Abstract
Key points
Habit cough is most commonly characterised by a repetitive loud barking cough that persists for prolonged periods.
The cough interferes with normal activity and substantially decreases the quality of life.
The sine qua non is the total absence of this troublesome cough once asleep.
The age distribution ranges from 4 years to late adolescence, with 85% of cases occurring from 8 to 14 years of age; similar cough in adults is much less common and poorly characterised.
Pharmacological treatment is ineffective.
A simple behavioural approach called suggestion therapy has been applied with success by many physicians.
The natural history in the absence of treatment can result in persistence for months to years.
Educational aims
To increase awareness of functional cough as a non-organically caused symptom in children and adolescents.
To provide the means of diagnosing a functional cough based on the distinguishing characteristics of this cause of chronic cough.
To understand the principles of treating a functional cough with a simple behavioural technique called suggestion therapy.
Summary
Involuntary cough without an identified underlying organic reason has been given various names and recommended treatments. Current experience in children and adolescents suggests that “habit cough” best describes this entity, and suggestion therapy is a highly effective treatment that most physicians can learn.
Short abstract
Diagnosis of the functional disorder called habit cough can be readily made by the unique clinical characteristics http://ow.ly/Al5B3094oxj
Cough is a common symptom; one that results in many visits to physicians. Most commonly, cough is a manifestation of acute bronchitis from a viral respiratory infection, and lasts for one to three weeks. The term chronic cough is used when coughing persists longer than 4 weeks [1]. Chronic cough can be from well-defined disorders such as tuberculosis, cystic fibrosis and primary ciliary dyskinesia, but the differential diagnosis can be extensive, including common and uncommon disorders [2]. A management pathway has been proposed as an effective means for evaluating chronic cough in children [3] and such pathways or algorithms have been found useful by a panel of selected members of the American College of Chest Physicians [4].
In considering the differential diagnosis of chronic cough, a unique entity is cough that is without an organic cause. Such a persistent involuntary cough without a cause is considered to be a functional disorder. One of the earliest detailed case reports accompanied by 1 year of follow-up was published by Bernstein [5]. He described a 12-year-old girl with what he called “the barking cough of puberty.” 2 months later, Baker [6] placed “chronic cough from habit or psychosomatic disease” in the differential diagnosis for chronic cough in children. The term “habit cough” was first used by Berman [7] in 1966. He reported six children (three in detail) in whom he “relied solely on the art of suggestion” to result in the cessation of cough. His 2-year follow-up supported the success of his therapy. Since then, several descriptive terms have been used for this condition: “functional or psychogenic cough” [8], “psychogenic cough tic” [9], “operant cough” [10], “honking” [11], “involuntary cough syndrome” [11] and “somatic cough syndrome” [12]. However, our experience has found “habit cough” to fit the syndrome best, and has been most acceptable to the families in diagnosing and explaining the nature of the disorder. The success of treatment by us and others has been consistent with Dr Berman’s observation that “the art of suggestion” was effective treatment [7].
Clinical characteristics of the classic habit cough
In 1991, we first reported our experience with this functional cough that we identified as the habit cough syndrome [13]. We described a 15-year-old girl who was coughing multiple times per minute during the clinic visit. The cough was a harsh cough sounding like a “barking dog” or “barking seal”. She had experienced this intractable coughing for many months, had been subjected to extensive medical evaluation and treatment with the initial presumption of asthma as the cause, and had experienced no benefit, including from eventually being subjected to several hospitalisations for intravenous antibiotics. Although interfering with getting to sleep, parents observed no cough at all during sleep nor had cough ever awakened her once asleep. She had been a good student with many friends and expressed regret about missing school because the cough was too intrusive to remain in class. Coughing was stopped during a 15-min course of a behavioural technique that we called suggestion therapy performed by one of the authors (M. Weinberger).
Our initial publication included nine patients seen in our clinic with the same characteristic symptoms, a harsh barking cough that was totally absent when sleeping [13]. All had initially been misdiagnosed as asthma. Symptoms had been present for up to 2 years (median of 2 months). Five had been previously hospitalised for the cough. Evaluation revealed no physiological or radiological abnormality. Either one of the authors of that publication or colleagues in the same clinic had treated each of them during a period of sustained repetitive symptoms with a brief session of a suggestion therapy technique. All of those patients became symptom free during a 15-min session. During the subsequent week, one remained completely asymptomatic and eight had transient minor relapses that were readily self-controlled by utilisation of autosuggestion instructed during the initial clinic visit. Seven of the nine could be contacted for determination of long-term outcome at periods up to 9 years (median 2.2 years) after the session. Six were totally asymptomatic; one had occasional minor self-controlled symptoms.
Subsequent to our observations reported in 1991, we reviewed the literature for this disorder and found a total of 18 studies. They were included in a 2014 systematic review and included 223 patients (46% male); 96% were children and adolescents [14]. Several clinical characteristics of this functional cough have been described with striking similarity by all authors despite differences in diagnostic approach or nomenclature (table 1). All case reports noted a predominantly daytime cough that was absent after patients actually fall asleep. The cough was described as a dry, repetitive, generally nonproductive, loud cough, often described as like a “barking seal” (see video 1, with sound, in the supplementary material). Multiple radiological, serological, clinical, pulmonary function and endoscopic evaluations invariably showed negative results. In contrast to organic causes of cough, increase with exercise was not noted nor was the cough present when asleep. An initial respiratory insult such as a viral respiratory infection was often described as an apparent initiating factor. The duration of cough prior to diagnosis ranged from 1 week to 16 years in the patients included in the systemic review, with the median duration for each report from weeks to months for children and 4 years for the few adults [14].
Table 1.
Clinical characteristics of habit cough
| Loud and repetitive (softer throat clearing variant in some) |
| Absent once asleep (sine qua non) |
| Mainly in children and adolescents |
| Affects both sexes |
| Duration ranges from weeks to many months |
| No consistent response to bronchodilators, steroids, antibiotics or antitussive medications |
| Multiple unscheduled visits for medical care and even hospitalisation are common |
| Normal physical examination other than cough; associated tics are rarely present |
| All clinical testing is otherwise normal |
| Initial respiratory illness such as a viral respiratory infection (common cold) is common |
| Commonly misdiagnosed as asthma |
| School is often missed because of cough |
| Secondary gain or school phobia is uncommonly associated |
Prevalence
The prevalence of habit cough is difficult to establish. The Mayo Clinic (Rochester, MN, USA) found only 62 cases in children consistent with a diagnosis of habit cough during an 18-year period [15]. Our initial report identified only nine patients during a prior 12-year period of reviewed charts [13]. Cohlan et al. [16] reported 33 cases of habit cough during 25 years of his clinical experience. Our most recent review of diagnoses of habit cough from 1995 to 2014 utilising a search programme of electronic medical records identified 140 paediatric patients with habit cough seen at a specialty allergy–pulmonary clinic (figure 1) [17].
Figure 1.
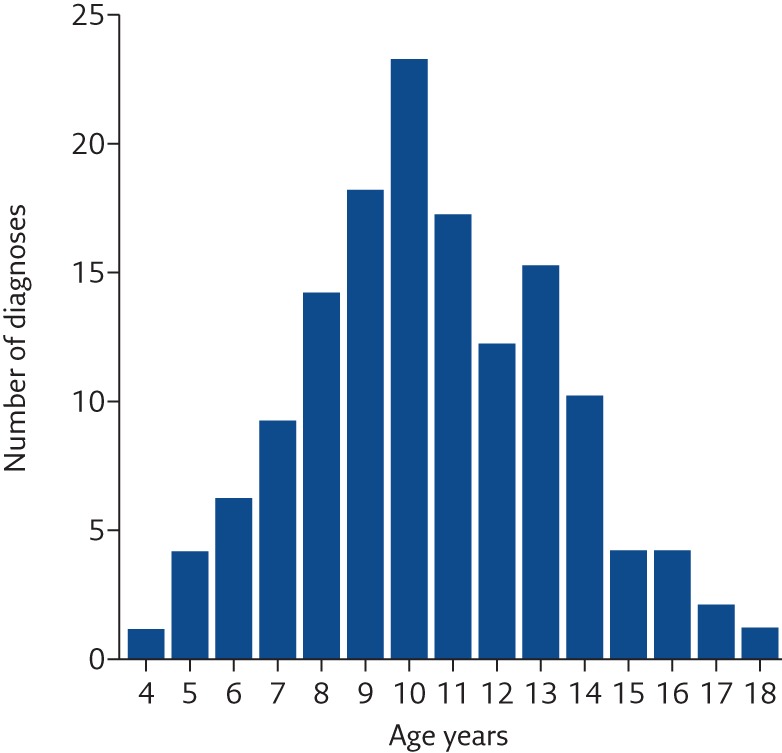
Ages of 140 patients diagnosed with habit cough at the pediatric allergy–pulmonary clinic.
Differential diagnostic considerations
There are many causes of cough that must be considered prior to considering a cough to be functional, although the unique clinical features of the habit cough syndrome readily distinguish that functional cough from organic coughs due to airway inflammation or anatomical abnormalities of the airway.
Asthma
Cough is a prominent symptom of asthma, and asthma is the most common cause of chronic cough. Although it is wheezing that characterises asthma, cough is associated with asthma as frequently as wheezing and may be the only or at least the most prominent symptom in some. However, the cough of asthma is characteristically made worse with activity and, in contradistinction to the habit cough, occurs during sleep, and the individual with a cough from asthma is frequently awakened by cough [18].
Airway malacia
Both tracheomalacia and bronchomalacia have previously been described as being misdiagnosed as asthma [19]. Inadequate rigidity of the tracheal or mainstem bronchial cartilage results in collapse, which causes cough by at least two mechanisms. During increased intrathoracic pressure, as in vigorous exhalation or coughing, the anterior and posterior walls of the airway may come in contact, resulting in an irritable focus that stimulates further cough [20]. Additionally, when secretions are present in the airway, the airway collapse during expiration prevents normal airway clearance of mucus. The retained secretions then act as a further stimulus for cough. While tracheomalacia and bronchomalacia can be troublesome in the infant, some cases do not cause problems until later in childhood [21]. While the sound of the cough in tracheomalacia may be similar to that of the functional habit cough, deep breathing during exercise is likely to accentuate the cough of tracheomalacia, whereas that is not generally a problem with the habit cough.
Protracted bacterial bronchitis
This is an important cause of chronic cough in infants and toddlers, who are unlikely candidates for functional cough, but protracted bacterial bronchitis can also occasionally occur in older children [22, 23]. While chronic bacterial bronchitis is a characteristic of cystic fibrosis and other causes of bronchiectasis, protracted bacterial bronchitis occurs predominantly in young children with no identifiable abnormalities of immunity or other underlying disease [24]. They have prolonged periods of cough with neutrophilia and high colony counts of bacteria in their lower airways demonstrable by bronchoalveolar lavage. A predominance of tracheal and bronchial malacia has been associated with protracted bacterial bronchitis [23]. Those abnormalities may be both contributing to cough and to retaining secretions in the lower airway, which predisposes the child to secondary infection. These patients are readily distinguished from those with habit cough by their young age and troublesome cough at night that frequently disturbs sleep.
Pertussis (whooping cough)
Infection with Bordetella pertussis, known in the past as the 100-day cough, causes a prolonged period of cough, and we have seen several cases where the primary care physician prescribed antiasthmatic medication because pertussis was not adequately considered. While the cough is characteristically spasmodic and associated with post-tussive gagging or emesis, the classical clinical symptom of a whoop is often not present in an immunised population. In fact, evidence for B. pertussis infection has been identified frequently in immunised children and adults with persistent cough for ≥2 weeks but <100 days [25, 26]. Establishing the diagnosis is important to prevent spread to contacts, especially to young infants who are at the greatest risk of hospitalisation and fatality from this infection. Diagnosis is most readily made by PCR identification of pertussis antigen from a properly collected nasal swab. As with other causes of organic cough, cough from pertussis generally disturbs sleep in contrast to the functional habit cough that is characteristically absent once the individual is asleep.
Controversial aetiologies of chronic cough
Prolonged cough has been frequently attributed to gastro-oesophageal reflux (GOR). However, despite anecdotal allegations, data have not been supportive of this as an aetiology of respiratory symptoms [27, 28]. When children with GOR and cough have been examined for inflammation in the lower airway, it was protracted bacterial bronchitis and not reflux that was associated with the cough [29, 30]. Sinusitis, post-nasal drainage and upper airway cough syndrome have also been attributed as causes of chronic cough, but the association of radiological evidence suggestive of sinus inflammation is most likely simply the result of simultaneous inflammation of the upper and lower airway rather than representing an aetiological relationship [31]. Post-nasal drip and the upper airway cough syndrome also lack credibility [32, 33]. Scepticism is justified before attributing these controversial aetiologies as the cause of cough, and their consideration may delay a more appropriate diagnosis and treatment.
Treatment
The functional cough that we and others have called the habit cough syndrome causes much morbidity for prolonged periods unless appropriately treated. In a report of 60 children aged 5–16 years (mean 10.5 years) from the Mayo Clinic, identified as having a functional cough but who received no specific treatment, 44 of these patients required an average of 6 months beyond the diagnosis for spontaneous resolution and 16 patients continued to be symptomatic a mean duration of 5.9 years later [15]. Since there is no evidence that any pharmacotherapy is effective, behavioural treatment is essential. The therapeutic approaches reported in the literature can be divided into two major groups:
vigorous psychological intervention with behavioural techniques or psychotherapy with or without psychotropic drugs; and
suggestion therapy using a variety of techniques.
Reports of the small number of adults with similar cough identified as functional described intense psychotherapy, counselling and speech therapy resulting in decreased symptoms [34, 35]. “Response suppression shaping” utilising painful electric shocks was used with reported success in two teenage boys with no relapses after 1.5 to 2.5 years of follow-up [36, 37]. Prior to this therapy, one coughed so severely that he lost consciousness. One of these patients received >100 sessions, while the other patient discontinued coughing immediately after one shock. One report indicated that an “elevated level of anxiety, neuroticism, affective lability, hyperactivity, low tolerance to frustration” were found in all 10 adult patients with a reported good response to prolonged psychotherapy [38].
One of the earliest reports of successful treatment of the functional habit cough was a dramatic and lasting resolution of a severe chronic cough in a 12-year-old girl after one session of suggestion therapy [5]. A few mild, self-controlled episodes of habit cough were noted during the first 3 days after the suggestion therapy session. Follow-up of over 1 year showed no relapse in that patient. Hypnosis was reported to have been used on the same child twice prior to suggestion therapy with no success. In 1966, Berman [7] reported six patients with what he called habit cough that were successfully treated with therapy that he indicated “relied solely on the art of suggestion”. The children were told that the cough was a habit, that there was no evidence of disease-causing symptoms, and therefore the cough was unnecessary and must stop. Within a few days, the cough gradually subsided and did not recur during a 2-year follow-up period. Special attention was paid in that report to the possibility of psychological or emotional disturbances as a cause of cough, but in only one case was there a suggestion of school phobia.
Kravitz et al. [9] and later Weinberg [11] reported treatment of 12 patients with symptoms consistent with habit cough in children using suggestion and reassurance for all, with the addition of psychotherapy and mild tranquillisers in some cases. They felt that school phobia was a factor in all but one of their patients. Lorin et al. [39] reported a striking case of an 11-year-old girl with habit cough that was so severe she had suffered rib fractures. She was diagnosed with an “adjustment reaction with obsessive, hysterical, and phobic features”. Her parents refused psychotherapy. A single session of suggestion therapy utilising a lollipop as a “distractor” was then tried with prompt cessation of symptoms; she remained asymptomatic 7 years later.
Hypnosis has been successfully used in children by Anbar and Hall [40] using a technique they term self-hypnosis. Anbar [41] reported one patient as successfully treated with self-hypnosis taught by telephone. Biofeedback and cognitive coping were described in treating one 11-year-old girl with classical habit cough [42]. She was described as cough-free after six 1-h sessions. Vocal fold injection with botulinum toxin was used in three children, ages 11–13 years, with transient improvement [43]. Subsequent control was reported as attained with four to eight sessions of behavioural therapy.
A form of suggestion therapy for children with symptoms consistent with habit cough utilised a bed sheet tightly wrapped around the child’s chest with strong verbal reinforcement that this would stop the cough [16]. 31 out of 33 children treated in this manner then became cough-free in 24–48 h after this treatment. The outcome from this bedsheet technique was examined by contacting the family from 10 months to 21 years later (median of 14 months). Contact was made for 18 of the children; cough was reported as absent in 17 of them. There has been a subsequent report of success with the same technique in six patients with no further symptoms 1 week after the treatment [44].
Suggestion therapy, as described in our initial report in 1991 [13], became the routine standard of care for habit cough by all physicians in our allergy and pulmonary specialty clinic. We searched for diagnoses of habit cough identified in our electronic medical record from 1995 to 2014; 140 patients with that diagnosis were identified [17]. Diagnosis of those patients was based on the history of repetitive cough that was absent once asleep. While spirometry was performed in most, other diagnostic measures were generally not. 58% of the 140 patients were male. Ages ranged from 4 to 18 years, with a median age of 10 years (figure 1). Most had a cough characterised by a loud barking sound. A repetitive, softer throat-clearing sound that parents called coughing was present in 10% of the patients, and 11% exhibited both patterns of coughing at times.
Duration of cough before the initial visit to our clinic averaged 4 months (median) and ranged from <1 month to periods in excess of 1 year (figure 2). Prior to the onset of cough, 11 had been receiving daily medication for other clinical problems; eight of them had been receiving behavioural medications such as lorazepam, sertraline or risperidone. Three were identified as having a prior history consistent with chronic asthma and had been receiving inhaled corticosteroids. 14 of the 140 had prior histories of occasional viral respiratory infection-induced asthmatic episodes without persistent symptoms, and had been treated with occasional albuterol and brief courses of an oral corticosteroid. In attempts to treat the cough prior to referral, frequent use of albuterol, oral corticosteroids, montelukast, inhaled corticosteroids, various antibiotics, gastric acid suppressants and cough suppressants had been prescribed. Many of the patients had frequent unscheduled medical care visits related to the cough and four had been hospitalised for treatment of the cough.
Figure 2.
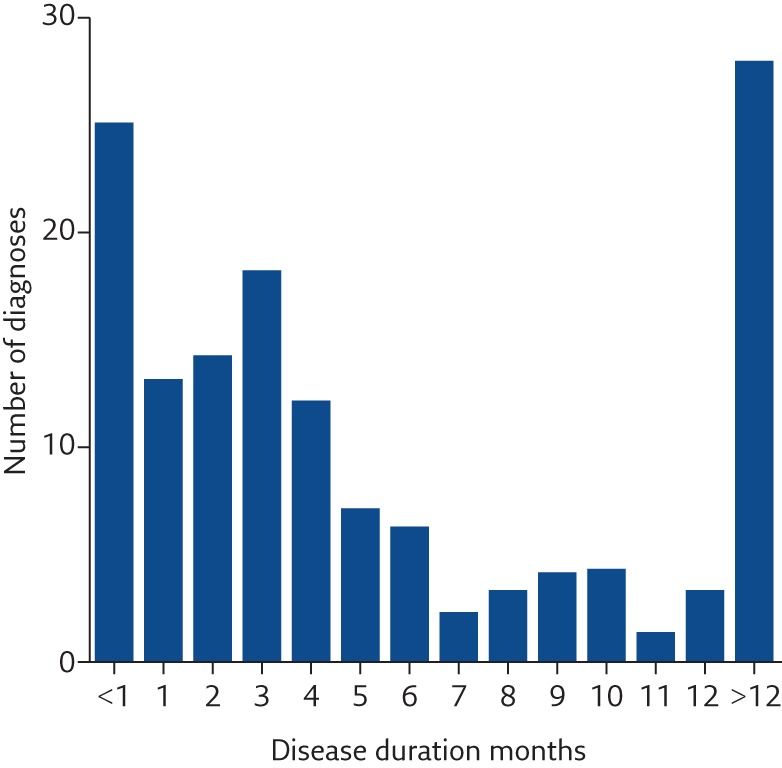
Duration of cough prior to diagnosis at the paediatric allergy–pulmonary clinic.
Our success with suggestion therapy was most apparent among those who were acutely symptomatic with active repetitive coughing at the time of the clinic visit. Treatment consisted of a single short session of suggestion therapy by a staff physician that utilised a distractor as an alternative behaviour to the cough. That consisted of an aerosol of very dilute lidocaine in normal saline to be inhaled or a glass of warm water sipped slowly when the urge to cough was perceived. We explained to the patient that slow, deep breaths of the aerosol or sipping of water would ease the irritation causing the cough and make it easier to hold back the cough with an emphasis on their holding back the cough. The cough was explained to the patient as a response to a perceived irritation in the airway that results in a vicious cycle of cough causing more irritation and thereby more cough. The patient was instructed to focus on the distractor while listening to a constant patter by the physician encouraging the patient to resist the urge to cough. As the session progressed, we emphasised to the patient that breaking the vicious cycle of “cough–irritation–cough” required suppressing the urge to cough (table 2).
Table 2.
Major elements of suggestion therapy
| Approach the patient with confidence that the coughing will be stopped. |
| Explain the cough as a vicious cycle that started with an initial irritant that is now gone, and now cough itself is causing irritation and more cough. |
| Instruct the patient to concentrate solely on holding back the urge to cough, for an initially brief timed period (e.g. 1 min). Progressively increase this time period and utilise an alternative behaviour, such as sipping lukewarm water or inhaling a soothing cool mist from a vaporiser, to “ease the irritation”. |
| Tell the patient that each second the cough is delayed makes it easier to suppress further coughing. |
| Repeat expressions of confidence that the patient is developing the ability to resist the urge to cough; “it’s becoming easier to hold back the cough, isn’t it” (nodding affirmatively generally results in a similar affirmation movement by the patient). |
| When ability to suppress cough is observed (usually by about 10 min), ask in a rhetorical manner, “you’re beginning to feel that you can resist the urge to cough, aren’t you?” (said with an affirmative head nod). |
| Discontinue the session when the patient can repeatedly respond positively to the question, “do you feel that you can now resist the urge to cough on your own?”. This question is only asked after the patient has gone 5 min without coughing. |
| Express confidence that if the urge to cough recurs that the patient can do the same thing at home (autosuggestion)#. |
#: autosuggestion involved expressing confidence that 15-min sessions at home concentrating on holding back the cough using sips of lukewarm water to “ease the irritation causing cough”.
A cough-free period was generally reached within the first 10 min. The complete session was then over in ∼15 min. Patients were advised that now that they have learned they can suppress the cough, they need to continue concentrating on suppressing the cough for the remainder of the day. They were further advised to treat minor recurrences promptly by isolating themselves, using sips of tepid (body temperature) water to “sooth the irritation” and concentrating on suppressing the urge to cough like they did in the clinic. It has been common for the patients to do this readily at home with generally prompt success. We termed this self-treatment at home as autosuggestion. Autosuggestion was provided routinely for those diagnosed as having active habit cough based on the history but not coughing during the clinic visit.
Outcome of suggestion therapy
Of 140 paediatric patients diagnosed with habit cough during a 20-year period at the paediatric allergy and pulmonary clinic, repetitive coughing was present during the clinic visit in 85 patients at the time seen. Complete cough cessation occurred during 15 min (sometimes as long as 30 min) of suggestion therapy in 81 (95%) of those patients. Autosuggestion instruction was provided to be used in case of recurrence once home. Families were provided with specific contact information and encouraged to contact us if troublesome cough returned. The effort to completely stop the cough failed in four patients, one of whom was misdiagnosed and did not have a functional cough, and three who were found to have complex social or psychological problems. No return of troublesome cough was reported in those whose cough stopped during suggestion therapy. Patients not coughing when seen but with a history consistent with habit cough and provided autosuggestion instruction also did not report return of sustained coughing
Complications encountered
While success is usual in the treatment of this functional disorder with suggestion therapy, occasional undesirable and perplexing outcomes have been observed. Three such cases are described.
The first one was an 8-year-old girl with classical habit cough that was stopped with usual suggestion therapy. She returned the following week with excessive drinking and urinating consistent with polydipsia and polyuria that was behavioural in nature. Once that was managed by restricting intake of water, she developed polyphagia. Psychiatric consultation was then obtained.
A second was a 10-year-old boy referred from north-western Iowa, 300 miles (∼480 km) from us with an initial history consistent with classical habit cough syndrome who had been seen initially by a local psychiatrist and eventually institutionalised. The nature of the treatment was unclear but appeared to have been verbally accusatory regarding the nature of the cough. Apparently, the coughing increased in severity to the extent that food ingestion was limited and considerable weight loss occurred. Upon arrival at our clinic, he exhibited a somewhat soft cough rather than the barking cough described at initiation of the problem several months earlier, but the cough occurred with each exhalation during all waking hours. Our usual suggestion therapy was ineffective. He was admitted to our extended care facility for attempted rehabilitation and only very gradually improved.
A third case was a 14-year-old boy, a very bright high achieving student, who had been diagnosed with depression the previous year according to the referring paediatrician. The boy himself stated that his problem had been chronic fatigue syndrome. His cough, present for about 2 months, was consistent with classical habit cough syndrome. The referring paediatrician had diagnosed this patient as habit cough syndrome, and had utilised local specialists to provide suggestion therapy and hypnosis without benefit prior to the referral. The boy and his parents were sceptical about further behavioural attempts at stopping the coughing, which had kept him out of school for the previous 2 months. There was no history to support school avoidance. To the contrary, he reported liking school, had friends and excelled academically. An attempt at suggestion therapy was unsuccessful. A bronchoscopy found no airway malacia but a large lingual tonsil impinging on his epiglottis was suspected to perhaps be a nidus of irritation acting as a stimulus for the cough. A lingual tonsil debulking by paediatric otolaryngology was associated with cessation of the cough but 2 days later, he began having pharyngeal spasms associated with a gulping sound occurring several times per minute during waking hours. This was associated with decreased oral intake, weight loss and continued inability to attend school. A further complaint was persistent headache. Sleep was impaired but parents described cessation of the “gulping” once he was asleep. Attempts at habit cessations by one of our psychologists skilled in that technique and teaching pharyngeal muscular control by our most experienced speech pathologist were not successful. This boy was subsequently referred to a psychologist experienced at biofeedback closer to his home, but he and his parents remained sceptical of such efforts.
These three cases are notable as outliers during 35 years of seeing several cases of habit cough annually that were rapidly cured with suggestion therapy. They stand as exceptions to the general experience that this functional disorder is responsive to suggestion therapy and is usually not associated with evidence for underlying psychopathology or additional somatisation.
Discussion
The aetiology of the habit cough remains unclear. While not examined in a controlled manner, those of us treating these children have had the clinical impression that they tend to be verbally and intellectually above average. The limited psychological testing performed in our initial report found no other evidence for somatisation or other psychological disorders [13]. Nonetheless, this functional cough is associated with considerable morbidity and disruption of life, and can result in considerable iatrogenic problems due to misdiagnosis. The demographics of habit cough from our 20-year review of patients with this disorder found 85% between the ages of 8 and 14 years with a mean age of 10 years (figure 1). Similar symptoms in the relatively small number of adults described in the literature suggest that chronic functional cough in adults may not be a manifestation of the same disorder experienced in most of the children and adolescents with chronic functional cough. Those reporting treatment of chronic functional cough in adults expressed conflicting views, but there was an emphasis on addressing psychological problems.
There is no evidence that use of psychotropic medications or psychotherapy results in cough cessation of children and adolescents with habit cough. The consequence of simply diagnosing and counselling the patient can result in a prolonged symptomatic course for many patients [15]. Suggestion therapy aimed at empowering the patient with the ability to resist the urge to cough results in rapid and sustained resolution of symptoms in almost all the patients for whom it had been used. Less common variations of the habit cough disorder, including habit sniffing, habit nose blowing and habit sneezing, also responded to suggestion therapy by the faculty of the paediatric allergy–pulmonary clinic [45].
Conclusion
Diagnosis of the functional disorder called habit cough can be readily made by the unique clinical characteristics (table 1). Treatment by a single session of suggestion therapy (table 2) performed by the treating physician has the merit of therapeutic simplicity with both immediate and long-term success. For the majority of patients, a careful history, spirometry and a chest radiograph should be sufficient to assure a physician as well as a patient’s family that an organic basis for the cough is unlikely. Actual cessation of the cough with a session of suggestion therapy then provides confirmation for even the most sceptical parents. Early recognition of habit cough is essential to prevent inappropriate unnecessary treatment and continued morbidity from the prolongation of distressing cough.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Video 1. 10-year-old boy with typical repetitive barking cough of the habit cough. Video 1 (5.4MB, mpg)
Footnotes
Supplementary materialThis article has supplementary material available from breathe.ersjournals.com
Conflict of interest None declared.
References
- 1.Chang AB, Landau LI, van Asperen PP, et al. Cough in children: definitions and clinical evaluation. Med J Aust. 2006; 184: 398–403. [DOI] [PubMed] [Google Scholar]
- 2.Weinberger M, Fischer A. Differential diagnosis of chronic cough in children. Allergy Asthma Proc 2014; 35: 95–103. [DOI] [PubMed] [Google Scholar]
- 3.Chang AB, Robertson CF, van Asperen PP, et al. A cough algorithm for chronic cough in children: a multicenter, randomized controlled study. Pediatrics 2013; 131: e1576–e1583. [DOI] [PubMed] [Google Scholar]
- 4.Chang AB, Oppenheimer JJ, Weinberger M, et al. Use of management pathways or algorithms in children with chronic cough: systematic reviews. Chest 2016; 149: 106–119. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein L. A respiratory tic: “the barking cough of puberty.” Report of a case treated successfully. Laryngoscope 1963; 73: 315–319. [DOI] [PubMed] [Google Scholar]
- 6.Baker DC., Jr Chronic cough in children. NY State J Med 1963; 63: 1535–1539. [PubMed] [Google Scholar]
- 7.Berman BA. Habit cough in adolescent children. Ann Allergy 1966; 24: 43–46. [PubMed] [Google Scholar]
- 8.Rabin CB. Disturbances of respiration of functional origin. J Asthma Res 1968; 5: 295–308. [DOI] [PubMed] [Google Scholar]
- 9.Kravitz H, Gomberg RM, Burnstine RC, et al. Psychogenic cough tic in children and adolescents. Nine case histories illustrate the need for re-evaluation of this common but frequently unrecognized problem. Clin Pediatr 1969; 8: 580–583. [DOI] [PubMed] [Google Scholar]
- 10.Munford PR, Liberman RP. Differential attention in the treatment of operant cough. J Behav Med 1978; 1: 289–295. [DOI] [PubMed] [Google Scholar]
- 11.Weinberg EG. “Honking”: psychogenic cough tic in children. S Afr Med J 1980; 57: 198–200. [PubMed] [Google Scholar]
- 12.Vertigan AE, Murad MH, Pringsheim T, et al. Somatic cough syndrome (previously referred to as psychogenic cough) and tic cough (previously referred to as habit cough) in adults and children: CHEST guideline and expert panel report. Chest 2015; 148: 24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lokshin B, Lindgren S, Weinberger M, et al. Outcome of habit cough in children treated with a brief session of suggestion therapy. Ann Allergy 1991; 67: 579–582. [PubMed] [Google Scholar]
- 14.Haydour Q, Alahdab F, Farah M, et al. Management and diagnosis of psychogenic cough, habit cough, and tic cough: a systematic review. Chest 2014; 146: 355–372. [DOI] [PubMed] [Google Scholar]
- 15.Rojas AR, Sachs MI, Yunginger JW, et al. Childhood involuntary cough syndrome: a long-term follow-up study. Ann Allergy 1991; 66: 106. [Google Scholar]
- 16.Cohlan SQ, Stone SM. The cough and the bedsheet. Pediatrics 1984; 74: 11–15. [PubMed] [Google Scholar]
- 17.Weinberger M, Hoegger M. The cough without a cause: habit cough syndrome. J Allergy Clin Immunol 2016; 137: 930–931. [DOI] [PubMed] [Google Scholar]
- 18.Weinberger M. Pediatric asthma and related allergic and nonallergic diseases: patient-oriented evidence based essentials that matter. Pediatric Health 2008; 2: 631–650. [Google Scholar]
- 19.Weinberger M, Abu-Hasan M. Pseudo-asthma: when cough, wheezing, and dyspnea are not asthma. Pediatrics 2007; 120: 855–864. [DOI] [PubMed] [Google Scholar]
- 20.Wood RE. Localized tracheomalacia or bronchomalacia in children with intractable cough. J Pediatr 1990; 116: 404–406. [DOI] [PubMed] [Google Scholar]
- 21.Weinberger M, Abu-Hasan M. Pseudo-asthma: when cough, wheezing, and dyspnea are not asthma. Pediatrics 2007; 120: 855–864. [DOI] [PubMed] [Google Scholar]
- 22.Marchant JM, Masters IB, Taylor SM, et al. Evaluation and outcome of young children with chronic cough. Chest 2006; 129: 1132–1141. [DOI] [PubMed] [Google Scholar]
- 23.Kompare M, Weinberger M. Protracted bacterial bronchitis in young children: association with airway malacia. J Pediatr 2012; 160: 88–92. [DOI] [PubMed] [Google Scholar]
- 24.Marchant JM, Gibson PG, Grissell TV, et al. Prospective assessment of protracted bacterial bronchitis: airway inflammation and innate immune activation. Pediatr Pulmonol 2008; 43: 1092–1099. [DOI] [PubMed] [Google Scholar]
- 25.Harnden A, Grant C, Harrison T, et al. Whooping cough in school age children with persistent cough: prospective cohort study in primary care. BMJ 2006; 333: 174–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Craig AS, Wright SW, Edwards KM, et al. Outbreak of pertussis on a college campus. Am J Med 2007; 120: 364–368. [DOI] [PubMed] [Google Scholar]
- 27.Størdal K, Johannesdottir GB, Bentsen BS, et al. Acid suppression does not change respiratory symptoms in children with asthma and gastro-oesophageal reflux disease. Arch Dis Child 2005; 90: 956–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang AB, Connor FL, Petsky HL, et al. An objective study of acid reflux and cough in children using an ambulatory pHmetry-cough logger. Arch Dis Child 2011; 96: 468–472. [DOI] [PubMed] [Google Scholar]
- 29.Chang AB, Cox NC, Purcell J, et al. Airway cellularity, lipid laden macrophages and microbiology of gastric juice and airways in children with reflux oesophagitis. Respir Res 2005; 6: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang AB, Cox NC, Faoagali J, et al. Cough and reflux esophagitis in children: their co-existence and airway cellularity. BMC Pediatr 2006; 6: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campanella SG, Asher MI. Current controversies: sinus disease and the lower airways. Pediatr Pulmonol 2001; 31: 165–172. [DOI] [PubMed] [Google Scholar]
- 32.Morice AH. Post-nasal drip syndrome – a symptom to be sniffed at? Pulm Pharmacol Ther 2004: 17: 343–345. [DOI] [PubMed] [Google Scholar]
- 33.Kemp A. Does post-nasal drip cause cough in Childhood? Paediatr Respir Rev 2006; 7: 31–35. [DOI] [PubMed] [Google Scholar]
- 34.Gay M, Glager G, Bartsch K, et al. Psychogenic habit cough: review and case reports. J Clin Psychiatry 1987; 48: 483–486. [PubMed] [Google Scholar]
- 35.Blager FB, Bay M, Wood RP. Voice therapy techniques adapted to treatment of habit cough: a pilot study. J Commun Disord 1988; 21: 393–400. [DOI] [PubMed] [Google Scholar]
- 36.Alexander AB, Chai H, Creer TL, et al. The elimination of chronic cough by response suppression shaping. J Behav Ther Exp Psychiatry 1973; 4: 75–80. [Google Scholar]
- 37.Creer TL, Chai H, Hoffman A. A single application of an aversive stimulus to eliminate chronic cough. J Behav Ther Exp Psychiat 1977; 8: 107–109. [Google Scholar]
- 38.Houst‘k J, Vyhnálek M, Suková B, et al. Psychogenic cough. Cesk Pediatr 1983; 38: 405–410. [PubMed] [Google Scholar]
- 39.Lorin MI, Slovis TL, Haller JO. Fracture of ribs in psychogenic cough. N Y State J Med 1978; 78: 2078–2079. [PubMed] [Google Scholar]
- 40.Anbar RD, Hall HR. Childhood habit cough treated with self-hypnosis. J Pediatr 2004; 144: 213–217. [DOI] [PubMed] [Google Scholar]
- 41.Anbar RD. Childhood habit cough treated with consultation by telephone: a case report. Cough 2009; 5: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Labbé EE. Biofeedback and cognitive coping in the treatment of pediatric habit cough. Appl Psychophysiol Biofeedbadk 2006; 31: 167–172. [DOI] [PubMed] [Google Scholar]
- 43.Sipp JA, Haver KE, Masek BJ, et al. Botulinum toxin A: a novel adjunct treatment for debilitating habit cough in children. Ear Nose Throat J 2007; 86: 570–572. [PubMed] [Google Scholar]
- 44.Wolff PS. An ingenious way to treat psychogenic cough. MCN Am J Matern Child Nurs 1988; 13: 118–120. [PubMed] [Google Scholar]
- 45.Weinberger M. The habit cough syndrome and its variations. Lung 2012; 190: 45–53. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Video 1. 10-year-old boy with typical repetitive barking cough of the habit cough. Video 1 (5.4MB, mpg)


