Abstract
Aims and Objectives:
To determine the prevalence and types of jaw pathologic findings as detected in panoramic radiographs of a sample of young women attending a teaching hospital in Al Madinah Al Munawarah, Saudi Arabia, and to determine the most important factors that predict the occurrence of jaw pathologic findings.
Materials and Methods:
The electronic clinical files of a representative sample of female patients who attended the outpatient dental clinics were retrieved. Patients were aged 18 to 25 years. Types of pathologic radiographic jaw findings and their prevalence were determined through screening of panoramic radiographs. Data were analyzed using the statistical analysis software [SPSS version 21 (IBM Corp.)]. Multiple linear regression was used to explore the significance of some types of dental lesions as predictor variables for the occurrence of jaw pathologic findings.
Results:
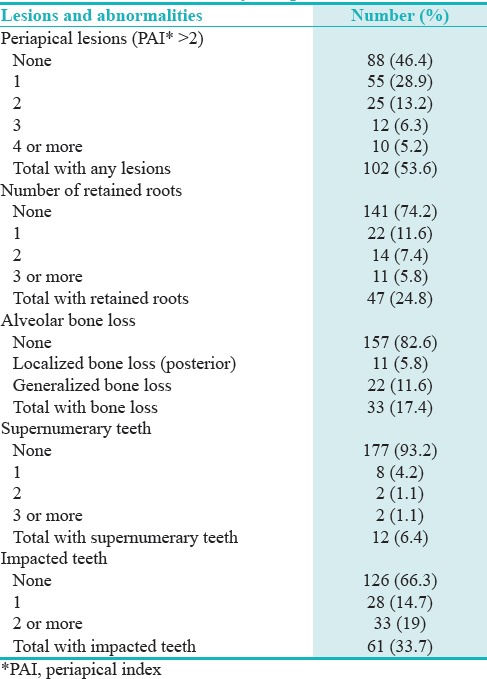
A total of 190 patients (mean age, 22.4 ± 2.46 years) were included in the study. Periapical lesions, retained roots, and alveolar bone loss were detected in 53.6%, 24.8%, and 17.4% of the participants, respectively. Other odontogenic abnormalities such as supernumerary and impacted teeth (6.4% and 33.7%, respectively) were also detected. Patients' age was found to be a good predictor for alveolar bone loss and number of periapical lesions (P ≤ 0.05).
Conclusions:
A high prevalence of periapical lesions, retained roots, and alveolar bone loss was found among a sample of young female dental attendees, as shown by their panoramic radiographs. Further studies are needed to explore potential risk factors for such a noticeable trend of poor oral health, and the needed strategies to counteract this trend.
KEYWORDS: Alveolar bone loss, jaw lesions, periapical lesions, young women
INTRODUCTION
Oral disease is considered globally one of the most common public health problems with important socioeconomic implications.[1] Among oral diseases, dental caries is the most common disease worldwide.[2] Poor oral health associated with dental caries and periodontal disease may lead to loss of teeth,[3] and can result in a number of debilitating diseases such as cardiovascular disease and adverse pregnancy outcomes.[4] In recent years, a substantial amount of research was conducted among Saudi women to investigate their health and health risk-related behaviors.[5,6] This favorably growing interest to collect data on women's health was notably paralleled by quite a reluctance to investigate their oral health and oral hygiene practices. Most of oral health research in this part of the world was conducted among children or among the general population, but young women received little attention.[7] In this era of globalization and social networking, oral health may be impacted by the changing trends in social habits of women such as smoking[8] and oral hygiene habits.
A previous study reported an alarmingly high prevalence of dental disease as indicated by a high mean number of decayed, missing and filled teeth (DMFT) among a sample of young women in the age range of 18–25 years in the Western region of Saudi Arabia.[7]
Al Madinah Al Munawarah (the “enlighted city” in Arabic) is the second holiest site in Islam after Makkah, and is situated in the Hijaz region of Western Saudi Arabia. Its 2 million population is multiracial; a characteristic that has significantly impacted their social habits including diet, oral hygiene, and other health behaviors. A substantial proportion of Al Madinah women, regardless of their nationality, attend the Dental College and Hospital of Taibah University to receive free dental treatment services.
We conducted this study among a sample of young women to target those who are in an important phase of life and to address a pivotal period of any woman's life, the age of founding families and child-bearing. With the obvious deficiency in current research on women's oral health, the aims of this study were to estimate the prevalence of jaw findings as detected in panoramic radiographs and to investigate the significance of DMFT components as predictors for the radiographic findings in a sample of young women attending the Taibah University Dental College & Hospital (TUDCH) in Al Madinah Al Munawarah.
MATERIALS AND METHODS
This descriptive retrospective study was approved by the Taibah University College of Dentistry Research Ethics Committee “TUCD-REC” on November 14th 2014. A waiver of informed consent was approved being a retrospective study, and confidentiality of the data was guaranteed. The study was carried out at TUDCH in Al Madinah Al Munawarah.
The study involved retrieving electronic files stored on the clinical software system used at TUDCH [CS R4 Clinical + Practice Management Software (Carestream Dental Ltd, Rochester, NY)] during the period of 2013–2014. Extracted data included patient's age and the panoramic radiographs taken during the standard screening visit for all patients visiting TUDCH, unless otherwise necessitated. The panoramic radiographs were taken utilizing a digital imaging system [CS 9000 Select 3D Extraoral digital Imaging System SM749 (Rochester NY)]. The electronic records selected were those of patients aged 18–25 years. Presence of a recent, high quality, clear panoramic radiograph was also an inclusion criterion. Patients with radiographs that were unclear or had distortion, overlapping, or positioning errors, were excluded from the study.
Records of patients with systemic disease were also excluded from the study. Patient records fulfilling the inclusion criteria were selected. Taking into consideration that 1668 patients in the age range 18–25 attended TUCDH during the period 2013–2014, sample size determination was calculated using special software (Epi Info software, Center for Disease Control) based on 80–90% power of the study and an expected frequency of 50% radiographic jaw findings and a confidence limit of 5%, the required sample size was 190. Data on DMFT of patients were retrieved from dental charts that existed in the clinical records to study the associations with radiographic findings.
Author SK, a radiologist with experience in interpretation of pathologies and abnormalities affecting the jaw bones and teeth performed the radiographic interpretation. Screened findings included alveolar bone loss (localized or generalized), radiolucent periapical bony lesions, retained roots, supernumerary teeth, and impacted teeth. All working conditions were similar and standardized each time during panoramic interpretation in the work station.
The periapical region was assessed by using the periapical index (PAI) score. This scoring system is described as follows: PAI: 1 = Normal periapical structures, 2 = Small changes in bone structure, 3 = Changes in bone structure with some mineral loss, 4 = Periodontitis with well-defined radiolucent area, and 5 = Severe periodontitis with exacerbating features. A score greater than 2 (PAI, 3) was considered to be an indication of periapical lesion.[9]
With regards to alveolar bone loss, we calibrated the measurements using the linear measurement tool of CS9000 software to estimate the alveolar bone height on panoramic radiographs using specific anatomic landmarks as a reference; namely the cementoenamel junction (CEJ) and alveolar crest. Bone loss was noted when the distance from the CEJ to the alveolar crest exceeded 2 mm.[10,11] Alveolar bone loss in panoramic radiograph was considered either localized if 30% or less of sites were affected, or generalized if more than 30% of sites were affected. All measurements were taken by the same calibrated operator.
STATISTICAL ANALYSIS
Descriptive statistics in the form of frequency distributions were used to describe the study sample and prevalence of radiographic lesions. Multiple linear regression was used to explore the significance of tooth caries, missing teeth, filled teeth, and the final DMFT score as predictor variables for the occurrence of various radiographic lesions. Data were analyzed using the statistical analysis software [SPSS version 21 (IBM Corp.)].
RESULTS
Panoramic radiographs of 190 patients were included in this study. Their mean age was 22.4 years (SD = 2.46). Panoramic radiographs revealed a wide variety of jaw lesions and abnormalities including retained roots, alveolar bone loss, periapical lesions, supernumerary teeth, and impacted teeth [Figure 1]. Jaw findings in number and percentage are shown in Table 1. A percentage of 53.6% had periapical lesions, and alveolar bone loss affected 17% of the study sample.
Figure 1.
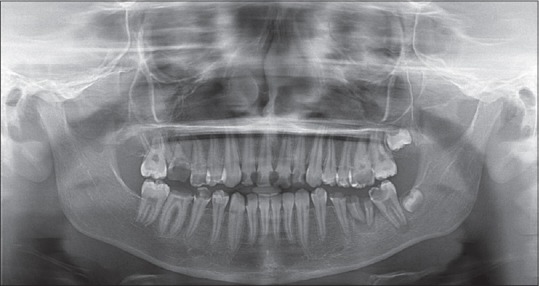
A panoramic radiograph of a 20-year-old female patient showing neglected mouth with multiple carious teeth, retained roots, and periapical lesions
Table 1.
Periapical lesions, retained roots, alveolar bone loss, supernumerary teeth, and impacted teeth among the study sample
Tables 2–6 display the details of regression models for the prediction of number of periapical lesions and level of alveolar bone loss. Based on the two regression models in this study, we can predict in a similar population the number of periapical lesions by
Table 2.
Regression analysis with dependent variable: number of periapical lesions. Predictor variables: age of the patient, carious teeth, missing teeth, and filled teeth
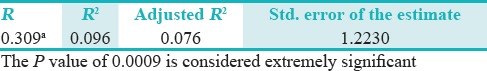
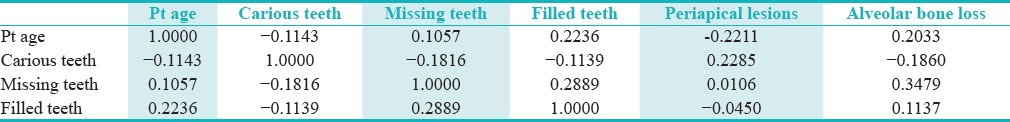
Table 6.
Correlation matrix of predictor variables for the two regression models
No. PA lesions = 2.942 – 0.106 × (Age of patient in years) + 0.069 × (no. of carious teeth) + 0.039 × (no. of missing teeth) + 0.002 × (no. of filled teeth).
The level of alveolar bone loss by
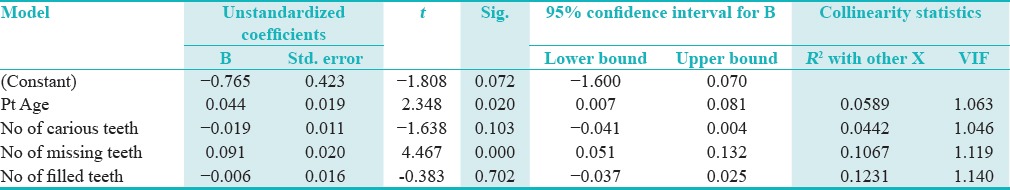
Level of alveolar bone loss= −0.765 + 0.044 × (Age of patient in years) – 0.019 × (no. of carious teeth) + 0.091 × (no. of missing teeth) – 0.006 × (no. of filled teeth).
Tables 2 and 4 show summary of the two models. Tables 3 and 5 show coefficients of the two models, and Table 6 shows the correlation matrix of the predictor variables and the dependent variables in the two models.
Table 4.
Regression analysis with dependent variable: Level of alveolar bone loss. Predictor variables: Age of the patient, carious teeth, missing teeth, and filled teeth
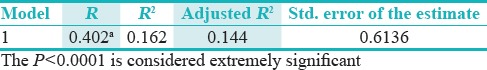
Table 3.
Coefficients and significance of their contribution to the model. Dependent variable: number of periapical lesions
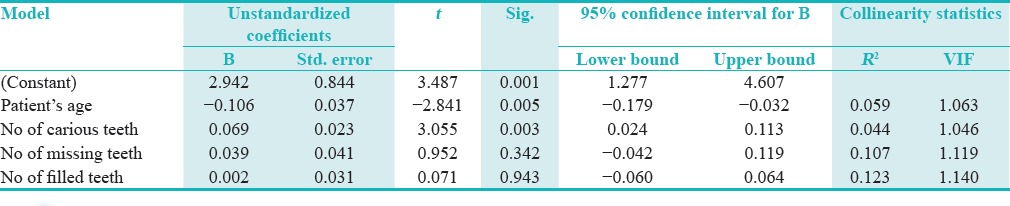
Table 5.
Coefficients and significance of their contribution to the model. Dependent variable: Level of alveolar bone loss
DISCUSSION
This retrospective study aimed at utilizing panoramic radiographs and dental charts available in electronic clinical records to estimate the prevalence of pathologic jaw findings, as well as aimed at investigating the significance of DMFT components as predictors for the radiographic findings in a sample of young women. More than 50% of the study sample had periapical lesions, approximately quarter of the sample had retained roots, and slightly less than 20% had alveolar bone loss that was in most of the cases generalized in nature. Other developmental nonpathologic findings included supernumerary teeth and impacted teeth that occurred in 6.4% and 33.7% of the sample, respectively. A previous study that was done in our center among the same age group found an alarmingly high DMFT index of approximately 9.[7] This prompted us to study their panoramic radiographs to document and report radiographic findings, if any.
Panoramic radiographs are routinely taken for all adult patients on their first screening visit to TUDCH. The use of panoramic radiographs as a routine screening tool has been criticized for their cost and radiation exposure to patients.[12] Panoramic radiographs that were taken for our patients were based on digital rather than plain film radiography. Using the digital technique the radiation dose is reduced by up to 80%,[13] and the technique is cost-effective as well. An added feature of digital radiographs is the ability to manipulate radiographs by zooming in and changing contrast, which is a useful tool in assessing bony defects.[14] This is particularly useful when scoring periapical lesions.[15] We assessed the presence of radiolucent periapical lesions radiographically because it is considered as an indicator for the presence of apical periodontitis (AP), which is an inflammation of the periodontium at the tooth apex due to dental pulp infection and tooth caries. AP affects bone density and is characterized radiographically by presence of periapical radiolucency. We used the PAI scoring system for identification of periapical lesions in panoramic images as advocated by several studies.[15,16,17,18]
More than half of our sample had periapical lesions (PAI > 2). While periapical lesions are not always the result of pulpal necrosis,[19] a high prevalence among a young age group indicates poor oral health. Furthermore, almost one in every four had retained roots, confirming the general trend of poor oral health. A recent study conducted in Malawi found a prevalence of 23.5% of periapical lesions in a sample of pregnant women.[20] Studies that were done in Western countries among the same age group, on the other hand, have found completely different results with excellent oral and dental health, which, as the researchers suggest, may reflect the use of fluoride and high levels of oral health education.[21] Taking into consideration the critical age range of our sample, the child bearing age, such patients may be susceptible to an increased risk of shorter pregnancy duration and intrauterine growth restriction as a result of such a high prevalence of periapical lesions.[20]
Another bone pathology in the form of alveolar bone loss affected 17% of the study sample, with most of the alveolar bone loss cases (11.6%) having a generalized pattern. On the other hand, localized posterior alveolar bone loss affected 5.8% of the patients. Alveolar bone loss is a hallmark of periodontitis, which is multifactorial in nature.[22] Because records of patients with any systemic diseases were not included in the study, one could exclude the assumption that the detected alveolar bone loss was indirectly related to a systemic illness rather than local factors such as dental plaque. However, this study did not investigate oral hygiene practices of the study sample. Therefore, an association between oral hygiene status and alveolar bone loss could not be established. Nevertheless, it is well-established that women who are in the child bearing age and who have periodontal disease are probably susceptible to adverse pregnancy outcomes. It was shown that periodontal disease is associated with preeclampsia,[23] preterm birth,[24] and low birth weight.[25] Mothers with periodontitis are six times more likely to have low birth weight children than mothers without periodontitis.[26] Furthermore, pregnancy itself has its own adverse impact on oral health due to hormonal changes.[27]
Perhaps pathologic alveolar bone loss itself can be considered as a predictor for many pathologies that may appear in a population of young females, however, the absence of full scale radiographic data for any given population, poses another limiting factor.
Regression analysis in this study indicated that patient age and number of carious teeth are statistically significant predictors of the number of periapical lesions. On the other hand, patient age, number of carious teeth, and number of missing teeth were statistically significant predictors for alveolar bone loss. The older our patients were the higher was the incidence of alveolar bone loss, and the lower is the incidence of periapical lesions. This can be explained by the fact that periapical bone lesions do not persist over the years and affected teeth tend to be either lost by extraction as a result of pain and loss of function, or treated endodontically, if restorable. DMFT was not used in the two regression models for periapical bone lesions and alveolar bone loss because of problems of multicollinearity of predictor variables (i.e., number of carious teeth, missing teeth and filled teeth). However, after the elimination of DMFT as a predictor, multicollinearity was not a problem. Furthermore, R2 values were less than 0.75 indicating independent variables. Based on the values of R2, regression models could explain 9.6% of the variance in number of periapical lesions, and they could explain 16.2% of variance in the level of alveolar bone loss. However, both models were extremely significant for the predictors of the number of periapical bone lesions and the level of alveolar bone loss (P = 0.0009 and P = 0.0001, respectively).
This study is considered the first study that provides an insight into the radiographic jaw findings of young females who reside in Al Madina Al Munawarah with interesting results. Hopefully, more studies are to follow focusing on females in different age groups and various ethnic backgrounds.
Another strength of this study is that it highlighted the use of prediction of bone pathology (periapical lesions and alveolar bone loss) in case panoramic radiographs were not available. This becomes even more important in pregnant women who may oppose radiographic examination due to cultural misbeliefs. A recent study conducted among a sample of pregnant women in Saudi Arabia reported that approximately 50% of the study sample believed that dental radiographs affect the fetus adversely.[28]
A limitation of this study is the relatively small sample size. However, the sample size was calculated to produce 85% power, which can be judged to be sufficient. In our previous study,[7] we included 419 patient records, however, we found only 190 patients who had panoramic radiographs saved in the R4 system. This discrepancy resulted as the patient record system was converted to the electronic R4 system with unexpected loss of some radiographic data.
Another limitation of the study emanates from the fact that it was a retrospective study that utilized only the data that are stored in the electronic patients' records, hence, the risk factors that may be associated with the current findings were not investigated.
The possible risk factors, though, could be one or more of the following poor oral hygiene, poor dietary habits, socioeconomic status, and genetic factors. All of the aforementioned factors are actually worth investigation. Previous studies have reported that young females in Saudi Arabia are likely to neglect oral hygiene habits and follow poor dietary habits.[29] Economic rush has been considered an important factor in changing dietary and oral health habits of the Saudis.[30] However, one should be careful in interpreting the results of this study since Al Madinah is a cosmopolitan city and its residents come from almost all over the Muslim world. The dietary and hygiene habits of such a multiethnic population are variable. Further studies are needed to investigate the racial and genetic susceptibility of these patients to dental and periodontal disease.
The findings of this study should alert local authorities such as the Ministry of Health to implement preventive oral health programs that target women, particularly young age groups. These preventive programs can be implemented as a joint collaboration between Ministry of Health and Ministry of Higher Education to address female university students. The need for such programs becomes particularly obvious when assessing the current status of primary care centers affiliated to the local Ministry of Health. The dental sector of primary care centers faces important challenges that makes oral health care fall short of patient expectations.[31] Lack of advanced dental treatment and high cost of dental treatment in private clinics[31] are two important factors that should motivate the local government to implement preventive programs. Within the same context, organized screening programs in the form of national mass screening campaigns targeting oral diseases, can be integrated in the health system to seek out undiagnosed patients or patients with difficulties in accessing the healthcare system. Another important aspect that can improve oral health care is to implement policies that target cultural attitudes that could hinder providing this type of care. One of the cultural attitudes that may be considered controversial is the difficulty, with which women can get transportation to access dental services in Saudi Arabia. AlBarakati (2009) investigated reasons for failed dental appointments among a sample of Saudi women. She found that 68% relied on a family member for transportation to their dental appointment, and another 76.2% reported that transportation difficulty is a relevant factor in missing the appointment, some of them attributed this to appointment conflicting with their husbands' work.[32] However, lately, people have started to use smartphone applications to get transportation in various areas of Kingdom of Saudi Arabia. In particular, women are the main recipients of these services which could replace the reliance on family members for transportation.
CONCLUSIONS AND RECOMMENDATIONS
A high prevalence of pathologic radiographic jaw findings were detected in a sample of young female patients in Al Madina Al Munawarah, indicating poor oral health. Risk factors contributing to these findings are urgently needed to be addressed to design policies that counteract this problem. Age and the number of decayed teeth were significant predictors for periapical lesions. Along with the number of missing teeth, they were also significant predictors for alveolar bone loss.
In the case where obtaining radiographs is difficult or unavailable, regression models from this study can be utilized to predict the presence of intrabony lesions in patients (after verification). It is anticipated that a research group that is fully dedicated to investigating all aspects of oral health of women in Al Madinah to be formed officially in the near future, with a vision to change women's attitudes and perceptions towards oral health as a major factor in determining quality of life and general systemic health.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2016 doi: 10.1111/odi.12428. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Shaffer JR, Leslie EJ, Feingold E, Govil M, McNeil DW, Crout RJ, et al. Caries Experience Differs between Females and Males across Age Groups in Northern Appalachia. Int J Dent. 2015;2015:938213. doi: 10.1155/2015/938213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neiswanger K, McNeil DW, Foxman B, Govil M, Cooper ME, Weyant RJ, et al. Oral Health in a Sample of Pregnant Women from Northern Appalachia (2011-2015) Int J Dent. 2015;2015:469376. doi: 10.1155/2015/469376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papapanou PN. Systemic effects of periodontitis: Lessons learned from research on atherosclerotic vascular disease and adverse pregnancy outcomes. Int Dent J. 2015;65:283–91. doi: 10.1111/idj.12185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daoud F, El Bcheraoui C, Tuffaha M, AlMazroa MA, Al Saeedi M, Nooh RM, et al. The health status of Saudi women: Findings from a national survey. J Public Health. 2015 doi: 10.1093/pubmed/fdv157. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.AlObaid A, Al-Badawi IA, Al-Kadri H, Gopala K, Kandeil W, Quint W, et al. Human papillomavirus prevalence and type distribution among women attending routine gynecological examinations in Saudi Arabia. BMC Infect Dis. 2014;14:643. doi: 10.1186/s12879-014-0643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khateeb SH B, Gafar A, Jaber S, Dar-Odeh N. Prevalence of Dental Caries among Young Women in Central Western Region of Saudi Arabia. Int J Adv Dent Med Sci. 2015;1:46–9. [Google Scholar]
- 8.Dar-Odeh NS, Abu-Hammad OA. The changing trends in tobacco smoking for young Arab women; narghile, an old habit with a liberal attitude. Harm Reduct J. 2011;8:24. doi: 10.1186/1477-7517-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orstavik D, Kerekes K, Eriksen HM. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2:20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 10.Hansen BF, Gjermo P, Bergwitz-Larsen KR. Periodontal bone loss in 15-year-old Norwegians. J Clin Periodontol. 1984;11:125–31. doi: 10.1111/j.1600-051x.1984.tb00840.x. [DOI] [PubMed] [Google Scholar]
- 11.Hansen BF, Gjermo P, Bellini HT, Ihanamaki K, Saxen L. Prevalence of radiographic alveolar bone loss in young adults, a multinational study. Int Dent J. 1995;45:54–61. [PubMed] [Google Scholar]
- 12.Rushton VE, Horner K, Worthington HV. Screening panoramic radiology of adults in general dental practice: Radiological findings. Br Dent J. 2001;190:495–501. doi: 10.1038/sj.bdj.4801014. [DOI] [PubMed] [Google Scholar]
- 13.Mouyen F, Benz C, Sonnabend E, Lodter JP. Presentation and physical evaluation of RadioVisioGraphy. Oral Surg Oral Med Oral Pathol. 1989;68:238–42. doi: 10.1016/0030-4220(89)90200-4. [DOI] [PubMed] [Google Scholar]
- 14.Corbet EF, Ho DK, Lai SM. Radiographs in periodontal disease diagnosis and management. Aust Dent J. 2009;54(Suppl 1):S27–43. doi: 10.1111/j.1834-7819.2009.01141.x. [DOI] [PubMed] [Google Scholar]
- 15.Ridao-Sacie C, Segura-Egea JJ, Fernandez-Palacin A, Bullon-Fernandez P, Rios-Santos JV. Radiological assessment of periapical status using the periapical index: Comparison of periapical radiography and digital panoramic radiography. Int Endod J. 2007;40:433–40. doi: 10.1111/j.1365-2591.2007.01233.x. [DOI] [PubMed] [Google Scholar]
- 16.Jimenez-Pinzon A, Segura-Egea JJ, Poyato-Ferrera M, Velasco-Ortega E, Rios-Santos JV. Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int Endod J. 2004;37:167–73. doi: 10.1111/j.0143-2885.2004.00759.x. [DOI] [PubMed] [Google Scholar]
- 17.Kirkevang LL, Horsted-Bindslev P, Orstavik D, Wenzel A. Frequency and distribution of endodontically treated teeth and apical periodontitis in an urban Danish population. Int Endod J. 2001;34:198–205. doi: 10.1046/j.1365-2591.2001.00370.x. [DOI] [PubMed] [Google Scholar]
- 18.Segura-Egea JJ, Jimenez-Pinzon A, Rios-Santos JV, Velasco-Ortega E, Cisneros-Cabello R, Poyato-Ferrera M. High prevalence of apical periodontitis amongst type 2 diabetic patients. Int Endod J. 2005;38:564–69. doi: 10.1111/j.1365-2591.2005.00996.x. [DOI] [PubMed] [Google Scholar]
- 19.Kontogiannis TG, Tosios KI, Kerezoudis NP, Krithinakis S, Christopoulos P, Sklavounou A. Periapical lesions are not always a sequelae of pulpal necrosis: A retrospective study of 1521 biopsies. Int Endod J. 2015;48:68–73. doi: 10.1111/iej.12276. [DOI] [PubMed] [Google Scholar]
- 20.Harjunmaa U, Jarnstedt J, Alho L, Dewey KG, Cheung YB, Deitchler M, et al. Association between maternal dental periapical infections and pregnancy outcomes: Results from a cross-sectional study in Malawi. Trop Med Int Health. 2015;20:1549–58. doi: 10.1111/tmi.12579. [DOI] [PubMed] [Google Scholar]
- 21.Peltola JS, Venta I, Haahtela S, Lakoma A, Ylipaavalniemi P, Turtola L. Dental and oral radiographic findings in first-year university students in 1982 and 2002 in Helsinki, Finland. Acta Odontol Scand. 2006;64:42–6. doi: 10.1080/00016350500419800. [DOI] [PubMed] [Google Scholar]
- 22.Hienz SA, Paliwal S, Ivanovski S. Mechanisms of Bone Resorption in Periodontitis. J Immunol Res. 2015;2015:615486. doi: 10.1155/2015/615486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Desai K, Desai P, Duseja S, Kumar S, Mahendra J, Duseja S. Significance of maternal periodontal health in preeclampsia. J Int Soc Prev Community Dent. 2015;5:103–107. doi: 10.4103/2231-0762.155734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pozo E, Mesa F, Ikram MH, Puertas A, Torrecillas-Martinez L, Ortega-Oller I, et al. Preterm birth and/or low birth weight are associated with periodontal disease and the increased placental immunohistochemical expression of inflammatory markers. Histol Histopathol. 2016;31:231–7. doi: 10.14670/HH-11-671. [DOI] [PubMed] [Google Scholar]
- 25.de Lima Coutinho Mattera MS, Chiba FY, de Oliveira da Mota MS, Pereira RF, Ervolino E, Neto AH, et al. Maternal periodontitis decreases plasma membrane GLUT4 content in skeletal muscle of adult offspring. Life Sci. 2016 doi: 10.1016/j.lfs.2016.02.010. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Gomes-Filho IS, Pereira EC, Cruz SS, Adan LF, Vianna MI, Passos-Soares JS, et al. Relationship Among Mothers' Glycemic Level, Periodontitis, and Birth Weight. J Periodontol. 2016;87:238–247. doi: 10.1902/jop.2015.150423. [DOI] [PubMed] [Google Scholar]
- 27.Stelmakh V, Slot DE, van der Weijden GA. Self-reported periodontal conditions among Dutch women during pregnancy. Int J Dent Hyg. 2016 doi: 10.1111/idh.12210. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Assery MK. A 22 year comparison survey of dental knowledge in Al-Jubail antenatal clinic population. Saudi Dent J. 2016;28:86–90. doi: 10.1016/j.sdentj.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Musaiger AO, Al-Mannai M, Abduljawad E. Association of oral hygiene habits and food intake with the risk of dental caries among undergraduate university women in Saudi Arabia. Int J Adolesc Med Health. 2014;26:585–589. doi: 10.1515/ijamh-2013-0337. [DOI] [PubMed] [Google Scholar]
- 30.Al-Shehri S. Oral health status of older people in residential homes in Saudi Arabia. Open J Stomatol. 2012;2:307–13. [Google Scholar]
- 31.Al-Jaber A, Da'ar OB. Primary health care centers, extent of challenges and demand for oral health care in Riyadh, Saudi Arabia. BMC Health Serv Res. 2016;16:628. doi: 10.1186/s12913-016-1876-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albarakati SF. Appointments failure among female patients at a dental school clinic in Saudi Arabia. J Dent Educ. 2009;73:1118–24. [PubMed] [Google Scholar]


