Abstract
This study investigated the interaction effects of meteorological factors and air pollutants on the onset of acute coronary syndrome (ACS). Data of ACS patients were obtained from the Taiwan ACS Full Spectrum Registry and comprised 3164 patients with a definite onset date during the period October 2008 and January 2010 at 39 hospitals. Meteorological conditions and air pollutant concentrations at the 39 locations during the 488-day period were obtained. Time-lag Poisson and logistic regression were used to explore their association with ACS incidence. One-day lag atmospheric pressure (AP), humidity, particulate matter (PM2.5, and PM10), and carbon monoxide (CO) all had significant interaction effects with temperature on ACS occurrence. Days on which high temperatures (>26 °C) and low AP (<1009 hPa) occurred the previous day were associated with a greater likelihood of increased incidence of developing ACS. Typhoon Morakot was an example of high temperature with extremely low AP associated with higher ACS incidence than the daily average. Combinations of high concentrations of PM or CO with low temperatures (<21 °C) and high humidity levels with low temperatures were also associated with increased incidence of ACS. Atmospheric pollution and weather factors have synergistic effects on the incidence of ACS.
Acute coronary syndrome (ACS) is a leading cause of morbidity and mortality worldwide1,2. In Taiwan, the age-adjusted incidence of ACS (/100,000 person-years) increased from 28.0 in 1999 to 44.4 in 2008 (p < 0.001), and the disease has been the second most common cause of mortality since 20103,4. ACS is also a common cause of emergency hospitalization and therefore imposes a major burden on healthcare resources in that country. In Taiwan, healthcare expenditure constitutes about 6% of the gross domestic product and is expected to escalate sharply over the next two decades because of the aging population and the rise in incidence of ACS5. A number of risk factors for ACS have been identified, including traditional factors such as hyperlipidemia and diabetes as well as environmental factors such as weather parameters and air pollution6. Previous studies have indicated that weather conditions play a role in the onset of cardiovascular disease7,8. Although it is clear that weather parameters do not act alone in determining health but rather act in concert with other such parameters, e.g., ambient air pollutants and aerosols of biological origin9, few studies have investigated the synergistic effects of ambient air pollution and individual meteorological parameters on health outcomes.
Because of geographic and climate variations, the subject of interest varies and there is a lack of consensus about which combinations of environmental conditions are likely to contribute to the onset of ACS10,11,12. For example, typhoons are of particular interest in Taiwan because they occur annually, often with deleterious effects, during the months of July through September. Their impact on health such as on the incidence of ACS is of particular concern to healthcare authorities in that country. However, most studies on the impact of extreme weather on cardiovascular events have been conducted in the United States and have focused mainly on Hurricane Katrina and Hurricane Sandy13,14. Therefore, large-scale studies on the relationship between typhoons and other extreme weather events on incidence of cardiovascular events such as ACS in Asia are needed.
It is important to understand whether certain environmental factors play a role in the development of ACS. In this study we explored the relationship between meteorological parameters and ACS incidence using data on patients registered in the Taiwan ACS Full Spectrum Registry, a database established to identify predictors of outcomes of patients with ACS one year after hospital discharge at 39 medical centers and regional hospitals across Taiwan15. The study period investigated in this study was October 2008 to January 2010, and included the days during which typhoon Morakot (7–9 August 2009) affected Taiwan. This typhoon was the most severe in half a century and caused catastrophic damage island wide. We chose to focus on Morakot because it serves as an extreme meteorological example with which to study the relationship between ACS and environmental factors.
Materials and Methods
Study population and definitions
Data in this study were obtained from the Taiwan ACS Full Spectrum Registry study, a prospective, national, multicenter, non-interventional observational study on outcome of patients with ACS treated at 39 major medical centers or regional hospitals in Taiwan from 1 October 2008 to 31 January 2010 (488 days)15. ACS was defined in that study as symptoms ranging from ST-elevation myocardial infarction (STEMI) to unstable angina to non-STEMI. Briefly, STEMI was defined in patients who presented with acute chest pain or overwhelming shortness of breath together with persistent electrocardiographic ST elevation of >1 mm in two or more contiguous leads, or with a new or presumed new left-bundle branch block pattern on electrocardiography. Unstable angina was defined in patients who presented with acute chest pain or overwhelming shortness of breath with neither ST elevation nor abnormal levels of cardiac enzymes. Non-STEMI was defined in patients who presented with acute chest pain or overwhelming shortness of breath with no ST elevation but with a classic rise and fall in level of at least one cardiac enzyme (troponin or MB fraction of creatine kinase). To ensure that the sample satisfactorily represented the ACS population in Taiwan and that the diagnosis and management of ACS were the same at all 39 sites (including 19 tertiary medical centers and 20 regional hospitals), sites were selected by members of the Scientific Committee of the Taiwan Society of Cardiology. The accuracy of documentation was examined in 5% of case report forms at each recruiting site16. Blood pressure (BP) was measured in all patients with an oscillometric semiautomatic sphygmomanometer as recommended by the American Heart Association Council on High Blood Pressure Research17. Patient BP was measured in both arms during the initial visit and then in the arm with higher BP during subsequent visits. The recorded value was an average of two measurements. Hypertension was defined according to the 2015 guidelines of the Taiwan Society of Cardiology and Taiwan Hypertension Society for the Management of Hypertension18. Data on patient baseline characteristics, risk factors, clinical presentation, clinical diagnosis, in-hospital interventions, and medications prescribed were collected from admission to discharge. This study was carried out in accordance with the Declaration of Helsinki and good clinical practice. Ethics committee approval was obtained at all trial sites (list of hospitals in Appendix). Written informed consent was obtained from each patient.
Inclusion criteria
Patients were aged 20 years or older and were admitted within 24 hours to the hospital from the emergency department with ACS symptoms. All patients provided informed consent and 3183 were eligible for inclusion and enrolled in the study. Of those patients, 3164 had a definite onset date.
Exclusion criteria
Patients were excluded from the study if ACS was precipitated by comorbidity such as trauma, if they were previously enrolled in this trial, or if they were participating in an investigational drug study.
Environmental data
Hourly measurements of temperature, relative humidity and air pollution (CO, NO2, PM10, PM2.5, SO2, and O3) were obtained from the database maintained by the Environmental Protection Administration (EPA), which has 77 monitoring stations covering most of the populated townships. Hourly measurements of atmospheric pressure (AP) were obtained from the database of the Central Weather Bureau (CWB), which has more than 700 monitoring stations throughout Taiwan. For each hospital, the three nearest monitoring stations were identified, and corresponding data of an environmental factor for that hospital were calculated as a weighted average from the three stations using reciprocals of distance to the hospital as weights. Daily data of any aforementioned environmental factor were collected and represented the average of the hourly measurements at each monitoring station. We also calculated the within-day standard deviation to represent the effect of short-term change.
Statistical analysis
The ACS Full Spectrum data include daily numbers of ACS patients enrolled at each of the 39 medical centers during the 488-day period. For each AP-temperature stratum, the number of days and patients were summarized and means and standard deviations of corresponding measurements and proportions of comorbidities were calculated. One-way ANOVA was used to compare the demographic measurements across strata, and the chi-square test was used to compare the comorbidity proportion across strata. The relationship between number of ACS patients and measurements of meteorological factors and ambient air pollution one, two, and three days prior (lag-1, lag-2, and lag-3) to admission were explored by logistic regression. We considered 39*488 (hospital-day) observations as the binary dependent variable with value = 1 if there was at least one ACS patient for the specific hospital-day, and 0 otherwise. Logistic regression was used to fit the above binary dependent variable with various combinations of lag variables and different cutoffs for AP and temperature. Correlations of clustered data for each hospital were adjusted using a generalized estimating equation (GEE). Using the quasi-likelihood under the independence model criterion19 for GEE, we selected the optimal lag day and cutoffs for AP and temperature. A two-tailed p < 0.05 was regarded as statistically significant. All analyses were performed with the statistical package SAS for Windows (Version 9.3, SAS Institute Inc., Cary, North Carolina, USA).
Results
Relationship between weather parameters and air quality
Correlations between meteorological and air pollutant measurements taken one day before ACS onset in each patient are listed in Table 1. There was a significant negative correlation between AP and temperature and positive correlations between CO and NO2 and between PM10 and PM2.5. The aforementioned pollutants had a consistent negative correlation with temperature.
Table 1. Pearson coefficients of correlation between meteorological and air pollutant daily measurements during the 488-day study period.
| AP* | T | RH | CO | NO2 | PM2.5 | PM10 | SO2 | O3 | |
|---|---|---|---|---|---|---|---|---|---|
| AP | 1 | ||||||||
| T | −0.78* | 1 | |||||||
| RH | −0.24 | 0.12 | 1 | ||||||
| CO | 0.37 | −0.34 | 0.06 | 1 | |||||
| NO2 | 0.41 | −0.41 | −0.07 | 0.89* | 1 | ||||
| PM2.5 | 0.22 | −0.17 | −0.2 | 0.38 | 0.5 | 1 | |||
| PM10 | 0.25 | −0.2 | −0.26 | 0.28 | 0.41 | 0.88* | 1 | ||
| SO2 | 0.14 | 0.04 | −0.14 | 0.34 | 0.46 | 0.66 | 0.61 | 1 | |
| O3 | −0.06 | 0.16 | −0.35 | −0.14 | −0.06 | 0.4 | 0.37 | 0.15 | 1 |
AP: air pressure, T: temperature, RH: relative humidity.
Daily meteorological and air quality conditions and the distribution of ACS patients
Table 2 lists the number of patients with ACS in each AP-temperature category and their average age, BMI, their sex, and comorbidities (diabetes, hypertension, and dyslipidemia). There were no significant differences in these demographic and clinical characters across the six AP-temperature strata. Other clinical measurements including heart rate, BP, smoking status, family ACS history, and previous coronary artery disease are listed in Supplementary Table 1. Of those variables, only family ACS history and heart rate differed significantly across the six AP-temperature categories.
Table 2. Distribution of ACS patients for 488-day study period *39 study hospitals, stratified by air pressure (AP) and temperature (T).
| high T (>26 °C) | mild T (21–26 °C) | low T (<21 °C) | p value! | ||||
|---|---|---|---|---|---|---|---|
| low AP (<1009 hpa) | high AP (≥1009 hpa) | low AP | high AP | low AP | high AP | ||
| Number of hospital days | 6288 | 748 | 2274 | 3021 | 164 | 6537 | ‒ |
| Total case no. | 1306 | 54 | 380 | 489 | 16 | 919 | |
| Case per hospital day | 0.21 | 0.07 | 0.17 | 0.16 | 0.1 | 0.14 | <0.001 |
| Gender (male %) | 1018/1306 (78.0%) | 42/54 (77.8%) | 300/380 (79.0%) | 364/489 (74.4%) | 15/16 (93.8%) | 727/919 (79.1%) | 0.238 |
| Age | 62.55 ± 13.44 | 64.31 ± 14.19 | 63.43 ± 14.1 | 63.22 ± 13.67 | 65.19 ± 15.63 | 63.29 ± 13.36 | 0.652 |
| BMI | 25.45 ± 3.84 | 24.7 ± 3.49 | 25.3 ± 4.08 | 25.4 ± 3.92 | 26.09 ± 6.09 | 25.44 ± 3.92 | 0.776 |
| Diabetes no. | 459 (35.4%) | 16 (29.6%) | 117 (30.8%) | 195 (40.1%) | 7 (43.75%) | 334 (36.7%) | 0.08 |
| Dyslipidemia no. | 512 (39.7%) | 17 (31.5%) | 155 (40.8%) | 190 (39.1%) | 7 (43.75%) | 344 (37.8%) | 0.739 |
| Hypertension no. | 796 (61.7%) | 36 (67.9%) | 254 (66.8%) | 312 (64.3%) | 12 (75%) | 591 (65.1%) | 0.3 |
*: ±one standard deviation.
!: Across-strata comparison: one-way ANOVA for age and BMI, and chi-square test for gender and comorbidity proportions.
Table 3 lists the metrological and air quality information for the 488 days in the study period. Temperatures were trichotomized into low, mild and high and AP was dichotomized into low and high based on the optimal cut points determined via quasi-likelihood under the independence model criterion (QIC) as shown in Supplementary Table 2. Days with low AP and low temperatures had the highest concentrations of CO, NO2, PM10 and PM2.5 but the lowest O3 concentration. The distribution of SO2 was relatively uniform. The within-day standard deviations (denoted as stdwd) of meteorological and air pollutant factors are listed in the row below the daily mean in Table 3. Most of the stdwd values are relatively small compared with the corresponding daily means. For example, the daily temperature ranged from 17 °C to 29 °C during the study period and the stdwd was roughly ±2 °C, suggesting that within-day temperature variation was modest.
Table 3. Mean and within-day standard deviation (stdwd) of meteorological and air pollutant factors, averaged over specific hospital-days stratified by temperature (T) and air pressure (AP).
| high T (>26 °C) | mild T (21–26 °C) | low T (<21 °C) | p value! | |||||
|---|---|---|---|---|---|---|---|---|
| low AP (<1009 hpa) | high AP (≥1009 hpa) | low AP | high AP | low AP | high AP | |||
| Number of hospital-days | 6288 | 748 | 2274 | 3021 | 164 | 6537 | ‒ | |
| RH | Mean | 73.54 ± 6.47 | 75.61 ± 4.55 | 73.47 ± 10.18 | 72.97 ± 8.21 | 79.05 ± 6.38 | 72.2 ± 9.89 | <0.001 |
| stdwd | 8.71 | 8.78 | 8.8 | 8.94 | 7.23 | 8.21 | ||
| CO | Mean | 0.48 ± 0.24 | 0.6 ± 0.25 | 0.58 ± 0.27 | 0.62 ± 0.26 | 0.57 ± 0.26 | 0.65 ± 0.46 | <0.001 |
| stdwd | 0.25 | 0.29 | 0.27 | 0.3 | 0.22 | 0.3 | ||
| NO2 | Mean | 15.92 ± 7.2 | 19.08 ± 7.62 | 20.51 ± 8.27 | 22.19 ± 8.48 | 20.18 ± 8.58 | 22.12 ± 8.2 | <0.001 |
| stdwd | 7.06 | 8.07 | 8.79 | 9.25 | 8.68 | 9.08 | ||
| PM10 | Mean | 50.06 ± 22.44 | 71.48 ± 31.3 | 64.24 ± 30.96 | 72.51 ± 41.43 | 56.19 ± 33.36 | 66.69 ± 34.72 | <0.001 |
| stdwd | 14.81 | 21.48 | 22.74 | 22.41 | 20.24 | 22.17 | ||
| PM2.5 | Mean | 29.57 ± 13.9 | 41.18 ± 19.25 | 37.08 ± 17.14 | 40.28 ± 21.51 | 35.1 ± 22.29 | 37.19 ± 18.62 | <0.001 |
| stdwd | 9.51 | 12.64 | 12.55 | 12.55 | 12.96 | 12.15 | ||
| SO2 | Mean | 4.25 ± 2.07 | 5.16 ± 2.32 | 3.92 ± 1.91 | 4.58 ± 2.6 | 3.03 ± 1.48 | 4.12 ± 2.13 | <0.001 |
| stdwd | 2.57 | 2.99 | 2.06 | 2.44 | 1.56 | 1.96 | ||
| O3 | Mean | 27.88 ± 12.71 | 33.54 ± 11.16 | 33.6 ± 13.08 | 32.02 ± 10.67 | 27.48 ± 8.53 | 25.92 ± 9.09 | <0.001 |
| stdwd | 16.95 | 21.56 | 17.12 | 17.98 | 13.07 | 13.16 | ||
| T | Mean | 28.87 ± 1.46 | 27.24 ± 0.8 | 24.34 ± 1.26 | 23.04 ± 1.45 | 19.53 ± 1.13 | 17.59 ± 2.45 | <0.001 |
| stdwd | 1.97 | 2 | 2.09 | 2.14 | 1.69 | 2.01 | ||
The stdwd was estimated by the hourly measurement of each day.
!: Across-strata comparison: one-way ANOVA for age and BMI, and chi-square test for gender and comorbidity proportions.
As seen in Table 1, PM10 and PM2.5 could not be used simultaneously in the same model because of the strong collinearity between the two. The same is true for CO and NO2. After extensive trials of the combinations including interactions by examining QIC (Quasi-likelihood-based Information Criterion)19 and AUC (area under curve of ROC), we retained the lag-1 effect for all the factors. For air pollutants, combinations of (PM10 + CO) in Model (1) and (PM 2.5 + NO2) in Model (2) were selected. Among the various cut-point combinations for AP-temperature that we tried, we found that [AP = 1009 hPa and temperature = 21 °C and 26 °C] and its proximities [AP = 1009 ± 1 hPa and temperature = 21 ± 1 °C and 26 ± 1 °C] had the lowest QIC and highest AUC, respectively. Table 4 lists the results from Model (1) and (2) by using cut-points [AP = 1009 hPa, temperature = 21 °C and 26 °C], and the models can be described as:
Table 4. Interactions of temperature with air pressure (AP), relative humidity (RH) and air pollutants for ACS: odds ratio (OR) of AP, RH, PM10 and CO (from Model (1)), and PM2.5 and NO2 (from Model (2)) in different temperature strata, after adjusting the offsets by hospital.
| high T (>26 °C) | mild T (21–26 °C) | low T (<21 °C) | ||||
|---|---|---|---|---|---|---|
| OR* (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Model (1) | ||||||
| Low AP: High AP | 2.236 (1.572, 3.181) | <0.0001 | 1.124 (0.899, 1.405) | 0.305 | 0.811 (0.434, 1.517) | 0.513 |
| RH per 1%↑ | 0.995 (0.982, 1.009) | 0.501 | 0.997 (0.987, 1.005) | 0.38 | 1.018 (1.009, 1.027) | <0.0001 |
| PM10 per 10 μg/m3↑ | 0.983 (0.948, 1.019) | 0.352 | 1.006 (0.983, 1.029) | 0.601 | 1.037 (1.006, 1.067) | 0.018 |
| CO per 1 ppm↑ | 0.822 (0.568, 1.191) | 0.301 | 0.952 (0.648, 1.398) | 0.8 | 1.122 (1.010, 1.246) | 0.032 |
| Model (2) | ||||||
| Low AP: High AP | 2.193 (1.54, 3.124) | <0.0001 | 1.116 (0.894, 1.392) | 0.334 | 0.793 (0.423, 1.488) | 0.471 |
| RH per 1%↑ | 0.993 (0.979, 1.008) | 0.356 | 0.997 (0.986, 1.005) | 0.318 | 1.018 (1.009, 1.026) | <0.0001 |
| PM2.5 per 10 μg/m3↑ | 0.961 (0.91, 1.015) | 0.152 | 0.980 (0.928, 1.035) | 0.459 | 1.069 (1.006, 1.137) | 0.032 |
| NO2 per 10 ppb↑ | 0.90 (0.801, 1.003) | 0.06 | 0.989 (0.861, 1.136) | 0.874 | 0.984 (0.866, 1.118) | 0.805 |
Model (1): Logit(Y) = α + β1 · APlow + β2 · Thigh + β3 · Tlow + β4 · APlow · Thigh + β5 · APlow · Tlow + β6 · RH + β7RH · Thigh + β8 · RH · Tlow + β9 · PM10 + β10 · PM10 · Thigh + β11 · PM10 · Tlw + β12 · CO + β13 · CO · Thigh + β14 · CO · Tlow + β15 · TAP6 + β16 · hospital1 + … + β53 · hospital38,
Model (2): Logit(Y) = α + β1 · APlow + β2 · Thigh + β3 · Tlow + β4 · APlow · Thigh + β5 · APlow · Tlow + β6 · RH + β7RH · Thigh + β8 · RH · Tlow + β9 · PM2.5 + β10 · PM2.5 · Thigh + β11 · PM2.5 · Tlw + β12 · NO2 + β13 · NO2 · Thigh + β14 · NO2 · Tlow + β15 · TAP6 + β16 · hospital1 + … + β53 · hospital38.
Here, binary Y is the indicator for ACS incidence in a hospital-day. APlow = 1 for AP < 1009 hPa and = 0 otherwise. Thigh = 1 for temperature >26 °C and = 0 otherwise, Tlow = 1 for temperature <21 °C and = 0 otherwise. RH is relative humidity, hospitali is an indicator variable for the ith hospital, and the capacity difference between the 39 hospitals was considered by the offset for each hospital (β13–β50) and total ACS patients from the previous six days (TAP6). We did not include SO2 and O3 and their stdwd values in the model because of their insignificant contribution to the model fit. For other pollutants, we fit Model (2) by retaining all variables in Model (1), except that we replaced PM10 and CO with PM2 .5 and NO2.
The upper part of Table 4 lists the adjusted interaction effects of temperature with AP, RH, PM10, and CO from Model (1), using a level of significance of 0.05. Under high temperature (>26 °C), low AP was associated with a significantly greater likelihood (OR, 2.236) of ACS onset than high AP. For other temperatures, AP variation had no significant effect. Under low temperature (<21 °C), we found that a 1% increase in RH was associated with an increased likelihood of ACS onset (OR = 1.018). For other temperatures, RH had no significant effect. Also under low temperature, we found that an increase in PM10 by 10 μg/m3 was associated with a slightly higher risk of ACS onset (OR = 1.037). Under other temperatures, PM10 variation had no significant effect. Also under low temperature, an increase in CO by 1 ppm was associated with significantly higher risk of ACS onset (OR = 1.122). The lower part of Table 4 lists the results for Model (2). Basically, the ORs and corresponding p values for AP and RH remained the same. Similar to PM10, an increase in PM2.5 concentration under low temperature was associated with a slightly higher risk of ACS (OR = 1.069). There was no significant effect under other temperatures. NO2 had no significant effect across all temperatures. In summary, both Model (1) and (2) suggest that on days with high temperature (>26 °C), low air pressure is a significant risk factor for ACS whereas on days with low temperature (<21 °C), high humidity and high air pollution are likely risk factors for ACS. On days with mild temperatures, however, none of the above environmental factors are significant. The receiver operating characteristic (ROC) curve for Model (1) is shown in Fig. 1. The area under the curve (AUC) for the model was roughly 0.76, indicating fair goodness of fit. The result for Model (2) was similar (data not shown).
Figure 1. Receiver operating characteristic (ROC) curve from logistic Model (1).
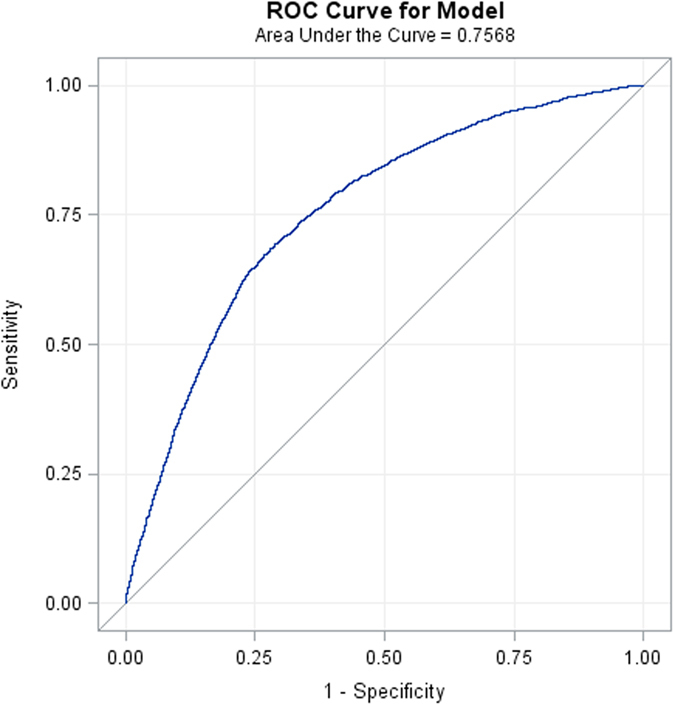
Area under the curve = 0.757, indicating fair model fit.
To assess the reliability of our results, we also conducted a series analysis under the cut-point with AP = 1009 ± 1 hPa and temperature = 21 ± 1 °C and 26 ± 1 °C. The associations between ACS onset and AP-temperature remained consistent after using these cut-points.
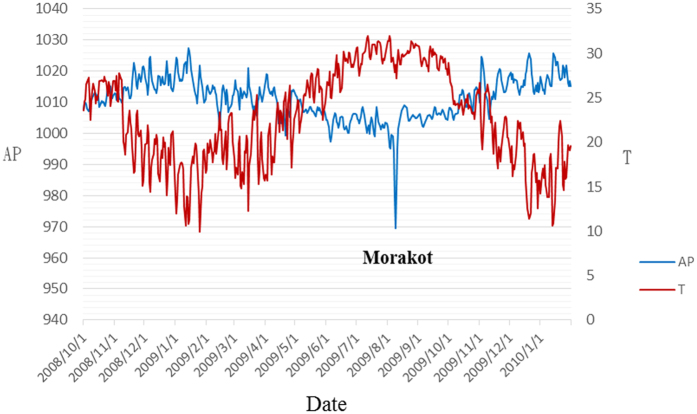
Daily ACS incidence and corresponding air pressure and temperature during the period of Typhoon Morakot
The data for the period covering Typhoon Morakot are shown in Table 5. During the week of Typhoon Morakot, the daily incidence of ACS was higher than the study average. The time courses of AP and temperature change during the study period shown in Fig. 2 demonstrate a sudden reduction in AP during the typhoon period. The incidence of ACS was also high in the cold season with high humidity (Oct. to Dec.). Both results coincide with the summarized conclusion from Model (1) and (2).
Table 5. Daily ACS incidences and corresponding air pressure and temperature before and after landfall of Typhoon Morakot (7–13 August 2009).
| Date | Mar | April | May | June | July | 8/7 | 8/8 | 8/9 | 8/10 | 8/11 | 8/12 | 8/13 | Sep | Oct | Nov | Dec | Jan |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACS | 5.1 | 6.6 | 8 | 9 | 8.29 | 10 | 9 | 7 | 10 | 9 | 7 | 12 | 8.57 | 9.48 | 10.17 | 10.9 | 8.7 |
| AP* | 1011 | 1008.9 | 1007.2 | 1002.2 | 1002.7 | 992.9 | 977.3 | 971.5 | 983.8 | 995.6 | 1001.9 | 1004.1 | 1003.7 | 1007.4 | 1012.5 | 1015 | 1016.1 |
| T | 20.1 | 22.3 | 26 | 28.2 | 29.8 | 28.32 | 27.83 | 27.68 | 27.22 | 28.23 | 29.71 | 28.8 | 29.5 | 25.5 | 22.5 | 18.1 | 17.3 |
*The overall average of 488 days is 6.48 case/day (95% CI: [6.09, 6.87]), with mean AP 1009.5 (95% CI: [1008.9, 1010.1]) and temperature 23.39 (95% CI: 22.95, 23.82]). For the “hot” week around the impact of Morakot (7–13 August), there were 9.14 incidences per day.
Figure 2. Trends in air pressure (AP) and temperature (T) during the study period.
Daily ACS incidence and corresponding residence areas during the period of Typhoon Morakot
The most severe damage caused by Typhoon Morakot occurred in southern Taiwan. We hypothesized that people living in southern Taiwan had significantly higher levels of psychological stress after the typhoon than people living in other parts of the island. However, as shown in Table 6, there was no significant difference in incidence of ACS among the 4 geographical residence areas.
Table 6. Daily ACS incidence and corresponding geographic residence areas during the period of Typhoon Morakot.
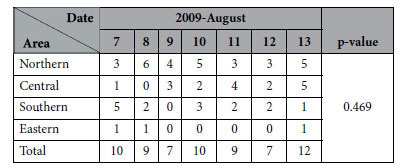
We used the chi-square test for independence to determine the correlation between ACS incidence and region.
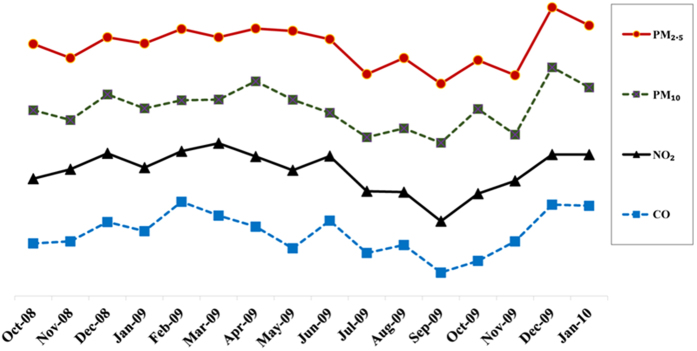
Time course of air quality during the study period in Taiwan (1 October 2008 to 31 January 2010)
As shown in Fig. 3, there was a downward trend in air pollution parameters after Typhoon Morakot (August 2009 to September 2009).
Figure 3. Time course of air quality during the study period in Taiwan (1 October 2008 to 31 January 2010) (standardized each pollutant).
Discussion
In this study we found that atmospheric pollution and weather factors have synergistic effects on the incidence of ACS in Taiwan. Previous studies have shown that temperature changes are associated with incident AMI20. Other studies have shown that temperature extremes or transitions/variability in temperature can trigger acute coronary events21,22. However, a systematic review on the effects of temperature on incident AMI revealed inconsistent findings23. Although some researchers reported that colder temperatures were associated with an increased risk of developing AMI, others reported that high temperature was a significant risk factor for AMI incidence. Possible reasons for this inconsistency may be due to geographic and climatic variations. However, another potentially important reason is that the studies included in the review used inconsistent methods23,24. Some studies adjusted for daily pollutant levels and climate parameters25,26, and some considered only temperature as a linear effect. Still others considered the possibility of lag effects of temperature in various hazard periods before AMI27,28. Furthermore, few studies were conducted in countries located in sub-tropical or tropical climates such as countries in East Asia.
The impact of ambient temperature on ACS morbidity has received attention in the past. However, temperature does not act alone in determining health, but acts in concert with other weather parameters, ambient air pollutants, and aerosol gases. The concept of “synoptic air masses” should be addressed29,30,31. It is reasonable to use a synoptic climatological approach to discern weather effects at a particular location and evaluate potential synergistic impacts of an entire suite of weather elements on environmental and biological parameters sensitive to weather. In our study, we determined the optimal cut points between temperature and pressure in conjunction with humidity and PM 2.5 or PM10 concentrations simultaneously to explore ACS occurrence rates. We trichotomized temperature into high (>26 °C), mild (21–26 °C) and low (<21 °C) categories to address the interaction between weather parameters and ambient air pollutants. As Table 4 shows, high temperature/low AP was associated with the highest risk of developing ACS (OR = 2.236, p < 0.0001). In the low temperature condition, for every 1% increase in RH there was a 1.8% increase in likelihood of developing ACS (OR = 1.018, p < 0.0001). Also, under low temperature, for every 10 μg/m3 increase in PM10 concentration there was a 3.7% increase in likelihood of developing ACS (OR = 1.037, p = 0.018). Also under low temperature, for every 10 μg/m3 increase in PM2.5 concentration there was a 6.9% increase in likelihood of developing ACS (OR = 1.069, p = 0.032). Again under low temperature, an increase in CO by 1 ppm was associated with an increased risk of developing ACS (OR = 1.122, p = 0.032). This indicates that in winter, which in Taiwan is associated with high levels of humidity, a high frequency of rain and increased air pollution, the risk of developing ACS may increase. This concurs with the fact that winter has poorer air quality than other seasons. Our findings indicate that low temperature combined with high ambient CO concentration is a risk factor for developing ACS. A similar finding was reported in a study conducted in Shanghai, China32. CO is a well-recognized cardiovascular toxin, even at lower levels. Exposure to CO has been shown to be associated with increased risk for arrhythmias33, acute myocardial infarction34, pulmonary edema, and cardiogenic shock35. Allred et al. found that patients with coronary artery disease are more susceptible to CO-induced cardiotoxicity36. To the best of our knowledge, no large-scale studies have been conducted on the interaction between weather parameters and ambient air pollutants and risk for ACS in Taiwan. The strength of our study is that the confounding variables such as diabetes, hypertension, dyslipidemia, BMI, age, and sex did not have a significant effect on ACS incidence across the six AP-temperature categories (Table 2). This makes the major interaction effects of temperature, weather parameters and air pollution clearer and more precise, without adjusting for possible confounding variables.
Ambient air particles are a complex mixture of inorganic and organic compounds originating from different sources37, each with complex particle size distributions. An increasing number of studies suggest that ultrafine particles (aerodynamic diameter smaller than approximately 0.1–0.2 μm) as compared with larger particles, which can dominate PM2.5 mass, may have greater adverse cardiovascular effects because of higher deposition efficiency and larger surface area38, as well as higher redox activity39. The association between short-term exposure to particulate air pollution and risk for myocardial infarction has been well studied. Studies have shown that short-term exposure to particulate matter (PM2.5, PM10) is a risk factor for MI and that the risk associated with exposure to PM2.5 is greater than the risk associated with exposure to PM1040. However, ambient PM mass measurements may not adequately represent risk for cardiovascular disease because they are uncharacterized by composition, source or oxidative potential41. A recent study demonstrated that the triggering of myocardial infarction by fine particles is enhanced when particles are enriched in secondary species (sulfate, nitrate, and/or organics)42. Previous experimental results indicated that the mean fine particulate and coarse particulate concentrations are higher in spring and winter than in summer and autumn in Taiwan43. Those results confirm our finding that air pollution is more severe in winter. Lee et al. showed that seasonal variation in composition of PM could be judged by atmospheric visibility44. They found that the seasonal mean visibilities in spring, summer, fall, and winter were only 5.4, 9.1, 8.2, and 3.4 km, respectively. Sulfate was a dominant component that affected both the light scattering coefficient and the visibility in Kaohsiung City, the largest urban city in southern Taiwan. On average, (NH4)2SO4, NH4NO3, total carbon, and fine particulate matter (PM2.5) contributed 53%, 17%, 16%, and 14% to total light scattering, respectively.
Another interesting finding in our study was the observation that the incidence of ACS was higher on the day of and on subsequent days after typhoon Morakot. On 5 August 2009, tropical storm Morakot developed into a typhoon and AP decreased steadily as the typhoon strengthened. The typhoon reached peak intensity early on 7 August with a minimum pressure of 945 hPa and sustained winds of 161 km/h (100 mph), equivalent to a Category 2 hurricane. Later that day, the typhoon made landfall in central Taiwan. About 24 hours later on 9 August, the storm moved off the west coast of the island into the Taiwan Strait, where it turned north-northwest. As seen in Fig. 2, the typhoon was an extreme example of high temperature/low AP, which concurred with our previous statement that high temperature combined with low atmospheric pressure is associated with the highest likelihood of developing myocardial infarction. In addition, this typhoon was a natural disaster, causing severe damage in Taiwan. Table 5 shows that in the typhoon period (7–12 August), the number of ACS cases was greater than average across the entire island. Previous studies have shown an increase in AMI during the immediate hours to weeks following natural disasters45. However, most studies have been conducted on the long-term effects of extreme weather events, such as Hurricane Katrina, which have been shown to be associated with an increased incidence of ACS occurring for up to six years after the hurricane13,46,47. A single-center study found a 3-fold increase in the proportion of admissions for AMI in the 2 years following Katrina (2.18% vs. 0.71%, p < 0.0001), and also noted that the post-Katrina group had higher rates of unemployment, lack of insurance, medication non-compliance, smoking, and substance abuse13. The short-term effect of extreme weather on ACS morbidity has also been investigated. For example, one study showed that 2 weeks following Hurricane Sandy, there was a marked increase in the incidence of myocardial infarction14. Furthermore, another study on Hurricane Sandy also demonstrated that diabetic adults aged 65 years and older were especially at risk for developing acute myocardial infarction the week after that extreme weather event48. The development of ACS in the above-mentioned studies was attributed to the psychological stress of the event and corresponding physiologic derangements49. Although we agree that acute psychological stress plays a role in triggering cardiac events, our results show that other factors are also involved. For example, the most severe damage caused by Typhoon Morakot occurred in southern Taiwan. It is reasonable to hypothesize that people living in southern Taiwan had significantly higher levels of psychological stress after the typhoon than people living in other parts of the island. Therefore, we analyzed the daily ACS incidence during the typhoon period according to corresponding residence areas and tried to find whether the ACS incidence was higher in southern Taiwan. However, there was no significant difference in incidence of ACS among the 4 geographical residence areas (Table 6). This finding implies that the increase in ACS incidence after exposure to extreme weather could not be explained by psychological stress alone. Our data suggest that changes in environmental factors combined with extreme weather may have triggered AMI development. Typhoons are predictable but still destructive. Although we cannot prevent natural disasters, it is feasible to organize ACS teams to cope with the potential for increased ACS patient care needs50.
There are other environmental factors that have been shown to be associated with increases in incidence of MI besides extreme weather events. Typhoons are frequently accompanied by high wind speeds and unstable weather conditions that also dilute and eliminate air pollutants51. One study conducted in Hsinchu Science Park in Taiwan demonstrated that the concentration of polar compounds dropped sharply from 41.4 ppbv before the typhoon to the stage of no detection during the storm, but rose again after the typhoon52. Our findings are also similar to those reported by Swerdel et al. on Hurricane Sandy in New Jersey14. In that study, the authors examined the levels of ambient fine particulate pollution (PM2.5) in New Jersey 2 weeks before and 2 weeks after Hurricane Sandy made landfall on October 29, 2012. They found that the levels of this pollutant were slightly lower in the 2 weeks following Sandy than in the preceding 2 weeks. Our study revealed a downward trend in air pollution during the typhoon period (Fig. 3). Another important environmental factor is influenza. Influenza outbreaks have been reported to be associated with an increase in incidence of MI53. During the days following typhoon Morakot in August 2009, there was no significant increase in influenza cases. In Taiwan, influenza outbreaks mainly occur from late November to March54. The aforementioned statements suggest that these two important environmental factors (influenza and air pollution) did not play a significant role in the incidence of ACS following Typhoon Morakot.
Our findings are similar to those reported by Houck et al. who found that rapid AP decreases are associated with the occurrence of AMI but not with that of stroke55. Although the mechanism is unclear, we hypothesize that changes in AP might contribute to plaque rupture. However, the relationship between AP and ACS risk is inconsistent because of geographic and climate variations and inconsistent methods.
There are some limitations to our study. First, we used data from EPA and CWB monitoring stations near the hospitals rather than obtaining data on exposure to environmental factors for each patient. Second, some cases may not have been enrolled in the registry databank. Third, we did not provide laboratory parameters or functional assessment data, which may have major impacts on ACS mortality. Fourth, we did not have data on living habits such as exercise and diet, which may confound our conclusions. Fifth, we did not assess PM composition or micro-pollutant exposure data in our study, so we cannot provide information on the lag effect of chemical components. Longer observation times may be needed in the future.
Conclusions
One-day lag AP, RH, PM2.5 and PM10 all had significant interaction effects with temperature on the occurrence of ACS. Days on which high temperatures (>26 °C) and low AP (<1009 hPa) occurred the previous day were associated with a greater likelihood of increased incidence of developing ACS. Typhoon Morakot was an example of high temperature with extremely low AP associated with higher ACS incidence than the daily average. These findings, however, should be interpreted with caution and longer observation periods are needed in the future. Combinations of higher PM2.5, PM10 or CO concentrations with lower temperature, and higher RH with lower temperature, were also associated with ACS occurrence. Better understanding of these meteorological patterns and air quality interactions may provide additional measures for cardiovascular disease prevention.
Additional Information
How to cite this article: Huang, C.-H. et al. The Interaction Effects of Meteorological Factors and Air Pollution on the Development of Acute Coronary Syndrome. Sci. Rep. 7, 44004; doi: 10.1038/srep44004 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
The work was funded by grants 104-CCH-NCUE-001 from the Changhua Christian Hospital Research Foundation. Taiwan ACS Full Spectrum Registry was supported by the Sanofi-Aventis Taiwan Co. Ltd. and Bristol-Myers Squibb (Taiwan) Ltd. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We express our gratitude and appreciation to the physicians and nurses participating in the ACS Full Spectrum registry. Principal investigators (in alphabetical order):Kuan-Cheng Chang, China Medical University Hospital; Chia-Lin Chao, Taoyuan General Hospital, Department of Health; Yi-Jen Chen, Wan-Fang Hospital; Chien-Cheng Chen, Show Chwan Memorial Hospital; Cheng-Yun Chen, Chia-Yi Christian Hospital; Chung-Yin Chen, Kuang Tien General Hospital; Fu-Tien Chiang, National Taiwan University Hospital; Shao-Yueh Chiang, Cheng Ching Hospital; Li-Ping Chou, Sin Lau Hospital The Presbyterian Church of Taiwan; Ching-Chang Fang, Tainan Municipal Hospital; Charles Jia-Yin Hou, Mackay Memorial Hospital; Tsuei-Yuan Huang, Chi-Mei Hospital; Gwo-Ping Jong, Taichung Armed Forces General Hospital; Yu-Lin Ko, Taipei Tzu Chi General Hospital; Chi-Tai Kuo, Linkou Chang Gung Memorial Hospital; Wen-Ter Lai, Kaohsiung Medical University Chung-Ho Memorial Hospital; Wen-Lieng Lee, Taichung Veterans General Hospital; Chun-I Lee, Pingtung Christian Hospital; Meng-Huan Lei, Lo-Tung Po-Ai Hospital; Ai-Hsien Li, Far Eastern Memorial Hospital; Yi-Heng Li, National Cheng Kung University Hospital; Jou-Wei Lin, National Taiwan University Hospital, Yun-lin Branch; Tin-Kwang Lin, Dalin Tzuchi General Hospital; Jih-Min Lin, Keelung Hospital, Department of Health; Shing-Jong Lin, Taipei Veterans General Hospital; Hung-Shun Lo, Cathay General Hospital; Guang-Yuan Mar, Kaohsiung Veterans General Hospital; Chun-Ming Shih, Taipei Medical University Hospital; Kou-Gi Shyu, Shin Kong Wu Ho-Su Memorial Hospital; Cheng-Dao Tsai, Changhua Christian Hospital; Chuen-Den Tseng, National Taiwan University Hospital; Kwo-Chang Ueng, Chung Shan Medical University Hospital; Ji-Hung Wang, Hualien Tzu Chi General Hospital; Kuang-Te Wang, Mackay Memorial Hospital, Taitung Branch; Ming-Shien Wen, Linkou Chang Gung Memorial Hospital; Szu-Chi Wen, Hsin Chu General Hospital, Department of Health; Chiung-Jen Wu, Kaohsiung Chang Gung Memorial Hospital; Shih-Ping Yang, Tri-Service General Hospital; Wei-Hsian Yin, Cheng-Hsin General Hospital. We would like to thank Dr. Chew-Teng Kor for her contributions to the statistical analysis assistance in the study.
Footnotes
The authors declare no competing financial interests.
Author Contributions All authors reviewed the manuscript. C.-H.H. and I.-B.L. performed the analysis, and wrote the manuscript. H.-C.L. collected the data and performed the analysis. C.-C.C. and I.-B.L. conceived and designed the experiments. C.-D.T., H.-K.H. performed the experiments and collected the data. C.-H.H., H.-C.L., C.-D.T., H.-K.H., I.-B.L. and C.-C.C. contributed to the discussion and manuscript revision.
References
- Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T. & Murray C. J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet 367, 1747–1757 (2006). [DOI] [PubMed] [Google Scholar]
- White H. D. & Chew D. P. Acute myocardial infarction. The Lancet 372, 570–584 (2008). [DOI] [PubMed] [Google Scholar]
- Taiwan Department of Health. Statistics data. Statistical analysis of 2009 mortality data. Press conference on 2009 mortality data. Available: http://www.doh.gov.tw. Accessed 2011 Jan 19.
- Lee C.-H. et al. Trends in the incidence and management of acute myocardial infarction from 1999 to 2008: get with the guidelines performance measures in Taiwan. Journal of the American Heart Association 3, e001066 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan W. S. H. Taiwan’s healthcare report 2010. EPMA Journal 1, 563 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet 364, 937–952 (2004). [DOI] [PubMed] [Google Scholar]
- Verberkmoes N., Hamad M. S., Ter Woorst J., Peels C. & van Straten A. Impact of temperature and atmospheric pressure on the incidence of major acute cardiovascular events. Netherlands Heart Journal 20, 193–196 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radišauskas R. et al. Trends of myocardial infarction morbidity and its associations with weather conditions. Medicina 50, 182–189 (2014). [DOI] [PubMed] [Google Scholar]
- Zanobetti A. & Peters A. Disentangling interactions between atmospheric pollution and weather. Journal of epidemiology and community health 69, 613–615 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheray K. R., Aitken P., Goggins W., Rainer T. & Graham C. A. Epidemiology of injuries due to tropical cyclones in Hong Kong: a retrospective observational study. Injury 43, 2055–2059 (2012). [DOI] [PubMed] [Google Scholar]
- Lin C.-H., Hou S.-K., Shih F. F.-Y. & Su S. The Effect of Tropical Cyclones (Typhoons) on Emergency Department Visits. The Journal of emergency medicine 45, 372–379 (2013). [DOI] [PubMed] [Google Scholar]
- Usher K. et al. Preparedness for and impact of tropical Cyclone Yasi in North Queensland, Australia. Prehospital and disaster medicine 28, 272–278 (2013). [DOI] [PubMed] [Google Scholar]
- Gautam S., Menachem J., Srivastav S. K., Delafontaine P. & Irimpen A. Effect of Hurricane Katrina on the incidence of acute coronary syndrome at a primary angioplasty center in New Orleans. Disaster medicine and public health preparedness 3, 144–150 (2009). [DOI] [PubMed] [Google Scholar]
- Swerdel J. N., Janevic T. M., Cosgrove N. M. & Kostis J. B. The Effect of Hurricane Sandy on Cardiovascular Events in New Jersey. Journal of the American Heart Association 3, e001354 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shyu K.-G. et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome-observations from the Taiwan ACS full spectrum registry. Acta Cardiologica Sinica 27, 135–144 (2011). [Google Scholar]
- Chua S.-K., Lo H.-M., Chiu C.-Z. & Shyu K.-G. Use of CHADS 2 and CHA 2 DS 2-VASc Scores to Predict Subsequent Myocardial Infarction, Stroke, and Death in Patients with Acute Coronary Syndrome: Data from Taiwan Acute Coronary Syndrome Full Spectrum Registry. PloS one 9, e111167 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering T. G. et al. Recommendations for blood pressure measurement in humans and experimental animals part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 45, 142–161 (2005). [DOI] [PubMed] [Google Scholar]
- Chiang C.-E. et al. Guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. Journal of the Chinese Medical Association 78, 1–47 (2015). [DOI] [PubMed] [Google Scholar]
- Pan W. Akaike’s information criterion in generalized estimating equations. Biometrics 57, 120–125 (2001). [DOI] [PubMed] [Google Scholar]
- Claeys M. J., Rajagopalan S., Nawrot T. S. & Brook R. D. Climate and environmental triggers of acute myocardial infarction. European heart journal ehw151 (2016). [DOI] [PubMed] [Google Scholar]
- Danet S. et al. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths a 10-year survey: The lille-world health organization monica project (monitoring trends and determinants in cardiovascular disease). Circulation 100, e1–e7 (1999). [DOI] [PubMed] [Google Scholar]
- Barnett A. G. et al. Cold periods and coronary events: an analysis of populations worldwide. Journal of epidemiology and community health 59, 551–557 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskaran K. et al. The effects of ambient temperature on the incidence of myocardial infarction–A systematic review. Heart (2009). [DOI] [PubMed]
- Goggins W. B., Chan E. Y. & Yang C.-Y. Weather, pollution, and acute myocardial infarction in Hong Kong and Taiwan. International journal of cardiology 168, 243–249 (2013). [DOI] [PubMed] [Google Scholar]
- Barnett A. G., Sans S., Salomaa V., Kuulasmaa K. & Dobson A. J. The effect of temperature on systolic blood pressure. Blood pressure monitoring 12, 195–203 (2007). [DOI] [PubMed] [Google Scholar]
- Saeki K. et al. The relationship between indoor, outdoor and ambient temperatures and morning BP surges from inter-seasonally repeated measurements. Journal of human hypertension 28, 482–488 (2014). [DOI] [PubMed] [Google Scholar]
- Claeys M. J. et al. Environmental triggers of acute myocardial infarction: results of a nationwide multiple-factorial population study. Acta Cardiol 70, 693–701 (2015). [DOI] [PubMed] [Google Scholar]
- Raven P., Niki I., Dahms T. & Horvath S. Compensatory cardiovascular responses during an environmental cold stress, 5 degrees C. Journal of Applied Physiology 29, 417–421 (1970). [DOI] [PubMed] [Google Scholar]
- Morabito M. et al. Winter air-mass-based synoptic climatological approach and hospital admissions for myocardial infarction in Florence, Italy. Environmental Research 102, 52–60 (2006). [DOI] [PubMed] [Google Scholar]
- Vanos J. K. et al. Synoptic weather typing applied to air pollution mortality among the elderly in 10 Canadian cities. Environmental Research 126, 66–75 (2013). [DOI] [PubMed] [Google Scholar]
- Vanos J. K., Hebbern C. & Cakmak S. Risk assessment for cardiovascular and respiratory mortality due to air pollution and synoptic meteorology in 10 Canadian cities. Environmental Pollution 185, 322–332 (2014). [DOI] [PubMed] [Google Scholar]
- Wang X.-D. et al. Short-term effects of air pollution on acute myocardial infarctions in Shanghai, China, 2013–2014. Journal of geriatric cardiology: JGC 13, 132 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandini C. et al. Carbon monoxide cardiotoxicity. Journal of Toxicology: Clinical Toxicology 39, 35–44 (2001). [DOI] [PubMed] [Google Scholar]
- Hsu P.-C. et al. Acute carbon monoxide poisoning resulting in ST elevation myocardial infarction: a rare case report. The Kaohsiung journal of medical sciences 26, 271–275 (2010). [DOI] [PubMed] [Google Scholar]
- McMeekin J. & Finegan B. Reversible myocardial dysfunction following carbon monoxide poisoning. The Canadian journal of cardiology 3, 118–121 (1987). [PubMed] [Google Scholar]
- Allred E. N. et al. Short-term effects of carbon monoxide exposure on the exercise performance of subjects with coronary artery disease. New England Journal of Medicine 321, 1426–1432 (1989). [DOI] [PubMed] [Google Scholar]
- Brook R. D. et al. Particulate matter air pollution and cardiovascular disease an update to the scientific statement from the American Heart Association. Circulation 121, 2331–2378 (2010). [DOI] [PubMed] [Google Scholar]
- Delfino R. J., Sioutas C. & Malik S. Potential role of ultrafine particles in associations between airborne particle mass and cardiovascular health. Environmental health perspectives, 934–946 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo J. A. et al. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circulation research 102, 589–596 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo C. et al. Short-term exposure to particulate air pollution and risk of myocardial infarction: a systematic review and meta-analysis. Environmental Science and Pollution Research 22, 14651–14662 (2015). [DOI] [PubMed] [Google Scholar]
- Zhang X. et al. Associations between microvascular function and short-term exposure to traffic-related air pollution and particulate matter oxidative potential. Environmental Health 15, 81 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich D. Q. et al. The triggering of myocardial infarction by fine particles is enhanced when particles are enriched in secondary species. Environmental science & technology 47, 9414–9423 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang G.-C., Wu Y.-S., Lee W.-J., Chou T.-Y. & Lin I.-C. Seasonal variation in concentration and metallic constituents of atmospheric particulates near the western coast of central Taiwan. Toxicology and industrial health 22, 193–201 (2006). [DOI] [PubMed] [Google Scholar]
- Lee C.-G., Yuan C.-S., Chang J.-C. & Yuan C. Effects of aerosol species on atmospheric visibility in Kaohsiung city, Taiwan. Journal of the Air & Waste Management Association 55, 1031–1041 (2005). [DOI] [PubMed] [Google Scholar]
- Strike P. C. & Steptoe A. Behavioral and emotional triggers of acute coronary syndromes: a systematic review and critique. Psychosomatic Medicine 67, 179–186 (2005). [DOI] [PubMed] [Google Scholar]
- Peters M. N. et al. Effect of Hurricane Katrina on chronobiology at onset of acute myocardial infarction during the subsequent three years. The American journal of cardiology 111, 800–803 (2013). [DOI] [PubMed] [Google Scholar]
- Peters M. N. et al. Natural disasters and myocardial infarction: the six years after Hurricane Katrina. in Mayo Clinic ProceedingsVol. 89 472–477 (Elsevier, 2014). [DOI] [PubMed] [Google Scholar]
- Lee D. C. et al. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Research & Care 4, e000248 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayman K. G., Sharma D., Wardlow R. D. & Singh S. Burden of cardiovascular morbidity and mortality following humanitarian emergencies: a systematic literature review. Prehospital and disaster medicine 30, 80–88 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai T. I., Shih F. Y., Chiang W. C., Shen S. T. & Chen W. J. Strategies of disaster response in the health care system for tropical cyclones: experience following Typhoon Nari in Taipei City. Academic emergency medicine 10, 1109–1112 (2003). [DOI] [PubMed] [Google Scholar]
- Chiang P.-C., Chang E., Chang T.-C. & Chiang H.-L. Seasonal source-receptor relationships in a petrochemical industrial district over Northern Taiwan. Journal of the Air & Waste Management Association 55, 326–341 (2005). [DOI] [PubMed] [Google Scholar]
- Nian H.-C. et al. Impact of inclement weather on the characteristics of volatile organic compounds in ambient air at the Hsinchu Science Park in Taiwan. Science of the Total Environment 399, 41–49 (2008). [DOI] [PubMed] [Google Scholar]
- Foster E. et al. Acute myocardial infarctions, strokes and influenza: seasonal and pandemic effects. Epidemiology and infection 141, 735–744 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan Y.-C. et al. Epidemiology of pandemic influenza A/H1N1 virus during 2009–2010 in Taiwan. Virus research 177, 46–54 (2013). [DOI] [PubMed] [Google Scholar]
- Houck P. D., Lethen J. E., Riggs M. W., Gantt D. S. & Dehmer G. J. Relation of atmospheric pressure changes and the occurrences of acute myocardial infarction and stroke. The American journal of cardiology 96, 45–51 (2005). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.