Abstract
Background:
Keratoconus is a progressive degenerative disorder of the cornea in which structural changes in the cornea cause it to become thin and conical in shape. Recently, collagen cross-linking (CXL) has been introduced as an effective intervention in management of progressive keratoconus. Accelerated CXL is a new protocol of this procedure which reduces corneal ultraviolet irradiation exposure time to 5 min. This study aimed to compare visual acuity, keratometry and topographic criteria of keratoconic eyes after conventional and accelerated CXL with a six-month follow-up.
Materials and Methods:
In this prospective interventional study we assessed eyes of 40 patients. Patients were divided into two groups randomly. One group underwent accelerated (5 min) CXL and the other underwent conventional (30 min) CXL. Visual acuity, topographic criteria and keratometry were assessed preoperatively and 6 months postoperatively.
Results:
In the present study we assessed 40 patients, 50% of which were right eye (OD) and 50% were left eye (OS). Mean age of patients in the accelerated group was 22.10 and in the conventional group was 22.80 years. Our results showed no significant differences between visual acuity, keratometric and topographic criteria in the two groups before intervention. Likewise our results manifested no significant difference between visual acuity, keratometric, refractive and topographic criteria after intervention.
Conclusion:
According to our survey topographic criteria and keratometry improvement in the accelerated and conventional protocol are the same. So accelerated protocol is suggested as a safe and effective option for management of progressive keratoconus.
Keywords: Accelerated method, conventional method, cornea collagen cross-linking, keratoconus
Introduction
Keratoconus is a non-symmetrical, non-inflammatory slowly progressive corneal degeneration and dystrophy that commonly presents in young adults characterized by changes in corneal collagen structures and organization. Decreased mechanical stability has a pivotal role in the progressive ectasia of the keratoconic cornea, leading to mild to severe impairment of visual acuity resulting from irregular astigmatism, progressive myopia, corneal thinning and central corneal scarring. Its incidence has been reported to be 1 in 2000 in the general population. Nevertheless some studies suggest the prevalence of keratoconus to be higher. Current interventions like spectacles and contact lenses, intracorneal ring segment implantation, lamellar keratoplasty and penetrating keratoplasty, have limitations.[1,2,3,4]
Recently, different studies demonstrated stiffening of the cornea with the use of ultraviolet A and riboflavin solution as a photosensitizer-initiated collagen cross-linking without any loss in corneal transparency. Collagen cross-linking (CXL) was introduced by Wollensak et al., to stabilize progressive keratoconus, to prevent some underlying pathophysiologic mechanisms of disease and avoid corneal transplantation.[4,5]
In the most commonly used CXL procedures, the UVA is illuminated for 30 min. Recent advances in UV light sources and CXL techniques have led to development of uniform, high-powered UVA light sources. These advances helped to develop a new accelerated technique for CXL that reduces exposure time to UVA.[6] A number of studies have investigated this new technique and compared it with conventional CXL. In their study carried out with the main purpose of comparison of early healing following conventional, transepithelial and accelerated corneal cross-linking, Touboul et al.,[7] demonstrated that accelerated CXL had a greater impact than conventional CXL on the anterior cornea. Matalia et al.,[8] evaluated the safety of accelerated CXL in their pilot study and concluded that accelerated CXL can be considered as a safe procedure for the treatment of keratoconus.[9] In another study, Rocha et al.,[10] showed that the rapid method of collagen cross-linking has similar efficacy in stiffening the cornea in comparison to standard cross-linking, but requires only 30 sec of UVA exposure.
In the present study the clinical results of conventional and accelerated collagen cross-linking for keratoconus after 6 months of follow-up, are presented and compared with each other.
Materials and Methods
Forty patients in which keratoconus progression was observed in the last 3 months were enrolled in the present study.
Keratoconus progression was confirmed by corneal topography in all eyes included in the study.
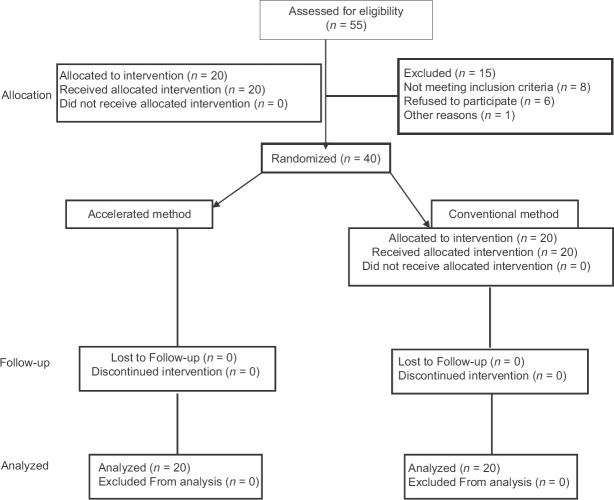
Inclusion criteria were a documented keratoconus and refractive error higher than 2 diopters and corneal thickness more than 400 microns. Patients with systemic diseases such as collagen vascular disease and poor compliance were excluded from the study [Figure 1].
Figure 1.
Consort flow chart
At baseline and 6 months after surgery all patients underwent visual acuity assessment, refractive error assessment and keratometeric and topographic evaluation.
Visual acuity was assessed by Snellen chart. Keratometeric criteria were measured by Pentacam anterior SimK. Topographic criteria were assessed by Pentacam Scheimpflug imagery. Patients were randomly divided into two groups, one of which underwent accelerated collagen cross-linking (18 mW/cm2 for 5 min) and the other underwent conventional collagen cross-linking (3 m W/cm2 for 30 min). Visual acuity, keratometric criteria and topographic criteria were assessed after 6 months.
Statistical analysis was performed with statistical software Statistical Package for the Social Sciences (SPSS®) version 18.0 software package (SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. SPSS Inc., Chicago, USA). All data are reported as mean ± standard deviation. Comparisons were performed using Student t-test. The level of statistical significance was set at P < 0.05.
Results
In this study we assessed 40 patients in two groups. Mean age of patients in the accelerated group was 22.10 and in the conventional group was 22.80 years which showed no significant difference (P = 0.41).
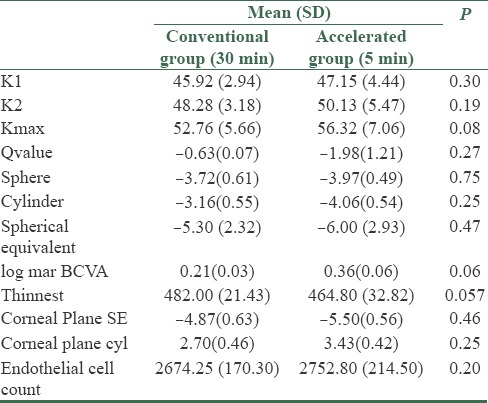
Our results manifested no significant difference between visual acuity, keratometric criteria and topographic criteria in the two groups before intervention. All pre-intervention data are summarized in Table 1.
Table 1.
Preoperational variables in two groups
Also, our results manifested no significant difference between visual acuity, keratometric criteria, refractive criteria and topographic criteria after intervention. All postoperative data are summarized in Table 2.
Table 2.
Postoperative variables in the two groups
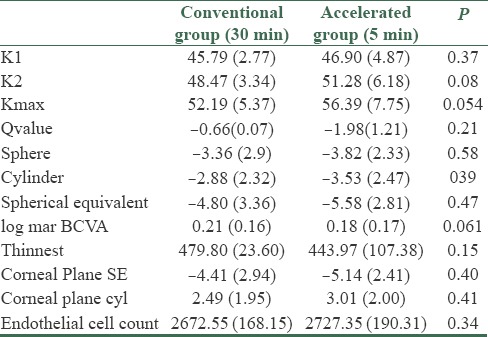
Mean ± standard error of log mar BCVA after collagen cross-linking in conventional and accelerated groups were 0.21 ± 0.03 and 0.36 ± 0.06 respectively, and there was no significant difference between them (P = 0.06).
Mean ± standard deviation of flattest K after collagen cross-linking in conventional group (30 min) was 45.79 ± 2.77 and in accelerated group (5 min) was 46.90 ± 4.87. Mean ± standard deviation of Steepest K was 48.47 ± 3.34 in conventional group (30 min) and in accelerated group (5 min) it was 51.28 ± 6.18. Mean ± SD of Kmax were 52.19 ± 5.37 and 56.39 ± 7.75 in conventional and accelerated groups, respectively. There was no significant difference between K1, K2 and Kmax in the two groups (P = 0.37, 0.08 and 0.054).
The mean ± SD of spherical equivalent was -4.80 ± 3.36 D, with a mean ± SD sphere of -3.36 ± 2.9 and mean ± SD of cylinder was -2.88 ± 2.32 in the conventional group and mean ± SD of spherical equivalent was -5.58 ± 2.85, with a mean ± SD sphere of -3.82 ± 2.33 and mean ± SD cylinder of -3.53 ± 2.47 in the accelerated group. We found no significant difference between spherical equivalents in the two groups (P value = 0.43).
Discussion
Keratoconus (KC) is a progressive degenerative disorder of the cornea in which structural changes in the cornea cause it to become thin and conical in shape. There are some therapeutic options for keratoconus including intrastromal implants, intraocular lenses, microwave remodeling and anterior lamellar keratoplasty.[11,12,13] The use of collagen corneal cross-linking (CXL) with riboflavin and ultraviolet (UV) has rapidly expanded in the world and is currently regarded as the only recognized treatment to slow or arrest KC progression, obtaining in some cases a significant improvement of corneal curvature and regularity.[2,4]
Efficacy of CXL in treatment of progressive keratoconus has been proved in lots of studies. Vinciguerra et al.,[2] have reported refractive, topographic, aberrometric, and tomographic outcomes 24 months after corneal cross-linking (CXL) in patients up to 18 years of age with progressive keratoconus. In their study 40 eyes underwent riboflavin-ultraviolet A-induced CXL and they reported that CXL improved uncorrected and best corrected visual acuity in studied patients, most likely by significantly reducing corneal asymmetry as well as total wave front aberrations. Wittiq-silva et al.,[3] in a prospective, randomized, control trial evaluated the efficacy and safety of collagen cross-linking in the management of progressive keratoconus. They enrolled 66 eyes of 49 patients with documented progressive keratoconus in their study and their results suggested temporary stabilization of all treated eyes after CXL. Caporossi et al.,[14] reported long-term results of 44 keratoconic eyes treated by collagen cross-linking. Their results showed a long-term stability of keratoconus after cross-linking without relevant side-effects. Agrawal[15] in a retrospective study assessed corneal collagen cross-linking for keratoconus in a one-year period. In this study 68 eyes were observed after CXL procedure for 12–16 months and the obtained results suggested CXL as an effective treatment for progressive keratoconus. Likewise Mencucci et al.,[16] in their study evaluated the safety and efficacy of collagen cross-linking as a parasurgical treatment of keratoconus and concluded that this procedure is safe and effective for stiffening of the cornea.
All these studies corroborated the fact that CXL is a safe and efficient option for keratoconus treatment but to the best of our knowledge there are few studies which have compared new techniques of collagen cross-linking with traditional ones.[17] Touboul et al.,[7] in their study compared early healing of cornea after accelerated, conventional and transepithelial collagen cross-linking protocols. In their study 24 patients with progressive keratoconus were divided into three groups to receive accelerated, transepithelial and conventional CXL. Corneal confocal microscopy was performed on each patient preoperatively and 1, 3 and 6 months postoperatively. Their results showed that accelerated CXL had a greater impact than conventional CXL on the anterior cornea, whereas transepithelial CXL did not appear to alter corneal morphology.
Our results show that there is no significant difference in visual acuity, refractive criteria and topographic criteria in keratoconic eyes after 6 months of follow-up (P > 0.05). To date, lots of studies have concluded that conventional (30 min) CXL has a great effect on the progression of keratoconus and it is accepted as a safe and efficient method in the management of keratoconus.
Conclusion
Our results manifested that the accelerated technique did not make significant difference in the improvement of visual acuity, refractive errors and topographic criteria of keratoconic eyes after 6 months of follow-up. Considering that the accelerated method has some advantages like better fluency of work in the ward with shorter duration of surgery, it can be suggested as a better option than the conventional method with the same therapeutic results.
Financial support and sponsorship
This work accomplished with support of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kanellopoulos AJ, Binder PS. Collagen cross-linking (CCL) with sequential topography-guided PRK: A temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007;26:891–5. doi: 10.1097/ICO.0b013e318074e424. [DOI] [PubMed] [Google Scholar]
- 2.Vinciguerra P, Albé E, Frueh BE, Trazza S, Epstein D. Two-year corneal cross-linking results in patients younger than 18 years with documented progressive keratoconus. Am J Ophthalmol. 2012;154:520–6. doi: 10.1016/j.ajo.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: Preliminary results. J Refract Surg. 2008;24:S720–5. doi: 10.3928/1081597X-20080901-15. [DOI] [PubMed] [Google Scholar]
- 4.Wollensak G. Crosslinking treatment of progressive keratoconus: New hope. Curr Opin Ophthalmol. 2006;17:356–60. doi: 10.1097/01.icu.0000233954.86723.25. [DOI] [PubMed] [Google Scholar]
- 5.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A–induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 6.Vega-Estrada A, Alió JL, Plaza Puche AB, Marshall J. Outcomes of a new microwave procedure followed by accelerated cross-linking for the treatment of keratoconus: A pilot study. J Refract Surg. 2012;28:787–93. doi: 10.3928/1081597X-20121011-07. [DOI] [PubMed] [Google Scholar]
- 7.Touboul D, Efron N, Smadja D, Praud D, Malet F, Colin J. Corneal confocal microscopy following conventional, transepithelial, and accelerated corneal collagen cross-linking procedures for keratoconus. J Refract Surg. 2012;28:769–76. doi: 10.3928/1081597X-20121016-01. [DOI] [PubMed] [Google Scholar]
- 8.Matalia H, Shetty R, Dhamodaran K, Subramani M, Arokiaraj V, Das D. Potential apoptotic effect of ultraviolet-A irradiation during cross-linking: A study on ex vivo cultivated limbal epithelial cells. Br J Ophthalmol. 2012;96:1339–45. doi: 10.1136/bjophthalmol-2012-301811. [DOI] [PubMed] [Google Scholar]
- 9.Tamayo GE. Predictable visual outcomes with accelerated corneal cross-linking concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012;38:2206. doi: 10.1016/j.jcrs.2012.10.023. [DOI] [PubMed] [Google Scholar]
- 10.Real LP, Rocha AP, Gardette JL. Artificial accelerated weathering of poly (vinyl chloride) for outdoor applications: The evolution of the mechanical and molecular properties. Polym Degrad Stab. 2003;82:235–43. [Google Scholar]
- 11.Ghanem RC, Netto MV, Ghanem VC, Santhiago MR, Wilson SE. Peripheral sterile corneal ring infiltrate after riboflavin-UVA collagen cross-linking in keratoconus. Cornea. 2012;31:702–5. doi: 10.1097/ICO.0b013e318226da53. [DOI] [PubMed] [Google Scholar]
- 12.Henriquez MA, Izquierdo L, Jr, Bernilla C, Zakrzewski PA, Mannis M. Riboflavin/Ultraviolet a corneal collagen cross-linking for the treatment of keratoconus: Visual outcomes and Scheimpflug analysis. Cornea. 2011;30:281–6. doi: 10.1097/ICO.0b013e3181eeaea1. [DOI] [PubMed] [Google Scholar]
- 13.Hovakimyan M, Guthoff R, Knappe S, Zhivov A, Wree A, Krüger A, et al. Short-term corneal response to cross-linking in rabbit eyes assessed by in vivo confocal laser scanning microscopy and histology. Cornea. 2011;30:196–203. doi: 10.1097/ICO.0b013e3181e16d93. [DOI] [PubMed] [Google Scholar]
- 14.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: The Siena eye cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Agrawal VB. Corneal collagen cross-linking with riboflavin and ultraviolet-A light for keratoconus: Results in Indian eyes. Indian J Ophthalmol. 2009;57:111–4. doi: 10.4103/0301-4738.44515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mencucci R, Paladini I. Corneal cross-linking for keratoconus. Acta Ophthalmologica. 2008:86. [Google Scholar]
- 17.Celik HU, Alagöz N, Yildirim Y, Agca A, Marshall J, Demirok A, et al. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012;38:1424–31. doi: 10.1016/j.jcrs.2012.03.034. [DOI] [PubMed] [Google Scholar]