Abstract
Purpose
Fractures of the lateral end of the clavicle are relatively uncommon. These fractures are unstable due to the various deforming forces which act on the fragments as well as the small distal fracture fragment. At most times the deforming forces are not taken into consideration, and the fracture is not fixed securely. In this study, we assessed a fixation technique using the precontoured locking plates to find out whether it provided a stable fixation with good functional outcome.
Methods
Totally, 32 patients with lateral end clavicle fracture (Neer's Type II) were included in the study. After the informed consent and preoperative investigations were obtained, open reduction and internal fixation was done using a 3.5 mm precontoured superior locking plate with lateral extension under general anesthesia. Postoperative X-rays were done on day 1 and every 6 weeks after operation, until radiological union was achieved. The postoperative pain was assessed using Visual Analogue Scale (VAS) on postoperative days 1, 2 and 10. Postoperatively arm pouch sling was given for 2 weeks followed by active mobilization. Patients were asked to do their daily routine work and avoid lifting heavy weights. The functional outcome was assessed at the end of 2nd and 6th months with the help of Disabilities of the Arm, Shoulder and Hand (DASH) scoring.
Results
There were no intraoperative complications in the procedure. The mean VAS score on postoperative day 1 was found to be 5 which decreased to 3 on day 2 and 0 on day 10. The mean DASH score was calculated as 11.63 at the end of postoperative month 2 and then 4.6 at the end of month 6. There was one case of malunion in whom the overhead abduction was restricted but was not painful and was managed conservatively.
Conclusion
The precontoured locking plates with lateral extension may be a good method to fix the fractures of the lateral end clavicle, which provide a stable fixation with good functional outcome with very few instances of stiffness and decreased range of motion of the shoulder with the hook plates and failure of fixation in screw and K-wire fixations. It may well be the answer to the fixation questions of the lateral clavicle fractures, although larger comparative studies between the surgical treatment methods are required to confirm the same.
Keywords: Lateral end clavicle fractures, Precontoured locking plates, Functional outcome
Introduction
Fractures of the clavicle are common injuries of adults, accounting for about 3% of all injuries.1 They are often caused by either a direct blow to the anterior chest wall or by a fall on the outstretched hand. The commonest site of fracture in clavicle is the midshaft followed by the lateral end, which accounts for about 25% of all the clavicle fractures.2, 3 Twenty-five percent of these fractures are unstable due to the displacing forces acting on the fracture fragments: an inferior force on the lateral clavicle fracture fragment and an anterosuperior force on the medial clavicle fragment. These fractures can be classified using the Neer's Classification.4 The lateral fractured fragment is small and hence, it is difficult to get an anatomical reduction and also poses problems in its fixation, which results in instability of the lateral clavicle fractures. Many treatment modalities have been used for the management of such fractures. Nonoperative methods are associated with high rates of nonunion (22%–50%),5, 6, 7 out of which 14% cases6 were symptomatic. Many operative treatment modalities have been tried for the management of lateral clavicle fracture including coracoclavicular screws,8, 9, 10 Kirschner wires,11 tension bands,12, 13, 14, 15 hook plates,16, 17 nonlocked18 and locked plates.16, 19, 20, 21, 22 The operative modalities are not without complications. These include non-united and malunited fractures, pin migration, impingement of the plate, bleeding, the requirement of removal of the plate16, 18 in all the fixation modalities. In this study, we have evaluated the functional and radiological outcomes of the patients in whom a locking plate was used for fixation of the lateral end of clavicle fractures, in the younger population.
Materials and methods
Patients
This study was conducted in Indraprastha Apollo Hospital, New Delhi from 2012 to January 2015. All patients with an acute fracture of lateral end clavicle (Neer's Type II) were considered for the study. We excluded the patients who had fractures more than 7 days old, and also patients with neurovascular deficits. All patients were adults, and no minors were included in this study. After informed consent had been obtained, 32 patients were included in this study. After initial management of the patient, surgery was planned, and the patient underwent surgery as soon as possible. In all the patients open reduction and internal fixation (ORIF) using a 3.5 mm pre-contoured superior locking plate with lateral extension was done.
Surgery
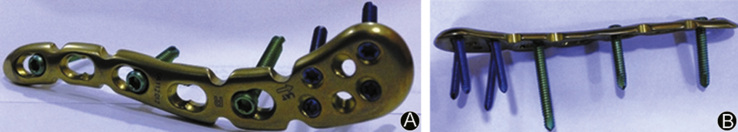
All the surgeries were performed by a single surgeon (the first author) under general anesthesia and in the supine position with a roll of towel in between the scapula to retract the clavicle. The head of the patient was turned towards the opposite side to get a clear view of the operating site. A horizontal incision was taken over the superior clavicle, centering the fracture. This was followed by subcutaneous dissection taking care of the supraclavicular nerves. Division of platysma exposed the clavicle. The reduction was achieved and maintained by a temporary Kirchner wire fixation. A precontoured locking compression plate (LCP, superior anterior clavicle plate with lateral extension) was used to fix the fracture, with the help of 3.5 mm locking and cortical screws on the medial side and 2.7 mm locking screws on the lateral side (Fig. 1). The closure was done in layers.
Fig. 1.
Precontoured lateral clavicle locking plate. A: superior view; B: side view.
Postoperative care
Postoperative period was uneventful in all the cases. Arm pouch was given to all the patients. Post operatively all the patients were advised mobilization of the elbow and wrist. Patients were discharged after 2 days and staple removal done at 1 week. Shoulder mobilization was started on 10 days after the pain subsided and the arm pouch was removed at 2 weeks. X-ray assessment of the clavicle was done on the 1st postoperative day and after every 6 weeks, until radiological union was achieved. The postoperative pain was assessed using Visual Analogue Scale (VAS) on 1st, 2nd, and 10th postoperative day. The analgesics were stopped after 2 days and advised to be taken if the VAS score was more than 4. The dressing was done on the 2nd day and suture removal on 7th postoperative day. The clinical outcome was assessed on the 2nd and 6th month postoperatively using Disabilities of the Arm, Shoulder and Hand (DASH) scoring system.23 The patients were also followed up with the Constant–Murley scoring at the second and sixth month postoperatively. The patient was kept in follow up till the bony union was achieved.
Results
Thirty-two cases of lateral clavicle fracture were included in this study with 71.85% of cases (23 cases) having a fracture in the left clavicle. There were no cases of bilateral clavicle fractures. The average age of the patients was 25.6 years, ranging from 18 to 28 years. The mode of injury of the fracture was road traffic accidents in 22 patients, followed by fall at home (9 patients) and fall on the street (2 patients). The mean duration of operative fixation since the time of injury was 2.2 days (ranging from 6 h to 5 days). None of the cases had any distal neurovascular deficit. The operating time ranged from 42 to 67 min (average: 53 min). In all cases, a 4-hole precontoured plate was used. There were no significant intra- or postoperative events noted in any of the cases. All the immediate postoperative X-rays showed satisfactory reduction and fixation. The average postoperative period of stay was 1.7 days (range: 1–3 days). None of the cases had any postoperative wound infection or neurovascular deficit.
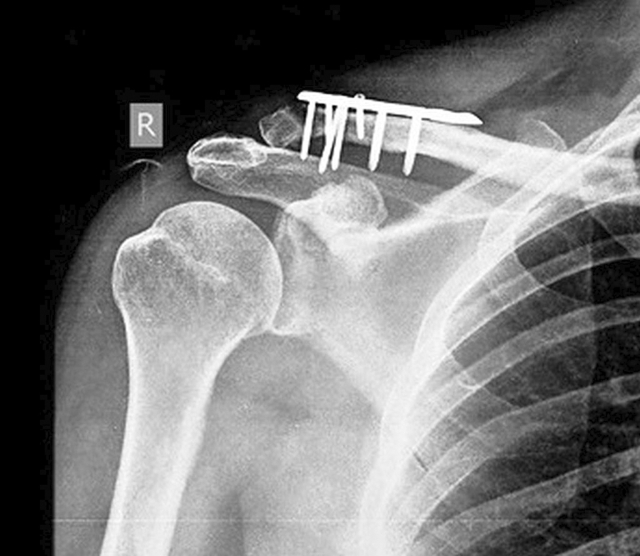
The mean VAS score on the 1st postoperative day was found to be 5 which decreased to 3 on the 2nd day and 0 on the 10th postoperative day. The mean time of bone union was found to be 15.3 weeks. The main complication was malunion which was seen in one case who was not symptomatic (Fig. 2) and nonunion in one case (Fig. 3). The mean DASH score was 11.63, 2 months postoperatively and 4.6 at the end of 6 months. The average Constant–Murley scores were 85 at 2 months postoperatively and 92 at 6 months postoperatively. According to the Constant–Murley score, the functional outcomes were excellent in 7 patients (21.85%), good in 19 (59.37%), moderate in 6 (18.75%). None of the plates had to be removed for any implant failures.
Fig. 2.
Malunion after ORIF of a lateral clavicle fracture.
Fig. 3.
Nonunion after ORIF of a lateral clavicle fracture.
Discussion
Clavicle fractures are one of the most common injuries in an adult population. It is also commonly associated with injuries to ribs, head and the upper extremities. These fractures are being encountered increasingly due to increase in high-velocity trauma as seen in the young population. Due to more soft tissue injuries associated with these accidental injuries, the fracture fragments are displaced and require adequate reduction and fixation. Moreover, the functional demands in younger patients are high, and hence there has been a recent increase in the operative fixation of these fractures.
With the advent of newer techniques of fixation, it is expected that the problems related to its fixation, complications, and outcomes would be reduced significantly. Clavicle fractures were generally treated by non-operative means. The lateral end clavicle fractures where the distal fractured fragment is small and the deforming forces are great, the nonoperative treatment fails as it is associated with the significant incidence of complications like malunion, nonunion, joint stiffness, etc.
The deforming forces are due to the powerful pull of the muscles along with the presence of the coracoacromial ligament and the coracoclavicular ligament and the weight of the arm. They are responsible for the instability of the fracture along with malunion and nonunion, which leads to functional disabilities. Hence, the need for surgical management in the form of stable fixation is necessary.
Various surgical procedures for lateral clavicle fractures have been used like K-wire fixation, screw fixation, tension band wiring, hook plates, non-locking and locking plates. We have used anterior locking compression plate with lateral extension, which provided a stable fixation of the fractured fragments and allowed early mobilization of the shoulder. This plate is anatomical and fits well to the contour of the lateral end of the clavicle. It also allows screw fixation in different planes in the lateral end of the clavicle and hence provides a multi-planar fixation of the distal fragment of the fracture and greater stability to the small unstable fragment. This implant not only neutralizes the forces acting upon the fracture fragments but also gives better hold in osteoporotic bones. We believe that all these factors contribute to a successful union of the clavicle fracture along with good functional outcomes.
Kalamaras et al13 were the first to report the concept of locking plate in distal clavicle fracture in their study where distal radius locking plate was used and finally concluded that the use of the locking plate gave good results and was promising for the management of the lateral clavicle fracture as it showed to have a better control on the distal fracture fragment. Rieser et al24 analyzed the biomechanical analysis of the lateral clavicle fracture treated with the help of various treatment modalities and reported that locking plate fixation provided a stable fixation biomechanically and the clinical outcome was also satisfactory. Hence, it was assumed that the lateral end clavicle plate was biomechanically stable and would give good results in the fracture fixation of the small distal fragments of the Neer's type II fractures which were included in this study.
So far, there have been limited studies of lateral clavicle fractures fixed with the help of locking LCP plates. In a small case series of Sajid et al,25 4 cases of lateral clavicle fractures were treated with the help of different modalities of treatment including lateral clavicle locking with bone grafting, lateral clavicle locking plate alone, lateral clavicle locking compression plate system and Small Fragment Locking Compression Plate System (Synthes™) and they recommended that the locking plate should be augmented with the coracoclavicular sling which is in direct contradiction to the biomechanical study by Rieser et al24 and on contemplating we decided not to augment the locking plates with coracoclavicular sling and our clinical results were excellent with no instability clinically or radiologically, postoperatively or at 6 months of follow-up and even though we had 1 case of radiological malunion none of them were symptomatic and hence did not require secondary surgery.
Anderson et al23 reported 13 cases of lateral clavicular fractures fixed with the locking LCP plate and concluded that superior locking plates provided high union rates along with good functions and low complications rates. Our results are comparable to their study.
Klein et al16 compared the fixation outcomes of the lateral clavicular fractures using precontoured locking plates with suture augmentation in 16 patients and lateral clavicle hook plates in 22 patients and have found, on evaluating the union rates in early and late they found that late fracture fixation was associated with more problems as compared with the early fracture fixation. In our study, we had fixed all the fracture early and found good results with the use of the pre contoured locking plates.
In a comparative study done by Chunlin et al26 the LCP plate was compared with the hook plate and in 66 patients (30 done by hook plate and 36 done by locking plate) it was seen that the clinical outcome was better in locking plate as compared to hook plate. The complication rates in this study were comparable to our study with a good surgical outcome.
In a recent review article by Sambandam et al27 they concluded by saying that the clinical outcome was equal in both the flexible fixation that is by tension band wiring and K-wires, and the rigid fixation like plating. They have also stated that the flexible implants are better as they can be removed very easily under local anesthesia whereas rigid implants required surgery under anesthesia for the plate removal. We have got excellent clinical results with the rigid fixation, and in our study, none of the plates had to be removed, and there were no complaints from the patient about discomfort from the implant.
In the last one decade, the incidence of ORIF of clavicle fractures has increased tremendously. This coincides with a favourable publication in 2007 in the Canadian Orthopaedic Trauma Society related to better outcomes of ORIF of clavicle fractures.28 However, it is mandatory to understand that all clavicle fractures (especially midshaft fractures) need not be fixed and can still be very treated well with conservative treatment. ORIF of shaft fractures has also been found to be associated with significant rates of reoperations.29 Hence, a judicial and scientific rationale must be used while treating clavicle fractures.
The fractures involving the lateral end clavicle fractures are a challenge for the treating surgeon. This is due to the constant pull of the muscles attached to the lateral end of the clavicle. Also, usually these fractures are comminuted, making the purchase of screws difficult. Herein lays the advantages of the lateral end clavicle locking plates. Due to the small size of the screws, multiple options of the screws are available. As many as six locking screws with separate alignment directions are available in Synthes™ lateral end clavicle plate. Also, since the screws are locking in nature, they have an increased pull-out strength and also need not take purchase in the far cortex. These advantages make the lateral end clavicle locking plates extremely useful in the management of these difficult fractures.
We believe that the main indication for ORIF in clavicle fractures should be a displaced fracture of lateral end of the clavicle and not the mid-shaft fractures. The complications like nonunion and malunion which were seen were due to the learning curve of the surgeon as seen in the post-operative X-rays, as in the later operated cases these complications were not seen.
In conclusion, precontoured locking plates provide adequate stable fixation for the lateral end clavicle fractures and are not associated with any major complications. This low profile implant is easy to use and fits well to the contour of the lateral end of the clavicle and offers multi planar screw fixation in this small fragment providing stability. It may well be the answer to the fixation woes of the lateral clavicle fractures. Although, larger comparative studies between the various surgical treatment methods are required to confirm the same.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Robinson C.M. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Jt Surg Br. 1998;80:476–484. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 2.Robinson C.M., Cairns D.A. Primary non-operative treatment of displaced lateral fractures of the clavicle. J Bone Jt Surg Am. 2004;86:778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Khan L.A., Bradnock T.J., Scott C. Fractures of the clavicle. J Bone Jt Surg Am. 2009;91:447–460. doi: 10.2106/JBJS.H.00034. [DOI] [PubMed] [Google Scholar]
- 4.Neer C.S., II Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 5.Nordqvist A., Petersson C., Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64:87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 6.Robinson C.M., Court-Brown C.M., McQueen M.M. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Jt Surg Am. 2004;86:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Rokito A.S., Zuckerman J.D., Shaari J.M. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002;61:32–39. [PubMed] [Google Scholar]
- 8.Ballmer F.T., Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Jt Surg Br. 1991;73:291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 9.Macheras G., Kateros K.T., Savvidou O.D. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28:693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 10.Yamaguchi H., Arakawa H., Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22:366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elb Surg. 2003;12:24–28. doi: 10.1067/mse.2003.128564. [DOI] [PubMed] [Google Scholar]
- 12.Shin S.J., Roh K.J., Kim J.O. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40:1308–1312. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Kalamaras M., Cutbush K., Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elb Surg. 2008;17:60–62. doi: 10.1016/j.jse.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Chen C.H., Chen W.J., Shih C.H. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–78. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Bezer M., Aydin N., Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma. 2005;19:524–528. doi: 10.1097/01.bot.0000164593.04348.e5. [DOI] [PubMed] [Google Scholar]
- 16.Klein S.M., Badman B.L., Keating C.J., Devinney D.S., Frankle M.A., Mighell M.A. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elb Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 17.Haidar S.G., Krishnan K.M., Deshmukh S.C. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elb Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Kona J., Bosse M.J., Staeheli J.W., Rosseau R.L. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4:115–120. doi: 10.1097/00005131-199004020-00002. [DOI] [PubMed] [Google Scholar]
- 19.Herrmann S., Schmidmaier G., Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 20.Kaipel M., Majewski M., Regazzoni P. Double-plate fixation in lateral clavicle fractures—a new strategy. J Trauma. 2010;69:896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 21.Oh J.H., Kim S.H., Lee J.H. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131:525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 22.Yu C., Sun Y.H., Zhao C.Q. Treatment of distal clavicle fracture with distal radius volar locking compression plate. Chin J Traumatol. 2009;12:299–301. [PubMed] [Google Scholar]
- 23.Anderson K. Evaluation and treatment of distal clavicle fractures. Clin Sports Med. 2003;22:319–326. doi: 10.1016/s0278-5919(02)00108-4. [DOI] [PubMed] [Google Scholar]
- 24.Rieser G.R., Edwards K., Gould G.C. Distal-third clavicle fracture fixation: a biomechanical evaluation of fixation. J Shoulder Elb Surg. 2012;22:848–855. doi: 10.1016/j.jse.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 25.Sajid S., Fawdington R., Sinha M. Locking plates for displaced fractures of the lateral end of clavicle: potential pitfalls. Int J Shoulder Surg. 2012;6(4):126–129. doi: 10.4103/0973-6042.106226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chunlin Z., Junwu H., Yi L. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distalclavicle fractures and a systematic literature review. Int Orthop. 2014;38:1461–1468. doi: 10.1007/s00264-014-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sambandam B., Gupta R., Kumar S. Fracture of distal end clavicle: a review. J Clin Orthop Trauma. 2014;5:65–73. doi: 10.1016/j.jcot.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Canadian Orthopaedic Trauma Society Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Jt Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 29.Leroux T., Wasserstein D., Henry P. Rate of and risk factors for reoperations after open reduction and internal fixation of midshaft clavicle fractures: a population-based study in Ontario, Canada. J Bone Jt Surg Am. 2014;96:1119–1125. doi: 10.2106/JBJS.M.00607. [DOI] [PubMed] [Google Scholar]