Abstract
Background
Melanoma therapy is challenging, especially in advanced cases, due to multiple developed tumor defense mechanisms. Photodynamic therapy (PDT) might represent an adjuvant treatment, because of its bimodal action: tumor destruction and immune system awakening. In this study, a combination of PDT mediated by a metal substituted phthalocyanine—Gallium phthalocyanine chloride (GaPc) and Metformin was used against melanoma. The study aimed to: (1) find the anti-melanoma efficacy of GaPc-PDT, (2) assess possible beneficial effects of Metformin addition to PDT, (3) uncover some of the mechanisms underlining cell killing and anti-angiogenic effects.
Methods
Two human lightly pigmented melanoma cell lines: WM35 and M1/15 subjected to previous Metformin exposure were treated by GaPc-PDT. Cell viability, death mechanism, cytoskeleton alterations, oxidative damage, were assessed by means of colorimetry, flowcytometry, confocal microscopy, spectrophotometry, ELISA, Western Blotting.
Results
GaPc proved an efficient photosensitizer. Metformin addition enhanced cell killing by mechanisms dependent on the cell line, namely apoptosis in the metastatic M1/15 and necrosis in the radial growth phase, WM35. Cell death mechanism relied on the inhibition of nuclear transcription factor (NF)-κB activation and tumor necrosis factor (TNF)—related apoptosis-inducing ligand (TRAIL) sensitization, leading to TRAIL and TNF-α induced apoptosis. Metformin diminished the anti-angiogenic effect of PDT.
Conclusions
Metformin addition to GaPc-PDT increased tumor cell killing through enhanced oxidative damage and induction of proapoptotic mechanisms, but altered PDT anti-angiogenic effects.
General significance
Combination of Metformin and PDT might represent a solution to enhance the efficacy, leading to a potential adjuvant role of PDT in melanoma therapy.
Introduction
Melanoma is a malignant tumor derived from melanocytes with one of the most rapidly increasing incidence in the world. In the past 50 years the mortality has also increased, without any clear path to melanoma prevention [1]. Melanoma registered globally approximately 160 000 new cases and 48 000 deaths/year [2]. Once distant sites from the skin become seeded, melanoma becomes one of the most aggressive tumors, with a life expectancy lower than 12 months. Many treatment strategies like: surgery, chemotherapy, radiotherapy, BRAF and mitogen-activated protein kinase (MAPK) pathway inhibitors, immunotherapy and anti-angiogenic therapies are used related to the stage of the disease. However, tumor resistance mechanisms hinder the efficacy of therapy; therefore future approaches need to focus on this direction. One possible solution might be the old molecule Metformin, due to the inhibition of the stemness character of melanoma cells [3]. Metformin is used as a hypoglicemiant drug in type 2 diabetes mellitus and lately became a promising drug in oncology. Retrospective studies revealed decreased cancer incidence and cancer-related mortality in obese and diabetic patients treated with Metformin [4]. Metformin triggers antitumor activity in several cancers (e.g. lung, breast, prostate and pancreas) [5]. In melanoma, Metformin was shown to induce cell death and arrested melanoma invasion and metastasis, via pro-apoptotic mechanisms [6]. In anti-melanoma therapy there are three ongoing clinical trials that are recruiting patients and are using Metformin in combination with BRAF inhibitors (ClinicalTrials.gov, Identifier: NCT01638676 and NCT02143050) and also in association with Dacarbazine (ClinicalTrials.gov, Identifier: NCT02190838). In a previous study conducted by our group, association of Metformin to PDT in Walker-256 carcinosarcoma experimental model improved the overall anti-tumor effects [7]. Based on these findings, the current research aims to study the possible anti-tumor role of Metformin as an adjuvant in photodynamic therapy against melanoma.
Photodynamic therapy (PDT) is a two steps oncological therapy: (1) administration of a photosensitizer (PS) (2) and tumor irradiation by light of a specific wavelength [8]. Light activation of the PS generates reactive oxygen species (ROS) in the targeted tumor area [9], that destroy tumor cells through cell death induction, destruction of tumor vessels and activation of an immune response [10].
Thus, PDT might be considered an ideal anticancer therapy, because of the primary tumor destruction and also immune activation. This immune reaction should be able to track down and destroy any remaining tumor cells of the primary tumor or distant micro metastases [11]. However, melanoma may be often resistant to PDT. The most important resistance mechanisms are: presence of melanin that absorbs PDT light and has an anti-oxidant effect, sequestration of the PS into melanosomes, apoptotic pathways errors and antioxidant defense that eventually lead to further tumor development [12]. Recent studies gave a new hope by providing encouraging PDT strategies to overcome the aggressiveness of melanoma [13, 14]. These strategies include finding new PS molecules, able to accumulate within tumor cells and to generate enough ROS upon light activation to overcome the resistance of melanoma cells. One group of these photosensitizers is represented by phthalocyanines (Pc). Phtalocyanines are macrocyle compounds activated by the same light wavelengths as porphyrins. Pc are second-generation PS that exhibit important effective tissue penetration due to their chemical stability, high yields of ROS generation and good spectroscopic properties [15]. These make them more suitable in melanoma PDT since they might overcome the melanoma defense. Unfortunately, there is insufficient data regarding their applicability in oncology. In anti-melanoma therapy one report states that aluminium tetrasulfophthalocyanines used at a photosensitizing concentration of 40 μg/mL in combination with a light dose of 4.5 J/cm2 induced melanoma cell death [16]. Gallium phthalocyanine (GaPc), indium (III) and iron (III) phthalocyanine chloride at a concentration of 2 μg/mL were potently phototoxic towards lung cancer cells in vitro upon light regimen exposures of 2.5 J/cm2, 4.5 J/cm2 and 8.5 J/cm2[17].
The present study evaluates the antitumor effects induced by the combined regimen of Gallium phthalocyanine chloride mediated-PDT with Metformin, used as an adjuvant, on two human lightly pigmented melanoma cell lines with different stages of development and aggression: a radial growth phase (WM35) and a metastatic cell line (M1-15), with focus on different mechanisms involved in oxidative stress induced cellular death, angiogenesis and inflammation.
Materials and methods
Chloro-gallium (III) phthalocyanine synthesis and characterisation
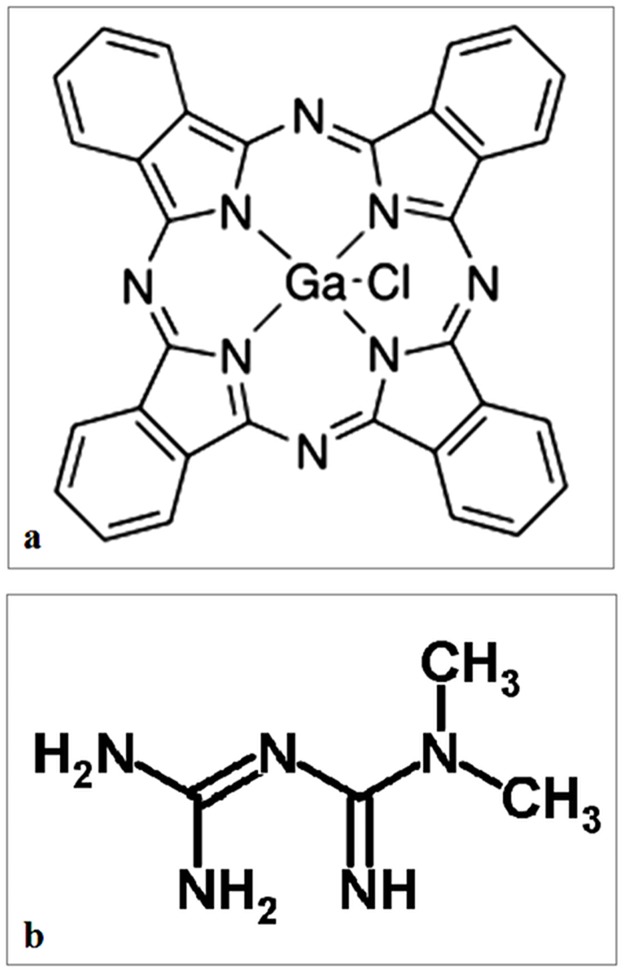
The preparation of Chloro-gallium (III) phthalocyanine (GaPc) was achieved, following a previously reported method [18]. Phthalonitrile (2.00 g, 0.72 mmol) and GaCl3 (0.315 g, 0.27 mmol) were placed in a preheated oil bath (215°C); after that 1-chloronaphthalene (0.35 mL) has been added. The reaction mixture was refluxed under dry inert gas (N2) for 1.5–2 h at the same temperature. After cooling, the product was added to methanol; the precipitate was filtered, washed intensely with methanol and acetone, and dried in vacuum. The products were purified by elution with CHCl3 through a short column (≈ 5 cm) of Al2O3 (Degree 3). Yield: 0.75 g (23%). Chemical formula is presented in Fig 1. UV/Vis (DMSO): λmax (ε) / (nm/M-1.cm-1); 680 (138038), 645 (83170), 610 (10000), 355 (26300). IR (KBr): νmax/cm-1; 1500 (C = C); 1H NMR (DMSO-d6) δ, ppm; 9.80 (8H, d, Pc), 8.60 (8H, d, Pc). MS: m/z = 1059.80. GaPcCl was solubilized in dimethylsulfoxide (DMSO) to prepare a stock solution of 10 μg/ml that was further used to prepare the final solutions in medium immediately before use for cell treatment. The DMSO final concentration in the medium was <0.05%, not toxic to the cells [19].
Fig 1. Chemical formula.
Chloro-gallium (III) phthalocyanine (a) and Metformin (b).
Melanoma bioassays
Cell cultures
The assessment was performed on radial growth phase-WM35 human melanoma (Wistar Institute, Philadelphia, PA, USA) [20] cells and a highly metastatic melanoma cell line M1-15 [21], donated by professor Andras Falus, Genetics Department, University Semmelweis, Budapest. Melanoma cells were cultured in RPMI medium supplemented with 5% fetal calf serum, 50 μg/ml gentamicin and 5 ng/ml amphotericin, all from Biochrom AG (Berlin, Germany), to avoid the medium influence on the cell lines properties, as previously described [22, 23]. For all experiments, the cells were used within 4 passages, to preserve their original melanoma characteristics [24, 25]. Cultures were fed twice weekly and incubated in a humid atmosphere at 37°C and 5% CO2. All experiments were conducted in triplicate in subdued light, as previously described [26].
Light source
PDT irradiation was done by a red light lamp obtained from OSRAM Opto Semiconductors, Bucharest, Romania (wave length 630 nm, lamp power 11.83 mW/cm2, measured at a distance of 5 cm from the lamp) with doses of 2.5 J/cm2 and respectively 5 J/cm2.
Cytotoxicity assay
The cells were seeded at a density of 104/well in ELISA 96 wells micro titration flat bottom plaques and allowed to settle for 24 h. Then cells were exposed for 24 h either to Metformin chloride (8 mM) (Sigma Chemical Co., St. Louis, MO, USA) solved in medium [27] or medium, washed then treated with GaPc, prepared as described above, in concentrations ranging from: 1–2000 μg/ml (1, 10, 25, 50, 100, 200, 500 and 1000) in medium for 24 h. Cells were then washed, afterwards irradiated with 2.5 J/cm2 and 5 J/cm2 and further incubated for 24 h with fresh medium. Experiments using single Metformin exposure in doses ranging from: 0–128 mM (0, 2, 4, 8, 16, 32, 128) were also performed. These cells were then exposed to irradiation in a dose of 2.5 J/cm2 to quantify the combined Metformin irradiation effect on cell viability. Viability was measured by colorimetric measurement of formazan, a coloured compound generated by mitochondrial reductase activity in viable cells using CellTiter 96® AQueous Non-Radioactive Cell Proliferation Assay (Promega Corporation, Madison, WI 53711 USA), as indicated by the producer, readings were done using an ELISA plate reader at 540 nm (Tecan, Männedorf, Switzerland). Untreated cultures exposed to medium were used as controls. Cytotoxicity is presented as OD 540. Pictures were taken through an inverted microscope (Olympus CKX 41, Hamburg, Germany), using a digital camera (Olympus, E 330) and original magnification 10 times.
Experimental design
Melanoma cells (WM35 and M1-15) seeded in Petri dishes at a density of 104/cm2 were exposed to either Metformin, or GaPc, or GaPc with previous Metformin treatment, untreated cells were used as controls. For confocal microscopy studies, WM35 cells were seeded on chamber slides, at a density of 5x103/cm2 (Nalgene, Rochester, NY, USA). Following the different exposure regimens, cells were washed, further incubated for 24 h with medium and afterwards tested for cell death induction (Annexin-FITC/PI staining- flowcytometry, confocal microscopy, TNF—related apoptosis-inducing ligand—TRAIL, ELISA), oxidative stress induced damage and alterations like (malondialdehyde—MDA, nitric oxide (NO) formation spectrophotometry, NF-κB activation, WB), melanogenesis (total melanin content spectrophotometry, tyrosinase protein, microftalmia transcription factor -MITF, WB) inflammation (tumor necrosis factor α -TNF-α, ELISA), cytoskeleton alterations (phalloidin staining, confocal microscopy) and also angiogenesis [vascular endothelial growth factor—VEGF, ELISA; hypoxia inducible factor (HIF)-1α, WB]. The melanin content of the cells was low and had no influence on the methods used for quantification. Moreover, the same method was used for control and treated groups.
Cell death mechanism
For the assessment of cell death mechanism, treated cells (as described in section 2.2.4) were stained with Annexin V-fluorescein isothiocyanate (FITC)/vital dye propidium iodide (PI) (BD Pharmingen Biosciences, San Jose, CA, USA). Viable cells were Annexin V (-)/ PI (-), early apoptotic cells were identified as Annexin V-FITC positive (green) cells, while necrotic cells were PI positive (red fluorescence), late apoptosis was shown by Annexin V (+)/PI (+). Differentiation among these cell populations was done by flow cytometric detection using a BD FACS Canto II flow cytometer (Becton Dickinson & Company, Franklin Lakes, NJ, USA) equipped with two lasers as excitation sources: blue (488 nm, air cooled, 20 mW solid state) and red (633 nm, 17 mW HeNe), as previously described [28]. For confocal microscopy assessment of cell death, cells, treated as above (section 2.5) were stained with Annexin V-FITC/PI, according to the manufacturer’s instructions and then fixed in 2% paraformaldehyde.
Cytoskeleton morphology
Phalloidin—FITC 50 μg/ml (Sigma Chemical Co., St. Louis, MO, USA) a marker for the actin miofilaments (green) was used in combination with DRAQ5 (Sigma) staining (red) for nuclei. Images were recorded using a 63 times oil immersion apochromat Zeiss objective (Zeiss LSM 710 Confocal Laser Scanning unit, Carl Zeiss AG, Oberkochen, Germany). For the annexin—FITC and Phalloidin—FITC excitation/emission of 490/525 nm, for PI a 630/680 nm excitation/emission, for DRAQ5 a 646 nm excitation/detection at 681 nm was used. Image combining, processing, and analysis were performed using the standard ZEN software package (Carl Zeiss MicroImaging GmbH, Oberkochen, Germany) [29].
Melanogenesis assessment
Total melanin content was determined through spectrophotometry (Sigma) as previously described [19]. Data were expressed as mg/ml. The enzymatic activity of tyrosinase, as DOPA oxidase, was determined through spectrophotometry as previously described [19, 30]. Data were expressed as Units/mg protein. All reactive were purchased from Sigma.
Inflammatory and neoangiogenesis markers
Were assessed by ELISA and Western Blot (WB). TRAIL, VEGF and TNF-α ELISA Immunoassay kits from R&D Systems, Inc (Minneapolis, USA) were used. Melanoma cells supernatants were treated according to manufacturer’s instructions; readings were done at 450 nm with correction wavelength set at 540 nm, using an ELISA plate reader (Tecan).
The cell lysates used for the following determinations were prepared as previously described [31]. Protein concentrations were determined by the Bradford method according to the manufacturer’s specifications (Biorad, Hercules, California, USA) and using bovine serum albumin as standard. For all assays the lysates were corrected by total protein concentration. For Western Blotting, lysates (20 μg protein/lane) were separated by electrophoresis on SDS PAGE gels and transferred to polyvinylidenedifluoride membranes, using Biorad Miniprotean system (BioRad, Hercules, Califormia, USA). Blots were blocked and then incubated with antibodies against: NF-κB, phospho- pNF-κB p65 (Ser536) (93H1) (pNF-kB), IκKα, IκKβ (L570) (IP Preferred), phospho-IκK α/β (Ser176/180) (16A6) (pIκK α/β) (Cell Signaling Technology, Inc, Danvers, USA), HIF1α, tyrosinase and MITF (Santa Cruz Biotechnology, Delaware Ave, Santa Cruz, USA) then further washed and incubated with corresponding secondary peroxidase-linked antibodies (Santa Cruz Biotechnology). Proteins were detected using Supersignal West Femto Chemiluminiscent substrate (Thermo Fisher Scientific, Rockford IL, USA), and a Gel Doc Imaging system equipped with a XRS camera and Quantity One analysis software (Biorad). GAPDH (Trevigen Biotechnology Gaithersburg, MD, Maryland, USA) was used as a protein loading control [24, 25].
Oxidative stress-induced damage
To investigate whether PDT can induce oxidative stress, quantification of malondialdehyde (MDA) a marker for the peroxidation of membrane lipids and nitric oxide (NO) formation were performed by spectrophotometry, as previously described. All reactives were purchased from Sigma. Data were expressed as nM/mg protein [32].
Statistical method
Statistical significance of the difference between treated and control group was evaluated by the two-way ANOVA, TTEST and Tukey Posttests. p value less than 0.05 was considered to represent a statistically significant difference. Inhibitory concentration 50% (IC50) was calculated for each cell line and irradiation dose. Statistical package Prism version 6.00 for Windows, GraphPad Software, San Diego, California, USA, www.graphpad.com was used for data analyses.
Results
Cell viability
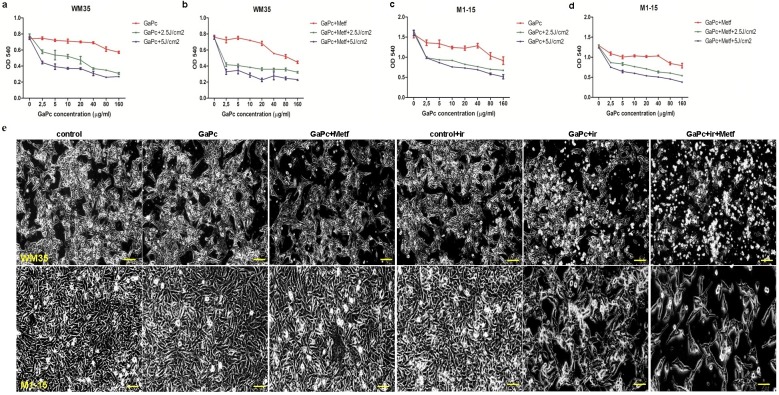
Viability was quantified by colorimetry (Figs 2 and 3). In WM35 melanoma, GaPc-DT reduced viability in a dose dependent manner (IC50 = 26.98 μg/ml at 2.5 J/cm2 and 20.11 μg/ml at 5 J/cm2) with no dark toxicity (IC50 = 161.5 μg/ml) at effective doses (Fig 3).
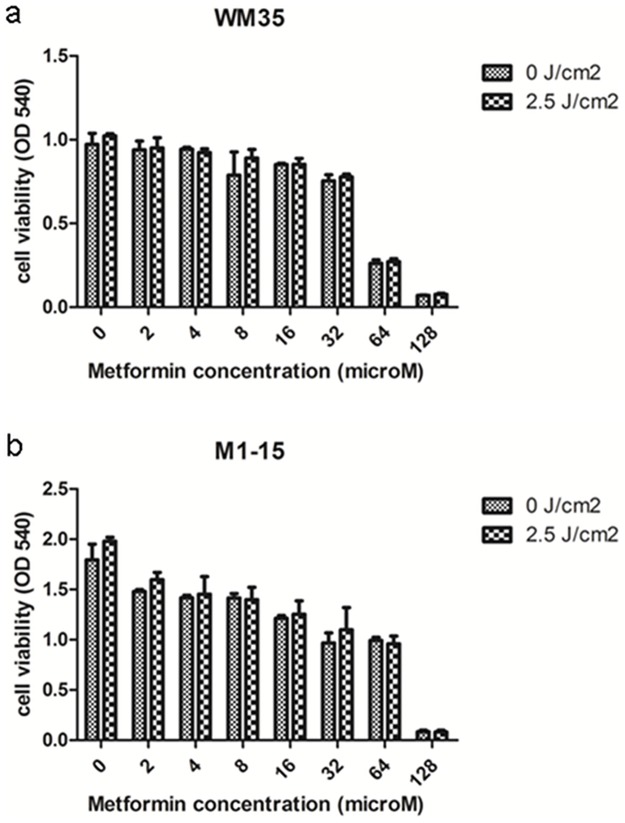
Fig 2. Viability testing after Metformin exposure.
Melanoma cell cultures exposed to different concentrations of Metformin or Metformin and irradiation (a)WM35 and (b)M1-15. OD 540 graphs were generated using GraphPad Software and show mean values ± standard deviation, n = 3 for each sample. Cell viability of both cell lines was decreased by increasing concentrations of Metformin, in a dose dependent manner; irradiation had no effect on the cell viability.
Fig 3. Viability testing after GaPc-PDT and Metformin exposure.
WM35 (a, b), M1-15 (c, d) melanoma cell cultures exposed to GaPc-PDT (a, c), respectively GaPc-PDT+ Metformin (b, d). OD 540 graphs were generated using GraphPad Software and show mean values ± standard deviation, n = 3 for each sample. Cell viability of both cell lines was decreased by GaPc-PDT depending on GaPc concentration and irradiation dose; Metformin increased the efficacy of GaPc-PDT especially in WM35 cells. e-images of WM35 (upper panels) and M1-15 (lower panels) cells subjected to GaPc-PDT and Metformin. Cells exposed to GaPc w/o Metformin, showed a normal morphology, compared to controls, while PDT irradiation of treated cells induced loss of cell adhesion, pleiomorphysm with spherical or bipolar shaped cells, signs of treatment induced photo-toxicity.
Metformin induced a dose dependent decrease in cell viability in both cell lines (Fig 2), independent of irradiation exposure (for WM35, IC50 = 49.5 mM and IC50 = 51.1 mM when Metformin exposure was followed by 2.5 J/cm2 irradiation; for M1-15, IC50 = 28.9 mM and IC50 = 29.5 mM with 2.5 J/cm2 irradiation). When only Metformin was used, the concentration of 8 mM induced a slight, not significant decrease of the viability for the metformin treated cells (p≤ 0.061724) compared to the controls. Therefore, a concentration of 8 mM Metformin, lower than therapeutically relevant plasma concentration of Metformin (20 mM/L) was further used for the PDT combined treatment [33].
Combination treatment of GaPc PDT with Metformin increased dark toxicity (IC50 = 60.22 μg/ml) and phototoxic effects of PDT with IC50 = 11.82 μg/ml at 2.5 J/cm2 and 6.07 μg/ml at 5 J/cm2. In the M1-15 metastatic melanoma line, PDT showed a similar pattern of viability decrease, dependent on the light dose (IC50 = 21.71 μg/ml at 2.5 J/cm2 and 12.18 μg/ml at 5 J/cm2), without dark toxicity (IC50 = 316.35 μg/ml). Improvement of the phototoxic effect due to Metformin addition was discreet (IC50 = 19.56 μg/ml at 2.5 J/cm2 and 11.42 μg/ml at 5 J/cm2), without increasing the dark toxicity of GaPc (IC50 = 327.3μg/ml). Based on these data, the following experiments were done using the GaPc concentration of 7.5 μg/ml and 10 μg/ml for ELISA measurements. PDT light dose was 2.5 J/cm2.
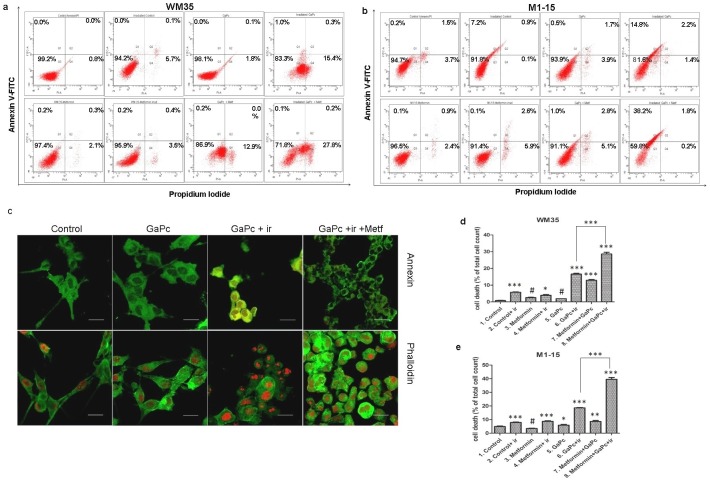
Cell death mechanism
Cell death mechanism was assessed by flowcytometric analysis and confocal microscopy following annexin/PI staining of treated cells with 7.5 μg/ml GaPc (Fig 4). In both cell lines, GaPc showed no significant cell death induction in the absence of irradiation. A high percentage of cell death was obtained in the GaPc-PDT group, with a significant increased cell death from 15.8% to 28.1% for WM35 and from 18.4 to 40.2% for M1-15, when Metformin was added. The main cell death mechanism was necrosis for WM35 and apoptosis for the M1-15 metastatic cell line. Metformin exposure, followed by irradiation increased tumor cell killing in the M1-15 (9.6%), while in the WM35 melanoma cells, it produced no significant effect on cell death. Combination with GaPc potentiated the antitumor effect in both cell lines. These results show that in both melanoma cell lines, Metformin effectively increased PDT induced cell death. This effect is leading to a better therapeutic response overcoming the melanoma activation of survival mechanisms. Moreover, tumor killing was not influenced by the melanoma stage.
Fig 4. Cell death assessment.
Comparative FACS analysis following GaPc-PDT + Metformin treatment versus controls in WM35 (a) and M1-15 (b) cells; c- confocal microscopy images of treated WM35 cells stained with annexin V-FITC/ PI (upper panels) and phalloidin-FITC and DRAQ5 (lower panels), original magnification 63x; PDT exposed cells showed annexin V positive (green) and some exhibit PI positive red fluorescence, while Metformin addition increased the number of annexin V/PI positive cells, there are also present stress related morphological changes; phalloidin staining showed cytoskeleton alterations like increased condensations of actin filaments, retraction of dendrites, spherical shaped cells and loss of cell adhesion in PDT w/o Metformin treated cells. d, e quantitative FACS results for WM35 (d) and M1-15 (e) are expressed as % of total dead cells—annexin V and PI positive cells, from the total cell number; ir = irradiated cells; # = not significant, * = p<5.0E-02, ** = p<1.0E-02, *** = p<1.0E-03. Each bar represents mean ± standard deviation (n = 3).
Cytoskeleton alterations
PDT alterations of the cytoskeleton were seen through confocal microscopy techniques, following phalloidin staining of the actin filaments (Fig 4c). Exposure to GaPc without irradiation did not induce any cytoskeleton alterations. However, in both cell lines exposed to PDT, the actin filaments exhibited condensations, disrupted microtubule network, retraction of dendrites, polymorphism with spherical shaped cells and loss of cell adhesion.
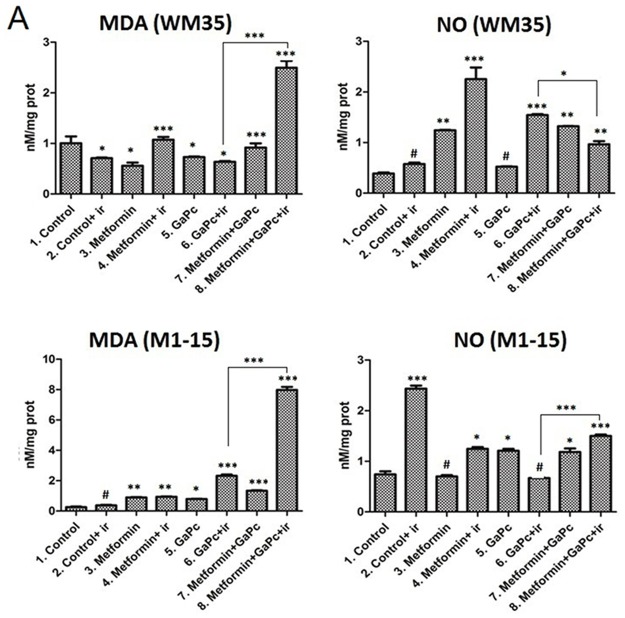
Oxidative stress damage
In order to quantify the oxidative stress and respectively nitrozative stress induced by PDT and combined treatment, MDA, a marker of lipid peroxidation and NO formation were measured (Fig 5).
Fig 5. Oxidative stress assessment.
Malondyaldehide (MDA), nitric oxide (NO) levels (nM/mg protein) measurements in WM35 (upper panels) and M1-15 (lower panels) were done by spectrophotometry. Each bar represents mean ± standard deviation (n = 3). ir = irradiated cells; # = not significant, * = p<5.0E-02, ** = p<1.0E-02, *** = p<1.0E-03.
Malondyaldehide
In both cell lines, GaPc and the combination of GaPc and Metformin without irradiation slightly increased lipid peroxidation. However, MDA levels were significantly elevated (from ~ 0.9 nM/mg protein to 2.6 nM/mg protein in WM35 and from 0.26 nM/mg proteins to 7.9 nM/mg proteins in M1-15) in cells subjected to the combined GaPc-PDT and Metformin therapy, as compared to controls. Moreover, Metformin addition proved beneficial to the oxidative stress induced damage in the treated melanoma cells, compared to GaPc-PDT.
Nitric oxide formation
In both cell lines, NO was increased with irradiation. Metformin addition had a different effect in the melanoma cells. In WM35, Metformin significantly increased the NO, while in the M1-15, it diminished the NO formation and both effects were enhanced by irradiation. When GaPc-PDT was used, NO was highly increased in the WM35 from 0.38 nM/mg protein to 1.54 nM/mg protein. In M1-15 the NO generation, following PDT was not significant. Metformin addition to GaPc-PDT increased NO levels only in M1-15, compared to GaPc-PDT.
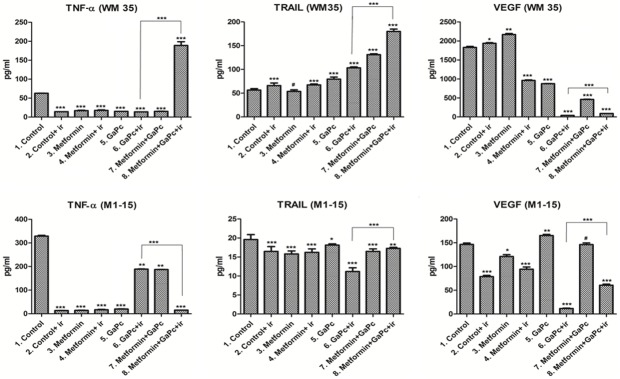
TNF-α and TRAIL expression
To assess the inflammation and its role in the induction of cell death, the levels of TNF-α and the TNF-related apoptosis-inducing ligand were measured by means of ELISA. In the WM35 line, GaPc-PDT and Metformin highly increased TNF-α levels, as well as TRAIL expression, compared to all other groups. This suggests that association of Metformin with GaPc-PDT induced efficient pro-inflammatory and pro-apoptotic responses (Fig 6). Moreover, the high levels of the inflammatory molecules were correlated with oxidative stress (MDA level) and tumor cell death. This effect was different in the case of M1-15. In the untreated M1-15, cells surprisingly secreted high levels of TNF-α, compared to the therapeutical regimen GaPc-PDT and Metformin. This finding emphases the intricate role of TNF-α in cancer. In the metastatic cell line, TNF-α might have a pro-tumoral effect, which explains the high levels in the controls, helping the cells evade from the apoptotic mechanisms. However, TNF-α level was strongly inhibited by the GaPc-PDT and Metformin and this was combined with a high expression of TRAIL, leading to an increased apoptotic cell death. To further study the effect of the therapy induced oxidative stress; we measured, by means of Western Blot, NF-κB activation.
Fig 6. Assessment of inflamatory and angiogenetic markers.
Protein expressions of TNF-α, TRAIL, VEGF (pg/ml) in melanoma cultures exposed to GaPc-PDT + Metformin were determined by ELISA, upper panels (WM35), lower panels (M1-15); Each bar represents mean ± standard deviation (n = 3), ir = irradiated cells; # = not significant, * = p<5.0E-02, ** = p<1.0E-02, *** = p<1.0E-03.
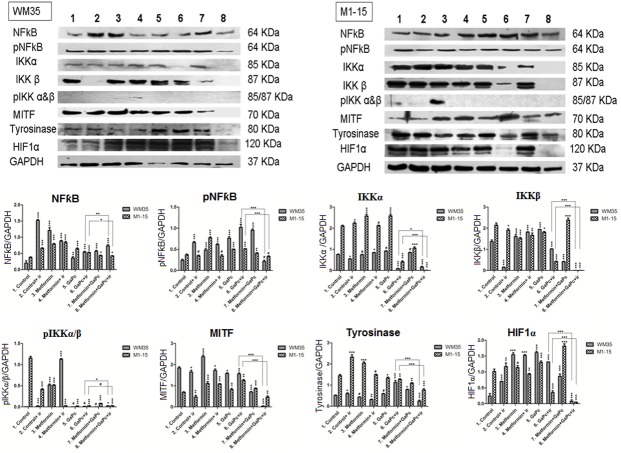
NF-κB activation
In order to assess the role of the NF-κB pathway activation in the survival of the melanoma cells treated with PDT, western blot was performed to quantify the protein levels of the total NF-κB protein and the active form, pNF-κB—p65 (at Ser 536) and also the IκKα, IκKβ and the phosphoryted pIκK. Phosphorylation of p65/RelA at Ser 536 regulates activation, nuclear localization, protein-protein interaction and transcriptional activity. The key in the NF-κB pathway activation involves a high molecular weight Ikappa Kinase (IκK) complex, consisting of three associated IκK subunits. IκKα, and IκKβ serve as the catalytic subunits of the kinase. Activation of the IκK depends on the phosphorylation at Ser 177 and Ser 181 in the activation loop of IκKβ and Ser 176 and Ser 180 in IκKα.
In WM35, irradiation, Metformin exposure and GaPc-PDT increased the expression of NF-κB and pNF-κB, compared to controls. Furthermore, there was a significant increase in NF-κB protein expression induced by GaPc-PDT and Metformin compared to GaPc-PDT (Fig 7). However, only a modest part of NF-κB protein was represented by the active form. In this respect, a higher amount of pNF-κB was obtained when cells were exposed to PDT alone, suggesting that Metformin addition to these cells increased the total NF-κB protein, but decreased NF-κB activation, a mechanism involved in survival of the melanoma cells leading to resistance to PDT. In the M1-15 melanoma, NF-κB protein was significantly increased following irradiation, Metformin and GaPc single exposure and respectively GaPc-PDT, compared to controls. When Metformin was added to GaPc-PDT, NF-κB decreased compared to GaPc-PDT. pNF-κB levels were higher when cells were treated with GaPc and GaPc-PDT. Metformin and GaPc-PDT decreased pNF-κB at control levels.
Fig 7. Protein expression measured by Western Blot.
Protein expressions of NF-κB, pNF-kB, IκKα, IκKβ, pIκK α/β, HIF1α, tyrosinase and MITF in melanoma cells treated with GaPc-PDT + Metformin, left panel (WM35), right panel (M1-15) were measured by WB. Image analysis of WB bands was done by densitometry, results were normalised to GAPDH.—WB images (upper panels) 1 = control, 2 = irradiated control, 3 = Metformin, 4 = irradiated Metformin, 5 = GaPc, 6 = GaPc-PDT, 7 = GaPc and Metformin, 8 = GaPc-PDT and Metformin; graphical representation of quantitative WB results for WM35 and M1-15 (lower panels); ir = irradiated cells; # = not significant, * = p<5.0E-02, ** = p<1.0E-02, *** = p<1.0E-03. Each bar represents mean ± standard deviation (n = 3).
In both cell lines, IκK complex proteins were increased in cells exposed to Metformin and GaPc, while PDT strongly inhibited both of them, leading to extremely low levels in Metformin and GaPc-PDT groups. The active pIκK form was strongly inhibited in the last four groups, when GaPc was used. This shows that even though there was a stimulation of the NF-κB protein following GaPc-PDT, the activation pathway was strongly inhibited by the combined Metformin and GaPc-PDT treatment.
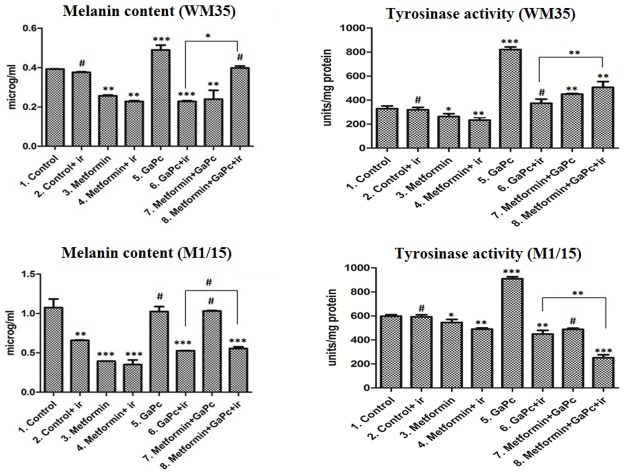
Melanogenesis
To assess the influence of the PDT and Metformin on melanogenesis in the melanoma cells, the total melanin content and the enzymatic activity of tyrosinase (Fig 8), as DOPA oxidase were measured by spectrophotometry. Expression levels of tyrosinase, the key melanogenic enzyme, and the microftalmia transcription factor—MITF, involved in melanogenesis regulation and also survival, differentiation and resistance to PDT were also quantified by means of Western Blotting (Fig 8).
Fig 8. Melanogenesis.
Total melanin content (μg/ml) and tyrosinase enzymatic activity (Units/mg protein) measurements in WM35 (upper panels) and M1-15 (lower panels) were done by spectrophotometry. Each bar represents mean ± standard deviation (n = 3). ir = irradiated cells; # = not significant, * = p<5.0E-02, ** = p<1.0E-02, *** = p<1.0E-03.
Melanin content
As expected, the melanin content was low, since both these cell lines are lightly pigmented. Exposure to GaPc enhanced melanin content, while PDT exhibited a strong inhibitory effect in both cell lines (Fig 8). Metformin and GaPc-PDT induced a melanogenic level similar to the control in WM35 cells while in the M1-15, there was no significant difference between the PDT groups.
Tyrosinase
Tyrosinase activity correlated with the levels of melanin (Fig 8). PDT inhibited the tyrosinase activity in both cell lines, while combined treatment only decreased tyrosinase activity in M1-15 cells. In WM35 melanoma, the tyrosinase protein level was increased by GaPc-PDT compared to controls, while Metformin and GaPc-PDT decreased tyrosinase, compared to controls. In M1-15 cells, GaPc-PDT decreased the tyrosinase, and the combined regimen enhanced this effect (Figs 7 and 8).
MITF
MITF levels were inhibited in WM35 cells by PDT exposure and Metformin potentiated this effect, when used in combination with PDT (Fig 7). Metformin exposure increased MITF expression in both cell lines. In M1-15, MITF protein was enhanced following GaPc-PDT, while Metformin and GaPc-PDT decreased MITF, compared to controls. Overall, melanogenesis was decreased by PDT in the metastatic M1-15 cell line and this effect was enhanced by combined treatment. In WM35 the effects were different. PDT increased melanogenesis. Addition of Metformin strongly inhibited the protein levels of tyrosinase and MITF and decreased melanin and tyrosinase activity compared to PDT alone. The inhibition exerted by the combined treatment on MITF expression was seen in both cell lines.
Neoangiogenesis markers
To assess the possible anti-angiogenic effects of the PDT experimental setting, the hypoxia inducible factor 1 (HIF-1α), involved in carcinomatous neoangiogenesis formation and it’s target, the main neoangiogenesis stimulator, vascular endothelial growth factor (VEGF) were measured by means of Western Blotting and ELISA (Figs 6 and 7).
HIF-1α
In WM35 cells, HIF1-α was increased by Metformin and GaPc treatment, and also by GaPc-PDT. When Metformin was combined with GaPc-PDT, HIF-1α was strongly inhibited (Fig 7). In the M1-15 cell line, HIF-1α basal level was increased. Metformin and GaPc had almost no effect on the protein expression. PDT diminished HIF-1α compared to controls and the combined treatment had a stronger effect.
VEGF
In both melanoma cell lines, GaPc-PDT and GaPc-PDT associated with Metformin showed an important antiangiogenic activity in contrast with the high levels of VEGF in the untreated cells (Fig 6). However, the combined treatment had a lower inhibitory effect on VEGF compared with GaPc-PDT alone. Overall, PDT inhibited neoangiogenetic promoting factors in both cell lines. This effect was stronger with the combined treatment in the case of HIF-1α.
Discussion
The present research investigates the possible benefits of using Metformin as an adjuvant in PDT against two human melanoma cell lines with different degrees of aggression: WM35, a radial growth phase line and M1-15, a metastatic melanoma line, with focus on cell death, oxidative stress induced damage, inflammation and angiogenesis.
In addition, we also studied the efficiency of Gallium phthalocyanine chloride (GaPc) as a photosensitizer in PDT against melanoma. In a previous study, we found good PDT efficacy against WM35 melanoma cells using as PS an Indium substituted Pc: chloride indium (III) Pc [ClIn (III)Pc], activated by red light at a dose of 6 J/cm2 [34].
In our study, GaPc decreased viability in both melanoma cell lines, in a dose related manner, without dark toxicity. PDT efficiency was increased in the case of WM35. This is consistent with results presented by others that found GaPc to be an efficient photosensitiser, in different cancers such as: colon cancer Caco-2 cells or lung cancer cells [35, 35, 36] Although, we found no evidence of GaPc-PDT assays in melanoma, another Pc used for PDT, aluminum tetrasulfophthalocyanine showed efficient melanoma cells killing. Pc’s properties can be improved by incorporating metals such as gallium, zinc and aluminium [17, 36]. Metallation of PCs with diamagnetic ions: Zn 2+, Al 3+, and Ga 3+, was reported to increase photosensitiser quantum yields and lifetimes (ΦT 0.56, 0.50 and 0.34 and τT 187, 126 and 35 μs) [37, 38]. This potentially increases the photosensitiser capabilities. However, the problem of tumor delivery still remains, mainly due to their lipophylic character, poor tumor specificity and the Pc tendency to aggregate. A number of possible delivery strategies have been suggested, ranging from the use of oil-in-water (o/w) emulsions to liposomes and nanoparticles as potential carrier vehicles reviewed in Josefson, et al [23, 39, 40, 41, 42, 43, 44] and to enhance the cellular uptake and subsequent antitumor efficacy of PDT [45, 46, 47].
Addition of Metformin to the GaPc-PDT treatment increased the therapy efficiency in both cell lines, similarly to our previous report for Walker carcinosarcoma PDT [7]. In the M1-15 metastatic melanoma, Metformin significantly increased PDT cell killing and induced apoptosis of the melanoma cells. However, the beneficial effect was relatively small in terms of viability decrease, when PDT was concerned; GaPc-PDT and Metformin increased the induction of apoptosis at a small dose of photosensitizer and light exposure.
The origin of the melanoma metastatic cells seems to be from a population of melanoma initiating cells, that resemble stem cells characters and are resistant to chemotherapy [48, 49]. These tumors stem cells are CD133 positive and induce chemoresistance by activating different survival proteins involved in the Akt/PKB and Bcl-2 pathway. Furthermore, activation of Akt/PKB pathway induces cellular antiapoptotic effects, increases protein synthesis and proliferation through rapamycin (mTOR) binding [50]. Metformin inhibits malignant metastatic and stem cell growth through blocking of the metabolic pathway AKT/mTOR. These effects were reported on different cell lines: hMCF-7 human mammary carcinoma and FSaII mouse fibrosarcoma cells [51] and combined with doxorubicine on in vivo and in vitro breast cancer tumors [52].
In cancerous cells, glucose metabolism is switched to aerobic glycolysis -Warburg effect, and generates a high amount of energy, as well as metabolites like lactate and ketones that promote tumor cells “immortality”. Metformin interferes with the mitochondrial metabolism and can lower both energy and glucose metabolites production [51]. These mechanisms might explain the addictive effect of Metformin to PDT efficiency.
In both cell lines, cell death correlated with the alteration of the cytoskeleton filaments and a high level of lipid peroxidation, indirect hallmarks of ROS, as a result of the Metformin induced inhibition of the antioxidant defense in melanoma cells. This is consistent with previous reports about the roles of PDT induced ROS leading to DNA damage and subsequent caspase activation followed by tumor cell death [53]. Cytoskeleton disorganization as a result of PDT has been reported in different cell lines: in a chronic myelogenous leukemia-derived cell line (K562), glioblastoma (D54Mg) in ALA mediated PDT, or WM35 in PDT with two mesoporphyrins meso-5,10,15,20-tetrakis (4-hydroxyphenyl) porphyrin (THOPP) and meso-5-(4-hydroxyphenyl)-10, 15, 20- tris (4-methoxyphenyl) porphyrin (THOMPP) [24, 54, 55]. PDT with zinc(II)-phthalocyanine (ZnPc) of three cell lines indirectly induced changes in microtubules and F-actin in HeLa cells, correlated with apoptosis [56].
In the current study we measured the protein levels of two members of the TNF family: TNF-α and TRAIL, secreted by the melanoma cells as a result of GaPc-PDT w/o Metformin, in an effort to understand their role in the switch between survival, leading to resistance to therapy and apoptosis in the melanoma cells. Similarly, with ROS, TNF-α has a dual role in melanomagenesis and response to therapy. Through binding to specific receptors, TNF-α can induce more than 5 pathways that end up with inflammation, apoptosis, proliferation, invasion, angiogenesis, metastasis or morphogenesis. Furthermore, these pathways lead to contradictory effects: both anti-apoptotic and pro-apoptotic [57]. Although, TNF-α is able to induce tumor cell death, its primary role is pro-inflammatory [58]. TNF-α is a negative prognostic factor in surgery and correlates with resistance to chemotherapy, while high tumor levels of TNF-α might be beneficial for the melanoma immunotherapy [44]. Melanoma WM35 cell line was previously found to be resistant to TNF-α but not to TRAIL induced apoptosis [59]. On the other hand, TRAIL selectively induces apoptosis of tumor and premalignant cells, but not normal cells [54]. Unfortunately, most primary cancer cells are resistant to TRAIL induced apoptosis due to preexistent p53 mutations, absence of specific death receptors from cell surface or presence of abundant decoy receptors [54]. TRAIL is involved in triggering the extrinsic pathway of apoptosis. Binding of TRAIL to surface death receptors initiates their trimerization and starts recruiting Fas-associated death receptor (FADD) leading to caspase-8 activation [54]. In type I cells, caspase-8 activation is enough for apoptosis, while, in type II cells, the extrinsic pathway should be completed with mitochondrial pathway activation to sustain the apoptotic process [60]. Expression of TRAIL receptor 2 on melanoma cells was correlated to a better prognosis [61].
In the WM35 melanoma cells, TNF-α as well as TRAIL expression and oxidative damage were strongly increased by the combined GaPc-PDT associated with Metformin, as opposed to single GaPc-PDT. In a previous PDT study, on WM35 cells, high levels of TNF-α generated by PDT were mainly anti-apoptotic and led to NF-kB activation, a mechanism involved in cell survival under oxidative stress [30]. In the current study, NF-kB expression, as well as the phosphorilated form was diminished, therefore, this mechanism of survival was not efficient in preventing oxidative cell death. Thus, the high expressions of both TNF family members led to the activation of apoptosis. The pro-apoptotic effects were strongly enhanced by Metformin treatment and are linked to the effects on mitochondrial glucose metabolism generated in the melanoma cells [51] that rendered the cells susceptible to a higher oxidative damage induced by PDT. This led to a combination of necrotic and apoptotic cell death. These effects were different in the highly metastatic M1-15 melanoma. M1-15 cells constitutively expressed high levels of TNF-α and TRAIL. This is probably due to the tumor promotion exerted by these molecules, by binding to pro-inflammatory receptors [62] and TRAIL decoy death receptors with roles in proliferation or decreased TRAIL sensitivity [57], [60, 62]. Combined exposure to Metformin and GaPc-PDT significantly decreased TNF-α, while endogenous TRAIL expression remained at high levels.
NO synthesis is mainly governed by iNOS, whose expression is regulated by the transcription factor NF-κB [34, 63, 64]. NF-κB protein was enhanced following GaPc-PDT, but the activation pathway was strongly inhibited by PDT, as proved by the decreased levels of IKκ and the phosphorilated form. The effect was increased by Metformin addition. As a result it also inhibited the expression of iNOS and, therefore, NO production, especially in M1-15 cells. On the other hand, NO may inhibit IKκ via S-nitrosylation, and decreases free NF- κB level, which creats a negative-feedback loop [65].
NF-κB and pNF-κB were slightly increased, following GaPc-PDT but this survival mechanism was not enough to prevent cell death [21, 44]. In these conditions, TRAIL induced apoptosis might be explained by the sensitization of the M1-15 melanoma to TRAIL, following the combined therapy. Sensitivity of tumor cells to TRAIL apoptosis may be restored by a number of substances and biological agents [61–66]: proteasome inhibitors, mainly, but not restricted to inhibition of NF-kB activation, AKT inhibition, mitogen-activated protein kinase (MAPK), protein kinase C (PKC) activation, reactive oxygen species, interferon, resveratrol, tunicamycin, histone deacetylase inhibitors, 2-methoxyestradiol, synthetic triterpenoids, peroxysome proliferators-activated receptor agonists, betulinic acid and telomerase-dependent virotherapy [61, 66]. Metformin exposure was involved in AKT inhibition [52, 53] and the combination with PDT increased therapeutically ROS induced damage, and decreased NF-κB activation. All these, were able to restore TRAIL sensitivity in M1-15 cells, leading to apoptosis. This behavior is consistent with a previous report, stating that inhibition of NF-κB in colon and mammary carcinoma cells switched the inflammatory LPS-induced tumor growth to tumor regression. This response was found to be independent of TNF-α, but dependent on TRAIL. Thus, an interesting future direction for increasing PDT efficiency in melanoma could be linked to exogenous TRAIL addition to this line of therapy, which has the potential to take advantage of the recovered TRAIL sensitivity in melanoma cells and to induce selective tumor cell apoptosis.
Both cell lines showed a low melanogenic level. Melanogenesis was inhibited by PDT in the metastatic M1-15 cells, while in the radial growth phase WM35, the effect was the opposite. Metformin seemed to have an inhibitory effect, while GaPc exposure increased melanogenesis. As such, combined treatment decreased melanogenesis activation due to the GaPc exposure. This is consistent with our previous PDT study, where we found increased melanogenesis following PDT with meso-substituted porphyrins on WM35 cells [29]. This effect was consistently seen on the total melanin content and the activity of the key melanogenic enzyme, tyrosinase. In WM35 cells, PDT induced a higher pigmentation level along with increased tyrosinase activity but it decreased the tyrosinase protein level. These differences can be explained by the activation of existing tyrosinase by PDT induced ROS [67]. However, ROS, especially hydrogen peroxide, in a high amount, may also be responsible for the inactivation of the tyrosinase [68]. Similarly, pigmentation could have been increased following PDT through ROS oxidation of melanin precursors. These differences were mainly seen in the WM35 cells, because of the low level of constitutive pigmentation that allowed the smaller modifications to became apparent. In the case of WM35, PDT also induced necrotic cell death, at a lower lipid peroxidation level compared to M1-15, possibly due to a lower melanoma resistance to oxidative stress. In patients with melanoma, the prognosis was shown to be influenced by the pigmentation. In patients with early stage (I and II) melanoma, pigmentation was correlated with a better survival, while in advanced stages, melanoma pigmentation impaired the prognosis [69]. This is probably due to the melanogenesis process that can delay tumor growth when is normal, while deregulation of pigment synthesis and/or pheomelanogenesis will have a stimulatory impact on tumor growth because of active melanin precursors, leading to ROS and accumulating mutations [69]. TRPM1 (melastatin) expression loss occurred at the transition of radial to vertical growth primary cutaneous melanoma [70]. Moreover, melanogenesis in metastatic melanomas was related to resistance to radio [71] and chemotherapy and also immunosuppressive effects [72], while the inhibition of melanogenesis restored melanoma sensitivity to gamma rays [73], cyclophosphamide and reverted the immunosuppression due to melanin synthesis [72]. Therefore, inhibition of melanogenesis is likely to improve the outcome of the therapy of metastatic melanoma [71]. Therefore, inhibition of melanogenesis, mostly seen in the metastatic M1-15 cell line represents a beneficial effect of the GaPc PDT, enhanced by Metformin addition.
Many factors were involved in stimulation of melanogenesis after UV exposure, like lipids peroxidation, ROS production, MAPK, TNF-α pathway, DNA damage—DNA repair processes enhanced by melanin [74, 75, 76]. Moreover, MITF expression was related to increased survival following oxidative stress [77]. Increased MITF was related to a lower prognosis in melanoma patients, resistance to therapies and particularly PDT, while decreased levels were associated with a better PDT therapeutic response [31]. Since MITF is very widely expressed in human melanomas, the found that the combination of PDT and Metformin had the ability to inhibit it, along with the inhibition of NF-κB pathway activation seems really promising. Moreover, this was consistent in both melanoma cell lines.
Neoangiogenesis is involved in tumor promotion, invasion and metastasis, critical steps in melanoma progression. Thus, we investigated the effects of GaPc-PDT and Metformin on the synthesis and expression of the main two factors involved in stimulating carcinomatous neoangiogenesis: VEGF and HIF-1α. HIF-1α is the transcription factor in charge of the cellular response to hypoxia, including generated by a growing malignant tumor environment that consists mainly in angiogenesis and apoptosis. Once stimulated, HIF-1α translocates into the nucleus, binds to the hypoxia-response element, and up-regulates the expression of VEGF and other angiogenic factors at mARN and protein levels [78, 79].
Our data showed that PDT and respectively Metformin and PDT inhibited the expression of the VEGF and HIF-1α, in the melanoma cells. However, future in vitro studies on co-culture models and in vivo studies are necessary to support these findings [80]. There is a strong, GaPc-PDT induced inhibition of VEGF and HIF-1α, consistent for both cell lines, while combined regimen decreased this effect. Previously, we have reported that the combination of Metformin and PDT reduced angiogenesis in vivo, on Walker carcinosarcoma [7]. There are reports showing a beneficial role of Metformin in the inhibition of neoangiogenesis [81, 82, 83]. Metformin also induced increased survival, accelerated tumor growth and increased VEGF-A in BRAF V600 mutant melanomas [84]. This is consistent with our findings of stimulating effects of Metformin on VEGF and HIF-1α in WM35 melanoma, since this cell type exhibits the BRAF-V600E-mutation. Interestingly, in the BRAF-V600E-mutated melanomas, it was reported that association of Metformin with anti-angiogenic therapies has a cumulative effect on cell killing [85]. In this respect, the combination of GaPc-PDT, with an inhibitory effect on angiogenesis and Metformin might explain the strong beneficial effect of cell death induction in WM35 cells. It was shown that HIF-1α is a direct target gene of NF-κB under non-hypoxic and certain hypoxic conditions. Activation of NF-κB leads to increased HIF-1α protein levels. HIF-1α also contributes to the activation of the NF-κB pathway; moreover, both proteins seem to be regulated by the same pathways, involving IKKβ hydroxylation [86]. This is consistent with our data, where there is a similar trend within these protein levels. Metformin was described to inhibit NF-κB activation in normal cell lines [35,87] senescent cells [88] and cancer cells [89]. The main antitumor mechanism seems to be related to reversible inhibition of the mitochondrial complex I function which has also been involved in the hypoxic inhibition of HIF-1α. The effect requires an intact mitochondrial inner membrane potential. Metformin reduced HIF-1α in colon cancer cells-HCT 116 p53−/− and significantly diminished downstream HIF dependent proteins like VEGF, and carbonic anhydrase 9 (CA9) in these cells, under hypoxic conditions (1.5% O2), however, it slightly increased HIF-1α, VEGF and CA9 under normal O2 concentration (21%)[87].
The aim of our study was to find if Metformin might increase melanoma cells sensitivity to PDT and improve the overall treatment response. Therefore, in our experimental setting, cells with prior 24h Metformin exposure were exposed to GaPc for 24h, irradiated then collected after an additional 24h period, following PDT irradiation. Cells exposed to Metformin were treated with medium in a similar manner. Since the Metformin inhibition of mithocondrial function is reversible [87], the time elapsed between exposure and the end of the experiments diminished the Metformin effects and allowed the cells to recover, in the absence of PDT. This could explain the reactive increase of NF-κB activation, HIF-1α and VEGF in groups without PDT. When combined treatment was used, the angiogenetic markers like VEGF and at a lower extent HIF-1α, although significantly inhibited compared to controls, remained at higher levels, compared to PDT alone. This could be partially explained by the experimental setting, as above, however, this effect might be also due to the stimulatory effect of Metformin on these molecules in normoxic conditions [87]. In melanoma, induction of melanogenesis was shown to increase HIF-1α and stimulate the expression of several downstream HIF-1 regulated genes, including VEGF. This was attributed to the role of melanogenesis intermediates that lead to ROS and consumption of intracellular oxygen due to the activation of the melanogenic pathway [90]. These are consistent with our data for the GaPc treated cells, where increased HIF-1α, was correlated with high melanogenesis. When GaPc PDT was used, cells exhibited higher HIF-1α in WM35 cells that correlated with the absence of melanogenesis inhibition (lower melanin, but tyrosinase activity was similar to controls). In M1-15 cells, lower HIF-1α correlated with inhibition of melanogenesis.
PDT is an ideal oncological approach because induces direct tumor cell photo damage and also targets tumor vasculature and activates the immune response [91, 92]. Despite these effects, there is a limited experience of PDT in melanoma and extensive clinical studies need to be taken into consideration, using selected photosensitizers and standard irradiation protocols and also several combination regimens with chemotherapy or immunotherapy, in order to obtain an established antitumor effect [11].
Conclusions
GaPc proved an efficient PS in PDT against these low pigmented melanoma cell lines: WM35 and M1-15. The beneficial antimelanoma effects of Metformin addition to PDT resided mainly in increased tumor cell killing through enhanced oxidative damage and induction of proapoptotic mechanisms, while the inhibition of tumor angiogenesis promoted by PDT was decreased by Metformin.
Abbreviations
- AKT/PKB
phosphatidylinositol 3-kinase and protein kinase B
- Bcl-2
B cell lymphoma 2
- BRAF
protooncogene B-Raf
- DMSO
dimethylsulfoxide
- DNA
deoxiribonucleic acid
- DRAQ5
far red fluorescent DNA dye
- ELISA
enzyme-linked immunosorbent assay
- FACS
flowcytometry
- FADD
Fas-associated death receptor
- FITC
fluorescein isothiocyanate
- GaPc
Gallium phthalocyanine chloride
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase human
- HIF-1α
hypoxia inducible factor 1 alpha
- IC50
Inhibitory concentration 50%
- ikK
inhibitor of nuclear factor kappa-B-kinase
- iNOS
nitric oxide synthase inducible
- LPS
lipopolysaccharide
- MAPK
mitogen-activated protein kinase
- mARN
messenger ribonucleic acid
- MDA
malondialdehyde
- MITF
microftalmia transcription factor
- mTOR
mammalian target of rapamycin
- NF-κB
nuclear transcription factor kB
- NO
nitric oxide
- Pc
phthalocyanines
- PDT
photodynamic therapy
- PI
propidium iodide
- PKC
protyein kinase C
- pNF-κB
phosphorilated nuclear transcription factor kB
- PS
photosensitizer
- ROS
reactive oxygen species
- RPMI
Roswell Park Memorial Institute
- SDS PAGE
dodecyl sulfate polyacrylamide gel electrophoresis
- TNF-α
tumor necrosis factor alpha
- TRAIL
TNF-related apoptosis-inducing ligand
- VEGF
vascular endotelial growth factor
- WB
western blotting
- WM1/15
metastatic cell line
- WM35
melanoma in radial growth phase
Data Availability
All relevant data are within the paper.
Funding Statement
This paper was supported by 1493/4/28.01.2014, 4945/4/08.03.2016 Iuliu Hațieganu” University of Medicine and Pharmacy, Cluj-Napoca, Romania and National Grant PN-III-P2-2.1-PED-2016-1521. We also affirm that the paper doesn’t have any grants or contracts from a government agency, a non profit foundation, or a company supporting the preparation of the manuscript or the described research. The OSRAM Opto Semiconductors, OSRAM Romania provided support in the form of salaries for authors [LG], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Berwick M, Buller DB, Cust A, Gallagher R, Lee TK, Meyskens F, et al. Melanoma epidemiology and prevention InMelanoma 2016. (pp. 17–49). Springer International Publishing. [DOI] [PubMed] [Google Scholar]
- 2.Eggermont AM, Spatz A, Robert C. Cutaneous melanoma. The Lancet. 2014. March 7;383(9919):816–27. [DOI] [PubMed] [Google Scholar]
- 3.Menendez JA. Metabolic control of cancer cell stemness: Lessons from iPS cells. Cell Cycle. 2015. December 17;14(24):3801–11. 10.1080/15384101.2015.1022697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005. June 4;330(7503):1304–5. Epub 2005 Apr 22. 10.1136/bmj.38415.708634.F7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salani B, Del Rio A, Marini C, Sambuceti G, Cordera R, Maggi D. Metformin, cancer and glucose metabolism. Endocrine-related cancer. 2014. December 1;21(6):R461–71. 10.1530/ERC-14-0284 [DOI] [PubMed] [Google Scholar]
- 6.Cerezo M, Tomic T, Ballotti R, Rocchi S. Is it time to test biguanide metformin in the treatment of melanoma? Pigment cell & Mel Res. 2015. January 1;28(1):8–20. [DOI] [PubMed] [Google Scholar]
- 7.Nenu I, Popescu T, Aldea MD, Craciun L, Olteanu D, Tatomir C, et al. Metformin associated with photodynamic therapy-a novel oncological direction. J Photochem Photobiol B. 2014;138:80–91. 10.1016/j.jphotobiol.2014.04.027 [DOI] [PubMed] [Google Scholar]
- 8.Dolmans DE, Fukumura D, Jain RK. Photodynamic therapy for cancer. Nat Rev Cancer. 2003;3:380–387. 10.1038/nrc1071 [DOI] [PubMed] [Google Scholar]
- 9.Agostinis P, Berg K, Cengel KA, Foster TH, Girotti AW, Gollnick SO, et al. Photodynamic therapy of cancer: an update. CA: a cancer journal for clinicians. 2011. July 1;61(4):250–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castano AP, Mroz P, Hamblin MR. Photodynamic therapy and anti-tumor immunity. Nat Rev Cancer 2006; 6: 535–545. 10.1038/nrc1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baldea I, Filip AG. Photodynamic therapy in melanoma-an update. J Physiol Pharmacol. 2012. April 1;63(2):109–18. [PubMed] [Google Scholar]
- 12.Sharma SK, Huang YY, Hamblin MR. Melanoma Resistance to Photodynamic Therapy In Resistance to Photodynamic Therapy in Cancer 2015. (pp. 229–246). Springer International Publishing. [Google Scholar]
- 13.Sharma KV, Davids LM. Depigmentation in melanomas increases the efficacy of hypericin-mediated photodynamicinduced cell death. Photodiagn Photodyn Ther 2012; 9: 156–63. [DOI] [PubMed] [Google Scholar]
- 14.Monge-Fuentes V, Muehlmann LA, de Azevedo RB. Perspectives on the application of nanotechnology in photodynamic therapy for the treatment of melanoma. Nano reviews. 2014. September 1;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swavey S, Tran M. Porphyrin and Phthalocyanine Photosensitizers as PDT Agents: A New Modality for the Treatment of Melanoma, Recent Advances in the Biology, Therapy and Management of Melanoma, Dr. Lester Davids (Ed.), 2013. http://www.intechopen.com/books/recent-advances-in-the-biology-therapy-and-management-of-melanoma/porphyrin-and-phthalocyanine-photosensitizers-as-pdt-agents-a-new-modality-for-the-treatment-of-melanoma.
- 16.Spikes JD. Phthalocyanines as photosensitizers in biological systems and for the photodynamic therapy of tumors. Photochem Photobiol. 1986. June 1;43(6):691–9. [DOI] [PubMed] [Google Scholar]
- 17.Maduray K, Odhav B. The in vitro photodynamic effect of laser activated Gallium, indium and iron phthalocyanine chlorides on human lung adenocarcinoma cells. J Photochem Photobiol B. 2013. November 5;128:58–63. Epub 2013 Aug 17. 10.1016/j.jphotobiol.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 18.Linsky JP, Paul TR, Nohr RS, Kenney ME. Studies of a series of haloaluminum,-gallium, and-indium phthalocyanines. Inorganic Chemistry. 1980. October;19(10):3131–5. [Google Scholar]
- 19.Baldea I, Costin GE, Shellman Y, Kechris K, Olteanu ED, Filip A, et al. Biphasic pro-melanogenic and pro-apoptotic effects of all-trans-retinoic acid (ATRA) on human melanocytes: Time-course study. Journal of dermatological science. 2013. November 30;72(2):168–76. 10.1016/j.jdermsci.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 20.Meier F, Nesbit M, Hsu MY, Martin B, Van Belle P, Elder DE, et al. Human melanoma progression in skin reconstructs: biological significance of bFGF. The American journal of pathology. 2000. January 31;156(1):193–200. 10.1016/S0002-9440(10)64719-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hegyesi H, Somlai B, Varga VL, Toth G, Kovacs P, Molnar EL, et al. Suppression of melanoma cell proliferation by histidine decarboxylase specific antisense oligonucleotides. Journal of investigative dermatology. 2001. July 31;117(1):151–3. 10.1046/j.0022-202x.2001.01406.x [DOI] [PubMed] [Google Scholar]
- 22.Slominski A, Zmijewski MA, Pawelek J. L?tyrosine and L?dihydroxyphenylalanine as hormone?like regulators of melanocyte functions. Pigment cell & melanoma research. 2012. January 1;25(1):14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolnicka-Glubisz A, Nogal K,?? d?o A, P?onka PM. Curcumin does not switch melanin synthesis towards pheomelanin in B16F10 cells. Archives of dermatological research. 2015. January 1;307(1):89–98. 10.1007/s00403-014-1523-1 [DOI] [PubMed] [Google Scholar]
- 24.Plonka PM, Slominski AT, Pajak S, Urbanska K. Transplantable melanomas in gerbils (Meriones unguiculatus). II: melanogenesis. Experimental dermatology. 2003. August 1;12(4):356–64. [DOI] [PubMed] [Google Scholar]
- 25.SÉOMI?SKI A, BOMIRSKI A. Phenotypic changes of Ab hamster melanoma during long-term culture. Anticancer research. 1985;5:403–10. [PubMed] [Google Scholar]
- 26.Kleemann B, Loos B, Scriba TJ, Lang D, Davids LM. St John's Wort (Hypericum perforatum L.) photomedicine: Hypericin-photodynamic therapy induces metastatic melanoma cell death. PloS one. 2014. July 30;9(7):e103762 10.1371/journal.pone.0103762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cerezo M, Tichet M, Abbe P, Ohanna M, Lehraiki A, Rouaud F, et al. Metformin blocks melanoma invasion and metastasis development in AMPK/p53-dependent manner. Molecular cancer therapeutics. 2013. August 1;12(8):1605–15. 10.1158/1535-7163.MCT-12-1226-T [DOI] [PubMed] [Google Scholar]
- 28.Olteanu D, Baldea I, Clichici S, Bolfa P, Cenariu M, Schrepler-Perde M, et al. In vitro studies on the mechanisms involved in chemoprevention using Calluna vulgaris on vascular endothelial cells exposed to UVB. Journal of Photochemistry and Photobiology B: Biology. 2014. July 5;136:54–61. [DOI] [PubMed] [Google Scholar]
- 29.Baldea I, Olteanu DE, Bolfa P, Tabaran F, Ion RM, Filip GA. Melanogenesis and DNA damage following photodynamic therapy in melanoma with two meso-substituted porphyrins. Journal of Photochemistry and Photobiology B: Biology. 2016. August 31;161:402–10. [DOI] [PubMed] [Google Scholar]
- 30.Ohkura T, Yamashita K, Mishima Y, Kobata A. Purification of hamster melanoma tyrosinases and structural studies of their asparagine-linked sugar chains. Arch Biochem Biophys 1984;235:63–77. [DOI] [PubMed] [Google Scholar]
- 31.Baldea I, Olteanu DE, Bolfa P, Ion RM, Decea N, Cenariu M, et al. Efficiency of photodynamic therapy on WM35 melanoma with synthetic porphyrins: Role of chemical structure, intracellular targeting and antioxidant defense. Journal of Photochemistry and Photobiology B: Biology. 2015. October 31;151:142–52. [DOI] [PubMed] [Google Scholar]
- 32.Filip A, Daicoviciu D, Clichici S, Mocan T, Muresan A, Postescu ID. Photoprotective Effects of Two Natural Products on Ultraviolet B-Induced Oxidative Stress and Apoptosis in SKH-1 Mouse Skin. J Med Food. 2011. July 1;14(7–8):761–6. 10.1089/jmf.2010.0142 [DOI] [PubMed] [Google Scholar]
- 33.Isoda K, Young JL, Zirlik A, MacFarlane LA, Tsuboi N, Gerdes N, et al. Metformin inhibits proinflammatory responses and nuclear factor-?B in human vascular wall cells. Arteriosclerosis, thrombosis, and vascular biology. 2006. March 1;26(3):611–7. 10.1161/01.ATV.0000201938.78044.75 [DOI] [PubMed] [Google Scholar]
- 34.Baldea I, Ion RM, Olteanu DE, Nenu I, Tudor D, Filip AG. Photodynamic therapy of melanoma using new, synthetic porphyrins and phthalocyanines as photosensitisers-a comparative study. Clujul Med. 2015;88(2):175 10.15386/cjmed-419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nombona N, Maduray K, Antunes E, Karsten A, Nyokong T. Synthesis of phthalocyanine conjugates with gold nanoparticles and liposomes for photodynamic therapy. Journal of Photochemistry and Photobiology B: Biology. 2012. February 6;107:35–44. [DOI] [PubMed] [Google Scholar]
- 36.Leanne B J, Ross W B. Photodynamic therapy and the development of metal-based photosensitisers. Metal-based drugs. 2008. September 7;2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali H, van Lier JE. Metal complexes as photo- and radio-sensitizers. Chemical Reviews.1999;99(9):2379–2450. [DOI] [PubMed] [Google Scholar]
- 38.Guldi DM, Mody TD, Gerasimchuk NN, Magda D, Sessler JL. Influence of large metal cations on the photophysical properties of texaphyrin, a rigid aromatic chromophore. J Am Chem Soc. 2000;122(34):8289–8298. [Google Scholar]
- 39.Bonnett R, Martinez G. Photobleaching of sensitisers used in photodynamic therapy. Tetrahedron.2001;57(47):9513–9547. [Google Scholar]
- 40.Dougherty TJ, Gomer CJ, Henderson BW, et al. Photodynamic therapy. J National Cancer Institute. 1998;90(12):889–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nyman ES, Hynninen PH. Research advances in the use of tetrapyrrolic photosensitizers for photodynamic therapy. J Photochem Photobiol B. 2004;73(1–2):1–28 [DOI] [PubMed] [Google Scholar]
- 42.Lang K, Mosinger J, Wagnerová DM. Photophysical properties of porphyrinoid sensitizers non-covalently bound to host molecules; models for photodynamic therapy. Coordination Chem Rev.2004;248(3–4):321–350. [Google Scholar]
- 43.Alvarez MG, Vittar NBR, Principe F, et al. Pharmacokinetic and phototherapeutic studies of monocationic methoxyphenylporphyrin derivative. Photodiagosis and Photodynamic Therapy.2004;1(4):335–344. [DOI] [PubMed] [Google Scholar]
- 44.Collins-Gold L, Feichtinger N, Wärnheim T. Are lipid emulsions the drug delivery solution? Modern Drug Discovery. 2000;3(3):44–46. [Google Scholar]
- 45.Muehlmann LA, Rodrigues MC, Longo JP, Garcia MP, Py-Daniel KR, Veloso AB, et al. Aluminium-phthalocyanine chloride nanoemulsions for anticancer photodynamic therapy: Development and in vitro activity against monolayers and spheroids of human mammary adenocarcinoma MCF-7 cells. Journal of nanobiotechnology. 2015. May 13;13(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muehlmann LA, Ma BC, Longo JP, Santos MD, Azevedo RB. Aluminum-phthalocyanine chloride associated to poly (methyl vinyl ether-co-maleic anhydride) nanoparticles as a new third-generation photosensitizer for anticancer photodynamic therapy. International journal of nanomedicine. 2014;9:1199 10.2147/IJN.S57420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pan X, Xie J, Li Z, Chen M, Wang M, Wang PN, Chen L, Mi L. Enhancement of the photokilling effect of aluminum phthalocyanine in photodynamic therapy by conjugating with nitrogen-doped TiO 2 nanoparticles. Colloids and Surfaces B: Biointerfaces. 2015. June 1;130:292–8. 10.1016/j.colsurfb.2015.04.028 [DOI] [PubMed] [Google Scholar]
- 48.Zabierowski SE, Herlyn M. Melanoma stem cells: the dark seed of melanoma. Journal of Clinical Oncology. 2008. June 10;26(17):2890–4. 10.1200/JCO.2007.15.5465 [DOI] [PubMed] [Google Scholar]
- 49.Boiko AD, Razorenova OV, van de Rijn M, Swetter SM, Johnson DL, Ly DP, et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature. 2010. July 1;466(7302):133–7. 10.1038/nature09161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Slattery ML, Herrick J, Lundgreen A, Fitzpatrick F, Curtin K, Wolff RK. Genetic variation in a metabolic signaling pathway and colon and rectal cancer risk: mTOR, PTEN, STK1, RPKAA1, PRKAG2, TSC1, TSC2, PI3K, and Akt1. Carcinogenesis. 2010. July 9:bgq142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Song CW, Lee H, Dings RP, Williams B, Powers J, Dos Santos T, et al. Metformin kills and radiosensitizes cancer cells and preferentially kills cancer stem cells. Scientific reports. 2012. April 12;2:362 10.1038/srep00362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.HIRSCH H, ILIOPOULOS D, TSICHLIS P, METFORMIN SK. Correction: Metformin Selectively Targets Cancer Stem Cells, and Acts Together with Chemotherapy to Block Tumor Growth and Prolong Remission. Cancer research. 2009;69(22):8832–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oleinick NL, Morris RL, Belichenko I. The role of apoptosis in response to photodynamic therapy: what, where, why, and how. Photochemical & Photobiological Sciences. 2002;1(1):1–21. [DOI] [PubMed] [Google Scholar]
- 54.Pluskalová M, Pešlová G, Grebe?ová D, Halada P, Hrkal Z. Photodynamic treatment (ALA-PDT) suppresses the expression of the oncogenic Bcr-Abl kinase and affects the cytoskeleton organization in K562 cells. Journal of Photochemistry and Photobiology B: Biology. 2006. June 1;83(3):205–12. [DOI] [PubMed] [Google Scholar]
- 55.Uzdensky A, Kolpakova E, Juzeniene A, Juzenas P, Moan J. The effect of sub-lethal ALA-PDT on the cytoskeleton and adhesion of cultured human cancer cells. Biochimica et Biophysica Acta (BBA)-General Subjects. 2005. February 11;1722(1):43–50. [DOI] [PubMed] [Google Scholar]
- 56.Acedo P, Stockert JC, Cañete M, Villanueva A. Two combined photosensitizers: a goal for more effective photodynamic therapy of cancer. Cell death & disease. 2014. March 1;5(3):e1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nenu I, Tudor D, Filip AG, Baldea I. Current position of TNF-? in melanomagenesis. Tumor Biol. 2015. September;36(9):6589–602. [DOI] [PubMed] [Google Scholar]
- 58.Lemke JV, Von Karstedt S, Zinngrebe J, Walczak H. Getting TRAIL back on track for cancer therapy. Cell Death & Differentiation. 2014. September 1;21(9):1350–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Griffith TS, Chin WA, Jackson GC, Lynch DH, Kubin MZ. Intracellular regulation of TRAIL-induced apoptosis in human melanoma cells. J Immunol. 1998. September 15;161(6):2833–40. [PubMed] [Google Scholar]
- 60.Wang S, El-Deiry WS. TRAIL and apoptosis induction by TNF-family death receptors. Oncogene. 2003. November 24;22(53):8628–33. 10.1038/sj.onc.1207232 [DOI] [PubMed] [Google Scholar]
- 61.Zhuang L, Lee CS, Scolyer RA, McCarthy SW, Zhang XD, Thompson JF, et al. Progression in melanoma is associated with decreased expression of death receptors for tumor necrosis factor-related apoptosis-inducing ligand. Human pathology. 2006. October 31;37(10):1286–94. 10.1016/j.humpath.2006.04.026 [DOI] [PubMed] [Google Scholar]
- 62.Luo JL, Maeda S, Hsu LC, Yagita H, Karin M. Inhibition of NF-?B in cancer cells converts inflammation-induced tumor growth mediated by TNF? to TRAIL-mediated tumor regression. Cancer cell. 2004. September 30;6(3):297–305. 10.1016/j.ccr.2004.08.012 [DOI] [PubMed] [Google Scholar]
- 63.Jakubowska M, Michalczyk-Wetula D, Pyka J, Susz A, Urbanska K, P?onka BK, et al. Nitrosylhemoglobin in photodynamically stressed human tumors growing in nude mice. Nitric Oxide. 2013. November 30;35:79–88. 10.1016/j.niox.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 64.Pustelny K, Bielanska J, Plonka PM, Rosen GM, Elas M. In vivo spin trapping of nitric oxide from animal tumors. Nitric Oxide. 2007. March 31;16(2):202–8. 10.1016/j.niox.2006.10.002 [DOI] [PubMed] [Google Scholar]
- 65.Reynaert NL, Ckless K, Korn SH, Vos N, Guala AS, Wouters EF, et al. Nitric oxide represses inhibitory? B kinase through S-nitrosylation. Proceedings of the National Academy of Sciences of the United States of America. 2004. June 15;101(24):8945–50. 10.1073/pnas.0400588101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cretney E, Shanker A, Yagita H, Smyth MJ, Sayers TJ. TNF-related apoptosis-inducing ligand as a therapeutic agent in autoimmunity and cancer. Immunology and cell biology. 2006. February 1;84(1):87–98. 10.1111/j.1440-1711.2005.01413.x [DOI] [PubMed] [Google Scholar]
- 67.Wood JM, Chavan B, Hafeez I, Schallreuter KU. Regulation of tyrosinase by tetrahydropteridines and H 2 O 2. Biochemical and biophysical research communications. 2004. December 24;325(4):1412–7. 10.1016/j.bbrc.2004.10.185 [DOI] [PubMed] [Google Scholar]
- 68.Schallreuter KU, Kothari S, Chavan B, Spencer JD. Regulation of melanogenesis-controversies and new concepts. Experimental dermatology. 2008. May 1;17(5):395–404. 10.1111/j.1600-0625.2007.00675.x [DOI] [PubMed] [Google Scholar]
- 69.Bro?yna AA, Jó?wicki W, Carlson JA, Slominski AT. Melanogenesis affects overall and disease-free survival in patients with stage III and IV melanoma. Human pathology. 2013. October 31;44(10):2071–4. 10.1016/j.humpath.2013.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bro?yna AA, Guo H, Yang SE, Cornelius L, Linette G, Murphy M, et al. TRPM1 (melastatin) expression is an independent predictor of overall survival in clinical AJCC stage I and II melanoma patients. Journal of Cutaneous Pathology. 2016. December 1. [DOI] [PubMed] [Google Scholar]
- 71.Bro?yna AA, Jó?wicki W, Roszkowski K, Filipiak J, Slominski AT. Melanin content in melanoma metastases affects the outcome of radiotherapy. Oncotarget. 2016. April 5;7(14):17844–53. 10.18632/oncotarget.7528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Slominski A, Zbytek B, Slominski R. Inhibitors of melanogenesis increase toxicity of cyclophosphamide and lymphocytes against melanoma cells. International journal of cancer. 2009. March 15;124(6):1470–7. 10.1002/ijc.24005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bro?yna AA, VanMiddlesworth L, Slominski AT. Inhibition of melanogenesis as a radiation sensitizer for melanoma therapy. International journal of cancer. 2008. September 15;123(6):1448–56. 10.1002/ijc.23664 [DOI] [PubMed] [Google Scholar]
- 74.Raghunath A, Sambarey A, Sharma N, Mahadevan U, Chandra N. A molecular systems approach to modelling human skin pigmentation: identifying underlying pathways and critical components. BMC research notes. 2015. April 29;8(1):170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Slominski A, Tobin DJ, Shibahara S, Wortsman J. Melanin pigmentation in mammalian skin and its hormonal regulation. Physiological reviews. 2004. October 1;84(4):1155–228. 10.1152/physrev.00044.2003 [DOI] [PubMed] [Google Scholar]
- 76.Spagnolo F, Queirolo P. Upcoming strategies for the treatment of metastatic melanoma. Archives of dermatological research. 2012. April 1;304(3):177–84. 10.1007/s00403-012-1223-7 [DOI] [PubMed] [Google Scholar]
- 77.Liu F, Fu Y, Meyskens FL. MiTF regulates cellular response to reactive oxygen species through transcriptional regulation of APE-1/Ref-1. Journal of Investigative Dermatology. 2009. February 28;129(2):422–31. 10.1038/jid.2008.255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kumar R, Harris-Hooker S, Kumar R, Sanford G. Co-culture of retinal and endothelial cells results in the modulation of genes critical to retinal neovascularization. Vascular cell. 2011. November 23;3(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yuan C, Wang P, Zhu L, Dissanayaka WL, Green DW, Tong EH, et al. Coculture of stem cells from apical papilla and human umbilical vein endothelial cell under hypoxia increases the formation of three-dimensional vessel-like structures in vitro. Tissue Engineering Part A. 2014. December 22;21(5–6):1163–72. 10.1089/ten.TEA.2014.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chen B, Pogue BW, Hoopes PJ, Hasan T. Vascular and cellular targeting for photodynamic therapy. Critical Reviews™ in Eukaryotic Gene Expression. 2006;16(4). [DOI] [PubMed] [Google Scholar]
- 81.Janjetovic K, Harhaji-Trajkovic L, Misirkic-Marjanovic M, Vucicevic L, Stevanovic D, Zogovic N, et al. In vitro and in vivo anti-melanoma action of metformin. European journal of pharmacology. 2011. October 15;668(3):373–82. 10.1016/j.ejphar.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 82.Niehr F, von Euw E, Attar N, Guo D, Matsunaga D, Sazegar H, et al. Combination therapy with vemurafenib (PLX4032/RG7204) and metformin in melanoma cell lines with distinct driver mutations. Journal of translational medicine. 2011. May 24;9(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tomic T, Botton T, Cerezo M, Robert G, Luciano F, Puissant A, et al. Metformin inhibits melanoma development through autophagy and apoptosis mechanisms. Cell death & disease. 2011. September 1;2(9):e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martin MJ, Hayward R, Viros A, Marais R. Metformin accelerates the growth of BRAFV600E-driven melanoma by upregulating VEGF-A. Cancer discovery. 2012. April 1;2(4):344–55. 10.1158/2159-8290.CD-11-0280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Medina VA, Rivera ES. Histamine receptors and cancer pharmacology. British journal of pharmacology. 2010. October 1;161(4):755–67. 10.1111/j.1476-5381.2010.00961.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Görlach A, Bonello S. The cross-talk between NF-?B and HIF-1: further evidence for a significant liaison. Biochemical Journal. 2008. June 15;412(3):e17–9. 10.1042/BJ20080920 [DOI] [PubMed] [Google Scholar]
- 87.Ochoa-Gonzalez F, Cervantes-Villagrana AR, Fernandez-Ruiz JC, Nava-Ramirez HS, Hernandez-Correa AC, Enciso-Moreno JA, et al. Correction: Metformin Induces Cell Cycle Arrest, Reduced Proliferation, Wound Healing Impairment In Vivo and Is Associated to Clinical Outcomes in Diabetic Foot Ulcer Patients. PloS one. 2016;11(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Moiseeva O, Simard X-D, Pollak M, Ferbeyre G. Metformin, aging and cancer. Aging (Albany NY). 2013. May; 5(5): 330–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wheaton WW, Weinberg SE, Hamanaka RB, Soberanes S, Sullivan LB, Anso E, Glasauer A, Dufour E, Mutlu GM, Budigner GS, Chandel NS. Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis. Elife. 2014. May 13;3:e02242 10.7554/eLife.02242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Slominski A, Kim TK, Bro?yna AA, Janjetovic Z, Brooks DL, Schwab LP, et al. The role of melanogenesis in regulation of melanoma behavior: melanogenesis leads to stimulation of HIF-1? expression and HIF-dependent attendant pathways. Arch Biochem Biophys. 2014. December 1;563:79–93. 10.1016/j.abb.2014.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dougherty TJ, Gomer CJ, Henderson BW, Jori G, Kessel D, Korbelik M, et al. Photodynamic therapy. Journal of the National Cancer Institute. 1998. June 17;90(12):889–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Popescu T, Nenu I, Aldea MD, Olteanu D, Gheban D, Tatomir C, et al. The effect of TSPP-mediated photodynamic therapy and Parecoxib in experimental tumours. Life sciences. 2014. November 11;117(2):75–83.. 10.1016/j.lfs.2014.09.022 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.