In this issue of the AJPH, Caceres et al. (pp. 570, e13) publish for a second time1 results from a systematic review of 31 studies that investigated sexual orientation–related differences in cardiovascular risk factors, such as tobacco use, obesity, and stress. Although the authors set out to review work conducted over the past 30 years, only articles from 2000 or later met their criteria. This is no accident.2 Measurement of sexual orientation in the general population did not begin in earnest until the turn of the century because of the need for health surveillance of sexual risk behaviors. Very quickly researchers began to document robust, and unexpected, health differences linked to sexual orientation in both men and women. Today, most national health surveillance systems within the United States measure sexual orientation in some form. And although there are lingering discussions of how to optimally measure these constructs, the emerging data are being rapidly mined, linking health disparities among sexual minorities to the social harm of discrimination.3
OLDER LESBIAN, GAY, AND BISEXUAL ADULTS
This new science also includes observations that behavioral risk factors associated with cardiovascular disease (CVD) vary by sexual orientation. Although the review did not observe a direct link to CVD, the most likely reasons are twofold. As they noted, CVD is a disease seen mostly among older adults and the reviewed studies had very few older lesbian, gay, and bisexual (LGB) adults within them. Will we have these data in the future? Perhaps. Few data sets now include sufficient numbers of older LGB adults that would support research investigating CVD prevalence.
However, some data systems are gradually accumulating larger sample sizes of sexual minorities, such as the National Health and Nutrition Examination Survey. With time, sample sizes will likely support this work to varying extent. But it is also true that age restrictions on sexual orientation measurement in surveys (often 60 years of age, sometimes 70 years) will remain a methodological barrier greatly limiting our capacity to identify disease disparities among older LGB adults.
DECLINE IN SEXUAL ORIENTATION DIFFERENCES . . .
The most difficult task that lies before us is making sense of why these health disparities exist, as well as taking steps to eliminate them.4 It will not be easy. For example, among the many things we know about cigarette smoking in the United States are two widely accepted truths. First, the prevalence of tobacco smoking has been declining over the years, likely a consequence of widespread public health interventions. Estimates from the 2005 National Health Interview Survey indicate that about 21% (95% confidence interval = 20.3%, 21.5%) of adults were then current smokers.5 By 2013, prevalence had declined to 18% (95% confidence interval = 17.2%, 18.4%) of US adults. Second, men are much more likely to smoke cigarettes than women are by an average ratio of 1.3–1.4 to 1.5 This gender difference is seen in studies of youths and of adults, within most racial/ethnic groups, and across levels of educational attainment and income.
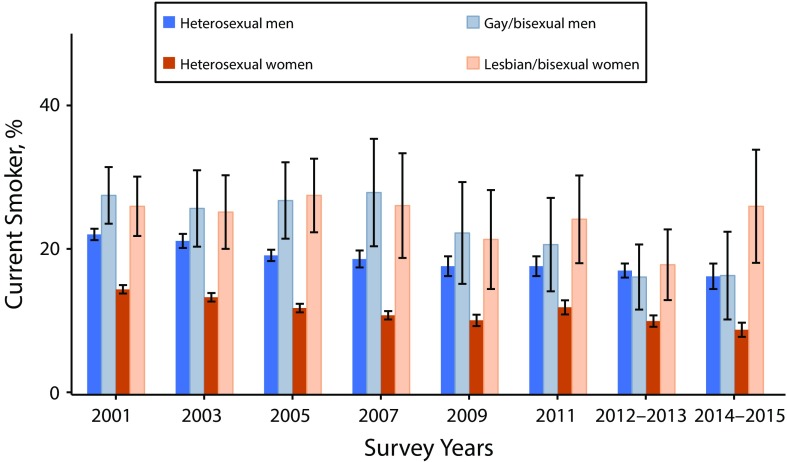
The one place where this truth about gender differences may not hold is among sexual minorities. The California Health Interview Survey (http://www.chis.ucla.edu) interviews approximately 40 000 to 50 000 Californians every two years and has measured sexual orientation since its inception in 2001. Figure 1 shows a secular decline in smoking among Californians consistent with national trends. Also apparent is the robust gender difference between heterosexual men and heterosexual women; the average gender ratio across survey years is 1.6 to 1. One can also identify two additional effects in the graph. First, there is an absence of gender differences among sexual minorities: lesbian or bisexual women are just as likely or more likely than gay or bisexual men to be current smokers. Second, there are hints of a gradual decline in sexual orientation differences that would be consistent with predictions from the minority stress theory: as levels of public acceptance of homosexuality have increased in recent years,6 the health disparity in smoking has been eradicated, but only for men. Gay or bisexual women still experience a more than 2 to 1 ratio of smoking compared with heterosexual women.
FIGURE 1—
Percentage Current Smokers by Sexual Orientation and Gender Over Time: California Health Interview Surveys, 2001–2015
Note. 95% confidence interval error bars shown.
. . . BUT NOT FOR LESBIANS AND BISEXUAL WOMEN
These effects are difficult to explain with minority stress theory alone. Fortunately, there are other, complementary models of how social conditions shape health risks. For example, the cumulative advantage/disadvantage hypothesis7 argues that health is a consequence not just of stress but also of the social advantages and disadvantages that we experience throughout life, often outside awareness. These influences from our social roles, our available resources, and our experiences with life accumulate to create diversities among us even when we share similar current social profiles.
Lesbians or bisexual women experience a somewhat different world than gay or bisexual men. The ways in which CVD risk factors cluster by gender, or not in the case of tobacco use among LGB adults, can create unexpected health consequences, a point well demonstrated in the high HIV infection rates of both Black men who have sex with men and Black heterosexual women in the US South.8 It can also create novel pathways for public health interventions, if we acknowledge the differences that exist among us, structure our research to be of broad benefit to all, and dig deep to isolate key motivators that can produce needed behavior change.
EVOLVING CHALLENGES
To advance the science of health equity in sexual minority populations, we need to remember these lessons. Each status characteristic, whether it is gender, age, geographic location, or race/ethnicity is associated with power and privilege and conferral of risk or benefit in patterns that have yet to be fully articulated. When it comes to tobacco use in California, something has clearly reduced sexual minority men’s smoking rates and we should celebrate that success. Perhaps, thankfully, minority stress is easing.6 But whatever the reason underlying the behavior change among gay and bisexual men, it has not had the same effect on lesbian and bisexual women for reasons we do not yet understand. It is time to find an effective approach to reducing sexual minority women’s health risks. Until we do, our job as public health practitioners is not done.
REFERENCES
- 1.Caceres BA, Brody A, Chyun D. Recommendations for cardiovascular disease research with lesbian, gay and bisexual adults. J Clin Nurs. 2016;25(23–24):3728–3742. doi: 10.1111/jocn.13415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cochran SD. Emerging issues in research on lesbians’ and gay men’s mental health: does sexual orientation really matter? Am Psychol. 2001;56(11):931–947. doi: 10.1037/0003-066x.56.11.931. [DOI] [PubMed] [Google Scholar]
- 3.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cochran SD, Mays VM. A strategic approach to eliminating sexual orientation–related health disparities. Am J Public Health. 2016;106(9):e4. doi: 10.2105/AJPH.2016.303271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Higgins ST, Kurti AN, Redner R et al. A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. Prev Med. 2015;80:89–100. doi: 10.1016/j.ypmed.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwadel P, Garneau CRH. An age-period-cohort analysis of political tolerance in the United States. Sociol Q. 2014;55(2):421–452. [Google Scholar]
- 7.DiPrete TA, Eirich GM. Cumulative advantage as a mechanism for inequality: a review of theoretical and empirical developments. Annu Rev Sociol. 2006;32:271–297. [Google Scholar]
- 8.Mays VM, Maas R, Ricks J, Cochran S. HIV in African American women: a social determinants approach in population-level HIV prevention and intervention. In: Baum A, Revenson T, Singer J, editors. Handbook of Health Psychology. 2nd ed. New York, NY: Taylor & Francis; 2012. pp. 771–802. [Google Scholar]