Abstract
Objectives
Although cocaine use has been linked to sexual HIV risk behavior for decades, the direct effects of cocaine on sexual desire and sexual decision-making are unexamined. Research suggests delay discounting (devaluation of future outcomes) and probability discounting (devaluation of uncertain outcomes) play roles in condom use decisions. This study examined the effect of cocaine administration on sexual desire, hypothetical condom use, and discounting tasks.
Methods
This double-blind, within-subjects study compared the effects of 0, 125 and 250 mg/70 kg oral cocaine HCl in 12 cocaine users. Measures included sexual desire and other subjective ratings, the Sexual Delay Discounting Task, the Sexual Probability Discounting Task, and monetary delay and probability discounting tasks.
Results
Cocaine caused dose-related increases in sexual desire and prototypical stimulant abuse-liability ratings. Relative to placebo, cocaine did not significantly alter condom use likelihood when condoms were immediately available or when sex was associated with 100% certainty of sexually transmitted infection (STI). In contrast, cocaine dose-dependently strengthened the effect of delay (sexual delay discounting) and STI uncertainty (sexual probability discounting) in decreasing condom use likelihood. Cocaine caused no significant change in monetary delay and probability discounting.
Conclusion
This is the first study showing that cocaine administration increases sexual desire. Detrimental effects of cocaine on sexual risk were only observed when safer sex required delay, or STI risk was uncertain (representative of many real-world scenarios), suggesting a critical role of discounting processes. Lack of monetary effects highlights the importance of studying clinically-relevant outcomes when examining drug effects on behavioral processes.
Keywords: Cocaine, delay discounting, HIV, sexual risk behavior, sexual desire, humans
Introduction
Cocaine users show substantially higher HIV prevalence (4–22%) (Booth et al. 1993; Booth et al. 2000; McCoy et al. 2004; Strathdee and Sherman 2003) than the national average (~0.5%) (Hall et al. 2015). Sexual risk behavior contributes substantially to these high rates (e.g., Booth et al. 1993; Bux et al. 1995; Edlin et al. 1994; Edwards et al. 2006; Grella et al. 1995; Hoffman et al. 2000; Joe and Simpson 1995). Efforts to reduce sexual risk behavior among drug users have largely aimed to improve HIV prevention knowledge and condom use skills (e.g., Heil et al. 2005; Herrmann et al. 2013; Malow et al. 1994; Winhusen et al. 2014). Although these efforts have improved knowledge and skills, changes in risk behavior have been modest (Prendergast et al. 2001; Semaan et al. 2002), suggesting that sexual risk decisions likely depend on behavioral processes aside from risk-reduction knowledge or skills (Johnson and Bruner 2012).
Delay discounting is a behavioral process whereby delaying an event reduces its value. Studies typically measure delay discounting by examining choices between smaller-immediate vs. larger-later money rewards. However, recent evidence shows stronger relations between delay discounting and clinical problems when the discounting task assesses clinically relevant outcomes rather than money (Johnson and Bruner 2012; Lawyer and Schoepflin 2013; Rasmussen et al. 2010; Schiff et al. 2015). The Sexual Delay Discounting Task examines the effect of delay discounting on episode-level sexual risk behaviors (Johnson and Bruner 2012). Participants select photographs of hypothetical potential sexual partners, and then rate their likelihood of choosing to have immediate unprotected sex vs. waiting a specified delay (at a range of different delays) to have condom-protected sex. Studies have shown that sexual delay discounting (i.e., the reduction in condom use likelihood as a function of delay) is: greater when responding for more desirable partners (Dariotis and Johnson 2015; Herrmann et al. 2014; Herrmann et al. 2015; Johnson and Bruner 2012; Johnson and Bruner 2013); more strongly related to self-reported sexual risk behavior relative to money discounting (Johnson and Bruner 2012); associated with greater self-reported drug use and risky sexual partners in adolescents/young adults (Dariotis and Johnson 2015); reliable over time (Johnson and Bruner 2013); greater for men than women (Johnson and Bruner 2013); greater in opioid-dependent women than control women (Herrmann et al. 2014); associated with drug use and unprotected sex among men who have sex with men (Herrmann et al. 2015); increased by acute alcohol administration (Johnson et al. 2016); and greater in those with Cocaine Use Disorder than demographically matched controls (Johnson et al. 2015a).
Collectively, the data support the notion that delay discounting may contribute to sexual risk behavior among a variety of populations, including cocaine users. However, questions remain about the relation between cocaine use and increased discounting. At least three non-mutually-exclusive hypotheses may describe this relation. First, other variables (e.g., genetics, behavioral history) may independently predispose a person to both cocaine use and increased delay discounting. Second, a history of chronic cocaine use may cause increased discounting. Third, cocaine intoxication may acutely increase delay discounting. Increased delay discounting among cocaine users in cross-sectional human studies not involving drug administration (e.g., Heil et al. 2005; Johnson et al. 2015a) is consistent with any of the above hypotheses. The observation with rats that delay discounting under non-drug conditions predicts subsequent cocaine self-administration lends support to the first hypothesis, but does not refute the second or third hypothesis (Perry et al., 2008; 2005). The well-replicated finding from nonhuman animal research that a chronic cocaine administration history increases delay discounting (Dandy and Gatch 2009; Koffarnus and Woods 2013; Logue et al. 1992; Mendez et al. 2010; Roesch et al. 2007; Setlow et al. 2009; Simon et al. 2007) lends support to the second hypothesis. Given that cocaine users report increased risk behavior while acutely intoxicated on cocaine (e.g., Colfax et al. 2004; Rendina et al. 2015), the present study aimed to test the third hypothesis (i.e., causal effect of acute cocaine intoxication on sexual risk behavior).
This randomized, double-blind, within-subject study administered 0, 125, or 250 mg/70 kg oral cocaine HCl in each of three separate sessions to non-treatment seeking cocaine users who met DSM-IV criteria for cocaine abuse or dependence. We specifically recruited participants who met abuse or dependence criteria in order to examine a clinically-relevant population. Cocaine doses were selected based on previous research showing robust and dose-related subjective effects (Smith et al. 2001). Participants completed the Sexual Delay Discounting Task and a money delay discounting task to determine whether potential cocaine effects on discounting were general, or specific to certain commodities. We also assessed probability discounting of both sexual and monetary outcomes. Using a similar framework as delay discounting tasks, probability discounting tasks determine how uncertainty influences an event’s value, typically by assessing choices between smaller-certain vs. larger-uncertain monetary rewards (Bickel et al. 2014; Rachlin et al. 1991). The Sexual Probability Discounting Task was developed to determine the effect of sexually transmitted infection (STI) contraction probability on condom use likelihood (Johnson et al. 2015a). In that study, greater odds against STI contraction were associated with substantial decreases in condom use likelihood. The present study also examined the effect of cocaine administration on the delay discounting of cocaine itself (see Johnson et al. 2015b). Moreover, despite decades of research linking cocaine use to sexual risk behavior, the present study is the first to experimentally examine effects of cocaine administration on sexual desire (Volkow et al. 2007). The study was well-positioned, therefore, to determine which processes may underlie risky sex decisions, and whether those processes are similarly affected across outcome type.
Methods
Ethics Statement
Johns Hopkins University Institutional Review Board approved the study, performed in accordance with the 1964 Declaration of Helsinki. Participants provided written informed consent.
Participants
Healthy cocaine users were recruited from the Baltimore, MD area via newspaper, radio, internet, and word-of mouth. Eligibility was assessed by an initial telephone screening, followed by an in-person interview and medical examination. Inclusion criteria were: 18–45 years of age; literate; meet DSM-IV criteria for current cocaine abuse or dependence; using cocaine within the past month; using cocaine for at least one year; and having unprotected and condom-protected sexual intercourse at least once each within the lifetime (this was required because hypotheses regarding condom use vs. non-use are best tested in individuals who have had experience with both options). Exclusion criteria were: History of severe psychiatric disorder; daily use of any psychiatric medications by prescription; current physical dependence on any drug except cocaine, caffeine, or nicotine; interest in treatment for substance use; pregnancy (confirmed by urinalysis), hypertension, breastfeeding, or not using an effective means of contraception (females only). A range of other criteria excluded those with susceptibility or history of cardiovascular illness or other serious medical disorders. Aside from formal criteria, one applicant was excluded for legal issues requiring random drug testing. Another was excluded because of a current opiate prescription and a history of injection heroin use. Participants received $280 for completing the study, including a $160 completion bonus, with the opportunity to earn additional compensation (maximum ~$28) based on performance in tasks not reported here. Participants could also receive a $100 bonus for referring someone who completed the study.
Screening Session Assessments
Assessments administered at the screening visit are shown in Table 1. We collected detailed data about drug use (e.g., DSM-IV drug abuse and dependence checklists based on Hudziak et al., 1993), sexual HIV risk behaviors (Behavioral Risk Assessment for Infectious Diseases [BRAID], Dunn et al., In Press; HIV Risk-taking Behavior Scale, Darke et al. 1991), verbal intelligence (Quick Test; Ammons and Ammons 1962), and ADHD symptoms (Adult ADHD Self-Report Scale; Kessler et al. 2005). In order to familiarize participants with study measures before potential drug effects would be experienced in subsequent laboratory sessions, participants were required to practice completing the subjective drug effects questionnaire, the Sexual Delay Discounting Task (described below), and the Sexual Probability Discounting Task (described below).
Table 1.
Formal self-report and behavioral assessments at the screening session, and timing of assessments relative to drug administration at experimental sessions.
| Time Administered | Measure |
|---|---|
| Screening Session | DSM-IV drug abuse and dependence checklists |
| BRAID | |
| HIV Risk Taking Behavior Scale | |
| Quick Test | |
| Adult ADHD Self-Report Scale | |
| Subjective drug effects questionnaire (practice) | |
| Sexual Delay Discounting Task (practice) | |
| Sexual Probability Discounting Task (practice) | |
| Drug Administration Sessions | |
| Minutes post-administration a | |
| 20 | Monetary Delay Discounting |
| 30 | Sexual Delay Discounting |
| 40 | Sexual Probability Discounting |
| 50 | Monetary Probability Discounting |
| 70 | Cocaine Craving Questionnaire |
| 80 | Cocaine Delay Discounting |
Note. DSM-IV checklists based on Hudziak et al. (1993) were used to assess drug abuse and dependence. The Behavioral Risk Assessment for Infectious Diseases (BRAID; Dunn et al., In Press) assessed sexual risk behaviors. The HIV Risk Taking Behavior Scale assessed injection drug use and sexual HIV risk behaviors (Darke et al., 1991). The Quick Test assessed verbal intelligence (Ammons and Ammons, 1962). The Adult ADHD Self-Report Scale assessed ADHD symptoms (Kessler et al. 2005). See text for discounting task details.
Measurements of physiological measures and subjective drug effects occurred ten minutes before administration and 10, 20, 30, 40, 50, 60, 70, 80, 90, 120, and 125 min post-administration.
Laboratory Procedures
Study protocol
At least 24 hours before each drug administration session, participants were called and reminded to abstain from drugs and alcohol for at least 24 hours and to abstain from eating or drinking for at least 12 hours before arriving the next day. Participants arrived at 7:30 a.m. for each session and provided a breath alcohol sample and a urine sample to test for drugs of abuse. Sessions were rescheduled if breath samples showed non-zero alcohol levels. Participants ate a low-fat breakfast consisting of two pieces of toast, two packets of jelly, and 355 ml of either apple or grape juice, which was finished by 8:00 a.m. to allow two hours before drug administration at 10:00 a.m. Participants could smoke cigarettes at the beginning of the session, but finished their last cigarette at least 30 min before drug administration. This ensured that participants who were smokers had completed all discounting tasks within ~2 hours of smoking to minimize the potential effects of nicotine withdrawal on study outcome measures. Moreover, previous human research suggests no interaction between nicotine maintenance vs. abstinence on cocaine subjective effects (Sobel et al., 2004).
Before drug administration, participants completed computerized practice examples using visual analog scales (VAS) like those used for the sexual discounting tasks. Briefly, seven scenarios were presented describing different levels of food deprivation and corresponding likelihood of eating dinner tonight (0, 5, 25, 50, 75, 95, and 100%). For each of these scenarios, participants were required to complete a VAS while specifying the described likelihood. If a participant did not specify the stated likelihood on the VAS, additional instruction was provided and the practice trial was repeated until the correct response was provided. At the first session, to ensure understanding, participants took a brief quiz on the content of the instructions for the monetary delay discounting task after they were read aloud by research staff. Incorrect answers prompted further instruction.
Drug Administration
During three drug administration sessions, participants orally ingested, with water, a size 00 opaque capsule containing either 0 (placebo), 125, or 250 mg/70 kg of cocaine HCl. Across sessions the capsules appeared identical and were each filled completely with a combination of cellulose and/or cocaine HCl. Drug administration was double-blind. Administration order was randomized across participants.
Laboratory Assessments
Table 1 shows the timing and order of all drug administration session assessments.
Physiological Measures
During the session, heart rate and blood pressure were measured using a Criticare 507S Non-Invasive Patient Monitor. Medical staff was contacted immediately if participant blood pressure exceeded 200/130 mmHg or if their submaximal heart rate (220-[age in years × 0.85]) was exceeded. Participants were permitted to leave the laboratory after study sessions were completed if cardiovascular discharge criteria were met (systolic blood pressure ≤ 150 mmHg, diastolic blood pressure ≤ 100 mmHg, heart rate ≤ 100 BPM). Sessions lasted approximately 4.5 hours (approximately 7:30 AM to 12:00 PM).
Subjective Drug Effects
Similar to previous studies (Johnson et al. 2010; Johnson and Griffiths 2013), during sessions, participants responded to 12 items measuring subjective drug effects on a 5-point scale (0=Not at all, 1=Possibly mild, but not sure, 2=Definitely mild, 3=Moderately, 4=Strongly). We also examined ratings of sexual desire, using a VAS ranging 0 to 100, where 0=None and 100=Intense.
Discounting Tasks
Sexual Delay Discounting
During screening, participants viewed 60 photographs of clothed men (30) and women (30) and selected the photographs of individuals they would choose to have sex with in a casual sex scenario. Among the selected photographs, participants chose the person they judged as least likely to have an STI. Although it was never implemented, women who chose a female partner were excluded, given the low rate of sexual HIV transmission between females (Chan et al. 2014). One participant was disqualified because she did not select at least one photo from the set. Two participants were excluded because while practicing the task during screening they indicated 100% condom use likelihood at all delays or probabilities of STI contraction; see below for task details). This was because the aim of the study was to examine factors contributing to risk behavior among individuals who engage in risk behavior. Individuals who endorse condom use in all scenarios are therefore not relevant to the experimental hypotheses.
During drug administration sessions, participants were shown the photograph of their selected partner and asked to read a modified (to remove mention of alcohol) vignette about a hypothetical sexual encounter with their selected partner (George et al. 2009). After reading the vignette, and immediately before completing the sexual delay discounting task, participants rated their level of sexual desire “right now” on a VAS ranging from 0 (none) to 100 (intense). This pre-task assessment of sexual desire was used for examining correlations with the Sexual Delay Discounting Task, and is distinct from the sexual desire ratings (as one of the 12 subjective effects) assessed throughout the time course. Participants were asked to rate their likelihood of using a condom in the vignette scenario if a condom were immediately available. Using a VAS similar to the practice scales described above, participants specified an integer percent ranging from 0 (“I will definitely have sex with this person right away without a condom”) to 100 (“I will definitely have sex with this person with a condom”). Next, participants rated their likelihood of using a condom in the same scenario with the exception that a condom was not immediately available, and the 100% value in the range represented “I will definitely wait [delay] to have sex with this person with a condom.” Seven delays were examined in separate scales: 2 min, 5 min, 15 min, 30 min, 1 hr, 3 hr, and 6 hr. These delays are shorter than those in previous studies (Johnson & Bruner 2012, 2013; Johnson et al. 2015a; Herrmann et al. 2014, 2015; Johnson et al. 2016) in an effort to assess discounting of condom-protected sex at delays to condom availability more relevant in real-world sexual situations.
Sexual Probability Discounting
Using a framework similar to the Sexual Delay Discounting Task, participants rated the likelihood of condom use given a particular probability of contracting an STI (Johnson et al. 2015a). This task included its own pre-task assessment of sexual desire, as in the Sexual Delay Discounting Task. The 8 probabilities assessed were 1 in 1 (100%), 1 in 3 (33%), 1 in 13 (8%), 1 in 100 (1%), 1 in 400 (0.25%), 1 in 700 (0.14%), 1 in 2,000 (0.05%), and 1 in 10,000 (0.01%) chance of contracting an STI. Risk was presented as probability of contracting an STI using two numbers (e.g., 1 in 3) rather than a percentage (e.g., 33%).
Monetary Delay Discounting
In this task participants chose between receiving a smaller amount of money immediately and $100 after a specified delay. At each of seven delays, examined in ascending order, the magnitude of smaller immediate money was adjusted across trials until an indifference point was detected, using an algorithm as previously described (Baker et al. 2003; Heil et al. 2006; Johnson and Bickel 2002). After determining the indifference point, the task moved to the next delay or concluded after the last delay. The seven delays were: 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, and 25 years.
Monetary Probability Discounting
Participants chose between receiving a smaller, certain amount of money and a probability of receiving $100. At each of seven probabilities, examined in descending order, the magnitude of the smaller certain money was adjusted across trials until a point of subjective equivalence was detected by algorithm as previously described (Yi et al. 2005). After determining the indifference point, the task moved to the next probability or concluded after the last probability. The seven probabilities were: 99%, 90%, 75%, 50%, 25%, 10%, and 1% chance.
Cocaine Delay Discounting
Similar to a previous task (Johnson et al. 2015b), participants chose between receiving fewer units of cocaine (crack rocks or powder vials worth $5 street value each) immediately and receiving 20 units of cocaine after a delay. Delays examined were: 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, and 25 years.
Cocaine Craving Questionnaire
Participants completed a VAS version of the brief Cocaine Craving Questionnaire (CCQ-Brief; Sussner et al. 2006). Participants rated each of 10 items from strongly disagree (0) to strongly agree (1). The CCQ-Brief is reliable, valid, and superior to single-item VAS measures of cocaine craving (Sussner et al. 2006). Higher sum scores indicate greater craving.
Data Analysis
The monetary and cocaine discounting tasks provided an indifference point (subjective value) for each delay or probability expressed as a proportion of the larger delayed/probabilistic reward. For the sexual tasks, the percentage scale value provided by the participant for each delay/probability was transformed to proportion (divided by 100). For each discounting task we applied a previously published criterion that flagged cases in which at least one delay (or odds-against) had a proportion value that was greater than the next lower delay (or odd-against) value by a magnitude of .2 (Johnson and Bickel 2008). This was done in order to characterize data orderliness, but no data were excluded from analyses. For each task the percentage of functions (for each participant within each dose condition) with systematic data (zero flagged values) was determined. For all discounting tasks, area-under-the-curve (AUC) was computed for each participant using proportion values at each delay or probability per Myerson et al. (2001) to provide an aggregate measure of discounting. In order to isolate the effect of delay on choices between unprotected vs. condom-protected sex in the sexual tasks, proportion values were standardized (i.e., divided by that participant’s value in the 0-delay condition) before AUC calculation. Probability was converted to odds-against for AUC calculation in the probability discounting tasks. Using AUC values for the discounting tasks, repeated measures ANOVA with planned comparisons (i.e., simple effects contrasts based on the F statistic) was used to examine the effects of cocaine dose on all study outcome measures. Pearson correlations examined relations between sexual desire ratings and AUC values from the sexual discounting tasks. Pearson correlations also examined the relation between CCQ-Brief scores and cocaine delay discounting AUC. For all pair-wise comparisons between dose conditions, effect size was calculated as Cohen’s d (Cohen, 1988) accounting for within-subjects correlations (Morris and DeShon, 2002). Analyses were performed using GraphPad Prism (version 6) and SPSS (version 23). For all analyses α was set at .05.
Results
Participant Characteristics
Of the 15 participants who qualified for drug administration, 12 participants completed the three drug administration sessions. Table 2 displays basic demographic information of study completers, including sex, race/ethnicity, marital status, tobacco smoking status, age, education, monthly income, cocaine use per month, reported instances of unprotected sex, and scores on the HIV Risk-taking Behavior Scale and Adult ADHD Self-Report Scale.
Table 2.
Basic demographics, drug use, and sexual behavior of the sample (n = 12).
| n (%) | Mean (SD) | ||
|---|---|---|---|
| Sex | Male | 8 (67) | |
| Female | 4 (33) | ||
| Race/ Ethnicity 1 | Caucasian/white | 8 (67) | |
| More than one race | 2 (17) | ||
| African American/Black | 2 (17) | ||
| Marital status | Single | 11 (92) | |
| Married | 1 (8) | ||
| Tobacco smoking status | Non-smoker | 2 (17) | |
| Smoker | 10 (83) | ||
| Age (years) | 27.25 (6.28) | ||
| Education (years) | 14.79 (1.74) | ||
| Monthly income (USD) | 1654.17 (1591.38) | ||
| Quick Test Score | 40.75 (3.84) | ||
| Cocaine uses per month | 5.00 (3.96) | ||
| Adult ADHD Self Report Scale 2 | Inattentive | 15.83 (4.76) | |
| Hyperactive/Impulsive | 15.00 (4.81) | ||
| HIV Risk-taking Behavior Scale 3 | Drug Use (Injection) | 1.58 (3.75) | |
| Sexual Behavior | 8.67 (4.56) | ||
| Unprotected sex | Lifetime unprotected sex due to unavailable condom4 |
8.55 (9.15) | |
| Number of unprotected sex partners past six months (From the BRAID 5) |
2.33 (2.57) |
Note.
One participant identified as Hispanic. The two participants who identified as more than one race both identified as Caucasian/white and African American/Black.
Score on the Adult ADHD Self Report Scale can range from 0–36 for each of the two subscales, with higher scores indicating greater ADHD symptoms.
Score on the HIV Risk-taking Behavior Scale can range from 0–30 on the Drug Use subscale and from 0–25 on the Sexual Behavior subscale, with higher scores indicating greater risk behavior.
One participant was excluded from the calculations of lifetime instances of unprotected sex because his response was provided as a percentage rather than a count (i.e., 80% of the time).
The Behavioral Risk Assessment for Infectious Diseases.
Subjective Drug Effects and Physiological Effects
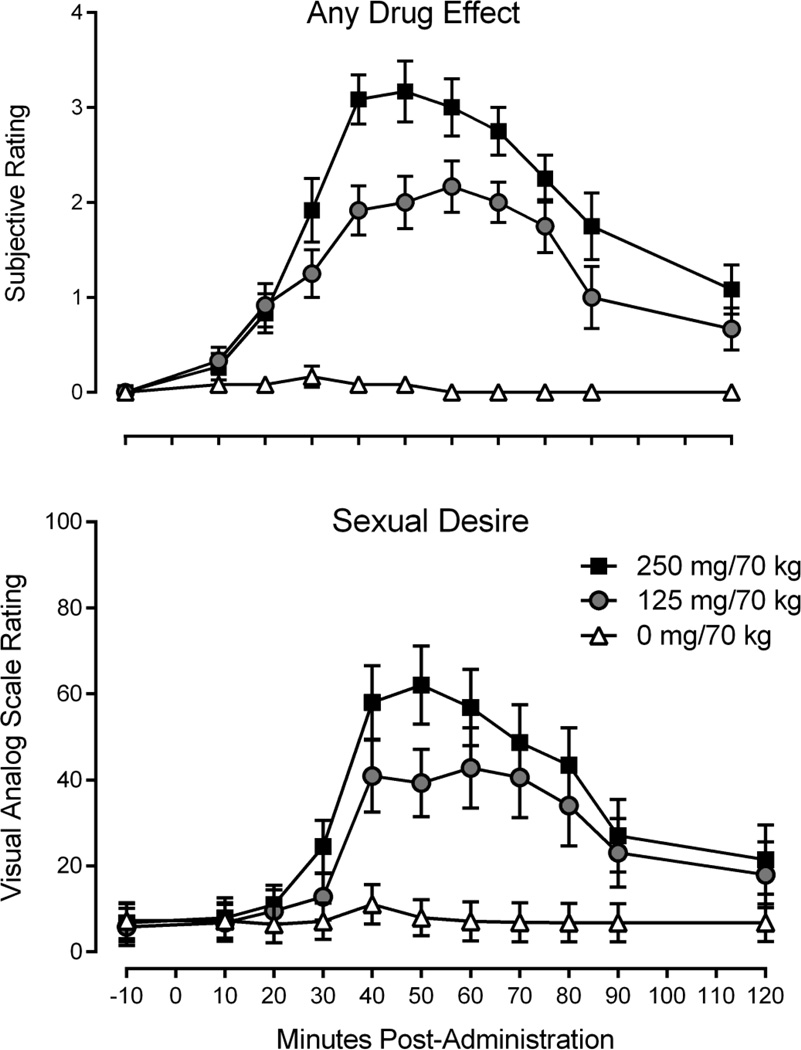
Table 3 summarizes mean peak subjective effects. In general, within-subjects contrasts revealed significantly higher peak ratings in both cocaine sessions relative to placebo, including peak ratings of sexual desire. Peak subjective effects ratings were also generally higher during 250 mg/70 kg sessions relative to 125 mg/70 kg sessions, including peak ratings of sexual desire. A timeline of subjective ratings of “any drug effect” and “sexual desire” as a function of cocaine dose is displayed in Figure 1. Table 4 summarizes mean peak physiological measures. Peak values for all measures were significantly higher in both cocaine sessions relative to placebo, and also significantly higher in 250 mg/70 kg sessions relative to 125 mg/70 kg sessions (with the exception of mean arterial pressure).
Table 3.
Means and standard deviations of peak subjective effects ratings
| Placebo | 125 mg/70 kg | 250 mg/70 kg | ||
|---|---|---|---|---|
| Any drug effect | 0.25 (0.45) | 2.25 (0.87)*** | 3.42 (0.79) *** | +++ |
| A rush | 0.17 (0.39) | 2.42 (0.90) *** | 3.33 (0.98) *** | ++ |
| Any good effects | 0.25 (0.45) | 2.42 (0.90) *** | 3.33 (0.78) *** | ++ |
| Any bad effects | 0.25 (0.45) | 0.75 (0.87) | 1.75 (1.42) ** | + |
| Any effects that you like | 0.25 (0.45) | 2.33 (0.98) *** | 3.33 (0.78) *** | ++ |
| High | 0.08 (0.29) | 2.25 (0.87) *** | 3.42 (0.79) *** | +++ |
| Drowsy/sleepy | 0.33 (0.89) | 0.67 (0.78) | 1.08 (1.24) | |
| Alert/energetic | 0.25 (0.62) | 2.58 (1.08) *** | 3.50 (0.90) *** | |
| Jittery | 0.25 (0.45) | 2.08 (1.08) *** | 2.75 (1.29) *** | |
| Calm/relaxed | 0.58 (1.16) | 1.33 (0.98) | 1.92 (1.08) * | + |
| Stimulated | 0.42 (0.67) | 2.50 (1.00) *** | 3.58 (0.79) *** | ++ |
| Sexual desire | 12.08 (15.69) | 50.42 (31.08) ** | 63.42 (32.19) *** | + |
Note. With the exception of sexual desire, participants rated items on a scale ranging from 0–4 (0 = Not at all, 1 = Possibly mild, but not sure, 2 = Definitely mild, 3 = Moderately, 4 = Strongly). Sexual desire was rated using a visual analog scale ranging from 0 to 100 (“None” and “Intense,” respectively). Peak subjective effects were calculated using the maximum value observed over the time course for each participant. Peak subjective effects were compared using repeated measures ANOVA with a within subjects factor of dose (three levels), and simple effects (based on the F statistic) contrasts comparing each dose.
Ratings at 125 and 250 mg/70 kg that are significantly different from placebo are indicated with
as p < .05,
as p < .01, and
as p < .001.
Ratings at which 125 and 250 mg/70 kg are significantly different are indicated with
as p < .05,
as p < .01, and
as p < .001. For comparisons between 250 mg/70kg and placebo, Cohen’s d ranged across measures from 0.64 to 4.80. For comparisons between 125 mg/70 kg and placebo, Cohen’s d ranged from 0.35 to 2.94. For comparisons between 250 and 125 mg/70 kg, Cohen’s d ranged from 0.37 to 1.64.
Figure 1.
Upper panel shows the time course of mean (±SEM) ratings for “any drug effect as the result of the pill” on a scale ranging from 0–4 (0 = Not At All, 1=Possibly mild, but not sure, 2=Definitely mild, 3=Moderately, 4=Strongly). Lower panel shows the time course of mean (±SEM) ratings of sexual desire on a visual analog scale ranging from 0 to 100 (“None” and “Intense,” respectively). See Table 1 for the timing of behavioral measures.
Table 4.
Means and standard deviations of peak physiological measures.
| Placebo | 125 mg/70 kg | 250 mg/70 kg | ||
|---|---|---|---|---|
| Systolic blood pressure | 120.67 (12.71) | 134.42 (13.03) *** | 143.92 (11.05) *** | ++ |
| Diastolic blood pressure | 69.17 (9.61) | 77.00 (12.00) ** | 81.67 (9.87) *** | + |
| Mean arterial pressure | 88.83 (11.99) | 98.00 (13.29) ** | 107.75 (15.25) ** | |
| Heart rate | 74.42 (9.93) | 92.92 (16.12) ** | 106.25 (14.97) *** | + |
Note. Peak physiological effects were calculated using the maximum value observed over the time course for each participant. Peak physiological measures were compared using repeated measures ANOVA with a within subjects factor of dose (three levels), and simple effects contrasts (based on the F statistic) comparing each dose.
Values at 125 and 250 mg/70 kg that are significantly different from placebo are indicated with
as p < .05,
as p < .01, and
as p < .001.
Values at which 125 and 250 mg/70 kg are significantly different are indicated with
as p < .05,
as p < .01, and
as p < .001. For comparisons between 250 mg/70kg and placebo, Cohen’s d ranged across measures from 1.19 to 2.23. For comparisons between 125 mg/70 kg and placebo, Cohen’s d ranged from 1.04 to 1.39. For comparisons between 250 and 125 mg/70 kg, Cohen’s d ranged from 0.65 to 0.97.
Discounting Task Orderliness
Discounting data were largely systematic across drug conditions; 89%, 97%, 100%, 97%, 100% of functions were systematic for the Sexual Delay Discounting Task, the Sexual Probability Discounting Task, the Monetary Delay Discounting Task, the Monetary Probability Discounting task, and the Cocaine Delay Discounting Task, respectively.
Sexual Delay Discounting Task
Sexual desire
Planned contrasts indicated significantly greater pre-task sexual desire in 250 mg/70 kg sessions vs. placebo sessions (means of 0.56 vs. 0.22, respectively, F(1,11)=10.67, p<0.01, Cohen’s d=01.08), and in 250 mg/70 kg sessions vs. 125 mg/70 kg sessions (means 0.56 vs. 0.41, respectively, F(1,11)=9.21,p=0.01, Cohen’s d=0.96). Sexual desire ratings in 125 mg/70 kg sessions tended be higher than placebo sessions, and these differences trended toward significance (means of 0.41 vs. 0.22, respectively, F(1,11)=4.74, p=0.05, Cohen’s d=0.65).
Condom use with no delay
Planned contrasts revealed that participants did not report significantly lower likelihoods of using an immediately available condom during 250 mg/70 kg sessions relative to placebo (Means of .80 vs. .82, respectively, F(1,11)=.05, p=.83, Cohen’s d=0.06), during 125 mg/70 kg sessions relative to placebo (Means of .87 vs. .82, respectively, F(1,11)=.22, p = .65, Cohen’s d=0.14), or during 250 mg/70 kg sessions relative to 125 mg/70 kg sessions (Means of .80 vs. .87, respectively, F(1,11)=.54, p = .48, Cohen’s d=0.22).
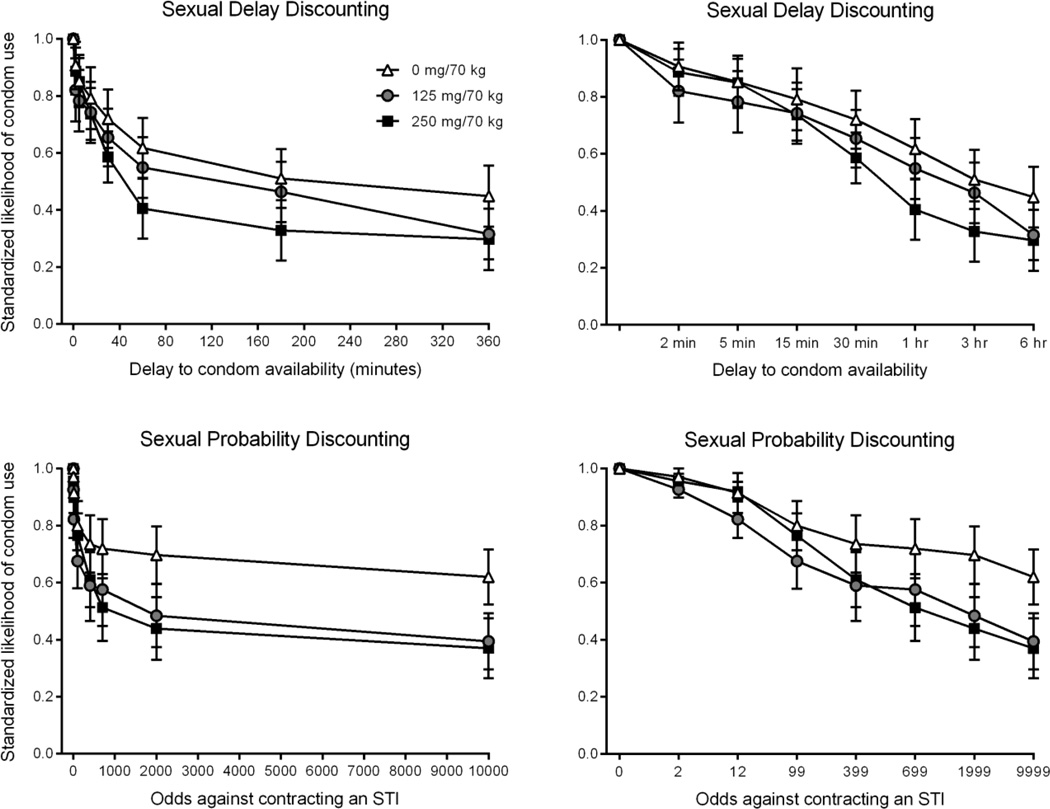
Delay discounting of condom-protected sex
The upper panels of Figure 2 show mean standardized likelihood of condom use as a function of delay and cocaine dose. Planned contrasts showed significantly greater AUC (i.e., less discounting) in placebo sessions relative to 250 mg/70 kg sessions (Means of 0.55 vs. 0.38, respectively, F(1,11)=6.16, p=0.03, Cohen’s d=0.72). Although AUC was greatest in the placebo condition, intermediate in the 125 mg/70 kg condition, and least in the 250 mg/70 kg condition as hypothesized, the differences between placebo sessions and 125 mg/70 kg sessions did not reach significance (Means of 0.55 vs. 0.48, respectively, F(1,11)=2.00, p=0.19, Cohen’s d=0.37), and the difference between the 125 mg/70 kg sessions relative to 250 mg/70 kg sessions did not reach significance (Means of 0.48 vs. 0.38, respectively, F(1,11)=1.49, p=0.25, Cohen’s d=0.37). AUC was not significantly correlated with pre-task sexual desire ratings in any session (r value range: −.47 to .24 all p values > 0.12).
Figure 2.
Upper panels show Sexual Delay Discounting Task data, and lower panels show Sexual Probability Discounting Task data. Left panels show delays or odds against displayed on a linear x-axis, allowing for curve shape assessment. Right panels show delays or odds against displayed on an x-axis with each value spaced equidistantly to facilitate inspection of all values (with x-axis labels showing specific values assessed). All panels show mean (±SEM) standardized likelihood of condom use (proportion of VAS).
Sexual Probability Discounting Task
Sexual desire
Planned contrasts indicated significantly greater pre-task sexual desire in 250 mg/70 kg sessions vs. placebo sessions (means of 59.75 vs. 13.42, respectively, F(1,11)=25.67, p <0.001, Cohen’s d=1.57), 125mg/70kg vs. placebo sessions (means of 44.16 vs. 13.42, respectively, F(1,11)=14.94, p=.002, Cohen’s d=1.20), and in 250 mg/70 kg sessions vs. 125 mg/70 kg sessions (means 59.75 vs. 44.16, respectively, F(1,11)=7.19,p=0.02, Cohen’s d=0.77).
Condom use with a 100% chance of STI contraction
Planned contrasts showed that participants did not report significantly lower likelihoods of using a condom given a 100% chance of STI contraction during 125 mg/70 kg sessions relative to placebo (Means of .94 vs. .98 proportion visual analog scale, F(1,11)=.73, p=.41, Cohen’s d=0.32), during 250 mg/70 kg sessions relative to placebo sessions (Means of .94 vs. .98, F(1,11)=.41, p=.54, Cohen’s d=0.23), or during 250 mg/70 kg sessions relative to 125 mg/70 kg sessions (Means of .94 vs. .94, F(1,11)=.00, p = .99, Cohen’s d=0.01).
Probability discounting of condom-protected sex
The lower panels of Figure 2 show mean standardized likelihood values as a function of STI risk and cocaine dose. Planned contrasts indicated significantly greater AUC in placebo sessions relative to 250 mg/70 kg sessions (means of 0.66 vs. 0.39, respectively, F(1,11)=9.32, p=0.01, Cohen’s d=0.88), and significantly greater AUC in placebo sessions relative to 125 mg/70 kg sessions (Means of 0.66 vs. 0.45, respectively, F(1,11)=7.92, p=0.02, Cohen’s d=0.83). AUC was greater in 125 mg/70 kg relative to 250 mg/70 kg sessions, although this was not significant (Means of 0.45 vs. 0.39, respectively, F(1,11)=1.06, p=0.33, Cohen’s d=0.30). AUC was not significantly correlated with pre-task sexual desire ratings in any session (r value range: −.17 to −.06; all p values > 0.60).
Money Delay Discounting Task
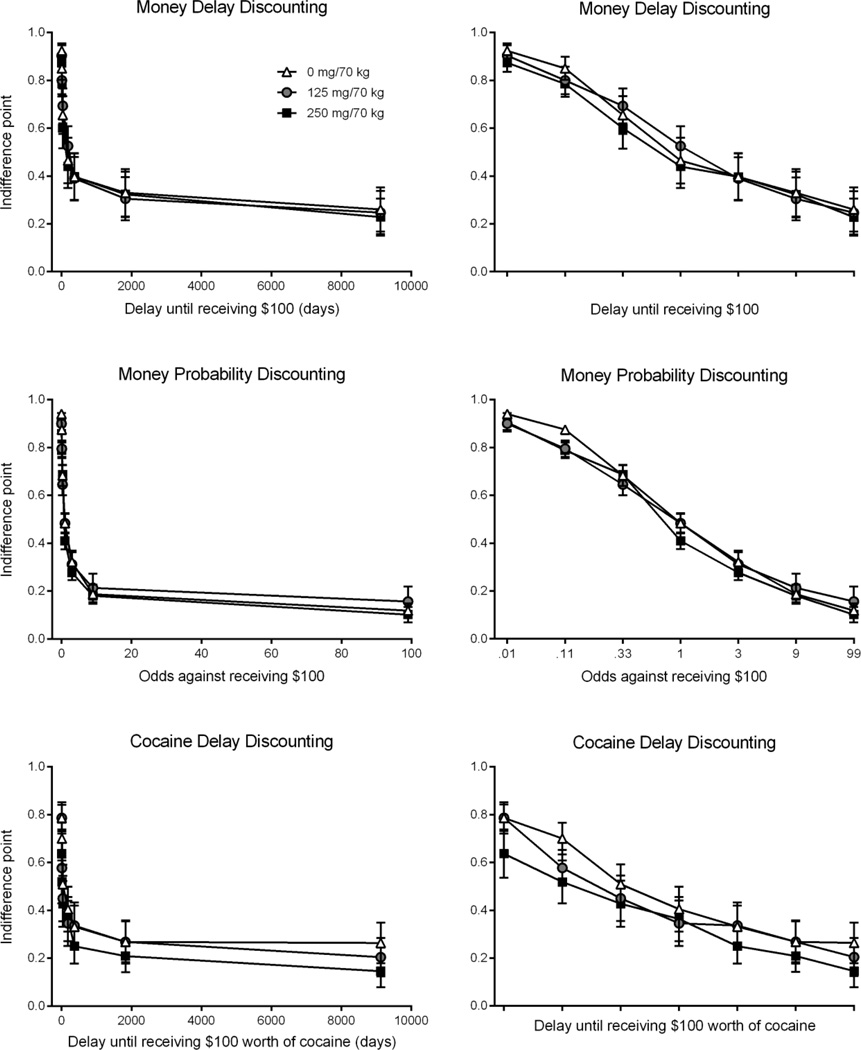
The upper panels of Figure 3 show monetary delay discounting results. Planned contrasts revealed no significant differences in AUC between placebo, 125 mg/70 kg, and 250 mg/70 kg sessions (Means of 0.32, 0.30, and 0.30, respectively, all p values > 0.37, Cohen’s d range: 0.01–0.16).
Figure 3.
Upper panels show monetary delay discounting results, middle panels show monetary probability discounting results, and lower panels show cocaine delay discounting results. Left panels show delays or odds against displayed on a linear x-axis, allowing for curve shape assessment. Right panels show delays or odds against displayed on an x-axis with each value spaced equidistantly to facilitate inspection of all values (with x-axis labels showing specific delays/probabilities assessed). All panels show mean (±SEM) standardized likelihood of condom use (proportion of visual analog scale).
Money Probability Discounting Task
The middle panels of Figure 3 show monetary probability discounting results. Planned contrasts indicated no significant differences in AUC between placebo, 125 mg/70 kg, and 250 mg/70 kg sessions (Means of 0.17, 0.20, and 0.16, respectively, all p values >0.28, Cohen’s d range: 0.19–0.52).
Cocaine Craving Questionnaire
Planned contrasts indicated significantly greater craving according to CCQ-Brief scores in 250 mg/70 kg sessions relative to placebo (means of 0.52 vs. 0.20, respectively, F(1,11)=29.25, p<0.01, Cohen’s d=2.17), and significantly greater craving in 125 mg/70 kg sessions relative to placebo (means of 0.52 vs. 0.20, respectively, F(1,11)=53.83, p<0.01, Cohen’s d=1.65). There were no significant differences in craving between 125 mg/70 kg and 250 mg/70 kg sessions (means of 0.52 for both doses, F=0.01, p=0.95, Cohen’s d=0.02).
Cocaine Delay Discounting Task
Data for one participant was missing due to experimenter error. The lower panels of Figure 3 show the discounting of delayed cocaine (using choices between immediate and delayed cocaine rewards). Planned contrasts showed AUC to be greatest in the placebo condition, intermediate in the 125 mg/70 kg condition, and least in the 250 mg/70 kg condition as hypothesized. However, these differences did not reach significance (Means of 0.26, 0.24, and 0.18, respectively, all p values > 0.13, Cohen’s d range: 0.19–0.51). AUC in the cocaine delay discounting task was significantly and negatively correlated with scores on the CCQ-Brief for the placebo session (r=−0.62, p=0.04), indicating that higher cocaine craving was associated with steeper discounting of cocaine. Discounting of cocaine and CCQ-Brief scores were not significantly correlated for the 125 mg/70 kg (r=−0.05, p=0.89) or 250 mg/70 kg sessions (r=0.06, p=0.85).
Discussion
This is the first experimental laboratory study with results suggesting that cocaine administration may play a causal role in condom use decisions. Moreover, it is the first laboratory study identifying potential behavioral mechanisms by which cocaine acutely sets the occasion for sexual risk behavior, i.e., sexual desire, delay discounting, and probability discounting. The major results of this study are that: 1) Cocaine administration caused dose-dependent increases in sexual desire and in sexual delay and probability discounting; 2) In contrast to sexual tasks, cocaine administration caused no significant increases in delay and probability discounting of money, and delay discounting of cocaine; 3) Cocaine administration caused dose-dependent increases in ratings of cocaine craving; 4) Cocaine administration caused dose-dependent increases in prototypical stimulant and abuse-liability-related subjective effects. Each result will be discussed, followed by study limitations and overall conclusions.
Despite decades of research linking cocaine use and sexual risk behavior (e.g., Booth et al. 1993), the present study is the first to show that cocaine administration causes significant and orderly dose-related and time-related increases in sexual desire ratings under double-blind laboratory conditions. This is also the first study to show that cocaine administration causes significant decreases in reported condom use likelihood under some conditions. A previous study found that intravenous but not oral administration of methylphenidate (pharmacologically similar to cocaine) significantly increased sexual desire ratings (Volkow et al. 2007). No attempt was reported to calibrate the two different doses used for intravenous and oral routes, so it is unknown if differential effects were due to route or dose. The present results showing that cocaine increases sexual desire may have profound implications for the connection between cocaine and sexual risk behavior that should be examined in future research.
Cocaine administration did not significantly decrease reported condom use likelihood under ideal circumstances of immediate condom availability. Rather, cocaine administration decreased reported condom use likelihood specifically when condom-protected sex was delayed (typical of naturalistic casual sex scenarios). Moreover, cocaine administration did not significantly decrease reported condom use likelihood under circumstances in which contracting an STI from one’s partner was certain. Rather, cocaine administration decreased reported likelihood of condom use specifically when the risk of STI contraction was uncertain. These data indicate that cocaine administration exacerbates the already detrimental effects of delay or STI contraction improbability on reported condom use likelihood. Had we only assessed condom use likelihood in the absence of delay or when STI contraction was certain, our conclusion would have been that cocaine administration does not affect condom use likelihood. This highlights not only the importance of considering delay and probability discounting processes in real-life risk scenarios, but also the possibility that other environmental parameters (e.g., financial cost of condoms; likelihood of erection failure when applying condom) might also play critical roles in condom use decisions. Perhaps the most important implication of these findings is that condom availability is critical during cocaine use in order to prevent risk behavior and STI transmission.
Given that cocaine administration increased sexual desire and decreased condom use likelihood as measured by the sexual discounting tasks, we examined relations between sexual desire and AUC in the sexual discounting tasks, reasoning that greater sexual desire might shift preference toward immediate unprotected sex. Although the lack of significant relation between sexual desire ratings and AUC does not support a mediating role of sexual desire in the link between cocaine administration and decreased condom use likelihood, this may be due to a relatively small sample size, as 100 or more participants are generally considered appropriate for mediation analyses with reliable measures (Hoyle and Kenny 1999). Future research with larger sample sizes may further examine a potential mediating role of sexual desire.
In contrast to the effects of cocaine administration on sexual delay and probability discounting, cocaine administration had no significant effect on monetary delay or probability discounting. This same general pattern was evident in our recent research examining the acute effects of alcohol (Johnson et al. 2016). Specifically, alcohol administration significantly increased delay and probability discounting of condom-protected sex (i.e., decreased condom use under conditions involving delay or STI contraction uncertainty), but had no effect on delay discounting of money and caused small but significant decreases in probability discounting of money. Aside from this commonality regarding acute effects, a growing literature has shown other examples of domain-dependent effects in delay discounting (Dariotis and Johnson 2015; Johnson and Bruner 2012; Lawyer and Schoepflin 2013; Rasmussen et al. 2010; Schiff et al. 2015). As an example, research suggests that sexual delay discounting, compared to monetary delay discounting, is more strongly related to self-reported sexual risk behavior (Johnson and Bruner 2012). One hypothesis might be that cocaine acutely increases the delay discounting of biologically relevant outcomes but not money. However, this hypothesis is not supported by the lack of significant effect of cocaine administration on cocaine delay discounting.
Cocaine administration significantly increased ratings of cocaine craving, consistent with previous results (e.g., Haberny et al. 1995; Jaffe et al. 1989; Nann-Vernotica et al. 2001), and is consistent with binge use patterns common with cocaine (O’Brien 2011). That is, increases in cocaine craving are consistent with the notion that cocaine effects may set the occasion for additional cocaine administration, constituting a positive feedback loop. We examined relations between cocaine craving and cocaine discounting, reasoning that greater cocaine craving might shift preference toward immediate cocaine even if the amount is small. In the placebo session, higher cocaine craving was associated with steeper discounting of cocaine. However, this relation was not significant in the two active dose conditions, leaving the relation between cocaine craving and cocaine discounting ambiguous.
The study showed cocaine to cause significant dose-related increases in abuse-liability subjective effects such as “high” and “good effects”, and in other subjective effects typical of cocaine (e.g., “stimulated”) (e.g. Smith et al. 2001). The study also replicated increases in heart rate, systolic and diastolic blood pressure. Our replication of these prototypical cocaine effects supports the present study’s ability to detect multiple known drug effects, and therefore the study’s likely ability to detect novel effects (e.g. discounting tasks). Moreover, the percentage of systematic discounting functions compares favorably to previous studies (e.g., Johnson 2012; Johnson and Bruner 2012; Johnson et al. 2015a), providing confidence in discounting results.
Several limitations should be noted. First, the discounting tasks used hypothetical rather than real consequences. Although the results suggest that acute cocaine administration decreases likelihood of delayed condom use in casual sex scenarios, sexual risk behavior was not directly assessed. However, studies have generally shown real and hypothetical monetary outcomes to result in similar discounting functions (Baker et al. 2003; Bickel et al. 2009; Green and Lawyer 2014; Johnson and Bickel 2002; Johnson et al. 2007; Lagorio et al. 2005; Lawyer et al. 2011; Madden et al. 2003; Madden et al. 2004; Matusiewicz et al. 2013). Moreover, the Sexual Delay Discounting Task has shown reliability and significant correlations with self-reported sexual risk behavior (Dariotis and Johnson 2015; Herrmann et al. 2015; Johnson and Bruner 2012). These correlations suggest that sexual delay discounting may contribute to sexual risk behavior (although it should be noted that the aforementioned validity and reliability research was conducted using different delays in the Sexual Delay Discounting Task). Another limitation is that cocaine is typically not used by the oral route. However, the oral route maximized the credibility of the blind relative to intranasal or smoked route, and has been successfully used in laboratory research, showing qualitatively similarity to intravenous cocaine (Smith et al. 2001). Our participants were predominantly young, Caucasian/white, intranasal cocaine users who met diagnostic criteria for cocaine use disorders. Although it was not an inclusion requirement, every single participant anecdotally reported having unprotected sex specifically because they did not have a condom immediately available at multiple times in the lifetime, demonstrating clinical relevance. Nonetheless, cocaine effects might differ for other groups such as those who consistently use condoms or those who may be better characterized as recreational users (i.e., do not meet cocaine use disorder criteria). Another limitation is that the various discounting tasks were assessed at fixed times post-administration. Therefore, differences across the time course of drug effects may account for why sexual but not money tasks were affected by cocaine administration. However, the fact that money probability discounting was assessed near peak subjective effects and yet showed no cocaine effect is not consistent with this interpretation. Another potential limitation is that different delays and probabilities were used across the money and sexual versions of discounting tasks. Although orderly data showing evidence of discounting was obtained with all tasks, it remains possible that the different delays and probabilities may have accounted for differences in results. A final limitation is that the credibility of the blind for oral cocaine administration was not formally assessed, although we judge the possibility of blinding via non-pharmacological effects (e.g., taste) to be low given that cocaine or placebo was administered by capsule.
Overall, this study has provided the most comprehensive examination to-date of the potential behavioral mechanisms linking cocaine use to sexual risk behavior. Cocaine administration may create ideal conditions for occasioning risk behavior by acutely increasing three (perhaps interactive) behavioral processes: sexual desire, sexual delay discounting (detrimental effect of delay on condom use), and sexual probability discounting (detrimental effect of STI improbability on condom use). Future research should determine possible interactions among these potential mechanisms. Moreover, STI prevention efforts, including harm-reduction efforts for cocaine users, should take these processes into account as potential contributors to cocaine-related sexual risk behavior.
Acknowledgments
This work was supported by the National Institute on Drug Abuse (NIDA) through R01DA032363, R01DA035277 and T32DA007209. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
All authors declare that they have no conflict of interest.
References
- Ammons RB, Ammons CH. Quick Test (QT): Provisional manual. Psychol Rep. 1962;11:111–161. [Google Scholar]
- Baker F, Johnson MW, Bickel WK. Delay discounting in current and never-before cigarette smokers: Similarities and differences across commodity, sign, and magnitude. J Abnorm Psychol. 2003;112:382–392. doi: 10.1037/0021-843x.112.3.382. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–677. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Pitcock JA, Yi R, Angtuaco EJ. Congruence of BOLD response across intertemporal choice conditions: Fictive and real money gains and losses. J Neurosci. 2009;29:8839–8846. doi: 10.1523/JNEUROSCI.5319-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski CF, Chitwood DD. Sex related HIV risk behaviors: Differential risks among injection drug users, crack smokers, and injection drug users who smoke crack. Drug Alcohol Depend. 2000;58:219–226. doi: 10.1016/s0376-8716(99)00094-0. [DOI] [PubMed] [Google Scholar]
- Booth RE, Watters JK, Chitwood DD. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. Am J Public Health. 1993;83:1144–1148. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bux DA, Lamb RJ, Iguchi MY. Cocaine use and HIV risk behavior in methadone maintenance patients. Drug Alcohol Depend. 1995;37:29–35. doi: 10.1016/0376-8716(94)01058-s. [DOI] [PubMed] [Google Scholar]
- Chan SK, Thornton LR, Chronister KJ, Meyer J, Wolverton M, Johnson CK, Arafat RR, Joyce PM, Switzer WM, Heneine W, Shankar A, Granade T, Owen MS, Sprinkle P, Sullivan V Centers for Disease Control and Prevention (CDC) Likely female-to-female sexual transmission of HIV--Texas, 2012. MMWR Morb Mortal Wkly Rep. 2014;63:209–212. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Celum C, Chesney M, Huang Y, Mayer K, Bozeman S, Judson FN, Bryant KJ, Coates TJ EXPLORE Study Team. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Dandy KL, Gatch MB. The effects of chronic cocaine exposure on impulsivity in rats. Behav Pharmacol. 2009;20:400–405. doi: 10.1097/FBP.0b013e328330ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dariotis JK, Johnson MW. Sexual discounting among high-risk youth ages 18–24: implications for sexual and substance use risk behaviors. Exp Clin Psychopharmacol. 2015;23:49–58. doi: 10.1037/a0038399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behavior among intravenous drug users. AIDS. 1991;5:181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Dunn KE, Barrett FS, Herrmann ES, Plebani JG, Sigmon SC, Johnson MW. Behavioral Risk Assessment for Infectious Diseases (BRAID): Self-report instrument to assess injection and noninjection risk behaviors in substance users. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2016.07.032. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlin BR, Irwin KL, Faruque S, McCoy CB, Word C, Serrano Y, Inciardi JA, Bowser BP, Schilling RF, Holmberg SD. Intersecting epidemics--crack cocaine use and HIV infection among inner-city young adults. Multicenter Crack Cocaine and HIV Infection Study Team. N Engl J Med. 1994;331:1422–1427. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- Edwards JM, Halpern CT, Wechsberg WM. Correlates of exchanging sex for drugs or money among women who use crack cocaine. AIDS Educ Prev. 2006;18:420–429. doi: 10.1521/aeap.2006.18.5.420. [DOI] [PubMed] [Google Scholar]
- George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, Hendershot CS, Kajumulo KF. Indirect effects of acute alcohol intoxication on sexual risk-taking: The roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38:498–513. doi: 10.1007/s10508-008-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green RM, Lawyer SR. Steeper delay and probability discounting of potentially real versus hypothetical cigarettes (but not money) among smokers. Behav Processes. 2014;108:50–56. doi: 10.1016/j.beproc.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Grella CE, Anglin MD, Wugalter SE. Cocaine and crack use and HIV risk behaviors among high-risk methadone maintenance clients. Drug Alcohol Depend. 1995;37:15–21. doi: 10.1016/0376-8716(94)01059-t. [DOI] [PubMed] [Google Scholar]
- Haberny KA, Walsh SL, Ginn DH, Wilkins JN, Garner JE, Setoda D, Bigelow GE. Absence of acute cocaine interactions with the MAO-B inhibitor selegiline. Drug Alcohol Depend. 1995;39:55–62. doi: 10.1016/0376-8716(95)01137-n. [DOI] [PubMed] [Google Scholar]
- Hall HI, An Q, Tang T, Song R, Chen M, Green T, Kang J Centers for Disease Control and Prevention (CDC) Prevalence of Diagnosed and Undiagnosed HIV Infection--United States, 2008–2012. MMWR Morb Mortal Wkly Rep. 2015;64:657–662. [PMC free article] [PubMed] [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addict Behav. 2006;31:1290–1294. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Heil SH, Sigmon SC, Mongeon JA, Higgins ST. Characterizing and improving HIV/AIDS knowledge among cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2005;13:238–243. doi: 10.1037/1064-1297.13.3.238. [DOI] [PubMed] [Google Scholar]
- Herrmann ES, Hand DJ, Johnson MW, Badger GJ, Heil SH. Examining delay discounting of condom-protected sex among opioid-dependent women and non-drug-using control women. Drug Alcohol Depend. 2014;144:53–60. doi: 10.1016/j.drugalcdep.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann ES, Heil SH, Sigmon SC, Dunn KE, Washio Y, Higgins ST. Characterizing and improving HIV/AIDS knowledge among cocaine-dependent outpatients using modified materials. Drug Alcohol Depend. 2013;127:220–225. doi: 10.1016/j.drugalcdep.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann ES, Johnson PS, Johnson MW. Examining Delay Discounting of Condom-Protected Sex Among Men Who Have Sex with Men Using Crowdsourcing Technology. AIDS Behav. 2015;19:1655–1665. doi: 10.1007/s10461-015-1107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman JA, Klein H, Eber M, Crosby H. Frequency and intensity of crack use as predictors of women's involvement in HIV-related sexual risk behaviors. Drug Alcohol Depend. 2000;58:227–236. doi: 10.1016/s0376-8716(99)00095-2. [DOI] [PubMed] [Google Scholar]
- Hoyle RHKD. Sample size, reliability, and tests of statistical mediation. In: Hoyle RHe., editor. Statistical strategies for small sample research. Thousand Oaks, CA: Sage; 1999. pp. 195–222. [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, Przybeck T. The use of the DSM-III-R Checklist for initial diagnostic assessments. Compr Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Jaffe JH, Cascella NG, Kumor KM, Sherer MA. Cocaine-induced cocaine craving. Psychopharmacology (Berl) 1989;97:59–64. doi: 10.1007/BF00443414. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD. HIV risks, gender, and cocaine use among opiate users. Drug Alcohol Depend. 1995;37:23–28. doi: 10.1016/0376-8716(94)01030-o. [DOI] [PubMed] [Google Scholar]
- Johnson MW. An efficient operant choice procedure for assessing delay discounting in humans: initial validation in cocaine-dependent and control individuals. Exp Clin Psychopharmacol. 2012;20:191–204. doi: 10.1037/a0027088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. J Exp Anal Behav. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Exp Clin Psychopharmacol. 2008;16:264–274. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F. Moderate drug use and delay discounting: a comparison of heavy, light, and never smokers. Exp Clin Psychopharmacol. 2007;15:187–194. doi: 10.1037/1064-1297.15.2.187. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. The Sexual Discounting Task: HIV risk behavior and the discounting of delayed sexual rewards in cocaine dependence. Drug Alcohol Depend. 2012;123:15–21. doi: 10.1016/j.drugalcdep.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. Test-retest reliability and gender differences in the sexual discounting task among cocaine-dependent individuals. Exp Clin Psychopharmacol. 2013;21:277–286. doi: 10.1037/a0033071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR, Johnson PS. Cocaine dependent individuals discount future rewards more than future losses for both cocaine and monetary outcomes. Addict Behav. 2015b;40:132–136. doi: 10.1016/j.addbeh.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Griffiths RR. Comparative abuse liability of GHB and ethanol in humans. Exp Clin Psychopharmacol. 2013;21:112–123. doi: 10.1037/a0031692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Johnson PS, Herrmann ES, Sweeney MM. Delay and probability discounting of sexual and monetary outcomes in individuals with cocaine use disorders and matched controls. PLoS One. 2015a;10:e0128641. doi: 10.1371/journal.pone.0128641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Strain EC, Griffiths RR. Effects of oral caffeine pretreatment on response to intravenous nicotine and cocaine. Exp Clin Psychopharmacol. 2010;18:305–315. doi: 10.1037/a0020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PS, Sweeney MM, Herrmann ES, Johnson MW. Alcohol Increases Delay and Probability Discounting of Condom-Protected Sex: A Novel Vector for Alcohol-Related HIV Transmission. Alcohol Clin Exp Res. 2016;40:1339–1350. doi: 10.1111/acer.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, Woods JH. Individual differences in discount rate are associated with demand for self-administered cocaine, but not sucrose. Addict Biol. 2013;18:8–18. doi: 10.1111/j.1369-1600.2011.00361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagorio CH, Madden GJ. Delay discounting of real and hypothetical rewards III: steady-state assessments, forced-choice trials, and all real rewards. Behav Processes. 2005;69:173–187. doi: 10.1016/j.beproc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Schoepflin FJ. Predicting domain-specific outcomes using delay and probability discounting for sexual versus monetary outcomes. Behav Processes. 2013;96:71–78. doi: 10.1016/j.beproc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Schoepflin F, Green R, Jenks C. Discounting of hypothetical and potentially real outcomes in nicotine-dependent and nondependent samples. Exp Clin Psychopharmacol. 2011;19:263–274. doi: 10.1037/a0024141. [DOI] [PubMed] [Google Scholar]
- Logue AW, Tobin H, Chelonis JJ, Wang RY, Geary N, Schachter S. Cocaine decreases self-control in rats: a preliminary report. Psychopharmacology (Berl) 1992;109:245–247. doi: 10.1007/BF02245509. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Exp Clin Psychopharmacol. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Raiff BR, Lagorio CH, Begotka AM, Mueller AM, Hehli DJ, Wegener AA. Delay discounting of potentially real and hypothetical rewards: II. Between- and within-subject comparisons. Exp Clin Psychopharmacol. 2004;12:251–261. doi: 10.1037/1064-1297.12.4.251. [DOI] [PubMed] [Google Scholar]
- Malow RM, West JA, Corrigan SA, Pena JM, Cunningham SC. Outcome of psychoeducation for HIV risk reduction. AIDS Educ Prev. 1994;6:113–125. [PubMed] [Google Scholar]
- Matusiewicz AK, Carter AE, Landes RD, Yi R. Statistical equivalence and test-retest reliability of delay and probability discounting using real and hypothetical rewards. Behav Processes. 2013;100:116–122. doi: 10.1016/j.beproc.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14:535–542. doi: 10.1016/j.annepidem.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Mendez IA, Simon NW, Hart N, Mitchell MR, Nation JR, Wellman PJ, Setlow B. Self-administered cocaine causes long-lasting increases in impulsive choice in a delay discounting task. Behav Neurosci. 2010;124:470–477. doi: 10.1037/a0020458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7:105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- Myerson J, Green L, Warusawitharana M. Area under the curve as a measure of discounting. J Exp Anal Behav. 2001;76:235–243. doi: 10.1901/jeab.2001.76-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nann-Vernotica E, Donny EC, Bigelow GE, Walsh SL. Repeated administration of the D1/5 antagonist ecopipam fails to attenuate the subjective effects of cocaine. Psychopharmacology (Berl) 2001;155:338–347. doi: 10.1007/s002130100724. [DOI] [PubMed] [Google Scholar]
- O'Brien CP. Drug Addiction; Goodman & Gilman's Pharmacologic Basis for Therapeutics. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman & Gilman's Pharmacologic Basis for Therapeutics. New York: McGraw-Hill; 2011. [Google Scholar]
- Perry JL, Larson EB, German JP, Madden GJ, Carroll ME. Impulsivity (delay discounting) as a predictor of acquisition of IV cocaine self-administration in female rats. Psychopharmacology (Berl) 2005;178:193–201. doi: 10.1007/s00213-004-1994-4. [DOI] [PubMed] [Google Scholar]
- Perry JL, Nelson SE, Carroll ME. Impulsive choice as a predictor of acquisition of IV cocaine self- administration and reinstatement of cocaine-seeking behavior in male and female rats. Exp Clin Psychopharmacol. 2008;16:165–177. doi: 10.1037/1064-1297.16.2.165. [DOI] [PubMed] [Google Scholar]
- Prendergast ML, Urada D, Podus D. Meta-analysis of HIV risk-reduction interventions within drug abuse treatment programs. J Consult Clin Psychol. 2001;69:389–405. doi: 10.1037//0022-006x.69.3.389. [DOI] [PubMed] [Google Scholar]
- Rachlin H, Raineri A, Cross D. Subjective probability and delay. J Exp Anal Behav. 1991;55:233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen EB, Lawyer SR, Reilly W. Percent body fat is related to delay and probability discounting for food in humans. Behav Processes. 2010;83:23–30. doi: 10.1016/j.beproc.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Rendina HJ, Moody RL, Ventuneac A, Grov C, Parsons JT. Aggregate and event-level associations between substance use and sexual behavior among gay and bisexual men: Comparing retrospective and prospective data. Drug Alcohol Depend. 2015;154:199–207. doi: 10.1016/j.drugalcdep.2015.06.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesch MR, Calu DJ, Schoenbaum G. Dopamine neurons encode the better option in rats deciding between differently delayed or sized rewards. Nat Neurosci. 2007;10:1615–1624. doi: 10.1038/nn2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff S, Amodio P, Testa G, Nardi M, Montagnese S, Caregaro L, di Pellegrino G, Sellitto M. Impulsivity toward food reward is related to BMI: Evidence from intertemporal choice in obese and normal-weight individuals. Brain Cogn. 2015 doi: 10.1016/j.bandc.2015.10.001. [DOI] [PubMed] [Google Scholar]
- Semaan S, Des Jarlais DC, Sogolow E, Johnson WD, Hedges LV, Ramirez G, Flores SA, Norman L, Sweat MD, Needle R. A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. J Acquir Immune Defic Syndr. 2002;30(Suppl 1):S73–S93. [PubMed] [Google Scholar]
- Setlow B, Mendez IA, Mitchell MR, Simon NW. Effects of chronic administration of drugs of abuse on impulsive choice (delay discounting) in animal models. Behav Pharmacol. 2009;20:380–389. doi: 10.1097/FBP.0b013e3283305eb4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon NW, Mendez IA, Setlow B. Cocaine exposure causes long-term increases in impulsive choice. Behav Neurosci. 2007;121:543–549. doi: 10.1037/0735-7044.121.3.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith BJ, Jones HE, Griffiths RR. Physiological, subjective and reinforcing effects of oral and intravenous cocaine in humans. Psychopharmacology (Berl) 2001;156:435–444. doi: 10.1007/s002130100740. [DOI] [PubMed] [Google Scholar]
- Sobel BF, Sigmon SC, Griffiths RR. Transdermal nicotine maintenance attenuates the subjective and reinforcing effects of intravenous nicotine, but not cocaine or caffeine, in cigarette-smoking stimulant abusers. Neuropsychopharmacology. 2004;29:991–1003. doi: 10.1038/sj.npp.1300415. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80:iii7–ii14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussner BD, Smelson DA, Rodrigues S, Kline A, Losonczy M, Ziedonis D. The validity and reliability of a brief measure of cocaine craving. Drug Alcohol Depend. 2006;83:233–237. doi: 10.1016/j.drugalcdep.2005.11.022. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Telang F, Jayne M, Wong C. Stimulant-induced enhanced sexual desire as a potential contributing factor in HIV transmission. Am J Psychiatry. 2007;164:157–160. doi: 10.1176/ajp.2007.164.1.157. [DOI] [PubMed] [Google Scholar]
- Winhusen TM, Somoza EC, Lewis DF, Kropp F, Theobald J, Elkashef A. An Evaluation of Substance Abuse Treatment and HIV Education on Safe Sex Practices in Cocaine Dependent Individuals. ISRN Addict. 2014;2014:912863. doi: 10.1155/2014/912863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi R, Johnson MW, Bickel WK. Relationship between cooperation in an iterated prisoner's dilemma game and the discounting of hypothetical outcomes. Learn Behav. 2005;33:324–336. doi: 10.3758/bf03192861. [DOI] [PubMed] [Google Scholar]