Abstract
Objectives. To examine the longitudinal patterns and predictors of depression trajectories before, during, and after Hong Kong’s 2014 Occupy Central/Umbrella Movement.
Methods. In a prospective study, between March 2009 and November 2015, we interviewed 1170 adults randomly sampled from the population-representative FAMILY Cohort. We used the Patient Health Questionnaire-9 to assess depressive symptoms and probable major depression. We investigated pre-event and time-varying predictors of depressive symptoms.
Results. We identified 4 trajectories: resistant (22.6% of sample), resilient (37.0%), mild depressive symptoms (32.5%), and persistent moderate depression (8.0%). Baseline predictors that appeared to protect against persistent moderate depression included higher household income (odds ratio [OR] = 0.18; 95% confidence interval [CI] = 0.06, 0.56), greater psychological resilience (OR = 0.63; 95% CI = 0.48, 0.82), more family harmony (OR = 0.68; 95% CI = 0.56, 0.83), higher family support (OR = 0.80; 95% CI = 0.69, 0.92), better self-rated health (OR = 0.28; 95% CI = 0.16, 0.49), and fewer depressive symptoms (OR = 0.59; 95% CI = 0.43, 0.81).
Conclusions. Depression trajectories after a major protest are comparable to those after major population events. Health care professionals should be aware of the mental health consequences during and after social movements, particularly among individuals lacking social support.
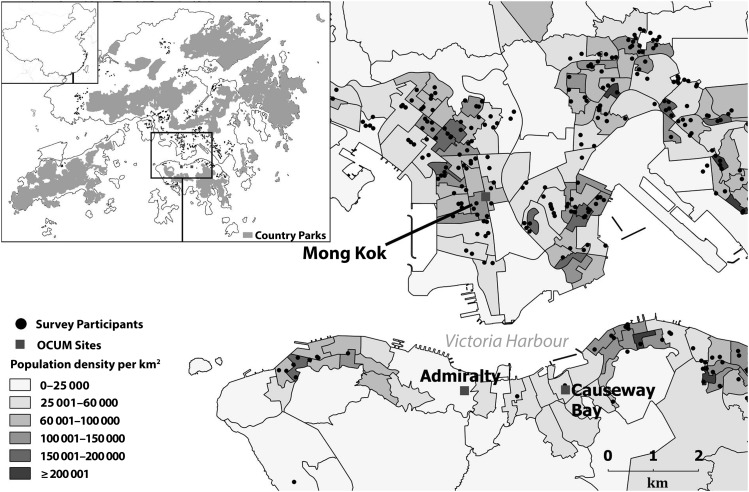
Social movements have become more common around the world in recent years.1 Yet compared with other major population events, such as natural disasters, technological disasters, and terrorist attacks,2 little is known about their mental health impact. In 2014, a massive civil disobedience campaign, “Occupy Central,” also known as the “Umbrella Movement” (OCUM), that called for universal suffrage took place in Hong Kong.3 An estimated one fifth of the 5.2 million–person population aged at least 18 years participated in the 79-day protest,4,5 during which major transportation arteries in the city center were blocked (Figure 1).
FIGURE 1—
Geographical Distribution of Survey Participants: Hong Kong, 2009–2015
Note. OCUM = Occupy Central/Umbrella Movement. The sample size was n = 1170. The diameter of black dots indicates the number of participants. Neighborhoods are shaded according to population density. The inset is a map of Hong Kong and Mainland China.
We previously reported that the absolute prevalence of probable major depression increased by 7.0% (95% confidence interval [CI] = 4.7, 9.2) 6 months after OCUM, regardless of personal involvement in the protests.6 We focused on depression because it is one of the most commonly seen, and therefore studied, psychological sequelae of major population events such as disasters.2,7 Although stress reactions from natural disasters often abate within 12 months, mental health consequences of human-made events, including social movements, appear to persist longer.8–10
We extended follow-up to 12 months after OCUM ended to assess the persistence of the previously observed effects. We also sought to characterize different longitudinal trajectories of depression, in which there may be population heterogeneity, as previously observed in the wake of natural disasters or terrorist acts.11,12 Finally, we assessed baseline and time-varying predictors of the different trajectories to identify potential areas of intervention that might mitigate the adverse mental health impact.
METHODS
We drew our sample from a prospective population-representative cohort study (described in detail elsewhere13): the FAMILY Cohort. The sampling unit of the FAMILY Cohort was a family living in the same household. The sample was obtained by stratified random sampling of households from all 18 districts in Hong Kong, with sample sizes proportionate to each of the district populations. We conducted wave 1 of household visits (n = 17 002 adults) from March 2009 to April 2011 and wave 2 (n = 12 448 adults) from August 2011 to June 2013. We successfully followed up with 73.2% of wave 1 participants in wave 2.13
We surveyed a randomly drawn sample of 887 adult (aged 18 years or older) participants who completed wave 2 within the first month of OCUM (wave 3). We, additionally, oversampled young adults, because of this demographic group’s higher levels of support for the protests,4 by randomly recruiting 283 participants aged 18 to 35 years from the same sampling frame. We followed up with these individuals (n = 1170) during OCUM (waves 3 and 4) and after OCUM (waves 5 and 6) using computer-assisted telephone interviews (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). We calculated cooperation and response rates according to prevailing accepted standards.14
Depressive Symptoms and Probable Major Depression
We assessed depressive symptoms during the 2 weeks before the telephone interviews using the Patient Health Questionnaire-9 (PHQ-9) in all waves. PHQ-9 is a standardized 9-item scale consistent with the diagnostic criteria for major depressive episode in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).15 It has been shown to be a reliable and valid measurement for depressive symptoms in the local population.16 We used scores (range = 0–27) of 0 to 4, 5 to 9, or 10 or greater to indicate none, probable mild, or probable moderate depression, respectively.17
We use the term “probable” because PHQ-9 is a screening instrument and not a diagnostic interview. Nevertheless, a meta-analysis has shown that a score of 10 or greater has a sensitivity of 85% and specificity of 89% for the diagnosis of major depression.18 We defined participants’ history of mental health disorders predating OCUM as the presence of a self-reported doctor diagnosis of depression, anxiety disorder, or schizophrenia.
Predictors
We analyzed baseline predictors at wave 2 because this wave immediately preceded OCUM, although on average it occurred more than 2 years before. Participants reported demographics (including age, gender, marital status, education, employment, and household income) at wave 2 using a structured questionnaire. We assessed the extent of protest participation during the first and second month of OCUM in terms of visiting, assembling (i.e., sitting down at protest sites), and staying overnight.
We used the Connor–Davidson Resilience Scale to assess resilience at wave 2 only. The Chinese version of the abbreviated Connor–Davidson Resilience Scale is a locally validated 2-item scale using a 5-point Likert-type response scale ranging from zero (not true at all) to 4 (true nearly all the time).19,20
We used the Family Harmony Scale-5 to assess 5 aspects of family harmony at each wave—identity, forbearance, conflict resolution, quality time with family, and effective communication—on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The Family Harmony Scale-5 has demonstrated acceptable test–retest reliability and good construct validity.21
We used the Family Adaptation, Partnership, Growth, Affect, Resolve scale to assess family support at each wave. This is a locally validated, 5-item scale using a 3-point Likert-type response scale ranging from zero (hardly ever) to 2 (almost always).22
We assessed neighborhood cohesion using the 5-item question for “social cohesion and trust” at each wave,23 which has shown satisfactory psychometric properties in the local population.24 We asked respondents how strongly they agreed on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree).
We assessed self-rated health by asking respondents to compare their current state of health with that of other individuals of the same age on a 5-point Likert-type response scale ranging from 1 (much worse) to 4 (much better).
We assessed stressful life events using the Recent Life Changes Questionnaire.25 We assessed the presence of 7 different stressful life events in the preceding year at waves 2 and 6. The interrater agreement (κ = 0.78) for the Recent Life Changes Questionnaire is excellent.26
Statistical Analysis
We used semiparametric group-based modeling, a type of latent growth curve analysis, to determine the depression trajectories. This method allows us to estimate the shape and the probability of each trajectory simultaneously. We used the Stata version 13 (StataCorp, LP, College Station, TX) plugin traj,27 which fits the semiparametric mixture model using maximum likelihood estimation. We used zero-inflated Poisson distribution to model depressive symptoms.
We determined the number of trajectories on the basis of the Bayesian information criterion.28 We selected the model with 4 trajectories because of fit statistics and clinical utility (Table A, available as a supplement to the online version of this article at http://www.ajph.org).29 We fitted models with an additional pre-event survey (wave 1) to examine changes in depression among the different trajectories before OCUM.
After determining the depression trajectories, we calculated the posterior probability of individuals belonging to each trajectory. The average posterior probability for the assigned trajectory ranged from 0.81 to 0.91, indicating good model adequacy.30 We assigned individuals to the trajectory with the highest posterior probability. We used the χ2 test to compare the baseline sociodemographics between trajectories. We estimated the association between pre-OCUM sociodemographics, resilience, family harmony, family support, neighborhood cohesion, baseline depressive symptoms, and self-rated health status and the probability of belonging to each of the trajectories using the multinomial logistic regression model (in which the resistant trajectory was the reference group).
For each trajectory, we also estimated the association of time-varying predictors, including intrafamilial sociopolitical conflict, family harmony, family support, neighborhood cohesion, self-rated health, and stressful life events, with the expected level of depressive symptoms. We adjusted all models for age, gender, marital status, education, household income, occupation, baseline depressive symptom score, and the presence of preexisting doctor-diagnosed depression, anxiety disorder, or schizophrenia.
We applied inverse probability of censoring weighting and poststratification weighting to the data. We defined the censoring weights as the inverse of the probability of participating in wave 3 (the first OCUM-specific survey), which we estimated using logistic regression with baseline characteristics including sociodemographics and PHQ-9.31 We then applied poststratification weighting using raking so that each wave would represent the general population.32 We used multiple imputation to handle incomplete data and combined the results from 20 imputed data sets using the Rubin rule.33 We carried out a sensitivity analysis using complete case data.
We conducted all analyses using R version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria) and Stata 13.
RESULTS
We followed up 1170, 893, 867, and 836 participants in waves 3, 4, 5, and 6, respectively. The cooperation rate for wave 3 was 73.9%, and the response rates for waves 4, 5, and 6 were higher than 70% (Figure A). The Cohen w effect size for sociodemographic differences by response status in wave 3 was small to medium (< 0.3). Incomplete data for each variable was less than 7%. Benchmarked against the Hong Kong census, poorer households and those living in public housing were overrepresented, although this conformed to the demographic distribution of the original cohort.6,13 Each wave was similar to census data after we applied poststratification weights (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
Trajectory Patterns
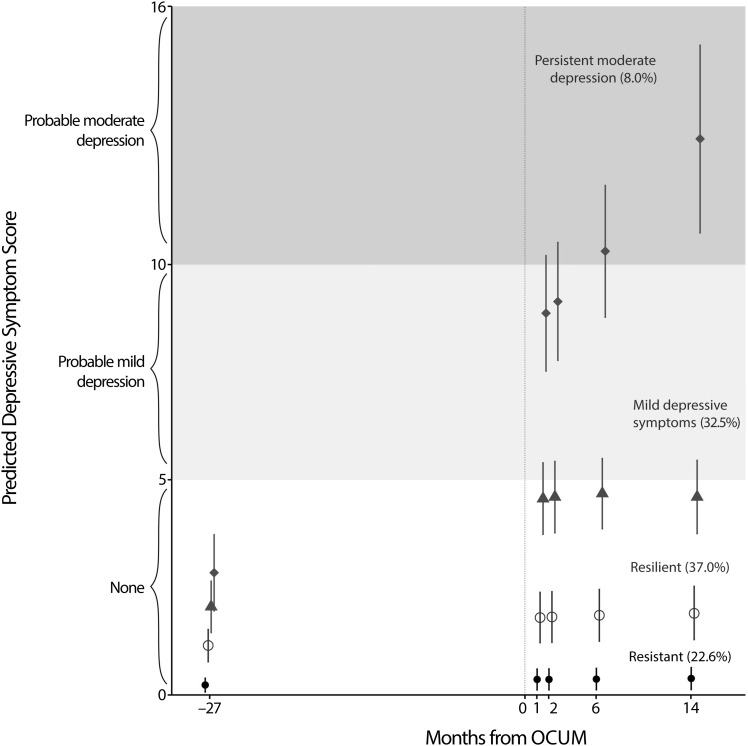
Figure 2 shows the distribution of participants and the predicted PHQ-9 scores for the 4 trajectories. The resistant group, comprising just less than one quarter of the sample, reported mean PHQ-9 scores of less than 0.5 throughout. The resilient group, made up of more than one third of respondents, reported mean scores of 1.0 to 2.0. The mild depressive symptoms group, accounting for almost one third of those sampled, reported elevated PHQ-9 scores just below the lower bound of probable mild depression during and after OCUM.
FIGURE 2—
Depression Trajectories Before, During, and After the Occupy Central/Umbrella (OCUM) Movement: Hong Kong, 2009–2015
Note. The dotted line indicates the OCUM debut. Percentages indicate the proportion of the weighted sample for each trajectory. Identified depression trajectories are shown with 95% confidence intervals.
The scores of the persistent moderate depression group, comprising 8.0% of the sample, reached levels deemed to be “probable moderate depression” 6 months after the protests, which persisted at the 14-month follow-up. These results were invariant when we included wave 1 data as a sensitivity test (Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
Participant Profiles by Trajectories
Table C (available as a supplement to the online version of this article at http://www.ajph.org) shows the sociodemographics and extent of protest participation by the 4 trajectories. We found gender, age group, marital status, employment status, and household income to be associated with depression trajectories. Respondents who were older, had less formal education, were economically inactive, and had lower household income were overrepresented in the persistent moderate depression trajectory (Table C).
The distribution of depression trajectories according to the extent of protest participation is shown in Table D (available as a supplement to the online version of this article at http://www.ajph.org). Figure C (available as a supplement to the online version of this article at http://www.ajph.org) shows that stressful life events were markedly more prevalent in the 2 depressive trajectories after OCUM.
Intrafamilial and Neighborhood Social Support Trends
Figure D (available as a supplement to the online version of this article at http://www.ajph.org) shows the trends of intrafamilial and neighborhood social support as well as self-rated health for the 2 extreme trajectories (i.e., resistant and persistent moderate depression) as illustration. For family support, family harmony, and baseline self-rated health, the 2 trajectories had different baselines before OCUM and the trends diverged afterward.
For neighborhood cohesion, however, both trajectories started at the same level and then diverged, although they tracked each other in parallel since OCUM—albeit at their post-OCUM baselines.
Baseline Predictors of Trajectories
Women appeared to report more mild depressive symptoms than did men (Table 1).
TABLE 1—
Baseline Predictors of Trajectories: Hong Kong, 2009–2015
| Baseline Predictors (Wave 2) | Resilient vs Resistant, OR (95% CI) | Mild Depressive Symptoms vs Resistant, OR (95% CI) | Persistent Moderate Depression vs Resistant, OR (95% CI) |
| Age group,a y | 0.99 (0.97, 1.00) | 0.99 (0.98, 1.01) | 1.00 (0.98, 1.03) |
| Gendera | |||
| Male (Ref) | 1 | 1 | 1 |
| Female | 1.46 (0.64, 3.36) | 1.87 (1.12, 3.12) | 1.74 (0.88, 3.42) |
| Marital statusb | |||
| Married (Ref) | 1 | 1 | 1 |
| Never married | 0.83 (0.36, 1.92) | 1.40 (0.66, 2.99) | 2.49 (0.93, 6.64) |
| Widowed, divorced, or separated | 2.20 (0.45, 10.83) | 3.48 (0.98, 12.30) | 1.04 (0.20, 5.47) |
| Employmentb | |||
| Economically inactive (Ref) | 1 | 1 | 1 |
| Employed | 1.61 (0.74, 3.49) | 1.00 (0.43, 2.32) | 0.62 (0.24, 1.63) |
| Unemployed | 0.66 (0.07, 6.35) | 1.06 (0.21, 5.32) | 0.73 (0.09, 5.77) |
| Educationb | |||
| Primary (Ref) | 1 | 1 | 1 |
| Secondary | 1.14 (0.40, 3.20) | 1.50 (0.60, 3.75) | 0.80 (0.22, 2.82) |
| Tertiary | 1.34 (0.47, 3.86) | 1.24 (0.43, 3.52) | 0.50 (0.10, 2.53) |
| Household income,b HKD | |||
| < 10 000 (Ref) | 1 | 1 | 1 |
| 10 000–19 999 | 1.11 (0.35, 3.53) | 0.81 (0.30, 2.16) | 0.63 (0.21, 1.89) |
| 20 000–39 999 | 0.77 (0.30, 1.97) | 0.67 (0.27, 1.67) | 0.18 (0.06, 0.56) |
| ≥ 40 000 | 0.68 (0.18, 2.58) | 0.75 (0.21, 2.76) | 0.22 (0.03, 1.61) |
| Connor–Davidson Resilience Scale (0–8)b | 1.01 (0.82, 1.26) | 0.97 (0.81, 1.16) | 0.63 (0.48, 0.82) |
| Family Harmony Scale (5–25)b | 0.97 (0.85, 1.11) | 0.86 (0.76, 0.98) | 0.68 (0.56, 0.83) |
| Family support (0–10)b | 0.92 (0.79, 1.08) | 0.95 (0.82, 1.11) | 0.80 (0.69, 0.92) |
| Neighborhood cohesion (5–25)b | 1.07 (0.95, 1.21) | 0.91 (0.78, 1.05) | 1.06 (0.92, 1.23) |
| Wave 1 depressive symptom score (0–27)b | 1.24 (0.87, 1.77) | 1.62 (1.20, 2.19) | 1.69 (1.24, 2.32) |
| Self-rated health (0–4)b | 0.75 (0.50, 1.13) | 0.53 (0.37, 0.76) | 0.28 (0.16, 0.49) |
Note. CI = confidence interval; HKD = Hong Kong dollars; OR = odds ratio.
We have presented unadjusted models only for age and gender because other covariates could not be common causes of these exposures and outcomes.
We examined each pre-event predictor in a separate model and adjusted for age, gender, marital status, education, employment, household income, wave 1 depressive symptom score, and the presence of preexisting doctor-diagnosed depression, anxiety disorder, or schizophrenia before the Occupy Central/Umbrella Movement.
Higher household income, resilience, greater family support and harmony, better self-rated health, and a lower depressive symptom score at baseline were all protectively associated with being in either or both of the depression trajectories.
Time-Varying Predictors of Depressive Symptom Score
Greater family harmony was associated with fewer depressive symptoms for the resistant, resilient, and mild depressive symptoms trajectories (Table 2). Greater family support was associated with fewer depressive symptoms for the mild depressive symptom trajectory. Better neighborhood cohesion was associated with fewer depressive symptoms for the resilient, mild depressive symptoms, and persistent moderate depression trajectories. Better self-rated health appeared to protect against depressive symptoms regardless of individual trajectories. Intrafamilial sociopolitical conflicts were associated with more depressive symptoms for the resilient and persistent moderate depression trajectories. Stressful life events were associated with more depressive symptoms, regardless of individual trajectories.
TABLE 2—
Time-Varying Predictors of Depressive Symptom Scores Before, During, and After the Occupy Central/Umbrella Movement by Trajectories: Hong Kong, 2009–2015
| Time-Varying Predictors (Waves 2–6) | Resistant (Ref), IRR (95% CI) | Resilient, IRR (95% CI) | Mild Depressive Symptoms, IRR (95% CI) | Persistent Moderate Depression, IRR (95% CI) |
| Intrafamilial sociopolitical conflicts | 1.14 (0.94, 1.38) | 1.11 (1.05, 1.18) | 1.01 (0.96, 1.06) | 1.09 (1.05, 1.12) |
| Stressful life events | 2.71 (1.49, 4.96) | 1.54 (1.18, 2.01) | 1.33 (1.15, 1.55) | 1.29 (1.07, 1.56) |
| Family Harmony Scale (5–25)a | 0.84 (0.74, 0.96) | 0.91 (0.89, 0.94) | 0.93 (0.89, 0.97) | 0.97 (0.94, 1.01) |
| Family support (0–10)a | 0.95 (0.85, 1.07) | 0.99 (0.95, 1.03) | 0.95 (0.92, 0.99) | 1.02 (0.99, 1.05) |
| Neighborhood cohesion (5–25)a | 0.92 (0.80, 1.06) | 0.95 (0.90, 1.00) | 0.96 (0.93, 1.00) | 0.97 (0.95, 1.00) |
| Self-rated health (0–4)a | 0.53 (0.31, 0.90) | 0.68 (0.62, 0.74) | 0.81 (0.74, 0.89) | 0.89 (0.81, 0.97) |
Note. CI = confidence interval; IRR = incidence rate ratio.
We adjusted models for age, gender, marital status, education, employment, household income, wave 1 depressive symptom score, and the presence of preexisting doctor-diagnosed depression, anxiety disorder, or schizophrenia before the Occupy Central/Umbrella Movement.
We repeated our analyses using cases with complete data only, which yielded similar findings (results not shown).
DISCUSSION
To our knowledge, this is the first study to examine longitudinal patterns and predictors of psychological sequelae of a major social movement. The prospective design of our study with multiple points of assessment before, during, and after is an advance on previous designs, which were mostly cross-sectional.34–36
Through this study, first, we showed that there was heterogeneity in psychological responses after a social movement. Second, our findings share similarities with trajectories of mental health that have previously been reported in the wake of natural disasters or terrorist attacks, thus extending the observations to mass social movements.11,12,37 Third, the associations we observed suggest potential risk and protective factors for adverse mental impacts, which could be targets for interventions.
Predictors of depression trajectories such as resilience and social support were similar to those observed in the disaster literature, possibly because of common mediators such as psychological stress. Social movements may generate stress via interpersonal conflict6,38 or the disruption of services,36 and we observed more stressful life events among the depressive trajectories after compared with before OCUM (Figure C). Because stress plays an important role in the etiology of depression,39 our findings could be interpreted in the context of exposure and reactivity to stress. Indeed, stressful life events and interpersonal conflicts were associated with more depressive symptoms. We also found that women were more likely to be classified in the mild depressive symptoms group, which is consistent with the generally less favorable long-term depression patterns in women (possibly because of affective, biological, and cognitive mechanisms interacting with stress exposure).40
Higher baseline resilience, a measure of the ability to cope with stress,41 was associated with lower odds of persistent moderate depression. This is consistent with reactivity to stress as a potential explanation of OCUM’s mental health impact. Similarly, the protective role of social support may have operated through stress buffering2,42; studies have shown family harmony and neighborhood cohesion to moderate the association between stress and depressive symptoms.21,24
Our longitudinal measurements of intrafamilial and neighborhood social support have addressed a gap in the literature regarding how major population events influence family relationships and wider community interactions.43 Natural disasters and terrorist attacks that threaten the entire community can be occasions for increased solidarity,44,45 whereas social movements may widen ideological divisions.6 Our observation of lower family support, regardless of individual trajectories, during and after OCUM (Figure D) are consistent with widespread anecdotal reports of a society torn apart by divided sympathies that reached down to the family unit.38 The persistent psychological distress in the aftermath of OCUM might, therefore, be related to the continued decline in social support. Indeed, we have shown lower social support before, during, and after a social movement to be associated with increased depressive symptomatology (Table 2).
Limitations
Our study has limitations. First, the original cohort was susceptible to selection bias and loss to follow-up bias. The FAMILY Cohort enrolled complete households in which all adult members agreed to participate, thus potentially selecting better functioning family units. However, the healthy volunteer effect could have occurred if individuals were sampled instead.13 The application of censoring weights did not appreciably alter results, suggesting that loss to follow-up had little influence on our results.
Second, even with our true longitudinal design, as opposed to a serial cross-sectional design involving different individuals, causality between OCUM and depressive symptoms cannot be definitively inferred. However, depressive symptoms were consistently low at both pre-event time points (Figure B), and it would be difficult to wholly attribute changes in depressive symptoms and social support to other causes.
Third, findings on social support and self-rated health are subject to reverse causality. Depressed individuals during and after the protests may have become more withdrawn and may have poorer self-perceived health. However, we assessed social support and self-rated health before the protests, thus subsequent psychological responses would not have influenced baseline measurements. We also adjusted for mental health history and baseline depressive symptoms to mitigate confounding by preexisting psychological vulnerabilities.
Fourth, we assessed depressive symptoms and major depression through a self-reported scale rather than diagnostic interviews. However, the PHQ-9 is a widely used and valid measurement for depressive symptoms,16 which are associated with functional impairment46 and predict the onset of major depression.47 Indeed, both the DSM-5 and the Research Domain Criteria project have moved toward dimensional approaches as opposed to categorical diagnoses.48,49 Nevertheless, the PHQ-9 has a diagnostic validity for major depression that is comparable to clinician-administered assessments.50
Fifth, we did not assess age of onset of depressive disorder,51 personality,52 and family history of depression,29 which have previously been shown to influence depression trajectories. Even so, we accounted for predisposition to depression by adjusting for preexisting psychiatric disorders and baseline depressive symptoms.
Conclusions
With a substantial proportion of the population displaying elevated depressive symptomatology 1 year after the protests, health care professionals should be vigilant about both the short- and medium-term psychological sequelae of social movements.6 By examining the heterogeneity in psychological responses, we also demonstrated that the protests did not affect the majority. This lends support for targeted interventions during and after protests, rather than mass interventions, because routine psychological debriefing following a traumatic event was found to be largely ineffective and might even be harmful.53
Future studies of major population events may develop clinical prediction rules that could lead to early identification and targeted intervention programs for people who are at the highest risk of psychopathology.54 Those who might benefit from early risk assessment and targeted interventions in the disaster setting include women, those with poorer social support, and those with a preexisting illness,43 which we have also identified as risk factors for probable depression in the context of a major social protest. Preventive measures, such as psychosocial interventions that boost baseline resilience55 and family harmony,56 might mitigate psychological reactions to stressful environments, as our findings demonstrate.
Implications for public health and social policies include the need for sustained resource mobilization infrastructures that foster community resilience and social connectedness.57 With the documented rise in the number of social movements,1 robust evidence is needed to inform strategies that may enhance resilience and mitigate the mental health impact of such population events.11
ACKNOWLEDGMENTS
The establishment of the original cohort was supported by the Hong Kong Jockey Club Charities Trust from 2007 to 2014.
We thank Cynthia Yau, Betty Yuan, and Charles Yiu for technical assistance.
HUMAN PARTICIPANT PROTECTION
The study protocol was approved by the University of Hong Kong/Hospital Authority Hong Kong West Cluster institutional review board. Informed verbal consent was obtained from all participants.
REFERENCES
- 1.Ortiz I, Burke S, Berrada M, Cortés H. World Protests 2006–2013. New York, NY: Initiative for Policy Dialogue, Columbia University; 2013. [Google Scholar]
- 2.Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- 3.Ng KC. What is Occupy Central? 10 key facts about Hong Kong’s pro-democracy movement. South China Morning Post. September 30, 2014.
- 4.Centre for Communication and Public Opinion Survey. Public opinion & political development in Hong Kong: survey results. 2014. Available at: http://www.com.cuhk.edu.hk/ccpos/images/news/TaskForce_PressRelease_141218_English.pdf. Accessed June 8, 2015.
- 5.Chung R T-Y, Pang K K-L. Mingpao sponsored “Survey on CE Election and Occupy Central Campaign” (seventh round) 2014. Available at: http://hkupop.hku.hk/english/report/mpCEnOCCw7/index.html. Accessed July 22, 2015.
- 6.Ni MY, Li TK, Pang H et al. Direct participation in and indirect exposure to the Occupy Central Movement and depressive symptoms: a longitudinal study of Hong Kong adults. Am J Epidemiol. 2016;184(9):636–643. doi: 10.1093/aje/kww103. [DOI] [PubMed] [Google Scholar]
- 7.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak. Part I: An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65(3):207–239. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 8.Solomon S, Green B. Mental health effects of natural and human-made disasters. PTSD Research Quarterly. 1992;3(1):1–8. [Google Scholar]
- 9.Kumar M, Fonagy P. Differential effects of exposure to social violence and natural disaster on children’s mental health. J Trauma Stress. 2013;26(6):695–702. doi: 10.1002/jts.21874. [DOI] [PubMed] [Google Scholar]
- 10.Moussa S, Kholy ME, Enaba D et al. Impact of political violence on the mental health of school children in Egypt. J Ment Health. 2015;24(5):289–293. doi: 10.3109/09638237.2015.1019047. [DOI] [PubMed] [Google Scholar]
- 11.Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68(12):2190–2198. doi: 10.1016/j.socscimed.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 12.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 13.Leung GM, Ni MY, Wong PT et al. Cohort profile: FAMILY Cohort. Int J Epidemiol. 2015 doi: 10.1093/ije/dyu257. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.ESOMAR. AAPOR standard definitions: final dispositions of case codes and outcome rates for surveys. 2015. Available at: https://www.esomar.org/knowledge-and-standards/research-resources/aapor-standard-definitions.php. Accessed January 3, 2016.
- 15.Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 16.Yu X, Tam WWS, Wong PT, Lam TH, Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. 2012;53(1):95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaishnavi S, Connor K, Davidson JR. An abbreviated version of the Connor–Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007;152(2–3):293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ni MY, Li TK, Yu NX et al. Normative data and psychometric properties of the Connor–Davidson Resilience Scale (CD-RISC) and the abbreviated version (CD-RISC2) among the general population in Hong Kong. Qual Life Res. 2016;25(1):111–116. doi: 10.1007/s11136-015-1072-x. [DOI] [PubMed] [Google Scholar]
- 21.Kavikondala S, Stewart SM, Ni MY et al. Structure and validity of family harmony scale: an instrument for measuring harmony. Psychol Assess. 2016;28(3):307–318. doi: 10.1037/pas0000131. [DOI] [PubMed] [Google Scholar]
- 22.Chan D, Ho S, Donnan S. A survey of family APGAR in Shatin private ownership homes. Hong Kong Practitioner. 1988;10(7):3295–3299. [Google Scholar]
- 23.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 24.Chou KL. Perceived discrimination and depression among new migrants to Hong Kong: the moderating role of social support and neighborhood collective efficacy. J Affect Disord. 2012;138(1–2):63–70. doi: 10.1016/j.jad.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 25.Miller MA, Rahe RH. Life changes scaling for the 1990s. J Psychosom Res. 1997;43(3):279–292. doi: 10.1016/s0022-3999(97)00118-9. [DOI] [PubMed] [Google Scholar]
- 26.Voyer M, Cappeliez P. Congruency between depressogenic schemas and life events for the prediction of depressive relapse in remitted older patients. Behav Cogn Psychother. 2002;30(2):165–177. [Google Scholar]
- 27.Jones BL, Nagin DS. A note on a Stata plugin for estimating group-based trajectory models. Sociol Methods Res. 2013;42(4):608–613. [Google Scholar]
- 28.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 29.Musliner KL, Munk-Olsen T, Laursen TM, Eaton WW, Zandi PP, Mortensen PB. Heterogeneity in 10-year course trajectories of moderate to severe major depressive disorder: a Danish National Register-based study. JAMA Psychiatry. 2016;73(4):346–353. doi: 10.1001/jamapsychiatry.2015.3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005.
- 31.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: Wiley; 2011. [Google Scholar]
- 32.Lumley T. Complex Surveys: A Guide to Analysis Using R. New York, NY: Wiley; 2010. [Google Scholar]
- 33.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. [Google Scholar]
- 34.Tan ES, Simons RC. Psychiatric sequelae to a civil disturbance. Br J Psychiatry. 1973;122(566):57–63. doi: 10.1192/bjp.122.1.57. [DOI] [PubMed] [Google Scholar]
- 35.Lyons HA. Psychiatric sequelae of the Belfast riots. Br J Psychiatry. 1971;118(544):265–273. doi: 10.1192/bjp.118.544.265. [DOI] [PubMed] [Google Scholar]
- 36.Hanson RF, Kilpatrick DG, Freedy JR, Saunders BE. Los Angeles County after the 1992 civil disturbances: degree of exposure and impact on mental health. J Consult Clin Psychol. 1995;63(6):987–996. doi: 10.1037//0022-006x.63.6.987. [DOI] [PubMed] [Google Scholar]
- 37.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- 38.Hong Kong Economic Times. [“Occupy Central” causing laceration in a family of four: rebuilding the mind and body of secondary school students and helping them walk out of the shadows]. 2015. Available at: http://www.hket.com/eti/article/00523597-6e57-407e-bc06-5104b4895cf1-487146?source=print&printable=true. Accessed June 8, 2015.
- 39.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 40.Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115(2):291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- 41.Connor KM, Davidson JR. Development of a new resilience scale: the Connor–Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 42.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consult Clin Psychol. 2007;75(5):671–682. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- 44.Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71(9):1025–1031. doi: 10.1001/jamapsychiatry.2014.652. [DOI] [PubMed] [Google Scholar]
- 45.Salib E. Effect of 11 September 2001 on suicide and homicide in England and Wales. Br J Psychiatry. 2003;183:207–212. doi: 10.1192/bjp.183.3.207. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Zhao S, Blazer DG, Swartz M. Prevalence, correlates, and course of minor depression and major depression in the national comorbidity survey. J Affect Disord. 1997;45(1–2):19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- 47.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. J Abnorm Psychol. 2000;109(2):345–351. [PubMed] [Google Scholar]
- 48.Regier DA, Narrow WE, Kuhl EA, Kupfer DJ. The conceptual development of DSM-V. Am J Psychiatry. 2009;166(6):645–650. doi: 10.1176/appi.ajp.2009.09020279. Comment in The age at onset of attention deficit hyperactivity disorder. Am J Psychiatry. 2010. [DOI] [PubMed] [Google Scholar]
- 49.Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry. 2014;13(1):28–35. doi: 10.1002/wps.20087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 51.Zisook S, Lesser I, Stewart JW et al. Effect of age at onset on the course of major depressive disorder. Am J Psychiatry. 2007;164(10):1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]
- 52.Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode: a 3-wave population-based study. Arch Gen Psychiatry. 2004;61(10):990–996. doi: 10.1001/archpsyc.61.10.990. [DOI] [PubMed] [Google Scholar]
- 53.van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PM. Single session debriefing after psychological trauma: a meta-analysis. Lancet. 2002;360(9335):766–771. doi: 10.1016/S0140-6736(02)09897-5. [DOI] [PubMed] [Google Scholar]
- 54.Shelton RC. The course of illness after initial diagnosis of major depression. JAMA Psychiatry. 2016;73(4):321–322. doi: 10.1001/jamapsychiatry.2015.3457. [DOI] [PubMed] [Google Scholar]
- 55.Yu X, Stewart SM, Chui JP, Ho JL, Li AC, Lam TH. A pilot randomized controlled trial to decrease adaptation difficulties in Chinese new immigrants to Hong Kong. Behav Ther. 2014;45(1):137–152. doi: 10.1016/j.beth.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 56.Fabrizio CS, Lam TH, Hirschmann MR et al. Parental emotional management benefits family relationships: a randomized controlled trial in Hong Kong, China. Behav Res Ther. 2015;71:115–124. doi: 10.1016/j.brat.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 57.Neria Y, Galea S, Norris FH. Disaster mental health research: current state, gaps in knowledge, and future directions. In: Neria Y, Galea S, Norris FH, editors. Mental Health and Disasters. Cambridge: Cambridge University Press; 2009. pp. 594–610. [Google Scholar]