Abstract
Introduction
The purpose of this study is to compare the efficacy of single 2 mm locking miniplates versus two 2 mm non-locking (conventional) miniplates in symphysis and parasymphysis fracture of mandible.
Method
This present study included 40 patients of maxillofacial trauma having mandibular symphysis/parasymphysis fractures in which open reduction and internal fixation is indicated. Patients were selected according to the inclusion criteria and divided into two groups, i.e. Group 1: consisted of 20 patients, requiring open reduction and internal fixation with 2 mm two non-locking titanium plate and Group 2: consisted of 20 patients, requiring open reduction and internal fixation with 2.0 mm single ultra-locking titanium plate. Fracture was then stabilized and postoperative clinical examination was carried out on 3rd day, 1st, 2nd, 4th, and 8th week.
Result
Results of this study suggested that the use of single 2.0 mm locking miniplate could be a viable option instead of using two miniplates in anterior mandibular fracture as advocated by Champy, as it provides equally good outcome along with placement of lesser implant material.
Discussion
Single locking miniplates give the advantage of equally good stability and early restoration of function with almost similar results as seen in osteosynthesis with two miniplates. It was also found that less precision was required in plate adaptation when using single locking miniplate. This study suggests that there is not much difference in surgical outcome with the use of either single locking miniplate or two conventional miniplates in anterior mandibular region.
Keywords: Symphysis/parasymphysis fracture, Locking plates, Non-locking (conventional plates)
1. Introduction
“Love of life is next to love of our own faces” – Sushruta – 600 B.C.
Face being the most admired point, defacement due to trauma or otherwise would greatly affect a person both bodily and psychologically. For this reason, any disfiguring trauma or defect to maxillofacial region needs urgent and skilled management. The cause of maxillofacial injuries varies from one country to another and even within the same country depending upon the existing socioeconomic, cultural, and environmental factors. Road traffic accidents are gaining new heights in developing countries like India, with increase in urbanization, hasty arrival of high-speed automobiles, and poor road conditions resulting in increase in incidence of traumatic injuries to the maxillofacial skeleton.1
Mandible, in spite of being the largest and strongest facial bone, by asset of its position on the face and its prominence, is frequently fractured when maxillofacial trauma is sustained. There is variety of anatomic and biomechanical reasons for this incident. Osteology of mandible, the muscular attachments and their influence, and presence of developing and developed dentition play an imperative role in producing the inhere-tent weakness and making secluded areas of mandible more vulnerable to fractures. These secluded areas of weakness include angle, sub-condylar region, and symphysis and parasymphysis region. The cantilevered nature of angle region, constriction of neck in sub-condylar region, presence of mental foramen, and long socket of canine tooth contribute to the compromised potency of mandible in these regions.1, 2, 3 The anatomy of mandible and vector of forces exerted by the masseter and temporalis muscles make symphysis/parasymphysis fractures predominantly challenging. These vector forces take apart the inferior border of the mandible at the site of fracture. With the advent of rigid internal fixation for mandibular fractures in the 1970s, the concepts of favorable and unfavorable have gone by the wayside, and have been substituted by the new concepts of regions of tension and compression, i.e. tension at superior border and compression at inferior border. This concept of tension and compression holds true for body and angle fractures, but in symphysis/parasymphysis region, there are overlapping tensile and compressive loads in both the directions. Besides, these torsional forces are also significant. Taking these anatomical factors into account, in the anterior region between the mental foramina, in addition to sub-apical plate, another plate near the lower border of mandible is necessary in order to neutralize torsional forces and this second plate is applied parallel to first plate with a gap of 4.5 mm between them.3
Conventional bone plate/screw systems require precise adaptation of the plate to the underlying bone but with the introduction of locking plates, the disadvantages of conventional miniplates have been overcome.4, 5, 6, 7, 8, 9, 10 Thus, miniplate fixation of mandible fractures along the ‘ideal lines of osteosynthesis’ and advantages of locking miniplate over conventional ones have prompted us to compare the efficacy of single 2 mm locking miniplates versus two 2 mm non-locking miniplates in symphysis and parasymphysis fracture of mandible in patients treated in our department.
2. Materials and methods
After taking ethical approval from institutional authority, 40 cases of symphysis and parasymphysis fracture with or without associated fracture elsewhere in the mandible or mid-face who reported to our department, to be treated by open reduction and internal fixation were included in the study. A well informed and written consent was obtained from all patients included in this study to use their photographs/particulars for discussion and display. The patients were then randomly selected for choice of plating system viz. 2.0 mm single ultra-locking titanium plates with 2.0 mm ultra-locking screws or 2 mm two non-locking titanium plates with 2 mm screws. In all cases, a thorough history was recorded along with patient's health history to rule out significant systemic conditions that would have a bearing on patients’ treatment protocol. Detailed clinical examination was carried out as per the protocol. Radiographic examination included the posterior anterior view of mandible and the ortho-pantomogram (OPG). Additional radiographic projections, if indicated were obtained. The radiographs were thoroughly assessed before any surgical treatment and choice of plating system. All patients selected in the study were randomly divided into 2 groups irrespective of any bias.
-
•
Group 1: consisted of 20 patients who had undergone open reduction and internal fixation with 2 mm two non-locking titanium plate (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
-
•
Group 2: consisted of 20 patients who had undergone open reduction and internal fixation with 2.0 mm single ultra-locking titanium plate (Fig. 5, Fig. 6, Fig. 7, Fig. 8).
Fig. 1.

Pre-operative occlusion.
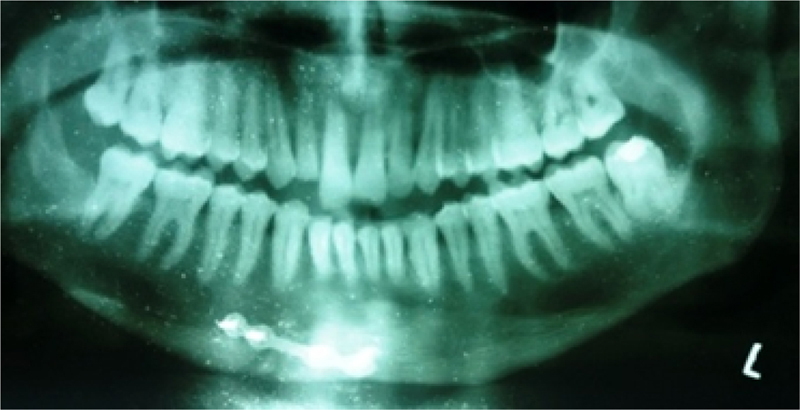
Fig. 2.
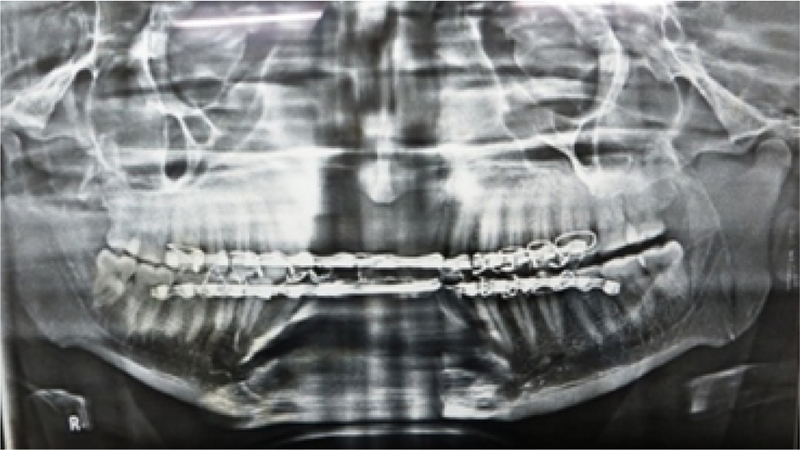
Pre-operative OPG.
Fig. 3.
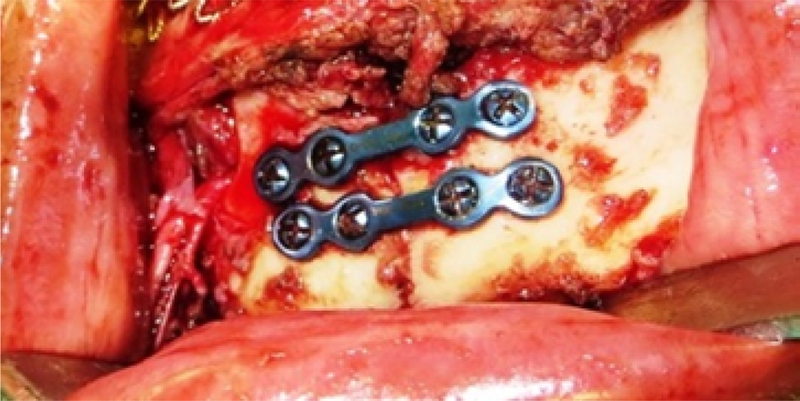
Conventional miniplates.
Fig. 4.

Post-operative OPG.
Fig. 5.

Pre-operative occlusion.
Fig. 6.
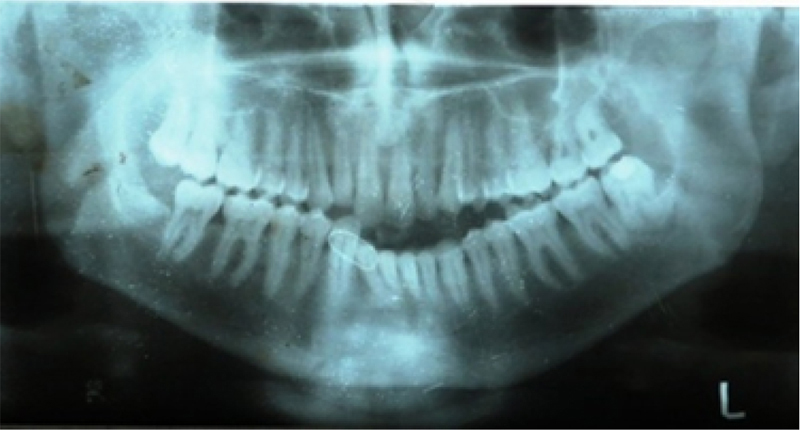
Pre-operative OPG.
Fig. 7.
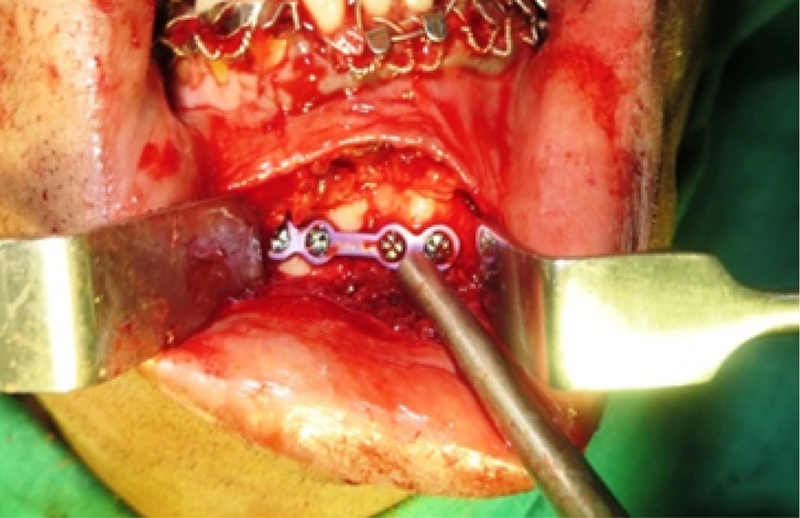
Locking miniplates.
Fig. 8.
Post-operative OPG.
Follow-up period was of at least 8 weeks, in which the patients were periodically recalled on 3rd day, 1st, 2nd, 4th, and 8th week post-operatively. Radiographic evaluation with OPG and posterior anterior view of mandible was done on the 3rd post-operative day, 4th, and 8th week. Assessment of patients was done under following parameters:
-
•
Pain: according to visual analog scale (0–10)
-
•
Occlusion: intact/deranged (based on clinical examination)
-
•
Stability of the fractured fragments: present/absent (based on clinical evaluation by digital palpation, i.e. alternatively applying pressure across the fractured segments and applying pressure alternatively intra-orally)
-
•
Infection: present/absent (case to be considered infected having pus discharge)
-
•
Incidence of hardware failure: present/absent (loosening of screws, plate fracture, according to radiographic and clinical observation)
-
•
Paraesthesia: present/absent (based on observation obtained from patient and clinically by performing - contact detection, static two point discrimination, and pin prick noci-ception)
-
•
Wound dehiscence: present/absent (based on clinical examination)
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) version 15.0 statistical Analysis Software.
3. Results
All the patients had an uneventful post-operative period and were discharged on the 3rd day after surgery. 20 patients in each group met the inclusion criteria and were included in the study; their mean age was 37.00 ± 10.48 in Group I and 36.80 ± 9.55 in Group II. The cause of trauma was road traffic accident in 35 (87.5%) patients, followed by fall in 3 patients, and interpersonal violence in 2 patients. Out of 40 patients in our study, 30 were male (75%) and 10 (25%) were female. In our study, single fracture occurred in 17 patients (42.5%) and two fractures in 23 patients (57.5%). In Group I, mean percentage change (decline from Visit 1) in pain score at Visit 2 was found to be 48.0% and in Group II, it is 55.24% which further declined to 88.67% at Visit 3 in Group I and 97.90% in Group II and from Visit 3 onwards, a 100% decline in pain score was observed in Group II, while in Group I, 100% decline in pain score was observed from Visit 4 (Table 1). Changes in pain score at all the visits were statistically significant. In our study, at Visit 1 and Visit 2, 14 patients (70.0%) from each group were suffering from paraesthesia. No difference in incidence of paraesthesia between the two groups was found at Visit 1 and Visit 2. At Visit 3, incidence of paraesthesia was found to be higher in Group I (65.00%) as compared to Group II (55.00%). Similarly, at Visits 4, 5, and 6, incidence of paraesthesia was found to be higher in Group I (35.0%, 20.0%, and 10.0% respectively) as compared to Group II (30.0%, 5.0%, and 0.0% respectively), but at none of the visits, the difference was found to be statistically significant. After application of bone plates, all fractures appeared to be well reduced and stable (based on clinical evaluation by digital palpation, i.e. alternatively applying pressure across the fractured segments and applying pressure alternatively intra-orally). At Visit 1, stability was found to be poor in all patients of Group I (100.0%) and Group II (100.0%) (Table 3). Difference in stability of both the groups was not found to be statistically significant. From Visit 2 onwards, stability of all the patients was found to be good. No difference in stability of both the groups was found at Visit 2 and visits thereafter. In this study, all 40 patients had normal occlusion post-operatively. We found pre-operative infection in 5 patients of Group I and 3 patients of Group II but after Visit 3 and visits thereafter, infection was not found in any of the group (Table 2). In any of our case, we did not report wound dehiscence post-operatively.
Table 1.
Intragroup comparison of change in pain scores at different visits (from Visit 1) (Wilcoxon Signed rank test).
| Group I |
Group II |
|||||
|---|---|---|---|---|---|---|
| Mean % change | Z | p | Mean % change | t | p | |
| Visit 2 | −48.00 | 3.955 | <0.001 | −55.24 | 3.951 | <0.001 |
| Visit 3 | −88.67 | 3.946 | <0.001 | −97.90 | 3.944 | <0.001 |
| Visit 4 | −100.00 | 3.941 | <0.001 | −100.00 | 3.944 | <0.001 |
| Visit 5 | −100.00 | 3.941 | <0.001 | −100.00 | 3.944 | <0.001 |
| Visit 6 | −100.00 | 3.941 | <0.001 | −100.00 | 3.944 | <0.001 |
Table 3.
Between group comparison of stability of fracture.
| Stability | Group |
Total | |||
|---|---|---|---|---|---|
| Non-lock | Lock | ||||
| Visit 1 | Acceptable | Count | 0 | 0 | 0 |
| % within group | |||||
| Poor | Count | 20 | 20 | 40 | |
| % within group | 100% | 100% | 100% | ||
| Total | Count | 20 | 20 | 40 | |
| % within group | 100.0% | 100.0% | 100.0% | ||
| Stability | Group |
Total | |||
|---|---|---|---|---|---|
| Non-lock | Lock | ||||
| Visit 2 | Good | Count | 20 | 20 | 40 |
| % within group | 100.0% | 100.0% | 100.0% | ||
| Total | Count | 20 | 20 | 40 | |
| % within group | 100.0% | 100.0% | 100.0% | ||
Table 2.
Between group comparison of incidence of infection.
| Visit | Group I (n = 20) |
Group II (n = 20) |
Statistical significance |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | χ2 | p | |
| Visit 1 | 5 | 25.00 | 3 | 15.00 | 0.625 | 0.429 |
| Visit 2 | 5 | 25.00 | 3 | 15.00 | 0.625 | 0.429 |
| Visit 3 | 0 | 0.00 | 0 | 0.00 | – | – |
| Visit 4 | 0 | 0.00 | 0 | 0.00 | – | – |
| Visit 5 | 0 | 0.00 | 0 | 0.00 | – | – |
| Visit 6 | 0 | 0.00 | 0 | 0.00 | – | – |
4. Discussion
Oro-facial trauma surgery is the base from which the specialty of maxillofacial surgery arose and has appreciably expanded and developed over the last 50 years.11 The only everlasting thing in this world is change. Advancements in biomaterials over the last decade have contributed to the dramatic advances in the overall therapeutic armamentarium of the oral and maxillofacial region. Over the years, many refinements have been made in the methods to treat mandibular fractures. Newer methods have been tried and older ones have had improvements. The principle objectives in the treatment of mandibular fracture are to re-establish normal occlusion and masticatory function with minimal disability and complications. Conservative treatment to achieve this is performed by immobilizing the mandible for the healing period by intermaxillary fixation which is achieved by dental wiring, arch bars, cap splint, and gunning splints which has its well-known problems.11
Nowadays, open reduction with internal fixation is the norm and tiny titanium miniplates are used to immobilize fragments of the jaw. Morbidity of this procedure is low with advantage that the patient returns to normal function within days of treatment.11 This intra-oral approach is preferred unless indicated otherwise, as it is esthetically accepted as timesaving and less traumatic. Miniplate osteosynthesis was first introduced by Michelet et al. in 1973 and further developed by Champy and Lodde et al. According to them, physically coordinated muscle function produces tension force at the upper border of the mandible and compressive forces at lower border, so the plates are applied close to tension zone of mandible. The screws used are mono-cortical to prevent injury to dentition and alveolar nerve.12
Conventional bone plate/screw system, as advocated by Champy, requires two plates to be adapted precisely in anterior mandibular region to the underlying bone to counteract the torsional as well as rotational forces. Without this intimate contact, tightening of the screws will draw the bone segments toward the plate, resulting in alterations in the position of the osseous segments and the occlusal relationship. Locking plate/screw systems offer certain advantages over other plates in this regard; the most significant advantage may be that it becomes unnecessary for the plate to have intimate contact with the underlying bone in all areas. As the screws are tightened, they “lock” to the plate, thus stabilizing the segments without the need to compress the bone to the plate. This obviates the risk that screw insertion will alter reduction.13 However, to the best of our knowledge, no such study has been undertaken to compare and evaluate the efficacy of single locking miniplate with two conventional miniplates in anterior mandibular region.
Initially, “the locking plate/screw system” was developed by Raveh et al.14 In 1999, Gutwald et al. performed the first biomechanical comparison of locking plates applied to mandible and concluded that a higher stability was achieved with the use of locking miniplates.15 Another advantage of the locking plate/screw system is that the screws are unlikely to get loose from the plate. This means that even if the screw is inserted into the fracture line, loosening of the screw will not occur.16 The possible advantage to this property of the locking plate/screw system is decreased incidence of inflammatory complications from loosening of hardware. It is known that loosening of hardware propagates inflammatory reaction and leads to infection. In conventional plates with similar dimensions, fixation is provided by screw thread inserted into bone, creating a friction lock between the plate and the bone which is essential to achieve stability after reduction. Torsional forces between bony fragments may lead to a loss of this friction lock and result in reduced primary stability.17 Cordey et al.18 stated that friction between screw head and plate is the main weak point of the entire fixation. In the locking plate/screw system, the thread on the screw head locks into the congruent thread of the plate, transforming the screw and plate into a unit, creating a rigid splint with higher mechanical stability.
Our study reviewed the efficacy of single 2.0-mm locking plate and two 2.0-mm non-locking plate (conventional plates) in 40 patients (20 in each group) requiring open reduction and internal fixation without maxilla-mandibular fixation. Open reduction and internal fixation was carried out in standard operating protocol using an intraoral approach. Out of 40 patients in our study, 30 were male (75%) and this male dominance was also reported by Haug et al.19 The finding of this study suggests that the highest incidence of trauma occurred in the 21–40-year-old age in both the groups. Single fracture occurred in 17 patients (42.5%) and two fractures in 23 patients (57.5%) in our study and this is in agreement with the study done by Ellis et al.20 as he encountered single fracture in 32.2% patients and two fractures in 61% patients.
In this study, patients in Group II experienced less pain than Group I and reason for this might be less stripping of surrounding musculature and periosteum as well as lesser amount of implant material was placed while using single plate system as it causes lesser amount of tissue inflammation resulting in decreased pain, but in contrast, when two conventional miniplates are used tissue retraction and periosteal stripping is more resulting in more pain.
In our study, lesser incidence of paraesthesia was noticed in patients of Group II, while Cabrini Gabrielli et al.21 reported 31.52% incidence of paraesthesia with the use of conventional 2-mm miniplates which improved during time. Saikrishna et al.22 in their study reported 35% and 15% of transient paraesthesia post-operatively with the use of locking plate system and non-locking plate system respectively which improved within time periods of 4 weeks and according to them, the main reason for postoperative paraesthesia with locking plate system was due to the need for more tissue retraction to accommodate the drill guide and subsequent placement of perpendicular screws, but we found more amount of paraesthesia in non-locking group when it is compared with locking group because when single miniplate is used, less amount of exposure is required resulting in lesser amount of tissue retraction and traction injury to nerve as compared to the use of 2 mini-plates. This might be the reason of lesser amount of paraesthesia with single miniplate in our study.
In this study, after application of bone plates, all fractures appeared to be well reduced and stable in both the groups and this finding is in agreement with Chritah et al.23 There were no intra-operative difficulties associated with placement of fixation hardware. Radiographs taken 3rd post-operative day, 4th week, and 6th week showed excellent reduction in all cases. So, our findings suggest that instead of using 2 conventional miniplates, a single miniplate can be used in anterior mandibular region, as there is no statistically significant difference in fracture stability in both the groups, lesser amount of implant material is also being used, and stability achieved with the use of single miniplate is equivocal to the use of 2 conventional miniplates.
Restoration of occlusion is one of the important goals of the management of fractures of maxillofacial region. The effect of not restoring the occlusion to its original condition is disabling and can cause severe effects, especially on temporo-mandibular joint. In this series, occlusion was checked pre-operatively and during the follow-up stages after surgery (based on clinical examination). In this study, all 40 patients had normal occlusion post-operatively and this finding is in agreement with Ellis20 while Nayak et al.17 reported occlusal discrepancy in 8% and 28% of their patients treated with locking plate and non-locking plate respectively. According to above-mentioned authors, reason for this might be that the inaccurate adaptation of conventional miniplates causes displacement of mobile bony fragments when the screws are tightened and thus can decrease primary stability resulting in occlusal discrepancy; in contrast, locking plate principle allows the mobile fragments of bone to stay in reduced position, even if plate is not precisely adapted and findings of this study revealed that even a single miniplate is enough to meet the criteria of anterior mandibular fixation in terms of occlusal harmony.
In our study, patients were evaluated pre-operatively and post-operatively at 1st, 3rd day, 1st, 2nd, 4th, and 8th week after surgery for the signs of infection. Swelling, local rise in temperature, local inflammation, and pus discharge were considered as indicators for the presence of infection. We found pre-operative infection in 5 patients of Group I and 3 patients of Group II but after Visit 3 and visits thereafter, infection was not found in any of the group because of judicious use of post-operative anti-microbial therapy, while Collins et al.25 reported 4.6% patients with complications in locking group and 5.2% in non-locking group and suggested no clinical advantage of 1 plate/screw system over the other. When complication rates of 2.0-mm locking plates are compared with standard 2.0-mm plates, there is no statistically significant difference. Verma et al.5 in their study reported 4.7% patients with infection in locking group and 13.6% patients in non-locking group and concluded that loosening of screws was present on surgical exploration in non-locking group as compared to locking group, while Prabhakar et al.13 reported 3.125% of infection with use of locking plate. Post-operative MMF (maxillo-mandibular fixation) may be another cause of post-operative infection because of the inability of patient to maintain proper oral hygiene resulting in accumulation of food debris and plaque which promotes bacterial contamination. All the above-mentioned authors have used post-operative MMF for 7–15 days and this might be the reason along with loosening of screws for increased incidence of infection. In this study, we did not use MMF in any of the patients and no incidence of loosening of screws/hardware failure was present during follow-up which justify our finding.
We did not report any case of wound dehiscence post-operatively in any of our group while Sauerbier et al.24 reported 7.5% of wound dehiscence with locking plate in their study because patients had a positive history for either alcohol or tobacco use or for both but in our study, some patients do have positive history of either alcohol or tobacco use or both but because of their compliance and no reported case of infection, we did not observe any case of wound dehiscence. None of our patient reported with hardware failure in any group, as we did not observe any case of infection and loosening of screws which promotes inflammation, which is in agreement with Collins et al.,25 while Nayak et al.17 reported 1% and 12% patients with plate fracture and 4% and 28% with loosening of screws in locking and non-locking group respectively and Saikrishna et al.22 reported 5% and 15% patients with hardware failure in locking and non-locking group respectively. Higher incidence of hardware failure is associated with the use of conventional miniplates because mandible has uneven surface and adapting conventional miniplates to the contours of bone can compensate for such incongruities. Repeated bending of these plates causes material fatigue and create predetermined breaking points but while using single locking mini-plate, intimate contact of plate to bone is eliminated resulting in less hardware failure.
5. Conclusion
In conclusion, single locking miniplates provide the advantage of equally good stability and early restoration of function with almost similar results as seen with two miniplate osteosynthesis. It was also found that less precision was required in plate adaptation. This study suggests that there is not much difference in surgical outcome with the use of either single locking miniplate or two conventional miniplates in anterior mandibular region and single locking miniplate has adequate strength to counter torsional and rotational forces acting in this region.
So, we strongly suggest that single 2.0 mm locking miniplate could be a viable option instead of using two miniplates as advocated by Champy, as it provides equally good outcome along with placement of lesser implant material. However, studies with larger sample size are required to validate our findings.
Ethical approval
Ethical approval was taken by Ethical committee of Kothiwal Dental College & Research Centre, Moradabad, Uttar Pradesh, India.
Conflicts of interest
The authors have none to declare.
References
- 1.Madsen M.J., McDaniel C.A., Haug R.H. A biomechanical evaluation of plating techniques used for reconstructing mandibular symphysis/parasymphysis fractures. J Oral Maxillofac Surg. 2008;66(10):2012–2019. doi: 10.1016/j.joms.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Malik N.A. 3rd ed. Jaypee Brother's Medical Publishers; 2012. Textbook of Oral & Maxillofacial Surgery. [Google Scholar]
- 3.Fonseca R.J. 3rd ed. Elsevier Saunders; 2005. Textbook of Oral and Maxillofacial Trauma. [Google Scholar]
- 4.Härle F., Champy M., Bill C. 2nd ed. Thieme Publication; 2009. Terry – Atlas of Craniomaxillofacial Osteosynthesis. [Google Scholar]
- 5.Verma A., Sachdeva A., Yadav S. Versatility of locking plates over conventional miniplates in mandibular fractures. J Innov Dent. 2011;I(January–April (I)) [Google Scholar]
- 6.Michelet F.X., Deymes J., Dessus B. Osteosynthesis with miniaturized screwed plates in maxillofacial surgery. J Oral Maxillofac Surg. 1973;1:79. doi: 10.1016/s0301-0503(73)80017-7. [DOI] [PubMed] [Google Scholar]
- 7.Champy M., lodde J.P., Schmitt R., Jaeger J.H., Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Oral Maxillofac Surg. 1978;6(February (1)):14–21. doi: 10.1016/s0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- 8.Cawood J.I. Small plate osteosynthesis of mandibular fractures. Br J Oral Maxillofac Surg. 1985;23(April (2)):77–91. doi: 10.1016/0266-4356(85)90057-9. [DOI] [PubMed] [Google Scholar]
- 9.Hober P.C. Advances in cranio-maxillofacial fracture management. Clin Plastic Surg. 1992;19(January (1)) [Google Scholar]
- 10.Elsharkawy R., Beheiri G., Hunish A. Locking versus standard 2.0-mm miniplates for fixation of mandibular angle fractures: a prospective study. Egypt Dent Assoc. 2013;59(1.3):581–584. [Google Scholar]
- 11.Mukherji R., Mukherji G., McCurk M. Mandibular fractures; historical perspective. Br J Oral Maxillofac Surg. 2006;44:222–228. doi: 10.1016/j.bjoms.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 12.Saito David M., Murr Andrew H. Internal fixation of mandibular fracture with champy technique. Oper Tech Otolaryngol. 2008;19:123–127. [Google Scholar]
- 13.Prabhakar C., Shetty J.N., Hemavathy O.R., Guruprasad Y. Efficacy of 2-mm locking miniplates in the management of mandibular fractures without maxillomandibular fixation. Natl J Maxillofac Surg. 2011;2(January–June (1)):28–32. doi: 10.4103/0975-5950.85850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alpert B., Gutwald R., Schmelzeisen R. New innovations in craniomaxillofacial fixation: the 2.0 lock system. Keio J Med. 2003;52(2):120–127. doi: 10.2302/kjm.52.120. [DOI] [PubMed] [Google Scholar]
- 16.Bolourian R., Lazow S., Berger J. Transoral 2.0-mm miniplate fixation of mandibular fractures plus 2 weeks’ maxillomandibular fixation: a prospective study. J Oral Maxillofac Surg. 2002;60:167–170. doi: 10.1053/joms.2002.29813. [DOI] [PubMed] [Google Scholar]
- 17.Nayak S.S., Pushpalatha C., Tammanavar P.S., Naduwinmani S.L., Mohan M. Efficacy of locking plates/screw system in mandibular fracture surgery. J Contemp Dent Pract. 2013;14(2):222–226. doi: 10.5005/jp-journals-10024-1303. [DOI] [PubMed] [Google Scholar]
- 18.Cordey J., Borgeaud M., Parren S.M. Force transfer between plate and the bone: relative importance of the bending stiffness of the screws friction between plate and bone. Injury. 2000;31:21–28. doi: 10.1016/s0020-1383(00)80028-5. [DOI] [PubMed] [Google Scholar]
- 19.Haug R.H., Prather J., Indrasano A.T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- 20.Ellis E., III, John G. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642–645. doi: 10.1053/joms.2002.33110. [DOI] [PubMed] [Google Scholar]
- 21.Cabrini Gabrielli M.A., Real Gabrielli M.F., Marcantonio E., Hochuli-Vieira E. Fixation of mandibular fractures with 2.0 mm miniplates: review of 191 cases. J Oral Maxillofac Surg. 2003;61(4):430–436. doi: 10.1053/joms.2003.50083. [DOI] [PubMed] [Google Scholar]
- 22.Saikrishna D., Shetty S.K., Marimallappa T.R. A comparison between 2.0-mm standard and 2.0-mm locking miniplates in the management of mandibular fractures. J Maxillofac Oral Surg. 2009;8(2):145–149. doi: 10.1007/s12663-009-0036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chritah A., Lazow S.K., Berger J.R. Transoral 2.0-mm locking miniplate fixation of mandibular fractures plus 1 week of maxillomandibular fixation: a prospective study. J Oral Maxillofac Surg. 2005;63:1737–1741. doi: 10.1016/j.joms.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 24.Sauerbier S., Kuenz J., Hauptmann S., Frederik C. Clinical aspects of a 2.0-mm locking plate system for mandibular fracture surgery. J Cranio-Maxillofac Surg. 2010;2010:1–4. doi: 10.1016/j.jcms.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 25.Collins C.P., Leonard G.P., Tolas A., Alcalde R. A prospective randomized clinical trial comparing 2.0-mm locking plates to 2.0-mm standard plates in treatment of mandible fracture. J Oral Maxillofac Surg. 2004;62:1392–1395. doi: 10.1016/j.joms.2004.04.020. [DOI] [PubMed] [Google Scholar]
Further reading
- 14.Potter J., Ellis E., 3rd Treatment of mandibular angle fractures with a malleable non-compression miniplate. J Oral Maxillofac Surg. 1999;57(28):8–92. doi: 10.1016/s0278-2391(99)90674-2. [DOI] [PubMed] [Google Scholar]


