Abstract
Lung cancer is the leading cause of cancer deaths worldwide. Less-known forces are involved in the etiology of lung cancer and have relevant implications for providers in ameliorating care. The purpose of this article is to discuss theories of causation of lung cancer using historical analyses of the evolution of the disease and incorporating related explanations integrating the relationships of science, nursing, medicine, and society. Literature from 160 years was searched and Thagard’s model of causation networks was used to exhibit how nursing and medicine were significant influences in lung cancer causation theory. Disease causation interfaces with sociological norms of behavior to form habits and rates of health behavior. Historically, nursing was detrimentally manipulated by the tobacco industry, engaging in harmful smoking behaviors, thus negatively affecting patient care. Understanding the underlying history behind lung cancer causation may empower nurses to play an active role in a patient’s health.
Keywords: cancer, nursing, epidemiology, medicine, tobacco and health
Causation of Lung Cancer: Historical Perspectives for Nursing
The most common yet preventable form of cancer in the world originates in the lung; with only a 15% 5-year survival rate for all stages in the United States (Siegel, Naishadham, & Jemal, 2013). Numerous elements have been attributed to the causation of lung cancer; however, none more strongly verified than cigarette smoking. Although the inhalation of tobacco smoke has been proven to be single-handedly responsible for lung cancer in active or former smokers, there are other forces involved in the etiology of the disease (Alberg, Brock, Ford, Samet, & Spivack, 2013). Scientific research aimed at understanding the evolving pathogenesis of disease is of the utmost importance in the treatment of lung cancer; however, associated causation determinants that emerge from physical and social science have relevant implications for nurses and virtually all health care providers in ameliorating care and eradication of the disease itself (Alberg et al., 2013; Glick, 2007).
The Purpose
Via historical analyses of the evolution of the disease, I discuss causation theories of disease and incorporate related explanations which integrate the relationships of science, nursing, medicine, and societal influences. Thagard’s (2000) model of causation networks is used to illustrate how causation theories develop within empirical science and evolve over time through both cognitive and social processes integrating concepts inherent to social science to progress into comprehensive theory. This article will exhibit how the professions of both nursing and medicine were significant influences in lung cancer causation theory.
The Concept of Causation
With historical roots in biology, causation has advanced in the discipline of epidemiology. The conceptual definition of causation has evolved from a solely empirical scientific origin to include related concepts of causative factors that are both multifactorial and pragmatic (Parascandola, 2011). A causal relationship is one that has a synergistic or complementary mechanism that by its operations makes a difference therefore procuring evidence about it (Joffe, 2011). Joffe (2011) described that evidence gathering can occur from either the mechanistic direction or the opposite direction of effect. Parascandola and Weed (2001) described the evolution of the concept of causation within the epidemiological debate; concluding that epidemiology should be defined as both deterministic (scientific cause and effect) and probabilistic (indeterministic and multifactorial; Parascandola, 2011). Epidemiology provides evidence on differences in outcomes between groups that are defined by different exposures based on the assumption that the alteration brought about by the mechanism occurs over time. Understanding the cause of disease has been debated over the years by epidemiologists resulting in confusion; however, most epidemiologists agree that to intervene effectively in disease, it is imperative to know that causal processes are operating discovered or undetected resulting in interactions where functions must be clarified (Glick, 2007; Joffe, 2011; Parascandola, 2011).
Epidemiology in the United States was traditionally founded in the study of infectious diseases with evidence of disease originating from official mortality statistics, pathology reports of autopsies, and observations from physician specialists (White, 1990). Lipton and Odegaard (2005) declared that after World War II, epidemiology needed to think differently about studying causation because of the emergence of chronic diseases. They raised the question “Does causation mean the same in acute infectious disease as it does in chronic disease?” (Lipton & Odegaard, 2005). After 1950, the cause versus risk factor debate emerged related to all diseases not having measurement methods to illustrate a cause and effect relationship (Lipton & Odegaard, 2005). Causation is a complex interaction of numerous factors and not based on a chain of events and is better defined pragmatically as an association that is probabilistic; meaning that incidence of disease decreases when exposure to causal agents decreases (Glick, 2007; Joffe, 2011; Parascandola, 2011).
Method
The literature search for this article was conducted via a review that included using the terms and related (MeSH) terms of lung cancer, causation, epidemiology, tobacco, nursing, and medicine in that order. The computerized search engines utilized were Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, Google Scholar, and the Cochrane Library. Only articles published in English were incorporated in the search. All types of publications were included and reference lists of relevant articles retrieved as full articles were checked for additional studies. No historical articles prior to 1854 were deemed relevant to the purpose of this article. More than 172 publications were reviewed, from 1854 to 2014; and 90 articles were chosen for their relevancy. All articles were reviewed for scientific merit utilizing current principles involved in critiquing quantitative and qualitative research.
In the late 19th and early 20th centuries, most research was reported in the form of surgical case studies that described both patterns in pathological cancer incidence and primarily surgical intervention. As lung cancer incidence increased in mid-20th century, research reports exemplified a descriptive statistical design. The first concept considered in the literature search was that of causation founded within the epidemiological realm; followed by the most common causation element of tobacco. The professions of medicine and nursing became evident within the evolving causation literature as they were key players in the growing incidence of people with lung cancer. Thagard’s model guided the historical investigation; therefore, the literature search was expanded to analyze social, behavioral, political, and heredity factors in addition to previous environmental disease causation influences. Finally, literature demonstrating how the profession of nursing can use lessons learned from the historical past and from their own profession’s involvement was investigated for nurses to be able to improve the lives of those afflicted with lung cancer and most importantly, the health and wellness of those without lung cancer.
History of Lung Cancer Causation Theories
Lung cancer is a chronic disease with multiple causation theories imbedded in the history of the disease that span more than 100 years. Prior to the early 20th century, lung cancer was a rare disease, accounting for 10% to 15% of all cancers and less than 140 cases per year in the United States (Alberg et al., 2013; Cornfield et al., 2009; “Editorials,” 1882; “Editorials and Medical Intelligence,” 1854; Fisher, 1958; Joffe, 2011; Witschi, 2001). Medical journal articles published in the last few decades of the 19th century described the occurrence of lung cancer and briefly postulated that radon exposure, arsenic, and possibly cigarettes were the cause of the disease; however, the articles were based on individual medical opinion documented as case studies only (“Editorials,” 1882; “Editorials and Medical Intelligence,” 1854; “Reports of Societies,” 1895).
1900 to 1950 Environmental Sources
Theories attributed to lung cancer in the first half of the 20th century involved several environmental sources. The influenza pandemic of 1918 was believed to be linked to the increase in lung cancer cases in that decade (Proctor, 2012; Witschi, 2001). Another virus, the Human Papillomavirus, was discovered in patients with head and neck cancer and proposed to cause bronchogenic cancer given the close vicinity of the body organs (Hajdu, 2011; Witschi, 2001). Exposure to chemicals such as arsenic, silicone, asbestos, radon, tar, and other chemicals were identified as possible causes of bronchogenic cancer. Arsenic, a chemical found in soil, copper and iron ores and refineries, as well as medicine, cosmetics, and insecticides was a common element of exposure. Early researchers noted an increase in lung cancer in miners, copper smelters, and farmers were reported to inhale the fumes of soil and pesticide dust (Hajdu, 2011). Medical providers reported arsenical keratosis in patients treated previously with Fowler’s solution to alleviate their symptoms of psoriasis and rheumatic fever (Robson & Jelliffe, 1963). Exposure to silicone dust was also blamed for lung cancer. Granite and stone workers were found to have an increase in laryngeal and lung cancer incidence in the 1930s (Alberg et al., 2013; Hajdu, 2011; White, 1990; Witschi, 2001). Asbestos was used in fibrous materials found in clothing and building materials in the early part of the 20th century and hypothesized to be a cause of lung cancer. It was not until the later part of the century that a strong causal relationship would be evident via medical science investigation in people with a specific type of lung cancer, mesothelioma (Hajdu, 2011). Radon, an invisible, odorless chemical found in soil and rock, first appeared as a possible contributing link to damaged lung epithelium in an autopsy on a miner in 1879; however, a significant increase in patients with radon exposure and various lung diseases did not emerge until the early 1930s (Hajdu, 2011). The advent of the automobile with accompanying roadway infrastructure was to blame for tar and air pollution associations to lung cancer. Polycystic hydrocarbons found in road tar, fire smoke, and automobile exhaust was identified as carcinogens by early epidemiologists (Alberg et al., 2013; Hajdu, 2011; White, 1990; Witschi, 2001).
1950 to The Present
The aforementioned environmental causation theories of lung cancer continued to be investigated within medical science (Miettinen & Rossiter, 1990); however, other environmental influences investigated pertained to bird dander, secondhand smoke, and a familial link. Early researchers noted that there was an increase in lung cancer in bird keepers and surmised that there was a causal link; however, subsequent researchers found no significant link when adjusted for tobacco exposure (J. Britton & Lewis, 1992). Secondhand tobacco smoke exposure was first identified as a causal factor of lung cancer in non-smokers living and working with smokers in the 1980s and was further confirmed to be a definitive risk factor for cancer in the last decade of the 20th century (Pope et al., 1995). Familial links to lung cancer manifestation first appeared in the literature in the 1960s when siblings were found to have an increase in lung cancer mortality; however, an additional confounding factor was surmised to be secondhand tobacco smoke exposure as well (Fraumeni, Wertelecki, Blattner, Jensen, & Leventhal, 1975). Lichenstein and colleagues (2000) studied more than 44,000 twins to assess lung cancer risk but found that there was actually no genetic risk and that causation of lung cancer in twin siblings was due to environmental causes. None of the proposed environmental causes of lung cancer noted in early epidemiological research compare in effect to the most significant culprit found in the environment, tobacco (Parascandola, 2011; Proctor, 2012; White, 1990).
Tobacco as Lung Cancer Causation
Tobacco was actually identified a possible cause of lung cancer in early medical literature of the late 1800s but only by a select few physicians (“Editorials,” 1882; “Editorials and Medical Intelligence,” 1854; “Reports of Societies,” 1895). The first published piece of literature attributing cigarette smoking to the growing incidence of lung cancer was in 1912, when Dr. Isaac Adler opined that as cigarette smoking increased, so did the number of cases of lung cancer (Proctor, 2012). Although there were a few other physicians in the world who also believed that tobacco was to blame for the increase in lung cancer incidence, it would not be until 1950 that medical research would reveal that tobacco was the most significant cause of lung cancer (Cornfield et al., 2009; Parascandola, 2011; Proctor, 2012; White, 1990). Landmark studies by Doll and Hill in 1950 in the United Kingdom and Hammond and Horn in 1954 in the United States forced the discipline of epidemiology to officially recognize cigarette smoking as the primary cause of lung cancer. Doll and Hill’s (1950) case-controlled study involved British physicians who smoked. They found that the death of the physicians was directly related to cigarette consumption. Hammond and Horn (1954) studied 192,174 males with lung cancer and concluded that the cigarette smoking habit leads to lung cancer. In both studies, a several year latency period was identified in how lung cancer manifests (Doll & Hill, 1956; Hammond & Horn, 1954). Subsequent lung cancer research demonstrating the link between cigarette smoking and lung cancer prompted the U.S. Surgeon General and Medical Research Council of the United Kingdom to publically issue official public health reports condemning the cigarette habit as dangerous to health (Use, 2000).
The Tobacco Industry’s Role in Lung Cancer Causation Theory
Late 1800s to 1950
Although tobacco smoking has been around since Native Americans introduced it to Christopher Columbus, it was not marketed to the general public, specifically men and the wealthy, until a few centuries later (Proctor, 2012). The printed word in magazines, journals, and newspapers in the late 1800s, enabled the tobacco industry to advertise the “pleasures” of smoking in almost every publication. The invention of a faster cigarette-making machine in 1876 was responsible for the mass-marketing campaign; facilitating the production of thousands of cigarettes per hour (Proctor, 2012; Witschi, 2001). The menthol cigarette was invented in 1920 to combat mucous irritation of cigarette smoke to deliver a “cooling effect” for more appealing smoking sensation (Anderson, 2011). During the World War I as well as World War II, cigarettes were given to soldiers in their ration packages and tobacco use increased 346% by 1920. Soldiers who were abstainers from tobacco came back from both World Wars addicted to cigarettes (Hammond & Horn, 1954; Ochsner, De Bakey, & Dixon, 1947; Proctor, 2012). Tobacco companies expanded their aggressive cigarette marketing to women as early as 1918, as a symbol of “liberation and equality” as women were fulfilling male-oriented jobs as a result of the wars (Amos & Haglund, 2000; Gardner & Brandt, 2006). Forceful marketing continued throughout the decades in the first half of the 20th century, expanding the focus to every profession; from laborers to medical professionals and even teenage boys to symbolize “manhood.” Cigarette use grew to become an epidemic in the 1940s to 1950s (Gilman & Zhou, 2004; Proctor, 2001). Tobacco companies enlisted the medical and nursing professions to promote the safety of their products in their advertising materials (Gardner & Brandt, 2006; Malone, 2006).
The Tobacco Industry Fights Back
After the breakthrough studies on the hazards of cigarette smoking by Doll and Hill and Hammond and Horn were published in medical literature and announced in the media in the early 1950s, tobacco companies joined forces in solidarity to fight the impact that such reports would have on their customers (Proctor, 2012). Tobacco corporations publically denied the research findings and established The Tobacco Industry Research Commission to fund “unbiased” research to continue to promote the safety of their product via strategic public relations campaigns to cast doubt into any future anti-tobacco research (Glantz, Barnes, Bero, Hanauer, & Slade, 1995; Proctor, 2012). “Safer” cigarettes were developed with lower tar and nicotine and promoted successfully to the public as tobacco use rates among men and women doubled by the 1960s (Vincent, Takita, Lane, Gutierrez, & Pickren, 1976; Youlden, Cramb, & Baade, 2008). After the U.S. Surgeon General Report of 1964 was released condemning tobacco smoking as the leading cause of lung cancer, tobacco companies responded that the report was hypothetical in origin and engaged the use of statisticians to cast doubt on the study methods used in the research (Fisher, 1958; White, 1990). They continued forceful political lobbying and robust media marketing that included teenagers as additional targeted customers (Glantz et al., 1995; Kuper, Adami, & Boffetta, 2002). The propaganda movie titled “Smoking and Health: The Need to Know” was produced by the tobacco industry and distributed to colleges and high schools nationwide to deflect the negativity that surrounded tobacco use (Proctor, 2012).
Smoking rates in men started to decline in the 1980s; however rates of tobacco use in women rose, attributable to the correlation between the women’s liberation movement and the “You’ve come a long way, Baby” marketing campaigns by Phillip Morris of the previous decades (Amos & Haglund, 2000; Malone, 2002). In 1990, tobacco promotion continued to target lower socioeconomic and less educated people as the educated professional smoking rate declined (Alberg et al., 2013; Amos & Haglund, 2000; Ezzati & Lopez, 2003). Cigarette companies designed packaging and utilized fashion models; targeting the vulnerability of teenage girls (Kaufman, 1994).
Tobacco Companies Exposed
In May 1994, The Brown and Williamson Tobacco Corporation internal documents were anonymously delivered to tobacco public health researcher, Dr. Stanton Glantz. These documents proved that tobacco companies had been hiding the physical endangerments of tobacco use and addiction since 1965 (Glantz et al., 1995). Attorney Generals of 46 states filed a federal lawsuit against all tobacco corporations which was settled by The Master Settlement Agreement in 1998. Restitution payments of US$206 billion dollars were paid to the complainants and the establishment of The American Legacy Foundation was mandated to conduct educational programs based on research findings (Glantz et al., 1995). After the settlement, tobacco companies continued to market to younger people in their teen years, when addiction occurs; capitalizing on their vulnerability to media persuasion. The evolution and implementation of tobacco restriction legislation at the turn of the millennium forced the tobacco industry to focus the majority of their marketing efforts abroad in countries with less tobacco restriction laws, including less-developed countries (Alberg et al., 2013; Ezzati & Lopez, 2003; Proctor, 2001; Smith, McLeod, & Wakefield, 2005; Youlden et al., 2008).
Health Care Providers’ Role in Lung Cancer Causation Theories
Medical Profession
The early years’ (1800–1900) medical journals published personalized accounts of physicians’ exposure to lung masses, including those that appeared cancerous. In 1882, a published discussion by a surgeon noted a causal link of lung tumors and smoking and warned of the abuse of tobacco smoking; noting that moderation was probably acceptable (“Editorials,” 1882). Another physician report in 1895 warned of the “habit” associated with “pleasurable irritation” of cigarette smoking (“Reports of Societies,” 1895). Tobacco smoking was opined by some to be responsible for the stunted growth of male teenage boys (“Preventive Medicine—The Use of Tobacco by Schoolboys—Medical Notes,” 1909). The invention of the X-ray machine in 1895 enabled physicians to diagnose lung tumors by visualization; however, the opportunity for medical students and physicians to view a black lung in an autopsy was rare, as lung cancer was a rare disease (Ochsner et al., 1947). In 1912, Isaac Adler was the first physician to publically write about the association of cigarette smoking to the development of lung cancer; however, his medical opinion was not well-received by his colleagues as like other men of that era, physicians smoked cigarettes (Doll & Hill, 1956; Nelson et al., 1994; Proctor, 2001). The manuscript, Tobaccoism or How Tobacco Kills, was published by Dr. John H. Kellogg, the director of a holistic medical sanatorium in 1922. The manuscript thoroughly describing the history of tobacco and the addiction that ensues from smoking as well as the huge financial burden on the government from tobacco-related diseases was rejected by his physician peers as non-scientific because of his reputation for dietary remedies for ailments (Kellogg, 1922). Observations were noted by physicians that smokers did not live as long as non-smokers; however, few would go on record as to the cause (Hammond & Horn, 1954). During the 1930s and 1940s, tobacco companies enlisted the help of physicians in their advertising campaign of cigarettes; the most successful being that of the “More Doctors . . . ” campaign in 1946. Not only did tobacco companies use real physician photos in their ads, they saved the American Medical Association (AMA) from financial demise through their generous contributions during the Great Depression (Gardner & Brandt, 2006). Physicians were employed by tobacco companies to find other causes of lung cancer (Nelson et al., 1994; White, 1990). One causal account, sponsored by the tobacco industry that was purported in medical journals included a genetic predetermination that people who get lung cancer would get it anyway and that smoking was responsible only for directing the site of cancer to the lungs (Doll & Hill, 1956).
Physician pioneers such as Doll and Hill, Hammond and Horn, and Wynder and Graham emerged with large case-controlled research studies that demonstrated the causal link between cigarette smoking and lung cancer in the early 1950s provoking the AMA and British Medical Research Council to address the causation issue (Doll & Hill, 1950; Hammond & Horn, 1954). The AMA responded by refusing to accept tobacco advertising in their journal; however, leadership rejected the link of tobacco to lung cancer as causal and considered it to be correlational only. The rationale behind their decision consisted of the following reasons: distrust of death certificates noting that cause of death could be erroneous; arsenic was considered the only known carcinogen; non-smokers got lung cancer; there was no increase in head and neck cancer related to smokeless tobacco use; and different mortality collection methods were believed to confound research outcomes (Gardner & Brandt, 2006; Glantz, 1995; White, 1990). Two thirds of physicians surveyed concurred with the AMA’s opinion; however, most began their own smoking cessation efforts that would continue to increase with each passing decade (Gardner & Brandt, 2006; Nelson et al., 1994). The specialty of oncology was officially recognized when The American Society of Clinical Oncology (ASCO) was founded in 1964 by seven cancer physicians to increase cancer treatment efforts and counteract the stigma associated with the incurable disease (http://www.cancerprogress.net/asco50).
After the National Cancer Act, also known as the “War on Cancer” was passed in 1971, AMA leadership decided to “fight tobacco” despite accepting more than US$18 million in research funding and support between 1964 and 1978 (Blum & Wolinsky, 1995). The concept of disbelief remained apparent even within cancer institute leadership. Wynder, considered the “father of tobacco control” wrote of his experience as a researcher at Memorial Sloan-Kettering Cancer Center. He wrote, shortly after his publicized disagreement with Dr. Clarence Little about tobacco (featured in the Journal of the American Medical Association; Wynder, 1997) that his new cancer center director, “while holding a cigarette” (Wynder, 1997) demanded censorship of Wynder’s tobacco research. Dr. Wynder appealed to the board of directors of the facility and the decision was overturned; however, the director was responsible for cutting the research funding so much that Dr. Wynder was forced to look for another research facility (Wynder, 1997).
The tobacco industry’s influence on the medical profession continued despite AMA’s endorsed support of anti-smoking exertions in the latter part of the 20th century manifesting itself as a paradox. For example, the 1985 AMA president owned property where tobacco was grown while AMA leadership supported anti-smoking research (Blum & Wolinsky, 1995). The AMA discouraged its members from accepting financial funding from the tobacco industry in 1995, although the industry continued to be one of the largest financial contributors to U.S. congressmen who were known as defenders of the tobacco corporations (Blum & Wolinsky, 1995). After the Master Settlement Agreement, AMA reorganized its stance on the anti-smoking movement to eliminate their double-standard way of conducting business and also supported the insertion of medical ethics curriculum into medical school education (Blum & Wolinsky, 1995).
As the 21st century began, the quandary that medicine found itself immersed in seemed to be resolved as all physician groups had no more disbelief that cigarette smoking caused lung cancer. Although smoking cessation interventions were and continue to be identified as insufficient within primary care practices; lack of patient support services and reimbursement is to be blamed (Carlston, Mattar, & Packard, 2012).
Nursing Profession
The profession of modern nursing evolved out of the need to care for patients that the medical profession could not meet. Early schools of nursing were run by physicians who required that nursing students be single and reside in dorms located within hospitals (Kalisch & Kalisch, 2004). In 1910, nursing recognized that cigarette smoking may be unhealthy as some advocated for a special diet designed to rid the body of stored up nicotine (Malone, 2006). Sophia Southall (1918) authored an expose in the American Journal of Nursing (AJN) titled “Shall We Smoke?” that discussed the health hazards of the cigarette habit and gave recognition to Kellogg and Dr. Kress of the Anti-Cigarette League for their efforts in exposing the damaging effects of cigarettes in 1918. Because of the profession’s predominance of women, nurses did not smoke, at least in public, as women were forbidden to smoke in the early 1900s (Kellogg, 1922).
Nurses as Smokers
As the profession expanded, more women became nurses and therefore also targets of the tobacco industry (Matheson & Bobay, 2007). Nurses were utilized in tobacco advertising; intended to promote the safety of smoking similar to that of the physician marketing campaign. According to Malone (2006), the editorial staff of AJN, the official publication of the American Nurses Association (ANA), only objected once, in 1932, to the use of a nurse in uniform because it implied that the nurse was working “on duty;” however continued to accept advertising dollars until 1950 (Malone, 2006). Nursing literature continued to be deficient in publishing articles about the ill-effects of tobacco on health as evidenced by only seven articles published in total from 1914 to 1954 (Malone, 2006). Nursing’s lack of a stance on tobacco smoking and the tobacco industry’s brilliant marketing to females was responsible for the increase in nurse smoking rates that climbed rapidly in the 1960s and 1970s. Nurses smoked in the nursing home, on duty and off duty (Rowe & Clark, 2000; Sarna, Bialous, Jun, et al., 2007).
Nurse researchers began conducting research in tobacco cessation in the late 1970s with the Nurses Health Survey commencing in response to tobacco’s marketing campaign (Sarna, Bialous, Jun, et al., 2007). The study described nurse smoking trends from 1976 to 2003. The study analysis found that women nurses continued to smoke even after women in society were beginning to cease and that 69% of nurses reported that they did not even try to quit smoking during the 27-year monitoring period. Licensed Practical Nursing smoking rates were consistent with smokers of lesser education. The Joint Commission on Accreditation of Healthcare Organizations’ 1993 mandate for smoke-free hospitals was considered a catalyst in smoking cessation among direct care provider nurses (Sarna, Bialous, Jun, et al., 2007). Research on women and smoking continued to grow as the number of doctoral-prepared nurses became interested in this important topic (Rowe & Clark, 2000).
It was not until the 1990s that some in nursing really initiated its activism against tobacco smoking via formation of groups like the Nightingales group (Malone, 2006). Nurse-managed tobacco cessation clinics emerged and professional nursing organizations incorporated smoke frees initiatives into their health policy agendas (Association, 1995) Nursing research remained deficient in smoking cessation articles until 2005, when more than 40 articles were published per year (Wells, Sarna, & Bialous, 2006). Tobacco Free Nurses was established with grant funding in 2003 to promote tobacco cessation education in nurses and has been successful in achieving its goals; however, Licensed Practitical Nursesmoking rates remain high (Sarna, Bialous, Wewers, et al., 2007).
Conceptual Themes in Lung Cancer Causation
In his book, How Scientists Explain Disease, philosopher Paul Thagard (2000) explained that medical theory should be defined with an underlying belief that the cause of disease and the cause of science are interconnected through physical, psychological, and social concepts. Thagard further elucidates that science is a result of individual minds and multifaceted social organization “schemas” that should include both cognitive and social rationalization to explicate scientific change. Causes of disease should be examined using medical explanation schemas. The origination for disease schemas can be logical, cognitive, social, or integrated cognitive-social. Thagard discusses that disease theories evolve or change through both cognitive and social processes experienced in conducting science.
Cancer is aptly applied within the molecular genetics schema that is a result of the discovery of cancer genetics made possible by Human Genome Project research (Collins et al., 1998). Cancer was once thought to be specific to its site origin; however, mutations that were first discovered as a cause in one type of cancer have been isolated in another type; thus demonstrating a common link. This schema leaves open whether mutations are inherited (familiar) or acquired through environmental exposures that damage tissue (like tobacco smoking, etc.). There are three genes involved in the molecular genetics disease explanation schema: oncogenes, tumor suppressor genes, and mutator genes. Oncogenes transform normal cells into cancerous ones; tumor suppressor genes help block that transformation and mutator genes develop as a result of exposures to environmental hazards (Thagard, 2000). Thagard (2000) clarified that the lung cancer explanation schema includes a causal network whereby heredity, behavior, environment, and virus causal elements affect mutations in cell growth genes and mutations in tumor suppressor genes resulting in a cancerous tumor are described in Figure 1.
Figure 1.
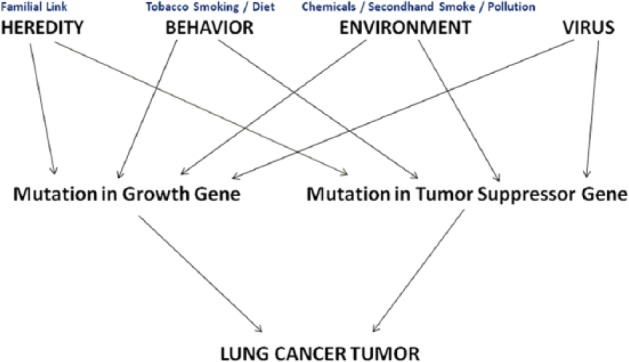
Mechanism of Lung Cancer Production
Note. Viral causation is missing from this figure, because of lack of evidence.
Thagard (2000) demonstrated that there are numerous cognitive processes involved in the determination and evolution of causations of disease. He illustrates how Cheng’s Power PC theory formula is best used by Epidemiology to explain the correlational cause that amount of smoking leads to increased risk of lung cancer. He also promotes the use of Hennekens and Buring’s Framework (Thagard, 2000) for the Interpretation of an Epidemiological study in explaining the causal connection between lung cancer and cigarette smoking. Both Cheng’s theory and Hennekens and Buring’s rationale of the development of lung cancer would not have been possible prior to the 1950s and 1960s when cigarette smoking was not scientifically identified as a cause of lung cancer but defined as a relationship with a strong associative bond. Epidemiology has since utilized frameworks that test a correlation as a possible cause of disease. For instance, the environmental elements of pesticides, road tar, silicone, viruses, bird dander, automobile smoke, and pollution that were hypothesized to be strong causes of lung cancer in the 20th century have since been proven to be insignificant correlational factors of the disease. Asbestos and radon have been identified as causes of lung cancer but with a much less statistical significance as compared with tobacco smoking (i.e., 2-fold compared with 20-fold risk, respectively). The case-controlled methods that physician scientists of the 1950s used to expose cigarette smoking as the overwhelming cause of lung cancer are still utilized within research today; however, with advances in data quality (Thagard, 2000).
Although the medical explanation is founded on the concepts of correlation, causes, and mechanisms, Thagard (2000) proposed a causal network instantiation to better explain the complex processes within disease involving the concepts of deduction, statistics, and single cause. Explanation is not deductive accounts for the fact that non-smokers can get lung cancer whereas some smokers do not. Explanation is not statistical takes into account that although smoking and air pollution can contribute to the development of lung cancer, there is not an exact computation to define risk and time for disease development. Explanation is not in terms of single causes is exemplified in smoking not being the solitary cause of lung cancer. Diseases are multifactorial such as in the case of a non-smoker exposed to years of daily secondhand smoke exposure and having a strong familial link to the disease developing lung cancer (Thagard, 2000).
Social processes, inclined to be discounted by the traditional philosophy of science, are a vital piece of the causation puzzle and play an important role in changing scientific ideas.
Although science is not a social construction, social processes advocate the use of consensus building among medical experts to reach an authoritative cause of disease and provide direction for disease prevention and management (Thagard, 2000). Social processes also have a detrimental effect as in the case of early lung cancer causations theories. The main social processes apparent in analyzing the history of lung cancer causation include social interest connections and power relations as well as concepts of disbelief, oppression, and greed.
Although cigarette smoking was suspected as far back as the early 1900s as disease causing, physicians such as Adler and Kellogg, who recognized this connection were rejected by their peers as eccentric and foolish. Although lack of lung cancer patients was to blame, there was no lack of cases of chronic lung diseases in smokers. Tobacco companies, in their quest for wealth via acceptability of their product by all citizens, engaged in a brilliant marketing campaign for more than a century. Cigarette smoking was a societal habit partaken by most physicians (predominantly male) and disbelief was rampant that “healers” would not engage in an activity that caused disease. The “More Physicians . . . ” advertising campaign of 1946 was responsible for deceiving millions of Americans that the dangerous addiction was safe. Physician smokers continued the habit for decades, while looking for other causes that justified lung cancer. It was not until the late 1950s that disbelief started to wane with the publications of Drs. Doll, Hill, Hammond, Horn, Wynder, and Graham and physicians started to stop smoking. The discipline of medicine and tobacco companies had a long and mutually lucrative relationship. This was obvious in the tobacco companies financial funding of the AMA for decades even after the 1964 U.S. Surgeon General’s report (Glantz, 1995; Proctor, 2012). The advancement of the subspecialty of oncology within the medicine realm and societal forces were instrumental in changing physician opinion of tobacco’s role in lung cancer formation from one of disbelief to acceptance.
The Context of Nurse Smoking
Much oppression is apparent when analyzing the nursing profession’s connection to tobacco smoking through a feminist perspective. Although Florence Nightingale is considered the founder of the nursing profession, the early education of nurses, almost exclusively female, was placed into the hand of a male-dominated medical profession. Nurses lacked autonomy, accountability, and control over the nursing profession (Roberts, 1994). In addition, female smoking was not acceptable in societal circles or in schools of nursing. The tobacco industry capitalized on this type of double oppression. During both World Wars and lasting through the women’s rights movement of the 1970s, tobacco smoking advertising was targeted at the “liberation” of women who were tired of being oppressed by a male-dominated society and finally allowed into the workforce. One of nursing’s mottos referred to being “bound in duty not women’s rights” and this statement fueled nurses’ desire to be considered significant within the medical setting (Fletcher, 2006). Like their medical colleagues, nurses were featured in marketing ads with the intent to promote the deception of product safety to the consumer. Early nurse leaders were dominated by their medical counterparts demonstrating that the lack of leadership in nursing was derived from society’s position of the female gender (Cleland, 1971).
As physicians were engaging in smoking cessation, nurses were trying to prove their independence in a sense by smoking as evidenced by physician smoking rates peaked in the 1960s and nurse smoking rates crested 20 years later. Nursing education eventually expanded to offer advanced degrees and grew independent from hospital schools of nursing run by the medical profession, enabling nurses to engage in anti-tobacco research; however, this did not occur until the 1980s. Cigarette smoking rates have declined among nurses but are still 4 times as high as physicians; exemplifying that the effects of oppression still exist within the profession. Sarna and Lillington (2002) reported that personal use of tobacco products by nurse researchers themselves most likely lead to the delay of tobacco abuse and cessation research (Sarna & Lillington, 2002). Nursing rates of smoking dropped just before anti-smoking was legislated in hospitals, and patients were prohibited to smoke on the units, and later regulations brought in no smoking throughout all hospitals (Sarna, Bialous, Jun, et al., 2007; Sarna, Bialous, Nandy, Antonio, & Yang, 2014).
Industries Responses to Smoking Rates
The concepts of oppression and greed and their relationship to tobacco smoking are not exclusive to the nursing profession. The tobacco industry continues to capitalize on exploiting the societal position of both the uneducated and poor as demonstrated by current statistical reports (“Tobacco and Socioeconomic Status,” 2014). Marketing campaigns aimed at getting teenagers, who want to be liberated from their parents, addicted to tobacco was proven highly effective as teenage smoking rates remain high as the teen years continue to be the age of tobacco addiction onset. Teens who succeed in higher education are the most successful at quitting smoking; however, addicted people of lower socioeconomic status are not (Katz, Wewers, Single, & Paskett, 2007). Poorer people are also persuaded by tobacco advertising that reward them with free items for buying their product.
Greed has played a part in the causation of lung cancer by the tobacco industry for over a century and is the underlying theme conjectured throughout the history of lung cancer causation. Not only did the tobacco industry generate billions on billions of dollars in revenue over the years, politicians and the U.S. government gained enormously. Politicians have been elected to Congress for decades powered by the tobacco industry to represent their special interests and keep regulation low. In the earlier years, the federal government’s silence about the role of tobacco in causing lung cancer was almost certainly clouded by the huge amount of tax revenue that the government received from the tobacco companies. Once the government officially acknowledged the ill-effects of tobacco and governments enacted anti-tobacco legislation; it has been demonstrated that making tobacco expensive and inconvenient has led to increased smoking cessation rates; consequently, tobacco tax dollars have had a positive effect on health (Fichtenberg & Glantz, 2002; Smith et al., 2005).
Implications for Nursing
Knowing and understanding the underlying history behind lung cancer causation can empower nurses in 2015, to take an active role in patient’s health as well as their own. Health care providers who smoke are less likely to promote smoking cessation in patients (Sarna, Bialous, Jun, et al., 2007). Nursing has long experienced oppressed group behaviors as described by Freire (Matheson & Bobay, 2007) to its detriment within the profession and these behaviors have contributed to manipulation by the tobacco industry.
Fully understanding oppression can lead nurses out of it and focus on the mission of improving the lives of oppressed patients (Dong & Temple, 2011; Dubrosky, 2013). Unfortunately, cancer patients continue to smoke at the same rate as non-cancer patients with denial of causation noted in one third of patients (Lehto, 2007; Sanders, Campbell, Donovan, & Sharp, 2007). Nurses can take an active role within the workplace in raising awareness and teaching patients to stop smoking. They can also take an active role within society by engaging in anti-tobacco legislation (Smith et al., 2005). As reported by Malone (2002, p.105), 1990 Tobacco industry letters documented a quotation by a company executive reporting “if mobilized, nurses could easily become formidable opponents for the tobacco industry.” This testimonial in addition to nursing being the largest and most respected profession in the United States, the consequences of such activism could be positively enormous (http://www.gallup.com/poll/1654/Honesty-Ethics-Professions.aspx). With respect to never-smokers with lung cancer, nurses need to educate these patients that their cancer is a completely different cancer type not caused by tobacco smoking but by different causation mechanisms. Nurses need to assist both smokers and non-smokers to combat the negative stigma that is attached to the diagnosis of lung cancer (Chapple, Ziebland, & McPherson, 2004; Hay, Shuk, Cruz, & Ostroff, 2005).
Conclusion
Smoking and lung cancer has a strong, pragmatic, multiple causal associations, meaning the incidence of smoking decreases when exposure to smoking decreases. Causation of chronic disease includes the identification of a host of environmental conditions and behaviors (vectors/vehicles) which may contain a causative agent for that disease to develop (Yerushalmy & Palmer, 1959). This could explain why all smokers do not get lung cancer and some never-smokers do; however, there is evolving medical evidence that each lung cancer is molecularly different (Alberg et al., 2013).
Thagard’s model of causal network effectively frames lung cancer as based not only on physical science but on the synergism of cognitive and social processes involved in disease explanation with tobacco smoking identified as a powerful carcinogen. Dominant social forces (see Table 1) suppressed the recognition of the cigarette smoking link to lung cancer incidence surmising millions of human lives could have been saved. Analyzing the changing perceptions of disease causation from a historical perspective can teach us to avoid the negative consequences of history. We must learn to investigate all possible causes of disease with the same merit despite the origination of the idea is from sociology science, or philosophy; accepted truth can lie within many forms of knowledge (Thagard, 2000). All health care providers have the responsibility to learn how disease causation evolves as the concepts innately effect how patients receive quality care. Importantly, ideas of disease causation interface with sociological norms of behavior to form habits and rates of health behavior, and nursing has a moral obligation to intercede and advocate for health, when these behaviors are harmful (Pooler, 2014). Future nursing research should focus on improving smoking cessation interventions through the utilization of self-efficacy measures and also by integrating them within healthy lifestyle education. Nurses need to take ownership of empowering patients to live healthy lifestyles by exemplifying a healthy lifestyle themselves.
Table 1.
Timeline of Social Forces as a Context in Lung Cancer Causation.
| Decade | Social Forces |
|---|---|
| 1800s | Smoking was only socially allowed by men (“Editorials,” 1882) |
| No smoking in public until age 21; high society started the trend (“Editorials,” 1882) | |
| Women who smoked were “fallen women” (Amos & Haglund, 2000; Kellogg, 1922) | |
| Anti-Cigarette League of America formed by teacher, Lucy Gaston (Tate, 2000) | |
| 1900 | Men smokers; women closet smokers if at all (Hammond & Horn, 1954; “Preventive Medicine—The Use of Tobacco by Schoolboys—Medical Notes,” 1909) |
| Woman arrested for smoking in public (Amos & Haglund, 2000) | |
| Laws against women smokers (G. A. Britton, 1998) | |
| 1910 | In response to World War I, women took male-oriented jobs and started dressing and smoking like men (Proctor, 2012) |
| Poorer people start to smoke (Proctor, 2001) | |
| 1920 | Tobacco money in billions range and was used for lobbying (Nelson et al., 1994) Smokers denial published as anecdotes that smoking cures aches and pains and asthma (Nelson et al., 1994) Annual expenditures on tobacco more than US$ 1.5 billion (Proctor, 2012) |
| 1930 | German and Spanish ID tobacco as hazardous to health—First countries to do so (Witschi, 2001) |
| Smoking found everywhere in society even among poor during Great Depression (Amos & Haglund, 2000) | |
| Nazi anti-smoking tobacco movement in Germany due to the country’s advances in tobacco research but was short-lived because people hated Hitler (Gilman & Zhou, 2004) | |
| 1940 | World War II |
| Federal Trade Commission gets involved in Tobacco trade complaints between tobacco co. and slows down “More Physicians . . . ” Campaign (Gardner & Brandt, 2006) | |
| Tobacco Co. employees have higher death Ins. claims than non-tobacco workers 1946–1954 (Cornfield et al., 2009) | |
| 1950 | 1954 Tobacco Cos. Publically deny research findings of both British and American studies (Glantz, Barnes, Bero, Hanauer, & Slade, 1995) |
| 1957 Statisticians reject physician studies as flawed (Fisher, 1958) | |
| American Cancer society begins first Cancer Act prevention study in 1959 (Thun & Heath, 1997) | |
| Sublime Tobacco published by Compton McKenzie in 1957 praising tobacco without harm (Mackenzie, 1957) | |
| 1959 U.S. Surgeon General’s Statement about tobacco and Lung Cancer link (Use, 2000) | |
| 1960 | U.S. Surgeon General Report of 1964 states that cigarette smoking causes lung cancer (Use, 2000) Tobacco Lobby stronger (Wynder, 1961) |
| 1970 | National Cancer Act 1971—Beginning of the “war on cancer” (Letton, 1996) |
| Federal Election Act of 1972—Demands public disclosure of politicians campaign contributions (Tobacco was highest contributor; Fleishman, 1972) | |
| Big shift to lower socioeconomic class (Kuper, Adami, & Boffetta, 2002) | |
| Women’s Rights movement (ERA; G. A. Britton, 1998) | |
| American Cancer Society “Great American Smoke Out” starts yearly in 1977 (November; Centers for Disease Control and Prevention, 1997) | |
| U.S. Contraband Cigarette Trafficking Act 1978 prohibits tobacco smuggling (Kuper et al., 2002) | |
| 1980 | California is the first state to increase tobacco tax which results in a decline in smokers in that state (Hu, Sung, & Keeler, 1995) |
| Men smoking rates decline; women with higher smoking rates than men (Youlden, Cramb, & Baade, 2008) | |
| Majority of lung cancer patients did not believe that smoking caused their lung cancer (Lehto, 2007) | |
| 1982—Surgeon General of the U.S. Public Health Service Report rule tobacco a carcinogen (Use, 2000) | |
| 1990 | 1992—U.S. Surgeon Gen declares war on the tobacco companies (Use, 2000) |
| Clinton administration Health Care Express for nationalized health care insurance (Brock & Daniels, 1994) | |
| CDC/American Cancer Society/National Cancer Institute start “American stop smoking intervention study” (Letton, 1996) | |
| 1994—U.S. states start to litigate against tobacco co. (Vernick, Rutkow, & Teret, 2007) | |
| 1995—California First statewide ban on indoor smoking (Slade, 1992) | |
| Joint Commission on Accredidation of Healthcare Organizations mandate smoke-free hospitals in 1993 (Sarna, Bialous, Jun, et al., 2007) | |
| Brown-Williamson Tobacco Co. documents exposed (Glantz et al., 1995) | |
| 2000 | Largest push for smoke-free legislation between 2004 and 2007 (Jha & Peto, 2014) |
| Smoke-free New York City (Schwartz, 1992) | |
| Cigarette taxes increases across states (Jha & Peto, 2014) | |
| 2006 Surgeon General Report SG report (U.S. Department of Health and Human Services, 2006) | |
| 2009 Family Smoking Prevention & Tobacco Control Act passed (Gostin, 2009) | |
| Female smoking plateau (Youlden et al., 2008) | |
| 2010–present | 2014—28 states with statewide smoking bans; 6 states with public places bans; 6 states with restrictions (http://www.fda.gov/) without any bans; however, large cities have indoor bans (Jha & Peto, 2014) |
| Food and Drug Association issues first order to stop sale & distribution of tobacco products in 2014 (http://www.fda.gov/) | |
| U.S. tobacco taxes yield US$32 billion in 2010 (Jha & Peto, 2014) |
Note. CDC = Centers for Disease Control and Prevention.
Author Biography
Tracy A. Ruegg has been a Certified Nurse Practitioner in Oncology for the past 20 years. She is also currently a PhD student @ the University of Utah College of Nursing where her research interest is focused on improving symptom management in cancer patients.
Footnotes
Author’s Note: The author of this article was a T32 NR013456-01 fellow of the University of Utah College of Nursing when the article was developed.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by funding for Open Access provided by The Ohio State University Open Access Fund.
References
- Alberg A. J., Brock M. V., Ford J. G., Samet J. M., Spivack S. D. (2013). Epidemiology of lung cancer: Diagnosis and management of lung cancer, 3rd ed.: American College of Chest Physicians evidence-based clinical practice guidelines. Chest, 143(5 Suppl.), e1S–29S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Society of Clinical Oncology. (n.d.). ASCO@50. Retrieved from http://www.cancerprogress.net/asco50
- Amos A., Haglund M. (2000). From social taboo to “torch of freedom”: The marketing of cigarettes to women. Tobacco Control, 9, 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson S. J. (2011). Marketing of menthol cigarettes and consumer perceptions: A review of tobacco industry documents. Tobacco Control, 20(Suppl. 2), ii20–ii28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association, A. A. N. (1995). Position statement: Cessation of tobacco use. Indianapolis, IN: American Nurses Association. [Google Scholar]
- Blum A., Wolinsky H. (1995). AMA rewrites tobacco history. The Lancet, 346(8970), 261. [DOI] [PubMed] [Google Scholar]
- Britton G. A. (1998). A review of women and tobacco: Have we come such a long way? Journal of Obstetric, Gynecologic & Neonatal Nursing, 27, 241–249. [DOI] [PubMed] [Google Scholar]
- Britton J., Lewis S. (1992). Pet birds and lung cancer. British Medical Journal, 305, 970–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brock D. W., Daniels N. (1994). Ethical foundations of the Clinton administration’s proposed health care system. Journal of American Medical Association, 271, 1189–1196. [PubMed] [Google Scholar]
- Carlston D. L., Mattar A. A., Packard J. (2012). Exploratory analysis of patients’ motivations to quit smoking and participate in smoking cessation classes. Family Medicine, 44, 727–730. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (1997). Impact of promotion of the Great American Smokeout and availability of over-the-counter nicotine medications, 1996. Morbidity and Mortality Weekly Report, 46(37), 867. [PubMed] [Google Scholar]
- Chapple A., Ziebland S., McPherson A. (2004). Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. British Medical Journal, 328, 1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland V. (1971). Sex discrimination: Nursing’s most pervasive problem. American Journal of Nursing, 71, 1542–1547. [PubMed] [Google Scholar]
- Collins F. S., Patrinos A., Jordan E., Chakravarti A., Gesteland R., Walters L. (1998). New goals for the US human genome project: 1998-2003. Science, 282, 682–689. [DOI] [PubMed] [Google Scholar]
- Cornfield J., Haenszel W., Hammond E. C., Lilienfeld A. M., Shimkin M. B., Wynder E. L. (2009). Smoking and lung cancer: Recent evidence and a discussion of some questions. 1959. International Journal of Epidemiology, 38, 1175–1191. [DOI] [PubMed] [Google Scholar]
- Doll R., Hill A. B. (1950). Smoking and carcinoma of the lung; preliminary report. British Medical Journal, 2, 739–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R., Hill A. B. (1956). Lung cancer and other causes of death in relation to smoking; a second report on the mortality of British doctors. British Medical Journal, 2, 1071–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong D., Temple B. (2011). Oppression: A concept analysis and implications for nurses and nursing. Nursing Forum, 46, 169–176. [DOI] [PubMed] [Google Scholar]
- Dubrosky R. (2013). Iris Young’s five faces of oppression applied to nursing. Nursing Forum, 48, 205–210. [DOI] [PubMed] [Google Scholar]
- Editorials. (1882). The Boston Medical and Surgical Journal, 107(21), 500–503. [Google Scholar]
- Editorials and medical intelligence. (1854). The Boston Medical and Surgical Journal, 49(26), 527–532. [Google Scholar]
- Ezzati M., Lopez A. D. (2003). Estimates of global mortality attributable to smoking in 2000. The Lancet, 362, 847–852. [DOI] [PubMed] [Google Scholar]
- Fichtenberg C. M., Glantz S. A. (2002). Effect of smoke-free workplaces on smoking behaviour: Systematic review. British Medical Journal, 325, 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher R. A. (1958). Lung cancer and cigarettes? Nature, 182, 108. [DOI] [PubMed] [Google Scholar]
- Fleishman J. L. (1972). Freedom of speech and equality of political opportunity: The constitutionality of the Federal Election Campaign Act of 1971. North Carolina Law Review, 51, 389. [Google Scholar]
- Fletcher K. (2006). Beyond dualism: Leading out of oppression. Nursing Forum, 41, 50–59. [DOI] [PubMed] [Google Scholar]
- Fraumeni J. F., Wertelecki W., Blattner W. A., Jensen R. D., Leventhal B. G. (1975). Varied manifestations of a familial lymphoproliferative disorder. American Journal of Medicine, 59, 145–151. [DOI] [PubMed] [Google Scholar]
- Gallup. (n.d.). Honesty/ethics in professions. Retrieved from http://www.gallup.com/poll/1654/Honesty-Ethics-Professions.aspx
- Gardner M. N., Brandt A. M. (2006). “The doctors’ choice is America’s choice”: The physician in US cigarette advertisements, 1930-1953. American Journal of Public Health, 96, 222–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman S. L., Zhou X. (2004). Smoke: A global history of smoking. London, UK: Reaktion Books [Google Scholar]
- Glantz S. A. (1995). Tobacco, history, and the AMA. The Lancet, 346, 510. [PubMed] [Google Scholar]
- Glantz S. A., Barnes D. E., Bero L., Hanauer P., Slade J. (1995). Looking through a keyhole at the tobacco industry: The Brown and Williamson documents. Journal of American Medical Association, 274, 219–224. [PubMed] [Google Scholar]
- Glick M. (2007). Editorial. Causation: A loosely founded concept in epidemiology. Journal of the American Dental Association, 138, 1532–1533. [DOI] [PubMed] [Google Scholar]
- Gostin L. O. (2009). FDA regulation of tobacco: Politics, law, and the public’s health. Journal of American Medical Association, 302, 1459–1460. [DOI] [PubMed] [Google Scholar]
- Hajdu S. I. (2011). Much overlooked causes of lung cancer. Annals of Clinical & Laboratory Science, 41, 97–101. [PubMed] [Google Scholar]
- Hammond E. C., Horn D. (1954). The relationship between human smoking habits and death rates: A follow-up study of 187,766 men. Journal of American Medical Association, 155, 1316–1328. [DOI] [PubMed] [Google Scholar]
- Hay J., Shuk E., Cruz G., Ostroff J. (2005). Thinking through cancer risk: Characterizing smokers’ process of risk determination. Qualitative Health Research, 15, 1074–1085. [DOI] [PubMed] [Google Scholar]
- Hu T.-W., Sung H.-Y., Keeler T. E. (1995). Reducing cigarette consumption in California: Tobacco taxes vs. an anti-smoking media campaign. American Journal of Public Health, 85, 1218–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha P., Peto R. (2014). Global effects of smoking, of quitting, and of taxing tobacco. New England Journal of Medicine, 370, 60–68. [DOI] [PubMed] [Google Scholar]
- Joffe M. (2011). The gap between evidence discovery and actual causal relationships. Preventive Medicine, 53, 246–249. [DOI] [PubMed] [Google Scholar]
- Kalisch P. A., Kalisch B. J. (2004). American nursing: A history. Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Katz M. L., Wewers M. E., Single N., Paskett E. D. (2007). Key informants’ perspectives prior to beginning a cervical cancer study in Ohio Appalachia. Qualitative Health Research, 17, 131–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman N. J. (1994). Smoking and young women: The physician’s role in stopping an equal opportunity killer. Journal of American Medical Association, 271, 629–630. [DOI] [PubMed] [Google Scholar]
- Kellogg J. H. (1922). Tobaccoism or how tobacco kills. Battle Creek, MI: Modern Medicine. [Google Scholar]
- Kuper H., Adami H. O., Boffetta P. (2002). Tobacco use, cancer causation and public health impact. Journal of Internal Medicine, 251, 455–466. [DOI] [PubMed] [Google Scholar]
- Lehto R. H. (2007). Causal attributions in individuals with suspected lung cancer: Relationships to illness coherence and emotional responses. Journal of the American Psychiatric Nurses Association, 13, 109–115. [Google Scholar]
- Letton A. H. (1996). The 25th anniversary of the National Cancer Act of 1971. Cancer, 78, 2597–2598. [PubMed] [Google Scholar]
- Lichtenstein P., Holm N. V., Verkasalo P. K., Iliadou A., Kaprio J., Koskenvuo M., . . .Hemminki K. (2000). Environmental and heritable factors in the causation of cancer—Analyses of cohorts of twins from Sweden, Denmark, and Finland. New England Journal of Medicine, 343, 78–85. [DOI] [PubMed] [Google Scholar]
- Lipton R., Odegaard T. (2005). Causal thinking and causal language in epidemiology: It’s in the details. Epidemiologic Perspectives & Innovations, 2, Article 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie C. (1957). Sublime tobacco. London: Chatto & Windus. [Google Scholar]
- Malone R. E. (2002). Nursing, our public deaths, and the tobacco industry. American Journal of Critical Care, 11, 102–105. [PMC free article] [PubMed] [Google Scholar]
- Malone R. E. (2006). Nursing’s involvement in tobacco control: Historical perspective and vision for the future. Nursing Research, 55(4S), S51–S57. [DOI] [PubMed] [Google Scholar]
- Matheson L. K., Bobay K. (2007). Validation of oppressed group behaviors in nursing. Journal of Professional Nursing, 23, 226–234. [DOI] [PubMed] [Google Scholar]
- Miettinen O. S., Rossiter C. E. (1990). Man-made mineral fibers and lung cancer: Epidemiologic evidence regarding the causal hypothesis. Scandinavian Journal of Work, Environment & Health, 16, 221–231. [DOI] [PubMed] [Google Scholar]
- Nelson D. E., Emont S. L., Brackbill R. M., Cameron L. L., Peddicord J., Fiore M. C. (1994). Cigarette smoking prevalence by occupation in the United States: A comparison between 1978 to 1980 and 1987 to 1990. Journal of Occupational Medicine, 36, 516–525. [PubMed] [Google Scholar]
- Ochsner A., De Bakey M., Dixon J. L. (1947). Primary cancer of the lung. Journal of American Medical Association, 135, 321–327. [DOI] [PubMed] [Google Scholar]
- Parascandola M. (2011). Causes, risks, and probabilities: Probabilistic concepts of causation in chronic disease epidemiology. Preventive Medicine, 53, 232–234. [DOI] [PubMed] [Google Scholar]
- Parascandola M, Weed D.L. (2001) Causation in epidemiology, J Epidemiol Ciommunity Health, 55, 905-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pooler C. (2014). Living with chronic lower pulmonary disease: Disruptions of the embodied phenomenological self. Global Qualitative Nursing Research, 1, 2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C. A., III, Thun M. J., Namboodiri M. M., Dockery D. W., Evans J. S., Speizer F. E., Heath C. W., Jr. (1995). Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. American Journal of Respiratory and Critical Care Medicine, 151(3, Pt. 1), 669–674. [DOI] [PubMed] [Google Scholar]
- Preventive medicine—The use of tobacco by schoolboys—Medical notes. (1909). The Boston Medical and Surgical Journal, 161, 93–96. [Google Scholar]
- Proctor R. N. (2001). Tobacco and the global lung cancer epidemic. Nature Reviews Cancer, 1(1), 82–86. [DOI] [PubMed] [Google Scholar]
- Proctor R. N. (2012). The history of the discovery of the cigarette-lung cancer link: Evidentiary traditions, corporate denial, global toll. Tobacco Control, 21, 87–91. [DOI] [PubMed] [Google Scholar]
- Reports of societies. (1895). The Boston Medical and Surgical Journal, 133(13), 321–326. [Google Scholar]
- Roberts S. J. (1994). Oppressed group behavior: Implications for nursing. Revolution: The Journal of Nurse Empowerment, 4, 28-31, 33-35. [PubMed] [Google Scholar]
- Robson A. O., Jelliffe A. M. (1963). Medicinal arsenic poisoning and lung cancer. British Medical Journal, 2, 207–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe K., Clark J. M. (2000). Why nurses smoke: A review of the literature. International Journal of Nursing Studies, 37, 173–181. [DOI] [PubMed] [Google Scholar]
- Sanders T., Campbell R., Donovan J., Sharp D. (2007). Narrative accounts of hereditary risk: Knowledge about family history, lay theories of disease, and “internal” and “external” causation. Qualitative Health Research, 17, 510–520. [DOI] [PubMed] [Google Scholar]
- Sarna L., Bialous S. A., Jun H., Wewers M. E., Cooley M., Feskanich D. (2007). Trends in smoking status in the Nurse’s Health Study (1976-2001). Communicating Nursing Research, 40, 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarna L., Bialous S. A., Nandy K., Antonio A. L., Yang Q. (2014). Changes in smoking prevalences among health care professionals from 2003 to 2010-2011. Journal of American Medical Association, 311, 197–199. [DOI] [PubMed] [Google Scholar]
- Sarna L., Bialous S. A., Wewers M. E., Froelicher E. S., Wells M., Balbach E. D. (2007). Web log analysis of the first two years of the tobacco free nurses website. Online Journal of Nursing Informatics, 11(3). [Google Scholar]
- Sarna L., Lillington L. (2002). Tobacco: An emerging topic in Nursing Research. Nursing Research, 51, 245–253. [DOI] [PubMed] [Google Scholar]
- Schwartz J. L. (1992). Methods of smoking cessation. The Medical Clinics of North America, 76, 451–476. [DOI] [PubMed] [Google Scholar]
- Siegel R., Naishadham D., Jemal A. (2013). Cancer statistics, 2013. CA: A Cancer Journal for Clinicians, 63, 11–30. [DOI] [PubMed] [Google Scholar]
- Slade J. (1992). A retreat in the tobacco war. Journal of American Medical Association, 268, 524–525. [PubMed] [Google Scholar]
- Smith K. C., McLeod K., Wakefield M. (2005). Australian letters to the editor on tobacco: Triggers, rhetoric, and claims of legitimate voice. Qualitative Health Research, 15, 1180–1198. [DOI] [PubMed] [Google Scholar]
- Southall S. J. (1918). Shall we smoke? The American Journal of Nursing, 18, 459–460. [Google Scholar]
- Tate C. (2000). Cigarette wars: The triumph of the little white slaver. Oxford, UK: Oxford University Press. [PubMed] [Google Scholar]
- Thagard P. (2000). How scientists explain disease. Princeton, NJ: Princeton University Press. [Google Scholar]
- Thun M. J., Heath C. W., Jr. (1997). Changes in mortality from smoking in two American Cancer Society prospective studies since 1959. Preventive Medicine, 26, 422–426. [DOI] [PubMed] [Google Scholar]
- Tobacco and socioeconomic status. (2014). Retrieved from http://www.tobaccofreekids.org/research/factsheets/pdf/0260.pdf
- U.S. Department of Health and Human Services. (2006). The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- Use R. T. (2000). A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Vernick J. S., Rutkow L., Teret S. P. (2007). Public health benefits of recent litigation against the tobacco industry. Journal of American Medical Association, 298, 86–89. [DOI] [PubMed] [Google Scholar]
- Vincent R. G., Takita H., Lane W. W., Gutierrez A. C., Pickren J. W. (1976). Surgical therapy of lung cancer. Journal of Thoracic Cardiovascular Surgery, 71, 581–591. [PubMed] [Google Scholar]
- Wells M., Sarna L., Bialous S. A. (2006). Nursing research in smoking cessation: A listing of the literature, 1996-2005. Nursing Research, 55(4S), S16–S28. [DOI] [PubMed] [Google Scholar]
- White C. (1990). Research on smoking and lung cancer: A landmark in the history of chronic disease epidemiology. Yale Journal of Biology Medicine, 63(1), 29–46. [PMC free article] [PubMed] [Google Scholar]
- Witschi H. (2001). A short history of lung cancer. Toxicological Sciences, 64, 4–6. doi: 10.1093/toxsci/64.1.4 [DOI] [PubMed] [Google Scholar]
- Wynder E. L. (1961). An appraisal of the smoking-lung-cancer issue. New England Journal of Medicine, 264, 1235–1240. [DOI] [PubMed] [Google Scholar]
- Wynder E. L. (1997). Tobacco as a cause of lung cancer: Some reflections. American Journal of Epidemiology, 146, 687–694. [DOI] [PubMed] [Google Scholar]
- Yerushalmy J., Palmer C. E. (1959). On the methodology of investigations of etiologic factors in chronic diseases. Journal of Chronic Diseases, 10, 27–40. [DOI] [PubMed] [Google Scholar]
- Youlden D. R., Cramb S. M., Baade P. D. (2008). The international epidemiology of lung cancer: Geographical distribution and secular trends. Journal of Thoracic Oncology, 3, 819–831. [DOI] [PubMed] [Google Scholar]


