Abstract
Background:
To identify somatic complaints dimensions, classify studied population and study the association of demographic and lifestyle factors with somatic complaints dimensions.
Methods:
In a cross-sectional study conducted on 4763 Iranian adults, somatic complaints were assessed using a comprehensive 30-item questionnaire. Self-administered standard questionnaires were used to assess demographic and lifestyle factors. Factor mixture modeling (FMM) was used to identify somatic complaints dimensions and classify studied population.
Results:
The mean age of participants was 36.58 ± 0.13 years, 55.8% were females, 81.2% were married, and 57.2% had college education. About 9.4% of individuals were obese, and 34.8% of participants had regular physical activity. Four domains of somatic complaints were extracted, including “psychological,” “gastrointestinal,” “neuro-skeletal,” and “pharyngeal-respiratory.” Females, obese and inactive participants, and those in low educations had significantly greater scores in terms of four domains than the others (P < 0.05). A two-class, four-factor structure fitted to the somatic complaints based on FMM. Two classes were labeled “high psychological complaints” (519 individuals (11%) and “low psychological complaints” (4243 individuals (89%). There were no significant differences between two classes in terms of demographic and lifestyle factors, except in educational level.
Conclusions:
This study suggested that somatic complaints had a dimensional-categorical structure within studied population so that it could be useful for dealing with diagnostic and therapeutic approaches. The results did not show any association between somatic complaints dimensions and demographic, lifestyle factors, except in educational level.
Keywords: Demographic factors, factor mixture modeling, lifestyles, somatic complaints
INTRODUCTION
Somatic complaints are physical symptoms of which presence, severity or consequences cannot be explained by any detectable physical disorder.[1] These are common in the general population, and they are prevalent in patients attending primary care, secondary care, and in different medical conditions.[2,3] The prevalence of somatic complaints varies depending on several factors such as gender, age, and socioeconomic status.[1,4] The reported prevalence rates in primary care varying between 25% and 50%[1,5] and these symptoms are more prevalent among women and in old age populations.[1,6] Furthermore, it is reported that individuals with less education tend to report more somatic symptoms.[7] Some studies showed relationships between less physical activity, higher body mass index (BMI), and higher levels of psychological, gastrointestinal, and respiratory somatic complaints.[8,9]
Some studies indicated that there is notable heterogeneity in term of somatic complaints among the studied populations.[10,11,12] Different statistical methods such as factor analysis and latent class analysis (LCA) have been used for dealing with identifying heterogeneity.[10,11] Factor mixture modeling (FMM)[13] is a relatively new methodological procedure that unifies factor analysis and LCA in a single analysis and allows the underlying structure to be simultaneously dimensional and categorical. The structure is considered categorical to classify individuals into subgroups and (latent classes) it is also considered dimensional to account for heterogeneity within groups using continuous latent variables (latent factors). Hence, the primary objective of the current study was to identify somatic complaints dimensions (latent factors) and to classify studied population (latent classes) based on constructed somatic complaints dimensions using FMM. Such stratification could provide the foundation for differentiating some subgroups of population with different somatic complaints dimensions for dealing with diagnostic and therapeutic approaches. Other objectives of our study were studying the association of some main demographic and lifestyle factors with somatic complaints dimensions and evaluating their association with the prevalence of somatic complaints latent class.
METHODS
Study design and participants
This cross-sectional study was conducted in the framework of SEPAHAN project that was performed in two phases in a large sample of the Iranian population adults in Isfahan province.[14] Data on 4762 subjects were used in the current study. Informed consent was obtained from all subjects. More details about the SEPAHAN's study design have presented elsewhere.[14] The Bioethics Committee of Isfahan University of Medical Sciences (IUMS), Isfahan, Iran, approved the study (Project numbers: #189069, #189082, and #189086).
Procedures and assessment of variables
Assessment of somatization
In SEPAHAN project, there is not a separate questionnaire to assess somatic complaints however, we found 31 common items among questions contained in SEPAHAN's questionnaires with the 47-item questionnaire used in the Lacourt et al.'s study[12] and the patient health questionnaire,[15] as standard tools for the assessment of somatic complaints, therefore, we established a 31-item validated questionnaire. It was used to evaluate the frequency of somatic complaints. Respondents could indicate to how much they had experienced each symptom in the past 3 months on a 4-points Likert scale (1 = never, sometimes, often, always). For one item (i.e., dry mouth), the rating scale was as: never, low, and high. We conducted a separate mini survey of 100 participants selected randomly to assess the reliability of this instrument. There was strong internal reliability, with a Cronbach's alpha score of 0.903.[16] In this study, we used 30 items from 31 items.
Assessment of other variables
Age (years), gender (male/female), marital status (married, single), self-reported weight (kg), and height (cm) were gathered using a self-administered standard questionnaire. BMI was calculated by dividing weight in kilograms by height in meters squared. Educational attainments categorized into three categories as lower than diploma (12 years formal education), diploma and more than diploma (including bachelor, master, and doctorate). General Practice Physical Activity Questionnaire was used to assess an individual's current physical activity status. It generates simple, 4-levels Physical Activity Index categorizing subjects as: active, moderately active, moderately inactive and inactive.[17] In the current analysis, participants were classified into two categories, i.e., inactive (including inactive and moderately inactive) and active (including moderately active and active) as indicated earlier.
Statistical analysis
At first, factor analysis (based on principal component extraction approach) was conducted on the thirty individual somatic complaints. The orthogonal varimax rotation procedure was used to find the interpretable factors. In this study, we retained factors with eigenvalues >2 as this cutoff could result in more interpretable somatic complaints profiles and explained sufficient amounts of overall variation. Four main somatic complaints profiles were extracted and labeled based on the loaded somatic complaints in each factor. Then, we used LCA to determine the number of latent classes in studied population, and two latent classes were identified. Finally, we conducted FMM with four factors and two latent classes using the FactMixtAnalysis package in the free Software Environment for Statistical Computing R. Factor means were allowed to be free across classes while factor loadings were restricted to be equal. Entropy index is provided, which is a useful criteria for assessment of the value and utility of the extracted classes. Entropy ranges from 0 to 1 and its higher values indicate better separation between classes and that individuals are properly classified.[18]
Quantitative and qualitative variables were presented as mean ± standard error and number (percent), respectively. Analysis of variance or independent Student's t-test was used for comparing quantitative variables among studied groups. Distribution of study participants in terms of categorical variables was compared between different classes using the Chi-square test. Data analyses were performed using Statistical Package for Social Sciences version 20 (SPSS Inc., Chicago, IL, U.S.A.).
RESULTS
Overall, 4762 adults contributed in the study. The mean age was 36.58 ± 0.13 years. They consisted of 2657 (55.8%) females and 3776 (81.2%) married. 2650 (57.2%) of the study participants had college education. About 3.5% of individuals were underweight, 37.1% were overweight and 9.4% were obese. 34.8% of participants had regular physical activity (moderately active and active).
Extraction of somatic complaints profiles using factor analysis
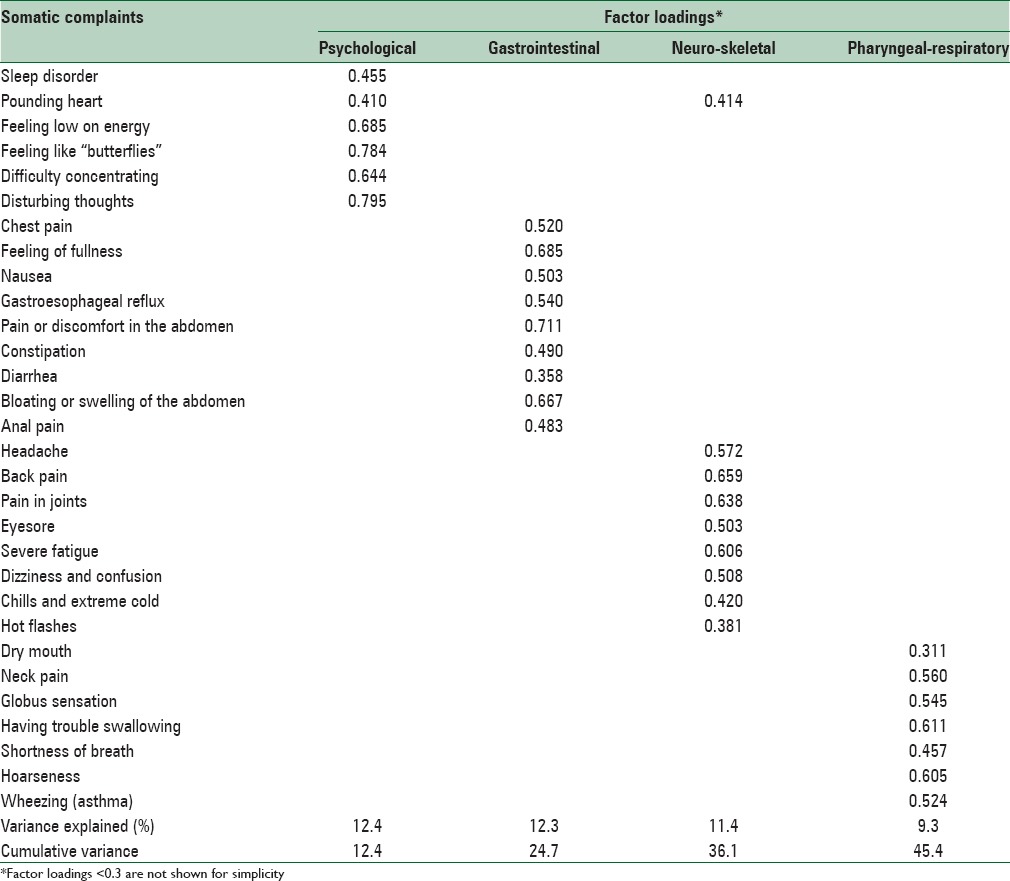
Four factors were extracted based on thirty individual somatic complaints and labeled as “psychological,” “gastrointestinal,” “neuro-skeletal,” and “pharyngeal-respiratory” [Table 1]. The four factors accounted for 12.4%, 12.3%, 11.4%, and 9.3% of the total variance, respectively.
Table 1.
Factor loadings for the four extracted somatic complaints profiles from thirty somatic complaints
Comparison of mean somatic complaints profiles across the different categories of demographic and lifestyle characteristics
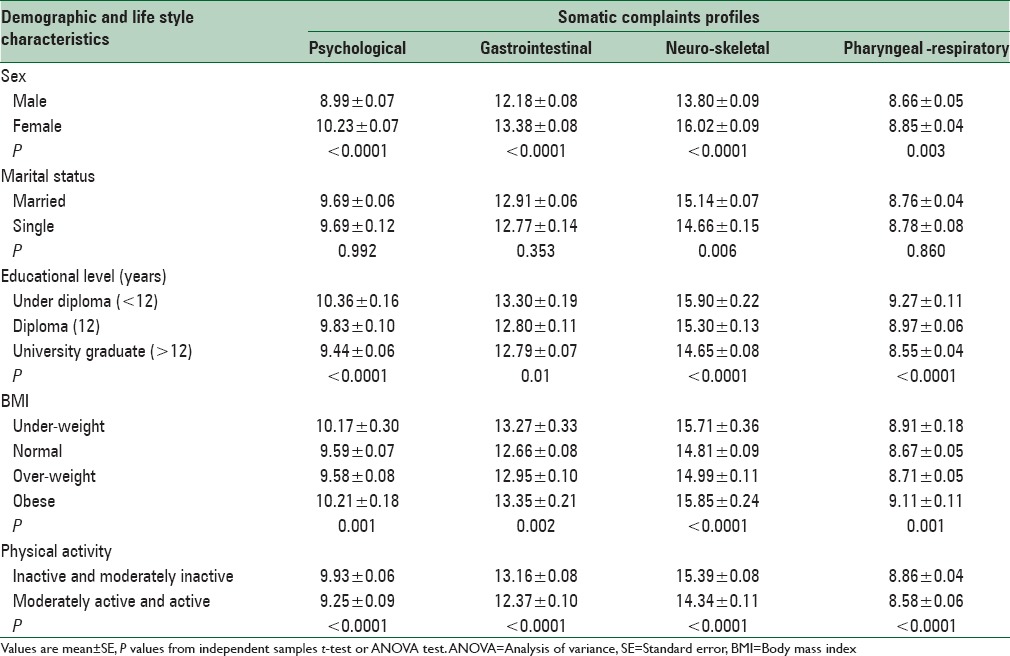
As shown in Table 2, means of four somatic complaints profiles for females, individuals with educational level of under diploma, obese and inactive participants were significantly greater than others (P < 0.05). Furthermore, mean neuro-skeletal profile for married participants was significantly greater than single participants (P < 0.01).
Table 2.
Comparison of mean somatic complaints profiles across the different categories of demographic and life style characteristics
Factor mixture modeling
The structure of study population in terms of four somatic complaints profiles (i.e., “psychological,” “gastrointestinal,” “neuro-skeletal,” and “pharyngeal-respiratory”) was examined using FMM. The two identified classes were labeled as “high psychological complaints” and “low psychological complaints;” as can be seen those participants in the first class experienced higher scores of psychological somatic complaints (mean: 0.249 vs. 0) while lower scores of somatic complaints in physical domains (gastrointestinal, neuro-skeletal, and pharyngeal-respiratory) [Table 3]. There were 519 individuals (11%) in the high psychological complaints class and 4243 individuals (89%) in the low psychological complaints class. Table 3 contains factor loadings and means for the two-class four-factor solution with free factor covariances and means. Approximately, all items loaded significantly on their respective factor.
Table 3.
Factor loadings and means for the final two-class four-factor factor mixture modeling solution

Demographic and lifestyle characteristics determinants of class membership
The distribution of demographic and lifestyle characteristics of study participants in extracted classes are presented in Table 4. The mean age was 36.59 ± 0.13 and 36.45 ± 0.40 years in low and high psychological complaints classes, respectively (P > 0.05). Although individuals belonging to high psychological complaints class were female predominant (57.4%), and the most of them was married (82.7); however, there are no significant differences between two classes. There was a significant difference between two classes in the term of educational level (P < 0.0001) and the majority of individuals belonging to low psychological complaints class had college education (58.8%). About 5.1% of individuals belong to high psychological complaints were underweight, 35.4% overweight and 11.1% were obese, suggesting no statistically significant different distribution of obesity over the somatic complaints profile's extracted classes. 68.9% and 64.8% of individuals affiliated to high and low psychological complaints classes, respectively, were physically inactive and moderately inactive, suggesting marginally higher levels inactivity among population belong to high psychological somatic complaints profile class (P < 0.1).
Table 4.
Demographic and life style characteristics of study participants in somatic complaints profile's classes

DISCUSSION
In this cross-sectional study, among a large sample of Iranian adults, we extracted four somatic complaints profiles (i.e., “psychological,” “gastrointestinal,” “neuro-skeletal” and “pharyngeal-respiratory”) from factor analysis. The current study based on FMM also provided support that our studied population comprises two-class, four-factor underlying structure of the somatic complaints. The two identified classes were labeled “high psychological complaints” and “low psychological complaints.” Although results of conducted statistical methods suggested that in this sample of the Iranian adults there were two distinct classes of individuals with inherent elevated psychological complaints, and with inherent low levels of psychological complaints; however, participants in both classes had other complaints profile, such as gastrointestinal, skeletal, and respiratory symptoms with different degrees. We did not find any study such as ours, which stratified a general population into more homogeneous subgroups based on somatic complaints using factor mixture models. However, some studies identified heterogeneity in terms of somatic complaints between different populations using clustering, factor analysis or LCA[10,11,12,19] For instance, in the Fink et al.'s study, three latent factors, i.e., “cardiopulmonary,” “musculoskeletal/pain,” and “gastrointestinal” using factor analyses was extracted.[10] Fink et al. also though LCA identified homogeneous subgroups of individuals with somatic complaints and revealed that individuals fell into three classes: nonbodily distress, modest bodily distress, and severe bodily distress.[10] Kato et al. using LCA classified individuals into the four classes. Individuals belonging to the first class did not show any health problems. Those assigned to the second, third, and fourth classes have abnormal tiredness, gastrointestinal problems, and pain-related symptoms, respectively.[11]
When comparing mean somatic complaints profiles across the different categories of demographic and lifestyle characteristics, we found that females, obese and inactive Iranian adults had more somatic complaints. These findings were consistent with other previous studies.[7,20,21,22,23,24,25,26,27,28,29] In the Kroenke and Spitzer's study, symptoms such as abdominal pain, back pain, bowel complaints, chest pain, and dizziness were more prevalent in females.[7] Furthermore, Park and Knudson showed the prevalence of somatic symptoms for women was more than twice as those for men.[24] Some studies suggested that psychological and gastrointestinal symptoms are more frequent in overweight and obese subjects.[9,25,26,27,30] In line with our study, Berg et al. showed that obese persons report more somatic and psychological symptoms (such as a headache and problem sleeping).[28] In addition, some studies investigated the effect of BMI on respiratory and skeletal symptoms and pains.[20,21,22,23] Yoo et al. showed that BMI associated significantly with musculoskeletal pains.[23] In addition, Nilsen et al. indicated that high BMI and low physical inactivity are associated with an increased risk of chronic pain in the low back and neck/shoulders in the general adult population.[8] In line with our study, Jarvis et al. showed that persons with a BMI of >30 were in relation with an increased risk of respiratory symptoms, such as wheeze and shortness of breath compared.[20] In the present study, individuals with less education had significantly higher scores of all somatic complaints profiles. In the Kroenke and Spitzer's study persons with less education tended to report more somatic symptoms.[7] We also found that individuals assigned to the high psychological complaints class have lower education. Previous studies showed that higher educational attainment was strongly associated with better mental health in adulthood,[31] because higher levels of education are thought to generate additional economic resources, fewer chronic stressors, healthier lifestyles, more social support, and ultimately, better mental health.[31]
CONCLUSIONS
This study using FMM showed that somatic complaints profiles had a dimensional-categorical structure within studied population. FMM in the current study served as a tool to decompose heterogeneity and identify natural somatic complaints subgroups. This modeling strategy could be considered a foundation for differentiating subgroups of population with different disease dimensions.
Financial support and sponsorship
The present article was extracted from a MSc thesis in Biostatistics at the School of Health, Isfahan University of Medical Sciences, with project number 394643. SEPAHAN was financially supported by a grant from the Vice Chancellery for Research and Technology, Isfahan University of Medical Sciences (IUMS). We are grateful to thank all staff of Isfahan University of Medical Sciences (MUI) who kindly participated in our study and staff of Public Relations Unit, and other authorities of IUMS for their excellent cooperation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
SEPAHAN was financially supported by a grant from the Vice Chancellery for Research and Technology, IUMS. We are grateful to thank all staff of IUMS (MUI) who kindly participated in our study and staff of Public Relations Unit, and other authorities of IUMS for their excellent cooperation.
REFERENCES
- 1.Hilderink PH, Collard R, Rosmalen JG, Oude Voshaar RC. Prevalence of somatoform disorders and medically unexplained symptoms in old age populations in comparison with younger age groups: A systematic review. Ageing Res Rev. 2013;12:151–6. doi: 10.1016/j.arr.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Steinbrecher N, Koerber S, Frieser D, Hiller W. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. 2011;52:263–71. doi: 10.1016/j.psym.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 3.Grassi L, Caruso R, Nanni MG. Somatization and somatic symptom presentation in cancer: A neglected area. Int Rev Psychiatry. 2013;25:41–51. doi: 10.3109/09540261.2012.731384. [DOI] [PubMed] [Google Scholar]
- 4.Creed F, Henningsen P, Fink P. Medically Unexplained Symptoms, Somatisation and Bodily Distress: Developing Better Clinical Services. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- 5.Escobar JI, Cook B, Chen CN, Gara MA, Alegría M, Interian A, et al. Whether medically unexplained or not, three or more concurrent somatic symptoms predict psychopathology and service use in community populations. J Psychosom Res. 2010;69:1–8. doi: 10.1016/j.jpsychores.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonzalez DS, Rodríguez M, García C, Prieto R, Saiz-Ruiz J. Gender differences in major depressive disorder: Somatic symptoms and quality of life. Rev Psiquiatr Salud Ment. 2009;2:119–27. doi: 10.1016/S1888-9891(09)72402-4. [DOI] [PubMed] [Google Scholar]
- 7.Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med. 1998;60:150–5. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Nilsen TI, Holtermann A, Mork PJ. Physical exercise, body mass index, and risk of chronic pain in the low back and neck/shoulders: Longitudinal data from the Nord-Trondelag Health Study. Am J Epidemiol. 2011;174:267–73. doi: 10.1093/aje/kwr087. [DOI] [PubMed] [Google Scholar]
- 9.Cremonini F, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Relationship between upper gastrointestinal symptoms and changes in body weight in a population-based cohort. Neurogastroenterol Motil. 2006;18:987–94. doi: 10.1111/j.1365-2982.2006.00816.x. [DOI] [PubMed] [Google Scholar]
- 10.Fink P, Toft T, Hansen MS, Ørnbøl E, Olesen F. Symptoms and syndromes of bodily distress: An exploratory study of 978 internal medical, neurological, and primary care patients. Psychosom Med. 2007;69:30–9. doi: 10.1097/PSY.0b013e31802e46eb. [DOI] [PubMed] [Google Scholar]
- 11.Kato K, Sullivan PF, Pedersen NL. Latent class analysis of functional somatic symptoms in a population-based sample of twins. J Psychosom Res. 2010;68:447–53. doi: 10.1016/j.jpsychores.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lacourt T, Houtveen J, van Doornen L. “Functional somatic syndromes, one or many?” An answer by cluster analysis. J Psychosom Res. 2013;74:6–11. doi: 10.1016/j.jpsychores.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Lubke GH, Muthén B. Investigating population heterogeneity with factor mixture models. Psychol Methods. 2005;10:21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- 14.Adibi P, Keshteli AH, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi R, et al. The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): Overview of methodology. J Res Med Sci. 2012;17(Spec 2):S291–S297. [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 16.Heidari Z, Keshteli AH, Feizi A, Afshar H, Adibi P. Somatic complaints are significantly associated with chronic uninvestigated dyspepsia and its symptoms: A large cross-sectional population based study. J Neurogastroenterol Motil. 2017;23:80–91. doi: 10.5056/jnm16020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Collaborating Centre for Nursing and Supportive Care (UK). Irritable Bowel Syndrome in Adults: Diagnosis and Management of Irritable Bowel Syndrome in Primary Care [Internet]. London: Royal College of Nursing (UK); 2008 Feb. Appendix J, The General Practice Physical Activity Questionnaire (GPPAQ) [Last accessed on 2006 Oct]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK51962/ [PubMed]
- 18.Lubke G, Muthén BO. Performance of factor mixture models as a function of model size, covariate effects, and class-specific parameters. Struct Equ Modeling. 2007;14:26–47. [Google Scholar]
- 19.Gara MA, Silver RC, Escobar JI, Holman A, Waitzkin H. A hierarchical classes analysis (HICLAS) of primary care patients with medically unexplained somatic symptoms. Psychiatry Res. 1998;81:77–86. doi: 10.1016/s0165-1781(98)00088-2. [DOI] [PubMed] [Google Scholar]
- 20.Jarvis D, Chinn S, Potts J, Burney P European Community Respiratory Health Survey. Association of body mass index with respiratory symptoms and atopy: Results from the European Community Respiratory Health Survey. Clin Exp Allergy. 2002;32:831–7. doi: 10.1046/j.1365-2222.2002.01380.x. [DOI] [PubMed] [Google Scholar]
- 21.Sano A, Hirano T, Watanabe K, Endo N, Ito T, Tanabe N. Body mass index is associated with low back pain in childhood and adolescence: A birth cohort study with a 6-year follow-up in Niigata City, Japan. Eur Spine J. 2015;24:474–81. doi: 10.1007/s00586-014-3685-0. [DOI] [PubMed] [Google Scholar]
- 22.Seaman DR. Body mass index and musculoskeletal pain: Is there a connection? Chiropr Man Therap. 2013;21:15. doi: 10.1186/2045-709X-21-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoo JJ, Cho NH, Lim SH, Kim HA. Relationships between body mass index, fat mass, muscle mass, and musculoskeletal pain in community residents. Arthritis Rheumatol. 2014;66:3511–20. doi: 10.1002/art.38861. [DOI] [PubMed] [Google Scholar]
- 24.Park J, Knudson S. Medically unexplained physical symptoms. Health Rep. 2007;18:43–7. [PubMed] [Google Scholar]
- 25.Truong EA, Olson KL, Emery CF. Repressive coping, stigmatization, psychological distress, and quality of life among behavioral weight management participants. Eat Behav. 2016;22:206–10. doi: 10.1016/j.eatbeh.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 26.Cambil-Martín J, Galiano-Castillo N, Muñoz-Hellín E, Díaz-Rodríguez L, Laguarta-Val S, Fernández-de-Las-Peñas C, et al. Influence of body mass index on psychological and functional outcomes in patients with multiple sclerosis: A cross-sectional study. Nutr Neurosci. 2016;19:79–85. doi: 10.1179/1476830514Y.0000000156. [DOI] [PubMed] [Google Scholar]
- 27.Horner TN, Jr, Utermohlen V. A multivariate analysis of psychological factors related to body mass index and eating preoccupation in female college students. J Am Coll Nutr. 1993;12:459–65. doi: 10.1080/07315724.1993.10718336. [DOI] [PubMed] [Google Scholar]
- 28.Berg IM, Simonsson B, Ringqvist I. Social background, aspects of lifestyle, body image, relations, school situation, and somatic and psychological symptoms in obese and overweight 15-year-old boys in a county in Sweden. Scand J Prim Health Care. 2005;23:95–101. doi: 10.1080/02813430510015313. [DOI] [PubMed] [Google Scholar]
- 29.Ruotsalainen H, Kyngäs H, Tammelin T, Kääriäinen M. Systematic review of physical activity and exercise interventions on body mass indices, subsequent physical activity and psychological symptoms in overweight and obese adolescents. J Adv Nurs. 2015;71:2461–77. doi: 10.1111/jan.12696. [DOI] [PubMed] [Google Scholar]
- 30.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66–72. doi: 10.1001/jama.290.1.66. [DOI] [PubMed] [Google Scholar]
- 31.Halpern-Manners A, Schnabel L, Hernandez EM, Silberg JL, Eaves LJ. The Relationship between Education and Mental Health: New Evidence from a Discordant Twin Study. Soc Forces. 2016;95:107–31. [Google Scholar]


