Abstract
Background:
Adnexal tumours are frequently diagnosed in asymptomatic postmenopausal women due to more liberal use of modern high-resolution imaging. This study's objective was to determine if there would be a difference in the intervention rates when using the Simple Rules Management Protocol (SRMP) as compared to the Risk of Malignancy Index in the Royal College of Obstetricians and Gynaecologists guideline (RMI/RCOG).
Methods:
This was a prospective randomised controlled trial with the participants and the researchers non-blinded, and the surgeons and pathologists blinded. We recruited pain-free postmenopausal women who were diagnosed with an adnexal tumour on ultrasound scan. Women were randomised to either of the two protocols, which then determined if they were offered conservative or surgical management. An intention-to-treat analysis was performed. The primary outcome measure was rate of surgical interventions for ovarian cysts up to 12 months after randomisation. The secondary outcome measures were the number of staging surgical procedures, surgical complications and number of delayed diagnoses of ovarian cancer.
Results:
A total of 148 women were randomised over 39 months with 73 in the RMI/RCOG arm and 75 in the SRMP arm with outcome data for 136 at 12 months. The two groups were balanced in terms of age, length of time since menopause and use of hormone replacement therapy. There were 18 out of 68 (28.1%) women in the RMI/RCOG arm who had surgery vs 7 out of 68 (10.3%) women in the SRMP arm (P=0.015, χ2-test). The difference in these proportions was 16.2% (95% confidence interval (CI): 3.4–28.9%) and the relative risk was 2.57 (95% CI: 1.15–5.76). There were no significant differences in the number of staging surgical procedures and the surgical complications between the two groups and there were no delayed diagnoses of ovarian cancer at 12 months.
Conclusions:
Surgical intervention rates in asymptomatic postmenopausal women with an ultrasound diagnosis of adnexal tumours are significantly lower when the novel SRMP protocol is used for triaging compared to the standard RMI/RCOG protocol without an increase in delayed malignant diagnoses.
Keywords: adnexal tumours, postmenopausal, ultrasound, ovarian cancer, ovarian cysts, management, Risk of Malignancy Index, Simple Rules
In recent years, there has been an increase in the number of women diagnosed with asymptomatic adnexal tumours. This is mainly due to liberal use of modern high-resolution abdominal and pelvic imaging such as ultrasound, MRI and CT. The diagnosis of an adnexal tumour often causes concern to women and health professionals due to perceived difficulties in distinguishing between benign and malignant ovarian tumours.
The best survival rates for patients with ovarian cancer are achieved when treatment is organised and carried out by gynaecological oncologists who work in cancer centres (Vernooij et al, 2007). However, women with asymptomatic benign tumours can be managed expectantly or by minimally invasive surgery. These procedures can be safely undertaken by general gynaecologists in their local hospitals. Achieving the right balance between the desire to treat all ovarian cancers effectively and without delay against the need to avoid unnecessary interventions in women with benign and clinically insignificant lesions is particularly important in postmenopausal women. They are more likely to have age–related, co-morbid conditions such as cardiac or pulmonary disease or diabetes mellitus that increase their risk of surgical and anaesthetic complications. They are also more likely to have had previous abdominal operations increasing further their risk of surgical complications (Ben-Ami et al, 2006; Ansaloni et al, 2010; Neufeld et al, 2013; Sztark et al, 2013; Krause et al, 2016).
In 2003 the Royal College of Obstetricians and Gynaecologists (RCOG) published a guideline on the management of ovarian cysts in postmenopausal women, which was reviewed with no changes in 2010 (RCOG, 2003). The guideline uses the Risk of Malignancy (RMI; Jacobs et al, 1990) model-based management protocol (RMI/RCOG) to facilitate triaging of women with adnexal tumours for surgery and it provides guidance as to whether the operation should be carried in a specialised cancer centre or by a general gynaecologist. In 2008 the International Ovarian Tumor Analysis collaboration developed a novel ultrasound-based diagnostic model ‘Simple Rules' (SR) for the differential diagnosis between benign and malignant adnexal tumours (Timmerman et al, 2008). This SR model has been incorporated into the RCOG Green Top guideline for the management of ovarian cysts in premenopausal women (RCOG, 2011). Reviews of published literature showed that the SR model may be more sensitive than RMI for the diagnosis of ovarian cancer (Geomini et al, 2009; Kaijser et al, 2014; Nunes et al, 2014). The SR model defines tumours as benign, indeterminate and malignant. Using the SR diagnostic model we developed a new protocol for the management of postmenopausal women diagnosed with adnexal cysts. This new ‘Simple rules management protocol' (SRMP) uses similar approach to the standard RMI/RCOG protocol and classifies adnexal lesions as low, intermediate and high risk of malignancy. The literature has found indeterminate tumours to have an intermediate risk of 18–45% of being malignant. This was used to compare with the RMI/RCOG protocol, which had an intermediate risk of malignancy of 20% (RCOG, 2003; Timmerman et al, 2008; Nunes et al, 2014).
In our previous pilot study on a sample of 67 women we found that 41 out of 67 (61.2% 95% confidence interval (CI): 48.5–72.9%) women would be offered surgery according to the RMI/RCOG protocol compared to 5 out of 67 (7.5%: 95% CI: 2.5–16.6%) when SRMP was used for triage (Nunes et al, 2012). The aim of this prospective randomised trial was to determine whether there are significant differences in the actual surgical intervention rates between the two management protocols for the management of postmenopausal women with incidentally detected adnexal tumours. Secondary outcomes were the number of staging surgical procedures, surgical complications and number of delayed diagnoses of ovarian cancer in the two groups.
Materials and methods
This was a prospective non-blinded single-centre randomised controlled trial conducted in an outpatient gynaecology clinic at University College Hospital, London, UK. Asymptomatic postmenopausal women who were diagnosed with adnexal tumours on ultrasound scan or other imaging modalities were invited to join the study.
The North London Research Ethical Committee 2 as well as the research and development committee at UCH approved the randomised controlled trial (10/H0724/48).
Study participants
Eligible women were identified when they attended the general gynaecology clinic, were postmenopausal and were found to have an adnexal tumour and no recent history of pelvic pain. An information leaflet about the study was given to all eligible women before assessment. They were then reviewed by a member of the research team who took a detailed clinical history, did a physical examination and performed an ultrasound scan. If the diagnosis of an adnexal mass was confirmed women were invited to join the study. Written informed consent was obtained from all women who agreed to take part.
Women were considered to be asymptomatic if they did not present with pain localised to the area of the cyst or the lower pelvis. Postmenopausal women were defined as those who had had 1 year of spontaneous amenorrhoea at or above the age of 40 where no illness or medication had caused the cessation of periods, or those at or above the age of 50 who had had a hysterectomy with ovarian conservation. Women aged 40–80 inclusive were eligible. We excluded all women who were unable or unwilling to give written consent and those with simple, unilateral, unilocular cysts of <2 cm. Women referred for an ultrasound scan from the tertiary oncology unit were excluded as majority of them had already had an RMI done and were usually aware of their results. In addition, they had already been informed that they were likely to have an ovarian cancer, which would require surgical or other treatment.
Severe pelvic adhesions were determined by the women's history (multiple laparotomies, frozen pelvis at previous operation) and examination (immobility of the cyst, frozen pelvis on ultrasound scan and/or presence of a peritoneal pseudo-cyst). Women who had already been booked for urogynaecological or general gynaecological surgery were also excluded.
Randomisation and blinding
A blocked randomisation list with varying block sizes was generated by an independent statistician using Stata 12.1 (Stata Corp., College Station, TX, USA). The randomisation numbers were placed in consecutively numbered, sealed, opaque envelopes and kept in a box locked in a filing cabinet. This randomisation ensured allocation concealment. When a patient consented, a clinic nurse, who was not part of the research team, opened the next envelope and informed the recruiting doctor of woman's trial allocation.
Neither the patient nor the recruiting doctors were blinded to the protocol allocation but the operating surgeons and the pathologists were. The surgeons were informed whether the tumour was of high or intermediate risk of cancer, but not about the protocol, which was used to determine that. The pathologist was informed of the operative findings only and their report was used to determine the nature of adnexal tumours.
Procedures
The women were randomised into either of the two groups. The first group was assessed and managed in accordance with the current RMI/RCOG protocol for the management of cysts in postmenopausal women (RCOG, 2003). The second group of women were assessed using a structured approach to morphological analysis of ovarian tumours referred to as SRMP, which enables discrimination between benign and malignant lesions without the need to measure tumour markers. According to the literature the SR is more sensitive for the preoperative diagnosis of ovarian cancer (Kaijser et al, 2014).
In the RMI/RCOG arm all the women underwent an ultrasound examination and had a CA125 blood test on the same day. The RMI was calculated as the product of the CA125 (U ml-1) laboratory value, a score for menopausal status (1 if premenopausal and 3 if postmenopausal) and a greyscale ultrasound score of 0, 1 or 3. Ultrasound features were bilaterality, ascites, multilocularity, solid areas and intra-abdominal metastases, and where none were present the score was 0, where 1 was present the score was 1 and where 2–5 were present the score was 3. (RMI=CA125 × M × U; Jacobs et al, 1990).
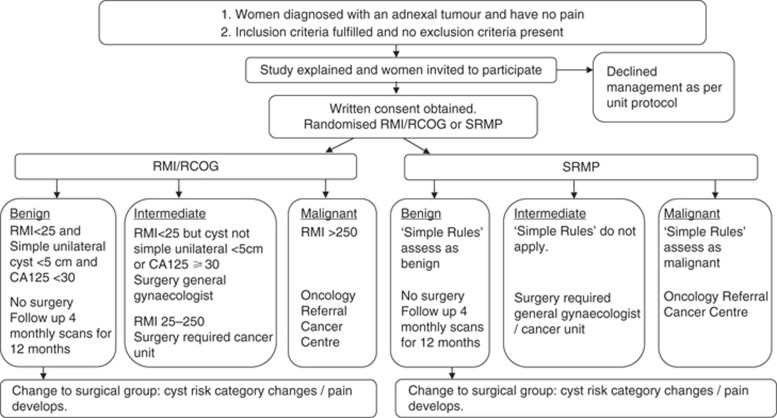
Women with all of the following features were classified as low risk of cancer and were offered conservative management: simple, regular, unilateral, unilocular cysts <5 cm, a CA125<30 U ml-1 and an RMI<25. A simple cyst was defined as a unilocular, anechoic, regular (smooth walls) cyst (Conway, 1998). Those with a RMI of 25–250 were considered to be at intermediate risk and were offered surgical removal by gynaecologists. Those with a RMI<25 but with a cyst which is not simple, unilateral, unilocular and <5 cm were also considered of indeterminate risk. Women with an RMI>250 were referred for surgery to the tertiary cancer centre as they were considered high risk (Figure 1).
Figure 1.
Flow diagram of patient selection and randomisation for the RCT: RCOG/RMI vs SRMP.
The second trial arm used SRMP. Women in this arm had an ultrasound scan assessment according to the Simple Rules Protocol. The ‘SR' uses 10 features to assess adnexal masses. There are five features that predict malignancy (M-features): (1) irregular solid tumour; (2) ascites; (3) at least four papillary structures; (4) irregular multilocular-solid tumour with a largest diameter of at least 100 mm; and (5) very-high-colour content on colour Doppler examination (score 4). There are five features to predict benignity (B-features): (1) unilocular cyst; (2) presence of solid components where the largest solid component has a largest diameter of <7 mm; (3) acoustic shadows; (4) smooth multilocular tumour <100 mm in largest diameter; and (5) no detectable blood flow on Doppler examination (score 1). If one or more M-features apply in the absence of a B-feature, the mass is classified as malignant. If one or more B-features apply in the absence of an M-feature, the mass is classified as benign. If no features apply or both M- and B-features apply, the mass cannot be classified and is considered indeterminate. In the SRMP the indeterminate tumours were classified to be of intermediate risk.
All primary ultrasound scans were performed by NN using a General Electric Voluson E8 ultrasound machine (GE Healthcare, Milwaukee, WI, USA) with a 4–9 MHz transvaginal probe or a Wide Band Convex 2–8 MHz transabdominal probe.
As previously described, women with a cyst classified as benign using SRMP were considered low risk and they were offered conservative management (Nunes et al, 2012). Those classified as malignant were high risk and were managed by gynaecological oncologists in the tertiary oncology unit. Women with tumours of indeterminate nature were considered intermediate risk and were offered surgery by general gynaecologists with interest in cancer.
Women selected for conservative management were offered three 4-monthly ultrasound scans for 12 months. Those within the RMI/RCOG arm had another CA125 test at their final follow-up visit. At follow-up visits women were asked about any change in their symptoms. The tumours were assessed on ultrasound scan looking for any changes in their morphology and size according to the protocol of the trial arm to which they were randomised. Women who began to experience pain or whose tumours were re-classified as intermediate or high risk on follow-up ultrasound scan were offered surgical treatment.
The decision about the surgical approach; that is, open vs minimally invasive, was made by the operating surgeon.
Outcome measures
Primary outcome measure
The primary outcome was the proportion of women who underwent surgery within 12 months from randomisation.
Secondary outcomes
Secondary outcomes included the number of staging surgical procedures carried out by a gynaecological oncologist, which was defined as an operation performed by the gynaecological oncology team where a systematic examination of the pelvis and abdomen was performed looking for metastatic spread with the appropriate biopsies done such as an omental biopsy or lymph node dissection. Other secondary outcomes were the number of women suffering surgical complications and the number of delayed diagnoses of ovarian cancer, which was defined as a diagnosis of an ovarian malignancy beyond the first visit but <1 year.
Statistical analysis
Sample size
A sample size of 148 patients was required to detect a difference of 31% in the intervention rate at the 5% significance level (two-sided) with 90% power, assuming that the intervention rate in RMI/RCOG arm is 62% and that there is 20% dropout.
Statistical analyses
Patients were analysed according to the groups to which they were randomised. The analysis of surgery offered included all randomised patients. The final analysis of those who had surgery included those who had surgery within 1 year or completed 1 year of follow-up ultrasound scans.
The results were described using relative risks (RR) and the risk differences with 95% CIs. The χ2-test was used to formally compare the intervention rates in the two trial arms. Fisher's exact test was used to compare complication rates and staging surgical procedures done by a gynaecological oncologist.
Statistical analysis was performed using Stata 14 software (Stata Corp).
Any adverse events were assessed for severity according to the University College Hospital Trial Coordinating Centre's criteria and recorded in the database.
This study was entered in the registry of randomised trials (ISRCTN89034131).
Results
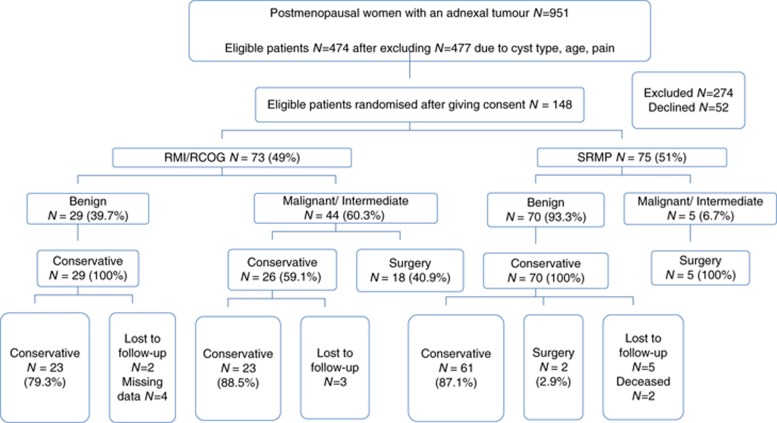
From April 2011 to June 2014, 951 postmenopausal women were diagnosed with adnexal tumours in our centre. The CONSORT flow diagram is seen in Figure 2. After excluding women with simple unilateral, unilocular cysts <2 cm (n=269), those outside the defined age range (n=121) and those with pain (87), there were 474 women remaining. A further 274 were not eligible. About 200 women fulfilled the final inclusion criteria, 148 of whom agreed to take part in the study and 52 of whom declined. About 73 women were randomised to RMI/RCOG and 75 to SRMP. Their ages ranged from 49 to 80 with a mean age of 63. The two groups were balanced in their demographic characteristics (Table 1).
Figure 2.
CONSORT diagram.
Table 1. Baseline patient characteristics by trial arm in the RMI/RCOG and the SRMP arms (N=148).
| RMI/RCOG (n=73) | SRMP (n=75) | |
|---|---|---|
|
Age (years) | ||
| Mean | 62.7 (7.6) | 63.8 (8.1) |
| Range | 49–80 | 50–80 |
|
Parity
n
(%) | ||
| 0 | 22 (30%) | 27 (36%) |
| 1 | 11 (15%) | 8 (11%) |
| 2 | 20 (27%) | 19 (25%) |
| ⩾3 | 20 (27%) | 21 (28%) |
|
Time since menopause (years) | ||
| Mean | 12.5 (8.8) | 13.7 (9.3) |
| Range | 0–37 | 1–33 |
|
Current HRT use
n
(%) | ||
| Yes | 10 (14%) | 11 (15%) |
|
Past HRT use
n(%) | ||
| Yes | 12 (16%) | 19 (25%) |
| No | 49 (67%) | 45 (60%) |
| NA | 10 (14%) | 11 (15%) |
| UK | 2 (3%) | 0 |
Abbreviations: HRT=hormone replacement therapy; NA=not applicable (patients currently using HRT); RCOG=Royal College of Obstetricians and Gynaecologists guideline; RMI=Risk of Malignancy Index; SRMP=Simple Rules Management Protocol; UK=Unknown. Values are either mean (s.d.) for continuous variables or n (%) for categorical variables.
Protocol assessment
About 44 (60.3%) of the RMI/RCOG patients were assessed as either indeterminate or malignant compared with 5 (6.7%) of the SRMP patients (Tables 2 and 3). This study shows that the rate of malignant or indeterminate diagnoses is higher for RMI/RCOG patients (P<0.001, χ2-test). The difference in these proportions is 53.6% (95% CI: 41.0–66.2%) and the RR is 9.0 (95% CI: 3.8–21.5). While there was one tumour assessed as malignant in each arm. The main difference was in the intermediate groups with 43 in the RMI/RCOG arm and 4 in the SRMP arm (Table 2).
Table 2. Patient assessment, follow-up and outcomes N=148.
| RMI/RCOG (n=73) n (%) | SRMP (n=75) n (%) | |
|---|---|---|
|
Protocol assessment classification | ||
| Protocol=Benign | 29 (39.7%) | 70 (93.3%) |
| Protocol=Indeterminate | 43 (58.9%) | 4 (5.3%) |
| Protocol=Malignant | 1 (1.4%) | 1 (1.3%) |
| Protocol=Surgery | 44 (60.3%) | 5 (6.7%) |
|
Study completion | ||
| Completed 4 months | 72 (98.6%) | 75 (100%) |
| Completed 8 months | 69 (94.5%) | 70 (93.3%) |
| Completed 12 months of study | 68 (93.2%) | 68 (90.7%) |
|
Surgical management | ||
| Surgery ⩽1 year | 18 (24.7%) | 7 (9.3%) |
| Declined/unfit for surgery | 26 (35.6%) | 0 |
Abbreviations: RCOG=Royal College of Obstetricians and Gynaecologists guideline; RMI=Risk of Malignancy Index; SRMP=Simple Rules Management Protocol.
Table 3. Results according to risk category N=148.
| RMI/RCOG (N=73) n (%) | SRMP (N=75) n (%) | |
|---|---|---|
|
Low risk | ||
| Assigned to category | 29 (39.7%) | 70 (93.3%) |
| Primary non-staging surgery, benign outcome | 0 | 0 |
| Primary non-staging surgery, malignant outcome | 0 | 0 |
| Primary staging surgery, benign outcome | 0 | 0 |
| Primary staging surgery, malignant outcome | 0 | 0 |
| Accepted follow-up | 29 (100%) | 70 (100%) |
| Completed follow-up | 23 (79.3%) | 61 (87.1%) |
| Lost to follow-up/missing data/deceased | 6 (20.7%) | 7 (10.0%) |
| Secondary non-staging surgery, benign outcome | 0 | 0 |
| Secondary non-staging surgery, malignant outcome | 0 | 0 |
| Secondary staging surgery, benign outcome | 0 | 2 (2.7%)a |
| Secondary staging surgery, malignant outcome | 0 | 0 |
|
Intermediate risk | ||
| Assigned to category | 43 (58.9%) | 4 (5.3%) |
| Primary non-staging surgery, benign outcome | 16 (37.2%) | 1(25.0%) |
| Primary non-staging surgery, malignant outcome | 0 | 1 (25.0%)b |
| Primary staging surgery, benign outcome | 0 | 0 |
| Primary staging surgery, malignant outcome | 1 (2.3%)c | 2 (50.0%)d |
| Requested ultrasound scan follow-up | 19 (44.2%) | 0 |
| Not fit for surgery, ultrasound scan follow-up | 7 (16.3%) | 0 |
| Surgery during follow-up | 0 | 0 |
|
High risk | ||
| Assigned to category | 1 (1.4%) | 1 (1.3%) |
| Primary non-staging surgery, benign outcome | 0 | 0 |
| Primary non-staging surgery, malignant outcome | 0 | 0 |
| Primary staging surgery, benign outcome | 0 | 0 |
| Primary staging surgery, malignant outcome | 1 (100%)e | 1 (100%)e |
| Referred tertiary oncology unit | 1 | 1 |
| Requested ultrasound scan follow-up | 0 | 0 |
| Not fit for surgery, follow-up | 0 | 0 |
| Surgery during follow-up | 0 | 0 |
|
Total patients | ||
| Surgery | 18 | 7 |
| Primary surgery | 18 | 5 |
| Primary surgery, benign outcome | 16 | 1 |
| Primary surgery, malignant outcome | 2 | 4 |
| Secondary surgery | 0 | 2 |
| Secondary surgery, benign outcome | 0 | 2 |
| Secondary surgery, malignant outcome | 0 | 0 |
Abbreviations: RCOG=Royal College of Obstetricians and Gynaecologists guideline; RMI=Risk of Malignancy Index; SRMP=Simple Rules Management Protocol.
Referred to oncology: one diagnosed with breast cancer, one diagnosed with endometrial cancer.
Papillary thyroid cancer probably having arisen in a dermoid.
Metastatic bowel cancer.
Two borderline ovarian tumours.
Borderline ovarian tumour.
Initial management
Out of the 44 women triaged for surgery in the RMI/RCOG arm, 18 (40.9%) had surgery as planned, 7 (15.9%) were not fit for surgery and 19 (43.2%) declined the operation for various reasons. All women who declined surgery were in the intermediate-risk group. All five women assigned to surgery in the SRMP arm had operations.
Thus, following the initial assessment, 18 out of 73 (24.7%) RMI/RCOG patients had surgery compared to 5 out of 75 (6.7%) SRMP. There is strong evidence that the rate of surgery is higher for RMI/RCOG patients (P=0.003, χ2-test). The difference in these proportions is 18.0% (95% CI: 6.6–29.4%) and the RR is 3.70 (95% CI: 1.45–9.44).
Primary analysis: management at 12 months (‘ITT' analysis)
The surgical status of 136 patients is known at 12 months. There were two women who had surgery during follow-up. One woman was offered surgery because of her personal recent diagnosis of breast cancer and the other was diagnosed with an early endometrial cancer. They were both in the SRMP arm, both operated on by gynaecological oncologists and both adnexal lesions were benign on histological examination. Neither woman had yet had her first follow-up ultrasound scan. After completion of follow-up, 18 out of 68 (26.5%) RMI/RCOG patients had surgery compared to 7 out of 68 (10.3%) in the SRMP arm (Tables 2 and 3). There is strong evidence that the rate of surgery is higher for RMI/RCOG patients (P=0.015, χ2-test). The difference in these proportions is 16.2% (95% CI: 3.4–28.9%) so, therefore, for every 100 patients we expect an additional 16 patients to have surgery after assessment by RMI/RCOG compared to assessment via Simple Rules. The RR is 2.57 (95% CI: 1.15–5.76),so there is a 2.6 times higher chance of surgery following assessment by RMI/RCOG compared to assessment via Simple Rules.
Secondary outcomes
Two women, one in each arm were identified as having high-risk tumours and they both had staging procedures (one laparoscopy and one laparotomy) by gynaecological oncologists. In both cases the histological diagnosis was a borderline tumour.
There were five women with low or intermediate risk tumours who were referred to the tertiary oncology centre. Two women categorised as having benign tumours had secondary staging surgery in the tertiary cancer unit as one of them had a concomitant breast and another endometrial cancer. Three women in the intermediate-risk group also had primary staging surgery. One had a large borderline tumour and it was anticipated that the surgery will be technically difficult, another was known to suffer from bowel cancer and the third woman with a borderline cyst was referred directly to the cancer centre by her GP and had surgery there.
There was little difference in the proportions of women referred to the tertiary oncology unit between the two groups of women (3 out of 73 (4.1%) in RMI/RCOG and 4 out of 75 (5.3%) in SRMP). The risk difference was 1.2% (95% CI: −0.6 to 2.9%). The RR was 1.28 (95% CI: 0.3–5.54; P=0.74).
Surgical complications occurred in 4 out of 73 (5.5%) women in the RMI/RCOG arm and 2 out of 75 (2.7%) in the SRMP arm. This was not statistically significant when either a total number of women in each arm or a total number of women who underwent surgical procedures in each arm were used as denominators. There were no delayed diagnoses of ovarian cancer detected up to 12 months of follow-up by the assigned protocol assessment.
Histological diagnoses are listed in Table 4. There were 25 women who had their surgery within the first year following the initial assessments. Six women with malignant tumours on histology (two invasive tumours and four borderline tumours) were identified as high or intermediate risks by either diagnostic model. Five of them had surgery within 2 months of the initial visit, while the remaining woman with a cardiac condition had her surgery delayed for 8 months in order to optimise her general health. There was one invasive malignancy and one borderline tumour in the RMI/RCOG arm and one invasive malignancy, and three borderline tumours in the SRMP arm.
Table 4. Histological diagnoses N=26.
| RMI/RCOG (N=73) n (%) | SRMP (N=75) n (%) | |
|---|---|---|
|
Benign | ||
| Cystadenoma/cystadenofibroma (two with a fibroma and one with a Brenner tumour) | 8 | 3 |
| Endometriomas | 3 | |
| Fibroma | 2 | |
| Fibrothecoma | 1 | |
| Benign stromal tumour and simple cyst | 1 | |
| Inclusion cyst with hydrosalpinx | 1 | |
| Total benign (n=19) | 16 | 3 |
|
Borderline | ||
| Borderline serous | 1 | 2 |
| Borderline mucinous (with a contralateral benign serous cystadenoma) | 1 | |
| Total borderline (n=4) | 1 | 3 |
|
Invasive malignancies | ||
| Papillary thyroid type carcinoma within a dermoid | 1 | |
| Metastatic colorectal cancer | 1 | |
| Total invasive malignancies (n=2) | 1 | 1 |
| Total patients who had surgery | 18 | 7 |
Abbreviations: RCOG=Royal College of Obstetricians and Gynaecologists guideline; RMI=Risk of Malignancy Index; SRMP=Simple Rules Management Protocol.
About 23 out of 26 (88.5%) women, who were assessed as needing surgery but were either deemed surgically unfit (7) or declined operations (19), completed their 12 months follow-up without any morphological changes that altered their category assessment. Two of them went on to have surgery after 1 year. They were found to have benign lesions on histological examination. Of the remaining three women who did not attend for follow-up visits, one had her 12-month scan elsewhere. The examination did not reveal any significant changes in the appearance of her adnexal lesion. We had no information about the remaining two women who were lost to follow-up. There were two women in the SRMP arm who had tumours classified as benign, who died before completing their 12 months of follow-up. One patient was diagnosed with small-cell lung cancer and the other was diagnosed with acute lymphoblastic leukaemia.
Discussion
Main findings
Our study has shown that the intervention rates were significantly higher in the RMI/RCOG protocol arm compared to women the SRMP arm. This occurred without an increase in delayed diagnoses of ovarian cancer during the 12 months of follow-up. The proportion of women classified as having high-risk tumours was the same in both arms of the study and the main difference between the protocols was in the proportions of women who were classified as having intermediate-risk lesions.
The significant difference in number of lesions classified as intermediate risk led to a significant difference in the actual intervention rates as well. This indicates that a large proportion of postmenopausal women with adnexal tumours in the United Kingdom may be undergoing unnecessary operations that could be avoided. Women classified as having tumours of intermediate risk are often anxious about the possibility of having an aggressive invasive tumour, which may have adverse effect of their psychological health and social well-being. The UKCTOCS trial found significantly higher anxiety levels in women with abnormal results on ultrasound screening (Barrett et al, 2014). The cost of surgery is high and avoiding unnecessary operations may result in significant savings to health providers and to society as a whole.
A relatively large number of women with intermediate-risk lesions in the RMI/RCOG arm of the study declined surgery. This could be partially explained by the delay in proving women with the risk assessment until the CA125 results were available. The majority of women who required intervention in the RMI group had relatively simple cysts and they were told that their RMI ultrasound score was low. However, when the result of serum CA125 became available their cysts were classified as intermediate risk. This could explain the higher non-compliance in this arm of the study. This trend was absent in the SRMP arm as the women assigned to this protocol were provided with instant information on the likely tumour nature and advice and management. In addition, women who have a priori preference for surgery are likely to have declined to participate in this study and to have directly requested surgical intervention. During follow-up of the intermediate-risk women who declined surgery, none of them had their cysts re-classified as high risk. This was the case for all women who had expectant care with follow-up ultrasound scans over 1 year.
The cysts that were indeterminate according to the SRMP analysis are the cysts where the rules were not applicable. This was only 5% (4 out of 75) of the women in that arm of the study. A recent meta-analysis showed that the proportion of women in whom the Simple Rules were not applicable varied between 10.7 and 23.9% (Nunes et al, 2014). However, all studies included in the meta-analysis were carried out on women who were scheduled to have surgical treatment. Our population was different as we only included asymptomatic women who attended outpatient clinics. They were more likely to be diagnosed with simple benign-looking cysts. This difference in patient selection could explain the higher relative proportion of cysts classified as benign, compared to other studies.
A significant proportion of women was deemed unfit for surgery, which confirms that the risks of operating on older women are increased and reiterates the need to develop effective strategies to reduce the number of avoidable procedures in this age group.
We decided to follow women up for 12 months, as there is evidence from the literature that this is a sufficient time span to detect changes in the morphology and size of the adnexal tumours, which could indicate their malignant nature (Horiuchi et al, 2003; Shih and Kurman, 2004; Suh-Burgmann et al, 2014). A study by Horiuchi et al (2003) showed that the majority of women who developed ovarian cancer in previously detected cysts had either borderline tumours or well-differentiated early stage invasive lesions. These results support a conservative approach to the care of women with benign-looking adnexal lesions on initial ultrasound scans. In contrast women diagnosed with aggressive disseminated invasive ovarian cancers typically had no detectable precursor lesions on previous imaging. Similar findings were also reported by Shih and Kurman (2004) in 2004. Suh-Burgmann et al (2014) found that growth of the tumours was clear by 7 months for all women subsequently diagnosed with a borderline or epithelial tumour when women over age 50 with complex adnexal tumours had ultrasound follow-up of their tumours.
Strengths and limitations
The main strength of our study is that it is the first randomised controlled trial looking at the use of the RMI/RCOG protocol, which is widely used in clinical practice in the United Kingdom and compared it to a novel alternative management strategy. The SR diagnostic model, which underpins our novel management protocol, had been extensively studied in the past and all the results showed that it was suitable for the use in clinical practice. The study was carefully planned and the power calculation was based on the results of a prospective audit, which had been carried out prior to starting the trial. Although it was not possible to blind women and all clinicians to the patient allocation, the pathologist and the surgeons were not aware which protocol was used in individual patients.
The main limitation was that this was a single centre study, which limits the applicability of the results in other units. Further prospective studies in different diagnostic units are needed to ensure that our findings are widely applicable.
We did not blind the recruiting physician once the woman was assigned to an arm of the trial that could have influenced their approach to the conduct of ultrasound scan. We also did not blind the patients to their trial allocation, which could have influenced their compliance with the protocol as they were less likely to follow a new rather than a traditional well-tested approach. Our data showed, however, that the compliance was less with the standard compared to the novel management protocol. Simple Rules require higher ultrasound skill than RMI, which may affect the performance of the test in unit with lower ultrasound skills.
Conclusion
In conclusion our study has shown that the introduction of ‘simple rules' into routine clinical practice could result in a significant reduction in the number of surgical procedures offered to postmenopausal women with incidental diagnoses of adnexal cysts on imaging. Further larger studies, including units with different levels of ultrasound expertise, are required to explore or confirm these findings.
Implications for clinicians or policymakers
This study shows that relatively minor changes in the management protocols for women with adnexal tumours could result in significant differences in the number of surgical interventions. The diagnosis of suspected ovarian cancer often causes anxiety to women and their carers, and they are typically urgently referred to gynaecological oncologists in cancer centres. Algorithms based on models with low specificity would therefore cause significant pressure on sub-specialist services and further increase the cost of care. Further multicentre studies are required to confirm our findings and would facilitate development of more effective and rational care for postmenopausal women with adnexal tumours.
Acknowledgments
I would like to acknowledge Mr Paul Bassett as the statistician who did the sample size calculation and generated the randomisation list. NN, XF, GD were supported by the research fund provided by the Gynaecology Ultrasound Centre Limited, London, UK. GA received a proportion of funding from the UK Department of Health's NIHR Biomedical Research Centre's funding scheme. The first author had full access to all the data in the study and had final responsibility for the decision to submit for publication. Trial registration number: ISRCTN89034131. http://www.controlled-trials.com/ISRCTN89034131/.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflict of interest.
References
- Ansaloni L, Catena F, Chattat R, Fortuna D, Franceschi C, Mascitti P, Melotti RM (2010) Risk factors and incidence of postoperative delirium in elderly patients after elective and emergency surgery. Br J Surg 97: 273–280. [DOI] [PubMed] [Google Scholar]
- Barrett J, Jenkins V, Farewell V, Menon U, Jacobs I, Kilkerr J, Ryan A, Langridge C Fallowfield LUKCTOCS trialists (2014) Psychological morbidity associated with ovarian cancer screening: results from more than 23000 women in the randomised trial of ovarian cancer screening (UKCTOCS). BJOG 121(9): 1071–1079. [DOI] [PubMed] [Google Scholar]
- Ben-Ami I, Vaknin Z, Schneider D, Halperin R (2006) Perioperative morbidity and mortality of gynecological oncologic surgery in elderly women. Int J Gynecol Cancer 16(1): 452–457. [DOI] [PubMed] [Google Scholar]
- Conway C, Zalud I, Dilena M, Maulik D, Schulman H, Haley J, Simonelli K (1998) Simple cyst in the postmenopausal patient: detection and management. J Ultrasound Med 17(6): 369–372. [DOI] [PubMed] [Google Scholar]
- Geomini P, Kruitwagen R, Bremer GL, Cnossen J, Mol BW (2009) The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol 113(2 Pt 1): 384–394. [DOI] [PubMed] [Google Scholar]
- Horiuchi A, Itoh K, Shimizu M, Nakai I, Yamazaki T, Kimura K, Suzuki A, Shiozawa I, Ueda N, Konishi I (2003) Toward understanding the natural history of ovarian carcinoma development: a clinicopathological approach. Gynecol Oncol 88: 309–317. [DOI] [PubMed] [Google Scholar]
- Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG (1990) A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynecol 97(10): 922–929. [DOI] [PubMed] [Google Scholar]
- Kaijser J, Sayasneh A, Van Hoorde K, Ghaem-Maghami S, Bourne T, Timmerman D, Van Calster B (2014) Presurgical diagnosis of adnexal tumours using mathematical models and scoring systems: a systematic review and meta-analysis. Hum Reprod Update 20(3): 449–462. [DOI] [PubMed] [Google Scholar]
- Krause AK, Muntz HG, McGonigle KF (2016) Robotic-assisted gynecologic surgery and perioperative morbidity in elderly women. J Minim Invasive Gynecol 23(6): 949–953. [DOI] [PubMed] [Google Scholar]
- Neufeld KJ, Leoutsakos JM, Sieber FE, Wanamaker BL, Gibson Chambers JJ, Rao V, Schretlen DJ, Needham DM (2013) Outcomes of early delirium diagnosis after general anesthesia in the elderly. Anesth Analg 117: 471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes N, Foo X, Widschwendter M, Jurkovic D (2012) A randomised controlled trial comparing surgical intervention rates between two protocols for the management of asymptomatic adnexal tumours in postmenopausal women. BMJ Open 2(6): e002248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes N, Ambler G, Foo X, Naftalin J, Widschwendter M, Jurkovic D (2014) Use of the IOTA simple rules for the diagnosis of ovarian cancer: a meta-analysis. Ultrasound Obstet Gynecol 44(5): 503–514. [DOI] [PubMed] [Google Scholar]
- RCOG (2003) Ovarian Cysts in Postmenopausal Women (Green-top Guideline 34), London, UK.
- RCOG (2011) Ovarian Masses in Premenopausal Women, Management of Suspected (Green-top Guideline No. 62), London, UK.
- Shih IeM, Kurman RJ (2004) Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol 164: 1511–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh-Burgmann E, Hung YY, Kinney W (2014) Outcomes from ultrasound follow-up of small complex adnexal masses in women over 50. Am J Obstet Gynecol 211: 623. [DOI] [PubMed] [Google Scholar]
- Sztark F, Le Goff M, André D, Ritchie K, Dartigues JF, Helmer C (2013) Exposure to general anaesthesia could increase the risk of dementia in elderly: 18AP1-4. Eur J Anaesthesiol 30: 245–245. [Google Scholar]
- Timmerman D, Testa AC, Bourne T, Ameye L, Jurkovic D, Van Holsbeke C, Paladini D, Van Calster B, Vergote I, Van Huffel S, Valentin L (2008) Simple ultrasound-based rules for the diagnosis of ovarian cancer. Ultrasound Obstet Gynecol 31(6): 681–690. [DOI] [PubMed] [Google Scholar]
- Vernooij F, Heintz P, Witteveen E, van der Graaf Y (2007) The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecol Oncol 105(3): 801–812. [DOI] [PubMed] [Google Scholar]