Abstract
Simple bone cysts (SBCs) are benign lesions often found in the long bones of children between their first and second decades. They occasionally occur in the mandible but rarely in the mandibular condyle. A case of a 7-year-old female child with an increasing enlargement of the left mandibular condyle is presented. A 2 cm × 3 cm lytic lesion was explored and curetted through an intraoral vestibular incision and proved to be an SBC. Postoperative recovery was uncomplicated with remodeling of the condylar observed at 3 years follow-up.
Keywords: Condyle, cyst, mandibular
INTRODUCTION
Simple bone cysts (SBCs) are benign lesions that develop in children in their first two decades. While usually within the medulla of long bones, 10% occur in the jaws with 75% of those being in the body of the mandible.[1] In over half of the cases, SBCs of the mandibular condyle present with temporomandibular joint symptoms with or without preauricular swelling.[2]
This report describing an SBC involving the mandibular condyle in a young patient presented with swelling aims to highlight the differential diagnoses and management of these lesions.
CASE REPORT
A 7-year-old Polynesian female child presented with a left preauricular swelling that had increased in size over 3 months. On examination, there was a 2 cm × 2 cm hard, raised, nontender mass that moved with the mandible. There were neither occlusal changes nor other relevant clinical findings.
Imaging revealed expansion of the condylar head due to a 2 cm × 3 cm well-demarcated radiolucent lesion extending inferiorly into the ramus [Figure 1]. Surgical exploration was performed under general anesthesia for biopsy and if suitable to proceed to definitive management. Access was through an intraoral approach using an external oblique incision with subperiosteal dissection. On approaching the condyle, a blue discoloration of the cortex was observed and a bony window was made to reveal an empty cavity. The internal walls were curetted to initiate bleeding and the wound closed with resorbable sutures. Uncomplicated mucosal healing was noted at 10 days follow-up.
Figure 1.

Sagittal computed tomography view of left mandibular condylar lesion
Histology confirmed the presence of an SBC with normal bone, hemosiderin deposits, reactive fibroblasts, and small amounts of osteoid formation but no cystic lining. Follow-up imaging over 3 years showed osseous regeneration of the condyle that had restored relatively normal condylar morphology [Figure 2].
Figure 2.

Orthopantomogram demonstrating remodeling of condyle postcurettage
DISCUSSION
The SBC is a common radiolucency in the mandible and is often noted in the body and symphysis that sometimes envelop the apices of teeth. As the aetiology of SBCs is unknown, these lesions have variously been named “traumatic bone cyst”, “solitary bone cyst”, “haemorrhagic bone cyst” and “unilateral bone cyst”. It has been speculated that SBCs arise as a result of occlusal trauma, causing intramedullary bleeding and aberrant healing with cavity formation.[1] Others believe that SBCs may arise as a developmental defect.
Rushton established criteria for the diagnosis of SBCs, with the following five features: they are single, with no epithelial lining, in the absence of infection, containing mainly fluid with bony walls.[3] Recently, the histopathological features have been described as containing a thin lining of fibrous tissue that may contain spindle cells, hemosiderin pigment, and a small number of chronic inflammatory cells.[4]
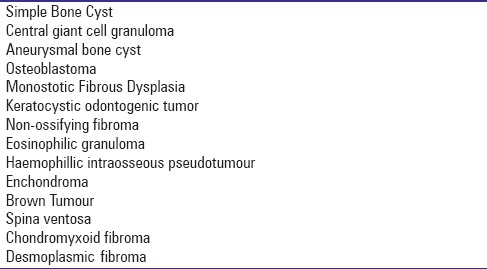
SBCs of the appendicular skeleton are treated with percutaneous drainage and steroid injection with surgery reserved for refractory cases or to prevent fractures.[5] In the maxillofacial skeleton, a radiolucent lesion has many differentials [Table 1], and surgical exploration is mandatory for tissue diagnosis.[6] Exploration and curettage are usually definitive for the management of the maxillofacial SBC.[5,7]
Table 1.
Differential for solitary SBS-like radiolucencies detected on radiographic examination7
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Harnet JC, Lombardi T, Klewansky P, Rieger J, Tempe MH, Clavert JM. Solitary bone cyst of the jaws: A review of the etiopathogenic hypotheses. J Oral Maxillofac Surg. 2008;66:2345–8. doi: 10.1016/j.joms.2007.08.035. [DOI] [PubMed] [Google Scholar]
- 2.Hatakeyama D, Tamaoki N, Iida K, Yonemoto K, Kato K, Makita H, et al. Simple bone cyst of the mandibular condyle in a child: Report of a case. J Oral Maxillofac Surg. 2012;70:2118–23. doi: 10.1016/j.joms.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 3.Rushton MA. Solitary bone cysts in the mandible. Br Dent J. 1946;81:37–49. [PubMed] [Google Scholar]
- 4.Allen D. Unicameral Bone Cyst. 2013. [Last accessed on 2015 15 Aug]. http://www.orthobullets.com/pathology/8035/unicameral-bone-cyst .
- 5.Wright JG, Yandow S, Donaldson S, Marley L Simple Bone Cyst Trial Group. A randomized clinical trial comparing intralesional bone marrow and steroid injections for simple bone cysts. J Bone Joint Surg Am. 2008;90:722–30. doi: 10.2106/JBJS.G.00620. [DOI] [PubMed] [Google Scholar]
- 6.Burgener FA, Kormano M, Puda T. Differential Diagnosis in Conventional Radiology, 3rd Edition. Investigative Radiology. Thieme. 2008 [Google Scholar]
- 7.Kim KA, Koh KJ. Recurrent simple bone cyst of the mandibular condyle: A case report. Imaging Sci Dent. 2013;43:49–53. doi: 10.5624/isd.2013.43.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]


