Abstract
Depression in mothers is a significant risk factor for the development of maladjustment in children. This paper focuses on modifiable risk processes linking depression in mothers and adaptation in their young children (i.e., infancy through preschool-age). First, the authors present evidence of the efficacy of interventions for reducing the primary source of risk – maternal depression. Second, they describe a central mechanism – parenting behaviors – underlying the relation between maternal depression and children’s adjustment. Third, the authors recommend two different integrated interventions that successfully treat mothers’ depression and enhance parenting skills with infants and young children. Finally, the paper notes the possible need for supplementary interventions to address severity and comorbidity of mothers’ depression, barriers to engaging in treatment, and the sustainability of program benefits.
In this paper, we describe key risk processes linking maternal depression to problematic developmental outcomes in young children and review evidence that these risk processes can be changed through behavioral interventions. We focus here on early development (i.e., infancy through preschool age) for several reasons. First, rates of maternal depression during that time are high (Ertel, Rich-Edwards, & Koenen, 2011). Second, mothers and children typically spend a great deal of time together early in life as compared to when children are in school. Third, the rapid changes in emotional and cognitive development make children especially vulnerable to the effects of maternal depression during this time (Bagner, Petit, Lewinsohn, & Seeley, 2010). Fourth, stressors associated with depression in mothers during children’s early development have been linked with enduring changes that increase risk of psychopathology later in development (Baram et al., 2012). Finally, interventions early in development may alter what otherwise might have been a negative trajectory of child outcomes (Cicchetti & Toth, 2009).
What accounts for the relation between maternal depression and adverse child outcomes, and what interventions can break this link? Two crucial points are implicated in the chain between maternal depression and child maladaptation and these are our suggested targets of intervention: (a) reduce the risk factor itself – maternal depression, with its various cognitive, affective, and behavioral features that are associated with adverse child development (Goodman & Gotlib, 1999), and (b) modify an especially critical and malleable consequence of that risk – dysfunctional parenting behaviors. Thus, the overall aims are to alleviate the mother’s depression, thereby reducing offspring’s early life exposure to its symptoms and correlates, and enhance parenting qualities that facilitate children’s healthy development. We provide evidence to support targeting these two risk processes in integrated interventions and for their feasibility, efficacy, and cost-effectiveness, even in the context of poverty and comorbid psychopathology.
Depression in Mothers
Worldwide, the prevalence of depression is more than two times greater in women than in men. Across races and ethnicities, about 10% of U.S. mothers experience a major depressive episode (MDE) per year, resulting in an estimated 1 in 10 children being exposed to maternal depression each year (Ertel et al., 2011); about 13% of women experience an MDE during the first postpartum year (O’Hara & Swain, 1996). Rates of major depressive disorder (MDD) are higher for those living in poverty, with almost 50% of low income mothers of infants and young children having depression (Knitzer, Theberge, & Johnson, 2008). We focus here on mothers because of their high rates of depression, the effects of depression exposure during pregnancy, and the greater amount of time mothers as compared to fathers typically spend with young children. Of note, however, depression in fathers also is associated with problems in children and should be the focus of study as well.
Depression in Mothers and Children’s Adjustment
Offspring of depressed mothers score lower on tests of cognitive development and are at increased risk of psychopathology as compared to children of nondepressed mothers. A meta-analytic review of 193 studies reported that depression in mothers was significantly associated with children’s internalizing (e.g. depression, anxiety) and externalizing (e.g. behavior disorders) problems (r’s =.23 & .21, respectively), beginning at the earliest ages at which such problems can be measured reliably and validly (i.e. 18 months). Maternal depression also was associated with children’s high negative affect and behavior (e.g. irritability, sadness, fear) and low positive affect and behavior (e.g. smiling, cooing, approach) (r’s =.15 & −.10, respectively) (Goodman et al., 2011). Although the latter are small effect sizes, they are known to be predictive of the later emergence of psychopathology (Dougherty, Klein, Durbin, Hayden, & Olino, 2010).
The relation between maternal depression and child adjustment varies, however. In particular, associations were stronger for younger children, girls (for internalizing problems, specifically), families living in poverty, ethnic minority parents, and unmarried parents (the latter were specific to externalizing problems and negative affect/behavior) (Goodman et al., 2011). Therefore, reducing depression, especially in mothers of infants and young children, may be one direct means of improving children’s developmental trajectories with regard to internalizing and externalizing problems, negative and positive affect, and cognitive and emotional development.
Depression can be treated
Depression in adults can be treated successfully with cognitive, behavioral, and interpersonal psychotherapies, as well as with antidepressant medications (ADMs). The benefits of ADMs are particularly robust for individuals with severe depression (see Hollon, 2016 for a review). ADMs are the most common treatment for depression in child-bearing age women (Ko, Farr, Dietz, & Robbins, 2012). Nevertheless, there are concerns about breastfeeding women taking ADMs. Fortunately, efficacious alternatives to medications are available.
Cognitive behavior therapy (CBT) teaches depressed individuals to recognize the connections among situations, thoughts, feelings, and behaviors, to examine the accuracy of their beliefs, and to consider alternative explanations for stressful events. In the treatment of current major depression, CBT is about equally as effective as ADMs and superior to pill-placebo (Hedges g = 0.53, a medium effect size) (Cuijpers et al., 2013). Importantly, CBT has enduring effects that last beyond the end of the acute treatment, and are about the same as remaining on ADMs. CBT also is about two and a half times more likely to prevent recurrence as compared to stopping ADMs (see Hollon, 2016 for a review). With regard to perinatal depression in particular, a meta-analytic review (Sockol, 2015) showed that interventions based on CBT resulted in significant reductions in depressive symptoms compared to controls, with even greater reductions in depression in studies that included higher proportions of mothers who were nonwhite, single, and had more than one child.
Interpersonal Therapy (IPT) aims to reduce depression associated with interpersonal difficulties and helps patients work through disputes, role transitions, and grief by targeting communication and relational processes. IPT is effective for treating depression in women, albeit often in combination with ADMs (e.g. Frank et al., 2000), and has been modified to be culturally relevant to women living in urban poverty (Grote et al., 2009). O’Hara and colleagues (2000) found that in women with a postnatal MDE, those randomly assigned to 12 weeks of IPT had significantly greater reductions in depressive symptoms, improvement in social adjustment, and recovery from their episode as compared to women in a waiting list control condition.
In addition to these treatments for current depressive episodes, mindfulness-based cognitive therapy (MBCT) is effective for preventing the recurrence of depression (see Piet & Hougaard, 2011 for a review). This is important because risk of recurrence is high (22% for those who have had one MDE, 67% for those who have had three or more episodes) (Keller, Lavori, Lewis, & Klerman, 1983). For mothers of infants, MBCT has been modified for the prevention of depression during the perinatal period (MBCT-PD) in particular, and has shown evidence of efficacy (Dimidjian et al., 2015).
Overall, empirical evidence indicates that depression can be treated effectively, evidence-based psychosocial treatments have enduring effects, and the recurrence of depression can be prevented. Moreover, these treatments can be effective with depressed individuals who are low-income, racial or ethnic minorities when additional steps are taken to decrease barriers and increase engagement (Levy & O’Hara, 2010). Thus, it may be possible to diminish the negative consequences of maternal depression on young children by reducing or even eliminating the very source of the risk itself through treatment.
Nevertheless, although effective empirically-based interventions for depression exist, many depressed mothers of young children remain untreated or receive inadequate treatment; this is especially true for mothers from racial/ethnic minorities and those with less education (Witt et al., 2011). Practical barriers that interfere with treatment seeking include cost, transportation, and childcare; psychological and cultural factors include stigma and distrust of the mental health system. At the systems level, too few mental health professionals are trained in evidence-based practices (Acri & Hoagwood, 2014). Thus, although there is a compelling case for treatment, far too few depressed mothers get any or adequate treatment.
Do the Benefits of Alleviating Depression in Mothers “Trickle down” to their Children?
Even if mothers get adequate treatment, do children benefit from successful treatment of their mother’s depression? A recent meta-analytic review of nine randomized controlled trials (RCTs) compared the effect of psychotherapy versus controls on mothers’ depression, parent functioning, and children’s outcomes (Cuijpers, Weitz, Karyotaki, Garber, & Andersson, 2015). Therapy was associated with significantly decreased levels of depression in mothers (g = 0.66; a medium effect size), improved mental health in children (g = 0.40; a small effect size), better mother-child interactions (g = 0.35; a small effect size), and less parenting/marital distress (g = 0.67; a medium effect size), with g representing the strength of the association (e.g., g = 0.66 indicates that the average person in the therapy group would score lower on depression than about 75% of those in the control condition) (Coe, 2002). Thus, psychotherapy can decrease mothers’ level of depression and may positively affect their parenting and their children’s mental health.
There was considerable variability across studies, however. For example, one investigation found that effective treatment of postpartum depression was not associated with improvements in emotionality, internalizing, and externalizing problems in infants at 18 months (Forman et al., 2007). Thus, treating depression in mothers, especially early, may be an important step toward minimizing its negative effects on children, but treatment alone may not be sufficient. Therefore, we propose an alternative approach: integrated interventions that reduce mothers’ depression while also explicitly focusing on a key mechanism in the complex relation between maternal depression and children’s adjustment – mothers’ parenting behaviors.
Mothers with Depression: Parenting as a Risk Process
Transmission of risk for maladjustment in children of depressed mothers occurs partly via children being exposed to mothers’ negative affect, cognitions, and behaviors, and to the stressors that often accompany depression (Goodman & Gotlib, 1999). Heritability of depression is modest (i.e., about 37%), indicating that the environment also plays a role in its transmission (Sullivan, Neale, & Kendler, 2000). We focus here on parenting in particular because of its strong impact on children throughout development, especially in infants, toddlers, and preschool-aged children; parenting is a central mechanism through which maternal depression affects children and can be modified successfully and cost-effectively.
Parenting behaviors that disrupt or fail to promote healthy development are an important mechanism through which maternal depression affects children (Goodman & Gotlib, 1999). Depression is associated with mothers’ being less able to provide their children with age-appropriate care, and with negative parenting behaviors (e.g., harsh, critical) known to contribute to the development of psychopathology. In a meta-analytic review of observational studies of depressed mothers interacting with their children, Lovejoy and colleagues (2000) found significant, moderate associations between maternal depression and more hostile (e.g., negative affect, coercive) and disengaged or withdrawn parenting (e.g., ignoring), and less positive parenting behaviors (e.g., affection, positive activities). This is especially concerning for infants, who rely on sensitive, responsive care, and toddlers and preschoolers, who rely on authoritative parenting in the context of positive emotions to promote healthy outcomes (Bornstein, 2006). These parenting issues are the precise targets of the interventions we are recommending here.
Parenting behaviors of mothers with their infants, toddlers, and preschool-aged children have been found to mediate (i.e., at least partially account for) the relation between maternal depression and infant and child development, even over the long term (e.g. Murray, Marwick, & Arteche, 2010), including in low income, ethnic minority families (Riley et al., 2009). Given that negative parenting sometimes persists even after mothers’ depression remits (Forman et al., 2007) and the uncertain benefits to children of focusing only on treating the mother’s depression, an integrated model of care that both reduces her depression and enhances her parenting skills is warranted. Such an integrated approach is consistent with the summary recommendation of the Institute of Medicine report on depression in parents (2009).
Interventions to Improve Parenting by Mothers of Infants and Young Children
Several approaches have been found to effectively enhance the quality of parenting by mothers of infants, toddlers, and preschool-aged children. We focus here on two programs – Home Visiting and Triple P – both of which have demonstrated feasibility of large scale dissemination and also have been found to reduce mothers’ depressive symptoms.
Home Visiting Programs (HVP), which aim to help mothers’ develop sensitive, responsive parenting skills that facilitate infant development, especially among low-income mothers, are feasible and effective in enhancing the quality of parenting of infants, but are less effective for mothers with depression (Ammerman, Putnam, Bosse, Teeters, & Van Ginkel, 2010). An adaptation of HVP’s, In-Home CBT (IH-CBT), implemented by therapists (typically masters level mental health professionals with prior experience with CBT for depressed adults) concurrently with home visiting, aims to promote new mothers’ engagement with the intervention by explicitly addressing her concerns (e.g. social isolation) and supporting her relationship with the home visitor.
The IH-CBT component consists of 15 weekly sessions of about 60 minutes each plus a booster session about one month post treatment, with all sessions administered in the home, typically with the child present. To reduce the mother’s depression, components of CBT are implemented, including behavioral activation, identification of automatic thoughts and schemas, thought restructuring, and cognitive rehearsal, with a focus on relapse prevention in later sessions. Sessions are structured; therapists follow a manual while also individualizing treatment for each mother (e.g. dealing with trauma or addiction, as needed). To ensure coordinated care and to support the home visitor who trains the mother on parenting skills, IH-CBT therapists collaborate and consult with the home visitors by maintaining regular contact throughout the sessions and at a joint closing session. IH-CBT therapists typically are supervised by doctoral level professionals, with a weekly 2-hour meeting of a team of 4 to 6 therapists.
In an RCT with an ethnically diverse sample of mothers of five-month-old infants, those in the IH-CBT condition were less likely than mothers receiving the HVP alone to meet diagnostic criteria for MDD at post-treatment (IH-CBT: 29.3% vs. HVP: 69.8%) and at follow-up (20.5% vs. 52.6%), reported fewer depressive symptoms, and obtained lower clinician ratings of depression severity (Ammerman, Putnam, Altaye, Stevens, et al., 2013). In addition, they reported increased social support, improved functioning in daily activities, and decreased psychological distress (Ammerman, Putnam, Altaye, Teeters, et al., 2013); these findings were maintained through to the 3-month follow-up (Ammerman et al., 2015). Because IH-CBT and HVP alone did not differ significantly regarding infants’ social and emotional functioning and observed parenting, Ammerman and colleagues (2015) combined data across groups and found that as mothers’ depression improved, there were parallel improvements in their parenting (e.g., more nurturing and stimulating).
Home visiting programs in general, and IH-CBT specifically, are cost-effective (Karoly, Kilburn, & Cannon., 2005). An economic analysis revealed that IH-CBT was cost-effective over three years, provided there was a willingness-to-pay threshold of $25,000/Quality Adjusted Life Years. This finding reflects an estimated 8 additional depression-free months in mothers in the first year following treatment (Ammerman, 2015).
Finally, a program called Moving Beyond Depression (MBD) has been established to facilitate dissemination of IH-CBT (e.g., see http://www.movingbeyonddepression.org). It has been implemented in nine states in the U.S. MBD staff members help new sites to implement the program, train staff, and offer ongoing training and support.
For mothers of toddlers and preschool-aged children, Triple P – Positive Parenting Program – has strong evidence for enhancing authoritative parenting in the context of positive emotions, preventing the development of emotional and behavioral problems in toddlers and preschoolers, maintaining gains, being cost effective, and being acceptable to parents from diverse cultures (Morawska et al., 2011; Sanders & Kirby, 2014). Similar to the adaptation of HVPs to address the challenges of parenting by new mothers with depression, Enhanced Triple P was developed for mothers with depression as an adjunctive treatment that teaches CBT skills (e.g. coping, identifying and challenging maladaptive thoughts) for managing their depression and improving parenting (Sanders, Markie-Dadds, Tully, & Bor, 2000). In addition, because depression in mothers often co-occurs with marital conflict, a second adjunctive component targets partner support.
Enhanced Triple P involves up to 15 weekly, 60- to 90-minute sessions, with standard parent training procedures (i.e., positive parenting, having reasonable expectations, recognizing and responding to children’s emotions) integrated with modules addressing mood management strategies, stress coping skills, and partner support skills. Alternatively, families may complete the parent training modules and then the Enhanced Triple P training in 3 to 10 additional individual sessions. Based on the initial assessment, modules are individually selected for a particular family and may include behavioral communication skills training to increase support from family, partners, or friends, or brief cognitive therapy strategies to help mothers manage their depression, anxiety, and stress. Families typically have been recruited through media and community outreach campaigns at child care centers and community health centers, or based on mothers’ depression screens conducted at child or mother routine care visits. Sessions are scheduled at hours convenient for the family and occur in the home or in local community health or neighborhood centers.
Dissemination is enhanced by an extensive training program for practitioners, typically masters level counselors, parent educators, or social workers, with training (2 days) and accreditation (a half day) by Triple P offered in several cities in the U.S. and around the world (http://www.triplep.net/glo-en/getting-started-with-triple-p/). The training program itself has been evaluated in at least three studies and was found to be associated with trainees’ enhanced skills in parent training and parent consultation (Seng, Prinz, & Sanders, 2006). These studies, however, did not include Enhanced Triple P training, which requires an additional 2- day training and half-day accreditation, also offered by Triple P.
A meta-analytic review of 12 studies encompassing diverse cultures and ethnicities revealed that Enhanced Triple P was significantly associated with short-term increases in mothers’ adjustment (d = 0.37), improved parenting practices (d = 0.71), and better social, emotional, and behavioral outcomes in children (d = 0.53). Results from follow-up studies were even stronger (d’s = 0.73, 0.81, and 0.79, respectively); d’s of 0.50 and 0.80 are considered medium and large effect sizes, respectively; d’s of 0.70 or higher indicate that the average person in the Enhanced Triple P group scored higher than 76% of the people in the control condition (Coe, 2002; Sanders, Kirby, Tellegen, & Day, 2014). Thus, Enhanced Triple P has been shown to reduce maternal depression, improve parenting, and prevent further growth of child behavior problems; it also has been found to be cost-effective and can be widely disseminated.
Summarizing across these two programs (i.e., IH-CBT; Enhanced Triple P), the evidence is strong for being able to improve parenting and effectively reduce depression in mothers of infants, toddlers, and preschool-aged children. Moreover, both approaches can be delivered at relatively low cost by paraprofessionals or masters level clinicians.
Efficacy of these interventions has been assessed using various evidence-based measures. For For the depression target, mothers’ depression typically is assessed with self-report (e.g. Beck Depression Inventory-II; Beck, Steer, & Brown, 1997) and clinical interviews (SCID; First, Spitzer, Gibbon, & Williams, 2002). A strong and feasible measure of the key, targeted parenting constructs is the HOME Inventory, which is a standardized observational measure of the home environment (Caldwell & Bradley, 1984). To assess the ultimate target - children’s social and emotional functioning - the Ages and Stages Questionnaire (Squires, Bricker, & Twombly, 2002) for infants and the Child Behavior Checklist for children ages 1.5 to 5 (Achenbach & Rescorla, 2000) are feasible measures of the targeted child outcomes, ideally obtained from multiple sources (e.g. a parent and another caregiver).
An Integrated Approach: Recommendations for Practice and Policy
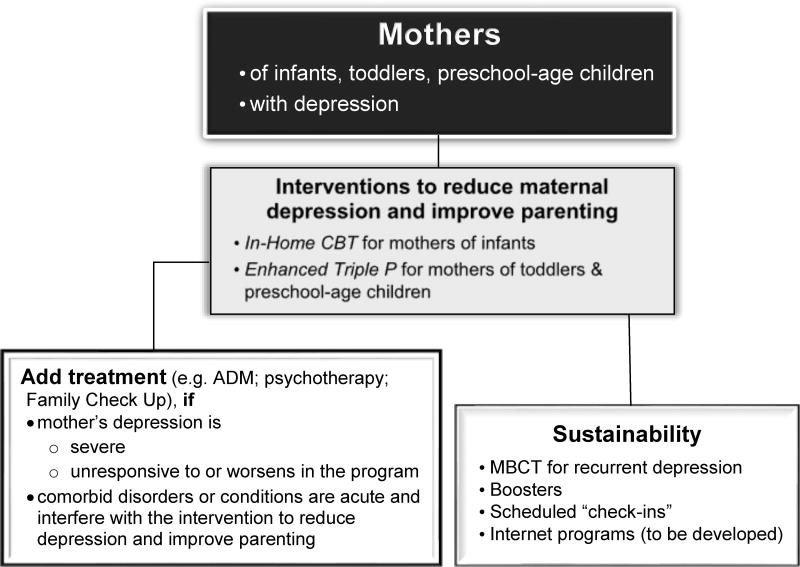
A strength of these two programs is that they efficiently address the two risk processes: depression in mothers and parenting. Within an integrated intervention, mothers can simultaneously learn to manage their depressive symptoms and enhance their parenting ability. A set of additional steps potentially can improve these approaches and enhance feasibility even further: some at the front end, concerning selection and entry into the intervention, and another at the back end, concerning maintenance or sustainability of the program benefits (see Figure 1). Both involve taking a more personalized approach to matching the treatment to each mother’s particular circumstances.
Figure 1.
Framework for interventions aimed at reducing mothers’ depression and enhancing parenting skills
At the front end, three sets of initial steps are promising for enhancing benefits over and above the empirical support for IH-CBT and Enhanced Triple P, and also address feasibility of their large-scale dissemination. First, as recommended by the U.S. Preventive Services Task Force, it is essential that all women with depression who are parenting infants be identified via universal screening with any of the several psychometrically sound screening tools (Siu & and the U. S. Preventive Services Task Force, 2016) and systems (Loudon, Nentin, & Silverman, 2015). Inextricably linked with screening must be systems for referral and follow-up to ensure entry into one of the empirically-supported treatments for women who screen positive for depression. The referral and follow-up might best be facilitated with co-location of mental health personnel within the medical setting so they can be immediately available (Reynolds & Frank, 2016) and thereby reduce the burden on the women to seek services in multiple clinics. Viable options include embedding the screening as well as the IH-CBT and Enhanced Triple P programs into routine obstetrical or pediatric care, such as women’s six-week postpartum check or at well-baby visits during the first year postpartum, consistent with a coordinated care model.
Second, mothers’ depression severity and common comorbid conditions must be addressed. For some women, their depression may be so severe or they may have co-occurring disorders (e.g. addiction) or life circumstances (e.g. inadequate housing; intimate partner violence) for which they might also benefit from (a) a more intensive evidence-based treatment for depression (reviewed previously), (b) another intervention for an acute or impairing co-morbid condition, or (c) assistance with major life stressors.
A third addition at the front end would be to address barriers to entering a program and to reduce drop-out rates. Programs are likely to be more successful to the extent that they are: affordable, offer flexible scheduling or alternatives to face-to-face meetings (e.g., telephone), locate services within the primary care setting to make them more accessible (if not in-home), assist women in prioritizing care for their own well-being and for their parenting, resolve misunderstandings or skepticism about the relevance and potential benefit of the interventions being offered, enhance motivation, work toward realistic expectations, and facilitate trust (Levy & O’Hara, 2010). For these various issues, we recommend an initial assessment and feedback/engagement session, similar to the Family Check-Up (FCU) approach (Shaw, Connell, Dishion, Wilson, & Gardner, 2009), during which a service provider respectfully addresses the mother’s particular concerns and barriers, provides assessment feedback, and collaboratively develops a plan for subsequent sessions to work on the agreed upon issues. We further recommend that progress in reducing mothers’ depression and enhancing parenting be monitored with routinely scheduled assessments over the course of the intervention to determine when providing additional treatment modules is warranted to address new or persisting barriers, comorbidities, or conditions interfering with the treatment plan.
At the back end, we recommend steps for enhancing maintenance and sustainability of the program benefits. Most importantly, we advocate a health maintenance model, whereby program staff contact families periodically (e.g., annually) and also at specified developmental transitions (see below). To prevent depression relapse, mothers with multiple prior episodes would be guided to MBCT, either in a group, if available, or alternatively, self-guided through a workbook (Williams, Teasdale, Segal, & Kabat-Zinn, 2007) or an online program that has shown promising evidence of effectiveness (Felder, Dimidjian, Beck, Boggs, & Segal, 2014). Another recommendation for enhancing maintenance of intervention gains is for pediatricians or family physicians to screen new mothers at routine well-child and vaccination visits and to make referrals as needed.
In terms of maintaining improvements in parenting behaviors, there is mixed evidence for booster sessions relative to a control condition, involving a follow-up assessment and referral to a local provider, if needed (Kolko, Lindhiem, Hart, & Bukstein, 2014). The most promising approaches to maintenance involve the original intervention teaching skills that will generalize over time and across situations (e.g. problem solving, stress management, anger management, communication), and after the intervention facilitating the use of internet relevant resources for information and contact (Eyberg, Edwards, Boggs, & Foote, 1998; Witkiewitz & Marlatt, 2011).
To maintain parent training effects, the intervention should teach parenting skills relevant not only for the age of the child at the time, but also for children as they mature. Although many of the parenting principles are appropriate across ages, others change as children develop; therefore, the parenting skills should be re-visited and updated across time. This could be accomplished by annual check-in calls or visits and by providing mothers with access to materials relevant to later ages, either on paper or via online parenting programs. Many of the latter are currently under construction and include essential training elements such as opportunities for questions-and-answer exchanges, assessments with feedback, and practice assignments; these programs have shown promising evidence of efficacy (e.g. Breitenstein, Shane, Julion, & Gross, 2015).
A broader issue is the work force that is required to implement these recommendations (Acri & Hoagwood, 2014). Well-trained and supervised paraprofessionals and master’s level clinicians are perfectly suited for coordinating referrals based on the screening tools as well as for administering the intervention. In addition to program specific training, providers will need to learn about infant development, maternal mental health, parenting of infants, engaging depressed mothers in treatment, building and maintaining a therapeutic relationship, and screening and referral for associated problems. Feasibility would be enhanced with active recruitment of talented eligible students, public funding for these training programs, and the use of online resources for training. Training itself must be evidence-based.
Overall, the main take-home message from this review is that efficacious interventions exist for reducing maternal depression and improving parenting, with good evidence for integrated programs that address both risk processes simultaneously. At the policy level, our conclusion is consistent with the National Research Council and Institute of Medicine (2009) recommendation of a coordinated approach that combines: (a) treating the mother’s depression and (b) training mothers on parenting skills. Given the number of years that have passed without those recommendations having been put into routine practice, and in light of the evidence that effective interventions exist, however, it is clear that these issues have not yet received adequate attention from policy makers, health care managers, and directors of training programs. We hope that the recommendations proposed here provide a clear path forward. Dissemination of these two programs into routine care, with the suggested modifications, will result in the reduction of risk (depression in mothers and adverse parenting) and, subsequently, better child adaptation.
Acknowledgments
This work was supported in part by grants from NIMH (R01MH100258; R01MH64735) and a Hobbs Discovery Grant, Vanderbilt University Central.
Contributor Information
Sherryl H. Goodman, Emory University.
Judy Garber, Vanderbilt University.
References
- Achenbach TM, Rescorla LA. ASEBA preschool forms & profiles. University of Vermont, Research Center for children, youth and families; Burlington, VT: 2000. [Google Scholar]
- Acri MC, Hoagwood KE. Addressing parental mental health within interventions for children: A review. Research on Social Work Practice. 2014;25:578–586. doi: 10.1177/1049731514546027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman, R. T. (2015, December 10, 2015). Personal communication
- Ammerman RT, Altaye M, Putnam FW, Teeters AR, Zou Y, Van Ginkel JB. Depression improvement and parenting in low-income mothers in home visiting. Archives of Women’s Mental Health. 2015;18:555–563. doi: 10.1007/s00737-014-0479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of in-home CBT for depressed mothers in home visitation. Behav Ther. 2013;44:359–372. doi: 10.1016/j.beth.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Teeters AR, Stevens J, Van Ginkel JB. Treatment of depressed mothers in home visiting: Impact on psychological distress and social functioning. Child Abuse Negl. 2013;37:544–554. doi: 10.1016/j.chiabu.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Bosse NR, Teeters AR, Van Ginkel JB. Maternal Depression in Home Visitation: A Systematic Review. Aggression and Violent Behavior. 2010;15:191–200. doi: 10.1016/j.avb.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Petit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:699–707. doi: 10.1016/j.jaac.2010.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baram TZ, Davis EP, Obenaus A, Sandman CA, Small SL, Solodkin A, Stern H. Fragmentation and Unpredictability of Early-Life Experience in Mental Disorders. American Journal of Psychiatry. 2012;169:907–915. doi: 10.1176/appi.ajp.2012.11091347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. Second. San Antonio: Texas: The Psychological Corporation; 1997. [Google Scholar]
- Bornstein MH. Parenting Science and Practice. Hoboken, NJ: John Wiley & Sons Inc; 2006. [Google Scholar]
- Breitenstein SM, Shane J, Julion W, Gross D. Developing the eCPP: Adapting an Evidence-Based Parent Training Program for Digital Delivery in Primary Care Settings. Worldviews on Evidence-Based Nursing. 2015;12:31–40. doi: 10.1111/wvn.12074. [DOI] [PubMed] [Google Scholar]
- Caldwell BM, Bradley RH. Home observation for measurement of the environment. University of Arkansas at little Rock; Little Rock: 1984. [Google Scholar]
- Cicchetti D, Toth SL. The past achievements and future promises of developmental psychopathology: The coming of age of a discipline. Journal of Child Psychology and Psychiatry. 2009;50:16–25. doi: 10.1111/j.1469-7610.2008.01979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe R. It’s the effect size, stupid: What effect size is and why it is important. Paper presented at the British Educational Research Association; Exeter, England. 2002. [Google Scholar]
- Cuijpers PC, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry. 2013;58:376. doi: 10.1177/070674371305800702. [DOI] [PubMed] [Google Scholar]
- Cuijpers PC, Weitz E, Karyotaki E, Garber J, Andersson G. The effects of psychological treatment of maternal depression on children and parental functioning: a meta-analysis. European Child & Adolescent Psychiatry. 2015;24:237–245. doi: 10.1007/s00787-014-0660-6. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, Beck A. Staying well during pregnancy and the postpartum: A pilot randomized trial of mindfulness-based cognitive therapy for the prevention of depressive relapse/recurrence. Journal of Consulting and Clinical Psychology. 2015;84:134–145. doi: 10.1037/ccp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty LR, Klein DN, Durbin CE, Hayden EP, Olino TM. Temperamental positive and negative emotionality and children’s depressive symptoms: A longitudinal prospective study from age three to age ten. Journal of Social and Clinical Psychology. 2010;29:462–488. doi: 10.1521/jscp.2010.29.4.462. [DOI] [Google Scholar]
- Ertel KA, Rich-Edwards JW, Koenen KC. Maternal Depression in the United States: Nationally Representative Rates and Risks. Journal of Women’s Health. 2011;20:1609–1617. doi: 10.1089/jwh.2010.2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg SM, Edwards D, Boggs SR, Foote R. Maintaining the Treatment Effects of Parent Training: The Role of Booster Sessions and Other Maintenance Strategies. Clinical Psychology: Science and Practice. 1998;5:544–554. doi: 10.1111/j.1468-2850.1998.tb00173.x. [DOI] [Google Scholar]
- Felder J, Dimidjian S, Beck A, Boggs JM, Segal Z. Mindful Mood Balance: A Case Report of Web-Based Treatment of Residual Depressive Symptoms. The Permanente Journal. 2014;18:58. doi: 10.7812/TPP/14-019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. New York. [Google Scholar]
- Forman DR, O’Hara MW, Stuart S, Gorman LL, Larsen KE, Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- Frank E, Grochocinski VJ, Spanier CA, Buysse DJ, Cherry CR, Houck PR, Kupfer DJ. Interpersonal psychotherapy and antidepressant medication: Evaluation of a sequential treatment strategy in women with recurrent major depression. Journal of Clinical Psychiatry. 2000;61:51–57. doi: 10.4088/JCP.v61n0112. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell A, Broth M, Hall C, Heyward D. Maternal Depression and Child Psychopathology: A Meta-Analytic Review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A Randomized Controlled Trial of Culturally Relevant, Brief Interpersonal Psychotherapy for Perinatal Depression. Psychiatr Serv. 2009;60:313–321. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD. The efficacy and acceptability of psychological interventions for depression: where we are now and where we are going. Epidemiology and psychiatric sciences. 2016:1–6. doi: 10.1017/S2045796015000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karoly LA, Kilburn MR, Cannon JS. Early childhood interventions: proven results, future promise. Santa Monica, CA: RAND; 2005. [Google Scholar]
- Keller MB, Lavori PW, Lewis CE, Klerman GL. Predictors of relapse in major depressive disorder. JAMA. 1983;250:3299–3304. [PubMed] [Google Scholar]
- Knitzer J, Theberge S, Johnson K. Reducing maternal depression and its impact on young children: Toward a responsive early childhood policy framework. New York: National Center for Children in Poverty; 2008. [Google Scholar]
- Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health (Larchmt) 2012;21:830–836. doi: 10.1089/jwh.2011.3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolko D, Lindhiem O, Hart J, Bukstein O. Evaluation of a Booster Intervention Three Years After Acute Treatment for Early-Onset Disruptive Behavior Disorders. Journal of Abnormal Child Psychology. 2014;42:383–398. doi: 10.1007/s10802-013-9724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy LB, Hara MW. Psychotherapeutic interventions for depressed, low-income women: A review of the literature. Clinical Psychology Review. 2010;30:934–950. doi: 10.1016/j.cpr.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Loudon H, Nentin F, Silverman ME. Using clinical decision support as a means of implementing a universal postpartum depression screening program. Archives of Women’s Mental Health. 2016;19:501–505. doi: 10.1007/s00737-015-0596-y. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Morawska A, Sanders M, Goadby E, Headley C, Hodge L, McAuliffe C, Anderson E. Is the Triple P-Positive Parenting Program acceptable to parents from culturally diverse backgrounds? Journal of Child and Family Studies. 2011;20:614–622. [Google Scholar]
- Murray L, Marwick H, Arteche A. Sadness in mothers’ ‘baby-talk’ predicts affective disorder in adolescent offspring. Infant Behavior and Development. 2010;33:361–364. doi: 10.1016/j.infbeh.2010.03.009. [DOI] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine. Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry. 2000;57:1039–1045. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Swain AM. Rates and risk of postpartum depression: A meta-analysis. International Review of Psychiatry. 1996;8:37–54. [Google Scholar]
- Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clinical Psychology Review. 2011;31:1032–1040. doi: 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, Frank E. US preventive services task force recommendation statement on screening for depression in adults: Not good enough. JAMA Psychiatry. 2016;73:189–190. doi: 10.1001/jamapsychiatry.2015.3281. [DOI] [PubMed] [Google Scholar]
- Riley AW, Coiro MJ, Broitman M, Colantuoni E, Hurley KM, Bandeen-Roche K, Miranda J. Mental Health and Functioning of Children of Low-Income Depressed Mothers: Influences of Parenting, Family Environment, and Raters. Psychiatr Serv. 2009;60:329–336. doi: 10.1176/appi.ps.60.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders MR, Kirby JN. A Public-Health Approach to Improving Parenting and Promoting Children’s Well-Being. Child Development Perspectives. 2014;8:250–257. doi: 10.1111/cdep.12086. [DOI] [Google Scholar]
- Sanders MR, Kirby JN, Tellegen CL, Day JJ. The Triple P-Positive Parenting Program: A systematic review and meta-analysis of a multi-level system of parenting support. Clinical Psychology Review. 2014;34:337–357. doi: 10.1016/j.cpr.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Sanders MR, Markie-Dadds C, Tully LA, Bor W. The triple P-positive parenting program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology. 2000;68:624. [PubMed] [Google Scholar]
- Seng AC, Prinz RJ, Sanders MR. The role of training variables in effective dissemination of evidence-based parenting interventions. International Journal of Mental Health Promotion. 2006;8:20–28. [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Dev Psychopathol. 2009;21:417–439. doi: 10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siu AL, the U. S. Preventive Services Task Force Screening for depression in adults: Us preventive services task force recommendation statement. JAMA. 2016;315:380–387. doi: 10.1001/jama.2015.18392. [DOI] [PubMed] [Google Scholar]
- Sockol LE. A systematic review of the efficacy of cognitive behavioral therapy for treating and preventing perinatal depression. Journal of Affective Disorders. 2015;177:7–21. doi: 10.1016/j.jad.2015.01.052. [DOI] [PubMed] [Google Scholar]
- Squires J, Bricker D, Twombly E. The ASQ: SE user’s guide: For the Ages & Stages Questionnaires: Social-emotional. Baltimore, MD: Paul H Brookes; 2002. [Google Scholar]
- Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Williams M, Teasdale JD, Segal ZV, Kabat-Zinn J. The Mindful Way through Depression: Freeing Yourself From Chronic Unhappiness. NY: Guilford Press; 2007. [Google Scholar]
- Witkiewitz KA, Marlatt GA. Therapist’s guide to evidence-based relapse prevention. Boston: Academic Press; 2011. [Google Scholar]
- Witt WP, Keller A, Gottlieb C, Litzelman K, Hampton J, Maguire J, Hagen EW. Access to adequate outpatient depression care for mothers in the USA: A nationally representative population-based study. The Journal of Behavioral Health Services & Research. 2011;38:191–204. doi: 10.1007/s11414-009-9194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]