Abstract
Background: Mental health and HIV disparities are well documented among sexual minorities, but there is a dearth of research on other chronic conditions. Cardiovascular disease remains the leading cause of death worldwide. Although sexual minorities have high rates of several modifiable risk factors for cardiovascular disease (including stress, tobacco use, and alcohol consumption), there is a paucity of research in this area.
Objectives: In this systematic review, we synthesized and critiqued the existing evidence on cardiovascular disease among sexual minority adults.
Search Methods: We conducted a thorough literature search of 6 electronic databases for studies published between January 1985 and December 2015 that compared cardiovascular disease risk or prevalence between sexual minority and heterosexual adults.
Selection Criteria: We included peer-reviewed English-language studies that compared cardiovascular disease risk or diagnoses between sexual minority and heterosexual individuals older than 18 years. We excluded reviews, case studies, and gray literature. A total of 31 studies met inclusion criteria.
Data Collection and Analysis: At least 2 authors independently abstracted data from each study. We performed quality assessment of retrieved studies using the Crowe Critical Appraisal Tool.
Main Results: Sexual minority women exhibited greater cardiovascular disease risk related to tobacco use, alcohol consumption, illicit drug use, poor mental health, and body mass index, whereas sexual minority men experienced excess risk related to tobacco use, illicit drug use, and poor mental health. We identified several limitations in the extant literature. The majority of included studies were cross-sectional analyses that used self-reported measures of cardiovascular disease. Even though we observed elevated cardiovascular disease risk, we found few differences in cardiovascular disease diagnoses (including hypertension, diabetes, and high cholesterol). Overall, 23 of the 26 studies that examined cardiovascular disease diagnoses used subjective measures. Only 7 studies used a combination of biomarkers and self-report measures to establish cardiovascular disease risk and diagnoses.
Authors’ Conclusions: Social conditions appear to exert a negative effect on cardiovascular disease risk among sexual minorities. Although we found few differences in cardiovascular disease diagnoses, we identified an elevated risk for cardiovascular disease in both sexual minority men and women. There is a need for research that incorporates subjective and objective measures of cardiovascular disease risk.
Public Health Implications: Cardiovascular disease is a major health concern for clinicians, public health practitioners, and policymakers. This systematic review supports the need for culturally appropriate interventions that address cardiovascular disease risk in sexual minority adults.
PLAIN-LANGUAGE SUMMARY
Sexual minorities experience negative health outcomes related to discrimination and marginalization. Therefore, health disparities among sexual minorities are a growing concern for leading health organizations. Cardiovascular disease remains the leading cause of death worldwide, and sexual minorities have higher rates of modifiable risk factors for cardiovascular disease (including stress, tobacco use, and alcohol consumption) than do heterosexuals. However, cardiovascular disease risk among sexual minorities remains understudied. This systematic review examined 31 studies that compared cardiovascular disease risk and diagnoses between sexual minority and heterosexual adults. We observed elevated cardiovascular disease risk for sexual minority women related to tobacco use, alcohol consumption, illicit drug use, poor mental health, and body mass index. Sexual minority men experienced excess cardiovascular disease risk related to tobacco use, illicit drug use, and poor mental health. Study findings were based primarily on subjective measures, with few studies including objective measures (such as biomarkers or physical examination). Overall, more research is needed to elucidate the mechanism by which psychosocial stressors affect cardiovascular disease risk in sexual minorities. However, these findings support the need for interventions to reduce cardiovascular disease risk in sexual minority adults.
Despite increased acceptance and recent gains in civil rights, particularly the Supreme Court’s decision on same-sex marriage,1 sexual minorities face significant discrimination and marginalization in the United States.2 Only 21 states provide protection from discrimination based on sexual orientation.3 Therefore, sexual minorities are vulnerable to discrimination in public accommodations (hospitals, nursing homes, restaurants, police stations, etc.).3 Experiences with stigma4,5 are associated with poor health outcomes,6 decreased life expectancy, and increased mortality among sexual minorities.7 These social conditions and related psychosocial stressors compromise the health of sexual minorities across the life span.
Leading government and health care organizations increasingly recognize health disparities among sexual minorities. In 2011, the Institute of Medicine (IOM) identified several factors that negatively affect the health of sexual minorities, including inadequate training of health care providers, discrimination, harassment, poverty, and lower rates of health insurance coverage.2 Healthy People 2020 added improving the safety, health, and well-being of lesbian, gay, bisexual, and transgender (LGBT) individuals as a new objective.8
Sexual minorities report higher rates of poor mental health,9–11 poor self-rated health,12 disability,13 and suicidal ideation14 than do heterosexuals. Although mental health and HIV/AIDS disparities are well documented among sexual minorities, little is known about disparities in other health conditions.15 The IOM identified the need to address these knowledge gaps regarding sexual minority health,2 including the dearth of research on disparities for chronic diseases such as cardiovascular disease (CVD).16,17
CVD is the leading cause of death worldwide, accounting for 46% of all noncommunicable disease deaths.18 In 2010, 33% of persons in the United States had at least 1 type of CVD, and this figure is expected to increase to 41% by 2030.19 CVD is associated with significant disability, including difficulties in performing activities of daily living, functional limitations, and decreased work productivity.20 The INTERHEART study revealed that 9 modifiable risk factors (hypertension, diabetes, lipids, smoking, alcohol consumption, obesity, diet, physical activity, and psychosocial factors) contribute to more than 90% of the risk of CVD.21
A number of modifiable risk factors for CVD are elevated in sexual minorities. Stress, related to discrimination and marginalization, has a deleterious effect on the health of sexual minorities.15,22 Stress contributes to low-grade nonspecific inflammation linked to chronic disease, including CVD,23 and mental health is associated with CVD morbidity and mortality.24,25 Alcohol, tobacco, and drug use may also be elevated in sexual minorities and may contribute to their higher CVD risk compared with that of heterosexual individuals.26–29 In addition, sexual minority women may have elevated body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), which can increase CVD risk.30–33
Because of the significant morbidity and mortality associated with CVD, it is a major health concern for clinicians, public health practitioners, and policymakers.34 Since there is growing evidence of CVD risk in sexual minorities and most work has focused on sexual minority men living with HIV, the IOM identified CVD research on sexual minorities as an area with an urgent need for further research.2 However, to date, no comprehensive synthesis of CVD in sexual minorities has been conducted. Therefore, we synthesized and critiqued the existing evidence from studies that compared CVD risk factors and CVD diagnoses between sexual minority and heterosexual adults.
METHODS
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Appendix A, available as a supplement to this article at http://www.ajph.org).35 We conducted a thorough literature search of the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, LGBT Life, PsycInfo, PubMed, and Web of Science. Appendix B, available as a supplement to this article at http://www.ajph.org, includes a description of the electronic database search. To identify additional studies, we also performed an ancestry and descendancy search of retrieved studies and of the 2011 IOM report.
Inclusion and Exclusion Criteria
Inclusion criteria were peer-reviewed English-language studies that compared CVD risk or CVD diagnoses between sexual minority and heterosexual individuals older than 18 years. We excluded reviews, case studies, and gray literature. Following the IOM report and previously used definitions,2,36 we defined sexual minority individuals as those who identified as lesbian, gay, or bisexual or reported same-sex attraction or same-sex behavior. Therefore, we excluded studies that used other definitions. We also excluded studies that focused on CVD risk in people living with HIV since most CVD research with sexual minorities has focused on HIV2 and systematic reviews have been conducted on this topic.37
Search Results
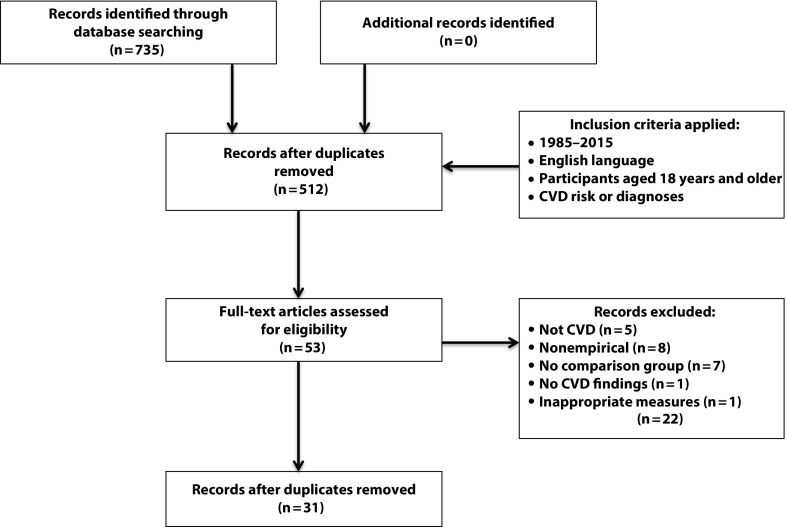
As shown in Figure 1, the initial search retrieved 735 studies. After excluding duplicates and reviewing titles and abstract, we applied inclusion and exclusion criteria. After examining titles and abstracts, we screened 45 studies for full text review, of which 14 did not meet inclusion criteria. We did not retrieve any additional studies through an ancestry and descendancy search. Therefore, the final sample consisted of 31 studies.
FIGURE 1—
Eligibility Criteria for Studies of Cardiovascular Disease (CVD) in Sexual Minorities Published Between January 1985 and December 2015
Data Abstraction
We performed data abstraction for a critical examination of data sources; this consisted of the following steps: data reduction, data display, data comparison, conclusion drawing, and verification.38 To facilitate comparisons, we organized the findings into matrices. From May 2015 and December 2015, the lead author (B. A. C.) abstracted data into evidence tables. In February 2016, at least 1 of 4 additional authors (R. E. L., J. E. P., P. M., and E. M. S.) then independently reviewed data abstraction for each study to ensure accuracy. There was only 1 data abstraction disagreement, which was resolved through discussion among all authors until group consensus was achieved. Detailed tables with study characteristics (Appendix C) and summary of findings (Appendix D) are available as supplements to this article at http://www.ajph.org.
Quality Assessment
We appraised the quality of included studies using the Crowe Critical Appraisal Tool (CCAT), which is valid and reliable in assessing methodological rigor.39 The CCAT is divided into 8 equally weighted categories scored on a Likert scale from 0 to 5 for a total possible score of 40, which represents the highest quality. Each study was appraised by at least 2 authors, and a third author was consulted to resolve any disagreements. In addition, we performed an evaluation of the statistical analyses conducted in each study, with an emphasis on statistical tests used, power, missing data, and correction for multiple tests. The quality appraisal, including the evaluation of statistical analyses, is available as a supplement to this article at http://www.ajph.org (Appendix E).
RESULTS
Table 1 provides details of study characteristics. The review included 31 studies, of which 30 were secondary analyses of existing data sources. Overall, 28 studies were conducted in the United States, 2 in Canada,57,58 and 1 in Switzerland.60 As determined by the CCAT, the quality of these studies ranged from 30 to 40, indicating moderate to high quality (Table 1). Table 2 presents a summary of findings related to CVD risk factors and CVD diagnoses.
TABLE 1—
Characteristics of Studies of Cardiovascular Disease in Sexual Minorities Published Between January 1985 and December 2015
| Authors | Data Source | % Sexual Minority | Location | Quality Score |
| Roberts et al.40 | • Not applicable | 50 | California | 31/40 |
| Clark et al.41 | • The Longitudinal Study of Adolescent to Adult Health (Add Health), 2008–2009 | 3.7 | US | 36/40 |
| Hatzenbuehler et al.42 | 4.2 | 38/40 | ||
| Strutz et al.43 | 23.7 | 39/40 | ||
| Everett & Mollborn44 | • Add Health, 2007–2008 | 13.6 | 37/40 | |
| Hatzenbuehler et al.45 | • Add Health, 1994–2009 | 4.4 | 37/40 | |
| Blosnich et al.46 | • Behavioral Risk Factor Surveillance System (BRFSS), 2010 | 2.1 | Multistate (10 states) | 35/40 |
| Blosnich & Silenzio47 | • BRFSS, 2010 | 2.0 | 35/40 | |
| Farmer et al.48 | • BRFSS, 2010 | 2.0 | 37/40 | |
| Conron et al.49 | • BRFSS, 2001–2008 | 3.4 | Massachusetts | 36/40 |
| Dilley et al.50 | • BRFSS, 2003–2006 | 2.4 | Washington | 37/40 |
| Fredriksen-Goldsen et al.51 | • BRFSS, 2003–2010 | 1.6 | 37/40 | |
| Garland-Forshee et al.52 | • BRFSS, 2003–2010 | 2.5 | Oregon | 36/40 |
| Matthews & Lee53 | • BRFSS, 2011 | 1.6 | North Carolina | 34/40 |
| Boehmer et al.54 | • California Health Interview Survey (CHIS), 2001–2005 | 3.4 | California | 35/40 |
| Wallace et al.55 | • CHIS, 2003–2007 | Not reported | 30/40 | |
| Cochran & Mays56 | • California Quality of Life Study, 2004–2005 | 9.9 | California | 35/40 |
| Steele et al.57 | • Canadian Community Health Survey 2.1, 2003 | 1.3 | Canada | 38/40 |
| Veenstra58 | 1.4 | 35/40 | ||
| Andersen et al.59 | • Chicago Health and Life Experiences of Women, 2001–2002 | 44.9 | Chicago, IL | 36/40 |
| • Comparison: National Study of Health and Life Experiences of Women, 2001 | United States | |||
| Wang et al.60 | • Geneva Gay Men’s Health Survey, 2002 | 50 | Switzerland | 33/40 |
| • Comparison: Swiss Health Survey | ||||
| Diamant & Wold61 | • Los Angeles County Health Survey, 1999 | 2.7 | Los Angeles, CA | 35/40 |
| Diamant et al.62 | • Los Angeles County Health Survey, 1997 | 1.9 | 36/40 | |
| Mays et al.63 | • Lesbian Health Survey, 1999–2001 | 22.5 | 33/40 | |
| • Comparison: Los Angeles County Health Survey, 1999–2000 | ||||
| Swartz64 | • Internet: survey of men who have sex with men in Chicago, 2007–2011 | 50 | Chicago, IL | 34/40 |
| • Comparison: National Survey on Drug Use and Health (NSDUH), 2008–2012 | United States | |||
| Blosnich et al.65 | • National College Health Assessment | 8.4 | United States | 37/40 |
| Farmer et al.66 | • National Health and Nutrition Examination Survey, 2001–2010 | 5.2 | United States | 37/40 |
| Farmer et al.67 | • National Health and Nutrition Examination Survey, 2001–2008 | 7.5 | United States | 37/40 |
| Ward et al.68 | • National Health Interview Survey | 2.3 | United States | 34/40 |
| Case et al.69 | • Nurses’ Health Study, 1993–1995 | 1.1 | United States | 37/40 |
| Valanis et al.70 | • Women’s Health Survey, 2008–2012 | 1.4 | United States | 35/40 |
TABLE 2—
Summary of Findings of Studies of Cardiovascular Disease in Sexual Minorities Published Between January 1985 and December 2015
| No. of Studies (n = 31) |
|||||||||
| Direction of Association | Tobacco Use | Alcohol Consumption | Illicit Drug Use | Psychosocial Factors | Obesity/ Overweight/BMI | CVD | HTN | DM | High Cholesterol |
| Mena | |||||||||
| Higher | |||||||||
| SMM | 7 | 2 | 1 | 8 | . . . | . . . | 3 | 1 | . . . |
| GM only | 1 | 1 | 3 | 1 | . . . | . . . | 2 | 1 | 1 |
| BM only | 1 | 1 | . . . | 1 | . . . | . . . | 2 | 1 | . . . |
| Lower | |||||||||
| SMM | . . . | . . . | . . . | . . . | 6 | 1 | . . . | 1 | . . . |
| GM only | . . . | . . . | . . . | . . . | 4 | . . . | . . . | . . . | . . . |
| BM only | . . . | . . . | . . . | . . . | . . . | . . . | 1 | . . . | . . . |
| Not significant | |||||||||
| SMM | 6 | 11 | 1 | 3 | 5 | 7 | 9 | 12 | 6 |
| Total | 15 | 15 | 5 | 13 | 15 | 8 | 17c | 16c | 7c |
| Womenb | |||||||||
| Higher | |||||||||
| SMW | 19 | 13 | 3 | 12 | 8 | 2 | . . . | . . . | . . . |
| LW only | . . . | . . . | . . . | 1 | 3 | . . . | 1 | . . . | . . . |
| BW only | 1 | 2 | . . . | 3 | . . . | . . . | 5 | 2 | . . . |
| Lower | |||||||||
| SMW | . . . | . . . | . . . | . . . | 1 | . . . | 2 | 1 | 1 |
| LW only | 1 | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . |
| BW only | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . |
| Not significant | |||||||||
| SMW | 1 | 3 | . . . | 3 | 8 | 10 | 14 | 14 | 6 |
| Total | 22 | 18 | 3 | 19 | 20 | 12 | 22c | 17c | 7c |
Note. BM = bisexual men; BMI = body mass index; BW = bisexual women; CVD = cardiovascular disease; DM = diabetes mellitus; GM = gay men; HTN = hypertension; LW = lesbian women; SMM = sexual minority men; SMW = sexual minority women. Of the 31 studies, 22 included men and 28 included women; 9 studies included only women and 3 included only men.
Heterosexual men = reference group.
Heterosexual women = reference group.
Includes medication use and screening.
Tobacco Use
Compared with heterosexual men, sexual minority men had significantly higher rates of tobacco use in 9 of 15 studies that measured this CVD risk factor (Table 2).46–51,60 Data from the Behavioral Risk Factor Surveillance System (BRFSS) revealed that bisexual men, but not gay men, were nearly twice as likely to smoke than were heterosexual men.52 In 20 of 22 studies, sexual minority women had significantly higher rates of tobacco use than did heterosexual women (Table 2). Although current tobacco use was lower among sexual minority women older than 40 years in 2 studies that used convenience sampling,63,70 lifetime smoking was higher. This indicates that tobacco use patterns may change across the life span for sexual minority women.
Moreover, 4 studies examined tobacco use differences based on race/ethnicity,63 type of residence,48 and veteran status.46,47 Among sexual minority women, only Latinas reported significantly higher rates of tobacco use than did their heterosexual peers. Although Black and Asian sexual minority women also reported higher rates of tobacco use than did heterosexual women of the same race, these differences were not statistically significant.63 Sexual minorities living in nonrural areas also reported significantly higher rates of tobacco use than did their heterosexual counterparts, but no differences were observed in rural areas.48 Among sexual minorities with military experience, there was significantly higher tobacco use, but these differences disappeared in multivariate analyses.47 On the contrary, in a different study, sexual minorities with no military experience reported higher rates of smoking compared with heterosexual participants, whereas those with military experience were similar to their heterosexual counterparts.65
Alcohol Consumption
Few differences were found across 15 studies that examined alcohol differences among men. However, sexual minority men older than 50 years were more likely to report excessive drinking than were older heterosexual men.51 Alcohol consumption was higher among sexual minority women in 15 of 18 studies that measured this CVD risk factor (Table 2).42,45,46,48,50,51,57,59,62,63,66,69,70 Higher rates of binge drinking were identified among bisexual women in 2 studies.44,49 Findings for alcohol use echo results for tobacco use, with only Latina sexual minority women reporting significantly higher alcohol use than did heterosexual women of the same race/ethnicity.63 Trends in alcohol use were also similar to those of tobacco use, with nonrural sexual minority women reporting greater alcohol use.48
Illicit Drug Use
Sexual minorities reported significantly greater drug use in 6 studies.35,40,50,65 An additional study reported significantly greater drug use among all sexual minorities, except bisexual men.49 The sample of bisexual men was small compared with other groups and therefore may have decreased the ability to detect significant differences. Only in 1 study did sexual minority men report lower illicit drug use than did their heterosexual peers.64
Psychosocial Factors
Psychosocial factors, including stress, are associated with CVD risk.21 Sexual minority men exhibited worse mental health outcomes in 10 of 13 studies. Of the 5 analyses that included depression or depressive symptoms, 4 demonstrated higher rates among sexual minority men in the United States.65,43,53,54 Only in 1 study, conducted in Switzerland, was there no significant difference in depression between sexual minority men and heterosexual men.60 Although stress is proposed as a factor that contributes to health disparities in sexual minorities,15,22 only 5 studies included measures of stress for men.46,48,55,56,64 Sexual minority men reported greater stress in all of these studies except 1.64 Compared with heterosexual men, sexual minority men had significantly worse mental health in 3 additional studies.50,51,53
Furthermore, poor mental health was more prevalent among sexual minority women in 16 of 19 studies. Sexual minority women reported significantly higher rates of depression in 4 studies.65,43,53,54 Bisexual women, but not lesbian women, had higher rates of depression in an additional 3 studies.59,69,70 In terms of stress, sexual minority women had elevated stress in 4 studies45,48,55,56; however, bisexual women in 1 study reported greater stress than did both lesbian and heterosexual women.46 Overall, bisexual women were more likely than lesbian women to report worse mental health throughout the included studies.
Anthropometric Measures
Sexual minority men were less likely to be overweight or obese in 10 of 15 studies that examined these variables.46–51,60 However, of the 20 studies that examined overweight, obesity, or BMI, a total of 11 found elevations among sexual minority women (Table 2). Sexual minority women also had higher waist–hip ratios and weight cycling, which are both CVD risk factors,71 compared with heterosexual women.40,69 These findings were based on self-reported data and convenience sampling, which may have biased results. Moreover, Latina and Black sexual minority women exhibited higher rates of obesity than did their heterosexual peers.63
Physical Activity and Diet
Insufficient physical activity and poor dietary habits significantly increase CVD risk.21 However, these risk factors were infrequently measured, with physical activity found in 11 studies and diet in only 4 (Appendix E). Few sexual orientation differences were found for physical activity and diet, but definitions varied widely across studies.
Cardiovascular Diseases
Detailed findings related to CVD diagnoses are available in Appendix D. CVD diagnoses remain less studied than do CVD risk factors. There were few sexual orientation differences in CVD prevalence, which might be explained by data collection methods. A total of 23 of 26 studies that assessed CVD diagnoses included self-report measures only.41,43,46,47,49–64,68–70 Sexual minority women reported elevated CVD in 3 studies.51,54,61 Only gay men younger than 40 years reported increased CVD in an additional study.54 The remaining studies found no significant differences in CVD.
Several studies examined CVD risk. In 2 studies, sexual minority men had higher risk for CVD,41,66 as indicated by increased diastolic blood pressure, heart rate, and C-reactive protein (a measure of acute inflammation).42 Similarly, elevations in CVD biomarkers were observed in sexual minority men who reported at least 2 stressful life events.45 Notably, although stressful life events increased CVD risk in sexual minority young adults, this was not observed for heterosexuals,45 indicating that sexual minorities may experience differential health outcomes as a result of stressful life events. In addition, in a secondary analysis of the National Health and Nutrition Examination Survey (NHANES), bisexual men had an increased risk of CVD that was unexplained by behaviors and demographic characteristics.67
Likewise, composite scores of biomarkers indicated that there was a higher risk of CVD in young sexual minority women (aged 24–34 years).41,45 These findings contradict another study in which CVD biomarkers were analyzed individually instead of using a composite score.42 The method used to analyze biomarkers may have contributed to these discrepancies.
Hypertension
Of the 17 studies that assessed hypertension in men, only 4 used direct blood pressure measurement.41,43,44,67 Gay men in 2 studies were approximately twice as likely to have hypertension than were heterosexual men.44,64 Overall, 3 studies found elevated rates of hypertension in sexual minority men,44,55,64 whereas only gay men had increased hypertension in an additional study.41 Gay men in a study conducted in Switzerland denied having a history of hypertension but reported being told they had elevated blood pressure upon examination by a health care provider, which may suggest higher levels of prehypertension.60 Bisexual men were more likely to report taking blood pressure medication in 2 of 3 studies that examined this variable.54,67 Moreover, results were conflicting in the 22 studies that examined hypertension among women. Lesbian women in only 1 study were more likely to report hypertension.59 In another study, only lesbian women older than 40 reported greater hypertension than heterosexual women.54 Overall, bisexual women reported higher rates of hypertension in 4 studies50,57,58,69 and greater use of blood pressure medication in 1 study.41
Diabetes
Few studies found differences in diabetes based on sexual orientation. However, sexual minority men in 3 of 16 studies reported higher rates of diabetes than heterosexual men.55,60,67 Among women, bisexual women were more likely to report a history of diabetes in 2 studies.50,62
High Cholesterol
Nine studies examined differences in cholesterol. Sexual minority men reported higher cholesterol than did heterosexuals in only 1 study.60 Similarly, sexual minority women had significantly lower total cholesterol than did heterosexual women in 1 study.66 The remaining studies found no significant sexual orientation differences in cholesterol.
DISCUSSION
These findings support prior evidence of elevated CVD risk factors in sexual minority adults, but we observed few differences in CVD diagnoses. Sexual minority women demonstrated increased rates of tobacco use, alcohol consumption, illicit drug use, poor mental health, and elevated BMI. Sexual minority men demonstrated CVD risk related to tobacco use, illicit drug use, and poor mental health. Results must be considered within the context of identified sampling, methodological, and measurement limitations.
Several of the included studies have limited generalizability. Only 1 study examined racial/ethnic differences in CVD. CVD risk differed across racial/ethnic groups, with Latina and Black sexual minority women experiencing greater CVD risk than did heterosexual women of the same race.63 Sexual minorities were younger and more likely to be White compared with heterosexuals. As data for sexual minority young adults are more readily available in population-based surveys, there was an abundance of younger participants throughout these studies. The health of older adults, who are at increased risk for CVD,72 must be further explored, as only 4 studies focused on older sexual minorities.40,51,55,70 Next, although health outcomes for sexual minorities have been shown to differ significantly on the basis of geographic location,7 few studies evaluated CVD differences based on state or type of residence (urban, suburban, or rural). It appears that nonrural sexual minority individuals experience greater CVD risk than do their heterosexual peers. In addition, we identified only 2 studies that focused on CVD risk in military veterans.47,65 Therefore, sampling frames used by population-based surveys may not adequately capture certain subgroups of sexual minorities, including racial/ethnic minorities, older adults, rural individuals, and military veterans.
We identified a number of methodological limitations. As shown in Table 1, 8 studies were based on data from the BRFSS, 5 from the National Longitudinal Study of Adolescent to Adult Health (Add Health), 3 from the Los Angeles County Health Survey, 2 from the NHANES, 2 from the California Health Interview Survey, and 2 from the Canadian Community Health Survey. This overlap of data sources may have produced skewed findings related to CVD risk. However, data collection years and measures differed across studies despite the overlap of data sources. Furthermore, results may be biased by data collection methods. The small number of sexual minorities identified may have been affected by social desirability bias. Participants may be more likely to disclose their sexual identity with computer-assisted self-interviewing (CASI) methods,73 but more than half of the studies in this review used face-to-face or computer-assisted telephone interviewing (CATI). Data collected with CATI produced lower numbers of sexual minorities. These methods are more susceptible to bias related to interviewer characteristics and may contribute to underreporting of sensitive topics.74 Most researchers used cross-sectional data at the state level. Given that there are regional differences in discrimination laws and acceptance of sexual minorities, significant variation in exposure to stressful experiences may exist.7 There is also a need for longitudinal studies of CVD in sexual minority individuals, as only 1 study in this systematic review analyzed longitudinal data.45 Our evaluation of statistical analyses conducted in the included studies revealed that, although most used appropriate statistical tests, few researchers reported performing a power analysis or correction for multiple tests, and listwise deletion was the preferred method for handling missing data. These limitations and their implications are discussed in detail in Appendix C.
A concern identified by Healthy People 2020 is whether sexual orientation is measured appropriately in population-based surveys.8 Whether 1 or a combination of measures should be used for assessing sexual orientation is inconclusive.75 In fact, only 4 studies used a combination of sexual orientation measures.43,54,66,67 Bias in measuring sexual orientation may produce inaccurate estimates of sexual minorities, which might explain the low number of sexual minority participants compared with previous national estimates.76 In addition, several studies aggregated data for homosexual and bisexual participants by gender, which might obscure differences between sexual minority subgroups. Since 30 of 31 studies in this review were secondary data analyses, there was inconsistency in variables used. Confounding should be considered, since some CVD risk factors (stress, physical activity, and diet) were infrequently measured, which limited comparisons across studies. In addition, CVD was mostly based on self-reported data. Only 7 studies, representing 2 data sources (Add Health and NHANES), combined biomarkers, physical examination, and self-reported data, but few CVD differences by sexual orientation were identified. CVD risk assessment may be more accurate when biomarkers and self-reported data are both collected; therefore, there is a need for the use of objective measures when evaluating CVD risk in sexual minorities. Moreover, stress is a hypothesized contributor to health disparities among sexual minority individuals.15 Thus, it is not surprising that the minority stress model was the preferred explanation for these disparities, yet few studies included any measures of stress.
Implications
Future research.
Future studies should address how intersectionality affects the health of sexual minorities. The IOM recommended several frameworks to guide health research with sexual minorities; however, theoretical frameworks were used in only 3 studies.44,45,58 Furthermore, as sexual minorities exhibited higher levels of stress, future research should examine the association between stress and CVD risk. Of the 31 studies included in this systematic review, only 8 focused exclusively on CVD. More studies are needed that focus on CVD and measure relevant risk factors and demographic characteristics related to CVD risk. Lastly, despite evidence of increased CVD risk, few interventions have been developed to address CVD risk in this population.77,78 The studies identified were descriptive. Therefore, there is a need for culturally tailored interventions to reduce CVD risk in sexual minorities.
Policy.
Population-based surveys should include sexual orientation as a demographic variable. Similarly, the inclusion of sexual orientation in electronic health records (EHRs) is an important policy for increasing the availability of clinical data such as biomarkers and clinical diagnoses. No studies in this review used EHR data. The inclusion of sexual orientation in EHRs may help increase understanding of disparities and health care utilization among sexual minorities.2
Practice.
Clinicians generally lack the knowledge and skills to appropriately address the health needs of sexual minorities.79,80 As sexual orientation is integrated into EHRs, clinicians should be educated on how sexual orientation may affect CVD risk. Although several public health programs focus on populations at excessive risk for CVD, such as racial/ethnic minority and low-income individuals,34 there is a dearth of work focused on sexual minorities. Clinicians and public health practitioners should develop health promotion strategies to address modifiable risk factors that contribute to CVD risk in sexual minorities.
Conclusions
This systematic review supports the findings of the IOM report on sexual minority health. Social conditions appear to exert a negative effect on the health of sexual minorities. Although we found few differences in CVD diagnoses, we did identify an elevated risk for CVD among sexual minority men and women. Sexual minority men experienced excess CVD risk related to tobacco use, illicit drug use, and poor mental health. Sexual minority women exhibited the greatest CVD risk related to tobacco use, alcohol consumption, illicit drug use, poor mental health, and elevated BMI. This review provides evidence that supports the need to target CVD risk in sexual minorities, particularly sexual minority women. These data indicate that clinicians and public health practitioners should develop primary and secondary prevention interventions that reduce CVD risk in sexual minorities.
ACKNOWLEDGMENTS
B. A. Caceres was supported in part by the NYU CTSA grant UL1 TR000038 from the National Center for Advancing Translational Sciences, National Institutes of Health.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary for this study because no human participants were involved.
Footnotes
See also Cochran and Mays, p. 497.
REFERENCES
- 1.Human Rights Campaign. Marriage Center. 2015. Available at: http://www.hrc.org/campaigns/marriage-center. Accessed January 25, 2016.
- 2.Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 3.Services & Advocacy for Gay, Lesbian, Bisexual, and Transgender Elders. Welcome home: improving housing security for LGBT older adults. 2015. Available at: http://www.sageusa.org/files/SAGEHousingStrtgy_Brief_web.pdf. Accessed January 12, 2017.
- 4.Herek GM. Hate crimes and stigma-related experiences among sexual minority adults in the United States: prevalence estimates from a national probability sample. J Interpers Violence. 2009;24(1):54–74. doi: 10.1177/0886260508316477. [DOI] [PubMed] [Google Scholar]
- 5.Lewis RJ, Kholodkov T, Derlega VJ. Still stressful after all these years: a review of lesbians’ and bisexual women’s minority stress. J Lesbian Stud. 2012;16(1):30–44. doi: 10.1080/10894160.2011.557641. [DOI] [PubMed] [Google Scholar]
- 6.Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995;36(1):38–56. [PubMed] [Google Scholar]
- 7.Hatzenbuehler ML, Bellatorre A, Lee Y, Finch BK, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Soc Sci Med. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US Dept of Health and Human Services. Lesbian, gay, bisexual, and transgender health. 2014. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. Accessed January 12, 2017.
- 9.American Psychological Association. Stress in America: the impact of discrimination. 2016. Available at: http://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf. Accessed January 12, 2017.
- 10.Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. J Consult Clin Psychol. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: results from a prospective study of bereaved gay men. Health Psychol. 2008;27(4):455–462. doi: 10.1037/0278-6133.27.4.455. [DOI] [PubMed] [Google Scholar]
- 12.Frost DM, Lehavot K, Meyer IH. Minority stress and physical health among sexual minority individuals. J Behav Med. 2015;38(1):1–8. doi: 10.1007/s10865-013-9523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fredriksen-Goldsen KI, Kim H-J, Barkan SE. Disability among lesbian, gay, and bisexual adults: disparities in prevalence and risk. Am J Public Health. 2012;102(1):e16–e21. doi: 10.2105/AJPH.2011.300379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer IH, Dietrich J, Schwartz S. Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. Am J Public Health. 2008;98(6):1004–1006. doi: 10.2105/AJPH.2006.096826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci. 2013;8(5):521–548. doi: 10.1177/1745691613497965. [DOI] [PubMed] [Google Scholar]
- 16.Coulter RWS, Kenst KS, Bowen DJ. Research funded by the National Institutes of Health on the health of lesbian, gay, bisexual, and transgender populations. Am J Public Health. 2014;104(2):e105–e112. doi: 10.2105/AJPH.2013.301501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boehmer U. Twenty years of public health research: inclusion of lesbian, gay, bisexual, and transgender populations. Am J Public Health. 2002;92(7):1125–1130. doi: 10.2105/ajph.92.7.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Global status report on noncommunicable diseases. 2014. Available at: http://www.who.int/nmh/publications/ncd-status-report-2014/en. Accessed January 12, 2017.
- 19.Heidenreich PA, Albert NM, Allen LA et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mozaffarian D, Benjamin EJ, Go AS et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. 2015. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 21.Yusuf S, Hawken S, Ôunpuu S et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case–control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 22.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen S, Janicki-Deverts D, Doyle WJ et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A. 2012;109(16):5995–5999. doi: 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mavaddat N, Parker RA, Sanderson S, Mant J, Kinmonth AL. Relationship of self-rated health with fatal and non-fatal outcomes in cardiovascular disease: a systematic review and meta-analysis. PLoS One. 2014;9(7):e103509. doi: 10.1371/journal.pone.0103509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ul-Haq Z, Mackay DF, Pell JP. Association between self-reported general and mental health and adverse outcomes: a retrospective cohort study of 19,625 Scottish adults. PLoS One. 2014;9(4):e93857. doi: 10.1371/journal.pone.0093857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bloomfield K, Wicki M, Wilsnack S, Hughes T, Gmel G. International differences in alcohol use according to sexual orientation. Subst Abus. 2011;32(4):210–219. doi: 10.1080/08897077.2011.598404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blosnich J, Lee JGL, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. doi: 10.1136/tobaccocontrol-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am J Public Health. 2010;100(10):1946–1952. doi: 10.2105/AJPH.2009.163147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hughes TL, Szalacha LA, Johnson TP, Kinnison KE, Wilsnack SC, Cho Y. Sexual victimization and hazardous drinking among heterosexual and sexual minority women. Addict Behav. 2010;35(12):1152–1156. doi: 10.1016/j.addbeh.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boehmer U, Bowen DJ, Bauer GR. Overweight and obesity in sexual-minority women: evidence from population-based data. Am J Public Health. 2007;97(6):1134–1140. doi: 10.2105/AJPH.2006.088419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boehmer U, Bowen DJ. Examining factors linked to overweight and obesity in women of different sexual orientations. Prev Med. 2009;48(4):357–361. doi: 10.1016/j.ypmed.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Struble CB, Lindley LL, Montgomery K, Hardin J, Burcin M. Overweight and obesity in lesbian and bisexual college women. J Am Coll Health. 2010;59(1):51–56. doi: 10.1080/07448481.2010.483703. [DOI] [PubMed] [Google Scholar]
- 33.Bowen DJ, Balsam KF, Ender SR. A review of obesity issues in sexual minority women. Obesity (Silver Spring) 2008;16(2):221–228. doi: 10.1038/oby.2007.34. [DOI] [PubMed] [Google Scholar]
- 34.National Forum for Heart Disease & Stroke Prevention. The public health action plan to prevent heart disease and stroke: ten-year update. 2014. Available at: http://www.nationalforum.org/content/public-health-action-plan-prevent-heart-disease-and-stroke. Accessed January 12, 2017.
- 35.Moher D, Shamseer L, Clarke M et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sell RL. Defining and measuring sexual orientation: a review. Arch Sex Behav. 1997;26(6):643–658. doi: 10.1023/a:1024528427013. [DOI] [PubMed] [Google Scholar]
- 37.Bavinger C, Bendavid E, Niehaus K et al. Risk of cardiovascular disease from antiretroviral therapy for HIV: a systematic review. PLoS One. 2013;8(3):e59551. doi: 10.1371/journal.pone.0059551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garrard J. Health Sciences Literature Review Made Easy: The Matrix Method. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2013. [Google Scholar]
- 39.Crowe M, Sheppard L, Campbell A. Comparison of the effects of using the Crowe critical appraisal tool versus informal appraisal in assessing health research: a randomised trial. Int J Evid-Based Healthc. 2011;9(4):444–449. doi: 10.1111/j.1744-1609.2011.00237.x. [DOI] [PubMed] [Google Scholar]
- 40.Roberts SA, Dibble SL, Nussey B, Casey K. Cardiovascular disease risk in lesbian women. Womens Health Issues. 2003;13(4):167–174. doi: 10.1016/s1049-3867(03)00041-0. [DOI] [PubMed] [Google Scholar]
- 41.Clark CJ, Borowsky IW, Salisbury J et al. Disparities in long-term cardiovascular disease risk by sexual identity: The National Longitudinal Study of Adolescent to Adult Health. Prev Med. 2015;76:26–30. doi: 10.1016/j.ypmed.2015.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hatzenbuehler ML, McLaughlin KA, Slopen N. Sexual orientation disparities in cardiovascular biomarkers among young adults. Am J Prev Med. 2013;44(6):612–621. doi: 10.1016/j.amepre.2013.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Strutz KL, Herring AH, Tucker Halpern C. Health disparities among young adult sexual minorities in the US. Am J Prev Med. 2015;48(1):76–88. doi: 10.1016/j.amepre.2014.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Everett B, Mollborn S. Differences in hypertension by sexual orientation among US young adults. J Community Health. 2013;38(3):588–596. doi: 10.1007/s10900-013-9655-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hatzenbuehler ML, Slopen N, McLaughlin KA. Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States [erratum in Health Psychol. 2016;35(2):166] Health Psychol. 2014;33(10):1185–1194. doi: 10.1037/hea0000126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blosnich JR, Farmer GW, Lee JGL, Silenzio VMB, Bowen DJ. Health inequalities among sexual minority adults: evidence from ten US states, 2010. Am J Prev Med. 2014;46(4):337–349. doi: 10.1016/j.amepre.2013.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blosnich JR, Silenzio VM. Physical health indicators among lesbian, gay, and bisexual US veterans. Ann Epidemiol. 2013;23(7):448–451. doi: 10.1016/j.annepidem.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farmer GW, Blosnich JR, Jabson JM, Matthews DD. Gay acres: sexual orientation differences in health indicators among rural and nonrural individuals. J Rural Health. 2016;32(3):321–331. doi: 10.1111/jrh.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–1960. doi: 10.2105/AJPH.2009.174169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dilley JA, Wynkoop Simmons K, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific Northwest. Am J Public Health. 2010;100(3):460–467. doi: 10.2105/AJPH.2007.130336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–1809. doi: 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Garland-Forshee RY, Fiala SC, Ngo DL, Moseley K. Sexual orientation and sex differences in adult chronic conditions, health risk factors, and protective health practices, Oregon, 2005–2008. Prev Chronic Dis. 2014;11:E136. doi: 10.5888/pcd11.140126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Matthews DD, Lee JGL. A profile of North Carolina lesbian, gay, and bisexual health disparities, 2011. Am J Public Health. 2014;104(6):e98–e105. doi: 10.2105/AJPH.2013.301751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Boehmer U, Miao X, Linkletter C, Clark MA. Health conditions in younger, middle, and older ages: are there differences by sexual orientation? LGBT Health. 2014;1(3):168–176. doi: 10.1089/lgbt.2013.0033. [DOI] [PubMed] [Google Scholar]
- 55.Wallace SP, Cochran SD, Durazo EM, Ford CL. The health of aging lesbian, gay & bisexual adults in California. Policy Brief UCLA Cent Health Policy Res. 2011;(PB2011-2):1–8. [PMC free article] [PubMed] [Google Scholar]
- 56.Cochran SD, Mays VM. Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexual individuals: results from the California Quality of Life Survey. Am J Public Health. 2007;97(11):2048–2055. doi: 10.2105/AJPH.2006.087254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Steele LS, Ross LE, Dobinson C, Veldhuizen S, Tinmouth JM. Women’s sexual orientation and health: results from a Canadian population-based survey. Women Health. 2009;49(5):353–367. doi: 10.1080/03630240903238685. [DOI] [PubMed] [Google Scholar]
- 58.Veenstra G. Race, gender, class, sexuality (RGCS) and hypertension. Soc Sci Med. 2013;89:16–24. doi: 10.1016/j.socscimed.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 59.Andersen JP, Hughes TL, Zou C, Wilsnack SC. Lifetime victimization and physical health outcomes among lesbian and heterosexual women. PLoS One. 2014;9(7):e101939. doi: 10.1371/journal.pone.0101939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang J, Häusermann M, Vounatsou P, Aggleton P, Weiss MG. Health status, behavior, and care utilization in the Geneva Gay Men’s Health Survey. Prev Med. 2007;44(1):70–75. doi: 10.1016/j.ypmed.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 61.Diamant AL, Wold C. Sexual orientation and variation in physical and mental health status among women. J Womens Health (Larchmt) 2003;12(1):41–49. doi: 10.1089/154099903321154130. [DOI] [PubMed] [Google Scholar]
- 62.Diamant AL, Wold C, Spritzer K, Gelberg L. Health behaviors, health status, and access to and use of health care: a population-based study of lesbian, bisexual, and heterosexual women. Arch Fam Med. 2000;9(10):1043–1051. doi: 10.1001/archfami.9.10.1043. [DOI] [PubMed] [Google Scholar]
- 63.Mays VM, Yancey AK, Cochran SD, Weber M, Fielding JE. Heterogeneity of health disparities among African American, Hispanic, and Asian American women: unrecognized influences of sexual orientation. Am J Public Health. 2002;92(4):632–639. doi: 10.2105/ajph.92.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Swartz JA. The relative odds of lifetime health conditions and infectious diseases among men who have sex with men compared with a matched general population sample. Am J Mens Health. 2015;9(2):150–162. doi: 10.1177/1557988314533379. [DOI] [PubMed] [Google Scholar]
- 65.Blosnich JR, Gordon AJ, Fine MJ. Associations of sexual and gender minority status with health indicators, health risk factors, and social stressors in a national sample of young adults with military experience. Ann Epidemiol. 2015;25(9):661–667. doi: 10.1016/j.annepidem.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 66.Farmer GW, Jabson JM, Bucholz KK, Bowen DJ. A population-based study of cardiovascular disease risk in sexual-minority women. Am J Public Health. 2013;103(10):1845–1850. doi: 10.2105/AJPH.2013.301258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Farmer GW, Bucholz KK, Flick LH, Burroughs TE, Bowen DJ. CVD risk among men participating in the National Health and Nutrition Examination Survey (NHANES) from 2001 to 2010: differences by sexual minority status. J Epidemiol Community Health. 2013;67(9):772–778. doi: 10.1136/jech-2013-202658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ward BW, Joestl SS, Galinsky AM, Dahlhamer JM. Selected diagnosed chronic conditions by sexual orientation: a national study of US Adults, 2013. Prev Chronic Dis. 2015;12:E192. doi: 10.5888/pcd12.150292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Case P, Austin SB, Hunter DJ et al. Sexual orientation, health risk factors, and physical functioning in the Nurses’ Health Study II. J Womens Health (Larchmt) 2004;13(9):1033–1047. doi: 10.1089/jwh.2004.13.1033. [DOI] [PubMed] [Google Scholar]
- 70.Valanis BG, Bowen DJ, Bassford T, Whitlock E, Charney P, Carter RA. Sexual orientation and health: comparisons in the Women’s Health Initiative sample. Arch Fam Med. 2000;9(9):843–853. doi: 10.1001/archfami.9.9.843. [DOI] [PubMed] [Google Scholar]
- 71.Myint PK, Kwok CS, Luben RN, Wareham NJ, Khaw K-T. Body fat percentage, body mass index and waist-to-hip ratio as predictors of mortality and cardiovascular disease. Heart. 2014;100(20):1613–1619. doi: 10.1136/heartjnl-2014-305816. [DOI] [PubMed] [Google Scholar]
- 72.Mozaffarian D, Benjamin EJ, Go AS et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 73.Gribble JN, Miller HG, Rogers SM, Turner CF. Interview mode and measurement of sexual behaviors: methodological issues. J Sex Res. 1999;36(1):16–24. doi: 10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–2047. [Google Scholar]
- 75.Cahill S, Makadon H. Sexual orientation and gender identity data collection in clinical settings and in electronic health records. LGBT Health. 2014;1(1):34–41. doi: 10.1089/lgbt.2013.0001. [DOI] [PubMed] [Google Scholar]
- 76.Gates GJ. How many people are lesbian, gay, bisexual, and transgender? 2011. Available at: http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Accessed January 12, 2017.
- 77.Fallin A, Lee YO, Bennett K, Goodin A. Smoking cessation awareness and utilization among lesbian, gay, bisexual, and transgender adults: an analysis of the 2009–2010 National Adult Tobacco Survey. Nicotine Tob Res. 2016;18(4):496–500. doi: 10.1093/ntr/ntv103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol. 2015;83(5):875–889. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carabez R, Pellegrini M, Mankovitz A, Eliason M, Ciano M, Scott M. “Never in all my years…”: nurses’ education about LGBT health. J Prof Nurs. 2015;31(4):323–329. doi: 10.1016/j.profnurs.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 80.Obedin-Maliver J, Goldsmith ES, Stewart L et al. Lesbian, gay, bisexual, and transgender–related content in undergraduate medical education. JAMA. 2011;306(9):971–977. doi: 10.1001/jama.2011.1255. [DOI] [PubMed] [Google Scholar]