Abstract
Positive behavior support (PBS) strategies in early childhood, which include proactively structuring environments to support and positively reinforce healthy dietary and physical activity behaviors, is critical to preventing pediatric obesity, particularly among low-income, ethnic minority children. Existing evidence-based family-centered preventive interventions effectively impact parents’ use of PBS strategies. Enhancing these programs to more directly target the key mechanisms of change specific to promoting children’s healthy lifestyle behaviors could serve as the foundation for the next generation of effective protocols for preventing pediatric obesity. Two established programs that target PBS that can be feasibly implemented in a variety of service delivery systems using a multi-tiered, adaptive approach and the next steps of translation are discussed.
Pediatric obesity is a complex public health problem affecting the majority of developed countries worldwide (National Research Council and Institute of Medicine, 2011). In the United States, the prevalence of overweight and obesity among children aged 2 to 5 years is 22.8% and 31.8% for youth aged 2 to 19 years with ethnic minorities, particularly Hispanic and American Indian youth, showing the highest rates (Ogden, Carroll, Kit, & Flegal, 2014). Cardiovascular disease risk factors (e.g., high blood pressure, cholesterol) frequently occur and tend to cluster in youth classified as overweight or obese (Goodman, Dolan, Morrison, & Daniels, 2005). By the time youth reach adolescence, an alarming 49% and 61% of those who are overweight and obese, respectively, exhibit at least one risk factor for cardiovascular disease over and above weight status (May, Kuklina, & Yoon, 2012).
Early childhood is a critical period for prevention because 60% of children who are overweight during the preschool period will be overweight at age 12 (Nader et al., 2006). According to the Centers for Disease Control and Prevention, poor diet and physical inactivity—the key contributors to obesity—are among the leading causes of preventable death in youth (Eaton et al., 2012). As such, diet and physical activity are often the primary behavioral targets of obesity prevention efforts. Yet despite the tremendous need to prevent obesity, few efficacious programs have been developed and implemented on a scale that has had an appreciable public health impact (Denzer, Reithofer, Wabitsch, & Widhalm, 2004).
Although national guidelines for youth dietary intake and physical activity are well defined, lifestyle behavior change is challenging. Healthcare professionals charged with the primary prevention of pediatric obesity report that low familial motivation to change and poor adherence with recommendations for lifestyle change are among the most critical barriers (Kolagotla & Adams, 2004). Further, parents’ maladaptive family management practices are associated with pediatric weight gain (e.g., Kitzman-Ulrich et al., 2010) and also hinder their ability to effectively implement healthy lifestyle recommendations in young children (Faith et al., 2012). Preventive interventions that teach caregivers the skills required to implement behavior change in accord with expert guidelines for obesity prevention are needed (e.g., Krebs, Jacobson, & American Academy of Pediatrics Committee on Nutrition, 2003).
This article highlights the central role of parents’ use of positive behavior support (PBS) strategies during early childhood for the prevention of obesity. PBS is an effective and widespread behavior management principle that emphasizes the use of nonaversive, reinforcing caregiver–child interactions and involves the use of specific strategies such as proactively structuring the child’s environment and reinforcing positive behaviors. Because few pediatric obesity interventions have assessed whether parental involvement results in improved parenting skills (e.g., PBS), and whether these changes, in turn, are related to child outcomes (Davison, Lawson, & Coatsworth, 2012), we draw from the broader field of prevention science to inform a family-centered blueprint for obesity prevention during the critical 0 to 6 age period. Family-centered prevention programs for children rely on developmental science to identify intervention targets and research has established these targets as critical mechanisms of action through meditational analyses (e.g., Sandler, Schoenfelder, Wolchik, & MacKinnon, 2011). Importantly, parenting mechanisms of action have been clearly defined, operationalized, and measured, a noted ongoing challenge in the field of pediatric obesity (Power et al., 2013). Although programs use a variety of labels for similar intervention targets, positive parenting is fundamental and explicitly targeted in nearly all evidence-based family-centered interventions (see Sandler, Ingram, Wolchik, Tein, & Winslow, 2015).
The goal of this Special Section is to identify the most critical modifiable risk and/or protective processes that should be addressed within prevention to benefit specific at-risk populations. We argue that targeting parents’ use of PBS strategies, both generally as they relate to positive child development and more specifically as they pertain to supporting healthy lifestyle behaviors, is critical for the prevention of obesity in early childhood, particularly among low-income, ethnic minority children who are at the highest risk for obesity and have been shown to benefit from the protective effects of positive parenting. PBS is among the most critical protective factors for pediatric obesity that is modifiable with existing, evidence-based interventions for young children. Certainly other risk (e.g., living in poverty, parent weight status) and protective factors (e.g., family meals, higher socioeconomic status) also contribute to the development of obesity in early childhood. Given the limited space allotted to this article, we focused on one protective factor (PBS) that is malleable in early childhood, a known mediator of program effects on obesity, and targeted by existing efficacious programs ready for delivery at scale.
We establish the importance of family-centered prevention and then present data from efficacious preventive interventions demonstrating that parents’ use of PBS is modifiable and has been shown to effect childhood obesity. We then describe the specific links between PBS strategies and intervening processes in the development of pediatric obesity (e.g., healthy food availability, opportunities for physical activity, child inhibitory control). Finally, we discuss the adaptation and delivery of two family-centered evidence-based parenting programs that target PBS and have been found to reduce obesity rates: ParentCorps (Brotman et al., 2012), and the Family Check-Up (FCU; Dishion et al., 2008).
The Family and Pediatric Obesity Prevention
Ecological models of child health and pediatric obesity (e.g., Fiese & Jones, 2012) underscore the importance of the family system. Recent meta-analyses of pediatric obesity interventions conclude that programs that involve parents are among the most efficacious, particularly when targeting ethnic minority youth (e.g., Janicke et al., 2014; Niemeier, Hektner, & Enger, 2012; Seo & Sa, 2010). Including caregivers in obesity prevention efforts is important in several ways: they model healthy lifestyle habits and are the gatekeepers of opportunities for healthy nutrition and physical activity. Importantly, positive parenting in childhood has also been shown to act as a buffer between disadvantaged environments (i.e., low SES) and negative obesity-related health outcomes, including metabolic syndrome, in adulthood (Miller et al., 2011). Recently published reviews on the topic underscore the significance of familial involvement and indicate that youth weight and/or health behaviors may be improved (1) when parents attend and are directly involved in sessions; (2) when parents are provided training in lifestyle modification; and (3) when strategies to improve positive parenting skills and lifestyle components are combined (e.g., Kitzman-Ulrich et al., 2010; Sung-Chan, Sung, Zhao, & Brownson, 2013).
Positive Behavior Support and Children’s Health
Family-centered prevention programs delivered during early childhood are efficacious at improving a range of child health outcomes, including weight gain/obesity and inhibitory control; notably, positive parenting consistently mediates intervention effects (Sandler et al., 2011). For example, improvements in positive parenting partially mediated the effects of the efficacious Incredible Years program on negative behaviors in low-income children aged 2 to 9; and changes were maintained at 18-months follow-up (Gardner, Burton, & Klimes, 2006). Recent studies also indicate that family-centered prevention programs affect pediatric obesity and associated mechanisms despite not explicitly targeting weight-related health behavior change nor incorporating obesity-specific intervention targets (e.g., diet, physical activity). In a long-term follow up of two prevention trials, Brotman and colleagues (Brotman et al., 2012) found that relative to controls, 4-year olds randomized to a family-based intervention targeting PBS, called ParentCorps, had a lower body mass index (BMI) and improved physical activity, sedentary behavior, and dietary intake three to five years later.
Participation in a randomized trial of the FCU at age 2 was associated with caregivers’ increased use of PBS at age 3. This in turn predicted parents serving more nutritious meals to the child (from ages 2 to 5), a less steep increase in child BMI from age 5 to 9.5, and reduced prevalence of obesity rates at age 9.5 among children classified as “at risk for obesity” at age 5 (Smith, Montaño, Dishion, Shaw, & Wilson, 2015). The identified pathway between PBS and reduced weight gain via the caregiver serving the child a healthier diet is a crucial finding for understanding the mechanisms in family-centered obesity prevention––a noted deficit of the existing literature (e.g., Janicke et al., 2014). Further, improvement in PBS has been shown to mediate the effects of the FCU program on inhibitory control (Lunkenheimer et al., 2008) in low-income ethnically-diverse young children (aged 2–5). Child inhibitory control, or the ability for delayed gratification and emotion regulation, has been associated with parenting, diet and physical activity, and pediatric obesity in cross sectional, longitudinal, and randomized intervention studies (for a review, see Anzman-Frasca, Stifter, & Birch, 2012). For example, in a prospective longitudinal cohort study (N = 1,061), poorer self-regulation at ages 3 and 5 predicted the highest BMI scores at each of six follow-up time points and the most rapid weight gain across over a nine-year period (Francis & Susman, 2009).
Developing a Family-Centered Pediatric Obesity Prevention Program
Despite the supporting evidence, there is a paucity of obesity prevention programs that focus on sustainable change mechanisms at the level of the family. Davison and colleagues (2012) provide a framework for developing, and potentially adapting, a family-centered program. Because of the strength of the empirical evidence demonstrating that existing parent training and family management programs alter critical family-level mechanisms that buffer against weight gain (i.e., PBS), we recommend systematic enhancement of the content and structure of these programs to potentially amplify the effects of the programs specifically for pediatric obesity prevention.
Due to their demonstrated effects on both PBS and obesity in population-based randomized trials, their efficacy across underserved, ethnic minority families, and their potential to be transported into to multiple service delivery systems that encounter large numbers of families (e.g., public schools, primary healthcare), we believe the FCU and ParentCorps are well positioned for enhancement for health behavior change, evaluation, and subsequent dissemination. Brief descriptions of the original ParentCorps and FCU programs are provided below to preface our discussion of enhanced content for obesity prevention. We describe the targeted populations of these prevention strategies consistent with the Institute of Medicine’s (1994) protractor model. Prevention programs are conceived and tested with specific populations based on risk. They are either universal (applied to broad populations), selective (given to subgroups at elevated risk), or indicated (highest risk subgroup; need for individualized intervention).
ParentCorps is a school-based universal prevention strategy specifically developed for socioeconomically and ethnically diverse families with young children (ages 3–6) living in urban settings. The curriculum comprises 14 weekly sessions (2 hours each) of group-based behavioral parent training (about 15 participants per group) aimed at promoting effective parenting and concurrent child sessions aimed at behavioral regulation skills and social competence. Teaching techniques in the parent groups (conducted by trained mental health professionals) include group discussions, role-plays, an animated video series, and a photo book of ParentCorps family stories and homework. Child groups are led by trained classroom staff and involve interactive lessons, experiential activities, and play. Additionally, school staff (teachers, teaching assistants, school leaders, support staff) are offered group and individual learning opportunities in the use of evidence-based practices for strengthening home-school connections and promoting children’s social, emotional, and behavioral regulation skills.
The FCU is a brief, selective/indicated prevention program based on parent management training for reducing problem behaviors, maternal depression, and problematic family interactions (e.g., coercive process, conflict) as well as promoting parental involvement and positive parenting. The FCU was designed to facilitate delivery in various service systems, including schools, community mental health, primary care, and as a home visiting program. Families with children age 2 to 17 who have family and child risk factors, such as socioeconomic disadvantage, maternal depression, academic failure, and child behavior problems, are eligible for the FCU. The intervention begins with an initial contact, ecological assessment, and feedback, which are completed in 2 or 3 one-hour sessions. For families that would benefit from additional support to improve parenting in the areas of positive behavior support, limit setting and monitoring, and relationship building, an individually tailored intervention follows. The duration of additional family support varies by family need and ranges from 1 to 15 support sessions with an average of 3 to 6 sessions. Specific intervention techniques include a 12-module parent training curriculum, psychoeducation, role-plays, and video feedback procedures. Facilitators with varying educational backgrounds and training in mental health (bachelor’s to doctoral) deliver the FCU.
Enhancements, which have been made to both programs (e.g., Dawson-McClure et al., 2014; Montaño, Smith, Chiapa, Miloh, & Dishion, 2014), include the addition of nutrition and physical activity content as well as addressing parenting and environmental barriers to these behaviors throughout the curriculums. Pilot testing of these enhanced versions has been done but there is not yet a rigorous evaluation. Below we outline (1) a plan for family-centered pediatric obesity prevention that targets PBS as it relates to lifestyle behavior change in addition to general child development and is based on the FCU and ParentCorps; (2) program components that impact PBS; (3) the assessment of outcomes to document efficacy and effectiveness; and (4) options for delivery. This outline was developed from the existing empirical literature in obesity prevention and family-centered prevention science and is intended to serve as a brief, evidence-based guide.
Theory of action
The foundation of an evidence-based prevention program is an empirically grounded theory of action. As outlined in Figure 1, increasing physical activity and improving dietary practices over time via PBS strategies reduces the likelihood of the child being classified as overweight or obese. Although not depicted visually, our model is embedded within a complex family system and social ecology. Specifically, although we focus on the protective role of PBS, we recognize that many factors influence parents’ ability to make use of these strategies, such as living in poverty and mental health issues.
Figure 1.
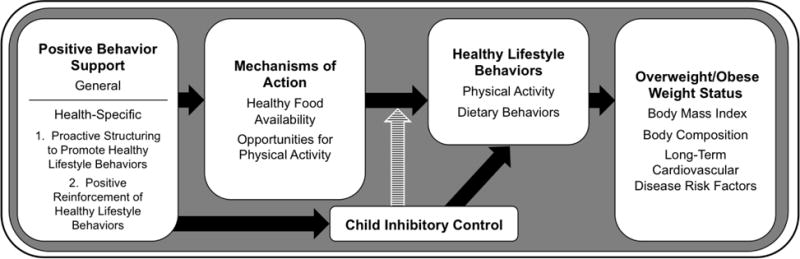
Pathway of a family-centered intervention strategy to prevent pediatric obesity
Two PBS skills specific to children’s healthy lifestyle behaviors are critical enhancements to the proposed approach to obesity prevention. First, parents learn to proactively structure the child’s environment to promote healthy lifestyle behaviors through anticipating the child’s needs and increasing facilitators of success. Specifically, PBS involves proactively serving healthy foods (e.g., fruits and vegetables) at mealtimes (Montaño, Smith, Dishion, Shaw, & Wilson, 2015), while limiting intake of calorically dense, high fat/sugar foods and ensuring the child’s schedule provides opportunities for physical activity through options such as after-school programs, outings to a neighborhood park, and active in-home activities (Kitzman-Ulrich et al., 2010). An example of proactive structuring is having vegetables on hand when the child requests a snack, as opposed to serving processed foods that are readily available through vending machines and in convenience stores. Second, parents are taught to actively and positively reinforce desired behaviors through verbal praise, incentives, and participating with the child in enjoyable physical activities.
Additionally, previous studies suggest that child inhibitory control may act as both a mediator and moderator of intervention effects. We place it as a mediating variable because of the evidence that family-centered preventive interventions improve young children’s inhibitory control by increasing PBS (Lunkenheimer et al., 2008) and as a moderator of the relationship between the mechanisms of action and healthy lifestyle behaviors because of evidence indicating that inhibitory control interacts with parenting in the development of child behavioral outcomes (e.g., Eisenberg et al., 2005).
Program components
There are currently many evidence-based parenting programs whose curricula include components and strategies to improve PBS or positive parenting. Although evidence shows that existing components effectively improve PBS, which in turn reduces obesity, we argue that enhancing curricula such that it impacts PBS broadly related to child development in addition to more specifically as it relates to child lifestyle behavior change may have the biggest impact on pediatric obesity. Previous research found that a PBS-based intervention for the prevention of cardiovascular health risk behaviors (e.g., cigarette smoking) in adolescents was more effective when general PBS was combined with PBS specific to health behavior, compared to a PBS for health behavior only intervention format (Prado et al., 2007). Thus, we provide examples focused on PBS in support of weight management that are intended to accompany efficacious general PBS parenting strategies for young children.
As previously noted, FCU and ParentCorps use a combination of strategies to improve PBS in general, including psycho-education, collaborative discussions between facilitators and parents, role-plays, and skills training practice in and between sessions. In the context of obesity prevention, PBS strategies can be introduced through didactic instruction by facilitators on topics such as enhancing the availability of healthy foods and building physical activity opportunities into the family schedule; video exemplars demonstrating appropriate use of PBS skills in various contexts but not limited to healthy lifestyle behaviors; and video feedback procedures involving parents and facilitators viewing brief segments of videotaped family interactions to draw parents’ attention to desired PBS skills and encouraging continued use or teaching more effective skills. Collaborative discussions involve problem solving current family issues with the facilitator providing solutions using a PBS framework. In-session role-play and practicing learned material in the home facilitate parent skill acquisition and provide an opportunity to build mastery. When targeting health behaviors, role-play prompts might include getting a picky eater to eat healthy foods, positive reinforcement of a child’s healthy dietary choices, or including a young child in age-appropriate meal preparation activities. Last, as with all family-centered prevention programs, process-based components would include facilitator strategies for engaging and retaining families, enhancing motivation for change, and taking a strengths-based, health promoting perspective.
The original FCU was revised from an intervention characterized by risk reduction to one of health promotion from a family management framework and a pilot feasibility trial was conducted in a weight management clinic within a children’s hospital (Montaño et al., 2014). Parent-reported questionnaire items concerning health behaviors and parent–child interaction tasks focused on healthy lifestyle behavior change goals and challenges (e.g., positive reinforcement of healthy dietary choices, setting limits on sedentary activity) were added to the FCU ecological assessment. The feedback session remained strengths-based and aimed at increasing parenting skills and motivation to change but with a focus on the role of parenting and family management skills in supporting healthy behaviors. The results of the pilot trial indicated appropriateness and acceptability for the adapted FCU program among the healthcare team and families and demonstrated feasible delivery in healthcare settings.
In adapting ParentCorps for obesity prevention, enhancements focus on building parents’ knowledge, belief, and skills for facilitating early childhood healthy lifestyle behaviors. For example, an animated DVD that shows caregivers engaging in daily interactions with their children (e.g., getting ready for school) may be expanded to include scenarios related to healthy lifestyle behaviors (e.g., family meals, playing outside). Because ParentCorps is group-based, discussions provide rich opportunities for caregivers to serve in the “expert” role, sharing successes and strategies for promoting child healthy lifestyle behaviors. An integral component of ParentCorps is the explicit discussion of the impact of culture on parenting practices. These discussions could be used to explore the role of culture and family values as they relate specifically to children’s weight and health. A recent pilot study of ParentCorps enhanced to incorporate child eating, activity and sleep with 91 families of pre-Kindergarten students in low-income urban communities demonstrated increases in child nutrition knowledge and physical activity and decreases in child television viewing (Dawson-McClure et al., 2014).
Outcome assessment
Child weigh status (BMI for child age and gender), the primary outcome of interest, is easy to assess objectively using height and weight measurements, sensitive to change through behavioral lifestyle interventions, and a risk indicator of serious health conditions. Body composition should also be considered as an outcome because changes in diet and physical activity are also often accompanied by healthy changes in the ratio of fat to lean muscle. This change results in metabolic improvement that buffers against cardiovascular disease later in development even in the absence of weight loss or reductions in BMI (Carnethon et al., 2003).
Measuring putative mediators is also important. PBS, child inhibitory control, physical activity, and dietary practices can all be assessed via parent report. Methods that are less prone to reporter bias would increase precision and predictive validity but can be more costly and challenging to obtain. These include observational assessments of parenting skills and child inhibitory control and electronic sensors (i.e., accelerometers) to measure physical activity. Family-centered preventive interventions often demonstrate long-term effects, mediated by family processes that might not be evident in the short term (Sandler et al., 2015). Thus, it will be important to plan to evaluate the long-term effects by measuring the outcomes and proposed mediators at multiple time points and conducting meditational analyses. Consistent with recent meta-analyses reporting the effects of obesity prevention programs that include parents (Janicke et al., 2014; Niemeier et al., 2012; Seo & Sa, 2010), we expect the family-centered obesity prevention program we describe here will have modest effects on child BMI in the range of a Cohen’s d of .25 to .35 with a high likelihood of maintaining a meaningful effect over time.
Program delivery
Achieving a population-level impact requires prevention strategies to fit within a variety of cultural frameworks and delivered using cost-effective strategies that effectively reach, engage, and retain families, particularly ethnic minorities, across service systems (e.g., primary care, public schools, faith-based organizations). No single delivery strategy can reach all families in need. In order to achieve the greatest impact, we suggest these prevention strategies be delivered as part of a multi-tiered system of care, in multiple service delivery systems, and aligned with the Institute of Medicine’s (1994) protractor model. Previous trials of ParentCorps, a universal program, delivered the program in diverse urban elementary schools (Brotman et al., 2012), and similar group-based programs have been embedded in various settings (see Sandler et al., 2015) indicating the viability of this type of program delivery strategy.
Some families, however, will require a higher level of care. For those families, the FCU, a selective/indicated program, can be delivered in the school or the family’s home. Placement into FCU can occur in either of two ways: (1) from the outset based on elevated risk when first identified; (2) through an adaptive approach based on failure to implement behavior change recommendations and/or benefit clinically from the universal intervention (Collins, Murphy, & Bierman, 2004). Complementary use of ParentCorps and FCU is increasingly relevant in settings that cannot sustain a group-based program for various reasons. Relatedly some families will prefer a one-to-one clinician-caregiver(s) model as opposed to a group-based program. It is important to note that ParentCorps and FCU have commendable rates of participation among families with young children (Brotman et al., 2012; Smith et al., under review).
For both programs, effects have been demonstrated to be equivalent across ethnic minority families (Brotman et al., 2012; Smith, Knoble, Zerr, Dishion, & Stormshak, 2014) and effective for families of varying socioeconomic status. Although parenting groups in general and the FCU have been evaluated and shown to be effective when embedded in most social service delivery systems, including community mental health agencies, public schools, and home visitation, the FCU program is arguably the most well-suited for delivery in primary healthcare settings (Asarnow & Landsverk, 2015) because it is individually tailored to the specific needs of each family, making it briefer than comparable group-based parent training programs–approximately 3–6 hours of contact between the provider and families with young children.
To be effectively delivered in primary healthcare, however, the integration of technology (eHealth, mHealth, and other behavioral intervention technologies) to assist in the dissemination of intervention content should be considered (Prado, Pantin, & Estrada, 2015). This is crucial for scale out in general as it decreases implementation costs and increases access for families traditionally underserved by behavioral health providers (ethnic minority and families in rural areas). Given that internet access and mobile phone ownership are nearly equal for all families across many subgroups (Lopez, Gonzalez-Barrera, Patten, & Pew Hispanic Center, 2013) technology-assisted delivery mechanisms are a promising next step. Comprehensive cost data (cost savings and benefit–cost) are currently not available for these programs and the various delivery options, particularly for obesity prevention, which signals an area for future evaluation.
Concluding Remarks
If behavioral science hopes to combat the national and global obesity epidemic, effective preventive interventions must be clinically effective and feasible for widespread implementation and uptake. There is concurrent pressing need to evaluate this obesity prevention program in the manner we proposed and for rapid translation. Programs that improve parent’s use of PBS skills in general, and more specifically to proactively structure the environment and reinforce healthy lifestyle behaviors, have the potential to impact the obesity epidemic across ethnically and sociodemographically diverse populations of young children. Because family-centered preventive interventions, including the FCU and ParentCorps, have documented protective effects on children’s weight gain over time, integrating the family-centered prevention literature with well-established lifestyle behavior targets can usher in a more effective and advanced approach to obesity prevention in early childhood than is currently available.
Acknowledgments
Justin D. Smith was supported by National Institute on Drug Abuse grant DA027828, awarded to C. Hendricks Brown. Guillermo Prado was supported by National Institute on Minority Health and Health Disparities grant R01 MD007724, awarded to Guillermo Prado and Sarah Messiah.
Contributor Information
Justin D. Smith, Northwestern University Feinberg School of Medicine
Sara M. St. George, University of Miami Miller School of Medicine
Guillermo Prado, University of Miami Miller School of Medicine.
References
- Anzman-Frasca S, Stifter CA, Birch LL. Temperament and childhood obesity risk: A review of the literature. Journal of Developmental & Behavioral Pediatrics. 2012;33(9):732–745. doi: 10.1097/DBP.0b013e31826a119f. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Landsverk JA. The research landscape for primary care and children’s behavioral health. Paper presented at the IOM/NRC Forum: Opportunities to promote children’s behavioral health: Health care reform and beyond; Washington, DC. 2015. [Google Scholar]
- Brotman LM, Dawson-McClure S, Huang KY, Theise R, Kamboukos D, Wang J, Ogedegbe G. Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics. 2012;129(3):e621–e628. doi: 10.1542/peds.2011-1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290(23):3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prevention Science. 2004;5:185–196. doi: 10.1023/B:PREV.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison KK, Lawson HA, Coatsworth JD. The family-centered action model of intervention layout and implementation (FAMILI) the example of childhood obesity. Health promotion practice. 2012;13(4):454–461. doi: 10.1177/1524839910377966. [DOI] [PubMed] [Google Scholar]
- Dawson-McClure S, Brotman LM, Theise R, Palamar JJ, Kamboukos D, Barajas RG, Calzada EJ. Early childhood obesity prevention in low-income, urban communities. Journal of Prevention & Intervention in the Community. 2014;42(2):152–166. doi: 10.1080/10852352.2014.881194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denzer C, Reithofer E, Wabitsch M, Widhalm K. The outcome of childhood obesity management depends highly upon patient compliance. European Journal of Pediatrics. 2004;163(2):99–104. doi: 10.1007/s00431-003-1376-7. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Shaw DS, Connell A, Gardner FEM, Weaver C, Wilson M. The Family Check-Up with high-risk indigent families: Preventing problem behavior by increasing parents’ positive behavior support in early childhood. Child Development. 2008;79(5):1395–1414. doi: 10.1111/j.1467-8624.2008.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Centers for Disease Control and Prevention Youth risk behavior surveillance - United States, 2011. Morbidity and mortality weekly report. Surveillance summaries (Washington, DC: 2002) 2012;61(4):1–162. [PubMed] [Google Scholar]
- Eisenberg N, Zhou Q, Spinrad TL, Valiente C, Fabes RA, Liew J. Relations among positive parenting, children’s effortful control, and externalizing problems: A three-wave longitudinal study. Child Development. 2005;76(5):1055–1071. doi: 10.1111/j.1467-8624.2005.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, Van Horn L, Appel LJ, Burke LE, Carson JAS, Franch HA, Wylie-Rosett J. Evaluating parents and adult caregivers as “agents of change” for treating obese children: Evidence for parent behavior change strategies and research gaps: a scientific statement from the American Heart Association. Circulation. 2012;125(9):1186–1207. doi: 10.1161/CIR.0b013e31824607ee. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Jones BL. Food and family: A socio-ecological perspective for child development. Advances in child development and behavior. 2012;42:307–337. doi: 10.1016/B978-0-12-394388-0.00009-5. [DOI] [PubMed] [Google Scholar]
- Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Archives of Pediatrics & Adolescent Medicine. 2009;163(4):297–302. doi: 10.1001/archpediatrics.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner FEM, Burton J, Klimes I. Randomised controlled trial of a parenting intervention in the voluntary sector for reducing child conduct problems: Outcomes and mechanisms of change. Journal of Child Psychology and Psychiatry. 2006;47(11):1123–1132. doi: 10.1111/j.1469-7610.2006.01668.x. [DOI] [PubMed] [Google Scholar]
- Goodman E, Dolan LM, Morrison JA, Daniels SR. Factor analysis of clustered cardiovascular risks in adolescence: Obesity is the predominant correlate of risk among youth. Circulation. 2005;111(15):1970–1977. doi: 10.1161/01.cir.0000161957.34198.2b. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Reducing risks for mental disorders: Frontiers for preventive intervention research. Washington, DC: National Academy Press; 1994. [PubMed] [Google Scholar]
- Janicke DM, Steele RG, Gayes LA, Lim CS, Clifford LM, Schneider EM, Westen S. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology. 2014 doi: 10.1093/jpepsy/jsu023. [DOI] [PubMed] [Google Scholar]
- Kitzman-Ulrich H, Wilson D, George S, Lawman H, Segal M, Fairchild A. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clinical Child and Family Psychology Review. 2010;13(3):231–253. doi: 10.1007/s10567-010-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolagotla L, Adams W. Ambulatory management of childhood obesity. Obesity Research. 2004;12(2):275–283. doi: 10.1038/oby.2004.35. [DOI] [PubMed] [Google Scholar]
- Krebs NF, Jacobson MS, American Academy of Pediatrics Committee on Nutrition Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- Lopez MH, Gonzalez-Barrera A, Patten E, Pew Hispanic Center . Closing the digital divide: Latinos and technology adoption. Pew Hispanic Center; Washington, DC: 2013. [Google Scholar]
- Lunkenheimer ES, Dishion TJ, Shaw DS, Connell AM, Gardner FEM, Wilson MN, Skuban EM. Collateral benefits of the Family Check-Up on early childhood school readiness: Indirect effects of parents’ positive behavior support. Developmental Psychology. 2008;44(6):1737–1752. doi: 10.1037/a0013858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics. 2012;129(6):1035–1041. doi: 10.1542/peds.2011-1082. [DOI] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, Seeman TE. Pathways to resilience: Maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychological Science. 2011;22(12):1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaño Z, Smith JD, Chiapa A, Miloh T, Dishion TJ. Adaptation and implementation of the Family Check-Up for the treatment of pediatric obesity within a primary care setting. Paper presented at the the annual meeting of the Society for Prevention Research; Washington, DC. 2014. [Google Scholar]
- Montaño Z, Smith JD, Dishion TJ, Shaw DS, Wilson MN. Longitudinal relations between observed parenting behaviors and dietary quality of meals from ages 2 to 5. Appetite. 2015;87(0):324–329. doi: 10.1016/j.appet.2014.12.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader PR, O’Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, Susman EJ. Identifying risk for obesity in early childhood. Pediatrics. 2006;118(3):e594–e601. doi: 10.1542/peds.2005-2801. [DOI] [PubMed] [Google Scholar]
- National Research Council and Institute of Medicine. Early childhood obesity prevention policies. Washington, DC: The National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemeier BS, Hektner JM, Enger KB. Parent participation in weight-related health interventions for children and adolescents: A systematic review and meta-analysis. Preventive Medicine. 2012;55(1):3–13. doi: 10.1016/j.ypmed.2012.04.021. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power TG, Sleddens EFC, Berge J, Connell L, Govig B, Hennessy E, St George SM. Contemporary research on parenting: Conceptual, methodological, and translational issues. Childhood Obesity. 2013;9(s1):S87–S94. doi: 10.1089/chi.2013.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado G, Pantin H, Briones E, Schwartz SJ, Feaster D, Huang S, Szapocznik J. A randomized controlled trial of a parent-centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. Journal of Consulting & Clinical Psychology. 2007;75(6):914–926. doi: 10.1037/0022-006X.75.6.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prado G, Pantin H, Estrada Y. Integrating evidence-based interventions for adolescents into primary care. American Journal of Preventive Medicine. 2015;48(4):488–490. doi: 10.1016/j.amepre.2014.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Ingram A, Wolchik SA, Tein JY, Winslow EB. Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives. 2015;9(3):164–171. doi: 10.1111/cdep.12126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler IN, Schoenfelder EN, Wolchik SA, MacKinnon DP. Long-term impact of prevention programs to promote effective parenting: Lasting effects but uncertain processes. Annual Review of Psychology. 2011;62:299–329. doi: 10.1146/annurev.psych.121208.131619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo DC, Sa J. A meta-analysis of obesity interventions among U.S. minority children. Journal of Adolescent Health. 2010;46(4):309–323. doi: 10.1016/j.jadohealth.2009.11.202. [DOI] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Hails KA, Dishion TJ, Shaw DS, Wilson MN. Family participation in an eight-year-long trial of the Family Check-Up program delivered via a health maintenance approach. Prevention Science. under review. Special Issue. [Google Scholar]
- Smith JD, Knoble N, Zerr AA, Dishion TJ, Stormshak EA. Multicultural competence and the Family Check-Up: Indirect effect on adolescent antisocial behavior through family conflict. Journal of Clinical Child & Adolescent Psychology. 2014;43(3):400–414. doi: 10.1080/15374416.2014.888670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Montaño Z, Dishion TJ, Shaw DS, Wilson MN. Preventing weight gain and obesity: Indirect effects of a family-based intervention in early childhood. Prevention Science. 2015;16(3):408–419. doi: 10.1007/s11121-014-0505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung-Chan P, Sung YW, Zhao X, Brownson RC. Family-based models for childhood-obesity intervention: A systematic review of randomized controlled trials. Obesity Reviews. 2013;14(4):265–278. doi: 10.1111/obr.12000. [DOI] [PubMed] [Google Scholar]


