Abstract
This paper reviews and then discusses selected findings from a seventeen year study about the population prevalence of people who inject drugs (PWID) and of HIV prevalence and mortality among PWID in 96 large US metropolitan areas. Unlike most research, this study was conducted with the metropolitan area as the level of analysis. It found that metropolitan area measures of income inequality and of structural racism predicted all of these outcomes, and that rates of arrest for heroin and/or cocaine predicted HIV prevalence and mortality but did not predict changes in PWID population prevalence. Income inequality and measures of structural racism were associated with hard drug arrests or other properties of policing. These findings, whose limitations and implications for further research are discussed, suggest that efforts to respond to HIV and to drug injection should include supra-individual efforts to reduce both income inequality and racism. At a time when major social movements in many countries are trying to reduce inequality, racism and oppression (including reforming drug laws), these macro-social issues in public health should be both addressable and a priority in both research and action.
Keywords: Macro-social, People who inject drugs, HIV, Racism, Income inequality, Drug-related arrests, Drug law reform, Health
Research on drug use and on people who use drugs often seems isolated from research on major societal trends, forces and conflicts even though these have been shown to affect many other health outcomes and behaviors (Des Jarlais et al., 2012; Drucker, 2011; Pickett & Wilkinson, 2009; Williams, 2012). This separation exists in part because much of this research focuses on individuals who use drugs (or do not do so) and on individual-level predictors of which individuals use drugs, how they use drugs, or the consequences of their drug use, and ignores macro-level structures and processes. While the Risk Environment Model – one of the most commonly used models for understanding HIV-related outcomes among drug users – emphasizes micro-, meso- and macro-level contexts (Rhodes, 2002; Rhodes, Singer, Bourgois, Friedman, & Strathdee, 2005), research guided by this model has largely failed to examine the implications of major societal trends, forces, or conflicts, focusing instead on neighborhood-level, network level and event-specific exposures (Friedman, Bolyard, et al., 2008; Strathdee et al., 2010).
This commentary takes a different approach. It is a reflection on some of our findings during seventeen years of studying drug use and related issues in 96 large metropolitan areas in the United States. In this research, all variables were characteristics of these metropolitan areas, such as level of income inequality, government expenditures in the metropolitan area, the population prevalence of people who inject drugs (PWID) in the area, or the HIV prevalence rate among its PWID. Thus, our focus is not on predicting individual outcomes or conditions, but rather on how metropolitan area characteristics are associated with the extent to which drug injection or HIV or HIV-related mortality among PWID occur in the metropolitan area. As we shall describe, knowledge of such associations can help us understand if and how policies and other macrosocial processes are associated with HIV epidemics or widespread injection drug use.
We will not attempt a summary of all the topics the project wrote about. [See these selected papers that describe trends in PWID or in HIV among PWID (Chatterjee et al., 2011; Cooper et al., 2008; Pouget, Friedman, Cleland, Tempalski, & Cooper, 2012; Tempalski et al., 2009, 2013; West et al., 2016); in services for PWID (Tempalski, Cleland, Chatterjee, Pouget, & Friedman, 2010); and predictors of service presence or coverage (Friedman et al., 2007; Tempalski et al., 2003, 2007, 2008).] Instead, we briefly and selectively summarize some key findings from five of these papers that directly addressed the predictors of PWID population prevalence or HIV prevalence or incidence at the metropolitan level, and then discuss some implications of these findings.
Findings from five analyses
Our first analyses looked at the predictors of three variables that Holmberg (1996) had generated in a creative effort to estimate the size of three Key Populations (men who have sex with men, PWID, and high-risk heterosexuals) and HIV prevalence and incidence among these populations as of approximately 1992. We analyzed the predictors of PWID population prevalence (per 10,000 adult population), of HIV prevalence among PWID, and of HIV incidence among PWID. In one analysis, we showed that metropolitan areas in states with laws against over the counter purchase of syringes had higher HIV prevalence rates and incidence rates than those in states where syringes could be purchased (Friedman, Perlis, & Des Jarlais, 2001). In further analyses, we found that income inequality in a metropolitan area (as well as laws against syringe purchase) was positively associated with the population prevalence of PWID and with HIV prevalence rates among PWID (Friedman, Perlis, Lynch, & Des Jarlais, 2001). We also analyzed the macro-contextual predictors of HIV incidence rates among PWID in the 52 metropolitan areas with HIV prevalence <20% where over-the-counter syringe sales were legal. (We had to restrict the analysis in this way because HIV incidence in a locality is highly correlated with both prevalence and with the presence or absence of over-the-counter sales laws.) In this analysis, metropolitan area income inequality was positively associated with HIV incidence rates among PWID.
A second analysis examined the relationships of deterrence and law enforcement to drug-related harms in 89 of these 96 large metropolitan areas in the year 1998 (Friedman et al., 2006). (Seven metropolitan areas had too much missing data to analyze.) The year 1998 was perhaps the last year in which high HIV prevalence rates could be interpreted as an unambiguously “bad” thing because highly-active antiretroviral therapy (HAART) was introduced in 1996 but took several years to reach large numbers of PWID in most US metropolitan areas. (After HAART became widely used, HIV prevalence rates would tend to increase or stay steady as a “good thing” because the therapy would keep infected PWID alive.) In this paper, we found that average arrest rates per capita for possession or sale of cocaine or heroin in 1994–1997, the number of police employees per capita in 1994–1997, and corrections expenditures per capita in 1995 (after appropriate controls like region of the country and laws against over-the counter syringe sales) were not associated with the population prevalence of PWID in 1998. On the other hand, they all were positively and independently associated with HIV prevalence rates in 1998.
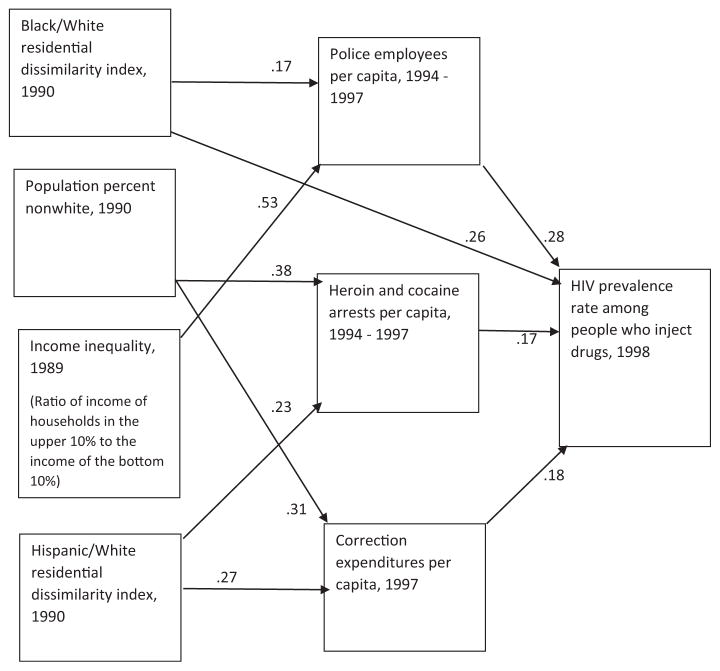
We revisited this analysis of HIV prevalence among PWID in 1998 in a later paper to see how other variables might help us interpret the results (Friedman, Tempalski, et al., 2008). Fig. 1 (copied from p. 263 of the paper) presents a path analysis of our findings. Here we can see that income inequality and measures of racial residential segregation are associated with police-related correlates of HIV prevalence rates.
Fig. 1.
Associations among selected variables for 96 large US metropolitan areas (adapted from Friedman, Tempalski, et al., 2008, p. 263). Paths with p ≥ 0.10 are not shown.
For this paper, we examined correlations among measures of income inequality, racial residential segregation, and the three measures of criminal justice systems for these metropolitan areas. The correlation matrix appears as Table 1. This matrix shows that the two measures of income inequality are both correlated with black-white residential dissimilarity (though not with Hispanic-white dissimilarity) and also with percent of the population that is nonwhite. Such correlations suggest the possible existence of a system of causation that leads to class inequality and structural racism being associated with each other.
Table 1.
Correlations among measures of income inequality, institutional racism, and criminal justice system variables in large US metropolitan areas.
| Income inequality measures
|
Institutional racism measures
|
Criminal justice system measures
|
Population percent nonwhite (as a contextual characteristic) | |||||
|---|---|---|---|---|---|---|---|---|
| Gini coefficient, 1989 | Ratio of incomes of upper 20% to those of lower 20%, 1989 | Black-white residential dissimilarity index, 1990 | Hispanic white residential dissimilarity index, 1990 | Arrests for cocaine or heroin per 10,000 adult population (average for 1994–1997) | Police employees per capita (average for 1994–1997) | Corrections expenditures per capita, 1997 | ||
| Gini coefficient | 1 | .939** | .284** | .161 | .254* | .463** | .132 | .420** |
| Ratio of upper 20% to lower 20% | 1 | .349** | .185 | .282** | .515** | .138 | .452** | |
| Black-white housing dissimilarity | 1 | .215* | .061 | .302** | −.069 | −.268 | ||
| Hispanic-white housing dissimilarity | 1 | .345** | .192 | .398** | .327** | |||
| Hard drug arrests | 1 | .240* | .352** | .423* | ||||
| Police employee per capita | 1 | .091 | .340** | |||||
| Corrections expenditures per capita | 1 | .417** | ||||||
| Population percent nonwhite | .209* | |||||||
p <.01.
p <.05.
N’s for the correlations range from 81 to 95 due to missing data.
A fourth paper revisited the issue of how drug-related arrests are related to the prevalence of PWID in a metropolitan area (Friedman et al., 2011). Specifically, in this paper, we focused on whether the arrest rate per capita for possession of heroin or cocaine during the period 1992–2002 was associated with change in the population prevalence rate of PWID. It was not.
The fifth analysis studied how metropolitan area characteristics were associated with changes in mortality rates (per 10,000 adult population) among PWID living with AIDS (Friedman, West, et al., 2013). Here, then, we are examining what metropolitan area characteristics were associated with successfully reducing mortality among PWID living with AIDS once HAART was discovered and introduced. What we found (among other things) was that rates of mortality reduction were worse in metropolitan areas with higher income inequality and/or a greater increase in rates of hard drug arrests per 10,000 adults.
Discussion
These results suggest that macro-social factors such as income inequality and racial/ethnic residential segregation are associated with higher rates of injection drug use, of HIV among PWID, and of mortality among PWID living with AIDS, and that drug arrests do not reduce injection drug use but do contribute to HIV and AIDS among PWID. There are of course limitations on what these associations mean. They are limited geographically, and notably do not include data from outside the USA. They by no means demonstrate that changes in institutional racism,1 income inequality or policing cause changes in the population density of PWID or in disease rates among PWID. (They do, however, strongly suggest that hard drug arrests have little impact on the rates of PWID in a metropolitan area.) Likewise, these analyses study rates for metropolitan areas rather than individuals, so even if these relationships do turn out to be causal, this might have relatively little to do with the fate of an individual at risk of becoming a PWID or who is already injecting.
However, while we should not ignore this lack of proof of causality, it remains true that racism, criminal justice systems and income inequality do seem to be associated with (later) rates both of HIV infection and of mortality among PWID. Some set of causal processes is taking place, and whatever those processes are, they seem to be generating these associations. Since income inequality, institutional racism, and criminal justice all are structures and processes at the macro-social level, if something else is causing these changes, it is also likely to be at the macro level. Research to resolve these issues of causation may be currently beyond the power of science to conduct, although qualitative research can suggest potential pathways. Research into possible pathways that might connect these macro-level processes with changes in HIV and mortality is also needed, and our team has been involved in research with individual, metropolitan and other levels of spatial analysis and in research to develop measures to study other pathways (Cooper et al., 2011, 2012a, 2012b, 2016; Friedman, Sandoval, et al., 2013; Friedman, Pouget, Sandoval, Jones, & Mateu-Gelabert, 2015; Friedman, Pouget, Sandoval, Jones, Nikolopoulos, et al., 2015; Nikolopoulos et al., 2015; Pouget, Sandoval, Nikolopoulos, & Friedman, 2015). Research on the time lag between a given macrosocial change and any effects it may have would also be useful.
The impact of income inequality, racialized social systems and systems of criminalization on health is not unexpected. Such findings are common in public health research (Chang, 2006; Charles & DeCicca, 2008; Des Jarlais et al., 2012; Drucker, 2011; Pickett & Wilkinson, 2009; Pinedo et al., 2015; Ramaswamy & Kelly, 2015; Rugh & Massey, 2010; Williams, 2012). We suspect that relationships of these or other similar macro-level variables will have similar associations in other countries with the population density of PWID, and with HIV rates and AIDS mortality among PWID, and urge that research be conducted on this issue internationally.
It will be useful for research to be conducted into (a) potential pathways that can transmit changes at the macro-level to the social contexts of small groups of people who might become injectors and/ or to people who use drugs and (b) whether and how changes in these pathway variables and social contexts in turn lead to changes in social networks and/or behaviors that can affect people’s health. We and others have written extensively on such pathways (1) in general (Friedman, Sandoval, et al., 2013; Pouget et al., 2016); (2) in the context of how “Big Events” sometimes lead to large-scale increases in drug injection or to HIV outbreaks (Friedman, Rossi, & Braine, 2009; Pouget et al., 2015; Strathdee et al., 2006); and (3) in terms of specific pathways that affect outcomes. These specific pathways have included research on (a) the extent of dignity attacks on some groups of people – and thus the stigmatizations that result from this (Friedman, Rossi, & Ralón, 2015; Harris & Rhodes, 2013; Hatzenbuehler, 2014; Hatzenbuehler & McLaughlin, 2014; Hatzen-buehler et al., 2014; Hatzenbuehler, Phelan, & Link, 2013; Hatzenbuehler, Schwab-Reese, Ranapurwala, Hertz, & Ramirez, in press), (b) how people use their time (Rossi et al., 2011), or (c) how to measure PWID’s altruistic and solidaristic actions and memberships and the relationships of these measures to risk behaviors (Friedman, Pouget, Sandoval, Jones, & Mateu-Gelabert, 2015; Friedman, Pouget, Sandoval, Jones, Nikolopoulos, et al., 2015). Such pathways are probably not deterministic, but involve interacting dialectics (Friedman & Rossi, 2011). An increase in income inequality (such as those seen in the USA and many other countries in recent decades) thus probably produces a tendency towards more HIV transmission among people who inject drugs, but interacting patterns of causation might prevent this increase from occurring. Much more research is needed on these issues.
For those who care about drug use and the fates of people who use drugs, the findings of the research reported here are nevertheless profound. They indicate that we have to pay attention to the “big issues” like income inequality, structural racism and other predictors both of flawed policies (like drug-related arrests or the failure to implement syringe exchange on a national scale in the United States or Russia) and of HIV incidence, prevalence and mortality as well as to the individual issues and care-related issues that take up most of our time in research and/or interventions. They also mean that when we think about “structural interventions” or the “risk environment,” we need to think about interventions or research beyond finding housing for drug users, arranging regular supplies of naloxone and syringes to rooms or parks where people gather to use drugs, and the like.2 Possible targets for intervention are drug laws and drug policies, which both feed and are fed by institutional and individual racism, a divided working class, income and wealth inequality, and a politics of scapegoating (Burris, Strathdee, & Vernick, 2003, Burris et al., 2004; Burris, Anderson, Craigg, Davis, & Case, 2010; Friedman et al., 2009; Friedman, Sandoval, et al., 2013; Friedman, 1998a, 1998b). The Black Lives Matter movement and the movement to reform criminal justice policies have directed attention to the harms posed by violent policing, repressive drug control policies, and criminal justice disparities, including drug-related policing and criminal sentencing (Alexander, 2010; Bassett, 2015). These have led to some Federal and state changes, including in sentencing policies, but the outcomes of these changes remain to be determined (Office of National Drug Control Policy, 2014). Many drug researchers have been leaders in analyses of the public health effects of policing and of incarceration (Cooper et al., 2012a; Drucker, 2011; Friedman et al., 2006; Rhodes & Simic, 2005).
We believe, however, that we need to “think even bigger” as well. For example, it may be that the best intervention to reduce drug use or HIV among PWID in a locality is to help workers to organize effective unions that can reduce income inequality and work with others to attack racism. Or perhaps to work with those who are systematically analyzing and attacking the structures that uphold the institutionalization of racism.
Current funding agencies might be unsympathetic to research designed to investigate whether these interventions work, and certainly it will be hard to approach any of this research using randomized controlled trials in which individuals are assigned to receive or not receive some treatment. Nonetheless, this paper, and this research project, indicate that for science and scholarship in this field to move ahead, we need to conduct research on such interventions and to test out these interventions at a macro scale. This is an opportune time for this work: for example, the current president of the American Public Health Association, Dr. Camara Jones, has prioritized tackling racism as a public health problem during her tenure; there is widespread attention to the health and other effects of mass imprisonment in the United States; and both before and after the Occupy movements, there has been increasing research attention to income and wealth inequalities and their effects (Alexander, 2010; Crutchfield & Weeks, 2015; Drucker, 2011; Friedman, Sandoval, et al., 2013; Pickett & Wilkinson, 2009; Pouget et al., 2016). “Health in all policies” approaches are gaining ground internationally. Even more important, since this is a time when major social movements in many countries are trying to reduce inequality, racism and repression, these macro-social issues in public health should be both addressable and a priority to be addressed in research and also in sociopolitical action.
Acknowledgments
We gratefully acknowledge support from National Institute on Drug Abuse Grants R01 DA13336 (Community Vulnerability and Responses to Drug-User-Related HIV/AIDS), R01 DA037568 (Metropolitan Trajectories of HIV Epidemics, Drug Use, and Responses in US Key Populations), R01 DA031597 (Developing measures to study how structural interventions may affect HIV risk), T32 DA 023356 (Program in Substance Use, HIV and Related Infections) and P30 DA11041 (Center for Drug Use and HIV Research). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funding agencies. We would like to acknowledge the support and advice of NIDA Project Officer Elizabeth Lambert for this research.
Conflict of interest: None of the authors have any conflicts of interest for this paper.
Footnotes
“Institutional racism” has been defined differently by different researchers. One definition, as given in Ramaswamy and Kelly (2015), is that is the “differential access to the goods, services, and opportunities of society by race.” In Friedman et al. (1998), we define it more broadly than this essentially distributionist approach. We argued that institutional racism also includes institutionalized power imbalance, which is a relational property, as well as dignity denial and attacks. We also suggested that institutional racism includes within itself relationships with core centers of society that provide it with support and also that, as in all power relationships, institutionalized racial power and domination bring forth discontent, resistance and sometimes open rebellion.
Changes in drug use or in related infectious diseases due to changes in medical insurance systems and related structures might also be studied. Such changes take time to diffuse into practice and then to have effects, if any, on the outcomes of interest at the population health level.
References
- Alexander M. The new Jim Crow: Mass incarceration in the age of colorblindness. New York: New Press; 2010. [Google Scholar]
- Bassett MT. #BlackLivesMatter – A challenge to the medical and public health communities. New England Journal of Medicine. 2015;372(12):1085–1087. doi: 10.1056/NEJMp1500529. http://dx.doi.org/10.1056/NEJMp1500529. [DOI] [PubMed] [Google Scholar]
- Burris SB, Anderson ED, Craigg A, Davis CS, Case P. Racial disparities in injection-related HIV: A case study of toxic law. 2010 82 Temple L Rev 1263. [Google Scholar]
- Burris SB, Blankenship KM, Donoghoe M, Sherman S, Vernick JS, Case P, et al. Addressing the risk environment for injection drug users: The mysterious case of the missing cop. The Millbank Quarterly. 2004;82(1):125–156. doi: 10.1111/j.0887-378X.2004.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris SB, Strathdee S, Vernick JS. Lethal injections: The law, science, and politics of syringe access for injection drug users. 2003 37 USF L Rev 813. [PubMed] [Google Scholar]
- Chang VW. Racial residential segregation and weight status among US adults. Social Science & Medicine. 2006;63(5):1289–1303. doi: 10.1016/j.socscimed.2006.03.049. [DOI] [PubMed] [Google Scholar]
- Charles KK, DeCicca P. Local labor market fluctuations and health: Is there a connection and for whom? Journal of Health Economics. 2008;27(6):1532–1550. doi: 10.1016/j.jhealeco.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Chatterjee S, Tempalski B, Pouget ER, Cooper HLF, Cleland CM, Friedman SR. Changes in the prevalence of injection drug use among adolescents and young adults in large U.S. metropolitan areas. AIDS & Behavior. 2011;157:1570–1578. doi: 10.1007/s10461-011-9992-0. http://dx.doi.org/10.1007/s10461-011-9992-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Brady JE, Friedman SR, Tempalski B, Gostnell K, Flom PL. Estimating the prevalence of injection drug use among Black and White adults in large U.S. metropolitan areas over time (1992–2002): Estimation methods and prevalence trends. Journal of Urban Health. 2008;85(6):826–857. doi: 10.1007/s11524-008-9304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HLF, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, Friedman SR. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes predicts drug injectors’ use of sterile syringes. American Journal of Public Health. 2011;86(6):929–945. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HLF, Des Jarlais DC, Tempalski B, Bossak BH, Ross Z, Friedman SR. Drug-related arrest rates and spatial access to syringe exchange programs in New York City health districts: Combined effects on the risk of injection-related infections among injectors. Health and Place. 2012a;18(2):218–228. doi: 10.1016/j.healthplace.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HLF, Des Jarlais DC, Tempalski B, Bossak BH, Ross Z, Friedman SR. Spatial access to sterile syringes and the odds of injecting with an unsterile syringe among injectors: A longitudinal multilevel study. The Journal of Urban Health. 2012b;89(4):678–696. doi: 10.1007/s11524-012-9673-y. http://dx.doi.org/10.1007/s11524-012-9673-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HLF, Linton S, Kelley ME, Ross Z, Wolfe ME, Chen YT, et al. Risk environments, race/ethnicity, and HIV status in a large sample of people who inject drugs in the United States. PLOS ONE. 2016;11(3):e0150410. doi: 10.1371/journal.pone.0150410. http://dx.doi.org/10.1371/journal.pone.0150410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crutchfield RD, Weeks GA. The effects of mass incarceration on communities of color. Issues in Science and Technology. 2015 Fall;32(1) [Google Scholar]
- Des Jarlais DC, Bramson H, Wong C, Gostnell K, Cepeda J, Arasteh K, et al. Racial/ethnic disparities in HIV infection among people who inject drugs: An international systematic review and meta-analysis. Addiction. 2012;107:2087–2095. doi: 10.1111/j.1360-0443.2012.04027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drucker E. A plague of prisons: Drugs, crime, and the epidemiology of mass incarceration. NY: The New Press; 2011. [Google Scholar]
- Friedman SR. The political economy of drug-user scapegoating – And the philosophy and politics of resistance. Drugs: Education, Prevention, and Policy. 1998a;5(1):15–32. [Google Scholar]
- Friedman SR. HIV-related politics in long-term perspective. AIDS Care. 1998b;10(Supplement 2):S93–S103. doi: 10.1080/09540129850124208. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Bolyard M, Khan M, Maslow C, Sandoval M, Mateu-Gelabert P, et al. Group sex events and HIV/STI risk in an urban network. Journal of Acquired Immune Deficiency Syndromes. 2008;49(4):440–446. doi: 10.1097/qai.0b013e3181893f31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Cooper HLF, Tempalski B, Keem M, Friedman R, Flom PL, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in U.S.A. metropolitan areas. AIDS. 2006;20(January 1):93–99. doi: 10.1097/01.aids.0000196176.65551.a3. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Jose B, Neaigus A, Goldstein M, Mota P, Curtis R, et al. Multiple racial/ethnic subordination and HIV among drug injectors. In: Singer M, editor. The political economy of AIDS. Amityville, New York: Baywood Press; 1998. pp. 105–127. [Google Scholar]
- Friedman SR, Perlis TE, Des Jarlais DC. Laws prohibiting over-the-counter syringe sales to injection drug users: Relations to population density, HIV prevalence and HIV incidence. American Journal of Public Health. 2001;91:791–793. doi: 10.2105/ajph.91.5.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Perlis T, Lynch J, Des Jarlais DC. Economic inequality, poverty, and laws against syringe access as predictors of metropolitan area rates of drug injection and HIV infection. 2000 Global Research Network Meeting on HIV Prevention in Drug-Using Populations. Third Annual Meeting Report; 2001. pp. 147–149. [Google Scholar]
- Friedman SR, Tempalski B, Brady JE, Friedman JJ, Cooper HLF, Flom PL, et al. Predictors of the degree of drug treatment coverage for injection drug users in 94 metropolitan areas in the United States of America. International Journal of Drug Policy. 2007;18:475–485. doi: 10.1016/j.drugpo.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Tempalski B, Cooper H, Lieb S, Brady J, Flom PL, et al. Metropolitan area characteristics, injection drug use and HIV among injectors. In: Thomas Y, Richardson D, Cheung I, editors. Geography and drug addiction. chapter 16 Springer; 2008. pp. 255–266. [Google Scholar]
- Friedman SR, Pouget ER, Chatterjee S, Cleland CM, Tempalski B, Brady JE, et al. Drug arrests and injection drug deterrence. American Journal of Public Health. 2011;101(June 6):1118–1125. doi: 10.2105/AJPH.2010.191759. http://dx.doi.org/10.2105/AJPH.2010.191759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Pouget ER, Sandoval M, Jones Y, Mateu-Gelabert P. Formal and informal organizational activities of people who inject drugs in New York City: Description and correlates. Journal of Addictive Disease. 2015 doi: 10.1080/10550887.2014.975612. http://dx.doi.org/10.1080/10550887.2014.975612. [DOI] [PMC free article] [PubMed]
- Friedman SR, Pouget ER, Sandoval M, Jones Y, Nikolopoulos GK, Mateu-Gelabert P. Measuring altruistic and solidaristic orientations towards others among people who inject drugs. Journal of Addictive Diseases. 2015 doi: 10.1080/10550887.2015.1059654. http://dx.doi.org/10.1080/10550887.2015.1059654. [DOI] [PMC free article] [PubMed]
- Friedman SR, Rossi D. Dialectical theory and the study of HIV/AIDS and other epidemics. Dialectical Anthropology. 2011;35:403–427. doi: 10.1007/s10624-011-9222-1. http://dx.doi.org/10.1007/s10624-011-9222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Rossi D, Braine N. Theorizing “Big Events” as a potential risk environment for drug use, drug-related harm and HIV epidemic outbreaks. International Journal on Drug Policy. 2009;20:283–291. doi: 10.1016/j.drugpo.2008.10.006. [DOI] [PubMed] [Google Scholar]
- Friedman S, Rossi D, Ralón G. Dignity denial and social conflicts. Rethinking Marxism: A Journal of Economics, Culture & Society. 2015;27(1):65–84. http://dx.doi.org/10.1080/08935696.2014.980675. [Google Scholar]
- Friedman SR, Sandoval M, Mateu-Gelabert P, Rossi D, Gwadz M, Dombrowski K, et al. Theory, measurement and hard times: Some issues for HIV/AIDS research. AIDS & Behavior. 2013;17(6):1915–1925. doi: 10.1007/s10461-013-0475-3. http://dx.doi.org/10.1007/s10461-013-0475-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, West BS, Pouget ER, Hall HI, Cantrell J, Tempalski B, et al. Metropolitan social environments and pre-HAART/HAART era changes in mortality rates (per 10,000 adult residents) among injection drug users living with AIDS. PLOS ONE. 2013;8(2):e57201. doi: 10.1371/journal.pone.0057201. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3578804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M, Rhodes T. Hepatitis C treatment access and up-take for people who inject drugs: A review mapping the role of social factors. Harm Reduction Journal. 2013;10(7) doi: 10.1186/1477-7517-10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML. Structural stigma and the health of lesbian, gay, and bisexual populations. Current Directions in Psychological Science. 2014;23:127–132. [Google Scholar]
- Hatzenbuehler ML, Bellatorre A, Lee Y, Finch B, Muennig P, Fiscella K. Structural stigma and all-cause mortality in sexual minority populations. Social Science & Medicine. 2014;103:33–41. doi: 10.1016/j.socscimed.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA. Structural stigma and hypothalamic-pituitary-adrenocortical axis reactivity in lesbian, gay, and bisexual young adults. Annals of Behavioral Medicine. 2014;47:39–47. doi: 10.1007/s12160-013-9556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Schwab-Reese M, Ranapurwala S, Hertz MF, Ramirez MR. Associations between antibullying policies and bullying in 25 states. JAMA Pediatrics. 2016 doi: 10.1001/jamapediatrics.2015.2411. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmberg SD. The estimated prevalence and incidence of HIV in 96 large US metropolitan areas. American Journal of Public Health. 1996;86(5):642–654. doi: 10.2105/ajph.86.5.642. http://dx.doi.org/10.2105/AJPH.86.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolopoulos GK, Sypsa V, Bonovas S, Paraskevis D, Malliori-Minerva M, Hatzakis A, et al. Big events in Greece and HIV infection among people who inject drugs. Substance Use and Misuse. 2015 doi: 10.3109/10826084.2015.978659. NIHMSID: 671922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. National drug control policy. 2014 Retrieved from http://www.whitehouse.gov/sites/default/files/ndcs_2014.pdf.
- Pickett K, Wilkinson RG. The spirit level: Why more equal societies almost always do better. London: Allen Lane; 2009. [Google Scholar]
- Pinedo M, Burgos JL, Zuniga ML, Perez R, Macera CA, Ojeda VD. Police victimization among persons who inject drugs along the U.S. – Mexico border. Journal of Studies on Alcohol and Drugs. 2015;76(September 5):758–763. doi: 10.15288/jsad.2015.76.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouget ER, Friedman SR, Cleland CM, Tempalski B, Cooper HLF. Estimates of the population prevalence of injection drug users among Hispanic residents of large U.S. metropolitan areas. Journal of Urban Health. 2012;89:527–564. doi: 10.1007/s11524-012-9670-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of Hurricane Sandy on people who inject drugs in New York city. Substance Use & Misuse. 2015 doi: 10.3109/10826084.2015.978675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouget ER, Sandoval M, Nikolopoulos GK, Mateu-Gelabert P, Rossi D, Smyrnov P, et al. Developing measures of pathways that may link macro social/ structural changes with HIV epidemiology. AIDS & Behavior. 2016 doi: 10.1007/s10461-016-1291-3. in press. First online: 21 January 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy M, Kelly PJ. Institutional racism as a critical social determinant of health. Public Health Nursing. 2015;32(July–August 4):285–286. doi: 10.1111/phn.12212. http://dx.doi.org/10.1111/phn.12212. [DOI] [PubMed] [Google Scholar]
- Rhodes T. The “risk environment”: A framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13:85–94. [Google Scholar]
- Rhodes T, Simic M. Transition and the HIV risk environment. British Medical Journal. 2005;331:220–223. doi: 10.1136/bmj.331.7510.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Rossi D, Zunino Singh D, Pawlowicz MP, Touzé G, Bolyard M, Mateu-Gelabert P, et al. Changes in time-use and drug use by young adults in poor neighbourhoods of Greater Buenos Aires, Argentina, after the political transitions of 2001–2002: Results of a survey. Harm Reduction Journal. 2011;8:2. doi: 10.1186/1477-7517-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rugh JS, Massey DS. Racial segregation and the American foreclosure crisis. American Sociological Review. 2010;75(5):629–651. doi: 10.1177/0003122410380868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: The past, present, and future. Lancet. 2010;376:268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Stachowiak JA, Todd CS, Al-Delaimy WK, Wiebel W, Hankins C, et al. Complex emergencies, HIV, and substance use: No “Big Easy” solution. Substance Use & Misuse. 2006;14:1637–1651. doi: 10.1080/10826080600848116. [DOI] [PubMed] [Google Scholar]
- Tempalski B, Cleland CM, Chatterjee S, Pouget ER, Friedman SR. Persistence of low drug treatment coverage for injection drug users in large US metropolitan areas. Substance Abuse Treatment, Prevention, and Policy. 2010;5(September):23. doi: 10.1186/1747-597X-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Cooper HL, Friedman SR, Des Jarlais DC, Brady J, Gostnell K. Correlates of syringe coverage for heroin injection in 35 large metropolitan areas in the US in which heroin is the dominant injected drug. International Journal of Drug Policy. 2008;19(Supplement 1):S47–S58. doi: 10.1016/j.drugpo.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Flom PL, Friedman SR, Des Jarlais DC, Friedman JJ, McKnight C, et al. Social and political factors predicting the presence of syringe exchange programs in 96 Metropolitan areas in the United States. American Journal of Public Health. 2007;97(3):437–447. doi: 10.2105/AJPH.2005.065961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Friedman SR, Des Jarlais DC, McKnight C, Keem M, Friedman R. What predicts which US metropolitan areas have syringe exchanges? International Journal of Drug Policy. 2003;14:417–424. [Google Scholar]
- Tempalski B, Lieb S, Cleland CM, Cooper H, Brady JE, Friedman SR. HIV prevalence rates among injection drug users in 96 large US metropolitan areas, 1992–2002. Journal of Urban Health. 2009;86:132–154. doi: 10.1007/s11524-008-9328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Pouget ER, Cleland CM, Brady JE, Cooper HLF, Hall HI, et al. Trends in the population prevalence of people who inject drugs in US metropolitan areas 1992–2007. PLOS ONE. 2013;8(6):e64789. doi: 10.1371/journal.pone.0064789. http://dx.doi.org/10.1371/journal.pone.0064789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West BS, Pouget ER, Tempalski B, Cooper HLF, Hall HI, Hu X, et al. Female and male differences in AIDS incidence among people who inject drugs in large US metro areas from 1993–2007. Annals of EPI. 2016 doi: 10.1016/j.annepidem.2015.01.006. http://dx.doi.org/10.1016/j.annepidem.2015.01.006. [DOI] [PMC free article] [PubMed]
- Williams DR. Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior. 2012;53(3):279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]