Abstract
Objectives
The aim of this study was to evaluate the implication of third molars in postoperative complications of mandibular angle fracture with open reduction and internal fixation (ORIF).
Materials and Methods
Data were collected on patients who presented with mandibular angle fracture at our Department of Oral and Maxillofacial Surgery between January 2011 and December 2015. Of the 63 total patients who underwent ORIF and perioperative intermaxillary fixation (IMF) with an arch bar, 49 patients were identified as having third molars in the fracture line and were followed up with until plate removal. The complications of postoperative infection, postoperative nerve injury, bone healing, and changes in occlusion and temporomandibular joint were evaluated and analyzed using statistical methods.
Results
In total, 49 patients had third molars in the fracture line and underwent ORIF surgery and perioperative IMF with an arch bar. The third molar in the fracture line was retained during ORIF in 39 patients. Several patients complained of nerve injury, temporomandibular disorder (TMD), change of occlusion, and postoperative infection around the retained third molar. The third molars were removed during ORIF surgery in 10 patients. Some of these patients complained of nerve injury, but no other complications, such as TMD, change in occlusion, or postoperative infection, were observed. There was no delayed union or nonunion in either of the groups. No statistically significant difference was found between the non-extraction group and the retained teeth group regarding complications after ORIF.
Conclusion
If the third molar is partially impacted or completely nonfunctional, likely to be involved in pathologic conditions later in life, or possible to remove with the plate simultaneously, extraction of the third molar in the fracture line should be considered during ORIF surgery of the mandible angle fracture.
Keywords: Mandibular fracture, Third molar, Open reduction
I. Introduction
Mandibular angle fracture is the most common mandibular fracture, accounting for 40% of all mandibular fractures1. Mandibular angle fracture is defined as a fracture line between the anterior border of the mandibular ramus and the body of the mandible2. The management of angle fracture is difficult because of its thin cross-sectional area and its attachment to the masticatory muscles applying forces in different vectors, its abrupt change in curvature, and the presence of lower third molars3.
Hanson et al.1 have reported that the presence of a lower third molar doubles the risk of angle fracture, and Rajandram et al.4 showed the presence of lower third molars in 60.4% of mandibular angle fractures. Partially erupted third molars produce an increased risk of mandibular angle fracture. As a result, previous studies have recommended that individuals such as sports players, who are exposed to high risk of facial trauma, wear protective facial gear and mouth guards4.
The extraction of the third molars in mandibular angle fracture remains controversial. Some researchers support the extraction of the tooth in the fracture line, as they believe it decreases the risk of infection and the need for removal of the third molars and plate in the future5. Other researchers have shown that extraction of the tooth can lead to loss of bone, increase the difficulty in reduction and plating, and increase both the surgical time of the procedure and the risk to the inferior alveolar nerve6.
The aim of this study was to evaluate the implication of the third molars in the postoperative infection, postoperative nerve injury, bone healing, change in occlusion, and temporomandibular disorder (TMD) of the mandibular angle fracture with open reduction and internal fixation (ORIF).
II. Materials and Methods
A retrospective review of patients who presented with mandibular angle fracture at our Department of Oral and Maxillofacial Surgery, Inje University Busan Paik Hospital (Busan, Korea) between January 2011 and December 2015 was conducted, and data were collected by reviewing medical records and radiographs. Of the 63 total patients who underwent ORIF and perioperative intermaxillary fixation (IMF) with an arch bar, 49 patients were identified as having third molars in the fracture line and were followed up with until plate removal. The inclusion criteria were as follows: patients having third molars in the fracture line, patients who underwent ORIF under general anesthesia and perioperative IMF with an arch bar, and patients who participated in follow-up until plate removal.
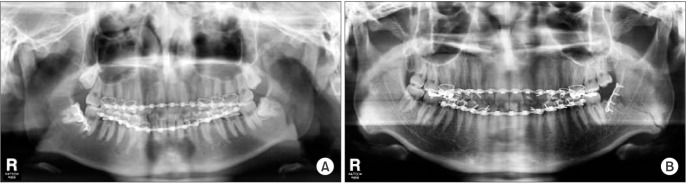
Panoramic radiographs and facial bone computed tomography of the patients were obtained, and demographic data, including age, sex, and medical history, were documented. All of the patients underwent ORIF surgery and perioperative IMF with an arch bar. Analgesics and antibiotics were administered in all cases for about 6 days from admission until discharge. Examination findings related to postoperative alveolar nerve function, change in occlusion, TMD, infection, and delayed union or nonunion were recorded, and additional images of panoramic radiographs (Fig. 1), mandible series, and modified Towne's view (Fig. 2) were obtained for follow-up.
Fig. 1. Postoperative panoramic radiographs. A. Non-extraction case. B. Extraction case.
Fig. 2. Mandible series+modified towne's view.

The data were statistically analyzed using the IBM SPSS Statistics version 22.0 for Windows (IBM Co., Armonk, NY, USA), and comparative analyses of the two groups were performed using the χ2 test. Differences were considered statistically significant if the confidence interval P-value was <0.05.
III. Results
Forty-nine patients with third molars in the fracture line underwent ORIF surgery with one or two miniplates under general anesthesia and perioperative IMF with an arch bar. Third molars in the fracture line were retained in 39 patients (Group 1) during ORIF. The non-extraction group consisted of 33 males (84.6%) and 6 females (15.4%). The age range for the non-extraction group was 14 to 48 years of age (mean age, 23.6±7.8 years). Third molars in the fracture line were removed in 10 patients (Group 2) during ORIF. The third molars in the lines of fracture were removed at the time of surgery because of crown root fractures in 2 patients and because of difficulties of reduction or possibilities of infection with a gap between the third molars and fractured bones in 8 patients. The extraction group consisted of 10 males (100%) and 0 females (0%). The age range for the extraction group was 16 to 53 years (mean age, 31.2±14.83 years). The mean hospitalization period was approximately 6 days, with IMF periods of about 3 to 5 days. The total follow-up period was about 6 months until the plate was removed.
Of the 39 patients, 4 patients in the non-extraction group complained of a neurosensory deficit of the inferior alveolar nerve after trauma, while 5 other patients complained of additional nerve injury after surgery. Of the 10 patients, 5 patients in the third molar extraction group complained of a neurosensory deficit of the inferior alveolar nerve after trauma, while 1 patient complained of additional nerve injury after surgery. All of the patients exhibited almost complete nerve recovery during the follow-up period.
Five patients in the non-extraction group complained of pain and swelling in their retained third molars during follow-up and were diagnosed with periapical abscess, pericoronitis, buccal space abscess, or submandibular space abscess. The patients received medication and underwent intra- or extra-oral incision and drainage. They consisted of 4 males (75.0%) and 1 female (25.0%). The age range was 19 to 34 years. The state of impaction of the lower third molars was vertical partial eruption (60.0%) and mesioangular partial eruption (40.0%). One patient with deviation of the mandible had to undergo a second operation including intra-oral incision and drainage on the retained third molar. This patient also required additional extra-oral incision and drainage procedures during the follow-up period because the infection spread into the submandibular space.(Table 1) After treatment for about 5 days, acute symptoms and signs of infection in the 5 patients subsided. No patient in the extraction group exhibited infection in the third molar extraction area or fracture line. However, there was no significant association between the two groups (P>0.05).
Table 1. Clinical data of patients with postoperative infection.
| Case no. | Sex/age (yr) | Types of impaction | Postoperative onset (day) | Symptom | Diagnosis | Treatment | Other complications |
|---|---|---|---|---|---|---|---|
| 1 | M/23 | Mesioangular, partial eruption | 58 | Pain, swelling | Periapical abscess | Intra-oral I&D medication | Postoperative numbness |
| 2 | M/19 | Vertical, partial eruption | 75 | Pain, swelling | Pericoronitis, tonsillitis | Medication | NS |
| 3 | M/25 | Vertical, partial eruption | 28 | Pain, swelling, pus discharge | Pericoronitis | Intra-oral I&D medication | NS |
| 4 | F/18 | Mesioangular, partial eruption | 45 | Pain, swelling | Buccal space abscess | Intra-oral I&D medication | NS |
| 5 | M/34 | Vertical, partial eruption | 47 | Pain, severe swelling, pus discharge | Buccal space, subman-dibular space abscess | Intra-oral, extra-oral I&D medication | Change of occlusion |
(M: male, F: female, I&D: incision and drainage, NS: non-specific)
Two patients in the non-extraction group complained of TMD symptoms such as noise or pain of the temporomandibular joint (TMJ). None of the patients in the extraction group exhibited signs or symptoms of TMD.
Only 1 patient with malocclusion as a result of left mandible deviation after surgery had to be operated on again. No patients exhibited delayed union or nonunion. None of the patients in the extraction group complained of changes in occlusion, delayed union, or nonunion.
There was no significant association between the two groups with regard to postoperative nerve injury, TMD, or change in occlusion (P>0.05).(Table 2)
Table 2. Comparisons between the non-extraction group and extraction group.
| Complication | Non-extraction group (n=13) | Extraction group (n=1) |
|---|---|---|
| Infection | 5 | 0 |
| Postoperative numbness | 5 | 1 |
| Temporomandibular disorder | 2 | 0 |
| Change of occlusion | 1 | 0 |
| Delayed union, nonunion | 0 | 0 |
IV. Discussion
This study included 49 patients, 43 males (87.8%) and 6 females (12.2%), divided into a non-extraction group and an extraction group. Of these patients, 17 patients (34.7%) had a mandible angle fracture on the right side, while 32 patients (65.3%) had a mandible angle fracture on the left side. Another study on mandibular angle fracture reported similar epidemiologic data. Patel et al.3 showed that the overwhelming majority of patients were men, comprising 85 of 103 patients (82.5%), whereas women accounted for 18 of 103 patients (17.5%) with mandibular angle fracture. Most fractures occurred at the left mandibular angle (34.9%), followed by the right side (34.9%) and both sides (5.8%).
In this study, all patients underwent IMF for the management of mandibular angle fracture. IMF is a reliable technique for reduction and stabilization before plate fixation, although the use of interdental wiring may have adverse effects on the teeth or surrounding tissue and require additional time7,8,9,10. Bhagol et al.11 explained that although superior and inferior plates are typically required for adequate fixation, a superior border plate placed at the point of maximal tension is sufficient for mandibular angle fracture. In this study, preoperative IMF using an arch bar was applied and used for approximately 3 to 5 days after surgery, with 1 or 2 miniplates placed at the superior area during ORIF surgery. Only 1 patient with malocclusion because of left mandible deviation after surgery required an additional operation. There were no cases of delayed union or nonunion in either group. It is speculated that closed reduction with IMF may reduce micromobility and improve stability.
Management of the third molars in fracture lines has been controversial. Yadavalli et al.6 proposed that the presence of third molars in fracture lines may be of great value in the repositioning of fractures because the presence of third molars prevents further injury to the bone tissue. The extraction of third molars makes it difficult to reduce the contact between fracture segments when the fragments are highly mobile6. Because extraction of the tooth increases the risk of contamination through the empty alveolus6,12, Yadavalli et al.6 used the following criteria for surgical removal of the third molars in the line of fracture: pericoronal or periodontal infection, cross caries, extensive periapical lesions, mobility, or exposure of the apical half or more of the root fracture.
McNamara et al.5 noted that the risks involved with extraction of third molars includes loss of bone, greater difficulty in reduction and plating, increased surgical time, and increased risk to the inferior alveolar nerve. In their study, the incidence of nerve injury was 16% for the retention group compared to 39% for the removal group. Therefore, they stated that the removal of third molars creates an additional risk of nerve injury and increases operating time4. In this study, 4 patients in the non-extraction group and 1 patient in the extraction group complained of postoperative nerve injury, and there was no significant difference between the groups. All of the patients exhibited gradual recovery of the nerve during the follow-up period.
The issue of postoperative infection has long been debated and represents a common complication of mandible angle fracture3. A 1994 study by Ellis and Walker12 found that the extraction of third molars in fracture lines seemed to increase postoperative infection3,4,13. In 2002, they proposed that the risk of postoperative infection increased if teeth were left in the fracture line3,4,13. Patel et al.3 defined infection as purulent discharge from the intraoral incision through a sinus tract to the skin, or a closed area of swelling that required incision and drainage of purulent material. They found no statistically meaningful relationship between tooth management in the line of the fracture and rate of postoperative infection3. They stated that the differences in rates of infection might be attributed to inherent differences in the socioeconomic status of patients, tobacco and alcohol use and abuse, nutritional status, and other medical co-morbidities3. However, in this study, the patients were mostly young and free of significant medical history such as uncontrolled diabetes, alcohol abuse, or severe smoking. Also, antibiotics were administered upon admission to the hospital until about 6 days from admission until discharge. As a result, there seemed to be no immediate infection or other complications. During the follow-up period, 5 patients in the non-extraction group received medication and underwent intra or extra-oral incision and drainage because of infection. All third molars were partially impacted. After treatment for 5 days, acute symptoms and sign of infections subsided. All infected third molars underwent extraction during the plate removal surgical procedure. None of the patients in the extraction group exhibited infection in the third molar extraction area or fracture line. This may be attributed to standard protocol at the time of surgery such as gentle curettage, copious irrigation, interrupted sutures offering strength and flexibility of the extraction site, and antibiotics. Complications differed between the two groups, but there was no significant difference.
Mandibular trauma was stated as the most frequent reason for TMD. Baltrusaityte et al.14 reported that mandibular fracture occurred various sings and symptoms of TMD. Alterations of the masticatory system caused by dislocation of body fragments and conservative treatment of mandibular fractures showed that inaccurate immobilization of the mandible after trauma resulted in a “new bite.” Consequently, conditions for the development of TMJ dysfunction occurred as a result of adapted dynamical masticatory movements and new occlusion14,15. Instances of deviation upon opening and the presence of joint sounds were higher in cases treated with miniplate fixation and were more susceptible to development of traumatic arthritis16. In this study, 2 patients in the non-extraction group exhibited symptoms of TMD. One of the patients complained of TMJ noise, while the other patient complained of intermittent TMJ pain after surgery. However, there was no statistically significant difference between the two patients, and both of them improved during the follow-up period.
One limitation of this study is the small number of patients in the extraction group. Therefore, further studies are necessary.
V. Conclusion
There was no statistically significant difference in postoperative complications between the extraction and non-extraction groups of third molars in the fracture line. If the third molar is partially impacted or completely nonfunctional, likely to be involved in pathologic conditions later in life, or possible to remove it with the plate simultaneously, extraction of the third molar in the fracture line should be considered during ORIF surgery of the mandible angle fracture.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Hanson BP, Cummings P, Rivara FP, John MT. The association of third molars with mandibular angle fractures: a meta-analysis. J Can Dent Assoc. 2004;70:39–43. [PubMed] [Google Scholar]
- 2.Al-Moraissi EA, Ellis E., 3rd What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2014;72:2197–2211. doi: 10.1016/j.joms.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Patel N, Kim B, Zaid W. A detailed analysis of mandibular angle fractures: epidemiology, patterns, treatments, and outcomes. J Oral Maxillofac Surg. 2016;74:1792–1799. doi: 10.1016/j.joms.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Rajandram RK, Nabil S, Shareif MS, Ishak I, Marhazlinda J, Nordin R, et al. Mandibular third molar and angle of mandible fractures: an unsolved clinical dilemma. Sains Malaysiana. 2013;42:39–43. [Google Scholar]
- 5.McNamara Z, Findlay G, O'Rourke P, Batstone M. Removal versus retention of asymptomatic third molars in mandibular angle fractures: a randomized controlled trial. Int J Oral Maxillofac Surg. 2016;45:571–574. doi: 10.1016/j.ijom.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Yadavalli G, Mythily PH, Shetty JN. Clinical evaluation of mandibular angle fractures with teeth in fracture line, treated with stable internal fixation. Indian J Stomatol. 2011;2:216–221. [Google Scholar]
- 7.Bell RB, Wilson DM. Is the use of arch bars or interdental wire fixation necessary for successful outcomes in the open reduction and internal fixation of mandibular angle fractures? J Oral Maxillofac Surg. 2008;66:2116–2122. doi: 10.1016/j.joms.2008.05.370. [DOI] [PubMed] [Google Scholar]
- 8.Fordyce AM, Lalani Z, Songra AK, Hildreth AJ, Carton AT, Hawkesford JE. Intermaxillary fixation is not usually necessary to reduce mandibular fractures. Br J Oral Maxillofac Surg. 1999;37:52–57. doi: 10.1054/bjom.1998.0372. [DOI] [PubMed] [Google Scholar]
- 9.Dimitroulis G. Management of fractured mandibles without the use of intermaxillary wire fixation. J Oral Maxillofac Surg. 2002;60:1435–1438. doi: 10.1053/joms.2002.36100. [DOI] [PubMed] [Google Scholar]
- 10.Kim MY, Kim CH, Han SJ, Lee JH. A comparison of three treatment methods for fractures of the mandibular angle. Int J Oral Maxillofac Surg. 2016;45:878–883. doi: 10.1016/j.ijom.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Bhagol A, Shigh V, Singhal R. Management of mandibular fractures. In: Motamedi MHK, editor. A textbook of advanced oral and maxillofacial surgery. 1st ed. Rijeka, Croatia: InTech; 2013. pp. 385–414. [Google Scholar]
- 12.Ellis E, 3rd, Walker L. Treatment of mandibular angle fractures using two noncompression miniplates. J Oral Maxillofac Surg. 1994;52:1032–1036. doi: 10.1016/0278-2391(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 13.Ellis E., 3rd Outcomes of patients with teeth in the line of mandibular angle fractures treated with stable internal fixation. J Oral Maxillofac Surg. 2002;60:863–865. doi: 10.1053/joms.2002.33852. [DOI] [PubMed] [Google Scholar]
- 14.Baltrusaityte A, Surna A, Pileicikiene G, Kubilius R, Gleiznys A, Baltrusaitis M. Dynamical changes of occlusion and articulation during treatment of mandibular angle fractures. Stomatologija. 2013;15:12–19. [PubMed] [Google Scholar]
- 15.Pullinger AG, Seligman DA. Trauma history in diagnostic groups of temporomandibular disorders. Oral Surg Oral Med Oral Pathol. 1991;71:529–534. doi: 10.1016/0030-4220(91)90355-g. [DOI] [PubMed] [Google Scholar]
- 16.Chaurasia NK, Guan J, Wang X, Sah G. Clinical analysis of changes in function of the temporomandibular joint after open reduction and internal fixation of mandible fracture. Indian J Oral Sci. 2015;6:60–64. [Google Scholar]