Abstract
Background:
The prosthetic treatment in cleft patients is challenging. Based on this, the aim of this study was to evaluate the longevity of prosthetic rehabilitation treatment with implant-supported overdenture (IOD) and implant-supported fixed denture (IFD) in cleft lip and palate patients in a period of 22 years.
Materials and Methods:
The medical records of 72 patients were analyzed (29 males and 43 females), and the survival rate of the implants was evaluated. Moreover, the prostheses’ time of use and the reason for the changing of these were also evaluated.
Results:
Four-hundred-seventeen implants were installed, and 370 implants survive today. The mean survival time of the implants was 7.6 years. Regarding the 97 prostheses made, the time of average use was 3.28 for the IFDs and 3.92 for IODs. The reasons for the replacements of the prostheses were mainly: fracture of the acrylic base (29.6%) and loss of vertical dimension of occlusion (VDO) (18.5%) in the IFDs. Moreover, in IODs, these were accounted for the loss of VDO due to teeth damage (17.2%) and implant loss (14.6%).
Conclusions:
The maintenance of the prostheses was challenging because the patients had difficulties returning for periodic control, but this fact did not result in the decrease of the success rate of the implants. The longevity of implants and prostheses was satisfactory; however, the prostheses showed repetitions mainly due to the wear of the teeth, with decreased vertical dimension and fracture of acrylic base.
Keywords: Cleft lip, cleft palate, dental prosthesis, denture complete, implant-supported
INTRODUCTION
The oral rehabilitation of the patient with cleft depends of the type and extent of craniofacial anomalies, requiring a multi- and interdisciplinary treatment protocol, starting from 1st days of life to adulthood. This process is of utmost importance to restore functional and esthetic characteristics in addition to reintegrate patient into society, which implies psychosocial aspects. The oral rehabilitation of these patients usually culminates in the installation of dental prostheses, which is one of the last stages of treatment.[1]
The full dentures over implants came as a treatment alternative to conventional dentures since the prosthetic rehabilitation with implant-supported overdenture (IOD) and implant-supported fixed denture (IFD) is, in some situations, the only option in edentulous patients with cleft lip and palate, since it has better retention and stability and masticatory efficiency compared to conventional dentures.[2,3,4]
Thus, there are improvements in the function of speech which positively influence the quality of life of these patients.[5,6] However, to prescribe dental implants, it is imperative to evaluate the biological and mechanical aspects. There are borderline cases of patients with cleft, due to inadequate procedures done early, and for this, the correct treatment is impaired and/or unfeasible.
The position of the implants, at the moment of installing, is not always favorable, due to the lack of bone or aspects associated with clefts, making it difficult to make the prosthesis. And so, there may be functional overload leading to abutments and prosthesis fracture and problems with prosthetic implants.
Factors such as the length of the cleft, maxillomandibular relationship, and extent of bone grafts are decisive for the placement and positioning of implants and consequently the type of prosthesis to be prescribed.[7] Such limitations can change the plan of treatment or even not prescribe.
IOD is the best indication if the patient has insufficient support lip, high smile line, or when prognathic appearance needs to be compensated.[8] According to Agustín-Panadero et al., IODs should be prescribed in patients with less motivation for oral hygiene and fully or partially reduced motor coordination, considering that they are easier to clean than IFD, which requires more complex procedures for cleaning.[9]
The IFD requires more bone because more implants are installed; however, comparing this treatment modality with IOD, patient satisfaction and oral health-related quality of life improved significantly in both types of treatment.
In relation to the preservation of IOD, irrespective of their retention, the longevity may be decreased by various factors such as: loss of retention, occlusal adjustments, loosening and fracture of the abutments and screws, fractures of the acrylic resin teeth, fracture in system of retention of the prosthesis, hyperplasia of soft tissue, bone loss surrounding implant, and loss of the implant.[4,10] It is also associated with failures of these prostheses fractures of the bar and/or clips. The long-term monitoring and proper maintenance should be made an essential part of any prosthetic rehabilitation.[11]
As the patient's cleft's rehabilitation process is complex and extensive, beginning from birth to adulthood, planning should be done in a very detailed way, ensuring patient satisfaction, and efficiency of the rehabilitation treatment. Thus, the aim of this study was to evaluate during 22 years the longevity and durability of implants and rehabilitation prosthetic treatment with IODs and IFDs in patients with cleft in the Hospital of Rehabilitation of Craniofacial Anomalies (HRAC)/University of São Paulo.
MATERIALS AND METHODS
Between the years 1991–2013, with a maximum period of observation of 22 years and a minimum of 5 months, the information of 72 medical records of patients from HRAC was analyzed, totalizing 52 IODs (34 uppers and 18 lowers), 44 IFDs (16 uppers and 28 lowers), and 1 upper IOD changed for IFD. The average age of patients was 52.8 years with ranging from 23 to 78 years, of those 29 participants were male and 43 female. The types of cleft were evaluated: unilateral cleft (47) and bilateral (25).
Patients were randomly selected and included only if used IOD [Figure 1] or IFD [Figure 2].
Figure 1.
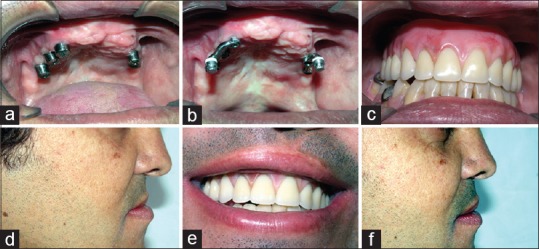
(a) Implants and healing caps; (b) bar and clips ready for capture; (c) implant-supported overdenture installed and occlusal vertical dimension reestablished; (d) patient's profile without implant supported overdenture; (e) patient's smile; (f) relationship between implant-supported overdenture and upper lip
Figure 2.

(a) Postoperative orthopantomogram; (b) occlusal relationship upper and lower implant-supported fixed denture; (c) Postoperative picture
The data concerning the 97 prostheses, 52 IODs and 44 IFDs and 1 prosthesis, which was initially upper IOD becoming IFD, were collected and evaluated the reason for the replacement of these prostheses. Radiographic images were used to assist in filling out the evaluation form. Date of implant placement, number of implants placed, number of lost implants, date of installation of the prosthesis, the prosthesis change, how many times the dentures were changed, and the reason for replacement were recorded and transformed in tabulated data.
The analysis of the results was done descriptively, and the interpretation through percentage was by comparing the collected data. The results were then organized into graphics for better assessment and analysis.
RESULTS
A total of 417 implants were placed, 370 survived until this date, 47 implants were lost (10 IFDs and 37 IODs), resulting in a rate of 88.7% successful implants, and 11.3% failed. The average survival implants period was 7.10 years for IFDs and 7.78 years for IODs [Chart 1] (showing the shortest period of 5 months and the largest of 22 years).
Chart 1.
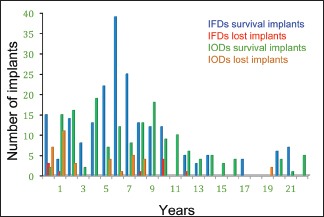
Implants quantity and survival period in years in the evaluated rehabilitation types
In relation to the 97 prostheses installed, only 12 were unchanged since their first installation, the remaining 85 prostheses had to be replaced, some of them more than once, but the retrospective review period was 22 years. Chart 2 shows the amount of changes of prostheses, according to the treatments.
Chart 2.
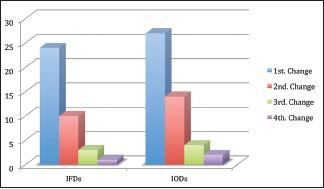
Quantity of changed prostheses during the evaluated treatments
The reasons for the prostheses replacements are displayed in Chart 3.
Chart 3.
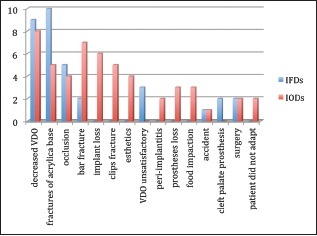
Reasons the prostheses replacement
DISCUSSION
This retrospective study evaluated the prosthetic rehabilitation treatment using IODs and IFDs in 72 patients (29 male and 43 female, mean age 52.8 years) from the beginning of the first implant placement by Professor Branemark in 1991, by the year 2013, and a follow-up since then with these prostheses and implants in the observation period (22 years).
The present study showed implants survival rate of 88.46% (n = 370), without considering the fact that these implants were installed in the maxilla or mandible. Maybe this is a bias for the present research, but it has been considered that cleft patients have problems with hygiene in general, irrespect if the prosthesis is in maxilla or mandible. Other authors[12] evaluated the cumulative rate of implants, in noncleft patients, for a period of time from 10 to 24 years with results of 85.9%, and Turkylmaz and Tözum followed at 20 years, 28 implants (lower protocol) and found 100% success rate.[13]
It was installed 44 IFDs and 52 IODs, and the implant survival rate was 207 (95.39%) for the IFDs and 163 (81.5%) for IODs. Attard and Zarb observed values of 87% for IFDs[14] and IODs rates that were higher than 90%.[15] Aykent et al. also evaluated the survival rate and cumulative success of implants after 12 years finding 95.2% values for the IFDs and 90.2% for IODs.[16] Conversely, Widbom et al. concluded in a study of IODs (n = 13) and IFDs (n = 14), a follow-up of an average of 5.7 years and 5.5 years, respectively; the cumulative survival of the implants was 77% for IODs and 46% for IFDs, and the probability of having implant failure was 3 times higher in IFDs than IODs.[17]
The quantity of implants lost was 10 and 37 IFDs and IODs, respectively. Most implants (48.9%) were lost until the 1st year after installation. Other studies have also reported that the implants failures tended to happen in the 1st year after installation.[18,19,20] The failures that culminated to implants loss occurred for other reasons and not by infection or peri-implantitis. According to the study of Ueda et al., an individual analysis of the lost implants did not show a typical failure pattern, but the loss of osseointegration without signs of infection was more frequent than peri-implantitis.[12]
According to Widbom et al., most technical and biological complications are related to retention system.[17] It was suggested that the IOD occlusal load is distributed more favorably when the implants are immobilized using a rigid bar compared to separated implants using the ball system.[21] However, Bressan et al. observed that patients treated with IOD bar system presented a most common complication hyperplasia of mucosal tissue under the bar, and few patients complained of retention loss.[22] Cune et al. found no significant difference in patient satisfaction but clinically verified the probing depth around the implants higher in the bar–clip system after 10 years in relation to the ball system.[23]
This retrospective study noted fracture related to components [Chart 3] in IODs (n = 5), problems that would be easily remedied if the patients systematically returned for further controls. Nevertheless, this return was not observed, considering the patients live in remote locations, return to service only when the problem is lodged and the need for repair is no longer viable, due to this, a large amount of prostheses replacement was made over 22 years. It was not evaluated in this study how many and which IODs were made with the retention system type, ball or clip–bar.
In a study by Nedir et al., overdentures retained by bar/clip had a significantly lower rate of complications compared with the retained by o-rings or ball system (42.9% vs. 77.5%, respectively). In that same study, the authors compared the fixed partial dentures (n = 265) and overdentures (n = 55) on implants and found that patients with overdenture had more complications than patients using fixed partial denture, 66% and 11.5%, respectively.[24] The incidents recurred with overdentures and the complication rate did not decrease with time. In absolute numbers, overdentures (47) required more replacements than FPDs (38). For patients with cleft, this ideal type of planning is not always possible because these patients have not sufficient amount of bone to install a larger quantity of implants, and there is often no interocclusal space to prescribe the bar–clip system for both IODs and IFDs.
The average duration of prostheses evaluated in this study was 3.92 years for IODs and 3.28 years for IFDs. The reasons most frequently reported in this research for the replacement of the prostheses were: loss of vertical dimension of occlusion (VDO) (17) and fracture of the acrylic base (15). The other reasons for the replacements were: occlusion (9 in total, 5 IFDs and 4 IODs), bar fracture (7 in total, 2 IFDs and 5 IODs), loss of implant (6 IODs), and esthetics (4 IODs).
There are few studies in the literature reporting the loss or replacement of IODs and IFDs. However, studies reporting intercurrences in these types of prostheses are displayed more frequently. Widbom et al. observed that for a total number of 13 IODs and 14 IFDs, 3 IODs and 2 IFDs presented teeth fracture and 5 IODs and 12 IFDs, acrylic-based fracture. The authors found that most biological and technical problems were related with retention system.[17]
Kuoppala et al. when evaluating IOD (48 with bar–clip system and 10 with ball system) for a period of 19 years found that the most frequent technical problems were loosening of the retaining mechanism (39.7%) and fracture of the base (5.2%). In that same study, 19 patients (32.8%) had the prosthesis redone, and 39 patients (67.2%) were still using the original overdentures (the oldest over 20 years).[25] Turkylmaz and Tözum evaluated mandibular IFDs for 20 years and observed 80% success rate with 21 repairs performed with replacement of artificial teeth, gold screw, and 19 settings including occlusal and the resin outline.[13]
In this investigation, there were cases involving the retention system (5 IODs) that would have been easily solved if patients followed faithfully the subsequent controls. What was clearly seen was that due to continental size of the country, coupled with the free care from the referral center, there was the difficulty of periodic returns, which could be solved by decentralization of care.
In the Bozini et al., meta-analysis, the values observed after 15 years were: acrylic base fracture, esthetics deficiency, and wear of the material where 8.8%, 9%, and 43.5%, respectively, in IFD in edentulous patients. It was observed, in this analysis, complications due to wear of the material with loss of VDO and fracture acrylic base, in IFDs and IODs. The damage of the element is mainly because of the wear of the teeth that keeps VDO (9 IFDs and 8 IODs) and the wear of the material invariably leads to fracture of the acrylic base (10 IFDs and 5 IODs).[26] However, it should be noted that the retrospective study did not assess the antagonist that is directly related to the longevity of the teeth and hence to the prosthesis.
Complications associated to the screws are commonly reported in the literature. Regardless of their design, the screw of the implants is susceptible to loosening or fracture because of the magnitude and direction of the strengths and limitations of the components. Several factors may contribute to these complications: inadequate preload screws, overload and parafunction, occlusal interferences, and extremely long cantilevers.[27,28] According to a study done by De Kok et al., prosthetic complications were rare and easy to handle when evaluated IODs and IFD in edentulous patients.[6] Dental adjustments occurred in 83.33% of the prostheses, loosening of the ball abutment system was 3.03%, loosening of the prosthetic screw 1.52%, and repair of the prosthesis teeth 4.55%.
This study noted that tooth wear acrylic resin (n = 17) carries out decrease in the occlusal vertical dimension and subsequent manufacture of new prosthesis, problem also reported by Aykent et al. in 6 overdentures for a total of 12.[16] They found the fracture components (n = 4), complication observed exclusively in overdentures.
CONCLUSIONS
The longevity of the prostheses IODs and IFDs as well as the survival rate of the implants in individuals with clefts is satisfactory and comparable to values found in literature.
Dentures are replaced mainly because patients do not regularly return to periodic inspections and return when the problem is already installed without being able to solve it only with replacement components or changing of the teeth, yet this fact did not result in decreased success of the prostheses and implants compared to other studies.
The quality of acrylic resin teeth is low if they were more resistant the longevity of the prostheses would be higher.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Freitas JA, Almeida AL, Soares S, Neves LT, Garib DG, Trindade-Suedam IK, et al. Rehabilitative treatment of cleft lip and palate: Experience of the Hospital for Rehabilitation of Craniofacial Anomalies/USP (HRAC/USP)-Part 4: Oral rehabilitation. J Appl Oral Sci. 2013;21:284–92. doi: 10.1590/1679-775720130127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hakan Tuna S, Pekkan G, Buyukgural B. Rehabilitation of an edentulous cleft lip and palate patient with a soft palate defect using a bar-retained, implant-supported speech-aid prosthesis: A clinical report. Cleft Palate Craniofac J. 2009;46:97–102. doi: 10.1597/07-216.1. [DOI] [PubMed] [Google Scholar]
- 3.Preciado A, Del Río J, Suárez-García MJ, Montero J, Lynch CD, Castillo-Oyagüe R. Differences in impact of patient and prosthetic characteristics on oral health-related quality of life among implant-retained overdenture wearers. J Dent. 2012;40:857–65. doi: 10.1016/j.jdent.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Vere J, Bhakta S, Patel R. Implant-retained overdentures: A review. Dent Update. 2012;39:370–2. doi: 10.12968/denu.2012.39.5.370. 374-5. [DOI] [PubMed] [Google Scholar]
- 5.Brennan M, Houston F, O’Sullivan M, O’Connell B. Patient satisfaction and oral health-related quality of life outcomes of implant overdentures and fixed complete dentures. Int J Oral Maxillofac Implants. 2010;25:791–800. [PubMed] [Google Scholar]
- 6.De Kok IJ, Chang KH, Lu TS, Cooper LF. Comparison of three-implant-supported fixed dentures and two-implant-retained overdentures in the edentulous mandible: A pilot study of treatment efficacy and patient satisfaction. Int J Oral Maxillofac Implants. 2011;26:415–26. [PubMed] [Google Scholar]
- 7.Murat S, Gurbuz A, Genc F. Prosthetic rehabilitation of a patient with bilateral cleft lip and palate using osseointegrated implants and extracoronal resilient attachments: A case report. Cleft Palate Craniofac J. 2011;48:342–7. doi: 10.1597/09-248. [DOI] [PubMed] [Google Scholar]
- 8.Zitzmann NU, Marinello CP. Treatment plan for restoring the edentulous maxilla with implant-supported restorations: Removable overdenture versus fixed partial denture design. J Prosthet Dent. 1999;82:188–96. doi: 10.1016/s0022-3913(99)70155-1. [DOI] [PubMed] [Google Scholar]
- 9.Agustín-Panadero R, Peñarrocha-Oltra D, Gomar-Vercher S, Ferreiroa A, Peñarrocha-Diago M. Implant-supported overdenture manufactured using CAD/CAM techniques to achieve horizontal path insertion between the primary and secondary structure: A clinical case report. J Adv Prosthodont. 2015;7:264–70. doi: 10.4047/jap.2015.7.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ELsyad MA. Prosthetic aspects and patient satisfaction with resilient liner and clip attachments for bar- and implant-retained mandibular overdentures: A 3-year randomized clinical study. Int J Prosthodont. 2012;25:148–56. [PubMed] [Google Scholar]
- 11.Ramstad T. Long-term prosthodontic follow-up and revisional treatment of patients with cleft lip and palate: Case presentation. Int J Prosthodont. 2001;14:417–22. [PubMed] [Google Scholar]
- 12.Ueda T, Kremer U, Katsoulis J, Mericske-Stern R. Long-term results of mandibular implants supporting an overdenture: Implant survival, failures, and crestal bone level changes. Int J Oral Maxillofac Implants. 2011;26:365–72. [PubMed] [Google Scholar]
- 13.Turkyilmaz I, Tözüm TF. 30-year outcomes of dental implants supporting mandibular fixed dental prostheses: A retrospective review of 4 cases. Implant Dent. 2015;24:620–4. doi: 10.1097/ID.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 14.Attard NJ, Zarb GA. Long-term treatment outcomes in edentulous patients with implant-fixed prostheses: The Toronto study. Int J Prosthodont. 2004;17:417–24. [PubMed] [Google Scholar]
- 15.Attard NJ, Zarb GA. Long-term treatment outcomes in edentulous patients with implant overdentures: The Toronto study. Int J Prosthodont. 2004;17:425–33. [PubMed] [Google Scholar]
- 16.Aykent F, Inan O, Ozyesil AG, Alptekin NO. A 1- to 12-year clinical evaluation of 106 endosseous implants supporting fixed and removable prostheses. Int J Periodontics Restorative Dent. 2007;27:358–67. [PubMed] [Google Scholar]
- 17.Widbom C, Söderfeldt B, Kronström M. A retrospective evaluation of treatments with implant-supported maxillary overdentures. Clin Implant Dent Relat Res. 2005;7:166–72. doi: 10.1111/j.1708-8208.2005.tb00061.x. [DOI] [PubMed] [Google Scholar]
- 18.Naert IE, Hooghe M, Quirynen M, van Steenberghe D. The reliability of implant-retained hinging overdentures for the fully edentulous mandible. An up to 9-year longitudinal study. Clin Oral Investig. 1997;1:119–24. doi: 10.1007/s007840050022. [DOI] [PubMed] [Google Scholar]
- 19.Jemt T, Johansson J. Implant treatment in the edentulous maxillae: A 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin Implant Dent Relat Res. 2006;8:61–9. doi: 10.1111/j.1708-8208.2006.00003.x. [DOI] [PubMed] [Google Scholar]
- 20.Koldsland OC, Scheie AA, Aass AM. Prevalence of implant loss and the influence of associated factors. J Periodontol. 2009;80:1069–75. doi: 10.1902/jop.2009.080594. [DOI] [PubMed] [Google Scholar]
- 21.Walton JN. A randomized clinical trial comparing two mandibular implant overdenture designs: 3-year prosthetic outcomes using a six-field protocol. Int J Prosthodont. 2003;16:255–60. [PubMed] [Google Scholar]
- 22.Bressan E, Tomasi C, Stellini E, Sivolella S, Favero G, Berglundh T. Implant-supported mandibular overdentures: A cross-sectional study. Clin Oral Implants Res. 2012;23:814–9. doi: 10.1111/j.1600-0501.2011.02225.x. [DOI] [PubMed] [Google Scholar]
- 23.Cune M, Burgers M, van Kampen F, de Putter C, van der Bilt A. Mandibular overdentures retained by two implants: 10-year results from a crossover clinical trial comparing ball-socket and bar-clip attachments. Int J Prosthodont. 2010;23:310–7. [PubMed] [Google Scholar]
- 24.Nedir R, Bischof M, Szmukler-Moncler S, Belser UC, Samson J. Prosthetic complications with dental implants: From an up-to-8-year experience in private practice. Int J Oral Maxillofac Implants. 2006;21:919–28. [PubMed] [Google Scholar]
- 25.Kuoppala R, Näpänkangas R, Raustia A. Outcome of implant-supported overdenture treatment – A survey of 58 patients. Gerodontology. 2012;29:e577–84. doi: 10.1111/j.1741-2358.2011.00524.x. [DOI] [PubMed] [Google Scholar]
- 26.Bozini T, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofac Implants. 2011;26:304–18. [PubMed] [Google Scholar]
- 27.Duyck J, Van Oosterwyck H, Vander Sloten J, De Cooman M, Puers R, Naert I. Magnitude and distribution of occlusal forces on oral implants supporting fixed prostheses: An in vivo study. Clin Oral Implants Res. 2000;11:465–75. doi: 10.1034/j.1600-0501.2000.011005465.x. [DOI] [PubMed] [Google Scholar]
- 28.Sahin S, Cehreli MC, Yalçin E. The influence of functional forces on the biomechanics of implant-supported prostheses – A review. J Dent. 2002;30:271–82. doi: 10.1016/s0300-5712(02)00065-9. [DOI] [PubMed] [Google Scholar]


