different results. However, our research project is rather typical for applied qualitative research in medical science when developing new technologies. Here, focus groups are used by the researchers to find out the potential requirements for the new technology. The researchers are often experts in a specific scientific topic and have no or only limited experience in conducting qualitative research in terms of focus groups. Therefore, our findings are of a particular importance for the researchers with little experiences in conducting focus groups, which can apply to every research, conducted first time. In addition, the little experience of our focus group moderators was a special advantage and strength of the study. More experienced moderators would have prevented some of the problems our moderators—as other unexperienced moderators—faced. As a result, the moderators would not have named these potential problems in the interviews and given no advice for preventing them.
Second, the study was conducted in Germany and thus represents problems and challenges of the German health care system. In other countries, physicians might have different work-shifts or there might be different possibilities in the health care system to reach the target groups. Therefore, more research on the methodology of focus groups in the context of the development of new technologies in health care in other countries and cultures with a consideration of additional relevant groups is needed.
Third, in our interviews, we focused mainly on the organization and conducting of focus groups. For two reasons, we did not address the aspect of data analysis: First, we conducted the interviews shortly after the focus groups had been completed, at a time when data analysis was still in progress. Second, analysis of qualitative data can be carried out in many different ways, depending on research questions and preferences of researchers, and some of the recommended methods are very complex. Had we discussed them in detail, it would have been too time-consuming in the interviews.
Concluding Remarks
Our results revealed a number of methodological challenges that might be typical of conducting focus groups in health research. We hope that our findings will be of use to researchers in similar research fields. Furthermore, we encourage other researchers who are interested in health research topics to gather more information about methodological aspects specific to this research field. Our results were achieved in the context of the development of a technical innovation. It might be interesting to endeavor to replicate them in other health care research projects dealing with technical innovations. Moreover, we would encourage researchers of other topics in health research to interview focus group moderators about their experiences in their specific research context. We hope that our results will serve as a useful basis for comparing results in different areas of health research.
Acknowledgments
We thank the focus group moderators in the INFOPAT program for their great willingness to share their experiences and for their openness during the interviews.
Author Biographies
Anja P. Tausch, PhD, is senior researcher at GESIS–Leibniz Institute for the Social Sciences, Mannheim, Germany.
Natalja Menold, PhD, is senior researcher and head of the Survey Instruments Unit at GESIS–Leibniz Institute for the Social Sciences, Mannheim, Germany.
http://www.soziologie.de/en/gsa/ethik-kommission/code-of-ethics.html, retrieved on 05/10/2015.
The language of the research project, focus groups, and interviews was German. The scheme was developed in German on the basis of the German text material from the transcribed interviews. The scheme and the citations were translated for the purpose of international publication by an experienced, qualified, and fully bilingual translator, whose mother tongue is English and who also has an MA in sociology from a German university. A German version of the full categorial system can be found in Tausch and Menold (2015).
All citations included in this publication were translated from German.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the German Federal Ministry of Education and Research (BMBF; FKZ 01KQ1003D).
References
- Baudendistel I., Winkler E., Kamradt M., Brophy S., Längst G., Eckrich F., . . .Ose D. (2015). The patients’ active role in managing a personal electronic health record: A qualitative analysis. Supportive Care in Cancer, 23, 2613-2621. doi: 10.1007/s00520-015-2620-1 [DOI] [PubMed] [Google Scholar]
- Carey M. A. (1994). The group effect in focus groups: Planning, implementing, and interpreting focus group research. In Morse J. M. (Ed.), Critical issues in qualitative research methods (pp. 225–241). Thousand Oaks, CA: Sage. [Google Scholar]
- Carr A., Hewlett S., Hughes R., Mitchell H., Ryan S., Carr M., Kirwan J. (2003). Rheumatology outcomes: The patient’s perspective. The Journal of Rheumatology, 30, 880–883. [PubMed] [Google Scholar]
- Coenen M., Stamm T., Stucki G., Cieza A. (2012). Individual interviews and focus groups in patients with rheumatoid arthritis: A comparison of two qualitative methods. Quality of Life Research, 21, 359–370. [DOI] [PubMed] [Google Scholar]
- Colucci E. (2007). “Focus groups can be fun”: The use of activity-oriented questions in focus group discussions. Qualitative Health Research, 17, 1422–1433. [DOI] [PubMed] [Google Scholar]
- Côté-Arsenault D., Morrison-Beedy D. (2005). Maintaining your focus in focus groups: Avoiding common mistakes. Research in Nursing & Health, 28, 172–179. [DOI] [PubMed] [Google Scholar]
- Creswell J. W., Plano Clark V. L. (2007). Designing and conducting mixed methods research. Thousand Oaks, CA: Sage. [Google Scholar]
- Daley C. M., James A. S., Ulrey E., Joseph S., Talawyma A., Choi W. S., . . .Coe M. K. (2010). Using focus groups in community-based participatory research: Challenges and resolutions. Qualitative Health Research, 20, 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo S., Kyngäs H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115. [DOI] [PubMed] [Google Scholar]
- Feldthusen C., Björk M., Forsblad-d’Elia H., Mannerkorpi K. (2013). Perception, consequences, communication, and strategies for handling fatigue in persons with rheumatoid arthritis of working age—A focus group study. Clinical Rheumatology, 32, 557–566. [DOI] [PubMed] [Google Scholar]
- Frazier L. M., Miller V. A., Horbelt D. V., Delmore J. E., Miller B. E., Paschal A. M. (2010). Comparison of focus groups on cancer and employment conducted face to face or by telephone. Qualitative Health Research, 20, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber D. E., Hamann H. A., Rasco D. W., Woodruff S., Lee S. J. C. (2012). Patient comprehension and attitudes toward maintenance chemotherapy for lung cancer. Patient Education and Counseling, 89, 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander J. A. (2004). The social contexts of focus groups. Journal of Contemporary Ethnography, 33, 602–637. [Google Scholar]
- Kamradt M., Baudendistel I., Längst G., Kiel M., Eckrich F., Winkler E., Ose D. (2015). Collaboration and communication in colorectal cancer care: A qualitative study of the challenges experienced by patients and health care professionals. Family Practice, 32, 686-696. doi: 10.1093/fampra/cmv069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingry M. J., Tiedje L. B., Friedman L. L. (1990). Focus groups: A research technique for nursing. Nursing Research, 39, 124–125. [PubMed] [Google Scholar]
- Kitzinger J. (1995). Qualitative research: Introducing focus groups. British Medical Journal, 311, 299–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzinger J. (2006). Chapter 3: Focus groups. In Pope C., Mays N. (Eds.), Qualitative research in health care (3rd ed., pp. 21–31). Malden, MA: Blackwell. [Google Scholar]
- Kroll T., Neri M. T., Miller K. (2005). Using mixed methods in disability and rehabilitation research. Rehabilitation Nursing, 30, 106–113. [DOI] [PubMed] [Google Scholar]
- Krueger R. A. (1988). Focus groups: A practical guide for applied research. Newbury Park, CA: Sage. [Google Scholar]
- Lehoux P., Poland B. D., Daudelin G. (2006). Focus group research and “the patient’s view.” Social Science & Medicine, 63, 2091–2104. [DOI] [PubMed] [Google Scholar]
- Mayring P. (2015). Qualitative Inhaltsanalyse [Qualitative content analysis] (12th ed.). Weinheim, Germany: Beltz. [Google Scholar]
- Morgan D. L. (Ed.). (1993). Successful focus groups: Advancing the state of the art. Newbury Park, CA: Sage. [Google Scholar]
- Morgan D. L. (1995). Why things (sometimes) go wrong in focus groups. Qualitative Health Research, 5, 516–523. [Google Scholar]
- Morgan D. L. (1996). Focus groups. Annual review of sociology, 22, 129–152. [Google Scholar]
- Morgan D. L. (2009). Focus groups as qualitative research (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Morgan D. L., Krueger R. A. (Eds.). (1998). Focus group kit. Thousand Oaks, CA: Sage. [Google Scholar]
- Nafees B., Lloyd A., Kennedy-Martin T., Hynd S. (2006). How diabetes and insulin therapy affects the lives of people with type 1 diabetes. European Diabetes Nursing, 3, 92–97. [Google Scholar]
- Nicholas D. B., Lach L., King G., Scott M., Boydell K., Sawatzky B. J., . . .Young N. L. (2010). Contrasting internet and face-to-face focus groups for children with chronic health conditions: Outcomes and participant experiences. International Journal of Qualitative Methods, 9, 105–121. [Google Scholar]
- Rasmusson K., Lappe D., Roberts C., Croasdell S., Meegan S., Budge D. (2014). Heart failure patient perspectives: Learning from focus groups to improve care. Heart & Lung, 43, 382–383. [Google Scholar]
- Rhodes S. D., Hergenrather K. C., Wilkin A., Alegría-Ortega J., Montaño J. (2006). Preventing HIV infection among young immigrant Latino men: Results from focus groups using community-based participatory research. Journal of the National Medical Association, 98, 564–573. [PMC free article] [PubMed] [Google Scholar]
- Stewart D. W., Shamdasani P. N., Rook D. W. (2007). Focus groups: Theory and practice (2nd ed.). Thousand Oaks, CA: Sage. [Google Scholar]
- Tausch A., Menold N. (2015). Methodische Aspekte der Durchführung von Fokusgruppen in der Gesundheitsforschung - Welche Anforderungen ergeben sich aufgrund der besonderen Zielgruppen und Fragestellungen? [Methodological aspects of conducting focus groups in health research - which requirements result from the particular target groups and research questions?]. GESIS Papers, 2015(12). Retrieved from http://www.gesis.org/fileadmin/upload/forschung/publikationen/gesis_reihen/gesis_papers/GESIS-Papers_2015-12.pdf [Google Scholar]
- Vincent D., Clark L., Marquez Zimmer L., Sanchez J. (2006). Using focus groups to develop a culturally competent diabetes self-management program for Mexican Americans. The Diabetes Educator, 32, 89–97. [DOI] [PubMed] [Google Scholar]