Abstract
Objective
We evaluated the effectiveness of short-term cash and food assistance to improve adherence to antiretroviral therapy (ART) and retention in care among people living with HIV (PLHIV) in Tanzania.
Methods
At three clinics, 805 participants were randomized to three groups in a 3:3:1 ratio, stratified by site: nutrition assessment and counseling (NAC) plus cash transfers (~$11/month, n=347), NAC plus food baskets (n=345), and NAC-only (comparison group, n=113, clinicaltrials.gov NCT01957917). Eligible PLHIV were: ≥18 years, initiated ART ≤90 days prior, and food insecure. Cash or food was provided for ≤6 consecutive months, conditional on visit attendance. The primary outcome was medication possession ratio (MPR) ≥95% at 6 months. Secondary outcomes were appointment attendance and loss to follow-up (LTFU) at 6 and 12 months.
Results
The primary intent-to-treat analysis included 800 participants. Achievement of MPR≥95% at 6 months was higher in the NAC+cash group compared to NAC-only (85.0% vs. 63.4%), a 21.6 percentage point difference (95% confidence interval (CI): 9.8, 33.4, p<0.01). MPR≥95% was also significantly higher in the NAC+food group versus NAC-only (difference=15.8, 95% CI: 3.8, 27.9, p<0.01). When directly compared, MPR≥95% was similar in the NAC+cash and NAC+food groups (difference=5.7, 95% CI: −1.2, 12.7, p=0.15). Compared to NAC-only, appointment attendance and LTFU were significantly higher in both the NAC+cash and NAC+food groups at 6 months. At 12 months, the effect of NAC+cash, but not NAC+food, on MPR≥95% and retention was sustained.
Conclusions
Short-term conditional cash and food assistance improves ART possession and appointment attendance and reduces LTFU among food-insecure ART initiates in Tanzania.
Keywords: Food security, HIV infection, adherence, retention, impact evaluation, cash transfers, food assistance
INTRODUCTION
Although early initiation of antiretroviral therapy (ART) among people living with HIV/AIDS (PLHIV) has significant clinical benefits and can virtually eliminate onward HIV transmission,[1, 2] these benefits hinge on high levels of ART adherence. Most treatment regimens require more than 80–95% ART adherence to maximize the probability of viral suppression,[3–6] the ultimate goal of HIV treatment.[2, 7] However, in sub-Saharan Africa (SSA) nearly 25% of PLHIV on treatment have sub-optimal adherence and overall, only 29% of PLHIV are virally suppressed.[8, 9] Thus, achievement of UNAIDS’ ambitious ’90-90-90’ strategy, which requires that by 2020, 90% of PLHIV who receive ART will have viral suppression, necessitates new and effective strategies to bolster ART adherence and retention in care.
In SSA, poor ART adherence and disengagement from care are often the detrimental consequences food insecurity.[10, 11] People are considered food secure when they have adequate physical, social, and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life.[12] Food insecurity hinders HIV treatment by increasing the likelihood of hunger or exacerbated side effects associated with ART, by increasing anxiety and stress, and by forcing PLHIV to make difficult choices between food and other goods and services, including HIV care.[11, 13] Thus, there is growing interest in the potential for food and economic programs to mitigate food insecurity, improve the health of PLHIV, and enhance the effectiveness of HIV treatment programs.
Interventions in the form of food baskets or cash transfers have the potential to achieve these goals. For example, four[14–17] of five studies of programs that provided food baskets or nutritional supplementation to PLHIV found positive effects on at least one measure of treatment adherence.[14–18] Likewise, cash incentives can also improve ART adherence and/or viral suppression compared to the standard of care.[19–22] Cash transfers are particularly attractive because they give beneficiaries freedom of choice, they may be cheaper to distribute and easier to monitor, and because their increasing adoption by anti-poverty programs across SSA may signal political and logistical readiness for cash transfer programs delivered at scale.[23, 24]
Despite these promising results, there are limited rigorous data from low- and middle-income countries about whether cash and food assistance programs for PLHIV are effective for improving adherence or retention.[25] To address this gap, we compared the standard of care to two models of short-term support for food insecure PLHIV in Tanzania who recently initiated treatment: cash transfers and food assistance. All three groups received nutrition assessment and counseling (NAC). We focused on ART initiates for several reasons including the increased risk of mortality associated with a low BMI in the first years of treatment,[26–28] the potential to accelerate habit formation,[29] and the goal to bolster household labor supply and productivity during the vulnerable time of treatment initiation.[30] The study’s objective was to examine the comparative effectiveness of cash and food assistance on ART adherence and retention in care at 6 and 12 months.
METHODS
Study Design
We conducted a 3-arm randomized trial to examine the comparative effectiveness of short-term cash and food assistance added to the standard of care HIV services that included NAC. We recruited participants from three facilities (two hospitals and one peri-urban clinic) in Shinyanga, a resource-limited region in Tanzania where HIV prevalence is 7.4%.[31] Participants were prospectively followed for 12 months. All facilities were implementing the President’s Emergency Plan for AIDS Relief Nutrition Assessment, Counseling, and Support (NACS) program.[32] Study procedures have been previously described,[33] the trial was pre-registered (clinicaltrials.org, NCT01957917), and here we report the study according to the CONSORT 2010 guidelines.[33, 34] The Tanzanian National Institute for Medical Research and the Committee for Protection of Human Subjects at the University of California, Berkeley approved this study.
Participants
Eligible PLHIV were: 1) ≥18 years of age; 2) newly initiated on ART ≤90 days prior; 3) food insecure, as measured with the Household Hunger Scale (HHS, score ≥2)[35]; and 4) willing and able to provide written informed consent. During the first two months of the study, PLHIV who were moderately (body mass index (BMI) 16–18.5 kg/m2) or severely malnourished (BMI<16 kg/m2) were excluded due to their need to receive special nutritional and clinical support for recovery. However, given the frequency of moderate malnutrition among ART initiates and the lack of any special nutritional or clinical services for this group at study sites, we determined that moderately malnourished patients would be eligible for inclusion.
Randomization and Masking
Participants were individually randomized to one of three study arms: NAC alone (standard-of-care comparison condition), NAC plus cash transfers, and NAC plus food assistance in a 1:3:3 ratio, stratified by site, using random permuted block sizes of 7, 14, and 21. Randomization procedures were conducted at the University of California, Berkeley using Stata 12 (College Station, Texas); procedures and group assignments were inaccessible to the local research team. Random assignments were listed in opaque sealed envelopes that were sequentially numbered. After written informed consent was obtained, research staff selected the next envelope in numeric order and broke the seal to reveal the group assignment. Participants and investigators were not masked.
Procedures
Participants in the comparison arm received the standard HIV primary care services available in Tanzania, including NAC. Participants in the cash and food arms received the standard of care services plus the opportunity to receive a monthly cash transfer or food basket for up to 6 consecutive months, conditional on attending scheduled visits with the HIV care provider (typically monthly). Visits meeting the condition for assistance were ≥26 days apart and occurred within a 4-day window (+/− 4 days) from the scheduled visit. Food baskets and cash transfers were distributed on the same two days per month.
The cash transfer was 22,500 Tanzanian Shillings (approximately $11 USD, $66 maximum during the intervention period) and was equivalently valued to the food basket. This value was selected to prevent undue coercion and be comparable to the Tanzania Social Action Fund (TASAF), a government-run anti-poverty program which provides $6–18 monthly to qualified households.[36] Cash, including transaction fees, was transferred via mobile money services (i.e., M-PESA). If participants did not have access to a mobile phone, cash was provided directly.
The food basket was valued at approximately $11 and included whole maize meal (12 kg), groundnuts (3kg), and beans (3kg), and was determined with the input of experts in academic, government, and donor organizations. The basket was intended to be applicable to other settings, not cost-prohibitive, be similar to prior programs, and use locally available food. Because the goal was to supplement, but not replace, the household’s food supply, the food basket was significantly smaller than food baskets evaluated in other studies to improve ART adherence.[14–18]
At baseline, 6, and 12 months, research assistants conducted in-person interviews in Kiswahili with participants about individual and household characteristics, food security, self-reported ART adherence, health service utilization, and preference for food or cash if given the choice. Visit attendance, CD4 count, pharmacy dispensing, and other clinical and prognostic markers were abstracted from medical and pharmacy records at baseline, 6 and 12 months.
Outcomes
The primary outcome was ART adherence at 6 months, measured as the proportion of patients with medication possession ratio ≥95% during the 0–6 month interval (MPR≥95%). MPR is the proportion of days in a specified interval that an individual is in possession of ≥1 ART dose.[37] MPR is computed from pharmacy dispensing records and achievement of ≥95% MPR is associated with short-term virologic outcomes.[37, 38] When patients transferred, opted-out of future study participation, or died, we truncated the 0–6 month interval to the last visit date.
We included several secondary outcomes. We assessed MPR≥95% at 12 months. In addition, because adherence thresholds between 80%–95% may be correlated with viral suppression,[4, 5, 37] we assessed secondary outcomes of MPR≥80% (binary) and MPR (continuous scale) for the 0–6 and 0–12 month intervals. We also assessed retention in care at 6 and 12 months in two ways. We first determined “appointment attendance,” the proportion of scheduled visits completed during the 0–6 and 0–12 month observation periods.[39] We also determined loss to follow-up (LTFU), defined as ≥90 days since the last scheduled visit.[40, 41] Patients who transferred clinics or opted-out of future participation were excluded from denominator of the LTFU indicator but those who died were retained in the denominator, similar to PEPFAR indicators.[42]
Statistical Analysis
The target sample size was determined using a non-inferiority design to compare the effectiveness of cash transfers versus food assistance on MPR≥95% at 6 months.[33] We estimated that 75% of participants in the food group would have an MPR≥95%,[9, 43, 44] and we set a non-inferiority limit (Δ) of 10 percentage points for the cash group to be determined non-inferior. The non-inferiority margin was determined as the largest loss of effect (inferiority) that would be clinically acceptable when comparing cash transfers to food baskets.[45] With these assumptions, power=80% and alpha=0.025 for a one-sided hypothesis test, 339 participants were required in each of the cash and food transfer arms, assuming 15% loss to follow-up. A secondary objective was to determine whether any assistance (NAC plus food or cash transfers, combined) was superior to NAC alone. For this objective, we required a comparison group of 110 participants to detect at least a 15 percentage point increase in MPR≥95%, assuming 60% of participants achieve MPR ≥95% in the NAC-only comparison arm, 15% loss to follow-up, and alpha=0.05. This was determined to be a clinically meaningful minimum detectable effect size and feasible to measure given study constraints.
We first assessed baseline differences in participant characteristics between arms using chi-square and Kruskal-Wallis tests. We then conducted an intent-to-treat (ITT) analysis by constructing a logistic regression model and expressing differences in the primary outcome between arms as risk differences with 95% confidence intervals (CI) using the margins command in STATA 14 (College Station, Texas). Following our pre-specified analysis plan,[33] we first assessed whether NAC plus cash transfers was non-inferior to NAC plus food assistance, defined as the lower 95% CI of the between-group difference in MPR≥95% lying above a threshold of −10% after applying Bonferroni’s correction for multiple comparisons.[46, 47] Because non-inferiority was evident, we conducted pairwise comparisons of the three groups using a Wald test with alpha = 0.05 and Bonferroni’s correction, using the pwcompare command in STATA.
We conducted several secondary analyses. These included an analysis of the primary outcome adjusted for site and factors imbalanced at baseline, and an analysis of results by quarter. We examined the effect of the intervention on secondary outcomes, including MPR≥80% and MPR at 6 and 12 months, MPR≥95% at 12 months, and appointment attendance and loss to follow-up at 6 and 12 months, by generating risk differences and 95% CIs from logistic and OLS regression models as appropriate. In addition, the effect of the interventions on the time to LTFU (the time between study enrollment and the last scheduled visit) was examined with a Kaplan-Meier plot; equality of survival functions was tested using the log-rank test. The effect of the interventions on the time to LTFU was examined using a Cox proportional hazards model with an interaction between study arm and categorical time at 3 and 6 months to relax the proportional hazards assumption. We present hazard ratios (HR) for each time interval and 95% CIs.
RESULTS
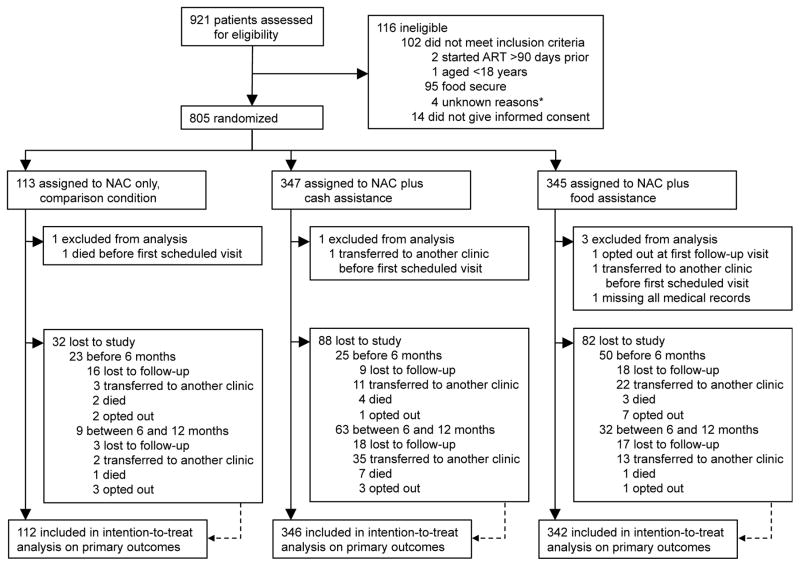
Recruitment and enrollment was conducted from December 2, 2013 until July 22, 2015. Follow-up continued until August 17, 2016 (Figure 1). We recruited and randomized 805 participants (805 of 819 (98%) eligible patients agreed to participate). Five patients transferred, died, opted out before their next scheduled visit (i.e., no follow-up time), or had no medical records and were subsequently excluded, leaving 800 participants for the primary ITT analysis at 6 months.
FIGURE 1.
Study profile.
*4 screened patients were excluded for an unknown reason (e.g., missing screening data)
At enrollment, 63% of participants were female, the median age was 35 years, median CD4 count was 200 cells/mm3, and median body mass index was 21.0 kg/m2 (Table 1). Participant characteristics were balanced between groups with the exception of occupation, language, and WHO clinical stage. During the study period, we distributed 1,794 cash transfers and 1,467 food baskets with no adverse events. When asked about their preferences at 6 months, most intervention participants preferred cash (65%), regardless of study arm.
TABLE 1.
Baseline sociodemographic and clinical characteristics of the intention-to-treat population.a
| Overall (n=800) | Study Group |
|||
|---|---|---|---|---|
| NAC only (n=112) | NAC + Cash (n=346) | NAC + Food (n=342) | ||
| Sociodemographic Characteristics | ||||
|
| ||||
| Age (years) | 35 (29–43) | 33 (28–40) | 35 (30–42) | 35 (29–44) |
| Sex | ||||
| Male | 291 (36%) | 39 (35%) | 128 (37%) | 124 (36%) |
| Female | 509 (64%) | 73 (65%) | 218 (63%) | 218 (64%) |
| Language | ||||
| Swahili | 489 (61%) | 80 (71%) | 205 (59%) | 204 (60%) |
| Sukuma/other | 311 (39%) | 32 (29%) | 141 (41%) | 138 (40%) |
| Education (highest) | ||||
| Some pre-/primary school | 121 (15%) | 16 (14%) | 57 (16%) | 48 (14%) |
| Primary school | 437 (55%) | 61 (54%) | 191 (55%) | 185 (54%) |
| Secondary school or more | 48 (6%) | 12 (11%) | 14 (4%) | 22 (6%) |
| No formal education | 194 (24%) | 23 (21%) | 84 (24%) | 87 (25%) |
| Married/partnership | 345 (43%) | 49 (44%) | 150 (43%) | 146 (43%) |
| Occupation | ||||
| Farmer | 405 (51%) | 47 (42%) | 192 (55%) | 166 (49%) |
| Business | 105 (13%) | 25 (22%) | 36 (10%) | 44 (13%) |
| Other | 181 (23%) | 27 (24%) | 73 (21%) | 81 (24%) |
| Unemployed | 109 (14%) | 13 (12%) | 45 (13%) | 51 (15%) |
| Currently working | 462 (58%) | 72 (64%) | 199 (58%) | 191 (56%) |
| Head of household | 489 (61%) | 68 (61%) | 207 (60%) | 214 (63%) |
| Household size | 3 (2–5) | 3 (2–5) | 3 (2–5) | 3 (2–5) |
| Severe household hungerb | 328 (41%) | 41 (37%) | 141 (41%) | 146 (43%) |
| Travel time to clinic (minutes) | 30 (20–60) | 30 (20–60) | 30 (20–60) | 30 (20–60) |
| Asset index | ||||
| 1 | 200 (25%) | 23 (21%) | 87 (25%) | 90 (26%) |
| 2 | 200 (25%) | 28 (25%) | 90 (26%) | 82 (24%) |
| 3 | 200 (25%) | 29 (26%) | 92 (27%) | 79 (23%) |
| 4 | 200 (25%) | 32 (29%) | 77 (22%) | 91 (27%) |
|
| ||||
| Clinical Characteristics | ||||
|
| ||||
| Body-mass index (kg/m2) | 21.0 (19.1–23.0) | 21.1 (19.8–23.3) | 20.7 (19.1–22.5) | 21.2 (19.1–23.4) |
| Weight (kg) | 56 (50–61) | 58 (50–64) | 55 (50–60) | 56 (50–62) |
| Days since ART started | 14 (12–44) | 14 (0–44) | 14 (12–44) | 14 (14–44) |
| CD4 cell count (cells per μL) | 200 (101–299) | 188 (97–319) | 192 (92–296) | 214 (105–297) |
| WHO clinical stage | ||||
| Stage 1 | 113 (14%) | 14 (13%) | 40 (12%) | 59 (17%) |
| Stage 2 | 230 (29%) | 41 (37%) | 88 (26%) | 101 (30%) |
| Stage 3 | 409 (51%) | 46 (41%) | 195 (57%) | 168 (49%) |
| Stage 4 | 44 (6%) | 10 (9%) | 20 (6%) | 14 (4%) |
| Pregnant | 23 (3%) | 1 (1%) | 12 (3%) | 10 (3%) |
Data are median (IQR) or n (%). NAC=nutrition assessment and counseling.
Number of patients missing data for included variables: CD4 cell count: n=163, Body-mass index: n=28. All other variables have fewer than 10 values missing (<2%).
According to the Household Hunger Scale.
Per our pre-specified analysis plan, at 6 months NAC+cash was non-inferior to NAC+food on the primary outcome of MPR≥95% (unadjusted difference=5.7, 95% CI: −1.2, 12.7, Table 2). In addition, participants in the pooled group of NAC+cash and NAC+food achieved significantly better MPR≥95% compared to the NAC-only group at 6 months (unadjusted difference=18.7, 95% CI: 9.4, 28.1, p<0.01). When disaggregated, the NAC+cash group attained significantly higher adherence than the comparison group on all indicators at 6 months, including MPR≥95%, MPR≥80%, and MPR in both the ITT and adjusted analyses. In particular, MPR≥95% was achieved by 85.0% of patients in the NAC+cash group compared to 63.4% in the NAC-only group, a 21.6 percentage point difference in unadjusted analyses (95% confidence interval (CI): 9.8, 33.4, p<0.01). In the NAC+food group, MPR≥95% and MPR were significantly greater (79.2%, 92.9%, respectively) than the comparison group (63.4%, 85.4%, respectively) at 6 months in both the ITT and adjusted analysis, although the effect on MPR≥80% was only significant in adjusted analyses (87.7% vs. 79.5%, adjusted difference=9.4, 95% CI: 0.1, 18.8, p<0.05). When directly compared, NAC+cash was statistically similar to NAC+food at improving 6-month MPR≥95% and MPR, although in both ITT and adjusted analyses MPR≥80% was significantly higher in the NAC+cash group (adjusted difference=5.8, 95% CI: 0.8, 10.8, p=0.02).
TABLE 2.
Summary of the effect of nutrition assessment and counseling (NAC) plus cash or food transfers on ART adherence and retention in care.
| Outcome | Overall | Study group |
Between-group differencea (%
[95% CI]) |
Adjusted between-group
differenceb (%
[95% CI]) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| NAC only | NAC + Cash | NAC + Food | NAC + Cash vs. NAC only | NAC + Food vs. NAC only | NAC + Cash vs. NAC + Food | NAC + Cash vs. NAC only | NAC + Food vs. NAC only | NAC + Cash vs. NAC + Food | ||
| Adherence to ART | ||||||||||
|
| ||||||||||
| 6 months | ||||||||||
| MPR≥95%c | 79.5% | 63.4% | 85.0% | 79.2% | 21.6 (9.8, 33.4)** | 15.8 (3.8, 27.9)** | 5.7 (−1.2, 12.7) | 23.5 (12.2, 34.7)** | 17 (5.5, 28.5)** | 6.4 (−0.1, 13.0) |
| MPR≥80%d | 88.9% | 79.5% | 93.1% | 87.7% | 13.6 (3.9, 23.3)** | 8.3 (−1.8, 18.3) | 5.3 (0, 10.7)* | 15.2 (6.2, 24.3)** | 9.4 (0.1, 18.8)* | 5.8 (0.8, 10.8)* |
| MPRe | 92.8% | 85.4% | 95.1% | 92.9% | 9.7 (5.6, 13.8)** | 7.5 (3.4, 11.6)** | 2.2 (−0.7, 5.1) | 10.5 (6.5, 14.4)** | 8.0 (4.1, 11.9)** | 2.5 (−0.3, 5.2) |
| 12 months | ||||||||||
| MPR≥95% | 67.5% | 55.4% | 74.9% | 64.0% | 19.5 (6.9, 32.1)** | 8.7 (−4.2, 21.5) | 10.8 (2.5, 19.2)** | 20.3 (8.4, 32.2)** | 9.5 (−2.6, 21.7) | 10.8 (3.0, 18.6)** |
| MPR≥80% | 85.8% | 81.3% | 89.3% | 83.6% | 8.1 (−1.6, 17.7) | 2.4 (−7.7, 38.1) | 5.7 (−0.5, 11.9) | 8.5 (−1.0, 18.0) | 2.5 (−7.3, 38.4) | 5.9 (−0.1, 12.0) |
| MPR | 90.1% | 83.3% | 93.0% | 89.5% | 9.7 (4.9, 14.5)** | 6.2 (1.4, 11.0)** | 3.5 (0.2, 6.8)* | 10.3 (5.6, 15)** | 6.6 (1.9, 11.3)** | 3.7 (0.5, 7.0)* |
|
| ||||||||||
| Retention in care | ||||||||||
|
| ||||||||||
| 6 months | ||||||||||
| Appointment attendancef | 93.5% | 82.6% | 96.1% | 94.5% | 13.5 (9.1, 17.8)** | 11.8 (7.5, 16.2)** | 1.7 (−1.4, 4.7) | 13.9 (9.5, 18.3)** | 12.2 (7.8, 16.6)** | 1.8 (−1.3, 4.8) |
| Lost to follow-up at 6 monthsg | 2.6% | 10.9% | 0.9% | 1.5% | −10.0 (−17.3, −2.8)** | −9.4 (−16.7, −2.1)** | −0.7 (−2.7, 1.4) | −10.3 (−17.7, −3.0)** | −9.6 (−17.0, −2.1)** | −0.8 (−2.8, 1.3) |
| 12 months | ||||||||||
| Appointment attendance | 92.1% | 83.4% | 94.7% | 92.3% | 11.3 (7.2, 15.5)** | 8.9 (4.7, 13.1)** | 2.4 (−0.5, 5.3) | 11.8 (7.6, 16.0)** | 9.2 (5.1, 13.4)** | 2.6 (−0.4, 5.5) |
| Lost to follow-up at 12 months | 9.5% | 17.3% | 6.7% | 9.7% | −10.6 (−20.1, −1.1)* | −7.6 (−17.4, 2.1) | −3.0 (−8.3, 2.3) | −11.9 (−21.7, −2.0)* | −8.5 (−18.6, 1.7) | −3.4 (−8.7, 1.9) |
ART=antiretroviral therapy; MPR=medication possession ratio; CI=confidence interval; LTFU=loss to follow-up
p<0.05
p<0.01
Unadjusted intent-to-treat estimate using Bonferroni’s adjustment for multiple comparisons.
Adjusted for site and for baseline imbalances including WHO clinical stage, occupation, and language.
The proportion of patients with MPR ≥95% during the 0–6 month interval.
The proportion of patients with MPR ≥80% during the 0–6 month interval.
The proportion of time an individual is in possession of ≥ 1 ART dose or prescription for ART.
The proportion of scheduled visits completed during the 0–6 month observation period.
The proportion of patients with no evidence of HIV primary care at 6 months, defined not seen for at least 90 days since the last appointment scheduled prior to 6 months.
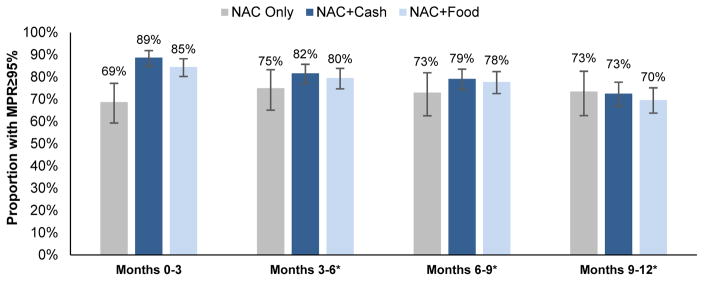
At 12 months, MPR≥95% was significantly greater among those in the NAC+cash group than the NAC-only group (74.9% vs. 55.4%, adjusted difference=20.3, 95% CI: 8.4, 32.2, p<0.01, Table 2). Furthermore, compared to the NAC-only group, MPR remained significantly higher in the NAC+cash group (93.0% vs. 83.3%, p<0.01) and in the NAC+food group (89.5% vs. 83.3%, p<0.01) in both ITT and adjusted analyses. Neither intervention significantly improved MPR≥80% at 12 months. When directly compared, NAC+cash was significantly more effective than NAC+food at improving both 12 month MPR≥95% (adjusted difference=10.8, 95% CI: 3.0, 18.6, p<0.01) and MPR (adjusted difference=3.7, 95% CI: 0.5, 7.0, p<0.05). When observed in 3-month intervals, MPR≥95% was higher in the cash and food groups only during the initial 3 months of the intervention period (Figure 2).
FIGURE 2.
Effect of nutrition assessment and counseling (NAC) plus cash or food transfers on ART adherence (MPR≥95%), by quarter.
MPR=medication possession ratio, NAC=nutrition assessment and counseling
*Restricted to individuals in possession of at least one dose during the interval.
Compared to the NAC-only group, significantly higher appointment attendance at 6 months was observed among those randomized to NAC+cash or NAC+food (Table 2): NAC+cash was associated with an adjusted 13.9 percentage point increase in appointment attendance at 6 months (95% CI: 9.5, 18.3, p<0.01) and NAC+food was associated with an adjusted 12.2 percentage point increase in appointment attendance (95% CI: 7.8, 16.6, p<0.01). At 12 months, appointment attendance remained significantly higher in the NAC+cash and NAC+food groups compared to the NAC-only group. There were no differences in appointment attendance between NAC+cash and NAC+food at 6 or 12 months.
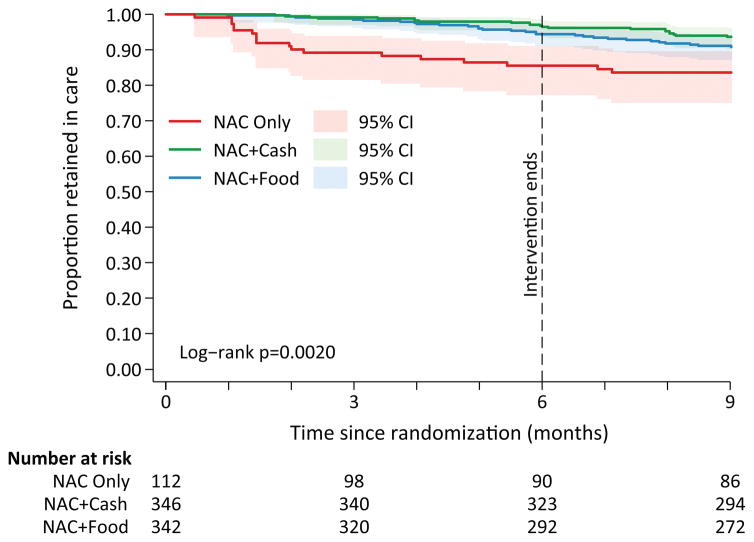
LTFU was significantly less likely in the two intervention groups at 6 months, with 10.9%, 0.9%, and 1.5% of participants LTFU in the NAC-only, NAC+cash, and NAC+food groups, respectively (Table 2). LTFU was not significantly different between the two intervention groups at 6 or 12 months. In the time to event analysis of LTFU, the effect of NAC+cash and NAC+food on preventing LTFU was concentrated in the first three months of the program (Figure 3, log rank test<0.01), but the proportion retained remained higher in both groups after the interventions had ended at 6 months. Both the NAC+cash (adjusted HR=0.07, 95% CI: 0.02, 0.24, p<0.01) and NAC+food groups (HRa=0.12, 95% CI: 0.04, 0.35, p<0.01) were associated with a significantly reduced hazard of LTFU during the first 0–3 months of follow-up, but not during the 3–6 or 6–9 month intervals (Table 3).
FIGURE 3.
Kaplan-Meier curves of the percent of participants in care over time, stratified by study arm (nutrition assessment and counseling (NAC) plus cash or food transfers)a,b
a. Log-rank test for equality of the survival functions: p<0.01
b. The proportion of participants retained in care was defined as one minus the probability of LTFU (≥3 months since the last scheduled visit). By definition, follow-up time between 9 and 12 months could not be classified as LTFU and is therefore not included on the graph.
TABLE 3.
| Study group | 0–3 months |
3–6 months |
6–9 months |
|||
|---|---|---|---|---|---|---|
| HRa | 95% CI | HRa | 95% CI | HRa | 95% CI | |
| NAC only | 1.0 | --- | 1.0 | --- | 1.0 | --- |
| NAC+Cash | 0.07 | (0.02, 0.24)** | 0.56 | (0.17, 1.83) | 1.13 | (0.24, 5.26) |
| NAC+Food | 0.12 | (0.04, 0.35)** | 0.94 | (0.30, 2.89) | 1.63 | (0.36, 7.38) |
HRa=adjusted hazard ratio. CI=confidence interval.
p<0.05
p<0.01
Adjusted for site and for baseline imbalances including WHO clinical stage, occupation, and language. The model includes an interaction between study arm and categorical time at 3 and 6 months to relax the proportional hazards assumption.
LTFU was defined as ≥3 months since the last scheduled visit. By definition, follow-up time between 9 and 12 months could not be classified as LTFU and is therefore not included in the model.
DISCUSSION
This study evaluated whether short-term cash or food assistance improves ART adherence and retention in care among food insecure HIV treatment initiates in Shinyanga, Tanzania. We found that at 6 months, both cash and food assistance increased medication possession and appointment attendance and reduced LTFU compared to the standard of care. At 12 months, 6 months after the intervention period was complete, cash remained significantly associated with better adherence and retention in care. When directly compared, there were few differences between cash and food assistance, although cash was associated with significantly greater MPR≥80% at 6 months and MPR and MPR≥95% at 12 months. Taken together, these data suggest that short-term cash and food assistance are both valuable tools to maximize the effectiveness of ART programs for food insecure PLHIV when provided at treatment initiation.
This study makes three key scientific contributions. First, although some, but not all, quasi-experimental studies have demonstrated that food or cash assistance may improve adherence to HIV treatment and/or care,[14–16, 18, 21, 25, 48, 49] this study is the first to directly compare each intervention against a comparison group using a randomized design. At the same time, there are multiple evaluations in the economic development literature describing the relative merits of cash versus food assistance. In these studies, although both food and cash transfers increase food expenditure and food consumption, food transfers result in larger increases in caloric intake, they may be preferred by beneficiaries, and they may be more appropriate when food markets are functioning poorly.[24, 50, 51] In contrast, cash transfers allow freedom of choice, are cheaper to implement, and may be more “efficient” (according to microeconomic theory) than food transfers.[24, 50, 51] Until now, there were no equivalent data on the comparative effectiveness of different types of support among HIV-infected populations. The data from this study suggest that, at 6 months, the two strategies were statistically similar at improving most measures of adherence and retention among PLHIV versus the standard of care. At 12 months, cash was superior to food on two of the three adherence outcomes.
A second contribution is that this study is the first, to our knowledge, to evaluate the effectiveness of conditional cash transfers (versus standard of care/no incentive) for improving ART adherence in SSA. Cash transfers have been shown to improve ART adherence, viral suppression, and/or retention in multiple studies in high-income countries.[19–22] Our findings suggest that cash transfer programs for PLHIV are acceptable, feasible, and effective in SSA. Furthermore, in addition to the few outcomes where cash was statistically superior to food, the ease of distribution through mobile money providers, lower distribution cost, and participant preference for cash suggests that short-term cash transfers may be a more promising intervention to consider for scale-up in many settings, an assertion suggested in other studies.[24, 50] Furthermore, it may be justified to consider expanding government-run cash transfer programs to HIV-affected households.[23, 36, 52, 53]
A third contribution of the study is the potential durability of the interventions’ effects on retention in care. Our analysis by quarterly interval indicates that the effect of cash and food transfers on LTFU is concentrated in the first three months after enrollment, which was by definition 0–90 days from the date of treatment initiation. However, after 12 months of follow-up, retention in care remained approximately 8–12 percentage points higher in the cash and food groups versus the comparison group (a statistically significant difference among NAC+cash recipients). Thus, although the effect of cash transfers on retention are observed immediately after program initiation, they are sustained at 12 months. This finding is somewhat unexpected because prior incentive programs in health generally,[54] and HIV treatment adherence specifically,[19, 21] typically find that behavior returns to baseline levels after incentives are removed. These data suggest that in some contexts, short-term incentives may incite longer-term benefits on retention, even after the incentives are withdrawn.
This study has several limitations. We did not measure viral suppression; however, MPR is closely correlated with short-term viral load.[37, 38] In addition, there is the potential for poor data quality and missing data in paper-based facility registers; however, missing data was not differential by study arm and it would likely result in underestimates of ART adherence and retention. Lastly, our study was not powered to detect small differences between the two interventions. This study also has significant strengths, including the randomized design, inclusion of a standard of care comparison group, the focus on ART initiates, and participant follow-up after the incentive period. Furthermore, the study focused on food insecure PLHIV who were at risk of malnutrition in order to mitigate the effects of food insecurity before the development of undernutrition.[26–28]
These findings demonstrate that short-term cash and food assistance for food insecure PLHIV initiating treatment improved ART adherence and retention in care during the incentive period. The early effects on adherence and retention were sustained in the cash group after the intervention was complete. Although the two interventions were statistically similar on some outcomes, the magnitude of cash transfers’ effects along with their simpler distribution warrants serious consideration of cash transfers along with other proven interventions as part of a comprehensive package of support at the time of treatment initiation. A larger-scale impact evaluation to determine the effectiveness of short-term support on viral load, cost-effectiveness, and issues related to the potential for scale and sustainability is warranted.
Acknowledgments
SOURCES OF SUPPORT: Funding for the study is provided by the National Institute of Mental Health (McCoy K01MH094246) and PEPFAR’s Food and Nutrition Technical Working Group. Dr. McCoy received research assistant support from National Institute of Health Fogarty Grant TW009338. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
The authors are grateful to Dr. Ramadhan Kabala, Dr. Nancy Czaicki, the local research team and clinic staff, and study participants.
Footnotes
CONTRIBUTORS
The evaluation was designed by SM, PN, SK, WD, and NP. SM, PN, and CF implemented the study and collected data with input from NK. CF and SM conducted the statistical analysis with input from NJ and WD. SM drafted the initial manuscript and all authors participated in reviewing the draft for intellectual content and assisting with revisions. All authors approved the final version of the protocol and manuscript.
DECLARATION OF INTERESTS
The authors have no conflicts of interest to declare.
PREVIOUS PRESENTATIONS: The preliminary results from this study were presented in 2016 by Dr. McCoy at AIDS 2016 in Durban, South Africa.
References
- 1.World Health Organization. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva: 2015. [PubMed] [Google Scholar]
- 2.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 4.Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–941. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 5.Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM. Adherence to Antiretroviral Therapy and Virologic Failure: A Meta-Analysis. Medicine (Baltimore) 2016;95(15):e3361. doi: 10.1097/MD.0000000000003361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kahana SY, Rohan J, Allison S, Frazier TW, Drotar D. A meta-analysis of adherence to antiretroviral therapy and virologic responses in HIV-infected children, adolescents, and young adults. AIDS Behav. 2013;17(1):41–60. doi: 10.1007/s10461-012-0159-4. [DOI] [PubMed] [Google Scholar]
- 7.Group ISS, Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, et al. Initiation of Antiretroviral Therapy in Early Asymptomatic HIV Infection. N Engl J Med. 2015;373(9):795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joint United Nations Program on HIV/AIDS (UNAIDS) 90-90-90: An ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014. [Google Scholar]
- 9.Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. Jama. 2006;296(6):679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 10.Singer AW, Weiser SD, McCoy SI. Does Food Insecurity Undermine Adherence to Antiretroviral Therapy? A Systematic Review. AIDS Behav. 2014 doi: 10.1007/s10461-014-0873-1. [DOI] [PubMed] [Google Scholar]
- 11.Young S, Wheeler AC, McCoy SI, Weiser SD. A Review of the Role of Food Insecurity in Adherence to Care and Treatment Among Adult and Pediatric Populations Living with HIV and AIDS. AIDS Behav. 2013 doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Food and Agriculture Organization of the United Nations. The State of Food Insecurity in the World. Rome. 2010 [Google Scholar]
- 13.Weiser SD, Young SL, Cohen CR, Kushel MB, Tsai AC, Tien PC, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729S–1739S. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–195. doi: 10.1097/QAI.0b013e31818455d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tirivayi N, Koethe JR, Groot W. Clinic-Based Food Assistance is Associated with Increased Medication Adherence among HIV-Infected Adults on Long-Term Antiretroviral Therapy in Zambia. J AIDS Clin Res. 2012;3(7):171. doi: 10.4172/2155-6113.1000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serrano C, Laporte R, Ide M, Nouhou Y, de Truchis P, Rouveix E, et al. Family nutritional support improves survival, immune restoration and adherence in HIV patients receiving ART in developing country. Asia Pac J Clin Nutr. 2010;19(1):68–75. [PubMed] [Google Scholar]
- 17.Martinez H, Palar K, Linnemayr S, Smith A, Derose KP, Ramirez B, et al. Tailored nutrition education and food assistance improve adherence to HIV antiretroviral therapy: evidence from Honduras. AIDS Behav. 2014;18(Suppl 5):S566–577. doi: 10.1007/s10461-014-0786-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Posse M, Tirivayi N, Saha UR, Baltussen R. The effect of food assistance on adherence to antiretroviral therapy among HIV/AIDS patients in Sofala Province, Mozambique: A retrospective study. J AIDS Clin Res. 2013;4(3) [Google Scholar]
- 19.Buzdugan R, Bautista-Arredondo S, McCoy SI. The promise of behavioral economics for HIV/AIDS treatment and care. 21th International AIDS Conference; Durban, South Africa. 2016. [Google Scholar]
- 20.Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Barnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. Aids. 2014;28(Suppl 2):S187–204. doi: 10.1097/QAD.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 21.Galarraga O, Genberg BL, Martin RA, Barton Laws M, Wilson IB. Conditional Economic Incentives to Improve HIV Treatment Adherence: Literature Review and Theoretical Considerations. AIDS Behav. 2013 doi: 10.1007/s10461-013-0415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.El-Sadr WM, Branson BM, Beauchamp G, Hall IH, Zingman LV, Lum G. Effect of Financial Incentives on Linkage to Care and Viral Suppression: HPTN 065. Conference on Retroviruses and Opportunistic Infections; Seattle. 2015. [Google Scholar]
- 23.Fiszbein A, Schady N. World Bank Policy Research Report. Washington, D.C: The World Bank; 2009. Conditional Cash Transfers: Reducing Present and Future Poverty. [Google Scholar]
- 24.Gentilini U. Revisiting the “Cash versus Food” Debate: New Evidence for an Old Puzzle? World Bank Res Obs. 2016;31:135–167. [Google Scholar]
- 25.Kawana BM, Mofu MJ, SIamusantu WS, Kabwe KF, Bwalya BB, Tembo G, et al. Cash or Food? Which Works Better to Improve Nutrition Status and Treatment Adherence for HIV Patients Starting Antiretroviral Therapy. Institute of Development Studies Special Collection. 2014:43–48. [Google Scholar]
- 26.Paton NI, Sangeetha S, Earnest A, Bellamy R. The impact of malnutrition on survival and the CD4 count response in HIV-infected patients starting antiretroviral therapy. HIV Med. 2006;7(5):323–330. doi: 10.1111/j.1468-1293.2006.00383.x. [DOI] [PubMed] [Google Scholar]
- 27.Zachariah R, Fitzgerald M, Massaquoi M, Pasulani O, Arnould L, Makombe S, et al. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. Aids. 2006;20(18):2355–2360. doi: 10.1097/QAD.0b013e32801086b0. [DOI] [PubMed] [Google Scholar]
- 28.Somi G, Keogh SC, Todd J, Kilama B, Wringe A, van den Hombergh J, et al. Low mortality risk but high loss to follow-up among patients in the Tanzanian national HIV care and treatment programme. Trop Med Int Health. 2012;17(4):497–506. doi: 10.1111/j.1365-3156.2011.02952.x. [DOI] [PubMed] [Google Scholar]
- 29.Gardner B. A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychol Rev. 2015;9(3):277–295. doi: 10.1080/17437199.2013.876238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bor J, Tanser F, Newell ML, Barnighausen T. In a study of a population cohort in South Africa, HIV patients on antiretrovirals had nearly full recovery of employment. Health Aff (Millwood) 2012;31(7):1459–1469. doi: 10.1377/hlthaff.2012.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Bureau of Statistics (NBS) Tanzania HIV/AIDS and Malaria Indicator Survey, 2011–12. Dar es Salaam: Tanzania Commission for AIDS (TACAIDS); 2013. [Google Scholar]
- 32.The Food and Nutrition Technical Assistance III Project (FANTA) Nutrition Assessment, Counseling, and Support (NACS): A User’s Guide. U.S. Agency for International Development (USAID), FHI 360; 2013. [Google Scholar]
- 33.McCoy SI, Njau PF, Czaicki NL, Kadiyala S, Jewell NP, Dow WH, et al. Rationale and design of a randomized study of short-term food and cash assistance to improve adherence to antiretroviral therapy among food insecure HIV-infected adults in Tanzania. BMC Infect Dis. 2015;15:490. doi: 10.1186/s12879-015-1186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7(3):e1000251. doi: 10.1371/journal.pmed.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ballard T, Coates J, Swindale A, Deitchler M. Household Hunger Scale: Indicator Definition and Measurement Guide. Washington, D.C: Food and Nutrition Technical Assistance II Project, AED; 2011. [Google Scholar]
- 36.Unit TM. Tanzania Second Social Action Fund. Dar Es Salaam, Tanzania: TASAF; 2011. Second Quarter Implementation Progress Report (October–December 2011) [Google Scholar]
- 37.McMahon JH, Jordan MR, Kelley K, Bertagnolio S, Hong SY, Wanke CA, et al. Pharmacy adherence measures to assess adherence to antiretroviral therapy: review of the literature and implications for treatment monitoring. Clin Infect Dis. 2011;52(4):493–506. doi: 10.1093/cid/ciq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong SY, Jerger L, Jonas A, Badi A, Cohen S, Nachega JB, et al. Medication possession ratio associated with short-term virologic response in individuals initiating antiretroviral therapy in Namibia. PLoS One. 2013;8(2):e56307. doi: 10.1371/journal.pone.0056307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS patient care and STDs. 2010;24(10):607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chi BH, Yiannoutsos CT, Westfall AO, Newman JE, Zhou J, Cesar C, et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 2011;8(10):e1001111. doi: 10.1371/journal.pmed.1001111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.World Health Organization. Retention in HIV Programmes: Defining the challenges and identifying solutions. Meeting Report. 2011 Sep 13–15; [Google Scholar]
- 42.President’s Emergency Plan for AIDS Relief (PEPFAR) PEPFAR Monitoring, Evaluation, and Reporting Indicator Reference Guide. Washington, D.C: 2015. [Google Scholar]
- 43.Rachlis BS, Mills EJ, Cole DC. Livelihood security and adherence to antiretroviral therapy in low and middle income settings: a systematic review. PLoS One. 2011;6(5):e18948. doi: 10.1371/journal.pone.0018948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mosha F, Muchunguzi V, Matee M, Sangeda RZ, Vercauteren J, Nsubuga P, et al. Gender differences in HIV disease progression and treatment outcomes among HIV patients one year after starting antiretroviral treatment (ART) in Dar es Salaam, Tanzania. BMC Public Health. 2013;13:38. doi: 10.1186/1471-2458-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schumi J, Wittes JT. Through the looking glass: understanding non-inferiority. Trials. 2011;12:106. doi: 10.1186/1745-6215-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJ, Group C. Reporting of noninferiority and equivalence randomized trials: an extension of the CONSORT statement. Jama. 2006;295(10):1152–1160. doi: 10.1001/jama.295.10.1152. [DOI] [PubMed] [Google Scholar]
- 47.Points to Consider on the Choice of Non-Inferiority Margin. London: European Agency for the Evaluation of Medicinal Products; 2004. [Google Scholar]
- 48.Ivers LC, Chang Y, Gregory Jerome J, Freedberg KA. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010;7:33. doi: 10.1186/1742-6405-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Metsch LR, Feaster DJ, Gooden L, Matheson T, Stitzer M, Das M, et al. Effect of Patient Navigation With or Without Financial Incentives on Viral Suppression Among Hospitalized Patients With HIV Infection and Substance Use: A Randomized Clinical Trial. Jama. 2016;316(2):156–170. doi: 10.1001/jama.2016.8914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gentilini U. Occasional Papers No 18. Rome: World Food Programme; 2007. Cash and Food Transfers: A Primer. [Google Scholar]
- 51.Gentilini U. Social Protection & Labor Discussion Paper. Washington, D.C: World Bank; 2014. Our Daily Bread: What is the Evidence on Comparing Cash versus Food Transfers? [Google Scholar]
- 52.Dissanayake R, Stephenson Z, Greenslade M. Evaluating social transfer programmes. Guidance for DFID country offices. Department for International Development; 2012. [Google Scholar]
- 53.UNAIDS. Report on the Global AIDS Epidemic. Geneva: 2012. [Google Scholar]
- 54.Dow W, White JS. Exepert Paper No 2013/13. United Nations Department of Economic and Social Affairs, Population Division; 2013. Incentivizing use of health care. [Google Scholar]