Abstract
Background:
Chemoresistance is a significant clinical problem in pancreatic cancer (PC) and underlying molecular mechanisms still remain to be completely understood. Here we report a novel exosome-mediated mechanism of drug-induced acquired chemoresistance in PC cells.
Methods:
Differential ultracentrifugation was performed to isolate extracellular vesicles (EVs) based on their size from vehicle- or gemcitabine-treated PC cells. Extracellular vesicles size and subtypes were determined by dynamic light scattering and marker profiling, respectively. Gene expression was examined by qRT-PCR and/or immunoblot analyses, and direct targeting of DCK by miR-155 was confirmed by dual-luciferase 3′-UTR reporter assay. Flow cytometry was performed to examine the apoptosis indices and reactive oxygen species (ROS) levels in PC cells using specific dyes. Cell viability was determined using the WST-1 assay.
Results:
Conditioned media (CM) from gemcitabine-treated PC cells (Gem-CM) provided significant chemoprotection to subsequent gemcitabine toxicity and most of the chemoresistance conferred by Gem-CM resulted from its EVs fraction. Sub-fractionation grouped EVs into distinct subtypes based on size distribution and marker profiles, and exosome (Gem-Exo) was the only sub-fraction that imparted chemoresistance. Gene expression analyses demonstrated upregulation of SOD2 and CAT (ROS-detoxifying genes), and downregulation of DCK (gemcitabine-metabolising gene) in Gem-Exo-treated cells. SOD/CAT upregulation resulted, at least in part, from exosome-mediated transfer of their transcripts and they suppressed basal and gemcitabine-induced ROS production, and partly promoted chemoresistance. DCK downregulation occurred through exosome-delivered miR-155 and either the functional suppression of miR-155 or restoration of DCK led to marked abrogation of Gem-Exo-mediated chemoresistance.
Conclusions:
Together, these findings establish a novel role of exosomes in mediating the acquired chemoresistance of PC.
Keywords: chemoresistance, exosomes, pancreatic cancer, ROS, microRNA
Pancreatic cancer (PC) remains one of the deadliest malignancies in the United States. According to recent cancer statistics, it will be overtaking the position of breast cancer as the third leading cause of cancer-related death by the end of this year (Siegel et al, 2016). Nearly 53 070 people are expected to be diagnosed with PC and ∼41 780 will succumb to its severity. The median survival of patients still remains 5–8 months and the 5 year survival rate is 7% (Siegel et al, 2016). This grim scenario largely reflects the inefficacy of current drug regimens against the advanced disease. Therefore, it is highly imperative that we understand causes of therapeutic failure at the molecular level and develop novel, mechanism-based therapies for effective PC treatment.
Gemcitabine (2′, 2′-difluoro-2′-deoxycytidine) remains the drug of choice that is used either alone or in combination with other drugs depending on the health status of PC patients (Von Hoff et al, 2013; Kleger et al, 2014). However, in either case, it has not resulted in marked lift in patient's survival likely due to the presence of innate or acquired chemoresistance mechanisms (Shi et al, 2002; Muerkoster et al, 2006; Hung et al, 2012). To overcome existing limitations in PC treatment, newer mechanism-based approaches have been tested that target intrinsic or acquired survival mechanisms or improve drug accumulation at the tumour site (Kim and Gallick, 2008; Ohhashi et al, 2008; Huanwen et al, 2009; Olive et al, 2009; Saiki et al, 2012). However, some of these approaches have entirely failed (Allison, 2012), whereas others have only resulted in a modest increase in patient's survival (Moore et al, 2007; Von Hoff et al, 2013).
Extracellular vesicles (EVs) shed by tumour cells serve as important mediators of intercellular communication and thus influence the process of carcinogenesis in various ways (EL Andaloussi et al, 2013; Raposo and Stoorvogel, 2013; Hosseini-Beheshti et al, 2016; Qu et al, 2016). Extracellular vesicle are heterogeneous in size, molecular contents as well as their cellular origin (Colombo et al, 2014; Patel et al, 2016). Exosomes are generally the most abundant type of EVs that range in size from 30 to 150 nm (Raposo and Stoorvogel, 2013; Patel et al, 2016). They are of endosomal origin and act as efficient carriers of RNAs (including miRNAs), proteins and other bioactive molecules (EL Andaloussi et al, 2013; Raposo and Stoorvogel, 2013). Recently, pancreatic tumour cells were reported to shed exosomes expressing glypican-1 as a surface marker that were detected in serum samples of PC patients (Melo et al, 2015). In another report, pancreatic tumour-derived exosomes were shown to promote liver metastasis via their induction of pre-metastatic niche formation (Costa-Silva et al, 2015). In a subsequent study, proteomic profiling of pancreatic tumour-derived exosomes revealed the presence of distinct integrin isoforms on the surface of exosomes that were involved in organ-specific homing of metastatic tumour cells (Hoshino et al, 2015).
The present study explored a novel exosome-mediated mechanism for the acquired chemoresistance of PC. We demonstrate that conditioned media (CM) of gemcitabine-treated PC cells (Gem-CM) and specifically its EV fraction (Gem-EV) confer chemoresistance to PC cells. Moreover, we show that exosomes are the major active subtype of Gem-EV that contribute to acquired chemoresistance by increasing the levels of superoxide dismutase 2 (SOD2) and catalase (CAT; ROS-detoxifying enzymes) likely through lateral transfer of their transcripts and through miR-155-mediated downregulation of gemcitabine-metabolising enzyme, deoxycytidine kinase (DCK).
Materials and methods
Reagents, plasmids and antibodies
The following reagents were used in the study: Roswell Park Memorial Institute Medium-1660, Dulbecco's modified Eagle medium, phosphate buffer saline (PBS), penicillin (10 000 U ml−1) streptomycin (10 000 μg ml−1), fetal bovine serum (FBS) and trypsin-EDTA were from Hyclone Laboratory (Logan, UT, USA); exosome-free FBS was from System BioScience (Palo Alto, CA, USA); sodium dodecyl sulphate-polyacrylamyde gel electrophoresis (SDS-PAGE) reagents and protein DC assay kit were purchased from Bio-Rad (Hercules, CA, USA); exosomes-anti-CD63 (10628D), total exosome RNA and protein isolation kit, and cDNA synthesis kit were from Invitrogen (Carlsbad, CA, USA); Taqman advanced miRNA cDNA synthesis kit and SYBR green/rox Q-PCR master mixes from Applied Biosystems (Carlsbad, CA, USA); Quickchange XL site-directed mutagenesis kit (Agilent Technologies, Santa Clara, CA, USA); Dual-Luciferase assay kit from Promega (Madison, WI, USA); and inhibitors for SOD2 (diethyldithiocarbamate, DDC) and CAT (3-amino-1,2,4-triazole, AT) purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibodies targeting CD9 (ab2215), ARF6 (ab77581), thrombospondin (THBS; ab88529), C3b (ab11871) and DCK (ab151966) were procured from Abcam (Cambridge, MA, USA), whereas SOD2 (13194) and CAT (14097) from Cell Signaling Technology (Danvers, MA, USA) and β-actin from Sigma-Aldrich (St Louis, MO, USA); respective anti-mouse or anti-rabbit horseradish peroxidase-conjugated secondary antibodies were procured from Santa Cruz Biotechnology; WST-1 proliferation assay reagent from Roche (Indianapolis, IN, USA). Deoxycytidine kinase-overexpressing plasmid (pDONR223-DCK; plasmid number 23381) from William Hahn and David Root laboratory was procured from Addgene (Cambridge, MA, USA). Deoxycytidine kinase 3′-UTR region (Genecoepia, Rockville, MD, USA); gemcitabine (2′,2′ difluoro 2′-deoxycytidine) and N-acetyl-L-cysteine (NAC) were from Sigma-Aldrich; anti-miR-155 or miRNA inhibitor negative controls and 2′,7′-dichloro-fluorescin diacetate (DCFDA) were purchased from Sigma-Aldrich. ON-TARGETplus Human DCK siRNAs, Non-targeting Control siRNAs Pool and DharmaFECT transfection reagent were from Dharmacon (Lafayette, CO, USA).
Cell culture, treatment and transfection
MiaPaCa and Colo-357 cells were procured and maintained as described earlier (Khan et al, 2015). Cell lines used in this study were authenticated by either in-house or commercial (Genetica DNA Laboratories, Burlington, NC, USA) short-tandem repeats genotyping. Cells were seeded in 96- or 6-well plates and treated with CM or soluble fraction (SF) or EVs fraction or subfraction of EVs (5 μg ml−1) collected from vehicle or gemcitabine-treated cells for 12 h or additional 24–72 h and used for further functional assays and/or mechanistic assays as described in pertinent figure legends. To dissect the role of SOD2 and CAT, PC cells were pretreated with DDC (1.0 μM) and AT (10 μM) for 1 h and further treated with Veh-Exo or Gem-Exo alone or in combination. Pancreatic cancer cells were transiently transfected with anti-miR-155 or miRNA inhibitor negative controls (50 nM) using X-tremeGENE HP DNA transfection reagent for 24 h. For DCK overexpression, cells were transiently transfected with pDONR223-DCK construct (lacking 3′-UTR region) or control plasmid using X-tremeGENE HP DNA transfection reagent.
Collection and fractionation of condition media
Cells were treated with vehicle (PBS) or gemcitabine (10 μM) for 8 h in regular media. Post treatment, cells were washed and cultured in exosome-free FBS-supplemented media for 48 h. Thereafter, CM was collected, centrifuged at 300 × g for 10 min to remove cell debris and designated as Veh-CM (from vehicle-treated cells) and Gem-CM (from gemcitabine-treated cells). Subsequently, Veh-CM and Gem-CM were subjected to ultracentrifugation (120 000 × g at 4 °C for 2 h) to collect respective SFs (Veh-SF and Gem-SF) and total EVs (Veh-EVs and Gem-EVs). Based on their size, EVs were further sub-fractioned by differential centrifugation into large (at 2000 × g for 30 min), medium (at 16 500 × g for 30 min) and small (at 120 000 × g for 2 h) EVs. Extracellular vesicles were washed and quantified using DC protein assay kit and used for subsequent analysis and PC cells treatment.
Size determination of EVs using dynamic light scattering
To determine the size, freshly sub-fractionated EVs (0.5 μg μl−1) were diluted (1 : 1000) in deionised water and 10 spectra were recorded for each fraction from three biological replicates at 25 °C using DelsaMax Pro light scattering analyser (Backman Coulter Inc., Atlanta, GA, USA).
Cell viability assay
Cells were seeded in 96-well plates (5 × 103 cells per well), grown for 24 h and treated with CM or SF or different EVs in exosome-depleted media. After 12 h of pretreatment, cells were further treated with gemcitabine (0–80 μM) for 72 h. In other experiments, PC cells were treated with SOD2/CAT inhibitors, NAC, DCK overexpression/control plasmid or anti-miR-155 prior to Veh-Exo/Gem-Exo and subsequent gemcitabine treatment, and cell viability was determined by WST-1 assay as described earlier (Bhardwaj et al, 2014).
Apoptosis assay
Cells (1 × 106 per well) were grown in six-well plates overnight under regular culture conditions, treated with CM or EVs or exosomes (12 h) prior to gemcitabine (10 μM) treatment for 72 h and extent of apoptosis was measured as previously described (Khan et al, 2015).
Measurement of reactive oxygen species
In vitro reactive oxygen species (ROS) level was measured by using DCFDA by earlier described method (Arora et al, 2013). Briefly, PC cells were incubated with DCFDA in regular growth medium for 30 min at 37 °C, subsequently cells were washed thrice with 1 × PBS and resuspended in 1 × PBS. Fluorescence intensity in cells was determined by fluorescence microscope (Nikon Eclipse TE2000-U, Melville, NY, USA) as well as with flow cytometry on a FACSCanto IIi (BD Biosciences, San Jose, CA, USA).
RNA isolation and quantitative real-time PCR
Total RNA from PC cells (by TRIzol method) and exosomes (using total exosome RNA isolation kit) was isolated and mRNA/miRNA expression analysis was performed using standard quantitative real-time PCR (qRT-PCR) procedures as described earlier (Srivastava et al, 2015), using specific primer sets (Supplementary Table 1). GAPDH and U6 served as housekeeping genes for mRNA and miRNA, respectively. To examine the level of mRNA in exosomes, seminested PCR was performed using gene-specific primers (Supplementary Table 1). Thermal cycle conditions used were 94 °C for 5 min followed by 40 cycles at 94 °C for 30 s, 60 °C for 30 s, 72 °C for 30 s and final extension at 72 °C for 7 min. Subsequently, the second round of PCR was performed using the product of first PCR as a template with same PCR parameters with different reverse primers.
SDS-PAGE and immunoblotting
Total protein from PC cells was isolated in NP40 buffer supplemented with protease phosphatase inhibitor cocktail. An additional 2.0% SDS was added to NP40 buffer for protein isolation from EVs. SDS-PAGE, immunoblotting performed and bands visualised as described earlier (Srivastava et al, 2015). Briefly, membrane immunoblotted with specific antibodies (1 : 1000) against C3b, THBS, ARF6, CD9, CD63, SOD2, CAT and DCK and β-actin served as loading control. Horseradish peroxidase-coupled secondary antibodies were used at 1 : 2500 dilutions. Proteins were visualised with the SuperSignal west femto maximum sensitivity substrate kit (Thermo Scientific, Logan, UT, USA) using ChemiDoc Imaging Systems (Bio-Rad).
Dual-luciferase 3′-UTR reporter assay
Dual-luciferase 3′-UTR reporter assay was performed to validate whether DCK is a direct target of miR-155 using a target reporter plasmids containing DCK 3′-UTR region as described previously (Srivastava et al, 2015). As a control, a mutant plasmid (MUT-DCK 3′-UTR) containing mutated miR-155-binding sites in DCK 3′-UTR was generated using Quickchange XL site-directed mutagenesis kit and also used in reported assay.
Statistical analysis
All experiments were performed at least three times and data expressed as mean±s.d. Wherever appropriate, the data were subjected to unpaired two-tailed Student's t-test and P<0.05 was considered statistically significant.
Results
Extracellular vesicles release from gemcitabine-treated PC cells promotes chemoresistance
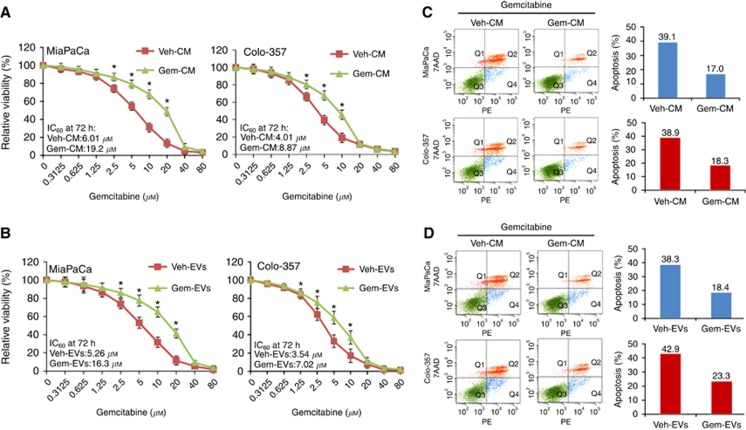
We hypothesised that PC cells, upon treatment with chemotherapy, release some factors in a counter-defence mechanism leading to their acquired chemoresistance. To test this possibility, we treated PC cell lines (MiaPaCa and Colo-357) with vehicle or gemcitabine for 8 h and then cultured them in fresh media for next 48 h. Conditioned media collected from vehicle- (Veh-CM) and gemcitabine-treated (Gem-CM) PC cells were used to pretreat naive culture of PC cells for 12 h, followed by gemcitabine treatment (0–80 μM) for next 72 h. Subsequent cell viability measurements demonstrated significantly reduced (P<0.01) gemcitabine toxicity in PC cells that had been pretreated with Gem-CM as compared to those pretreated with Veh-CM. Overall increase in IC50 values for Gem-CM pretreated MiaPaCa and Colo-357 cells was ∼3.2- and 2.2-fold, respectively, relative to the cells that received Veh-CM pretreatment (Figure 1A).
Figure 1.
Conditioned media and its vesicular fraction from gemcitabine-treated pancreatic cancer cells provide chemoresistance.PC cells were pretreated with (A) conditioned media from vehicle-(Veh-CM) or gemcitabine-treated (Gem-CM) PC cells, or (B) their extracellular vesicular fractions (Veh-EVs and Gem-EVs) for 12 h. Subsequently, cells were exposed with gemcitabine (0–80 μM) and viability measured by WST-1 assay after 72 h. Data shown as mean±s.d.; (n=3) *P<0.05. (C, D) Cells were treated with (C) Veh-CM or Gem-CM, and (D) Veh-EVs or Gem-EVs for 12 h prior to gemcitabine (10 μM) treatment for 72 h and number of apoptotic cells were determined.
We next investigated whether the acquired chemoresistance involved SF or EV fraction of CM. For this, CM was fractionated into SF (Veh-SF/Gem-SF) and EVs (Veh-EVs/Gem-EVs) through ultracentrifugation and these sub-fractions were used to treat PC cells prior to gemcitabine exposure. Data revealed that Gem-SF pretreatment had only minimal (∼1.2-fold) chemoprotective effect in both the PC cell lines against gemcitabine (Supplementary Figure 1), whereas significantly greater (P<0.01) chemoprotection was provided by Gem-EVs. IC50 values for Gem-EVs-treated PC cells were increased ∼3.09-fold (in MiaPaCa) and ∼2.0-fold (in Colo-357) with respect to those pretreated with Veh-EVs (Figure 1B). This chemoprotection was further confirmed through flow-cytometry-based apoptosis assay. Pancreatic cancer cells treated with Gem-CM prior to gemcitabine (10 μM) treatment had lower apoptotic indices (17.0% and ∼18.3%) compared to Veh-CM pretreated (39.1% and 38.9%) MiaPaCa and Colo-357 cells, respectively, (Figure 1C). Similarly, percentage of apoptotic MiaPaCa and Colo-357 cells was decreased (18.4% and 23.3%, respectively) upon pretreatment with Gem-EVs in comparison to those pretreated with Veh-EVs (38.3% and 42.9%, respectively; Figure 1D). Together, these findings establish a clear role of EVs in acquired chemoresistance of PC.
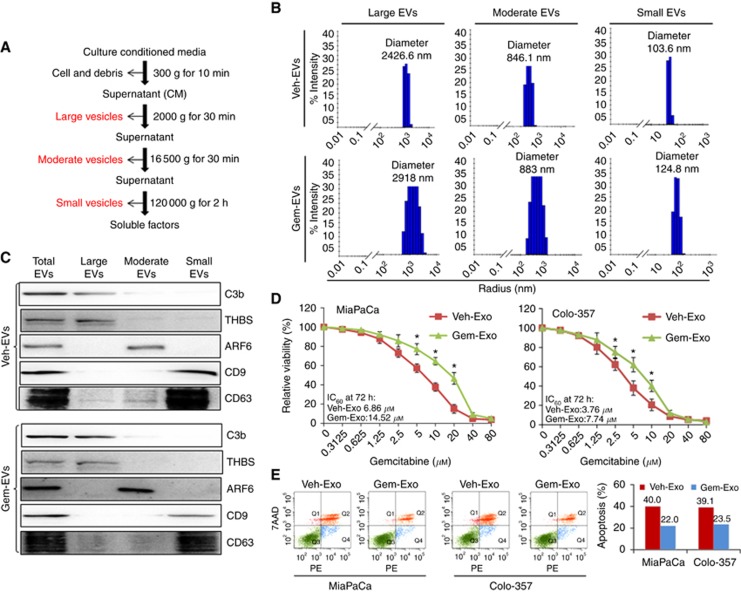
Exosomes are the main EVs imparting acquired chemoresistance
As EVs may represent heterogeneous population of different size and origin (Colombo et al, 2014; Patel et al, 2016), we sub-fractionated them into large-, moderate- and small-sized EVs by differential centrifugation as depicted in Figure 2A. Size distribution of these sub-fractions was measured by dynamic light scattering analysis. Average size of the large, moderate and small EVs was recorded to be >2000, ∼800 and <150 nm, respectively (Figure 2B). Interestingly, the sizes of different EVs sub-fractions from gemcitabine-treated PC cells tended to be towards somewhat higher side as compared to those treated with vehicle only (2918 vs 2426.6 nm (large) 883 vs 846.1 nm (moderate), and 124.8 vs 103.6 nm (small); Figure 2B). Moreover, protein amount of secreted exosomes from gemcitabine-treated MiaPaCa and Colo-357 cells is also significantly higher ∼1.75- and 1.52-fold, respectively, as compared to vehicle-treated PC cells (Supplementary Figure 2). We next performed immunoblot analysis to investigate the nature of different EV sub-fractions using antibodies against membrane-specific biomarkers. Data revealed that large-, moderate- and small-sized sub-fractions from both Veh- or Gem-EVs were positive for C3b and thrombospondin (apoptotic bodies, ABs), ARF6 (microvesicles, MVs) and CD63 and CD9 (exosomes, Exo) markers, respectively (Figure 2C).
Figure 2.
Exosomal fraction is mainly responsible for acquired chemoresistance conferred by extracellular vesicles.(A) EVs were sub-fractionated by differential centrifugation. (B) Sizes of the different EVs were determined by dynamic light scattering. (C) Expression of specific markers for apoptotic bodies (C3b and THBS), microvesicles (ARF6) and exosomes (CD63 and CD9) by immunoblotting. (D) Cells were treated for 12 h with Veh-Exo or Gem-Exo prior to the gemcitabine (0–80 μM) treatment and viability was determined by WST-1 assay after 72 h. Data expressed as mean±s.d.; (n=3) *P<0.05. (E) Cells were pretreated with Veh-Exo or Gem-Exo for 12 h followed by gemcitabine (10 μM) treatment for 72 h. Thereafter, apoptotic indices were measured by flow cytometry.
To examine the specific sub-fraction(s) of EVs mediating acquired chemoresistance, PC cells were pretreated with ABs, MVs and Exo separately, and their effect on gemcitabine cytotoxicity was examined. We observed that Gem-Exo provided significant chemoprotection to PC cells by decreasing gemcitabine sensitivity (Figure 2D), whereas both Gem-ABs and Gem-MVs failed to provide any protection (Supplementary Figure 3). IC50 values of gemcitabine in Gem-Exo-pretreated MiaPaCa and Colo-357 were recorded to be ∼14.5 and 7.7 μM, respectively, as compared to that from Veh-Exo pretreated cells (∼6.8 and 3.7 μM, respectively), indicating more than two fold change. We further confirmed these findings by performing apoptosis analysis on Gem-Exo and Veh-Exo pretreated PC cells (Figure 2E). Together, these data establish exosomes to be major mediators in gemcitabine-induced acquired chemoresistance in PC cells.
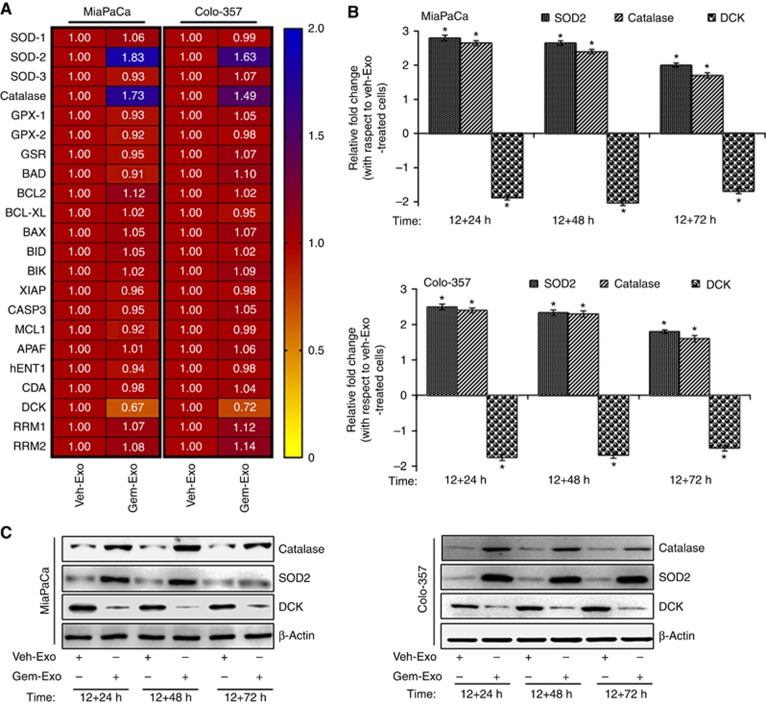
Expression of CAT and SOD2 is increased, whereas DCK is downregulated in PC cells exhibiting acquired chemoresistance
Several studies have suggested that genes involved in survival pathways may confer cancer chemoresistance (Wang et al, 1999, 2014; Kim and Gallick, 2008). In other reports, a role of enzymes involved in ROS detoxification and drug metabolism has been suggested in cancer chemoresistance (Duxbury et al, 2004; Ohhashi et al, 2008; Yeung et al, 2008; Liou and Storz, 2010). Therefore, we used a qPCR-based custom array to identify differentially expressed genes in Veh-Exo- and Gem-Exo-pretreated PC cells. We observed that out of several genes tested in our analysis, expression of CAT and SOD2 (both encoding ROS-detoxifying enzymes, CAT and SOD2, respectively) was upregulated in Gem-Exo-pretreated MiaPaCa (1.73- and 1.83-fold, respectively) and Colo-357 (1.49- and 1.63-fold, respectively) cells as compared to that of Veh-Exo-treated cells. However, we recorded a decrease in the expression of DCK (encoding DCK, a gemcitabine-metabolising enzyme) by 1.47- and 1.38-fold in Gem-Exo-pretreated MiaPaCa and Colo-357 cells, respectively (Figure 3A). Differential expression of these genes were further confirmed at protein level by immunoblot assay. Interestingly, we observed a greater fold change for DCK (3.1-fold, MiaPaCa and 2.6-fold, Colo-357) at protein level (Supplementary Figure 4) relative to that at the transcript level (Figure 3A). We next examined whether the differential expression of CAT, SOD2 and DCK was sustained for the duration of subsequent gemcitabine treatment. Therefore, PC cells were treated with Veh-Exo or Gem-Exo for additional 24, 48 and 72 h followed by gene expression analyses at mRNA (Figure 3B) and protein (Figure 3C) levels. Considering primary changes at the transcript levels and established role of exosomes as carriers of RNAs (Azmi et al, 2013; Patel et al, 2016), we examined relative levels of CAT, SOD2 and DCK in Gem-Exo and Veh-Exo by seminested PCR. As expected, we observed increased levels of CAT and SOD2 transcripts in Gem-Exo as compared to that in Veh-Exo; however, no DCK transcript was detected in any of the exosomal fractions (Supplementary Figure 5), suggesting an alternative mechanism for its regulation. To further support our findings on possible exosome-mediated lateral transfer of CAT and SOD2 transcripts, we analysed their expression in Gem-treated PC cells at 8, 8+24 and 8+48 h. The data show that expression of SOD2 and CAT in PC cells is increased within 8 h of gemcitabine treatment and continues to increase with time (Supplementary Figure 6). It is; however, likely that SOD2 and CAT upregulation in Gem-Exo-treated PC cells may occur through other, not yet identified, mechanisms as well.
Figure 3.
Gem-Exo modulates the expression of catalase (CAT), superoxide dismutase 2 (SOD2) and deoxycytidine kinase (DCK) in PC cells.(A) PC cells were treated with Veh-Exo or Gem-Exo for 12 h and expression of genes involved in cell survival, ROS detoxification and gemcitabine metabolism was analysed. Three genes (SOD2, CAT and DCK) exhibited differential expression in both cell lines, which were confirmed at both mRNA and protein levels (Supplementary Figure 4). (B, C) To examine whether the changes in gene expression sustained for the duration of subsequent gemcitabine treatment, Veh-Exo- or Gem-Exo-pretreated cells were grown for additional 24, 48 or 72 h and expression of CAT, SOD2 and DCK was examined at (B) mRNA and (C) protein levels. GAPDH (for mRNA) and β-actin (for protein) served as internal controls. Bars represent mean±s.d.; n=3. *P<0.05.
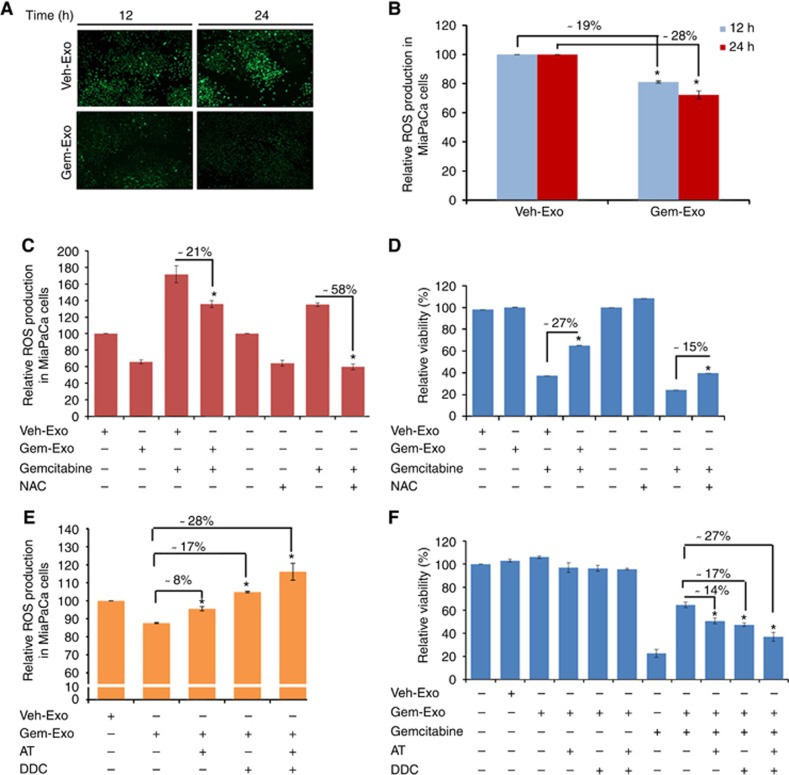
Reduction in ROS levels by CAT and SOD2 is partly responsible for acquired chemoresistance of PC cells
As CAT and SOD2 are ROS-detoxifying enzymes, we examined the levels of ROS in Veh-Exo- and Gem-Exo-treated PC cells. A significant decrease (P<0.01) in ROS levels was observed in Gem-Exo-treated PC cells as compared to that in Veh-Exo-treated cells (Figure 4A and B). More importantly, Gem-Exo was also effective in reducing gemcitabine-induced increase in ROS levels in PC cells, although relatively less effective in comparison with NAC (Figure 4C). In contrast, Gem-Exo provided greater chemoprotection as compared to NAC pretreatment (Figure 4D), suggesting only a partial role of ROS detoxification in Gem-Exo-induced acquired chemoresistance. To directly establish the participation of CAT and SOD2 in Gem-Exo-mediated ROS reduction and consequent chemoprotection, we pretreated MiaPaCa cells with specific inhibitors of CAT (AT) and SOD2 (DDC) prior to Gem-Exo treatment either alone or in combination, and their effect on ROS levels and cell viability was examined. As expected, pretreatment of PC cells with AT and DDC abrogated Gem-Exo-mediated decrease in ROS levels with their combination being more effective (Figure 4E). However, subsequent cell viability analyses of treated PC cells demonstrated that Gem-Exo-induced acquired chemoresistance was partly abrogated upon pretreatment with CAT and SOD2 inhibitors (Figure 4F). Together, these data suggest a partial role of CAT and SOD2 in Gem-Exo-induced chemoresistance of PC cells via causing a decrease in total cellular ROS levels.
Figure 4.
Decrease in basal and gemcitabine-induced reactive oxygen species levels by increased activity of catalase and superoxide dismutase 2 (SOD2) is partly responsible for acquired chemoresistance of pancreatic cancer cells.To examine whether enhanced expression of CAT and SOD2 resulted in decreased ROS levels, we treated MiaPaCa cells, with Veh-Exo or Gem-Exo for 12 and 24 h. Cells were then incubated with DCFDA (20 μM) for 30 min, washed and analysed for ROS level by (A) fluorescence microscope and (B) flow cytometry. Representative images are shown from three independent experiments. (C, D) PC cells were pretreated with Veh-Exo or Gem-Exo (for 12 h) or with an effective ROS scavenger, NAC (10 mM; for 1 h) followed by gemcitabine treatment (10 μM) alone or in combinations. Effect on (C) ROS level (after 24 h) and (D) cell viability (after 72 h) were determined through flow cytometry and WST-1 assays, respectively. (E) In additional experiments, cells were treated with inhibitors of catalase (AT; 10 μM) or SOD2 (DDC; 1.0 μM) alone or in combinations 1 h prior to Veh-Exo or Gem-Exo treatment, and intracellular ROS level measured. (F) Cells pretreated with CAT and SOD2 inhibitors were examined for their role in abrogating exosome-induced gemcitabine resistance by WST-1 assay. Data are presented as mean±s.d.; n=3. *P<0.05.
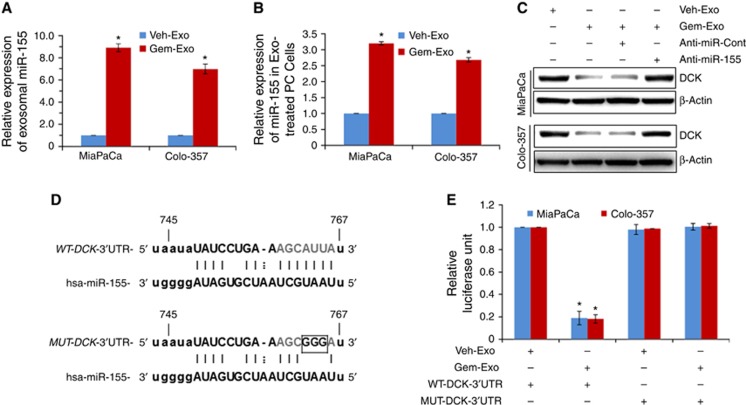
miR-155 inhibits DCK expression in Gem-Exo-treated PC cells
Having observed only partial role of CAT and SOD2 in exosome-mediated chemoresistance, we focused our attention on DCK, whose expression was decreased in Gem-Exo-treated PC cells. We first investigated the mechanism that caused DCK downregulation in Gem-Exo-treated PC cells as no DCK transcript was detected in exosomes from either vehicle or gemcitabine-treated PC cells (Supplementary Figure 5). Hence, we performed in silico analysis using the algorithms TargetScan (http://www.targetscan.org) and miRanda (http://www.microrna.org) to shortlist DCK-targeting miRNAs. Our analysis identified eight putative DCK-targeting miRNAs (data not shown), whose presence was examined in Veh-Exo and Gem-Exo- by qRT-PCR. miR-155 was found to be the most differentially expressed miRNA in Gem-Exo vs Veh-Exo exhibiting ∼9.0- and 6.5-fold higher levels in the former derived from MiaPaCa and Colo-357 cells, respectively (Figure 5A). Accordingly, we also observed enhanced levels of miR-155 (∼3.2- and 2.7-fold) in Gem-Exo-treated cells as compared to Veh-Exo-treated MiaPaCa and Colo-357 cells, respectively (Figure 5B). We next validated whether functional suppression of miR-155 by specific anti-miRs in Gem-Exo-treated cells would alter DCK expression. The data revealed that DCK expression was restored by anti-miR-155 treatment in Gem-Exo-treated PC cells (Figure 5C). To confirm direct targeting of DCK 3′-UTR by miR-155, we next performed luciferase-based 3′-UTR reporter assay using plasmids containing wild-type (WT) or mutated (MUT) 3′-UTR regions of DKC (Figure 5D). We observed >75% decrease in luciferase activity in Gem-Exo-treated PC cells that were transfected with WT-3′-UTR of DCK containing reporter plasmid, whereas those transfected with MUT-3′-UTR of DCK did not show any response to the suppressor activity of Gem-Exo (Figure 5E). These data provide strong evidence that Gem-Exo-mediated delivery of miR-155 causes DCK downregulation in PC cells by directly targeting its 3′-UTR.
Figure 5.
Downregulation of DCK expression in pancreatic cancer cells occurs through exosome-mediated delivery of miR-155.(A) Exosomes (Veh-Exo/Gem-Exo) were isolated, and expression of miR-155 examined through qRT-PCR. U6 was used as internal control. (B) Expression of miR-155 was also examined in Veh-Exo or Gem-Exo-treated PC cells through qRT-PCR. (C) PC cells were pretreated with control or miR-155-targeting miRs for 12 h followed by Veh-Exo/Gem-Exo treatment for 12 h. Thereafter, total protein was isolated and expression of DCK was measured by immunoblotting. (D) Schematic representation of firefly luciferase reporter construct containing DCK 3′-UTR with either wild-type (WT) or mutant (MUT) miR-155 target site. (E) PC cells were transiently co-transfected with reporter plasmids (200 ng) 24 h prior to Veh-Exo or Gem-Exo treatment for additional 24 h. Subsequently, protein lysates were made and luciferase (Firefly; test and Renilla, transfection efficiency control) activity assessed using dual-luciferase assay system. Data presented as normalised fold change in luciferase activity (mean±s.d.; n=3, *P⩽0.05).
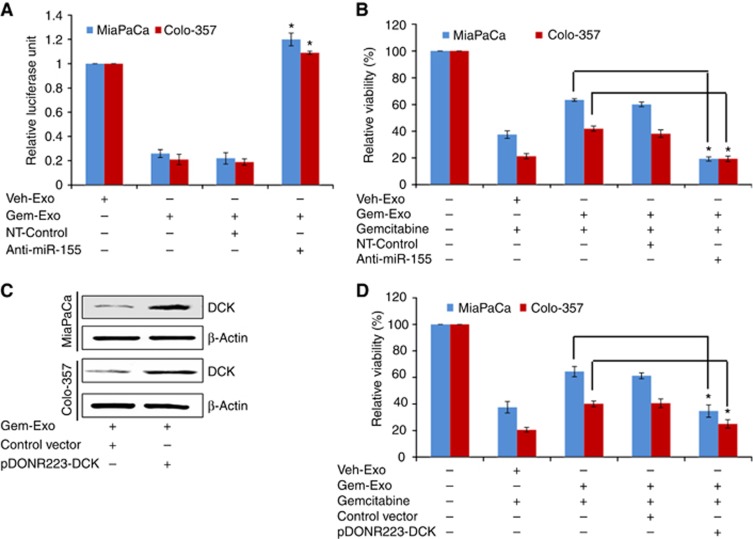
Functional suppression of miR-155 or restoration of DCK expression abrogates exosome-mediated acquired chemoresistance in PC cells
To confirm the involvement of miR-155 in Gem-Exo-mediated chemoresistance, we transfected PC cells with control anti-miR or anti-miR-155 for 12 h followed by 12 h treatment with Veh-Exo or Gem-Exo. Thereafter, its effects on suppression of miR-155 activity and cell viability in presence of gemcitabine were examined by luciferase-based 3′-UTR reporter and WST-1 assays, respectively. Decreased luciferase activity in Gem-Exo-treated PC cells upon transfection of anti-miR-155 was observed as compared to that in cells transfected with control anti-miR, suggesting the functional inhibition of miR-155 through anti-miR-155 (Figure 6A). Moreover, we observed that anti-miR-155-treated PC cells became more sensitive to gemcitabine as compared to those treated with non-target (NT) sequence control (Figure 6B). Further, we tested the effect of direct restoration of DCK in Gem-Exo-induced acquired chemoresistance. For this, we transfected PC cells with DCK overexpression plasmid, which contains the entire coding sequence of DCK, but lacks the 3′-UTR, prior to Gem-Exo treatment. Expression of DCK was examined by immunoblot analysis. We observed that DCK overexpression plasmid was able to restore DCK expression in Gem-Exo-treated PC cells (Figure 6C). Next, the effect of DCK restoration on the viability of Gem-Exo-treated PC cells in the presence or absence of gemcitabine was determined. A significant abrogation of Gem-Exo-induced chemoprotection in MiaPaCa and Colo-357 cells was reported upon forced DCK overexpression as compared to cells transfected with control plasmid (Figure 6D). In a converse approach, expression of DCK was silenced in PC cells treated with Veh-Exo through transient transfection of DCK-targeting specific siRNAs pool and effect on gemcitabine-induced cytotoxicity was measured by WST-1 assay. DCK siRNAs efficiently silenced DCK expression by 24 h, an effect that sustained at least up to 72 h post transfection (Supplementary Figure 7A). As expected, silencing of DCK enhanced the resistance to gemcitabine toxicity in Veh-Exo-treated PC cells (Supplementary Figure 7B). Collectively, our findings suggest that Gem-Exo-mediated downregulation of gemcitabine metabolism enzyme, DCK, provides survival advantage to the gemcitabine-treated PC cells.
Figure 6.
Restoration of DCK expression abrogates Gem-Exo-induced acquired chemoresistance in PC cells.(A) PC cells were transiently transfected with wild-type reporter plasmids 24 h prior to control or anti-miR-155 transfection. After 12 h, cells were treated with Veh-Exo or Gem-Exo for additional 24 h and luciferase activity assessed. Data presented as mean±s.d.; n=3. (B) PC cells were pretreated with control anti-miR or anti-miR-155 for 12 h followed by 12 h treatment with Veh-Exo or Gem-Exo. Thereafter, cells were exposed to gemcitabine (10 μM) for additional 72 h, and viability was measured through WST-1 assay. Data represent as mean±s.d.; n=3. *P<0.05. (C, D) PC cells were transiently transfected with control or DCK overexpression plasmid and treated with Gem-Exo for 12 h. Post treatment, (C) protein was collected and DCK expression was determined through immunoblotting. β-Actin served as loading control. (D) Cells were further treated with gemcitabine (10 μM) and viability measured by WST-1 after 72 h.
Discussion
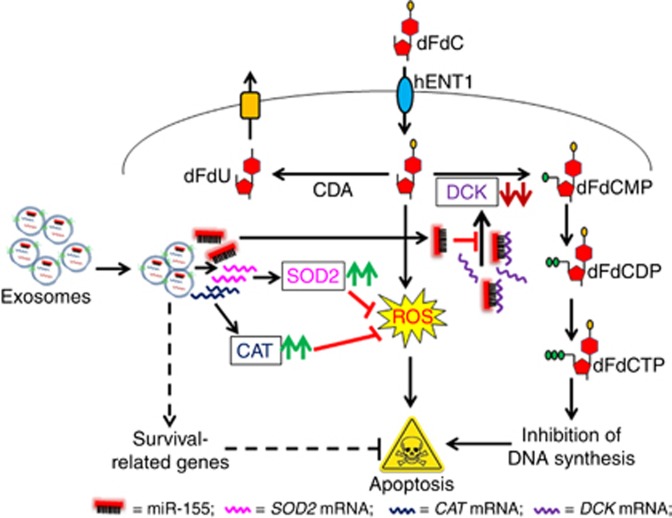
Pancreatic cancer is largely an untreatable disease due to the presence of several intrinsic or acquired chemoresistance mechanisms (Muerkoster et al, 2006; Hung et al, 2012) that still remain to be properly understood. This study made an effort to characterise one such acquired chemoresistance mechanism that could underlie, in part, for the poor therapeutic efficacy of gemcitabine as a single agent or in combination. We hypothesised that upon encountering chemotherapeutic insult, pancreatic tumour cells may release factors that would enable them to fight it or any subsequent insults more effectively. Our findings from this study provide us strong support for this hypothesis and establish exosomes to be important and novel mediators in the process of acquired chemoresistance (Figure 7).
Figure 7.
Mechanistic representation of exosomes-mediated acquired chemoresistance in PC.Exosomes from gemcitabine-treated PC cells deliver CAT and SOD2 transcripts leading to enhanced expression of reactive oxygen species (ROS)-detoxifying enzymes, catalase (CAT) and superoxide dismutase 2 (SOD2), respectively. Reduction in basal as well as gemcitabine-induced ROS levels by CAT and SOD2 protects PC cells from ROS-induced cell death. On the other hand, miR-155 delivered via exosomes downregulates the expression of DCK, which encodes for gemcitabine-metabolising enzyme, deoxycytidine kinase (DCK). Deoxycytidine kinase is required for phosphorylation of gemcitabine (2′, 2′-difluoro-2′-deoxycytidine, dFdC) into gemcitabine-monophosphate (dFdCMP), which is then converted to active metabolite form of gemcitabine (gemcitabine-triphosphate (dFdCTP)). dFdCTP incorporates into DNA, halts the replication process, and ultimately results in apoptotic cell death.
Several mechanisms have been proposed and/or experimentally validated to be operational in pancreatic tumour as well as its host to cause its unusual chemoresistance. One mechanism that gained extensive attention lately is the unique histoarchitecture of pancreatic tumours that provides indirect chemoprotection (Olive et al, 2009). It was shown that excessive fibrosis in the surrounding of tumour cells, referred to as desmoplasia, acted as a physical barrier for drug delivery and its targeting significantly improved therapeutic outcome in a preclinical model (Olive et al, 2009). However, this approach failed in clinical trial further underscoring the complexity of underlying molecular mechanisms of PC chemoresistance (Allison, 2012). Recently, we and others have focused on additional mechanisms that involve cell-to-cell and/or cell-to-matrix interactions through release of soluble growth factors, direct intercellular interactions and generation of growth favourable niches within tumour microenvironment (Singh et al, 2010, 2012; Castells et al, 2012; Binenbaum et al, 2015). We demonstrated that stromal-derived chemokine, CXCL12, conferred gemcitabine resistance in PC cells (Singh et al, 2010). Moreover, we suggested that the activation of this signalling pathway could also promote desmoplasia through bi-directional tumour–stromal interactions (Singh et al, 2012). Our other findings not only supported the importance of this chemokine pathway, but also indicated its role in promotion of tumour spread as an unintended effect of chemotherapy (Arora et al, 2013). This notion was further supported by our observation of chemotherapy-induced pro-angiogenic signalling that could potentially facilitate cancer cell's escape to new chemoprotective and growth-permissive niches (Khan et al, 2015). In the same line, our present findings add another novel mode for acquired chemoresistance in PC that could be of significance for many other cancer types as well.
Exosomes are a novel class of cellular entity that has gained enormous momentum lately as facilitators of tumour growth and metastasis (Azmi et al, 2013; Costa-Silva et al, 2015; Rodriguez et al, 2015; Song et al, 2016). It was recently reported that exosomes assist in the process of pre-metastatic niche formation for evolving pancreatic tumours by travelling to distant locations (Costa-Silva et al, 2015). Another study from the same group established exosomes as important mediators in organ-specific homing of tumour cells (Hoshino et al, 2015). The data from current study suggest that exosomes may confer chemoresistance to themselves or neighbouring PC cells via intercellular transfer of involved molecular factors. Specifically, our data suggested that exosomes caused direct transfer of SOD2 and CAT transcripts that encode for ROS-detoxifying enzymes. Moreover, we observed indirect downregulation of gemcitabine-metabolising enzyme, DCK, in pancreatic tumour cells via transfer of its targeting miRNA (miR-155). Exosomal transfer of proteins, RNA, DNA and miRNAs from donor to the recipient cells have been reported in multiple studies and suggested to induce phenotypic and/or genotypic changes in the receiving cells (EL Andaloussi et al, 2013; Chevillet et al, 2014). By this virtue, exosomes may impact several aspects of tumour development and therapy, and may have shorter- as well as longer-term implications, some of which are now starting to be recognised.
Generation of ROS by chemotherapeutic drugs is suggested to be one important mechanism for its cytotoxic efficacy (Trachootham et al, 2009; Donadelli et al, 2011). Tumour cells try to counter-balance this abrupt increase in ROS by altering the expression of ROS-detoxifying enzymes. Both CAT and SOD2, shown to be partly implicated in acquired resistance of PC in our study, have been suggested to promote chemoresistance in cancer (Dalla et al, 2012; Xu et al, 2014). Similarly, in other studies a role of gemcitabine-metabolising enzymes has been reported to underlie chemoresistant nature of PC cells (Duxbury et al, 2004; Amit and Gil, 2013; Binenbaum et al, 2015). Specifically, human equilibrative nucleoside transporter-1 and DCK have been shown to induce gemcitabine resistance in cancer cells by limiting its uptake and conversion to active metabolite form, respectively (Ohhashi et al, 2008; Nordh et al, 2014). In this regard, our finding of exosome-mediated suppression of DCK is of great relevance. More importantly, it also point out towards a novel mechanism of DCK regulation in PC that occurs through exosome-mediated transfer of its targeting miRNA. MiRNAs are small non-coding regulatory RNAs that negatively modulate gene expression via binding to 3′-UTR of their target genes (Bhardwaj et al, 2010, 2013). As miRNA binding to its target 3′-UTR does not have to be perfect, a single miRNA can regulate the expression of multiple genes (Srivastava et al, 2014). Therefore, our observation on exosomal transfer of miR-155 may have additional consequences that yet need to be determined. Recently, miR-155 was shown to be a major factor in PC survival, invasion and migration (Gironella et al, 2007), which further supports our notion of its broader pathological implications.
In summary, we have established a novel mechanism of acquired chemoresistance in PC, which involves exosomes as carriers of mRNAs and miRNA having a role in ROS detoxification and gemcitabine metabolism. Specifically, we have identified CAT, SOD2 and DCK as important genes involved in exosome-mediated PC chemoresistance. Moreover, our findings have revealed miR-155 to be a novel regulator of DCK expression in PC. Together, these findings not only define a novel role of exosomes, but also unravel a novel molecular basis for unusual chemoresistance of PC.
Acknowledgments
This work was supported by funding from NIH/NCI (R01CA175772, and U01CA185490 (to APS)) and USAMCI. We also thank Mr Steven McClellan, for his assistance with flow cytometry.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflict of interest.
Supplementary Material
References
- Allison M (2012) Hedgehog hopes lifted by approval... and stung by failure. Nat Biotechnol 30(3): 203. [DOI] [PubMed] [Google Scholar]
- Amit M, Gil Z (2013) Macrophages increase the resistance of pancreatic adenocarcinoma cells to gemcitabine by upregulating cytidine deaminase. Oncoimmunology 2(12): e27231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora S, Bhardwaj A, Singh S, Srivastava SK, McClellan S, Nirodi CS, Piazza GA, Grizzle WE, Owen LB, Singh AP (2013) An undesired effect of chemotherapy: gemcitabine promotes pancreatic cancer cell invasiveness through reactive oxygen species-dependent, nuclear factor kappaB- and hypoxia-inducible factor 1alpha-mediated up-regulation of CXCR4. J Biol Chem 288(29): 21197–21207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azmi AS, Bao B, Sarkar FH (2013) Exosomes in cancer development, metastasis, and drug resistance: a comprehensive review. Cancer Metastasis Rev 32(3-4): 623–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj A, Arora S, Prajapati VK, Singh S, Singh AP (2013) Cancer ‘stemness'- regulating microRNAs: role, mechanisms and therapeutic potential. Curr Drug Targets 14(10): 1175–1184. [DOI] [PubMed] [Google Scholar]
- Bhardwaj A, Singh S, Singh AP (2010) MicroRNA-based cancer therapeutics: big hope from small RNAs. Mol Cell Pharmacol 2(5): 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj A, Srivastava SK, Singh S, Arora S, Tyagi N, Andrews J, McClellan S, Carter JE, Singh AP (2014) CXCL12/CXCR4 signaling counteracts docetaxel-induced microtubule stabilization via p21-activated kinase 4-dependent activation of LIM domain kinase 1. Oncotarget 5(22): 11490–11500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binenbaum Y, Na'ara S, Gil Z (2015) Gemcitabine resistance in pancreatic ductal adenocarcinoma. Drug Resist Updat 23: 55–68. [DOI] [PubMed] [Google Scholar]
- Castells M, Thibault B, Delord JP, Couderc B (2012) Implication of tumor microenvironment in chemoresistance: tumor-associated stromal cells protect tumor cells from cell death. Int J Mol Sci 13(8): 9545–9571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevillet JR, Kang Q, Ruf IK, Briggs HA, Vojtech LN, Hughes SM, Cheng HH, Arroyo JD, Meredith EK, Gallichotte EN, Pogosova-Agadjanyan EL, Morrissey C, Stirewalt DL, Hladik F, Yu EY, Higano CS, Tewari M (2014) Quantitative and stoichiometric analysis of the microRNA content of exosomes. Proc Natl Acad Sci USA 111(41): 14888–14893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo M, Raposo G, Thery C (2014) Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Dev Biol 30: 255–289. [DOI] [PubMed] [Google Scholar]
- Costa-Silva B, Aiello NM, Ocean AJ, Singh S, Zhang H, Thakur BK, Becker A, Hoshino A, Mark MT, Molina H, Xiang J, Zhang T, Theilen TM, Garcia-Santos G, Williams C, Ararso Y, Huang Y, Rodrigues G, Shen TL, Labori KJ, Lothe IM, Kure EH, Hernandez J, Doussot A, Ebbesen SH, Grandgenett PM, Hollingsworth MA, Jain M, Mallya K, Batra SK, Jarnagin WR, Schwartz RE, Matei I, Peinado H, Stanger BZ, Bromberg J, Lyden D (2015) Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol 17(6): 816–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalla PE, Fiorini C, Dando I, Menegazzi M, Sgarbossa A, Costanzo C, Palmieri M, Donadelli M (2012) Role of mitochondrial uncoupling protein 2 in cancer cell resistance to gemcitabine. Biochim Biophys Acta 1823(10): 1856–1863. [DOI] [PubMed] [Google Scholar]
- Donadelli M, Dando I, Zaniboni T, Costanzo C, Dalla PE, Scupoli MT, Scarpa A, Zappavigna S, Marra M, Abbruzzese A, Bifulco M, Caraglia M, Palmieri M (2011) Gemcitabine/cannabinoid combination triggers autophagy in pancreatic cancer cells through a ROS-mediated mechanism. Cell Death Dis 2: e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duxbury MS, Ito H, Zinner MJ, Ashley SW, Whang EE (2004) RNA interference targeting the M2 subunit of ribonucleotide reductase enhances pancreatic adenocarcinoma chemosensitivity to gemcitabine. Oncogene 23(8): 1539–1548. [DOI] [PubMed] [Google Scholar]
- EL Andaloussi S, Mager I, Breakefield XO, Wood MJ (2013) Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov 12(5): 347–357. [DOI] [PubMed] [Google Scholar]
- Gironella M, Seux M, Xie MJ, Cano C, Tomasini R, Gommeaux J, Garcia S, Nowak J, Yeung ML, Jeang KT, Chaix A, Fazli L, Motoo Y, Wang Q, Rocchi P, Russo A, Gleave M, Dagorn JC, Iovanna JL, Carrier A, Pebusque MJ, Dusetti NJ (2007) Tumour protein 53-induced nuclear protein 1 expression is repressed by miR-155, and its restoration inhibits pancreatic tumour development. Proc Natl Acad Sci USA 104(41): 16170–16175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic MM, Molina H, Kohsaka S, Di GA, Ceder S, Singh S, Williams C, Soplop N, Uryu K, Pharmer L, King T, Bojmar L, Davies AE, Ararso Y, Zhang T, Zhang H, Hernandez J, Weiss JM, Dumont-Cole VD, Kramer K, Wexler LH, Narendran A, Schwartz GK, Healey JH, Sandstrom P, Labori KJ, Kure EH, Grandgenett PM, Hollingsworth MA, de SM, Kaur S, Jain M, Mallya K, Batra SK, Jarnagin WR, Brady MS, Fodstad O, Muller V, Pantel K, Minn AJ, Bissell MJ, Garcia BA, Kang Y, Rajasekhar VK, Ghajar CM, Matei I, Peinado H, Bromberg J, Lyden D (2015) Tumour exosome integrins determine organotropic metastasis. Nature 527(7578): 329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosseini-Beheshti E, Choi W, Weiswald LB, Kharmate G, Ghaffari M, Roshan-Moniri M, Hassona MD, Chan L, Chin MY, Tai IT, Rennie PS, Fazli L, Tomlinson Guns ES (2016) Exosomes confer pro-survival signals to alter the phenotype of prostate cells in their surrounding environment. Oncotarget 7(12): 14639–14658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huanwen W, Zhiyong L, Xiaohua S, Xinyu R, Kai W, Tonghua L (2009) Intrinsic chemoresistance to gemcitabine is associated with constitutive and laminin-induced phosphorylation of FAK in pancreatic cancer cell lines. Mol Cancer 8: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung SW, Mody HR, Govindarajan R (2012) Overcoming nucleoside analog chemoresistance of pancreatic cancer: a therapeutic challenge. Cancer Lett 320(2): 138–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MA, Srivastava SK, Bhardwaj A, Singh S, Arora S, Zubair H, Carter JE, Singh AP (2015) Gemcitabine triggers angiogenesis-promoting molecular signals in pancreatic cancer cells: Therapeutic implications. Oncotarget 6(36): 39140–39150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MP, Gallick GE (2008) Gemcitabine resistance in pancreatic cancer: picking the key players. Clin Cancer Res 14(5): 1284–1285. [DOI] [PubMed] [Google Scholar]
- Kleger A, Perkhofer L, Seufferlein T (2014) Smarter drugs emerging in pancreatic cancer therapy. Ann Oncol 25(7): 1260–1270. [DOI] [PubMed] [Google Scholar]
- Liou GY, Storz P (2010) Reactive oxygen species in cancer. Free Radic Res 44(5): 479–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, LeBleu VS, Mittendorf EA, Weitz J, Rahbari N, Reissfelder C, Pilarsky C, Fraga MF, Piwnica-Worms D, Kalluri R (2015) Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature 523(7559): 177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore MJ, Goldstein D, Hamm J, Figer A, Hecht JR, Gallinger S, Au HJ, Murawa P, Walde D, Wolff RA, Campos D, Lim R, Ding K, Clark G, Voskoglou-Nomikos T, Ptasynski M, Parulekar W (2007) Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 25(15): 1960–1966. [DOI] [PubMed] [Google Scholar]
- Muerkoster SS, Lust J, Arlt A, Hasler R, Witt M, Sebens T, Schreiber S, Folsch UR, Schafer H (2006) Acquired chemoresistance in pancreatic carcinoma cells: induced secretion of IL-1beta and NO lead to inactivation of caspases. Oncogene 25(28): 3973–3981. [DOI] [PubMed] [Google Scholar]
- Nordh S, Ansari D, Andersson R (2014) hENT1 expression is predictive of gemcitabine outcome in pancreatic cancer: a systematic review. World J Gastroenterol 20(26): 8482–8490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohhashi S, Ohuchida K, Mizumoto K, Fujita H, Egami T, Yu J, Toma H, Sadatomi S, Nagai E, Tanaka M (2008) Down-regulation of deoxycytidine kinase enhances acquired resistance to gemcitabine in pancreatic cancer. Anticancer Res 28(4B): 2205–2212. [PubMed] [Google Scholar]
- Olive KP, Jacobetz MA, Davidson CJ, Gopinathan A, McIntyre D, Honess D, Madhu B, Goldgraben MA, Caldwell ME, Allard D, Frese KK, Denicola G, Feig C, Combs C, Winter SP, Ireland-Zecchini H, Reichelt S, Howat WJ, Chang A, Dhara M, Wang L, Ruckert F, Grutzmann R, Pilarsky C, Izeradjene K, Hingorani SR, Huang P, Davies SE, Plunkett W, Egorin M, Hruban RH, Whitebread N, McGovern K, Adams J, Iacobuzio-Donahue C, Griffiths J, Tuveson DA (2009) Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science 324(5933): 1457–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel GK, Patton MC, Singh S, Khushman M, Singh AP (2016) Pancreatic cancer exosomes: shedding off for a meaningful journey. Pancreat Disord Ther 6(2): e148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu L, Ding J, Chen C, Wu ZJ, Liu B, Gao Y, Chen W, Liu F, Sun W, Li XF, Wang X, Wang Y, Xu ZY, Gao L, Yang Q, Xu B, Li YM, Fang ZY, Xu ZP, Bao Y, Wu DS, Miao X, Sun HY, Sun YH, Wang HY, Wang LH (2016) Exosome-transmitted lncARSR promotes sunitinib resistance in renal cancer by acting as a competing endogenous RNA. Cancer Cell 29(5): 653–668. [DOI] [PubMed] [Google Scholar]
- Raposo G, Stoorvogel W (2013) Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol 200(4): 373–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez M, Silva J, Herrera A, Herrera M, Pena C, Martin P, Gil-Calderon B, Larriba MJ, Coronado MJ, Soldevilla B, Turrion VS, Provencio M, Sanchez A, Bonilla F, Garcia-Barberan V (2015) Exosomes enriched in stemness/metastatic-related mRNAS promote oncogenic potential in breast cancer. Oncotarget 6(38): 40575–40587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saiki Y, Yoshino Y, Fujimura H, Manabe T, Kudo Y, Shimada M, Mano N, Nakano T, Lee Y, Shimizu S, Oba S, Fujiwara S, Shimizu H, Chen N, Nezhad ZK, Jin G, Fukushige S, Sunamura M, Ishida M, Motoi F, Egawa S, Unno M, Horii A (2012) DCK is frequently inactivated in acquired gemcitabine-resistant human cancer cells. Biochem Biophys Res Commun 421(1): 98–104. [DOI] [PubMed] [Google Scholar]
- Shi X, Liu S, Kleeff J, Friess H, Buchler MW (2002) Acquired resistance of pancreatic cancer cells towards 5-Fluorouracil and gemcitabine is associated with altered expression of apoptosis-regulating genes. Oncology 62(4): 354–362. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1): 7–30. [DOI] [PubMed] [Google Scholar]
- Singh AP, Arora S, Bhardwaj A, Srivastava SK, Kadakia MP, Wang B, Grizzle WE, Owen LB, Singh S (2012) CXCL12/CXCR4 protein signaling axis induces sonic hedgehog expression in pancreatic cancer cells via extracellular regulated kinase- and Akt kinase-mediated activation of nuclear factor kappaB: implications for bidirectional tumor-stromal interactions. J Biol Chem 287(46): 39115–39124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Srivastava SK, Bhardwaj A, Owen LB, Singh AP (2010) CXCL12-CXCR4 signalling axis confers gemcitabine resistance to pancreatic cancer cells: a novel target for therapy. Br J Cancer 103(11): 1671–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X, Ding Y, Liu G, Yang X, Zhao R, Zhang Y, Zhao X, Anderson GJ, Nie G (2016) Cancer cell-derived exosomes induce mitogen-activated protein kinase-dependent monocyte survival by transport of functional receptor tyrosine kinases. J Biol Chem 291(16): 8453–8464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava SK, Arora S, Singh S, Bhardwaj A, Averett C, Singh AP (2014) MicroRNAs in pancreatic malignancy: progress and promises. Cancer Lett 347(2): 167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava SK, Bhardwaj A, Arora S, Tyagi N, Singh S, Andrews J, McClellan S, Wang B, Singh AP (2015) MicroRNA-345 induces apoptosis in pancreatic cancer cells through potentiation of caspase-dependent and -independent pathways. Br J Cancer 113(4): 660–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trachootham D, Alexandre J, Huang P (2009) Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach? Nat Rev Drug Discov 8(7): 579–591. [DOI] [PubMed] [Google Scholar]
- Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van CE, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369(18): 1691–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CY, Cusack JC Jr, Liu R, Baldwin Jr AS (1999) Control of inducible chemoresistance: enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-kappaB. Nat Med 5(4): 412–417. [DOI] [PubMed] [Google Scholar]
- Wang WB, Yang Y, Zhao YP, Zhang TP, Liao Q, Shu H (2014) Recent studies of 5-fluorouracil resistance in pancreatic cancer. World J Gastroenterol 20(42): 15682–15690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X, Wells A, Padilla MT, Kato K, Kim KC, Lin Y (2014) A signaling pathway consisting of miR-551b, catalase and MUC1 contributes to acquired apoptosis resistance and chemoresistance. Carcinogenesis 35(11): 2457–2466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeung BH, Wong KY, Lin MC, Wong CK, Mashima T, Tsuruo T, Wong AS (2008) Chemosensitisation by manganese superoxide dismutase inhibition is caspase-9 dependent and involves extracellular signal-regulated kinase 1/2. Br J Cancer 99(2): 283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.