Abstract
Background:
One of the most critical and crucial steps in surgical extraction is cutting the bone or osteotomy, for which many techniques are used, e.g., chisels and mallet, rotary instruments, and ultrasound bone-cutting instruments. If they are not used judiciously, they can be hazardous.
Objectives:
To assess the efficiency of piezosurgery unit over micromotor while performing surgical extraction of lower third molars by assessing the time taken for the surgery and measuring postoperative parameters such as pain, trismus, and swelling.
Materials and Methods:
Thirty patients having bilateral impacted third molars with the same difficulty index were selected for the study. One side surgical removal was done using micromotor and other side by piezosurgery with an interval of 15 days. After each surgery, time taken to finish was measured and patients were followed up on postoperative days 1, 3, 5, 7, and 15 for assessing pain, trismus, and swelling. Data obtained were statistically analyzed.
Results:
The mean time taken for the micromotor group is 37.90 min whereas by the piezosurgery group is 54.63 min, showing a statistically significant difference (P < 0.001). Furthermore, there is statistically significant difference (P < 0.001) in the level of pain, trismus, and swelling on postoperative days 1, 3, 5, and 7. Even the intragroup comparison of piezosurgical group for trismus and swelling showed no statistically significant difference on postoperative day 7, indicating faster recovery of trismus and swelling. On postoperative day 15, there was no difference in any parameter in both groups indicating complete symptom-free recovery in both groups.
Conclusion:
It takes more time to perform surgical extraction of third molars when piezosurgical unit is used. Despite that, it causes less pain postoperatively with faster improvement in trismus and quicker reduction in swelling.
Keywords: Extraction, lower third molars, micromotor, odontectomy, pain, piezosurgery, swelling, trismus
INTRODUCTION
Over a period, the scope of oral and maxillofacial surgery has changed leaps and bounds with drastic diversification, but still the mainstay of practice remains dentoalveolar surgery.
Surgical extraction of lower third molar is one of the most common minor oral surgical procedures practiced in oral and maxillofacial surgery on day to day basis.
The credit for rationalizing the technique of surgical extraction of lower third molars goes to Dr. George B. Winter. He also coined the term “Exodontia” which was the title of his first publication which appeared in “Dental Items of Interest” way back in 1913. He later came out with a second edition in 1926 which was the most extensive treatise on the case with profuse illustration under the title “The Impacted Mandibular Third Molar.”
Surgical extraction of lower third molar may range from relatively easy to extremely difficult depending on various factors, for example, the location of the tooth that is its depth from the crystal bone as well as its location in relation to distal surface of the second molar and ascending border of the mandibular ramus, its angulation in relation to the second molar, and the density of the bone.[1]
The odontectomy of impacted mandibular third molars produces a great degree of injury to the soft tissues as well as to the bony structures of the oral cavity, which significantly results in a potential inflammatory reaction.[2]
This later produces the usual postoperative surgical consequences of pain, edema, and limited mouth opening that is trismus due to muscle spasm.[3]
Several therapeutic protocols have been evaluated to support improvements in the postoperative period and reduce the social cost, namely, preoperative antibiotic administration, use of various flaps, osteotomy by high- or low-speed instrument, primary or secondary closure of the wound, use of postoperative ice pack, postoperative administration of several antibiotics, and use of various steroids systemically as well orally.
One of the most critical and crucial steps in surgical extraction is cutting the bone or osteotomy, for which many techniques are used, and if they are not used judiciously, they can be hazardous.[4]
Rotary cutting instruments are potentially dangerous because they produce a significant rise in temperature during osteotomy, which can produce marginal osteonecrosis and impair regeneration and healing process.[5]
The use of ultrasound methods in oral surgery was first proposed at the end of the 1970s by Horton et al.[6] In the year 2004, a new surgical device “Piezosurgery” (Mectron) was introduced to the oral and craniomaxillofacial surgery developed by Prof. Vercellotti whose concept was inspired from the ultrasonic scalers used in the everyday dental clinics. It differed from the usual scalers in having more oscillating force, thus enabling the surgeon to effectively work on bone and dentin.[7]
Current literature and some studies highly debate the efficiency of the piezosurgery over the conventional micromotor in reducing the postoperative parameters such as pain, swelling, and trismus, and the intraoperative time needed for the bone osteotomy.
The purpose of this comparative analysis is to find out the efficiency of the piezosurgery over the conventional micromotor in reducing the postoperative parameters such as pain, swelling, and trismus. This analysis will also measure the time taken for the entire surgical procedure using conventional micromotor and piezosurgical unit.
MATERIALS AND METHODS
Patients with bilateral impacted mandibular third molars reporting to the Department of Oral and Maxillofacial Surgery of A. B. Shetty Memorial Institute of Dental Sciences, Mangalore, were referred to the radiologist to obtain full-mouth orthopantomogram and two intraoral periapical radiographs with respect to right and left inferior third molars.
Only those patients having same angulation, same depth from the occlusal surface of the adjacent second molar, and the same ramus relation, i.e., same difficulty index bilaterally as described by Pederson[8] in whom bony osteotomy was necessary were selected for the study. Patients having pericoronitis, acute alveolar abscess, oral submucous fibrosis, on antibiotics for any infection, who consumed alcohol or who smoke tobacco and not willing to give consent for the study were excluded from the study. Thirty cases in total were selected for the study.
The grouping of the impacted third molar was done randomly into Group I (Micromotor, Surgic XT Plus, NSK, Japan for bone osteotomy) [Figure 1a and b] and Group II (Piezosurgery Satelec Acteon for bone osteotomy) [Figure 2a and b].
Figure 1.

(a and b) Micromotor which was used for bone osteotomy of Group I
Figure 2.

(a and b) Piezosurgical unit which was used for bone osteotomy of Group II
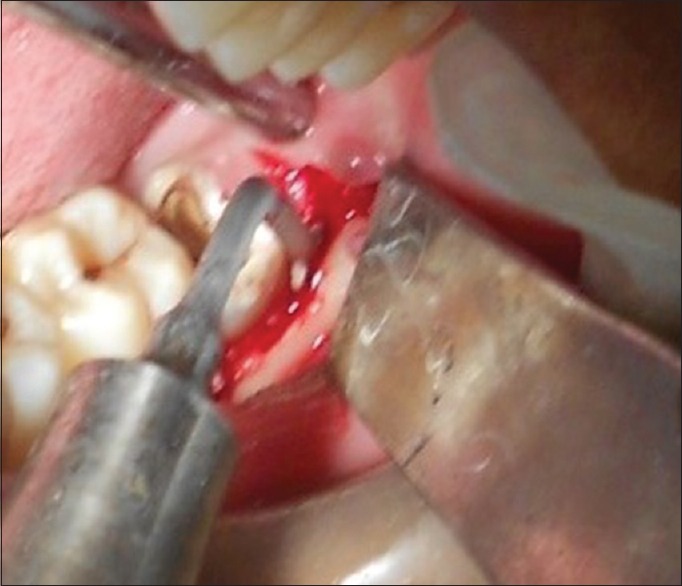
Surgical extraction of third molar on either side was done at an interval of 15 days. All other variables were constant during the surgical procedure, i.e., prior to surgery chlorhexidine mouth rinse was used and patients face was painted with povidone iodine solution, same agent used for local anesthesia (lignocaine 2%), same nerve blocks (inferior alveolar, long buccal, and lingual nerve block), same incision line (modified wards incision),[9] Group I bone osteotomy was done by micromotor [Figure 3] at 35,000 rpm using carbide round bur no. 6 and carbide straight fissure bur no. 702 and Group II bone osteotomy was done by piezosurgical unit [Figure 4] using vibration frequency between 28 and 36 kHz and using piezosurgical tips LC1-90°, LC2 and BS1, tooth sectioning was done by rotary instruments for both the groups, through irrigation was done with saline during bone osteotomy and tooth sectioning, sharp edges of the bone was filed using bone file, thorough curettage of the socket followed by copious irrigation with saline, in both the groups the flap was closed by primary closure using 3-0 black-braided silk suture.
Figure 3.

Osteotomy done by micromotor unit
Figure 4.
Osteotomy done by piezosurgical unit
After the surgical removal of third molars, the patients were given ice pack and were told to apply ice pack every half an hour interval for first 2 days followed by hot fermentation every half an hour interval for next 2 days, with the same list of postoperative instructions, equal number of analgesics (tablet diclofenac 50 mg 1-0-1 for 5 days), antibiotics (capsule amoxicillin 500 mg 1-1-1 for 5 days), and chlorhexidine mouth rinses (Hexidine Mouthwash four times a day for 1 week).
The time taken from the start of incision till the finishing of suture placement was recorded in all the surgical procedures.
After the surgical extraction in each group, follow-up was carried out on postoperative day 1, 3, 5, 7, and 15 to evaluate pain, trismus, and swelling.
Pain was assessed with the help of visual analog scale (VAS)[10] on the scale of 0–10 (0 indicating no pain and 10 indicating worst possible pain) preoperatively, postoperatively just after the surgical procedure is over, and then on postoperative day 1, 3, 5, 7, and 15 in both groups.
Limitation of mouth opening (trismus) was measured as the distance between the mesial incisal corner of the right upper and lower central incisors with the help of metallic scale.[11,12] Measurements were recorded in millimeter unit and were noted preoperatively, postoperatively just after the surgical procedure is over, and then on postoperative day 1, 3, 5, 7, and 15 in both groups.
Swelling was assessed by measuring the distance between two landmarks,[13] the first landmark located in the cutaneous region 2 cm mesial to the mandibular angle and parallel to the ala-tragal line, was marked with a dermatographic pencil to allow repetition of the measurement in the same cutaneous region, postoperatively [Figure 5a] and the second landmark situated on the lingual side of distal trigonum region (5 mm from the distal cuspid of second molar) [Figure 5b]. An autoclaved geometric divider was used to measure the distance between these two landmarks – the distance between the two points on the divider was measured in millimeters on a metallic scale.
Figure 5.
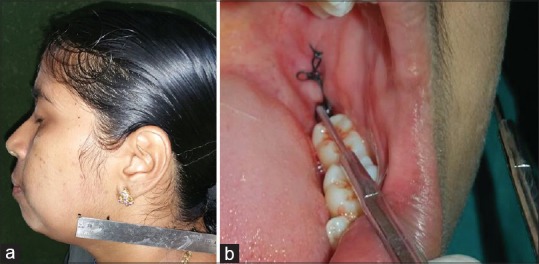
(a) First cutaneous landmark to measure swelling. (b) Second intraoral landmark to measure swelling
The time required for surgical removal of impacted third molars was evaluated using stopwatch from the start of the incision till completion of suturing. Time was measured only in minutes.
The data obtained were tabulated and filled in Microsoft Office Excel spreadsheet and were statistically analyzed. Inter- and intra-group comparison was done using nonparametric test, i.e., Wilcoxon signed-rank test, Friedman test and parametric test, i.e., paired t-test, repeated measures ANOVA.
RESULTS
Table 1 shows the age and gender distribution of the cases who participated in the study.
Table 1.
The demographic data of the study
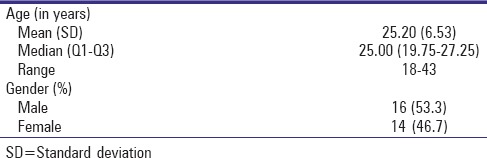
Table 2 shows the comparative results of pain in both study groups. It showed the mean pain of all the thirty cases when they underwent odontectomy with micromotor and piezosurgery, preoperatively, postoperatively, and on the follow-up visits of day 1, 3, 5, 7, and 15. It shows that there is statistically significant less pain in the piezosurgical group as compared to the micromotor group postoperatively and on follow-up visits of day 1, 3, 5, and 7, whereas on the follow-up of day 15, there is no statistical significance in the level of pain in both groups. In fact, patients did not have any pain in both groups on postoperative day 15. The results of pain comparison in both study groups are shown in Figure 6.
Table 2.
Comparing pain in micromotor and piezosurgery group
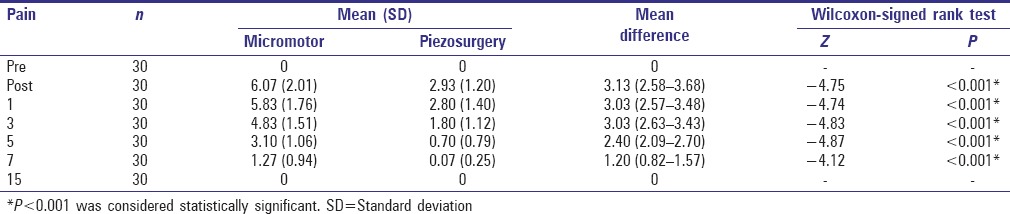
Figure 6.
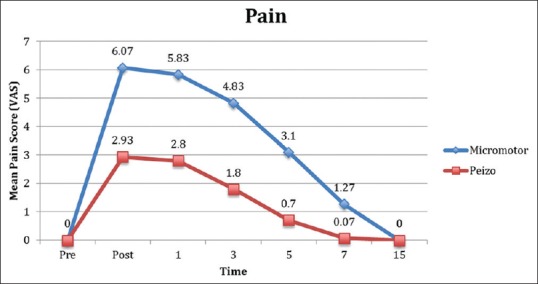
Pain comparison in both study groups
Tables 3 and 4 show the intragroup mean level of pain of the cases keeping the score of preoperative level of pain as the baseline. It showed that there was statistically significant pain postoperatively and on postoperative days 1, 3, 5, and 7 when compared to the pain which the patients had preoperatively, but none of the patients experienced pain preoperatively as the mean value is 0. It also shows that on postoperative day 15, all the patients were pain-free as the mean value is the same as that of preoperative pain score that is 0. It also shows that over a period, as the days pass by after the surgical procedure with micromotor, the pain decreases gradually.
Table 3.
Comparing pain in micromotor group at different follow-up days
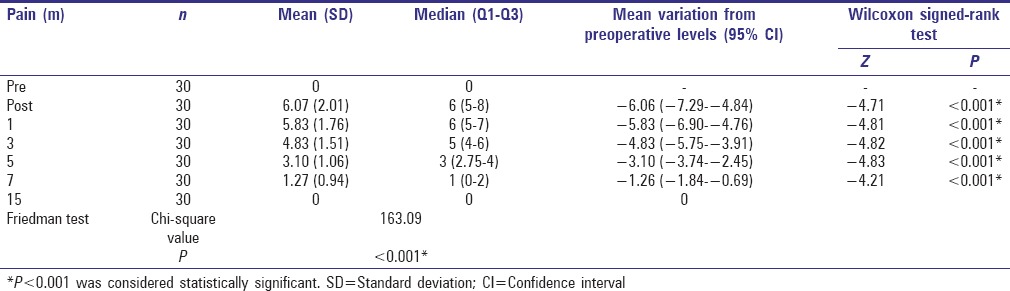
Table 4.
Comparing pain in piezosurgery group at different follow-up days
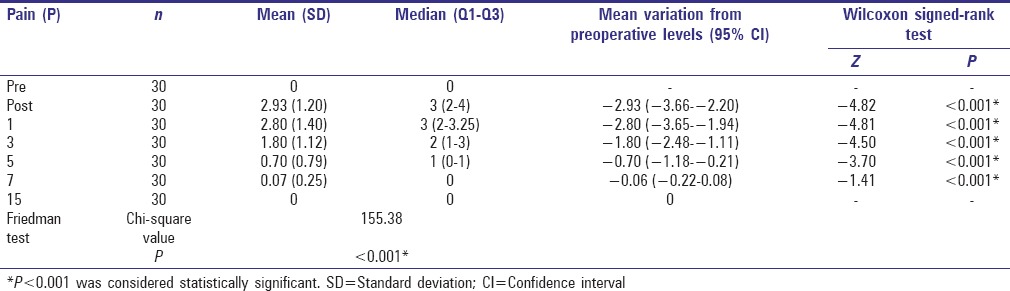
Table 5 and Figure 7 show that the mean mouth opening in both groups before the start of procedure is 45.13 mm; this is because, in both groups, the procedures were performed on the same patients, so the preoperative values before the start of the procedure are the same. Just after finishing the odontectomies in both groups when the mean trismus value was measured, there was no significant difference on comparison in both groups. On postoperative day 1, 3, 5, and 7, when the data were compared statistically using paired t-test, there was a statistically significant difference in the values of both groups, indicating more trismus in the group where osteotomy was performed using micromotor. On postoperative day 15, again, there was no statistical difference in the values of both groups, indicating that the mouth opening has almost become normal in both groups. In both groups, there was maximum trismus on postoperative day 3, and after postoperative day 3, the measurement of mouth opening again increased with time.
Table 5.
Comparing trismus in micromotor and piezosurgery group
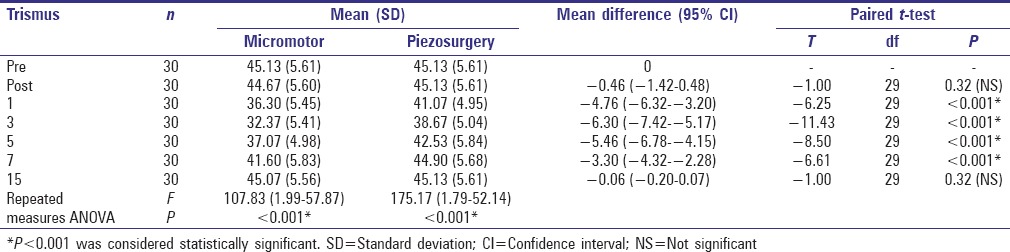
Figure 7.
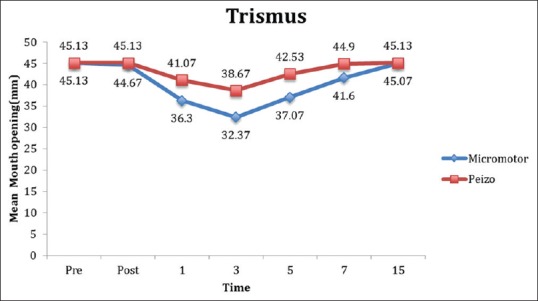
Trismus comparison in both study groups
Table 6 shows the trismus comparison in each respective groups postoperatively and on follow-up visits at day 1, 3, 5, 7, and 15, with the baseline trismus value preoperatively, which is same in both groups. When comparison was done in micromotor group, it showed that statistical significant trismus was present on postoperative day 1, 3, 5, and 7, whereas in piezosurgical group, it showed that statistical significant trismus was present on postoperative day 1, 3, and 5 only. Thus, there is faster trismus recovery in the piezosurgical group as compared to the micromotor group.
Table 6.
Intragroup comparison of trismus status in micromotor and piezosurgery groups
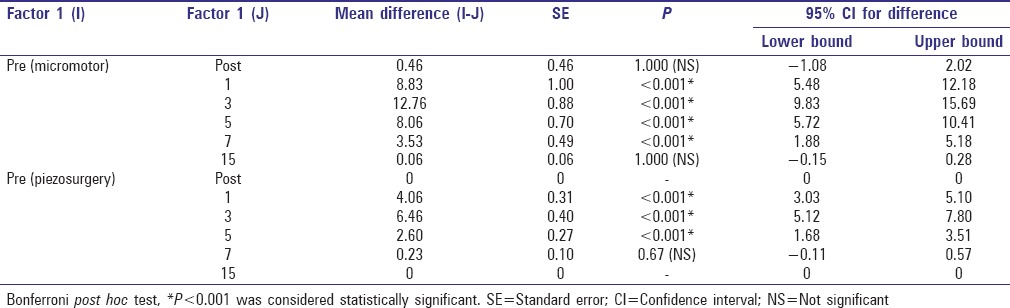
Table 7 and Figure 8 show the comparison of the mean reading of swelling obtained from both groups. As the cases are same, their preoperative value obtained in both groups is same that is 39.90 mm. A statistical significant difference in the measurements of swellings was noted on postoperative day 1, 3, 5, and 7. There was not any statistical significance in the swelling on postoperative day 15. In fact, on postoperative day 15, patients’ condition returned to the same as what it was preoperatively. In both groups, patients had maximum measurement for swelling on postoperative day 3 which reduced over the period.
Table 7.
Comparing swelling in micromotor and piezosurgery group
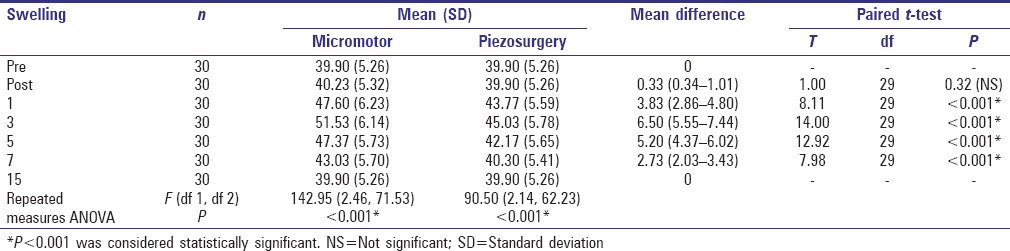
Figure 8.
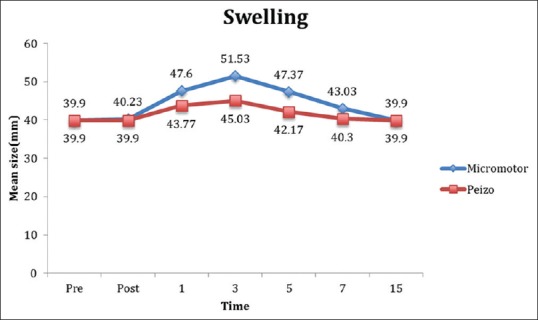
Swelling comparison in both study groups
Table 8 shows the swelling status within their respective groups postoperatively and on follow-ups at postoperative day 1, 3, 5, 7, and 15, with respect to their baseline measurement, which was found preoperatively, which is same in both groups. Within the group, there was statistical significant swelling on postoperative day 1, 3, 5, and 7 as compared to the measurement done preoperatively, whereas in piezosurgery group, there was statistical significant swelling on postoperative day 1, 3, and 5, whereas on day 7, there was no statistical significant difference in swelling as compared to the preoperative measurements, suggesting faster recovery of swelling in piezosurgery group.
Table 8.
Intragroup comparison of swelling status in micromotor and piezosurgery groups
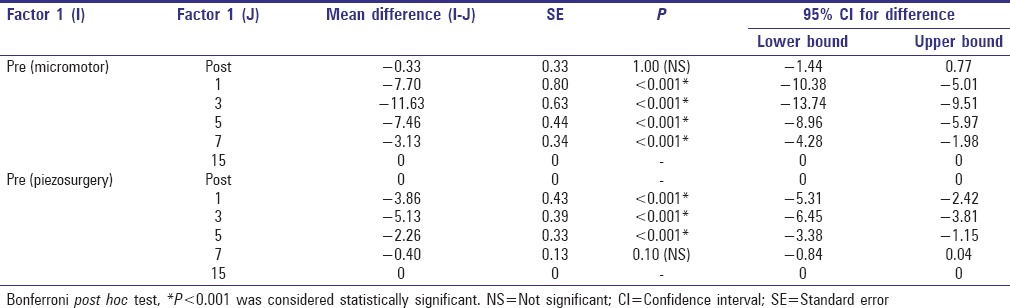
Table 9 and Figure 9 show the mean time taken for both procedures, which clearly shows that there is a statistical difference in the time interval in performing both procedures. The mean time taken for the Group I (micromotor group) is 37.90 min whereas the mean time taken by the Group II (piezosurgery group) is 54.63 min.
Table 9.
Comparing time taken in micromotor and piezosurgery group
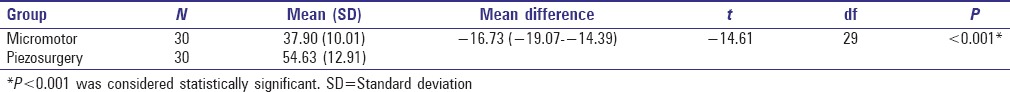
Figure 9.
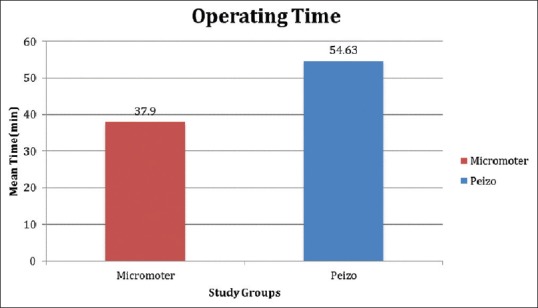
Time taken in both study groups
DISCUSSION
In 1975, Horton et al.[6] conducted an experimental study to rule out the effects on healing of the alveolar bone when the bone osteotomy was performed by three different methods, i.e., with the help of chisel, rotary bur, and ultrasonic instrument. The results of their study concluded that the best healing of the alveolar bone was obtained when the osteotomy was performed by chisel followed by ultrasonic instrument and finally by the rotary instrument.
Piezosurgery is a new innovative technique which works on the principle of oscillation and is very helpful in performing osteotomy of mineralized tissue as it provides clean, sharp cuts of the bone. It also helps in preserving the integrity of soft tissues as its surgical action ceases on contact with the nonmineralized tissues.[14,15,16]
Piezosurgery generates very small oscillations in the amplitude of 60–200 μm horizontally and 20–60 μm vertically which is comparatively very less when compared to oscillating micro saws; thus, it provides precise and safe osteotomy cuts.[16] It is very easy to handle the device when compared to rotary handpiece or an oscillating saw as there is no need for supplemental force to oppose the rotation or oscillation of the instrument.[17] In addition, piezosurgery has an added advantage over burs and micro saws in that its ultrasonic vibrations break down the irrigation liquid into very small particles (cavitation phenomenon, which is implosion of gas bullae into blood vessels during bone cutting which produces a hemostatic effect and so reduces blood loss) that are washed out from the operating field, which ultimately gives a clear, unhindered vision of the operating filed.[18]
There are also reports on the histologic studies using this instrument,[6,19] stating that the piezosurgical unit cuts the bone like a chisel rather than burnishing it like a rotary bur. The edges of the bone cut perpendicular to the surface were irregular with lacunar osteocytes immediately adjacent to the cut surface, and there was no evidence of disruption of adjacent vascular structures.
In our study, to find out the efficiency of piezosurgery over micromotor in third molar odontectomies, we evaluated three variables postoperatively, that is, pain, trismus, and swelling, and a fourth variable was the time taken to complete the entire surgical procedure.
The level of pain felt was evaluated based on VAS.[10] The VAS was higher when the odontectomies were performed using micromotor with a statistical significant difference from the piezosurgical group. Studies done by Troedhan et al.[20] concluded that there was 50% reduction in the pain when piezosurgery was used for surgical extraction for third molars. The studies done by Barone et al.[2] showed a higher VAS with conventional instruments but their results were not statistically significant, even the results of Sivolella et al.[21] were at par with their study with no significant reduction in pain in the piezosurgical group. Rullo et al.[22] reported that there was reduction in pain when odontectomy was performed with piezosurgical instrument only for “simple extraction” cases, whereas in “complex extraction” cases, the postoperative pain was significantly greater in the piezosurgical group. The cause for this results was attributed to the longer time taken for the extraction of complex cases with more release of mediators of pain such as prostaglandin E2, bradykinin, and other mediators.[23] Mantovani et al.[24] concluded that despite more time taken for the surgical procedure, the VAS was lower in the piezosurgical group even the findings of our study conclude the same results which can be attributed to the minimal damage to the soft tissue caused by piezosurgery.
Trismus was evaluated by the most universally accepted and frequently cited methods.[11,12] The result of trismus shows that there is statistically significant greater mouth opening in the piezosurgical group on postoperative days 1, 3, 5, and 7. Even the improvement of trismus in the piezosurgery group is at faster rate with no trismus on postoperative day 7 when compared to the conventional micromotor group as proved statistically. Studies by Barone et al.[2] showed significant improvement in mouth opening on postoperative days 1, 3, and 7; on postoperative day 5, the mouth opening in piezosurgical group was better than the micromotor group, but the statistical significant level in the difference was not reached. Significant higher values were recorded in the piezosurgical group on postoperative days 3, 5, and 7 in the comparative study done by Goyal et al.[25] Results of Sortino et al.[13] showed that 24 h postextraction values of piezosurgery group were statistically better than the rotary group. Even the results of Piersanti et al.[26] which evaluated trismus everyday postoperatively found statistically better trismus value on postoperative day 2. There was no statistical difference in the trismus values between the groups in the study done by Sivolella et al.[21] as measurements were done on postoperative days 7 and 30. In our study, we had a statistical significant difference between both groups on postoperative day 7. Our follow-up of the study was only until postoperative day 15, which showed the same trismus value in both groups, indicating complete recovery of the case after the surgery in both groups.
In our study, the technique used for measurement of swelling provided a volumetric measurement rather than a sum of linear measurements.[13] The results of swelling show that there is significant decreased swelling in the piezosurgical group on postoperative days 1, 3, 5, and 7 as compared to the micromotor group. Furthermore, in the piezosurgical group, there was not any statistical significant swelling present on postoperative day 7 which was present in micromotor group, indicating faster swelling reduction with the extraction performed by piezosurgical group. Barone et al.[2] mentioned that the measurement of swelling has highly observational bias as it involves three dimensional registration and intraoral swelling can also manifest as facial edema, and their study showed significantly higher value of swelling in the micromotor group. Goyal et al.[25] measured swelling as described by Schultze-Mosgau et al.[27] and concluded that significant lower values of swelling was present in piezosurgery group on postoperative day 3, 5, and 7 which was localized to the buccal region in most cases. A 40.06% lower measurements in swelling was observed in the piezosurgery group 24 h after the surgical extraction, which was considered statistically significant value in the study done by Sortino et al.[13] Troedhan et al.[20] concluded that there was 50% reduction in the swelling when piezosurgery was used for surgical extraction for third molars. There was no significant difference in the swelling on postoperative day 7 and 30 in a study done by Sivolella et al.[21] whereas our study showed statistical significant difference in swelling on postoperative day 7, even Mantovani et al.[24] showed statistical significant difference in swelling especially on postoperative day 7, so were the results of study done by Piersanti et al.[26]
According to the study done by Oikarinen,[28] there is a direct effect of duration of operation on postoperative pain, trismus, and swelling. However, Benediktsdόttir et al.[29] reported that postoperative outcomes were independent of the time taken for the surgical procedure. Our study shows that despite more time (mean time = 54.63 min) taken by piezosurgery unit as compared to the micromotor (mean time = 37.90 min), there was statistically significant reduction in the postoperative pain, trismus, and swelling; these findings are also supported by the study done by Goyal et al.,[25] Sivolella et al.,[21] and Mantovani et al.,[24] which can be attributed to the less injury to the soft tissue by piezosurgery as its surgical action ceases on contacting the nonmineralized tissue. The time taken to perform the procedure by piezosurgery in the study done by Barone et al.[2] was higher but not so high that a statistical difference was obtained. In the study performed by Sortino et al.,[13] there was 25.83% more time taken by the piezosurgical group which was statistically significant. Troedhan et al.[20] concluded that once the technique of using piezosurgical unit is mastered, it does not consume more time than the conventional surgical techniques. Rullo et al.[22] concluded that for “simple extraction,” there was no statistical difference in time taken for performing the surgery in both groups with significant less pain in the piezosurgical group; however, for “complex extraction,” there was a statistical difference in the time taken to perform the surgical procedure with more time needed by the piezosurgical group, and also there was significantly more pain in the piezosurgical group. Although our study considered the mean value to statistically analyze the time taken for all the procedures, no attempt was made to analyze the time taken according to the difficulty of extraction.
CONCLUSION
Piezosurgical unit is more efficient in controlling the postoperative pain with faster improvement in trismus and quicker reduction in swelling; however, it is more time-consuming and an expensive tool for the surgical removal of the third molar.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Akadiri OA, Obiechina AE. Assessment of difficulty in third molar surgery – a systematic review. J Oral Maxillofac Surg. 2009;67:771–4. doi: 10.1016/j.joms.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Barone A, Marconcini S, Giacomelli L, Rispoli L, Calvo JL, Covani U. A randomized clinical evaluation of ultrasound bone surgery versus traditional rotary instruments in lower third molar extraction. J Oral Maxillofac Surg. 2010;68:330–6. doi: 10.1016/j.joms.2009.03.053. [DOI] [PubMed] [Google Scholar]
- 3.Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Creminelli L, Santoro F. Assessing postoperative discomfort after third molar surgery: A prospective study. J Oral Maxillofac Surg. 2007;65:901–17. doi: 10.1016/j.joms.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 4.Praveen G, Rajesh P, Neelakandan RS, Nandagopal CM. Comparison of morbidity following the removal of mandibular third molar by lingual split, surgical bur and simplified split bone technique. Indian J Dent Res. 2007;18:15–8. doi: 10.4103/0970-9290.30916. [DOI] [PubMed] [Google Scholar]
- 5.Kerawala CJ, Martin IC, Allan W, Williams ED. The effects of operator technique and bur design on temperature during osseous preparation for osteosynthesis self-tapping screws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:145–50. doi: 10.1016/s1079-2104(99)70108-3. [DOI] [PubMed] [Google Scholar]
- 6.Horton JE, Tarpley TM, Jr, Wood LD. The healing of surgical defects in alveolar bone produced with ultrasonic instrumentation, chisel, and rotary bur. Oral Surg Oral Med Oral Pathol. 1975;39:536–46. doi: 10.1016/0030-4220(75)90192-9. [DOI] [PubMed] [Google Scholar]
- 7.Vercellotti T. Essentials in Piezosurgery: Clinical Advantages in Dentistry. 1st ed. San Francisco: Quintessence Publishing Co; 2009. [Google Scholar]
- 8.Pederson GW. Oral Surgery. Philadelphia: WB Saunders; 1988. [Google Scholar]
- 9.Baqain ZH, Al-Shafii A, Hamdan AA, Sawair FA. Flap design and mandibular third molar surgery: A split mouth randomized clinical study. Int J Oral Maxillofac Surg. 2012;41:1020–4. doi: 10.1016/j.ijom.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17:45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 11.Laureano Filho JR, de Oliveira e Silva ED, Batista CI, Gouveia FM. The influence of cryotherapy on reduction of swelling, pain and trismus after third-molar extraction: A preliminary study. J Am Dent Assoc. 2005;136:774–8. doi: 10.14219/jada.archive.2005.0261. [DOI] [PubMed] [Google Scholar]
- 12.Neupert EA 3rd, Lee JW, Philput CB, Gordon JR. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992;50:1177–82. doi: 10.1016/0278-2391(92)90149-t. [DOI] [PubMed] [Google Scholar]
- 13.Sortino F, Pedullà E, Masoli V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: Comparison of postoperative recovery. J Oral Maxillofac Surg. 2008;66:2444–8. doi: 10.1016/j.joms.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Stübinger S, Kuttenberger J, Filippi A, Sader R, Zeilhofer HF. Intraoral piezosurgery: Preliminary results of a new technique. J Oral Maxillofac Surg. 2005;63:1283–7. doi: 10.1016/j.joms.2005.05.304. [DOI] [PubMed] [Google Scholar]
- 15.Robiony M, Polini F, Costa F, Vercellotti T, Politi M. Piezoelectric bone cutting in multipiece maxillary osteotomies. J Oral Maxillofac Surg. 2004;62:759–61. doi: 10.1016/j.joms.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Schlee M, Steigmann M, Bratu E, Garg AK. Piezosurgery: Basics and possibilities. Implant Dent. 2006;15:334–40. doi: 10.1097/01.id.0000247859.86693.ef. [DOI] [PubMed] [Google Scholar]
- 17.Vercellotti T, Nevins ML, Kim DM, Nevins M, Wada K, Schenk RK, et al. Osseous response following resective therapy with piezosurgery. Int J Periodontics Restorative Dent. 2005;25:543–9. [PubMed] [Google Scholar]
- 18.Eggers G, Klein J, Blank J, Hassfeld S. Piezosurgery: An ultrasound device for cutting bone and its use and limitations in maxillofacial surgery. Br J Oral Maxillofac Surg. 2004;42:451–3. doi: 10.1016/j.bjoms.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 19.McFall TA, Yamane GM, Burnett GW. Comparison of the cutting effect on bone of an ultrasonic cutting device and rotary burs. J Oral Surg Anesth Hosp Dent Serv. 1961;19:200–9. [PubMed] [Google Scholar]
- 20.Troedhan A, Kurrek A, Wainwright M. Ultrasonic piezotome surgery: Is it a benefit for our patients and does it extend surgery time? A retrospective comparative study on the removal of 100 impacted mandibular 3rd molars. Open J Stomatol. 2011;1:179–84. [Google Scholar]
- 21.Sivolella S, Berengo M, Bressan E, Di Fiore A, Stellini E. Osteotomy for lower third molar germectomy: Randomized prospective crossover clinical study comparing piezosurgery and conventional rotatory osteotomy. J Oral Maxillofac Surg. 2011;69:e15–23. doi: 10.1016/j.joms.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 22.Rullo R, Addabbo F, Papaccio G, D’Aquino R, Festa VM. Piezoelectric device vs. conventional rotative instruments in impacted third molar surgery: Relationships between surgical difficulty and postoperative pain with histological evaluations. J Craniomaxillofac Surg. 2013;41:e33–8. doi: 10.1016/j.jcms.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 23.Smith WL, Marnett LJ. Prostaglandin endoperoxide synthase: Structure and catalysis. Biochim Biophys Acta. 1991;1083:1–17. doi: 10.1016/0005-2760(91)90119-3. [DOI] [PubMed] [Google Scholar]
- 24.Mantovani E, Arduino PG, Schierano G, Ferrero L, Gallesio G, Mozzati M, et al. A split-mouth randomized clinical trial to evaluate the performance of piezosurgery compared with traditional technique in lower wisdom tooth removal. J Oral Maxillofac Surg. 2014;72:1890–7. doi: 10.1016/j.joms.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Goyal M, Marya K, Jhamb A, Chawla S, Sonoo PR, Singh V, et al. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a Piezotome or a conventional handpiece: A prospective study. Br J Oral Maxillofac Surg. 2012;50:556–61. doi: 10.1016/j.bjoms.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 26.Piersanti L, Dilorenzo M, Monaco G, Marchetti C. Piezosurgery or conventional rotatory instruments for inferior third molar extractions? J Oral Maxillofac Surg. 2014;72:1647–52. doi: 10.1016/j.joms.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 27.Schultze-Mosgau S, Schmelzeisen R, Frölich JC, Schmele H. Use of ibuprofen and methylprednisolone for the prevention of pain and swelling after removal of impacted third molars. J Oral Maxillofac Surg. 1995;53:2–7. doi: 10.1016/0278-2391(95)90486-7. [DOI] [PubMed] [Google Scholar]
- 28.Oikarinen K. Postoperative pain after mandibular third-molar surgery. Acta Odontol Scand. 1991;49:7–13. doi: 10.3109/00016359109041135. [DOI] [PubMed] [Google Scholar]
- 29.Benediktsdóttir IS, Wenzel A, Petersen JK, Hintze H. Mandibular third molar removal: Risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:438–46. doi: 10.1016/j.tripleo.2003.10.018. [DOI] [PubMed] [Google Scholar]


