Abstract
Skillful, collaborative conversations are powerful tools to improve physical and mental health. Whether you are a parent talking with your child about the dangers of substance abuse, an educator concerned about a student’s signs of psychological distress, a veteran worried about a buddy who is contemplating suicide, or a healthcare professional wanting to better engage patients to increase treatment compliance, having the skill, confidence and motivation to engage in conversations can truly transform the health and well-being of those you interact with. Kognito develops role-play simulations that prepare individuals to effectively lead real-life conversations that measurably improve social, emotional, and physical health. The behavior change model that drives the simulations draws upon components of game mechanics, virtual human simulation technology and integrates evidence-based instructional design components as well as principles of social-cognitive theory and neuroscience such as motivational interviewing, emotional regulation, empathy and mindfulness. In the simulations, users or enter a risk-free practice environment and engage in a conversation with intelligent, fully animated, and emotionally responsive virtual characters that model human behavior. It is in practicing these conversations, and receiving feedback from a virtual coach, that users learn to better lead conversations in real life. Numerous longitudinal studies have shown that users who complete Kognito simulations demonstrate statistically significant and sustained increases in attitudinal variables that predict behavior change including preparedness, likelihood, and self-efficacy to better manage conversations. Pending the target population, each online or mobile simulation resulted in desired behavior changes ranging from increased referrals of students, patients or veterans in psychological distress to mental health support services, or increasing physician patient-centered communication or patient self-confidence and active involved in the decision-making processes. These simulations have demonstrated a capability to address major health and public health concerns where effective conversations are necessary to bring about changes in attitudes and behaviors.
Keywords: Simulations, behavior change, virtual humans, motivational interviewing, role play
Introduction
The importance of developing conversation skills cannot be understated in terms of their potential to have a positive impact on the health of the world’s population. An article in The Journal of the American Medical Association summarized the importance of communication this way: “Excellent medical care combines sophistication in scientific knowledge with equally sophisticated communication skills to understand the needs of the individual patient, to address his/her feelings and concerns with sensitivity and compassion, and to educate patients about their choices in care…. The benefit of good communication on patient care and outcomes is unequivocal” (1). But health conversations don’t just happen at the doctor’s office. Former California highway patrol officer, Sgt. Kevin Briggs in the “Guardian of the Golden Gate Bridge”, convinced more than 200 people not to take their lives by jumping from the bridge. He recounted one survivor stating: “He never made me feel guilty for being in the situation I was in. He made me feel like, ‘I understand why you are here, but there are alternatives’.” (2).
Skillful, collaborative conversations are powerful tools to improve physical and mental health. Whether you are a healthcare professional who wants to better engage patients and increase adherence to treatment, a patient who wants to better communicate your goals, preferences, or challenges to your physician, an educator concerned about a student showing signs of psychological distress, a veteran worried about a buddy who is contemplating suicide, or a parent talking with your child about the dangers of substance use, having the skill and motivation to engage in such conversations can truly transform the health and well-being of those you interact with.
Recent developments in technology and research offer new and unique ways for people to learn how to effectively lead health conversations that measurably improve social, emotional, and physical health. The developments span diverse areas, including virtual humans, simulations, social cognitive communication strategies such as motivational interviewing (MI) and shared-decision making, and the increasing adoption of online and mobile instructional technologies within health and behavioral health.
Kognito (www.kognito.com) is a NYC-based developer of research-proven role-play conversations featuring virtual humans that are utilized to prepare individuals, including health professionals, build the skills and knowledge to drive positive change in social, emotional, and physical health through the power of conversations. What follows here discusses: (I) the Kognito Conversation PlatformTM that draws upon components of a behavior change model as well as game mechanics and virtual human simulation technology; (II) the advantages of using virtual humans; (III) the behavior change model which underlies Kognito’s conversation simulations; and (IV) research that demonstrates the efficacy of Kognito’s simulations to improve health behaviors in settings such as primary care, schools, and at home.
The Kognito Conversation PlatformTM
Kognito’s simulations are designed using the proprietary Kognito Conversation PlatformTM, a ground-breaking group of development, delivery, API, data collection, and analytic technologies integrated with principles of neuroscience, social cognition, adult learning, applied game mechanics, and storytelling (see Figures 1,2 for sample screenshots).
Figure 1.

Screenshot from At-Risk in Primary Care: Adolescent where healthcare professionals learn to conduct screening and brief interventions with adolescents at-risk for mental health and substance use disorders.
Figure 2.

Screenshot from Together Strong: where veterans and military personnel learn how to support their buddies exhibiting signs of post-deployment stress and motivate them to seek help.
How a simulation works
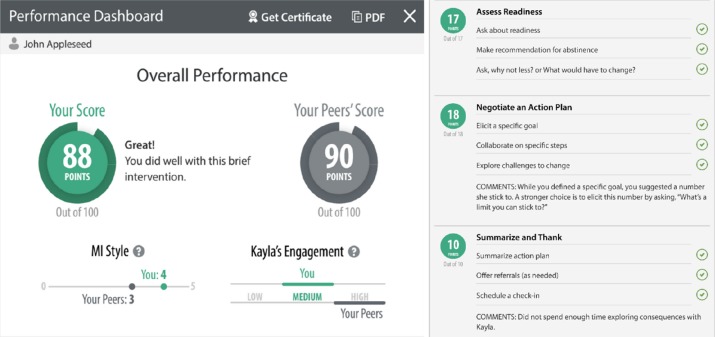
In a simulation, the user or “player” enters a risk-free practice environment, assumes a role (e.g., a healthcare professional, patient, or family member) and engages in a conversation with intelligent, fully animated, and emotionally responsive virtual humans that model human behavior. Virtual humans are coded to possess an individual personality and memory and adapt their behaviors to the decisions of the player throughout the conversation. Players communicate with the virtual human by selecting from a dynamic menu of dialogue options. Each option represents a specific conversation tactic based on social-cognitive and communication skills that may be more or less effective or ineffective in accomplishing the goal. Once the user chooses a dialogue option, they see their virtual human “perform” the dialogue and then observe the verbal and non-verbal response of the non-player virtual human. A virtual coach provides personalized feedback and give users an opportunity to revise their choice. The relationship between the user’s dialogue decision and the response of the emotionally responsive virtual humans are controlled by a set of mathematical behavioral models and algorithms specifically designed to simulate real interactions with patient types, for example, that represent particular personality traits or conditions. These algorithms ensure that users are repeatedly exposed to target conversation and behavior patterns as a way to develop skills and knowledge. To successfully complete the conversation, users must apply effective conversation tactics and adapt their decisions based on the virtual human’s behavior. At the end of each conversation, users are provided with summary feedback from the virtual coach and a performance dashboard with detailed feedback on how well they performed on each of the conversation goals (see Figure 3).
Figure 3.
Screenshot of performance dashboard that provides detailed feedback on how well the user achieved each conversation goal.
Advantages of virtual humans
Learning through role-play with trained instructors has been widely used in health and behavioral health education and practice settings. The cost and logistics, however, of organizing live skill practice and assessment sessions with trained actors (or standardized patients), the challenge of standardizing the experience, and the discomfort participants often experience role-playing in a workshop setting are significant barriers to effective adoption. Recent development and research into the efficacy of virtual humans as an alternative to the traditional, live role-play methodology provides an opportunity to eliminate many of these barriers. This alternative also provides a highly effective learning experience—building and assessing communication and conversation competencies in a digital, standardized, and risk-free medium that is available 24/7.
Virtual humans are defined as automated, three-dimensional agents that converse, understand, reason, and exhibit emotions (see Figure 4). Their use has many educational and economic advantages allowing users to practice how to leverage conversations and drive meaningful change in behaviors and attitudes. Role-playing with virtual humans decreases the likelihood of negative transference reactions or the user feeling embarrassed or judged which often happens in live role-plays especially in the presence of peers (3,4). Both negative emotions in general and social evaluative threat in particular are known to impede cognitive performance, learning, and retention (5-11). Another advantage is that virtual humans are coded to support high fidelity of the learning experience. This includes consistent delivery of accurate knowledge, realistic and engaging role-plays, and appropriate feedback. Adding to the fidelity is that virtual humans do not fatigue, have a neutral appearance, are not subject to trainer bias, and will continually respond in the most efficacious way to promote skill development. Also, users find it easier to talk to and explore different communication strategies with virtual humans as there is little fear of making mistakes or being judged, especially when practicing in the privacy of one’s home or office (12). Lastly, the appearance and voice/language of the virtual human can be customized to each user and conversation setting to provide a high level of personalization, localization, and cultural appropriateness. These factors make digital simulations appropriate alternatives or supplements to traditional workshops and other non-interactive learning experiences.
Figure 4.

A screenshot from At-Risk for Students, a mental health simulation where students learn how to speak with and motivate fellow students experiencing psychological distress to seek help.
Kognito Behavior Change Model
The Kognito Behavior Change Model includes two parts: the instructional design component that draws from the science of education and learning theory, and the conversation component that integrates evidence-based communication strategies drawn from models in social cognition and neuroscience.
Instructional design component—simulations rooted in learning theory
There has been widespread agreement based on extensive research that skills are best learned when knowledge is actively constructed, rather than through the traditional didactic model where knowledge is presented and learners passively accept it (13-17). In Kognito simulations, learners are afforded multiple opportunities to actively make decisions, thereby creating unique pathways of experience on an individual level. As learners devise their own experience through the simulation, they actively construct knowledge based on the decisions they make (13-15).
Research has also demonstrated that skills acquisition and mastery is most likely to occur when active learning strategies are used. Situated learning gives learners agency and allows the brain to make meaningful connections through physical, embodied experiences that are as authentic as possible related to the context where the learning will be applied (18-22). By employing this theory in a virtual space, Kognito provides users with an opportunity to both learn and practice in a safe, simulated environment that mimics the authenticity of the same real-world contexts. This allows for experimentation with various communication tactics without fear of consequences or judgement.
According to Cognitive Load Theory, the processing capabilities of the brain’s working memory are limited, and in order to allow for as much processing power as possible, information must be presented in such a way as to reduce extraneous cognitive load (23). Kognito simulations encompass several instructional design strategies to reduce extraneous cognitive load in order to increase encoding capabilities in working memory, therefore resulting in deeper and more meaningful learning. Furthermore, evidence shows that communication skills change and endure when behavior change models incorporate deliberate practice, include personalized attention with ongoing feedback, and self-performance assessment, and also when they utilize role-plays, and provide a connection between the learned content and the current practice (24). Kognito simulations are designed in this way and include:
❖ Self-pacing so that learners can reflect on their skills and adjust their strategies at their own pace;
❖ Continuous analysis and feedback on performance via virtual human verbal and nonverbal reactions to conversation tactics, virtual coaches, and feedback meters (e.g., indicating trust built);
❖ Graphics that cue learners to specific content;
❖ Dashboards that summarize performance and make recommendations for future practice; and
❖ Virtual human inner thoughts or thought bubbles that provide users with context around a perspective and understanding outside of their own.
Conversation component
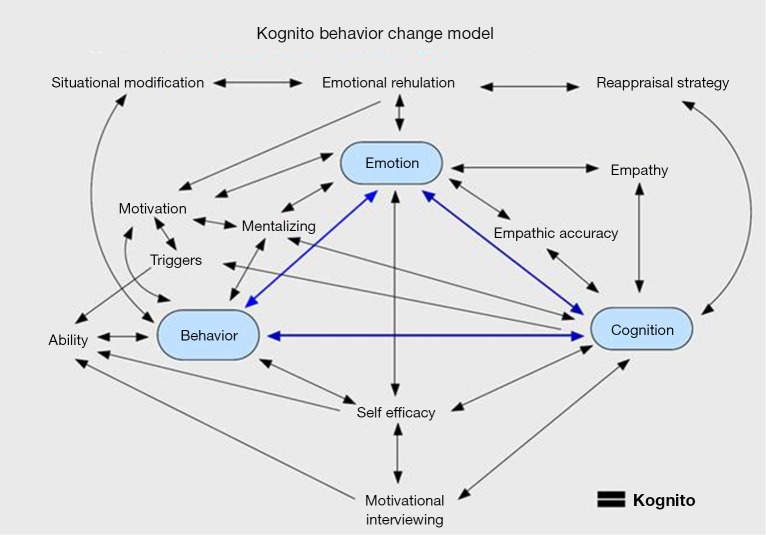
Kognito simulations integrate several interrelated communication strategies drawn from social/cognitive models and neuroscience (see Figure 5). These include:
Figure 5.
Conversation components of the Kognito Behavior Change Model.
-
MI is a set of communication strategies originally designed by clinical psychologists for use in counseling sessions with problem drinkers (25). MI is a goal-oriented, person-centered counseling approach designed to help people resolve their ambivalence about behavior change. By strategically evoking the person’s own thoughts and feelings, the counselor facilitates the exploration of internal conflicts and amplifies the person’s existing motivation (26). The simulations discussed in this paper integrated the four core MI communication skills and the four elements of the MI spirit. The four core MI communication skills are:
Ask open-ended questions to invite the person to share their thoughts while focusing the conversation in a particular direction.
Affirm the person’s strengths, values, or efforts. This builds trust and instills the power to change.
Listen closely and reflect the person’s statements to selectively emphasize them and confirm understanding.
Summarize what the person has told you to show that you’re listening, link to related information, or transition to a new topic.
These techniques have been associated with effective therapy and are thought to encourage strong rapport and support behavior change (27). The four elements of the MI spirit are:
Partnership—the counselor respects that the person is the expert on themselves and works with them, not “on” them.
Acceptance of the person’s perspective, inherent value, and autonomy.
Compassion for the person’s needs and welfare. The counselor commits to acting in the person’s best interest.
-
Evocation of the person’s existing expertise and motivation, rather than installing what the counselor thinks is “missing.”
Mentalizing is the ability to recognize and accept that other people have their own thoughts, beliefs, intentions, and emotions which may be different from one’s own and that this is OK. Mentalizing promotes a non-judgmental or non-critical stance toward the engaged individual and this is crucial for healthy interaction. While all healthy adults understand that other beings have independent minds, both the inclination to attend to the minds of others and the ability to accurately assess what others think or know varies among individuals. Practicing mindfulness has been shown to increase the frequency and accuracy of mentalizing in clinical populations, leading to better mental health outcomes (28-30).
Empathy is the capacity to feel the emotions of another being (31,32). In most cases, an empathic response is incumbent on mentalizing; a person will be able to feel the emotions of another if they are able to temporarily put aside their own, perhaps different viewpoint (33). In fact, neuroimaging research has shown that mentalizing and empathy rely on overlapping yet distinct brain networks (34). An intact empathic response is important for healthy social and emotional functioning and research has shown that empathic responsiveness can be enhanced through training in a variety of populations and circumstances (35-37).
Empathic accuracy, also sometimes described as “cognitive empathy”, is the ability to correctly assess or identify the emotions of another (38). This skill may be thought of as the ability to “read people”. Empathic accuracy and empathy are conceptually distinct. Empathy does not necessarily imply the ability to accurately identify a shared emotion, and empathic accuracy does not necessarily require that one feel the emotions of another. However, research has shown a bidirectional relationship between empathy and empathic accuracy, as long as there is sufficient expression (39). Empathic accuracy also varies across individuals, and high empathic accuracy is predictive of healthy interpersonal relationships (40,41). Recent work has shown that it can be improved with training (42).
Situation modification is when one attempts to avoid, leave, or modify circumstances that are likely to elicit unwanted emotions and to enter into situations that are likely to elicit desired emotions (43).
Reappraisal strategy is when one changes the way they interpret the meaning of a stimulus, for example, seeing eating cake as a hindrance to one’s diet plan rather than a delicious treat (44,45). Reappraisal is an especially important strategy, as it has been shown to have lasting effects on the way in which one responds to an emotional stimulus (46-49). The tendency to reappraise is correlated with improved mental health, social functioning, and well-being.
Research overview
Kognito has partnered with leading academic institutions and non-profits to conduct numerous empirical studies analyzing the impact of Kognito simulations on users’ attitudes, skills, and behaviors. These studies have led three Kognito simulations to be listed in SAMHSA’s National Registry of Evidence-Based Programs and Practices with five currently under review, and they have also inspired journal publications, and dozens of referred conference presentations. Below is a summary of findings based on a sample of studies conducted on Kognito simulations whose users comprise three settings: (I) educators (Tables 1,2); (II) family/caregiver (Table 3); and (III) primary care (Tables 4,5,6).
Table 1. Results from At-Risk for High School Educators: a simulation to build mental health awareness, reduce stigma, and increase educators’ skill and motivation to recognize when students are exhibiting signs of psychological distress and know how to approach and discuss a referral to support services.
| Simulation goals | Sample size & demographics | Study design | Results |
|---|---|---|---|
| Recognize when students exhibit signs of psychological distress, including anxiety, depression, and thoughts of suicide | N=31,144 | Quasi-experimental design | Statistically significant changes in preparedness, likelihood/behavioral intent, and self-efficacy in ability to identify, talk to, and refer students in psychological distress |
| Approach students to discuss their concern | Years of teaching experience (mean, 11.1 years) | Longitudinal group analysis to examine changes in behavior | Behavior changes: 3-month follow-up found statistically significant increases in the number of students who teachers referred to support services |
| Make a referral to school support personnel | Age (mean, 42.3 years) | Multivariate analysis, Hotelling’s T2 | At 3-month follow up point, 57% reported an increase in the number of conversations they had with other adults in their school about students they were concerned about |
| Gender: 65.3% female | Independent samples t-tests | Statistically significant increase in the number of educators that felt that part of their role is to help students in psychological distress | |
| Paired samples t-tests | Satisfaction data: 95% said they would recommend to colleague, 80% said it was based on scenarios relevant to their work with students, 79.% stated the simulation will aid them in getting timely help to their students, 80% rated the simulation as “excellent” to “very good” |
Data used in this table was accepted for review by the National Registry of Evidenced-Based Programs and Practices.
Table 2. Results from At-Risk for University and College Students: a simulation to build mental health awareness, reduce stigma, increase self-help behaviors, and increase students’ skill and motivation to recognize when fellow students are exhibiting signs of psychological distress and know how to approach and discuss a referral to support services.
| Simulation goals | Sample size & demographics | Study design | Results |
|---|---|---|---|
| Recognize when a fellow student exhibits signs of psychological distress, including anxiety, depression, and thoughts of suicide | N=254 | Quasi-experimental design | Statistically significant changes in preparedness, likelihood, and self-efficacy to identify, talk to, and refer a fellow student in psychological distress |
| Manage conversations with a fellow student they are concerned about to determine the need for referral | Participants were recruited from 10 academic institutions in the U.S. | Longitudinal within group analysis to examine changes in behavior | Behavior changes: 3-month follow-up found statistically significant increases in the number of fellow students that participants were concerned about, approached to have a discussion with and referred to mental health support services |
| If necessary, make a referral to mental health support services | Average age, 19.6 years | ANOVA | Participants reported a statistically significant increase in likelihood that they themselves would seek help when feeling psychologically distressed |
| Gender: 52.9% female | Independent samples t-tests | Satisfaction data: 92% said they would recommend the simulation to friends and peers, 96% said it was based on scenarios relevant to them and their fellow students, 95% stated the simulation will aid them in getting help to their fellow students, and 78% rated the simulation “excellent” to “very good” | |
| Year in school: 67% (freshman), 17% (sophomore), 8% (junior), 4% (senior) | Paired samples t-tests | ||
| 10% resident advisors |
Data used in this table was accepted for review by the National Registry of Evidenced-Based Programs and Practices.
Table 3. Results from Family of Heroes: a resiliency and PTSD simulation for military families about managing challenging interactions with their veterans while adjusting to post-deployment life. This includes how to identify signs of post-deployment stress and speak with the veteran to motivate them to seek help at the VA (40). Simulation was created in collaboration between Kognito (New York, NY) and the Department of Veterans Affairs of NY/NJ - VISN 3 (50).
| Simulation goals | Sample size & demographics | Study design | Results |
|---|---|---|---|
| Increased knowledge of the prevalence of psychological distress among veterans | N=94 | Randomized Controlled Trial | Statistically significant changes in preparedness to recognize signs of post-deployment stress, discuss concern with veterans and motivate them to seek help at the VA |
| Identify the signs of post deployment stress including PTSD, traumatic brain injury, depression and thoughts of suicide | Average age, 37.5 years | Repeated measures ANOVA | Statistically significant change in self-efficacy to motivate veterans to seek help at the VA |
| Talk with their veteran about their concern | Participants were recruited from 27 states | Statistically significant change in likelihood or behavioral intent to approach a veteran and discuss concern and to mention the VA as a helpful resource | |
| Motivate their veteran to seek help | Relationship to veteran: 37% spouse or partner, 23% son or daughter; 8% mother or father; 22.9% brother or sister; 14% friend | Behavior changes: 1-month follow-up found a 46% increase (statistically significant) in the number of family members who approached their veteran to discuss concerns and identified the need for their veteran to seek help | |
| Increase the number of veterans experiencing post-deployment stress who seek help | Gender: 72% female | One-month follow-up found that 22% of the veterans approached by their family member decided to seek help for their psychological distress. This is in comparison to 12% at the control group | |
| Average time veteran home: 11 months | Satisfaction data: 99% said they would recommend the simulation to family or friends of veterans; 90% said it was based on scenarios relevant to them and their veteran; 98% stated the simulation helped them to be better prepared for similar conversations in real life; 98% rated the simulation “excellent” to “very good” | ||
| Veterans previously diagnosed with: 24% (PTSD), 26% (anxiety), 13% (substance use disorder), 3% (traumatic brain injury) | Average experience time was 18 minutes (experience is designed from 7–15 minute modules) |
Table 4. Results from At-Risk in Primary Care: a professional development simulation for primary care professionals on how to conduct screening, brief interventions, and referral to treatment with patients suffering from substance use, depression, anxiety, and PTSD (51).
| Simulation goals | Sample size & demographics | Study design | Results |
|---|---|---|---|
| Recognize risk factors, and warning signs of alcohol and substance use, depression, and suicidal thoughts | N=614 | Quasi-experimental design | Statistically significant changes in knowledge and skill to: (I) identify risk factors and warning signs of behavioral health disorders, (II) recognize when a patient is exhibiting signs and symptoms, (III) screen patients for behavioral health disorders, (IV) discuss treatment options, (V) engage in collaborative decision-making about treatment plans, and (VI) build intrinsic motivation in patients to adhere to the suggested treatment plan |
| Conduct brief interventions using motivational interviewing to build patients’ motivation and increase protective behaviors | Participants recruited from six different states in the Midwest, Southwest, and Northeast regions of the U.S. | Longitudinal within group analysis to examine changes in behavior | Behavior change: 3-month self-reported follow-up data revealed that as a result of the simulation there was a: (I) 51% increase in the number of at-risk patients who participants identified; (II) 60% increase in patients screened; (III) 58% increase in patients with which treatment options were discussed; and (IV) 53% increase in patient collaborative decision-making about treatment plans |
| Engage in collaborative treatment planning with patients | Work role: 35% nurse, 11% doctor, 17% nursing or medical student, 21% mental health or social worker | ANOVA | Satisfaction data: 94% said they would recommend to colleague; 99% said they would recommend to fellow nursing or medical students; 97% stated the simulation enhanced their skill as a healthcare professional; 86% rated the simulation as “excellent” to “very good” |
| Refer patients to treatment services and follow up on referrals | Industry experience, mean =7.4 (9.87) | Independent samples t-tests | |
| Gender, 79% female | Paired samples t-tests |
Table 5. Results from Primary Care Office Visit: Antibiotics: physicians and patient simulation to promote effective communication and collaborative decision-making between physicians and patients in order to improve health outcomes, including the overuse of antibiotics.
| Simulation goals | Sample size & demographics | Study design | Results | |
|---|---|---|---|---|
| Health care professionals | ||||
| Promote effective communication and collaborative decision-making skills in health care professionals | N=35 | Within group design | Statistically significant changes at 1-month follow-up in patient-centered communication and focus on patients’ psychosocial needs. At the one-month follow-up survey, 77% of physicians reported that the simulation had a positive impact on the way they communicate with patients; 65% indicated that it helped them have a conversation with patients about antibiotics; 94% intend to further invite patients to ask questions and participate; 93% agreed or strongly agreed that as result of the simulation, physicians would be better prepared, confident, and able to effectively engage in a conversation about antibiotics with patients | |
| To improve patients’ understanding and beliefs about the correct usage of antibiotics | Average age, 40.3 years | Repeated measures ANOVA | Satisfaction data: 89% said they would recommend to other physicians; 100% would recommend to medical students or residents; 94% more confident in having an effective conversation about antibiotics with patients; 88% more confident in sharing information in a way patients will understand | |
| Primary care professionals drawn from NYU Langone Medical Center’s: (I) Bellevue Hospital, Gouverneur Health, (II) Veterans Affairs NY Harbor Healthcare System’s New York Campus, and (III) NYU’s Faculty Group Practice |
Independent samples t-tests | Physicians also reported that the simulation was a much better learning tool than the standardized patient model as they felt more comfortable and free to make decisions within the virtual space | ||
| Gender: 54% male (74% attending, 26%, residents) | Repeated measures ANOVA | Statistically significant changes at 1-month follow-up in accurate beliefs about the use of antibiotics. For lower activated patients, statistically significant increases in confidence in ability to ask their physician questions and preference for being actively involved in the decision-making process with their provider | ||
| Patients | ||||
| Promote effective communication and collaborative decision-making skills in patients | N=34 | – | – | |
| To improve patients’ understanding and beliefs about the correct usage of antibiotics | Average age, 57.6 years; patients were drawn from New York City’s Health + Hospital Bellevue Ambulatory Care Practice; gender (47% male); literacy level (7-8th grade, 32.4%; high school, 67.6%) | – | Statistically significant increase from pre- to post- that remained significant at 1-month follow up point in the accuracy of patients’ beliefs about antibiotics, including: (I) that taking antibiotics when they have a cold will not help them get better more quickly; (II) that their doctor should not prescribe an antibiotic when they experience common cold symptoms; (III) that they should not stop taking their antibiotics when starting to feel better. Satisfaction data: 87% would recommend simulation to friends and family; 97% rated it as a very useful tool saying that it would help them to be better prepared for a doctor’s appointment, increase their assertiveness when communicating with their physician, and to help them create a treatment plan and learn specific content about antibiotics |
|
Data used in this table was the result of funding by the Robert Wood Johnson Foundation: study PI was Antoinette Schoenthaler, EdD, Population Health and Medicine, NYU School of Medicine, Center for Healthful Behavior Change.
Table 6. Results from Change Talk: A simulation designed for pediatricians and other health professionals to develop motivational interviewing to bring about change in the behaviors of parents and children related to reducing the risk of childhood obesity.
| Simulation goals | Sample size & demographics | Study design | Results |
|---|---|---|---|
| Promote the effective use of motivational interviewing to bring about change in patients who are experiencing childhood obesity and gaining buy-in of primary caretakers in support of treatment recommendations | N=26,200 | Within group longitudinal study (post simulation survey, 1-month follow up survey) | 97% of physicians were “satisfied” with the simulation; 78% said they were “very satisfied” or “extremely satisfied” |
| N=307 completed pre-, post- and follow-up surveys for continuing medical education credits | Descriptive and qualitative | In the post-simulation survey, 93% said that as result of participating in the simulation, they intend to make a change in practice to provide better patient care | |
| In the 1-month follow up survey, 88% said that they did make a change as a result of the simulation. Changes included: (I) asking patients if it is ok to talk about healthy eating, (II) doing more motivational interviewing, (III) placing “more emphasis on meeting patients at their current stage of change instead of moving to action plan, (IV) eliciting “increased buy-in and completion of recommendations made to youth and primary caretaker(s) |
|||
| Average experience time was 16 minutes (experience is designed to be 10–12 minutes) and about 20% of users visited the app more than once |
Data used in this table was from the American Academy of Pediatrics (AAP) Continuing Medical Education serving. The simulation was developed in collaboration with AAP, Institute for Healthy Childhood Weight.
Discussion
The summary data of the above six studies show that the Kognito simulations are effective on several levels:
Generalizability
The simulations are effective in driving sustainable changes in skills, self-efficacy, and behavior no matter the target population (e.g., healthcare professionals, patients, educators, students, or military families). This generalizability of impact is due in part to the advantage of providing users with the ability to practice in a risk-free environment, thus reducing the anxiety typically present in face-to-face role-plays, and the neutrality of the virtual humans which makes it easier for the user to open up. This is further supported by a recent study demonstrating a significant impact of four Kognito simulations with Native American and Alaska Native learners (52).
Efficiency
The simulations included in these studies ranged from some with one 10-minute simulated conversation to some with three 10–15-minute simulated conversations. The studies show that a brief 10-minute simulation can result in significant changes which can be further enhanced with additional practice opportunities over time.
Skill building
The simulations result in statistically and sustained changes in the level of users’ preparedness to effectively manage health conversations. The skills include conversation skills such as those associated with motivational interviewing and shared-decision making covered in the Kognito Behavior Change Model.
Self-efficacy
Practicing the simulations yielded an increase in self-efficacy or one’s perceived ability to manage conversations in real life. Measures of self-efficacy were based on Bandura’s integrative framework of personal efficacy: the level of confidence in ability predicts the level of control of behavior (53). By mastering one’s ability, Bandura theorizes that people are more likely to change and improve their behavior in future circumstances (53). Thus, combining user skill acquisition with increased self-efficacy has yielded a host of self-reported, positive behavioral changes pending the simulation and its associated goals.
Satisfaction with user experience
Users were highly satisfied with the simulations, reporting that the scenarios with the virtual humans were relevant and similar to situations they face in real life, and more than 90% said they would recommend it to their colleagues.
Engagement
Important components of assessing user engagement is the duration of time users spend engaged with the simulation and the frequency of re-playing it. In the two studies that examined these elements, it was shown that users often spent more time in the simulation than required and a significant portion of them decided to play it more than once. When queried why they spent more time, users stated they were curious about different reactions, were having fun, wanted to explore different approaches, and even see the results of instigating a negative response from the virtual humans in the simulation.
User behavior change
Another positive effect of the simulations is that users showed statistically significant changes in the frequency they decided to initiate a health conversation which resulted in statistically significant changes in self-reported targeted behavior changes (e.g., number of referrals to mental health services of students by teachers, number of screening and brief interventions conducted by primary care professionals, and communication style of pediatricians when speaking with parents and children about obesity prevention).
Users changing the behaviors of others
The Family of Heroes simulation seeks to better equip military families with the skills and motivation to speak with their veterans about seeking help for post-deployment stress. The results of families practicing this simulation nearly doubled the number of veterans who sought help. With over 62,000 individuals in NY/NJ accessing the simulation, we can project an outcome of thousands of additional veterans deciding to seek help as a result of a family member engaging in a Kognito conversation.
Conclusions
In a broader sense, Kognito simulations have demonstrated a capability to address major health and public health concerns where effective conversations are necessary to bring about changes in social, emotional, and physical health. Whether online or mobile, there is a research-proven approach to create realistic and risk-free learning environments that are contextually rich and enable users to harness the power of conversations and positively impact their health and the health of others. Innovative use of these types of simulations increases participant engagement so learners not only enjoy the experience but also find themselves transformed from passive receivers to active constructors of the learning experience.
Additional research is needed to: (I) conduct randomized controlled trials that examine the impact on long term health outcomes of those approached by individuals who completed a Kognito conversation; (II) determine the value of repeated practice opportunities over longer time periods in sustaining motivation and capability to impact health behaviors through conversations; and (III) compare the efficacy of simulated role-plays with face-to-face and other methods to bring about changes in health behaviors. In conclusion, the authors are truly excited about the possibilities of reaching large numbers of geographically dispersed and often vulnerable populations to bring about positive changes in people’s lives.
Acknowledgements
None.
Footnotes
Conflicts of Interest: G Albright and R Goldman are members of Kognito; C Adam, D Serri and S Bleeker are employees of Kognito.
References
- 1.Levinson W, Pizzo PA. Patient-physician communication: it's about time. JAMA 2011;305:1802-3. 10.1001/jama.2011.556 [DOI] [PubMed] [Google Scholar]
- 2.Briggs K, Mellinger S. Guardian of the Golden Gate: Protecting the Line Between Hope and Despair. Olathe: Ascend Books, 2015. [Google Scholar]
- 3.Nestel D, Tierney T. Role-play for medical students learning about communication: guidelines for maximising benefits. BMC Med Educ 2007;7:3. 10.1186/1472-6920-7-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stevenson K, Sander P. Medical students are from Mars--business and psychology students are from Venus--- University teachers are from Pluto? Med Teach 2002;24:27-31. 10.1080/00034980120103441 [DOI] [PubMed] [Google Scholar]
- 5.Baumeister RF, Twenge JM, Nuss CK. Effects of social exclusion on cognitive processes: anticipated aloneness reduces intelligent thought. J Pers Soc Psychol 2002;83:817-27. 10.1037/0022-3514.83.4.817 [DOI] [PubMed] [Google Scholar]
- 6.Bolte A, Goschke T, Kuhl J. Emotion and intuition. Psychol Sci 2003;14:416-21. 10.1111/1467-9280.01456 [DOI] [PubMed] [Google Scholar]
- 7.Kuhlmann S, Piel M, Wolf OT. Impaired memory retrieval after psychosocial stress in healthy young men. J Neurosci 2005;25:2977-82. 10.1523/JNEUROSCI.5139-04.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lupien SJ, Gaudreau S, Tchiteya BM, et al. Stress-induced declarative memory impairment in healthy elderly subjects: relationship to cortisol reactivity. J Clin Endocrinol Metab 1997;82:2070-5. [DOI] [PubMed] [Google Scholar]
- 9.Payne JD, Jackson ED, Ryan L, et al. The impact of stress on neutral and emotional aspects of episodic memory. Memory 2006;14:1-16. 10.1080/09658210500139176 [DOI] [PubMed] [Google Scholar]
- 10.Payne JD, Jackson ED, Hoscheidt S, et al. Stress administered prior to encoding impairs neutral but enhances emotional long-term episodic memories. Learn Mem 2007;14:861-8. 10.1101/lm.743507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smallwood J, Fitzgerald A, Miles LK, et al. Shifting moods, wandering minds: negative moods lead the mind to wander. Emotion 2009;9:271-6. 10.1037/a0014855 [DOI] [PubMed] [Google Scholar]
- 12.McGaghie WC, Siddall VJ, Mazmanian PE, et al. Lessons for continuing medical education from simulation research in undergraduate and graduate medical education: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest 2009;135:62S-68S. 10.1378/chest.08-2521 [DOI] [PubMed] [Google Scholar]
- 13.Lane C, Rollnick S. The use of simulated patients and role-play in communication skills training: a review of the literature to August 2005. Patient Educ Couns 2007;67:13-20. 10.1016/j.pec.2007.02.011 [DOI] [PubMed] [Google Scholar]
- 14.Rosenbaum ME, Ferguson KJ, Lobas JG. Teaching medical students and residents skills for delivering bad news: a review of strategies. Acad Med 2004;79:107-17. 10.1097/00001888-200402000-00002 [DOI] [PubMed] [Google Scholar]
- 15.Andrade AD, Bagri A, Zaw K, et al. Avatar-mediated training in the delivery of bad news in a virtual world. J Palliat Med 2010;13:1415-9. 10.1089/jpm.2010.0108 [DOI] [PubMed] [Google Scholar]
- 16.Aspegren K. BEME Guide No. 2: Teaching and learning communication skills in medicine-a review with quality grading of articles. Med Teach 1999;21:563-70. 10.1080/01421599978979 [DOI] [PubMed] [Google Scholar]
- 17.Joyner B, Young L. Teaching medical students using role play: twelve tips for successful role plays. Med Teach 2006;28:225-9. 10.1080/01421590600711252 [DOI] [PubMed] [Google Scholar]
- 18.Driscoll MP. Chapter Heading. In: Driscoll MP. Psychology of learning for instruction. 3rd edition. Boston, MA: Pearson Allyn & Bacon, 2014: 153-82. [Google Scholar]
- 19.Merriam SB. Adult learning theory for the twenty-first century. New Directions for Adult and Continuing Education 2008;2008:93-8.
- 20.Black JB. An embodied/grounded cognition perspective on educational technology. In: Khine MS, Saleh IM. New science of learning. New York: Springer, 2010: 45-52. [Google Scholar]
- 21.Lave J, Wenger E. Situated learning: Legitimate peripheral participation. Cambridge: Cambridge University Press; 1991. [Google Scholar]
- 22.Ericsson KA, Prietula MJ, Cokely ET. The making of an expert. Harv Bus Rev 2007;85:114-21, 193. [PubMed] [Google Scholar]
- 23.van Merriënboer JJ, Sweller J. Cognitive load theory and complex learning: Recent developments and future directions. Educational Psychology Review 2005;17:147-77. 10.1007/s10648-005-3951-0 [DOI] [Google Scholar]
- 24.van de Wiel MW, Van den Bossche P, Janssen S, et al. Exploring deliberate practice in medicine: how do physicians learn in the workplace? Adv Health Sci Educ Theory Pract 2011;16:81-95. 10.1007/s10459-010-9246-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller WR. Motivational interviewing with problem drinkers. Behavioural Psychotherapy 1983;11:147-72. 10.1017/S0141347300006583 [DOI] [Google Scholar]
- 26.Miller WR, Rollnick S. Applications of motivational interviewing. In: Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3rd edition. New York: Guilford press; 2012. [Google Scholar]
- 27.Miller WR, Rollnick S. Motivational interviewing: Helping people change. 3rd edition. New York: Guilford press; 2012. [Google Scholar]
- 28.Bateman A, Fonagy P. Mentalization based treatment for borderline personality disorder. World Psychiatry 2010;9:11-5. 10.1002/j.2051-5545.2010.tb00255.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bateman AW, Fonagy P. Mentalization-based treatment of BPD. J Pers Disord 2004;18:36-51. 10.1521/pedi.18.1.36.32772 [DOI] [PubMed] [Google Scholar]
- 30.Allen JG, Fonagy P. editors. The handbook of mentalization-based treatment. Malden: John Wiley & Sons; 2006. [Google Scholar]
- 31.Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev 2004;3:71-100. 10.1177/1534582304267187 [DOI] [PubMed] [Google Scholar]
- 32.Stotland E. Exploratory investigations of empathy. In: Berkowitz L. editors. Advances in experimental social psychology. New York: Academic Press, 1969;4:271-314. [Google Scholar]
- 33.Gallagher HL, Frith CD. Functional imaging of 'theory of mind'. Trends Cogn Sci 2003;7:77-83. 10.1016/S1364-6613(02)00025-6 [DOI] [PubMed] [Google Scholar]
- 34.Völlm BA, Taylor AN, Richardson P, et al. Neuronal correlates of theory of mind and empathy: a functional magnetic resonance imaging study in a nonverbal task. Neuroimage 2006;29:90-8. 10.1016/j.neuroimage.2005.07.022 [DOI] [PubMed] [Google Scholar]
- 35.Şahin M. An investigation into the efficiency of empathy training program on preventing bullying in primary schools. Children and Youth Services Review 2012;34:1325-30. 10.1016/j.childyouth.2012.03.013 [DOI] [Google Scholar]
- 36.Pecukonis EV. A cognitive/affective empathy training program as a function of ego development in aggressive adolescent females. Adolescence 1990;25:59-76. [PubMed] [Google Scholar]
- 37.Riess H, Kelley JM, Bailey R, et al. Improving empathy and relational skills in otolaryngology residents: a pilot study. Otolaryngol Head Neck Surg 2011;144:120-2. 10.1177/0194599810390897 [DOI] [PubMed] [Google Scholar]
- 38.Ickes W. Empathic accuracy. Journal of Personality 1993;61:587-610. 10.1111/j.1467-6494.1993.tb00783.x [DOI] [Google Scholar]
- 39.Zaki J, Bolger N, Ochsner K. It takes two: the interpersonal nature of empathic accuracy. Psychol Sci 2008;19:399-404. 10.1111/j.1467-9280.2008.02099.x [DOI] [PubMed] [Google Scholar]
- 40.Lakey B, Drew JB. A social-cognitive perspective on social support. In: Pierce GR, Lakey B, Sarason IG, et al. editors. Sourcebook of social support and personality. New York: Springer US, 1997: 107-40. [Google Scholar]
- 41.Noller P, Venardos C. Communication awareness in married couples. Journal of Social and Personal Relationships 1986;3:31-42. 10.1177/0265407586031003 [DOI] [Google Scholar]
- 42.Mascaro JS, Rilling JK, Tenzin Negi L, et al. Compassion meditation enhances empathic accuracy and related neural activity. Soc Cogn Affect Neurosci 2013;8:48-55. 10.1093/scan/nss095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gross JJ, Thompson RA. Emotion regulation: Conceptual foundations. In: Gross JJ. editor. New York: Guilford Press; 2007. [Google Scholar]
- 44.Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann N Y Acad Sci 2012;1251:E1-24. 10.1111/j.1749-6632.2012.06751.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gross JJ. The emerging field of emotion regulation: an integrative review. Review of General Psychology 1998;2:271-99. 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- 46.Kross E, Ayduk O. Facilitating adaptive emotional analysis: distinguishing distanced-analysis of depressive experiences from immersed-analysis and distraction. Pers Soc Psychol Bull 2008;34:924-38. 10.1177/0146167208315938 [DOI] [PubMed] [Google Scholar]
- 47.Woud ML, Holmes EA, Postma P, et al. Ameliorating intrusive memories of distressing experiences using computerized reappraisal training. Emotion 2012;12:778-84. 10.1037/a0024992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Erk S, Mikschl A, Stier S, et al. Acute and sustained effects of cognitive emotion regulation in major depression. J Neurosci 2010;30:15726-34. 10.1523/JNEUROSCI.1856-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Macnamara A, Ochsner KN, Hajcak G. Previously reappraised: the lasting effect of description type on picture-elicited electrocortical activity. Soc Cogn Affect Neurosci 2011;6:348-58. 10.1093/scan/nsq053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Albright G, Goldman R, Shockley KM, et al. Using an Avatar-Based Simulation to Train Families to Motivate Veterans with Post-Deployment Stress to Seek Help at the VA. Games Health J 2012;1:21-8. 10.1089/g4h.2011.0003 [DOI] [PubMed] [Google Scholar]
- 51.Using Role-Play Simulations with Virtual Humans to Train Healthcare Providers to Screen and Manage Patients with Depression and Suicidal Ideation, 2015. Available online: http://crise.ca/iasp2015/default_141.html
- 52.Bartgis J, Albright G. Online role-play simulations with emotionally responsive avatars for the early detection of Native youth psychological distress, including depression and suicidal ideation. Am Indian Alsk Native Ment Health Res 2016;23:1-27. 10.5820/aian.2302.2016.1 [DOI] [PubMed] [Google Scholar]
- 53.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]