Abstract
Purpose
Maxillofacial injuries are frequently associated with multiple trauma and can determine functional and aesthetic bad outcomes. The severity of maxillofacial injuries may be considerable and can divert clinicians' attention from other concomitant injuries which is less evident but potentially life-threatening. The aim of this study was to find out the concomitant injuries in patients referred to the Emergency Department (ED) of the University Hospital of Messina (North-East Sicily, Italy) for maxillofacial traumas.
Methods
We retrospectively evaluated data of 240,833 patients admitted at the ED of the University Hospital of Messina from January 2008 to December 2015 because of maxillofacial injuries leading to hospitalization and surgical treatment. Patients who primarily received treatment care at different institutions, pediatric trauma patients and adult patients who were transferred in accordance with pre-existing agreements in case of paucity of beds were excluded. Finally we included 447 (0.2%) patients over the 8 years. Data were evaluated with emphasis on epidemiology (age, gender, mechanism of trauma), primary survey and abnormalities and pattern of trauma.
Results
The most frequent cause of maxillofacial trauma was road accidents (319 patients, 71.4%), among which motorcycle ones were prevalent. The maxillofacial injured who presented major lesions were 98 patients and minor lesions occurred in 349 patients; 443 (99.1%) patients underwent maxillofacial surgery, immediate or delayed depending on the severity of concomitant injuries (χ2 = 557.2, p < 0.0001). Five concomitant neglected lesions were found to be associated with severe maxillofacial traumas (χ2 = 17.13, p < 0.0001 vs minor lesions). All of the neglected lesions occurred in paucisymptomatic patients who showed painless abdomen, no hemodynamic instability, no signs of hematoma of anterior and posterior abdominal wall or other suspicious clinical signs and symptoms.
Conclusion
Among the patients admitted firstly in other surgical wards different from the Maxillofacial Surgery Unit, diagnosis was more difficult, especially for blunt abdominal traumas, in which patients showed only vague and nonspecific symptoms concealing serious and life-threatening injuries. We recommend the routine use of whole body CT scan, when the maxillofacial injuries appear prevalent, mainly in patients affected by maxillofacial major lesions.
Keywords: Maxillofacial injuries, Concomitant lesions, Multiple trauma, Emergency department
Introduction
In western countries, trauma is the first leading cause of death before the 4th decade of life, as well as the third major cause in patients over 40 years old, being preceded only by cardiovascular diseases and neoplasms.1, 2 Maxillofacial injuries are frequently associated with multiple trauma, and may cause functional and aesthetic bad outcomes, because of the frequency of permanent deficits and potentially disfiguring scars that can dramatically affect patient's quality of life. These traumas are often complicated by traumatic brain injuries and/or serious facial substance loss.3 Fractures involving the middle and upper third of the face are more frequent compared to mandibular ones. The former are classified according to Le Fort (in type I or horizontal maxillary fracture, type II or pyramidal fracture, and type III or craniofacial disjunction), whereas the latter can be isolated or associated with lesions of the inferior alveolar ridge.4, 5, 6
In the worldwide literature, epidemiological data vary mainly according to different geographical areas, e.g. hospitals located in mountain areas of Central-Northern Europe and India report a broader series of cases.7, 8, 9 Diagnostic accuracy together with type and timing of treatments significantly affect the clinical evolution of such traumas, allowing to improve functional results and limit cosmetic damages. Interestingly, the severity of maxillofacial injuries may be considerable, and can divert clinicians' attention from other concomitant injuries that are less evident but potentially life-threatening.10, 11, 12, 13 The aim of this study was to find out the concomitant injuries in patients admitted for maxillofacial traumas to the Emergency Department (ED) of the University Hospital Messina (North-East Sicily, Italy).
Materials and methods
From January 2008 to December 2015, the data of 240,833 patients admitted at our ED because of maxillofacial injuries leading to hospitalization and surgical treatment were retrospectively evaluated. In our University Hospital, all index admission records, investigations and follow-up records are traceable from a single unique identification number, greatly facilitating research activities on the database.
Patients who primarily received treatment care at different institutions were not included. Pediatric trauma patients were excluded. Moreover, adult patients who were transferred in accordance with pre-existing agreements in case of paucity of beds were not included in this study. Applying the above criteria, we included 447 (0.2%) patients over the 8 years. Data were evaluated with emphasis on epidemiology (age, gender, mechanism of trauma), primary survey and abnormalities and pattern of trauma. Each patient record was individually reviewed. Follow-up information of patients was as much retrieved as available in records. Patients lost to follow-up were not contacted by telephone/by post due to logistic reasons.
All patients recruited were classified distinguishing the maxillofacial injuries, isolated or multiple, in major (e.g.: Le Fort type I, II, III and mandibular fractures) or minor lesions (e.g. involving orbital floor, zygomatic, maxillary sinus and antral wall, nasal and alveolar ridge). Mandibular fractures were considered separately when involving the anterior (symphyseal and parasymphyseal), middle (body) and posterior (condylar process, head, angle and ramus) portion. When fractures were multiple, the most severe one was considered in order to categorize the patient.
All patients were assessed at the ED, according to the Advanced Trauma Life Support guidelines and diagnosed by means of a multislice computed tomography (CT) of brain and face. CT examination was extended to the spine, neck, chest and abdomen (CT was injected for the study of chest and abdomen) when multiple simultaneous injuries occurred and/or integrated with targeted X-ray of selected skeletal region, routine laboratory tests and ultrasound scan. Furthermore, American Society of Anaesthesiologists' (ASA) classification of Physical Health, a routinely used system to predict the perioperative morbidity and mortality, was assessed in all the surgical patients as grading system for preoperative health.14 The distribution of ASA score was ASA1 (n = 86), ASA2 (n = 255), ASA3 (n = 91), ASA4 (n = 11) and ASA5 (n = 4). For all the 447 patients, 328 (73.4%) were directly admitted to the Maxillofacial Surgery Unit and underwent bone synthesis by use of screws and plates and/or autologous bone grafts; while the remaining 119 patients, who underwent a delayed maxillofacial treatment for concomitant serious injuries, were hospitalized and previously managed (115/119, 96.6%) in other wards, e.g. 49 in neurosurgery (for severe brain and spine injuries), 31 in thoracic (for sever chest trauma with or without pneumothorax), 27 orthopedic (for complex fractures), 9 in general surgery (for hemoperitoneum, spleen and liver injuries), and 3 intensive care unit (for coma or severe respiratory distress), respectively.
Results were expressed as mean ± standard deviation (SD). The chi-square (χ2) test was used to analyze categorical data. The level for statistical significance was set at p < 0.05. Statistical analysis was performed using SPSS version 21.
Results
Among the 447 patients, 383 (85.7%) were males aged (34.6 ± 14.1) years, and 64 (14.3%) were females aged (47.4 ± 19.6) years (p < 0.001 vs male group). The most frequent cause of maxillofacial trauma was road accidents, and among these, motorcycle ones were prevalent. Other causes and general data of patients are shown in Table 1.
Table 1.
General data of the 447 patients with maxillofacial injuries.
| Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 383 (85.7) |
| Female | 64 (14.3) |
| Age: mean ± SD, range (years) | |
| Male | 34.6 ± 14.1, 16–78 |
| Female | 47.4 ± 19.6, 18–89 |
| Injury mechanism | |
| Road accidents | 319 (71.4) |
| Accidental falls | 87 (19.5) |
| Workplace injuries | 23 (5.1) |
| Violencea | 18 (4.0) |
| Injury type | |
| Associated lesion | 358 (80.1) |
| Isolated lesion | 89 (19.9) |
| Major lesions | 98 (21.9) |
| Le Fort type I | 2 (0.4) |
| Mandibular fractures | 96 (21.5) |
| Minor lesions | 349 (78.1) |
| Nasal fractures | 117 (26.2) |
| Orbital floor fractures | 108 (24.2) |
| Maxillary fractures | 57 (12.7) |
| Zygomatic fractures | 54 (12.1) |
| Alveolar fractures | 12 (2.7) |
| Facial crash | 1 (0.2) |
| Maxillofacial surgery | 443 (99.1) |
| Neglected concomitant lesions | 5 (1.1) |
| Splenic fractures | 3 (0.7) |
| Kidney injury | 1 (0.2) |
| Pelvic fracture | 1 (0.2) |
Distribution of gender showed significant difference (p < 0.001). Differences between proportions of patients undergoing immediate or delayed maxillofacial surgery based on major or minor lesions reached statistical significance (χ2 = 557.2, p < 0.0001); moreover, proportions of concomitant lesions were significantly different between major and minor lesions groups (χ2 = 17.13, p < 0.0001).
One patient was the victim of a gunshot wound. Four patients died before maxillofacial surgical treatment.
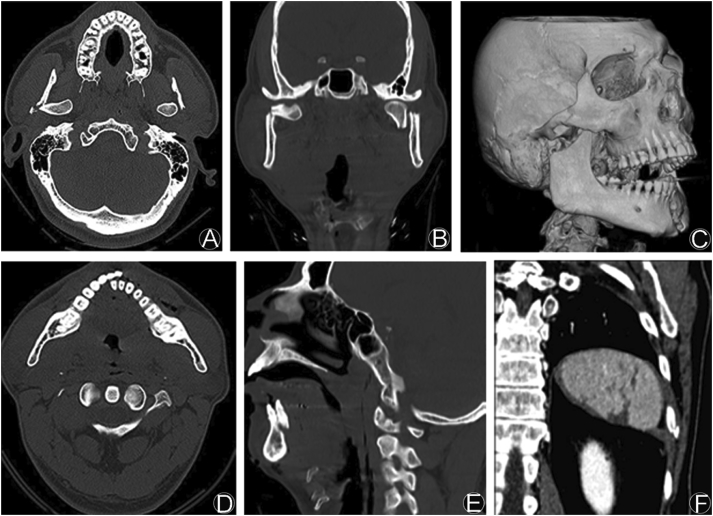
Lesions were associated in 358 (80.1%) cases, more frequently with traumatic brain injury or polytrauma, or isolated in 89 (19.9%) cases. In this study, maxillofacial injured patients presented major lesions were 98 patients (Fig. 1A–E) and minor ones were 349 patients. In detail, the former group included 2 Le Fort type I and 96 mandibular fractures (45 involving the posterior segment, 32 the anterior, and 19 the middle, respectively), whereas the latter included 117 nasal, 108 orbital floor, 57 maxillary, 54 zygomatic (Fig. 2), and 12 alveolar fractures. In only one case a “facial crash” was observed; this condition is a well-known lesion characterized by the simultaneous involvement of almost all facial bones (Table 1). In 66 (14.8%) patients a cutaneous involvement (i.e. wounds, hematoma, lacerations and abrasion) occurred and a careful debridement was necessary; nevertheless, aesthetic results did not worsen. Twelve patients required an orotracheal intubation at ED for acute obstruction or damage of the upper airways. Overall, no early mortality (within 48 h) was observed; however, four patients (0.9%) died before maxillofacial surgical treatment.
Fig. 1.
Complex and multiple mandibular fractures in a 33-year old Italian male, victim of a motorcycle accident. A and B: Bilateral avulsion of condylar processes, axial and coronal views; C, D and E: Displaced symphyseal fracture involving the alveolar ridge, 3D reconstruction, axial and sagittal views. F: The same patient had Grade IV laceration of the spleen (coronal view) requiring urgent splenectomy, which was neglected.
Fig. 2.
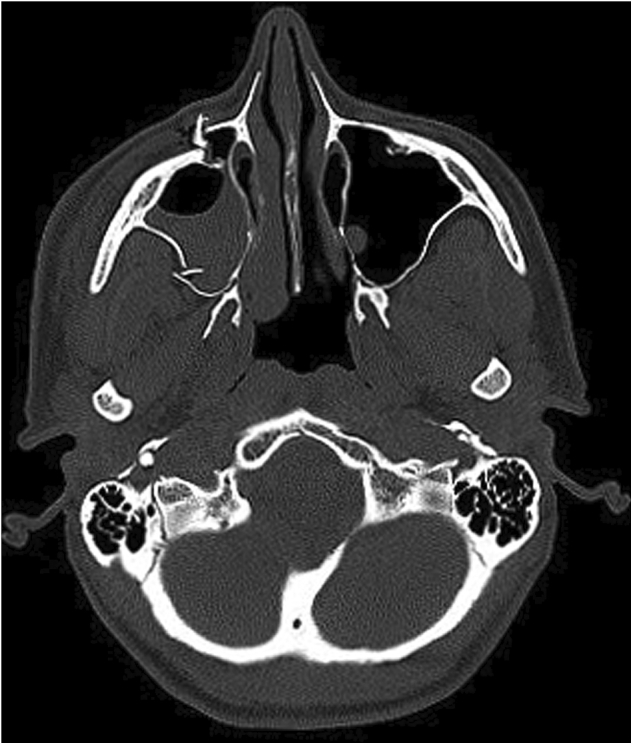
Right zygomaticomaxillary complex fracture in a 39-year old Belarusian female, victim of domestic violence.
Overall, 443 (99.1%) patients underwent maxillofacial surgery, immediate or delayed depending on the severity of concomitant injuries: considering the proportion of patients classified in major and minor lesions, a significant statistical difference was found (χ2 = 557.2, p < 0.0001).
In detail, 5 concomitant lesions that associated to severe maxillofacial traumas were nearly neglected, including 3 splenic fractures (Fig. 1F), 1 kidney injury and 1 pelvic fracture with active bleeding (χ2 = 17.13, p < 0.0001 vs minor lesions); all cases occurred in paucisymptomatic patients, who showed painless abdomen, no hemodynamic instability, no signs of hematoma of anterior and posterior abdominal wall or other suspicious clinical signs and symptoms.
Discussion
Maxillofacial injuries may occur isolated or, more frequently, associated with simultaneous injuries elsewhere. The missed concomitant lesions are reported in the literature up to 22%.15, 16 When a maxillofacial trauma occurred in a multiple injured patient, obviously the facial and brain CT was extended to spine, neck, chest and abdomen, which allows a more precise diagnosis of potential life-threatening underestimated organ lesions.
In our experience, among the patients admitted firstly in other surgical wards different from the Maxillofacial Surgery Unit, diagnosis was more difficult, especially for blunt abdominal traumas, in which patients showed only vague and nonspecific symptoms concealing serious and life-threatening injuries. Furthermore, we observed a penetrating neck wound involving the contralateral orbital floor, favorably managed by a multidisciplinary approach.17
In the present study, it was found that the incidence was significantly higher in males (86%) as compared to females (14%). This is coincidence with Sohns et al's study18 on 784 patients, which noticed that the incidence of facial fractures was 64% in males and 36% in females. It has been shown in previous studies that in developing countries, the most common mode of injury is road traffic accidents.19, 20 In developing nations, the bad maintenance of roads, poor driving skills, lack of enforcement of traffic rules and regulations such as the use of seat belts and helmets are probable reasons responsible for extensive maxillofacial fractures. In developed nations, assault is the most common cause.21 In more recent literature, the most frequently reported cause of maxillofacial trauma is road accident, concerning patients aged between 20 and 40 years, and males.22, 23, 24, 25, 26 Males present a greater risk of involvement due to the daily-life activities, e.g. driving car, heavy work conditions, sports with physical contact.27, 28, 29, 30 In particular, the leading cause of trauma in our series was represented by motorcycle accidents. Therefore, the reduction of such traumatic events can be obtained only by an insistent traffic education program and the routine use of craniofacial protection.31, 32 Moreover, in our opinion, the highest frequency of facial fractures in the 3rd–4th decades of life is related to the most intense phase of life.
The particularity of the maxillofacial trauma, which is often burdened by functional deficits and disabling aesthetic sequelae, leads to underline the need for a greater social commitment in order to achieve, in the next decades, a reduction of the incidence of this disease: a particularly complex and expensive disease for the National Health System. On the other hand, medical personnel in trauma centres in several countries have realised that undiagnosed injuries are common and are now focusing their attention on reducing the incidence of these injuries. To avoid missed injuries, re-evaluating patients 24 h after admission by means of an anamnesis protocol, physical examination, review of complementary tests and request for new tests is necessary.33
Missed injuries can be minor, requiring only conservative treatment, or can be clinically significant, requiring a prompt recognition. Few studies have defined “clinically significant” post hoc,34 with most studies not providing any definition. Even if the incidence of clinically significant missed injuries is unknown, they are more likely to lead to prolonged morbidity or mortality. Although mortality as a result of missed injuries is rare, a prospective study indicated that approximately 1% of the cohort required a surgical intervention for injuries detected after the hospital discharge.35 Injuries are often neglected during the primary and secondary surveys in trauma patients; namely, studies have suggested that a formal tertiary survey protocol lowers the number of missed injuries. Current international guidelines consider tertiary surveys, but do not mandate or formalise their implementation.36
In our study, 99% of patients needed maxillofacial surgery, immediate or delayed depending on serious concomitant injuries. This percentage is significant if compared with proportion of patients with major/minor lesions. Interestingly, the number of concomitant lesions associated to severe maxillofacial traumas that was nearly neglected was 5, reaching a significant difference with respect to minor lesions: all cases occurred in paucisymptomatic and unsuspected patients. Based on these findings, we recommend the routine use of whole body CT scan when the maxillofacial injury appear prevalent, mainly in patients affected by maxillofacial major lesions.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Aldrian S., Koenig F., Weninger P. Characteristics of polytrauma patients between 1992 and 2002: what is changing? Injury. 2007;38:1059–1064. doi: 10.1016/j.injury.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Marucci-Wellman H.R., Courtney T.K., Corns H.L. The direct cost burden of 13 years of disabling workplace injuries in the U.S. (1998–2010): findings from the Liberty Mutual Workplace Safety Index. J Saf Res. 2015;55:53–62. doi: 10.1016/j.jsr.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Christensen J., Sawatari Y., Peleg M. High-energy traumatic maxillofacial injury. J Craniofac Surg. 2015;26:1487–1491. doi: 10.1097/SCS.0000000000001789. [DOI] [PubMed] [Google Scholar]
- 4.Patterson R. The Le Fort fractures: René Le Fort and his work in anatomical pathology. Can J Surg. 1991;34:183–184. [PubMed] [Google Scholar]
- 5.Kelly K.J., Manson P.N., Vander Kolk C.A. Sequencing LeFort fracture treatment (Organization of treatment for a panfacial fracture) J Craniofac Surg. 1990;1:168–178. doi: 10.1097/00001665-199001040-00003. [DOI] [PubMed] [Google Scholar]
- 6.Gassner R., Tuli T., Hächl O. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg. 2003;31:51–61. doi: 10.1016/s1010-5182(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 7.van Hout W.M., Van Cann E.M., Abbink J.H. An epidemiological study of maxillofacial fractures requiring surgical treatment at a tertiary trauma centre between 2005 and 2010. Br J Oral Maxillofac Surg. 2013;51:416–420. doi: 10.1016/j.bjoms.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Lebeau J., Kanku V., Duroure F. Facial injuries treated in the Grenoble University Hospital. Epidemiological analysis of 961 patients managed in one year. Rev Stomatol Chir Maxillofac. 2006;107:23–29. doi: 10.1016/s0035-1768(06)76977-7. [DOI] [PubMed] [Google Scholar]
- 9.Bali R., Sharma P., Garg A. A comprehensive study on maxillofacial trauma conducted in Yamunanagar, India. J Inj Violence Res. 2013;5:108–116. doi: 10.5249/jivr.v5i2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conforte J.J., Alves C.P., Sánchez M.P. Impact of trauma and surgical treatment on the quality of life of patients with facial fractures. Int J Oral Maxillofac Surg. 2016;45:575–581. doi: 10.1016/j.ijom.2015.11.022. [DOI] [PubMed] [Google Scholar]
- 11.Shah N., Palan S., Mahajan A. Why and how maxillofacial disability and impairment due to trauma should be quantified for compensation: a need for nationwide guidelines. J Maxillofac Oral Surg. 2014;13:425–430. doi: 10.1007/s12663-013-0527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arslan E.D., Solakoglu A.G., Komut E. Assessment of maxillofacial trauma in emergency department. World J Emerg Surg. 2014;9:13. doi: 10.1186/1749-7922-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Follmar K.E., Debruijn M., Baccarani A. Concomitant injuries in patients with panfacial fractures. J Trauma. 2007;63:831–835. doi: 10.1097/TA.0b013e3181492f41. [DOI] [PubMed] [Google Scholar]
- 14.Gervais H.W. [The ASA Classification – solid like a rock in anesthesiology] Anaesthesist. 2017;66:3–4. doi: 10.1007/s00101-016-0252-6. [DOI] [PubMed] [Google Scholar]
- 15.Tuckett J.W., Lynham A., Lee G.A. Maxillofacial trauma in the emergency department: a review. Surgeon. 2014;12:106–114. doi: 10.1016/j.surge.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Brooks A., Holroyd B., Riley B. Missed injury in major trauma patients. Injury. 2004;35:407–410. doi: 10.1016/S0020-1383(03)00219-5. [DOI] [PubMed] [Google Scholar]
- 17.Fama F., Cicciù M., Nastro-Siniscalchi E. Nonfatal cervical-neck lesion with a wooden foreign body: diagnosis and management. J Craniofac Surg. 2016;27:175–176. doi: 10.1097/SCS.0000000000002338. [DOI] [PubMed] [Google Scholar]
- 18.Sohns J.M., Staab W., Sohns C. Current perspective of multidetector computed tomography (MDCT) in patients after midface and craniofacial trauma. Clin Imaging. 2013;37:728–733. doi: 10.1016/j.clinimag.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Erol B., Tanrikulu R., Görgün B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience) J Craniomaxillofac Surg. 2004;32:308–313. doi: 10.1016/j.jcms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Oji C. Maxillofacial injuries. Plast Reconstr Surg. 1996;97:866–868. doi: 10.1097/00006534-199604000-00035. [DOI] [PubMed] [Google Scholar]
- 21.Brown R.D., Cowpe J.G. Patterns of maxillofacial trauma in two different cultures. A comparison between Riyadh and Tayside. J R Coll Surg Edinb. 1985;30:299–302. [PubMed] [Google Scholar]
- 22.Lee K. Global trends in maxillofacial fractures. Craniomaxillofac Trauma Reconstr. 2012;5:213–222. doi: 10.1055/s-0032-1322535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiara O., Mazzali C., Lelli S. A population based study of hospitalised seriously injured in a region of Northern Italy. World J Emerg Surg. 2013;8:32. doi: 10.1186/1749-7922-8-32. eCollection 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sivolella S., Brunello G., Ferrarese N. Nanostructured guidance for peripheral nerve injuries: a review with a perspective in the oral and maxillofacial area. Int J Mol Sci. 2014;15:3088–3117. doi: 10.3390/ijms15023088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Erdogan M.O., Sogut O., Colak S. Roles of motorcycle type and protective clothing in motorcycle crash injuries. Emerg Med Int. 2013;2013:760205. doi: 10.1155/2013/760205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eckstein M., Chan L., Schneir A. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma. 2000;48:643–648. doi: 10.1097/00005373-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Mijiti A., Ling W., Tuerdi M. Epidemiological analysis of maxillofacial fractures treated at a university hospital, Xinjiang, China: a 5-year retrospective study. J Craniomaxillofac Surg. 2014;42:227–233. doi: 10.1016/j.jcms.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Gioffrè Florio M., Famà F., Gullo G. Management of polytrauma: our experience. Chir Ital. 2005;57:485–489. [PubMed] [Google Scholar]
- 29.Calderale S.M., Sandru R., Tugnoli G. Comparison of quality control for trauma management between Western and Eastern European trauma center. World J Emerg Surg. 2008;3:32. doi: 10.1186/1749-7922-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pape H.C., Neugebauer E., Ridley S.A. Cost-drivers in acute treatment of severe trauma in Europe: a systematic review of literature. Eur J Trauma Emerg Surg. 2009;35:61–66. doi: 10.1007/s00068-008-8013-0. [DOI] [PubMed] [Google Scholar]
- 31.Famà F., Beccaria A., Malara C. Management of maxillofacial injuries in an emergency unit: our experience. Chir Ital. 2009;61:55–60. [PubMed] [Google Scholar]
- 32.Roumeliotis G., Ahluwalia R., Jenkyn T. The Le Fort system revisited: trauma velocity predicts the path of Le Fort I fractures through the lateral buttress. Plast Surg (Oakv) 2015;23:40–42. doi: 10.4172/plastic-surgery.1000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zamboni C., Yonamine A.M., Faria C.E. Tertiary survey in trauma patients: avoiding neglected injuries. Injury. 2014;45:S14–S17. doi: 10.1016/S0020-1383(14)70014-2. [DOI] [PubMed] [Google Scholar]
- 34.Keijzers G.B., Del Mar C., Geeraedts L.M., Jr. What is the effect of a formalised trauma tertiary survey procedure on missed injury rates in multi-trauma patients? Study protocol for a randomised controlled trial. Trials. 2015;16:215. doi: 10.1186/s13063-015-0733-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keijzers G.B., Campbell D., Hooper J. A prospective evaluation of missed injuries in trauma patients before and after formalizing the trauma tertiary survey. World J Surg. 2014;38:222–232. doi: 10.1007/s00268-013-2226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tammelin E., Handolin L., Söderlund T. Missed injuries in polytrauma patients after trauma tertiary survey in trauma intensive care unit. Scand J Surg. 2016 Feb 29 doi: 10.1177/1457496915626837. pii: 1457496915626837 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]