Osteoradionecrosis of the jaw is a complication of radiation therapy to the head and neck region. Many preventive strategies for osteoradionecrosis have been proposed that have yet to be validated by high‐level evidence. The use of hyperbaric oxygen has been suggested as a means for prevention and treatment, and this study aimed to establish a standard approach for using hyperbaric oxygen at one institution.
Keywords: Osteoradionecrosis, Prevention, Management, Hyperbaric oxygen
Abstract
Background.
Osteoradionecrosis of the jaw (ORN) is an infrequent yet potentially devastating complication of radiation therapy to the head and neck region. Treatment options include antimicrobial therapy, local sequestrectomy, resection, and the use of hyperbaric oxygen (HBO). Published data on ORN are difficult to compare because of the lack of a universally accepted classification and staging system, and the literature on the use of HBO to either prevent or successfully manage ORN is controversial and inconclusive. Therefore, we aimed to establish a standard approach for using HBO at our institution.
Materials and Methods.
A literature search was conducted of articles published in the English language between January 1980 and January 2016. Retrieved articles were evaluated by two independent reviewers. Isolated case reports, abstracts, case series, review articles, and cohort studies without a control group were excluded; summary data were extracted from the remaining studies. A panel of experts from Head and Neck Oncology and Oral Medicine from the Dana‐Farber Cancer Institute and Brigham and Women's Hospital reviewed the summary data and established multidisciplinary guidelines on the use of HBO for the prevention and management of ORN.
Results.
Seven studies were evaluated and reviewed by the multidisciplinary panel. There was no consistent evidence in support of HBO for either the prevention or management of ORN.
Conclusion.
Based on the available evidence and expert opinion, routine use of HBO for the prevention or management of ORN is not recommended and is rarely used at our institution.
Implications for Practice.
The Division of Head and Neck Oncology of Dana‐Farber/Brigham and Women's Cancer Center does not recommend the routine use of HBO for the prevention or management of ORN. Adjunctive HBO may be considered for use on a case‐by‐case basis in patients considered to be at exceptionally high risk who have failed conservative therapy and subsequent surgical resection.
Introduction
Osteoradionecrosis of the jaw (ORN) is an infrequent yet potentially devastating complication of head and neck radiation therapy (RT). ORN is defined as non‐healing exposed necrotic bone in a previously irradiated site that has been present for at least 3 months [1]. ORN may be associated with pain, infection, disability, and a diminished quality of life [2], [3]. ORN can develop spontaneously without a clear precipitating event, or it can be secondary to denture‐induced trauma or periodontal disease [1]. However, most cases develop following dental extractions [1], [4]. The median time reported from initiation of RT to ORN onset is 13 months (range: 2–122 months) [4]. For this reason, it is standard of care for patients to undergo dental evaluations prior to RT and to have infected teeth, teeth at high risk for infection, or teeth with a poor prognosis extracted at this time [5], [6], [7]. It is also recommended that the remaining dentition be well‐maintained subsequent to completing RT in order to avoid future extractions and thus reduce the risk of developing ORN [6].
To date, many preventive strategies for ORN have been proposed that have yet to be validated by high‐level evidence. These measures include, but are not limited to, pre‐RT dental evaluation and treatment, antibiotic treatment following post‐RT extractions, pentoxifylline and tocopherol prophylaxis, or hyperbaric oxygen (HBO) prophylaxis [8], [9]. Once diagnosed, treatment of ORN ranges from conservative surgical approaches, such as local surgical debridement and sequestrectomy, to more extensive surgical intervention, such as resection with or without osteomyocutaneous flaps. Surgical approaches may be complemented by adjunctive medical therapies such as antibiotics (topical and/or systemic), pentoxifylline and tocopherol, or HBO [8], [10], [11]. Currently, there are no consensus statements or universal guidelines for the prevention or management of ORN, leaving clinicians and patients faced with uncertainty as to best‐care decisions.
The use of HBO to treat ORN was initially suggested by Marx in 1983 [12] and was later proposed as a means to prevent ORN in 1985 [13]. The proposed mechanism focuses on the potential role of HBO to facilitate wound healing by increasing local tissue oxygen tension, resulting in enhanced collagen synthesis, angiogenesis, bone regeneration, and oral tissue epithelization to overcome the underlying pathogenesis of ORN that consists of hypoxia, hypocellularity, and hypovascularity due to the effects of RT [10], [14]. Many clinicians have subsequently utilized HBO prior to dental extractions in order to prevent ORN or as monotherapy or adjunctive therapy for treating existing ORN [15], [16], [17], [18], [19], [20]. A recent Cochrane systematic review concluded that there was “some evidence” to support the use of HBO to prevent the development of ORN following tooth extraction in an irradiated field, but further research is necessary to validate this approach [21]. Considering the lack of irrefutable supporting evidence, the high cost of treatment (average cost of 1 HBO session = $1,333; average cost of 30 sessions = $40,000; personal communication with billing departments of the Norman Knight Hyperbaric Medicine Center, Boston, MA, and St. Elizabeth's HBO Medical Center, Brighton, MA), and the limited number of HBO facilities, the use of HBO in this clinical setting remains controversial. The objective of this report is to provide pragmatic and evidence‐based clinical guidelines for the use of HBO at our institution to prevent and treat ORN based on the current available literature.
Materials and Methods
A review of English language publications reporting on ORN prevention and treatment utilizing HBO between January 1980 and January 2016 was performed using PubMed and Medline. Ninety citations were identified and evaluated for content and level of evidence by two independents reviewers (A.S. and G.J.H.). Inclusion criteria required both of the following: (a) articles published in the English language and reporting on ORN prevention or treatment using HBO and (b) randomized clinical trials and cohort studies (prospective or retrospective) with a control group. Exclusion criteria were as follows: (a) studies not published in the English language and (b) single case reports, case series, review articles, and cohort studies without a control group.
Each study was evaluated for the following parameters: study design, study endpoints, ORN stage, and ORN prevention and treatment regimens. Each study was also evaluated for overall strengths, limitations, and level of evidence according to the Centre for Evidence‐Based Medicine system [22]. An expert panel composed of medical oncologists, surgical oncologists, radiation oncologists, and oral medicine specialists met in September 2015 to review and discuss the summary data and establish multidisciplinary guidelines.
Results
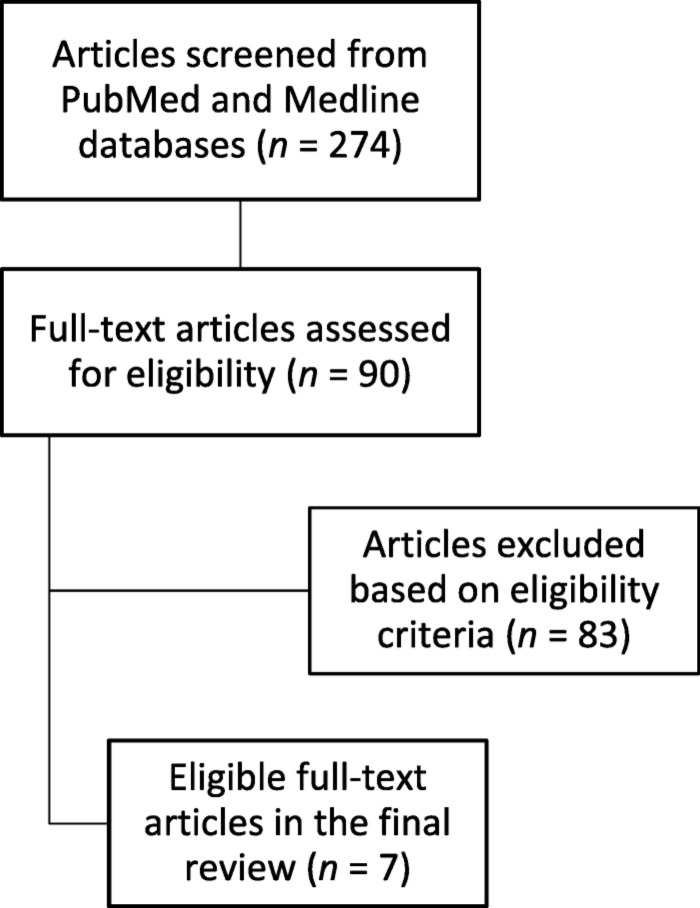
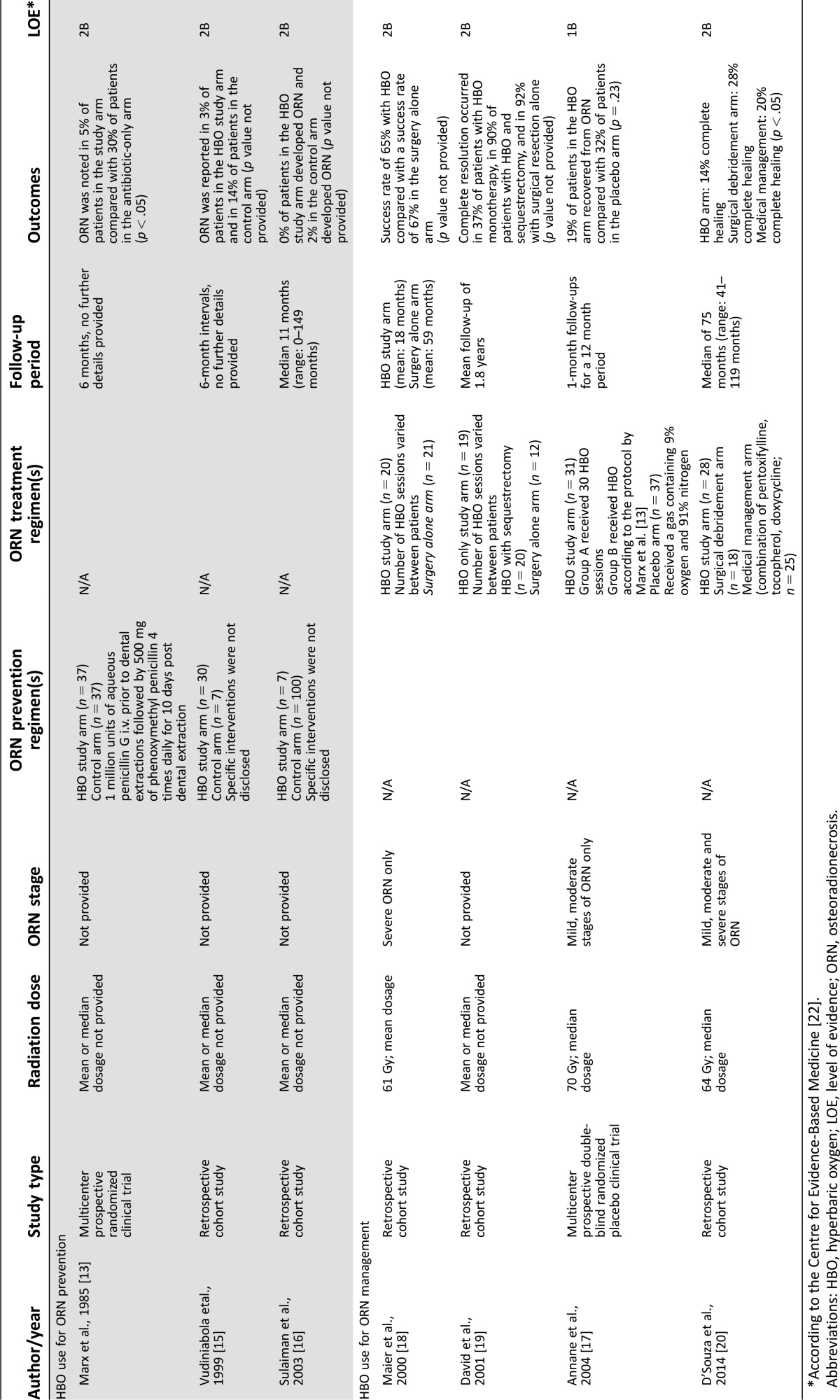
A total of seven studies met the inclusion criteria: three for prevention and four for management of ORN (Fig. 1, Table 1).
Figure 1.
Flow diagram of literature search and study selection.
Table 1. Studies that met inclusion criteria on the use of HBO for the prevention and management of ORN.
*According to the Centre for Evidence‐Based Medicine [22].
Abbreviations: HBO, hyperbaric oxygen; LOE, level of evidence; ORN, osteoradionecrosis.
The Use of HBO for the Prevention of ORN Prior to and Following Dental Extraction(s) in Previously Irradiated Patients
There were three studies in this category: one randomized clinical trial and two retrospective cohort studies [13], [15], [16]. In the 1985 study by Marx et al. [13] including 3 centers, 74 patients who had previously received RT and were scheduled for dental extraction(s) were randomized to receive either HBO only (without antibiotics) or preoperative and postoperative oral antibiotics only (control arm). Patients in the HBO arm received 20 sessions (dives) of HBO prior to dental extractions followed by an additional 10 HBO sessions following dental extractions, while those in the antibiotic arm received 1 million units of aqueous penicillin G intravenously prior to dental extractions followed by 500 mg of phenoxymethyl penicillin 4 times daily for 10 days post dental extractions. ORN was documented in 2 of 37 patients (5%) in the HBO arm compared with 11 of 37 patients (30%) in the antibiotic arm.
Vudiniabola et al. [15] in 1999 performed a retrospective cohort study and included 37 patients who were post RT, scheduled for dental extraction(s), and at risk for ORN. Thirty patients (30/37; 81%) received HBO according to the protocol by Marx et al. [13], while seven patients (19%) did not. Information regarding other interventions (e.g., antibiotic therapy) were not described. ORN was reported in one patient who received HBO and in one patient who did not receive HBO (3% versus 14%, respectively). Subsequently, Sulaiman et al. [16] in 2003 carried out a retrospective cohort study and included 107 patients who were post RT, scheduled for dental extraction(s), and at risk for ORN. Seven patients received pre‐extraction HBO treatment according to the protocol by Marx et al. [13], while 100 patients did not. Information regarding other interventions such as antibiotic therapy were not described. None of the 7 patients (0%) who received HBO developed ORN, and 2 of 100 patients (2%) who did not receive HBO developed ORN.
The Use of HBO for the Management of ORN
There were four studies in this category: one prospective randomized clinical trial and three retrospective cohort studies [17], [18], [19], [20]. Annane et al. [17] in 2004 performed a prospective double‐blind, randomized, placebo‐controlled, multicenter clinical trial that investigated the use of HBO monotherapy (without surgery) and adjunctive HBO (with surgery) for the management of ORN (only mild to moderate stages of ORN were assessed, and severe ORN characterized as mandibular fracture or bony resorption to the inferior border of the mandible was not included). The primary outcome measure was recovery from ORN at one‐year follow‐up. “Recovery” was defined as the absence of pain, bone exposure, pathologic fracture, cutaneous fistula, and by evidence of stabilization or regression on radiographic findings. The HBO arm consisted of two groups: group A received 30 HBO sessions as monotherapy without surgery, whereas group B received 20 HBO sessions as adjunctive therapy prior to surgical resection of necrotic bone followed by 10 sessions postoperatively. Patients in the placebo arm received a gas containing 9% oxygen and 91% nitrogen. Six of 31 patients (19%) in the HBO arm recovered from ORN compared with 12 of 37 patients (32%) in the placebo arm. As a result of this, the study was terminated early due to worse outcomes in the HBO arm.
Three single‐center retrospective cohort studies have investigated the use of HBO as monotherapy or as an adjunctive treatment modality for ORN [18], [19], [20]. In 2001, David et al. [19] reported complete resolution of ORN in 7 of 19 patients (37%) when HBO was used as monotherapy, whereas when HBO was used as adjunctive therapy, 18 of 20 patients (90%) treated with sequestrectomy and 11 of 12 patients (92%) treated with surgical resection showed complete resolution. Complete resolution criteria included the absence of bone exposure, closure of fistula if initially present, and a pain‐free status. No further details on ORN stages were provided.
In a retrospective cohort study of patients with severe ORN (defined as failed surgical intervention and/or evidence of severe osteolytic destruction on radiographic imaging), Maier et al. [18] reported a success rate of 13 of 20 patients (65%) with HBO monotherapy, which was comparable to the success rate of 14 of 21 patients (67%) treated with surgery only. The criteria for “success” wasn't provided. In 2014, D'Souza et al. [20] assessed the benefit of HBO monotherapy compared with surgical debridement and medical management using a combination of pentoxifylline, tocopherol, and doxycycline, based on the ORN staging system proposed by Notani et al. [23] (Table 2). A total of 71 patients were enrolled with grade 1 (n = 28), grade 2 (n = 16), and grade 3 (n = 27) ORN. Treatment response was categorized as complete healing (criteria not specified), stable ORN with control of patient symptoms, and progressive ORN. HBO resulted in complete healing of ORN in 4 of 28 patients (14%), stable disease in 2 of 28 patients (7%), and progressive disease in 22 of 28 patients (79%). Surgical debridement provided complete healing of ORN in 5 of 18 patients (28%), stable disease in 4 of 18 patients (22%), and progressive disease in 9 of 18 patients (50%). Medical (nonsurgical) management resulted in complete healing of ORN in 5 of 25 patients (20%), stable disease in 12 of 25 patients (48%), and progressive disease in 8 of 25 patients (32%).
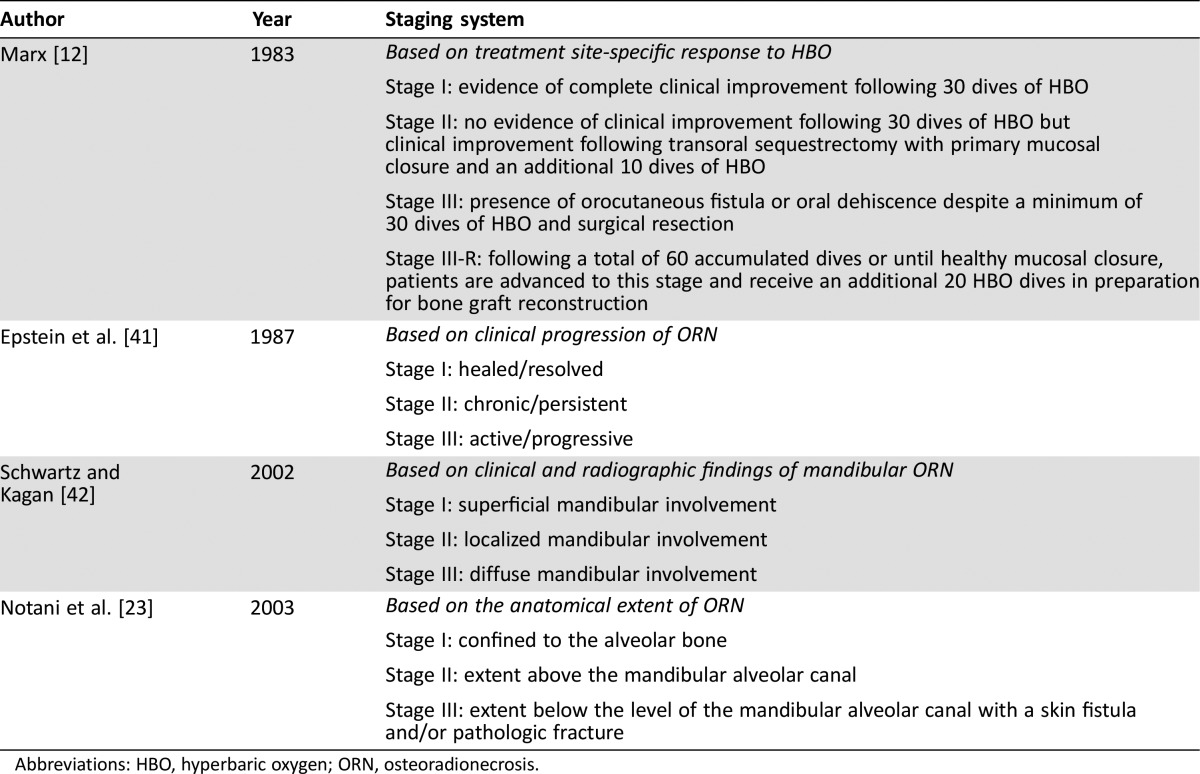
Table 2. Osteoradionecrosis of the jaw staging systems.
Abbreviations: HBO, hyperbaric oxygen; ORN, osteoradionecrosis.
Discussion
Since the first reported case of ORN in 1922 [24], various preventive and treatment approaches have been proposed. Because infection plays a significant role in the development of ORN, preventive measures have focused on a comprehensive dental evaluation and removal of all existing and potential sources of infection prior to RT. This includes restoration of all carious teeth, scaling and root planing to improve periodontal health, and extraction of teeth with questionable or hopeless prognosis that may require extraction in the future following RT. The goal is to restore the patient to optimal dental health. Careful planning of RT also plays a key role in minimizing the risk of ORN by limiting radiation dose to the mandible and maxilla, where possible. Post RT, patients are asked to maintain their dental health by seeing their dentist regularly and by using fluoride treatments [6]. In spite of these measures, some patients may still require extractions due to the very high risk of dental caries and tooth loss in this patient population [25], [26].
HBO generated much attention within the scientific community and amongst clinicians as a promising new preventive modality for ORN and as therapy for the management of existing ORN [27]. In 1983, Marx proposed the theory that hypoxia, hypocellularity, and hypovascularity were the basis for development of ORN [12]. Based on this concept, high oxygen tension provided by HBO putatively leads to enhanced collagen synthesis, angiogenesis, and the facilitation of epithelization for improved wound healing [10].
Since then, several published studies questioned the role of HBO in preventing and managing ORN. However, there is great heterogeneity among the studies, and the results are vastly conflicting from study to study [13], [15], [16], [17], [18], [19], [20], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]. The only prospective randomized clinical trial on ORN prevention prior to dental extraction(s) demonstrated improved outcomes with HBO prophylaxis compared with antibiotic prophylaxis [13]. In this trial, ORN developed in 5% of patients in the HBO‐only arm versus 30% in the antibiotic‐only arm. However, critical details such as the site and number of extracted teeth for each patient, median radiation dose given to study participants, and methodology for randomization or blinding were not provided. Two retrospective cohort studies investigating ORN prevention had large discrepancies in the numbers of patients between the HBO arms and control arms, which render the results difficult to interpret [15], [16]. If the numbers of patients are pooled from these two studies, a total of 3 of 130 patients (2%) in the HBO arm and 1 of 14 patients (7%) in the non‐HBO arm developed ORN. Moreover, a survey conducted on hyperbaric medicine physicians and radiation oncologists revealed that the majority were concerned by the lack of evidence to support the use of HBO for ORN prevention and expressed the need for more randomized clinical trials to support its clinical application [38].
Retrospective case series with small sample sizes suggest that combining HBO with surgical intervention may be beneficial in the resolution of ORN, but these studies lacked control arms, and the HBO protocols and definitions for ORN varied greatly amongst the studies [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37]. The highest level of evidence available to date on the management of ORN using HBO comes from the Annane et al. [17] 2004 multicenter trial. The trial was terminated early due to worse outcomes in the HBO arm (19% resolution with HBO versus 32% resolution with placebo). However, this trial did not investigate the role of HBO in severe forms of ORN. Three further retrospective studies demonstrated no benefit from using HBO as monotherapy to treat ORN and demonstrated superior outcomes when conventional surgical therapies were used alone [18], [19], [20]. Nevertheless, in 2012, the Royal College of Surgeons of England and the British Society for Disability and Oral Health published a clinical guideline on the prevention and management of ORN [6]. This guideline recommends the use of HBO prior to and following dental extractions in order to prevent ORN. In addition, it was suggested that HBO may potentially be considered for the management of advanced and severe cases of ORN [6].
The highest level of evidence available to date on the management of ORN using HBO comes from the Annane et al. 2004 multicenter trial. The trial was terminated early due to worse outcomes in the HBO arm (19% resolution with HBO versus 32% resolution with placebo).
From reviewing all included studies, we identified several important limitations. First, most studies were retrospective, single‐center studies with vast differences in follow‐up times and small numbers of subjects, often with uneven distribution of patients in the study arms. Second, critical details on the number of extractions performed, extraction techniques, degree of baseline bone damage, and details of specific treatments provided to patients in the non‐HBO arms were consistently lacking. Third, in patients who developed ORN, only a few studies reported on disease staging and, as such, it is difficult to be certain whether the severity of lesions was comparable between treatment arms (or between studies). Last, radiation dose to the oral cavity is typically associated with risk of ORN and deterioration of tooth/teeth structure leading to extractions [39]. However, most of the included studies were conducted in the era of older radiation techniques prior to the use of intensity‐modulated radiation therapy, which provides a greater degree of accuracy to deliver radiation to the site of interest and spares radiation exposure to healthy jaw bone [40]. In addition, studies did not provide the range of radiation doses delivered to the mandible and/or maxilla for each patient, which also may affect the risk of ORN after extractions.
Several staging systems for ORN exist in the literature (Table 2). However, to date, no single system has been universally accepted. Marx [12] proposed the first ORN staging system based solely on treatment response to HBO, while Epstein et al. [41] devised a staging system based on clinical progression of ORN. The systems by Schwartz and Kagan [42] and Notani et al. [23] are all based on a combination of clinical and radiographic findings for only mandibular ORN, but the definition of extent of disease is vague and remains unclear.
Aside from the relatively high cost burden (average cost of 30 HBO sessions = $40,000; personal communication with billing departments of the Norman Knight Hyperbaric Medicine Center, Boston, MA, and St. Elizabeth's HBO Medical Center, Brighton, MA) and limited patient access to local facilities for HBO, several safety concerns should be considered when discussing HBO intervention with patients [1]. Treatment complications of HBO include middle ear barotrauma, myopia, pneumothorax, arterial air embolism, and pulmonary oxygen toxicity [1]. Furthermore, HBO is contraindicated in patients with chronic obstructive pulmonary disease or chronic heart failure [1]. Other considerations include the risk of cancer progression or recurrence in this patient population [1], although this has been refuted by several review articles [43], [44], [45]. Furthermore, it has been postulated that HBO may in fact possess tumor‐inhibitory effects in certain cancer subtypes [43], [44], [45]. One possible mechanism to account for the tumor‐inhibitory effects of HBO is that HBO results in the production of excessive amounts of reactive oxygen species and, through excessive oxidative stress, causes tumor inhibition [45].
In summary, the current available evidence based on two retrospective cohort studies and one prospective randomized clinical trial indicates that there may be a slightly reduced risk of ORN with the use of prophylactic HBO [13], [15], [16]. These data must be interpreted with caution due to significant heterogeneity between studies. Three retrospective studies and a single prospective randomized clinical trial demonstrated improved outcomes when conventional surgical therapies were used alone compared with HBO in the management of ORN [17], [18], [19], [20]. One limitation of the current study is the risk of literature review bias as a result of the study design.
Based on our review of the literature, we propose the following recommendations for the use of HBO for ORN prevention and management. These guidelines are independent of the radiation dose received to the mandible or maxilla, or to specific extraction sockets.
One possible mechanism to account for the tumor‐inhibitory effects of HBO is that HBO results in the production of excessive amounts of reactive oxygen species and, through excessive oxidative stress, causes tumor inhibition.
Recommendations
HBO for the Prevention of ORN
The Division of Head and Neck Oncology‐ Dana‐Farber/Brigham and Women's Cancer Center (HNO‐DF/BWCC) does not recommend the routine use of HBO for the prevention of ORN prior to dental extractions in patients who have been treated with RT to the head and neck area.
Suggested Best Practice Guidelines for Patients Who Have Received Head and Neck RT, Are at Risk for ORN, and Require Dental Extractions.
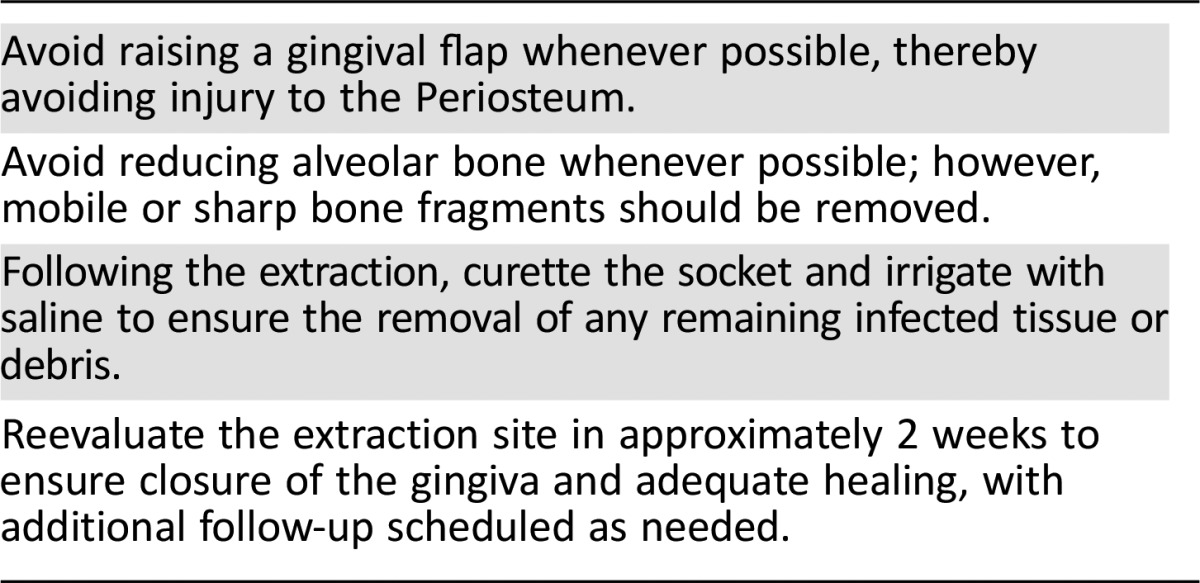
Because of the known risk of poor healing after RT and the risk for development of ORN after dental extraction following head and neck RT, initiation of appropriate systemic antibiotic treatment and topical chlorhexidine 0.12% rinses are recommended on the day of extraction(s) and continuation until documented healing has occurred on follow‐up evaluation. It is recommended that dental extractions be performed with as little trauma as possible according to the guidelines listed in Table 3. This recommendation is based on expert opinion (level 5 evidence) [22].
Table 3. Suggested guidelines for dental extractions using an atraumatic technique.
HBO for the Management of ORN
HNO‐DF/BWCC does not recommend HBO monotherapy or HBO as an adjunctive therapy for the routine management of ORN.
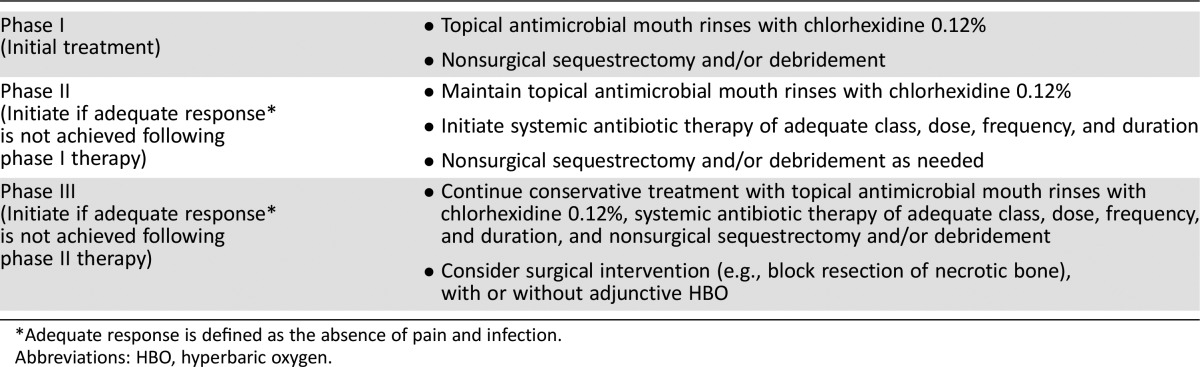
Suggested Best Practice Guidelines for Patients Who Have Received Head and Neck RT and Developed ORN.
A conservative approach to management (antibiotics and/or nonsurgical sequestrectomy) is advised (Table 4). Appropriate antibiotics, based on microbial culture, should be administered in cases of active ORN infection, signs and symptoms of soft tissue infection/cellulitis, or infected dentition. Patients with symptomatic ORN who do not respond adequately to conservative treatment or patients with extensive ORN may be considered for surgical intervention (i.e., site debridement and block resection with or without osteomyocutaneous flaps). Adequate response is defined as the absence of pain and infection. Adjunctive HBO in conjunction with surgery may be considered on a case‐by‐case basis, with considerations for high‐risk patients who have failed conservative therapy and subsequent surgical resection.
Table 4. Suggested treatment sequence for osteoradionecrosis of the jaw based on expert consensus.
*Adequate response is defined as the absence of pain and infection.
Abbreviations: HBO, hyperbaric oxygen.
Conclusion
ORN can be a devastating disease with a significant impact on quality of life. Due to limited data demonstrating efficacy as well as cost and patient access considerations, the use of HBO for ORN remains controversial. Based on a critical review of the literature, HNO‐DF/BWCC does not recommend the routine use of HBO for the prevention or management of ORN. Adjunctive HBO may be considered for use on a case‐by‐case basis in patients considered to be at exceptionally high risk who have failed conservative therapy and subsequent surgical resection. Current research continues to investigate various methods to best address prevention and management of this disease. As new data emerge, HNO‐DF/BWCC will continue to review and revise the aforementioned recommendations.
Contributor Information
Robert Haddad, Email: Robert_haddad@dfci.harvard.edu.
Hani Mawardi, Email: hmawardi@partners.org.
Author Contributions
Conception/Design: Ahmed Sultan, Glenn J. Hanna, Nathaniel S. Treister, Robert Haddad, Hani Mawardi
Collection and/or assembly of data: Ahmed Sultan, Glenn J. Hanna
Data analysis and interpretation: Ahmed Sultan, Glenn J. Hanna, Danielle N. Margalit, Nicole Chau, Laura A. Goguen, Francisco M. Marty, Guilherme Rabinowits, Jonathan D. Schoenfeld, Stephen T. Sonis, Tom Thomas, Roy B. Tishler, Nathaniel S. Treister, Alessandro Villa, Sook‐Bin Woo, Robert Haddad, Hani Mawardi
Manuscript writing: Ahmed Sultan, Nathaniel S. Treister, Alessandro Villa, Sook‐Bin Woo, Hani Mawardi
Final approval of manuscript: Ahmed Sultan, Glenn J. Hanna, Danielle N. Margalit, Nicole Chau, Laura A. Goguen, Francisco M. Marty, Guilherme Rabinowits, Jonathan D. Schoenfeld, Stephen T. Sonis, Tom Thomas, Roy B. Tishler, Nathaniel S. Treister, Alessandro Villa, Sook‐Bin Woo, Robert Haddad, Hani Mawardi
Disclosures
The authors indicated no financial relationships.
References
- 1. Nabil S and Samman N. Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: A systematic review. Int J Oral Maxillofac Surg 2011;40:229–243. [DOI] [PubMed] [Google Scholar]
- 2. Wong JK, Wood RE, McLean M. Conservative management of osteoradionecrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:16–21. [DOI] [PubMed] [Google Scholar]
- 3. Chrcanovic BR, Reher P, Sousa AA et al. Osteoradionecrosis of the jaws–a current overview–part 1: Physiopathology and risk and predisposing factors. Oral Maxillofac Surg 2010;14:3–16. [DOI] [PubMed] [Google Scholar]
- 4. Reuther T, Schuster T, Mende U et al. Osteoradionecrosis of the jaws as a side effect of radiotherapy of head and neck tumour patients–a report of a thirty year retrospective review. Int J Oral Maxillofac Surg 2003;32:289–295. [DOI] [PubMed] [Google Scholar]
- 5. Margalit DN, Losi SM, Tishler RB et al. Ensuring head and neck oncology patients receive recommended pretreatment dental evaluations. J Oncol Pract 2015;11:151–154. [DOI] [PubMed] [Google Scholar]
- 6. Kumar N, Brooke A, Burke M et al. The oral management of oncology patients requiring radiotherapy, chemotherapy and/or bone marrow transplantation. Clinical Guidelines. The royal college of surgeons of england/the british society for disability and oral health. 2012:1–58. Available at: https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/. Accessed January 3, 2017. [Google Scholar]
- 7. Pfister DG, Spencer S, Brizel DM et al. Head and neck cancers, version 2.2014. Clinical practice guidelines in oncology. J Natl Compr Canc Netw 2014;12:1454–1487. [DOI] [PubMed] [Google Scholar]
- 8. Peterson DE, Doerr W, Hovan A et al. Osteoradionecrosis in cancer patients: The evidence base for treatment‐dependent frequency, current management strategies, and future studies. Support Care Cancer 2010;18:1089–1098. [DOI] [PubMed] [Google Scholar]
- 9. Patel V, Gadiwalla Y, Sassoon I et al. Prophylactic use of pentoxifylline and tocopherol in patients who require dental extractions after radiotherapy for cancer of the head and neck. Br J Oral Maxillofac Surg 2016;54:547–550. [DOI] [PubMed] [Google Scholar]
- 10. Rice N, Polyzois I, Ekanayake K et al. The management of osteoradionecrosis of the jaws—A review. Surgeon 2015;13:101–109. [DOI] [PubMed] [Google Scholar]
- 11. Patel V, Gadiwalla Y, Sassoon I et al. Use of pentoxifylline and tocopherol in the management of osteoradionecrosis. Br J Oral Maxillofac Surg 2016;54:342–345. [DOI] [PubMed] [Google Scholar]
- 12. Marx RE. A new concept in the treatment of osteoradionecrosis. J Oral Maxillofac Surg 1983;41:351–357. [DOI] [PubMed] [Google Scholar]
- 13. Marx RE, Johnson RP, Kline SN. Prevention of osteoradionecrosis: A randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J Am Dent Assoc 1985;111:49–54. [DOI] [PubMed] [Google Scholar]
- 14. Grassmann JP, Schneppendahl J, Hakimi AR et al. Hyperbaric oxygen therapy improves angiogenesis and bone formation in critical sized diaphyseal defects. J Orthop Res 2015;33:513–520. [DOI] [PubMed] [Google Scholar]
- 15. Vudiniabola S, Pirone C, Williamson J et al. Hyperbaric oxygen in the prevention of osteoradionecrosis of the jaws. Aust Dent J 1999;44:243–247. [DOI] [PubMed] [Google Scholar]
- 16. Sulaiman F, Huryn JM, Zlotolow IM. Dental extractions in the irradiated head and neck patient: A retrospective analysis of memorial sloan‐kettering cancer center protocols, criteria, and end results. J Oral Maxillofac Surg 2003;61:1123–1131. [DOI] [PubMed] [Google Scholar]
- 17. Annane D, Depondt J, Aubert P et al. Hyperbaric oxygen therapy for radionecrosis of the jaw: A randomized, placebo‐controlled, double‐blind trial from the orn96 study group. J Clin Oncol 2004;22:4893–4900. [DOI] [PubMed] [Google Scholar]
- 18. Maier A, Gaggl A, Klemen H et al. Review of severe osteoradionecrosis treated by surgery alone or surgery with postoperative hyperbaric oxygenation. Br J Oral Maxillofac Surg 2000;38:173–176. [DOI] [PubMed] [Google Scholar]
- 19. David LA, Sandor GK, Evans AW et al. Hyperbaric oxygen therapy and mandibular osteoradionecrosis: A retrospective study and analysis of treatment outcomes. J Can Dent Assoc 2001;67:384. [PubMed] [Google Scholar]
- 20. D'Souza J, Lowe D, Rogers SN. Changing trends and the role of medical management on the outcome of patients treated for osteoradionecrosis of the mandible: Experience from a regional head and neck unit. Br J Oral Maxillofac Surg 2014;52:356–362. [DOI] [PubMed] [Google Scholar]
- 21. Bennett MH, Feldmeier J, Hampson N et al. Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst Rev: 2012;5:CD005005. [DOI] [PubMed] [Google Scholar]
- 22.Centre for Evidence‐Based Medicine hierarchy system . Available at http://www.cebm.net. Accessed March 23, 2016.
- 23. Notani K, Yamazaki Y, Kitada H et al. Management of mandibular osteoradionecrosis corresponding to the severity of osteoradionecrosis and the method of radiotherapy. Head Neck 2003;25:181–186. [DOI] [PubMed] [Google Scholar]
- 24. Lyons A and Ghazali N. Osteoradionecrosis of the jaws: Current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg 2008;46:653–660. [DOI] [PubMed] [Google Scholar]
- 25. Hong CH, Napenas JJ, Hodgson BD et al. A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer 2010;18:1007–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Deng J, Jackson L, Epstein JB et al. Dental demineralization and caries in patients with head and neck cancer. Oral Oncol 2015;51:824–831. [DOI] [PubMed] [Google Scholar]
- 27. Tahir AR, Westhuyzen J, Dass J et al. Hyperbaric oxygen therapy for chronic radiation‐induced tissue injuries: Australasia's largest study. Asia Pac J Clin Oncol 2015;11:68–77. [DOI] [PubMed] [Google Scholar]
- 28. van Merkesteyn JP, Bakker DJ, Borgmeijer‐Hoelen AM. Hyperbaric oxygen treatment of osteoradionecrosis of the mandible. Experience in 29 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:12–16. [DOI] [PubMed] [Google Scholar]
- 29. Mounsey RA, Brown DH, O'Dwyer TP et al. Role of hyperbaric oxygen therapy in the management of mandibular osteoradionecrosis. Laryngoscope 1993;103:605–608. [DOI] [PubMed] [Google Scholar]
- 30. Mansfield MJ, Sanders DW, Heimbach RD et al. Hyperbaric oxygen as an adjunct in the treatment of osteoradionecrosis of the mandible. J Oral Surg 1981;39:585–589. [PubMed] [Google Scholar]
- 31. Aitasalo K, Niinikoski J, Grenman R et al. A modified protocol for early treatment of osteomyelitis and osteoradionecrosis of the mandible. Head Neck 1998;20:411–417. [DOI] [PubMed] [Google Scholar]
- 32. Gupta P, Sahni T, Jadhav GK et al. A retrospective study of outcomes in subjects of head and neck cancer treated with hyperbaric oxygen therapy for radiation induced osteoradionecrosis of mandible at a tertiary care centre: An indian experience. Indian J Otolaryngol Head Neck Surg 2013;65:140–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Skeik N, Porten BR, Isaacson E et al. Hyperbaric oxygen treatment outcome for different indications from a single center. Ann Vasc Surg 2015;29:206–214. [DOI] [PubMed] [Google Scholar]
- 34. Narozny W, Sicko Z, Kot J et al. Hyperbaric oxygen therapy in the treatment of complications of irradiation in head and neck area. Undersea Hyperb Med 2005;32:103–110. [PubMed] [Google Scholar]
- 35. Bui QC, Lieber M, Withers HR et al. The efficacy of hyperbaric oxygen therapy in the treatment of radiation‐induced late side effects. Int J Radiat Oncol Biol Phys 2004;60:871–878. [DOI] [PubMed] [Google Scholar]
- 36. Curi MM, Dib LL, Kowalski LP. Management of refractory osteoradionecrosis of the jaws with surgery and adjunctive hyperbaric oxygen therapy. Int J Oral Maxillofac Surg 2000;29:430–434. [DOI] [PubMed] [Google Scholar]
- 37. Gal TJ, Yueh B, Futran ND. Influence of prior hyperbaric oxygen therapy in complications following microvascular reconstruction for advanced osteoradionecrosis. Arch Otolaryngol Head Neck Surg 2003;129:72–76. [DOI] [PubMed] [Google Scholar]
- 38. Heyboer M 3rd, Wojcik SM, Grant WD et al. Professional attitudes in regard to hyperbaric oxygen therapy for dental extractions in irradiated patients: A comparison of two specialties. Undersea Hyperb Med 2013;40:275–282. [PubMed] [Google Scholar]
- 39. Gomez DR, Estilo CL, Wolden SL et al. Correlation of osteoradionecrosis and dental events with dosimetric parameters in intensity‐modulated radiation therapy for head‐and‐neck cancer. Int J Radiat Oncol Biol Phys 2011;81:e207–213. [DOI] [PubMed] [Google Scholar]
- 40. Ben‐David MA, Diamante M, Radawski JD et al. Lack of osteoradionecrosis of the mandible after intensity‐modulated radiotherapy for head and neck cancer: Likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys 2007;68:396–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Epstein JB, Wong FL, Stevenson‐Moore P. Osteoradionecrosis: Clinical experience and a proposal for classification. J Oral Maxillofac Surg 1987;45:104–110. [DOI] [PubMed] [Google Scholar]
- 42. Schwartz HC and Kagan AR. Osteoradionecrosis of the mandible: Scientific basis for clinical staging. Am J Clin Oncol 2002;25:168–171. [DOI] [PubMed] [Google Scholar]
- 43. Moen I and Stuhr LE. Hyperbaric oxygen therapy and cancer–a review. Target Oncol 2012;7:233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Feldmeier J, Carl U, Hartmann K et al. Hyperbaric oxygen: Does it promote growth or recurrence of malignancy? Undersea Hyperb Med 2003;30:1–18. [PubMed] [Google Scholar]
- 45. Daruwalla J and Christophi C. Hyperbaric oxygen therapy for malignancy: A review. World J Surg 2006;30:2112–2131. [DOI] [PubMed] [Google Scholar]