Abstract
Purpose
The administrative data from trauma centers could serve as potential sources of invaluable information while studying epidemiologic features of car accidents. In this cross-sectional analysis of Shahid Rajaee hospital administrative data, we aimed to evaluate patients injured in car accidents in terms of age, gender, injury severity, injured body regions and hospitalization outcome in the recent four years (2011–2014).
Methods
The hospital registry was accessed at Shiraz Trauma Research Center (Shiraz, Iran) and the admission's unit data were merged with the information gathered upon discharge. A total number of 27,222 car accident patients aged over 15 years with International Classification of Diseases 10th revision (ICD-10) external causes of injury codes (V40.9-V49.9) were analyzed. Injury severity score and injured body regions were determined based on converting ICD-10 injury codes to Abbreviated Injury Scale (AIS-98) severity codes using a domestically developed electronic algorithm. A binary logistic regression model was applied to the data to examine the contribution of all independent variables to in-hospital mortality.
Results
Men accounted for 68.9% of the injuries and the male to female ratio was 2.2:1. The age of the studied population was (34 ± 15) years, with more than 77.2% of the population located in the 15–45 years old age group. Head and neck was the most commonly injured body region (39.0%) followed by extremities (27.2%). Injury severity score (ISS) was calculated for 13,152 (48.3%) patients, of whom, 80.9% had severity scores less than 9. There were 332 patients (1.2%) admitted to the intensive care units and 422 in-hospital fatalities (1.5%) were recorded during the study period. Age above 65 years [OR = 7.4, 95% CI (5.0–10.9)], ISS above 16 [OR = 9.1, 95% CI (5.5–14.9)], sustaining a thoracic injury [OR = 7.4, 95% CI (4.6–11.9)] and head injury [OR = 4.9, 95% CI (3.1–7.6)] were the most important independent predictors of death following car accidents.
Conclusion
Hospital administrative databases of this hospital could be used as reliable sources of information in providing epidemiologic reports of car accidents in terms of severity and outcomes. Improving the quality of recordings at hospital databases is an important initial step towards more comprehensive injury surveillance in Fars, Iran.
Keywords: Car accidents, Epidemiology, Injury severity score, Mortality predictors, Injury surveillance
Introduction
The World Health Organization (WHO) declared that in eastern Mediterranean region, car occupants accounted for the highest proportion of road traffic accident (RTA) fatalities in middle income countries (36%). In Iran, however, the value for car accidents reaches up to 48%, which signifies the necessity of ongoing researches focus on epidemiology of car accidents.1 With an estimated population of 74 million and more than 11.9 million registered four-wheel vehicles in 2011,2, 3 Iran was in the top 5 countries for deaths resulting from RTAs.1 Classically, motorcyclist and pedestrians have been identified as the vulnerable road users in developing countries. In the light of widespread enforcement of motorcycle safety laws in Iran, the incidents and mortalities resulting from motorcycle accidents have dropped over the recent years, which is justified by an increase in mortality rate of car accident victims.4
So far, the Iranian forensic medicine organization claims the main role in surveillance of deaths and specifically RTA mortalities in Iran.5, 6, 7 Meanwhile, hospital emergency departments play a major role following the forensic medicine organization. Considering the fact that the quality and reliability of data vary between surveillance systems8 and non-fatal car accident injuries are less likely to be covered in forensic medicine or police department surveillance systems in Iran,9 the administrative data from trauma centers could serve as potential sources of invaluable information while studying epidemiologic features of injuries.
Fars is the 4th most populous province in Iran located in the south west of the country with more than 4 million residents facing a RTA mortality rate of 42 per 100,000 population in 2011, approximately 2.5 times of the global mortality rate in the same period.5 Shahid Rajaee trauma hospital is the largest trauma referral center in Fars province, affiliated to Shiraz University of Medical Sciences.10 In this cross-sectional analysis of Shahid Rajaee hospital administrative data, we aimed to evaluate patients injured in car accidents in terms of age, gender, injury severity, injured body regions and hospitalization outcome from the year 2011–2014.
Materials and methods
This study was conducted at Shiraz Trauma Research Center affiliated to Shiraz University of Medical Sciences as a cross-sectional evaluation of car accident patients with respect to their age, gender, injury severity, injured body region and outcome of hospitalization. The study involved all referees from January 2011 to December 2014 and the main source of information was the Shahid Rajaee Hospital Information System. Two hospital registry databases were accessed in Shiraz Trauma Research Center and patients' information gathered upon admission were merged with data recruited after discharge.
Sample size and study subjects
Emergency Medical Services' (EMS) policy in Shiraz is to refer all of the RTA patients to Shahid Rajaee trauma center. Therefore, car accident cases registered to this hospital represent a powerful sample of the entire injured patients involved in car crashes in Shiraz. Inclusion criteria were adult individuals (older than 15 years) riding in any four wheeled motorized vehicle (driver or occupant) involved in an accident with International Classification of Diseases 10th revision (ICD-10) external causes of injury codes (V40.9-V49.9). We excluded patients admitted for surgical procedures other than emergency trauma intervention or those with complications of previous trauma surgeries (infection). A total number of 27,222 cases of injuries met the inclusion and exclusion criteria.
Measurements and data collection
Data collection was performed at two stages along the process of hospitalization for each patient. Upon the initial assessment in the triage and screen, the admission unit of Shahid Rajaee hospital generated a unique 8 digit number (Serial Code) which was used by all other information gathering units of the hospital. Baseline demographics of trauma patients including identifications, Serial Code, age, gender, admission and discharge date and time, length of hospitalization, and injury mechanisms were recorded at the time of admission by trained staff (24 h a day/7 days a week). Upon discharge, the hard copied records were transferred to the medical records unit, where trained staff routinely extracted information regarding external causes of the injury, the ultimate injury diagnosis, surgical interventions and final outcome. ICD-10 coding system was used to recode patients' information upon registration.
Injured body regions and severity scoring
An algorithm was developed to convert each ICD-10 rubric to its relevant Abbreviated Injury Scale (AIS-98) score where possible. The article by Hass et al11 provides details of the procedure. In summary, each injury-related ICD-10 diagnosis code was assigned to an appropriate AIS severity code (number) where possible. Conservatively, we transformed the ICD-10 diagnoses to the lowest AIS-98 severity score. In cases where the ICD-10 diagnoses could not be transformed to an accurate AIS severity score, an AIS score of 99 (missing) was used and that particular injury was not used in calculating the ISS. Specifically, in cases where the ICD-10 describes injuries to multiple or unidentified body regions, the 99 (missing) code was used (e.g., S09.7 multiple injuries of head). We also assigned each ICD-10 injury codes to 1 of 6 ISS body regions with the same procedure. Three of the most severe injuries reported for each patient were identified and each AIS code was squared and the three squared numbers were added to produce the ISS (ISS = A2 + B2 + C2 where A, B, C are the AIS scores of the three most severe injured ISS body regions). Converting ICD-10 to AIS-98 was possible for 13,152 patients (48.3% of the total).
In patients with injuries to more than one body areas, the most severely injured body region (considering AIS severity scores) was reported. If injuries were equally severe on different body regions, the patient was declared to have multiple injuries. The outcome of hospitalization was determined considering survival or death following admission. In-hospital mortality rate was therefore defined as the number of patients dying after hospital admission divided by the total number of visited patients. The proportion of mortalities occurring in the first 48 h of admission to those occurring beyond this period was also determined.
Statistical analysis
The patients' information was recruited in the form of a Microsoft Excel Spreadsheet which was imported to the SPSS software for statistical analysis. Upon the initiation of statistical inference, an alpha level of 0.05 was considered statistically significant. Normality was checked using the one sample Kolmogorov–Smirnov test in case of continuous variables (age, length of stay and ISS). Summary statistics for normally distributed continuous variables were mean and standard deviation (mean ± SD), whereas, non-normally distributed variables were summarized using the median and interquartile range (median IQR). Categorical variables were presented by frequency and percentage [n (%)] for each category. The outcome of hospitalization was considered as the dependent variable. Association of each independent baseline variable with mortality was tested using the Pearson chi-squared or the independent t-tests where appropriate. A binary logistic regression model was applied to the data to examine the contribution of all independent variables to in-hospital mortality. All of the independent variables were entered to the model simultaneously and the significance and odds ratio (OR, 95% CI) for each category of independent variables were reported. Changes of the studied population over time were analyzed using the chi-squared test for trends and the Kruskal–Wallis H test where appropriate.
Results
A total number of 27,222 injured patients in car accidents were registered from 2011 to 2014. Men accounted for 68.9% of the injuries and the male to female ratio was 2.2:1. Mean age of the studied population was (34 ± 15) years, with more than 77.2% of the patients located in the 15–45 years age group. Head and neck (39.0%) were the most commonly injured body regions followed by hip and extremities (27.2%). Victims with multiple injuries accounted for 12.7% of the total. ISS was calculated for 13,152 patients (48.3%), of whom, 80% had severity scores less than 9. There were 332 patients (1.2%) requiring intensive care and 422 in-hospital fatalities were recorded during the study period (1.5%). Detailed demographic characteristics of the studied population are reflected in Table 1.
Table 1.
Demographics of 27,222 patients injured in car accidents from 2011 to 2014.
| Demographic characteristics | (n, %) |
|---|---|
| Gender | |
| Female | 8465 (31.1) |
| Male | 18,757 (68.9) |
| Age (years) | |
| 15–24 | 8770 (32.2) |
| 25–34 | 8454 (31.1) |
| 35–44 | 3792 (13.9) |
| 45–54 | 2988 (11.0) |
| 55–64 | 1935 (7.1) |
| >65 | 1283 (4.7) |
| Injured body region (n = 27,155) | |
| Head and neck | 1063 (39.0) |
| Spinal cord & vertebral column | 936 (3.4) |
| Thorax | 1799 (6.6) |
| Abdomen, pelvis & lower back | 2946 (10.8) |
| Hip & extremities | 7404 (27.2) |
| Multiple injuries | 3467 (12.7) |
| ISS (n = 13,152) | |
| 1–3 | 3631 (27.6) |
| 4–8 | 7016 (53.3) |
| 9–15 | 374 (2.8) |
| 16–24 | 1367 (10.4) |
| >25 | 764 (5.8) |
| Length of hospital stay (d) | |
| <1 | 13,401 (49.2) |
| 1–2 | 7917 (29.1) |
| 2–7 | 3189 (11.7) |
| 7–30 | 2372 (8.7) |
| >30 | 343 (1.3) |
| ICU admission | |
| Yes | 332 (1.2) |
| No | 26,890 (98.8) |
| Outcome | |
| Survived | 26,800 (98.5) |
| Died | 422 (1.5) |
Bivariate analysis of mortality
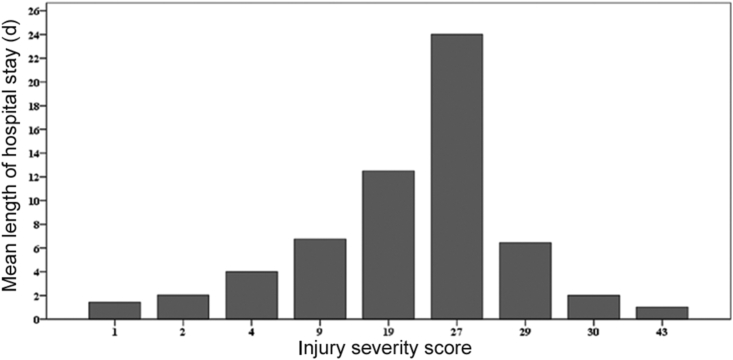
Mortality was significantly associated with age, gender, injured body region, injury severity and length of hospital stay (LOS) (all p < 0.001). Males had a crude mortality rate of 1.8% comparing to a value of 1.0% for females (p < 0.001). According to the age groups, individuals older than 65 years had the highest mortality rate (8.1%) while 15–24 year age group had the lowest value (0.8%, p < 0.001). Car accident victims sustaining head injuries accounted for the highest mortality rate, 2.4% as compared to a value of 0.6% for patients sustaining injuries to the extremities (p < 0.001). Fatal car accidents had a significantly higher injury severity as reflected by a median ISS of 9 (9–16), while the value was 5 (1–9) in the case of non-fatal injuries (p < 0.001). Although the majority of deaths occurred in less than 48 h of hospitalization (53.3%), overall non-survivors had a significantly longer LOS comparing to survivors [median LOS 2 (0–10) vs. median LOS 1 (0–2) respectively] (p < 0.001, Table 2). Fig. 1 reveals a bidirectional effect of ISS on LOS.
Table 2.
Bivariate analysis of mortality predictors (n = 27,222).
| Predictors | Outcome |
|||
|---|---|---|---|---|
| Survivors (n = 26,800) | Non-survivors (n = 422) | Total | p value | |
| Age (years) | <0.001 | |||
| 15–24 | 8696 (99.2) | 74 (0.8) | 8770 (100.0) | |
| 25–34 | 8369 (99.0) | 85 (1.0) | 8454 (100.0) | |
| 35–44 | 3746 (98.8) | 46 (1.2) | 3792 (100.0) | |
| 45–54 | 2935 (98.2) | 53 (1.8) | 2988 (100.0) | |
| 55–64 | 1875 (96.9) | 60 (3.1) | 1935 (100.0) | |
| >65 | 1179 (91.9) | 104 (8.1) | 1283 (100.0) | |
| Gender | <0.001 | |||
| Female | 8377 (99.0) | 88 (1.0) | 9149 (100.0) | |
| Male | 18,423 (98.2) | 334 (1.8) | 20,448 (100.0) | |
| Injured body region (n = 27,155) | <0.001 | |||
| Head and neck | 10,347 (97.6) | 256 (2.4) | 10,603 (100.0) | |
| Spinal cord & vertebral column | 919 (98.2) | 17 (1.8) | 936 (100.0) | |
| Thorax | 1761 (97.9) | 38 (2.1) | 1799 (100.0) | |
| Abdomen, pelvis & lower back | 2908 (98.7) | 38 (1.3) | 2946 (100.0) | |
| Hip & extremities | 7363 (99.4) | 41 (0.6) | 7404 (100.0) | |
| Multiple injuries | 3437 (99.1) | 30 (0.9) | 3467 (100.0) | |
| ISS (n = 13,152)a | 5 (1–9) | 9 (9–16) | 5 (1–9) | <0.001b |
| Length of hospital staya | 1 (0–2) | 2 (0–10) | 1 (0–2) | <0.001b |
| ICU admission | <0.001 | |||
| Yes | 122 (36.7) | 210 (63.3) | 332 (100.0) | |
| No | 26,678 (99.2) | 212 (0.8) | 26,890 (100.0) | |
Values are expressed as n (%) unless stated otherwise.
Summary statistics are median and interquartile range.
Mann Whitney U two sided asymptotic significance.
Fig. 1.
Mean length of hospital stay by injury severity score.
Regression analysis of in-hospital mortality
A binomial logistic regression model was employed to obtain a realistic estimate of mortality risk. Age, gender, injured body region, ISS, and LOS were the predictors and mortality was the dependent variable. Age, gender and injured body region and ISS were entered as categorical predictors with proper dummy coding while LOS was considered as a continuous predictor. Considering the missing information for ISS and injured body region, there were only 13,136 (48.3%) patients included in the regression analysis. Table 3 reflects the regression coefficients and odds ratios for predictors included in the model. The most important risk factors of death, as reflected by higher Wald statistics, were age above 65 years [OR = 7.4, 95% CI (5.0–10.9)], ISS above 16 [OR = 9.1, 95% CI (5.5–14.9)], sustaining a thoracic injury [OR = 7.4, 95% CI (4.6–11.9)] or a head injury [OR = 4.9, 95% CI (3.1–7.6)].
Table 3.
Logistic regression coefficients and odds ratios for predictors of mortality among car accident patients.
| Predictors | Ba | S.E.b | Waldc | Dfd | p value | OR (95% CI)e |
|---|---|---|---|---|---|---|
| Gender | <0.001 | |||||
| Female | – | – | – | – | – | 1 |
| Male | 0.51 | 0.15 | 11.58 | 1 | <0.001 | 1.67 (1.24–2.24) |
| Age | 143.98 | 5 | <0.001 | |||
| 15–24 | – | – | – | – | – | 1 |
| 25–34 | 0.25 | 0.19 | 1.70 | 1 | 0.19 | 1.28 (0.88–1.85) |
| 35–44 | 0.34 | 0.23 | 2.24 | 1 | 0.13 | 1.40 (0.89–2.20) |
| 45–54 | 0.60 | 0.23 | 7.05 | 1 | <0.001 | 1.81 (1.16–2.82) |
| 55–64 | 1.16 | 0.22 | 29.11 | 1 | <0.001 | 3.20 (2.09–4.88) |
| >65 | 2.00 | 0.20 | 104.58 | 1 | <0.001 | 7.37 (5.02–10.8) |
| Injured body region | 83.26 | 4 | <0.001 | |||
| Hip & extremities | – | – | – | – | – | 1 |
| Head & neck | 1.59 | 0.23 | 50.01 | 1 | <0.001 | 4.92 (3.16–7.66) |
| Spinal cord & vertebral column | 0.49 | 0.37 | 1.78 | 1 | 0.18 | 1.62 (0.79–3.33) |
| Thorax | 2.00 | 0.24 | 67.94 | 1 | <0.001 | 7.42 (4.60–11.9) |
| Abdomen, pelvis & lower back | 1.40 | 0.25 | 32.05 | 1 | <0.001 | 4.05 (2.49–6.58) |
| ISS | 81.45 | 3 | <0.001 | |||
| 1–3 | – | – | – | – | – | 1 |
| 4–8 | 1.42 | 0.31 | 20.53 | 1 | <0.001 | 4.13 (2.23–7.63) |
| 9–15 | 1.93 | 0.27 | 52.70 | 1 | <0.001 | 6.91 (4.10–11.6) |
| 16–75 | 2.21 | 0.25 | 75.38 | 1 | <0.001 | 9.08 (5.52–14.9) |
| Length of hospital stay | 0.02 | 0.00 | 43.99 | 1 | <0.001 | 1.02 (1.01–1.03) |
| Constant | −7.64 | 0.35 | 478.22 | 1 | <0.001 |
Regression coefficient.
Standard error of the regression coefficient.
Ration of the squared regression coefficient to the squared standard error.
Degrees of freedom.
Odds ratios and 95% confidence intervals.
Time trends
From the year 2011–2014, we experienced an increasing trend for incidence of traumatic brain injury (TBI) while sex ratios, ISS, LOS, ICU admission rate, in-hospital mortality and deaths within 48 h showed a decreasing pattern. All changes were significant at 0.05 level (see Table 4).
Table 4.
Trends of TBI incidence, ISS, length of hospital stay (LOS) and outcomes during the study period.
| Variables | Years |
|||||
|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | Total | p value | |
| Frequency of admission | 1936 | 6673 | 8739 | 9874 | 27,222 | |
| Sex ratio | 2.72 | 2.22 | 2.21 | 2.12 | 2.21 | <0.001a |
| TBI incidence | 533 (27.5) | 2195 (32.9) | 3272 (37.1) | 3068 (31.1) | 9068 (33.3) | <0.001a |
| ISS (median [IQR]) | 9 (4–9) | 9 (1–9) | 4 (1–9) | 4 (1–9) | 5 (1–9) | <0.001b |
| LOS (median [IQR]) | 3 (1–8) | 1 (0–2) | 0 (0–1) | 0 (0–1) | 1 (0–2) | <0.001b |
| ICU admission rate | 69 (3.6) | 92 (1.4) | 89 (1.0) | 82 (0.8) | 332 (1.2) | <0.001a |
| Mortality rate | 92 (4.8) | 112 (1.7) | 109 (1.2) | 109 (1.1) | 422 (1.6) | <0.001a |
| Proportion of deaths within 48 h | 46 (50.0) | 58 (51.7) | 62 (56.8) | 60 (55.1) | 226 (53.5) | <0.001b |
Values are represented as n (%) unless stated otherwise.
Chi-squared test for trend.
Kruskal–Wallis test in comparing mean ranks.
Discussion
Over the recent years, the Iranian population has experienced a change in the pattern of RTAs as car accidents comprise the majority of cases now. Epidemiologic studies in Iran have mainly focused on fatal injuries considering all motor vehicle accidents. Little attention has been paid to nonfatal injuries specifically regarding car accidents. In this retrospective study, we used the Shahid Rajaee hospital administrative data to build a report on injuries resulting from car accidents in Shiraz from the year 2011–2014. We reported a sex ratio of 2.2:1 among victims of car accidents with a decreasing pattern from 2.72 in 2011 to 2.12 in 2014. Such a little change in a large population as in our study, is worthy of note since it implies an increasing incidence of car accidents among women. In preceding years, studies from around the country have reported relatively higher sex ratios among car crash patients, which further signifies this decreasing trend.12, 13, 14 This finding may be explained through the fact that over time, more women are actively involved in outdoor activities including driving and even driving as an occupation.
Sex ratio in RTAs is a general terminology since it could refer to various conditions including being involved only in a RTA and not being injured, being involved in a RTA and sustaining some degrees of injuries and even being involved and suffering a fatal injury at the scene. It should be mentioned that we specifically reported the M/F ratio among those who sustained at least one injury in a car accident. Gender was associated with mortality and it was a significant predictor of mortality, however, sex was not a potent predictor after adjusting for covariates. Our findings are in agreement with results of large studies of trauma patients indicating that males suffer a higher risk of mortality after adjusting for multiple covariates.15 Female sex hormones, which reduce susceptibility to developing life threatening complications, are known to be responsible for this survival advantage compared to equivalently injured men.
Car occupants studied in this study aged (34 ± 14) years on average, which lies in agreement with previous studies in the region, emphasizing the 15–45 years old group as the most commonly involved in 4 wheeled vehicle crashes.16, 17, 18 On the global scale, the United States and European Union have reported an average age of 38.2 years and 38.5 years for car occupants being injured in traffic accidents.19 This little difference is not of clinical relevance however. Although the elderly comprised the smallest proportion of car accident patients, death rate was the highest in this age group. After controlling for confounders, individuals older than 45 years had a statistically higher risk of death comparing to 15–24 year olds. This lies in agreement with the existing literature4 and may be explained by the relatively lower physiologic reserve and higher prevalence of preexisting medical conditions among the elderly.20
Car accident victims sustaining head injuries had the highest mortality rate (2.4%). Regression analysis also reflected a 4.9 times risk of death for the head injured comparable to the existing literature in Iran21, 22 and throughout the world.23 It is worth to note that sustaining a thoracic injury increased the odds of death far more than head injuries did. This finding may be explained through the fact that major head injuries cause death immediately on the scene, preventing a case to be registered in hospital records.23 Meanwhile, patients with serious thoracic injuries survive long enough to reach the hospital care but expire early after hospitalization. We experienced an increasing trend of incidence for head injuries from 27.5% to 31.1% during the study period, however, the overall mortality rate decreased. This finding may be explained through the fact that, since the enforcement of mandatory seatbelt law in 2011, seatbelt usage has increased steadily among car users in Iran resulting in less severe or fatal head injury in a car accident.24 Nonetheless, rapid motorization in our community along with inadequate traffic education and slow implementation of safety regulations may be contributors of increased head injury incidence observed here. Another explanation involves the increasing trend in referring all cause trauma patients to this center in Shiraz.
Herein, ISS was calculated based on converting ICD-10 injury codes to AIS-98 severity codes using a domestically developed electronic algorithm discussed in details above. Strong evidence exists in support of such population-based ISS calculation method.11, 25 The injured car accident patients had a median ISS of 5 (1–9) indicative of an overall minor severity. This is comparable to a value of 6 reported by Abbasi et al26 and 7 by Eftekhar et al,21 both of whom used the medical records directly to calculate the ISS. Although some authors have questioned the role of ISS in predicting trauma associated mortalities, the majority of existing studies in trauma literature consent on its significant role.27 Since its introduction in 1974 with little modifications in 1997, ISS has maintained its popularity among trauma researchers as a predictor of trauma outcome. Nonetheless, there are only two published studies21, 28 addressing the severity of injuries in trauma victims on a large scale in Iran, both of which were conducted in Tehran. Our results indicated that non-survivors had a significantly higher ISS and even after adjusting for age, gender, injured body regions and LOS, ISS remains a significant predictor of mortality among car crashers which is in accordance with previous reports.17, 22 In addition, it should be noted that from the year 2011–2014, we faced a significant reduction in ISS which was associated with significant decreases in LOS, ICU admission rate and overall in-hospital mortality rate during the same period. This finding supports the use of ICD-10 derived ISS in predicting the outcomes of hospitalization in car accident victims. Yet, the change in severity of injuries experienced at Shahid Rajaee hospital should be considered as another explanation for the decreasing trend of mortality. In preceding years, only critically injured patients with higher injury severity were transferred to this center, however, over time Shahid Rajaee hospital is becoming the referral center for all traffic related accidents of any severity.
Another aspect of in-hospital mortality of car accident patients yet to be discussed is around the relationship between injury severity and LOS with respect to mortality. We showed that non-survivors had significantly higher ISS and LOS (Table 2), meanwhile, ISS exerts a bidirectional effect on LOS (Fig. 1). Up to a value of 27, an increase in ISS results in a steady increase in LOS since recovery from injury with higher severity takes more time. Beyond this point, however, the LOS decreases dramatically since this extent of injuries results in early death with medical care being frequently ineffective. At the same time, we experienced a significant 1.01% increase in mortality risk as a result of each one day increase in LOS. This might be interpreted in the context of a higher chance of developing infectious complications in case of extended hospitalization following trauma.
While analyzing the in-hospital mortality rate, one should consider the proportion of mortalities occurring early after hospitalization. It is worthy of note that definition of early death following a car accident varies considerably across trauma centers. The majority consent on a 24 h period as the cut off, while some authors have used longer intervals (48 or 72 h following trauma).23 In our center, 53.5% of mortalities occurred within 48 h of admission (early death). This is in agreement with findings of other studies.23, 29 From 2011 to 2014, the proportion of deaths occurring within 48 h of admission increased significantly from 50% to 57%. Considering the simultaneous decreasing trend of ISS and overall mortality from car accidents over the recent years, we emphasize the role of pre-hospital determinants of mortality (vehicle speed, seatbelt use, vehicle safety standards, ISS, injury mechanism, duration of transportation to hospital) being more pronounced in deaths occurring within 48 h of hospital admission comparing to those occurring beyond this window.23, 30 With precautions therefore, we conclude that timing of in-hospital trauma mortality may also be used as an index of the in-hospital trauma quality of care. The majority of deaths occurring later imply lower quality of care. The observed shift in timing of mortality therefore indicates improving of quality of care in Shahid Rajaee hospital from 2011 to 2014. In this study we were able to analyze the possible contribution of age, gender, injury severity, injured body region and LOS to mortality. In future studies, host factors, injury severity, time to definite care and quality of care should be considered as important predictors.
Information on crash site was not available in this study since the only source of information was the hospital trauma registry. Further, the incidence and prevalence of car accidents and relative morbidities were not provided since it would result in an underestimation of the incidence. Using the ICD-10 derived ISS scores might be interpreted as a limitation in that the conversion process might not provide accurate ISS as calculated directly from medical records. In addition, not all ICD-10 codes were translatable to AIS severity codes which resulted in missing values of ISS for more than 50% of the total. However, this method provides good information on injury severity that might otherwise be unavailable. A study population of more than 27,000 records is large enough to reveal major trends. It is proposed that trauma registry at Shahid Rajaee hospital could be improved through education of physicians while describing injuries. Finally, it is known that car accidents comprise a significant proportion of RTAs which itself is the third cause of death in Iran. Nonetheless, considerable variation exists among responsible organizations (police departments, legal medicine organizations and trauma centers) while reporting car accident statistics which in turn, makes the results incomparable across these organizations and prevents the authorities to draw meaningful conclusions.31 A comprehensive trauma registry approach with the assistance of forensic medicine organizations and police departments will not only improve the quality of epidemiologic studies of car accidents in Fars, but also significantly contributes to develop preventive strategies and provide better quality of care.
In conclusion, among car accident victims referred to Shahid Rajaee hospital, sustaining thoracic/head injury, age above 65 years and ISS above 16 are the most important independent predictors of death. The in-hospital mortality rate, however, should be viewed with caution since pre-hospital determinants along with host factors are important predictors. The hospital administrative databases in this center could be used as reliable sources of information in trauma epidemiology. Improving the quality of recordings upon admission and discharge may be important initial steps towards more comprehensive injury surveillance in Fars and Iran.
Acknowledgments
The authors would like to appreciate the contribution of deputy dean of School of Medicine and sponsorship of deputy chancellor of Shiraz University of Medical Sciences. This project was funded by Shiraz University of Medical Sciences in the context of a thesis project supervise by Dr. Mahnaz Yadollahi (No. 9301388562, dated 1/31/2015).
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.World Health Organization . World Health Organization; 2013. Global Status Report on Road Safety 2013: Supporting a Decade of Action.http://www.who.int/violence_injury_prevention/road_safety_status/2013/en/ [Google Scholar]
- 2.Statistical center of Iran . 2013. Iran statistical Yearbook 1392.https://www.amar.org.ir/Portals/1/yearbook/1392/3.pdf Report of the 2011 Census of Housing and Population of Iran. Tehran. [Google Scholar]
- 3.Soori H., Hussain S.J., Razzak J.A. Road safety in the eastern Mediterranean region–findings from the global road safety status report. East Mediterr Health J. 2011;17:770–776. doi: 10.26719/2011.17.10.770. [DOI] [PubMed] [Google Scholar]
- 4.Bhalla K., Naghavi M., Shahraz S. Building national estimates of the burden of road traffic injuries in developing countries from all available data sources: Iran. Inj Prev. 2009;15:150–156. doi: 10.1136/ip.2008.020826. [DOI] [PubMed] [Google Scholar]
- 5.Heydari S., Hoseinzadeh A., Ghaffarpasand F. Epidemiological characteristics of fatal traffic accidents in Fars province, Iran: a community-based survey. Public health. 2013;127:704–709. doi: 10.1016/j.puhe.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Mohammadi G. Road traffic fatalities among pedestrians, bicyclists and motor vehicle occupants in Sirjan, Kerman. Iran Chin J Traumatol. 2009;12:200–202. [PubMed] [Google Scholar]
- 7.Peymani P., Heydari S.T., Hoseinzadeh A. Epidemiological characteristics of fatal pedestrian accidents in Fars Province of Iran: a community-based survey. Chin J Traumatol. 2012;15:279–283. [PubMed] [Google Scholar]
- 8.McKenzie K., Enraght-Moony E.L., Walker S.M. Accuracy of external cause-of-injury coding in hospital records. Inj Prev. 2009;15:60–64. doi: 10.1136/ip.2008.019935. [DOI] [PubMed] [Google Scholar]
- 9.Moafian G., Aghabeigi M.R., Heydari S.T. An epidemiologic survey of road traffic accidents in Iran: analysis of driver-related factors. Chin J Traumatol. 2013;16:140–144. [PubMed] [Google Scholar]
- 10.Yadollahi M., Paydar S., Sabetianfard Jahromi G. Types and causalities in dead patients due to traumatic injuries. Arch Trauma Res. 2015;4:e26028. doi: 10.5812/atr.26028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haas B., Xiong W., Brennan-Barnes M. Overcoming barriers to population-based injury research: development and validation of an ICD10-to-AIS algorithm. Can J Surg. 2012;55:21–26. doi: 10.1503/cjs.017510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasouli M.R., Saadat S., Haddadi M. Epidemiology of injuries and poisonings in emergency departments in Iran. Public Health. 2011;125:727–733. doi: 10.1016/j.puhe.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Roudsari B.S., Sharzei K., Zargar M. Sex and age distribution in transport-related injuries in Tehran. Accid Anal Prev. 2004;36:391–398. doi: 10.1016/S0001-4575(03)00032-0. [DOI] [PubMed] [Google Scholar]
- 14.Mohammadzadeh M., Paravar M., Mirzadeh A.S. Seat belt usage in injured car occupants: injury patterns, severity and outcome after two main car accident mechanisms in Kashan, Iran, 2012. Arch Trauma Res. 2015;4:e22203. doi: 10.5812/atr.22203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu T., Xie J., Yang F. The influence of sex on outcomes in trauma patients: a meta-analysis. Am J Surg. 2015;210:911–921. doi: 10.1016/j.amjsurg.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Barrimah I., Midhet F., Sharaf F. Epidemiology of road traffic injuries in qassim region, Saudi Arabia: consistency of police and health data. Int J Health Sci (Qassim) 2012;6:31–41. doi: 10.12816/0005971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eid H.O., Abu-Zidan F.M. New injury severity score is a better predictor of mortality for blunt trauma patients than the injury severity score. World J Surg. 2015;39:165–171. doi: 10.1007/s00268-014-2745-2. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . 2013. Road Safety in the Eastern Mediterranean Region: Facts from the Global Status Report on Road Safety.http://applications.emro.who.int/dsaf/EMROPUB_2013_EN_1429.pdf [Google Scholar]
- 19.National Highway Traffic Safety Administration . US Department of Transportation, National Highway Traffic Safety Administration; Washington, DC: 2015. Traffic Safety Facts 2013 Data – Pedestrians.http://www-nrd.nhtsa.dot.gov/Pubs/812124.pdf Publication No. DOT-HS-812–124. [cited 2015 Feb 17]. Available at: Accessed February 17, 2016. [Google Scholar]
- 20.Hashmi A., Ibrahim-Zada I., Rhee P. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2014;76:894–901. doi: 10.1097/TA.0b013e3182ab0763. [DOI] [PubMed] [Google Scholar]
- 21.Eftekhar B., Zarei M.R., Ghodsi M. Comparing logistic models based on modified GCS motor component with other prognostic tools in prediction of mortality: results of study in 7226 trauma patients. Injury. 2005;36:900–904. doi: 10.1016/j.injury.2004.12.067. [DOI] [PubMed] [Google Scholar]
- 22.Moini M., Rezaishiraz H., Zafarghandi M.R. Characteristics and outcome of injured patients treated in urban trauma centers in Iran. J Trauma. 2000;48:503–507. doi: 10.1097/00005373-200003000-00023. [DOI] [PubMed] [Google Scholar]
- 23.Sobrino J., Shafi S. Timing and causes of death after injuries. Proc (Bayl Univ Med Cent) 2013;26:120–123. doi: 10.1080/08998280.2013.11928934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Soori H., Nasermoadeli A., Ainy E. Association between mandatory seatbelt laws and road traffic injuries in Iran. Southeast Asian J Trop Med Public Health. 2011;42:1540–1545. [PubMed] [Google Scholar]
- 25.Tohira H., Jacobs I., Mountain D. Validation of a modified table to map the 1998 abbreviated Injury Scale to the 2008 scale and the use of adjusted severities. J Trauma. 2011;71:1829–1834. doi: 10.1097/TA.0b013e31823cc5c5. [DOI] [PubMed] [Google Scholar]
- 26.Abbasi H.R., Mousavi S.M., Akerdi A.T. Pattern of traumatic injuries and injury severity score in a major trauma center in Shiraz, southern Iran. Bull Emerg Trauma. 2013;1:81–85. [PMC free article] [PubMed] [Google Scholar]
- 27.Schluter P.J. The trauma and injury severity score (TRISS) revised. Injury. 2011;42:90–96. doi: 10.1016/j.injury.2010.08.040. [DOI] [PubMed] [Google Scholar]
- 28.Zargar M., Modaghegh M.-H.S., Rezaishiraz H. Urban injuries in Tehran: demography of trauma patients and evaluation of trauma care. Injury. 2001;32:613–617. doi: 10.1016/s0020-1383(01)00029-8. [DOI] [PubMed] [Google Scholar]
- 29.Abdelrahman H., El-Menyar A., Al-Thani H. Time-based trauma-related mortality patterns in a newly created trauma system. World J Surg. 2014;38:2804–2812. doi: 10.1007/s00268-014-2705-x. [DOI] [PubMed] [Google Scholar]
- 30.Gunst M., Ghaemmaghami V., Gruszecki A. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent) 2010;23:349–354. doi: 10.1080/08998280.2010.11928649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hatamabadi H.R., Vafaee R., Haddadi M. Necessity of an integrated road traffic injuries surveillance system: a community-based study. Traffic Inj Prev. 2011;12:358–362. doi: 10.1080/15389588.2011.566656. [DOI] [PubMed] [Google Scholar]