Abstract
A high proportion of children have overweight and obesity in the United States and other countries. Accurate assessment of anthropometry is essential to understand health effects of child growth and adiposity. Gold standard methods of measuring adiposity, such as dual X-ray absorptiometry (DXA), may not be feasible in large field studies. Research staff can, however, complete anthropometric measurements, such as body circumferences and skinfold measurements, using inexpensive portable equipment. In this protocol we detail how to obtain manual anthropometric measurements from children, including standing and sitting height, weight, waist circumference, hip circumference, mid-upper arm circumference, triceps skinfold thickness, and subscapular skinfold thickness, and procedures to assess the quality of these measurements. To demonstrate accuracy of these measurements, among 1,110 school-aged children in the pre-birth cohort Project Viva we calculated Spearman correlation coefficients comparing manual anthropometric measurements with a gold standard measure of body fat, DXA fat mass1. To address reliability, we evaluate intra-rater technical error of measurement at a quality control session conducted on adult female volunteers.
Keywords: Medicine, Issue 120, Anthropometry, Body Composition, Adiposity, Body Mass Index (BMI), Measurement Reliability, Technical Error of Measurement (TEM)
Introduction
Overweight and obesity remain at epidemic levels, with approximately one-third of US children and two-thirds of adults having overweight or obesity, according to 2011 - 2012 estimates2. Overweight, obesity, and excess body fat confer greater risk of adverse cardiometabolic outcomes, including Type 2 diabetes and cardiovascular diseases, as well as other adverse physical and psychological health outcomes, including asthma and depression3,4,5,6.
Most studies that examine associations between obesity and later-life health outcomes assume accurate measurements of weight and length/height. Categories of weight status in adults and children include underweight (body mass index (BMI) < 18.0 kg/m2 for adults and < 5th age-sex-specific percentile for children), normal weight (BMI 18.0 to < 25.0 kg/m2 for adults and 5th to < 85th percentile for children), overweight (BMI 25.0 to < 30.0 kg/m2 for adults and 85th to < 95th percentile for children), and obesity (BMI ≥ 30 kg/m2 for adults and ≥ 95th percentile for children). Even minor measurement errors can influence these categorizations, especially in children for whom errors that appear small on an absolute scale can represent a large error relative to the child's size7. For example, in a prior study of children under 2 years of age, comparisons of length measured by the conventional clinical paper-and-pencil method with the recumbent length-board method indicated that paper-and-pencil method systematically overestimated length by an average of 1.3 (1.5) cm — an error that results in substantial misclassification7.
Using BMI to estimate adiposity offers many advantages for research, including the low equipment cost and minimal burden of height and weight measurement, as well as the opportunity to leverage self-report and clinical measures. However, even with accurate measurement of height and weight, variation in BMI does not necessarily reflect variation in adiposity, since BMI incorporates both lean and fat mass1. Thus, methods that directly measure adiposity are also important for understanding relationships with health outcomes.
Gold standard methods of adiposity and body composition measurement generally rely on technological methods, including air displacement plethysmography (ADP), hydrostatic weighing, magnetic resonance imaging (MRI), and computed tomography (CT), as well as dual X-ray absorptiometry (DXA)8,9,10. While these methods provide some of the most accurate measures of body composition, many of them are not practical in pediatric research studies, especially those that are field-based. For example, hydrostatic weighing requires that individuals be completely submerged in water. ADP equipment has, until quite recently, been available only to measure infants up to 8 kg or children and adults over the age of 6 years, but not toddlers or preschool-age children. CT scans emit a large amount of radiation compared with the other techniques, and the long acquisition time for MRI makes it impractical for many studies8. DXA emits about 1/500 the radiation dose of a CT scan, approximately the equivalent of one day of natural background radiation11, making it an attractive option for research studies involving children. All of these methods, however, are expensive to purchase and none are portable, making them infeasible for field-based studies with limited funding. Bioelectrical impedance analysis (BIA), which measures the impedance of a minute electrical signal sent through the body to estimate body composition, can be less expensive and more portable, but assumptions underlying the calculation of body fat are not applicable to small children10.
In contrast to these technology-based measures, manual anthropometric measures can be performed by a trained observer in most field settings and at a substantially lower equipment cost. Manual anthropometry includes measurements of height, weight, circumferences, and skinfold thicknesses8. Other advantages of manual anthropometry are that it involves no unnecessary radiation exposure, and skilled staff can obtain them efficiently. However, a common concern about manual anthropometric measurements is that they may be both inaccurate and imprecise12.
Obtaining accurate and precise measurements is possible with standardized procedures, adequate training, and sufficient attention to quality control (QC) procedures. The Project Viva team has developed a manual anthropometry training protocol that can yield high-quality, reproducible measures of stature, circumferences, and skinfold thickness. Over more than a decade, we have applied this training and QC protocol to mothers and children in Project Viva, a longitudinal, pre-birth cohort study13. Project Viva staff collected anthropometric measures on child during visits at birth (0 - 3 days), and with both the mother and child at the following time points: infancy (4.9 - 10.6 months), early childhood (2.8 - 6.3 years), mid-childhood (6.6 - 10.9 years), and early teen (11.5 - 16.5 years)13.
This paper describes the protocol we developed and refined for measurement of height, weight, skinfold thicknesses (triceps and subscapular skinfolds), and body circumferences (waist, hip, and mid-upper arm circumferences [MUAC]) in Project Viva. We also describe how we have assessed both manual anthropometric measurement precision by means of technical error of measurement (TEM) calculations and accuracy in comparison to gold standard DXA measurements.
Protocol
All the procedures are approved by the Harvard Pilgrim Health Care Institutional Review Board.
1. Training Procedures
- Have the trainees (research assistants) complete a multi-day, multiple hour training program to learn proper positioning, watch training videos, and receive in-person training from an experienced auxologist.
- Instruct the trainees to practice performing measurements on each other, while an auxologist or resident anthropometry expert evaluates each trainee's technique and makes appropriate adjustments.
- Organize a workshop with external volunteers, optimally of a variety of ages and body types, ideally a representative sample of the study population. Have the trainees measure each volunteer a minimum of two times per measurement.
After completing the training program, have the trainees spend approximately an additional 40 - 50 h practicing manual anthropometry techniques on one another and volunteers. During this time, observe the trainees, monitoring adherence to protocol and proper technique. Give each trainee the necessary amount of training based on innate skill level and previous experience.
2. Preparation of Subjects
Instruct participants to wear light clothing that allows easy access to the extremities and torso while maintaining modesty, optimally a standard outfit provided by the research staff.
3. Height
Measure height using a well-constructed stadiometer, which can be wall-mounted or portable. Either way, take measurements while ensuring that the stadiometer is set up against a wall on a hard, flat surface. NOTE: Among children under the age of 2 years, measure recumbent length instead of standing height. Recumbent length measurements require different procedures8, not detailed in this protocol.
Ask the participant, before stepping on the stadiometer, to remove any items that could impede measurements. For example, shoes, thick socks, hats, and hair accessories (e.g. hats, headbands, hair bands on the crown of head).
Guide the participant back onto the board until the participant's buttocks, shoulder blades, or back of head make contact with the board.
While facing the participant, instruct the participant to stand on the board with feet spread approximately 2 feet apart. Ask the participant to slowly inch his/her legs back together until the legs, mid-thighs, knees, or feet make contact.
Instruct the participant to stand as straight as possible, without slouching or leaning. Ensure that feet are flat on the bottom of the height board or floor, and arms hang down by the participant's sides. Confirm that weight is evenly distributed between the left and right sides of the body.
Visually verify that the mid-axillary line is perpendicular to the floor. Instruct the participant to move his/her feet away from the back of the stadiometer if necessary to achieve this position. NOTE: The mid-axillary line is an imaginary line in the coronal plane midway between the anterior axillary line and the posterior axillary line, extending from the center of the axilla down through the most superior part of the iliac crest (Figure 1).
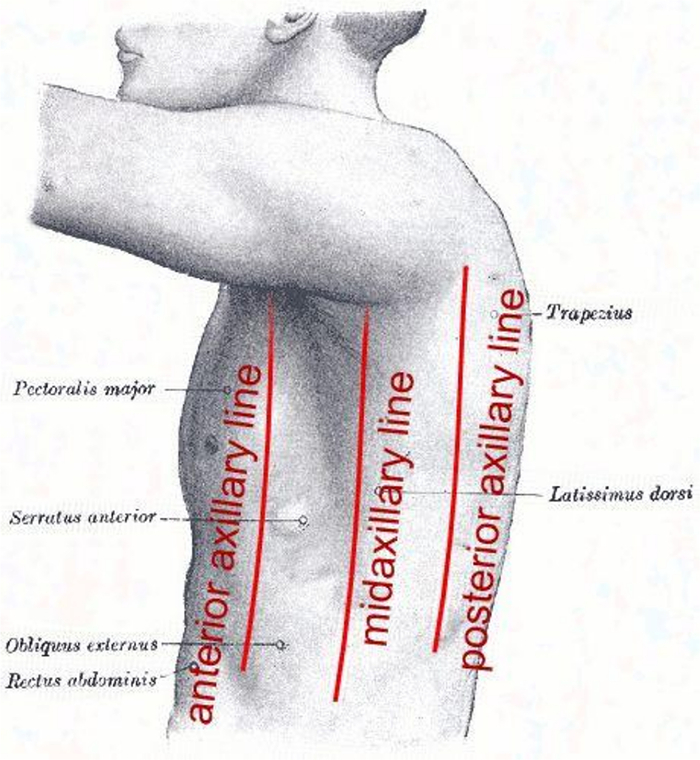 Figure 1:Location of the Mid-axillary Line. A coronal line halfway between the anterior and posterior axillary lines15. Please click here to view a larger version of this figure.
Figure 1:Location of the Mid-axillary Line. A coronal line halfway between the anterior and posterior axillary lines15. Please click here to view a larger version of this figure.
Ask the participant to stand up straight. Ensure that one or more of the following body parts makes contact with back of the stadiometer: feet, head, shoulders, or buttocks.
- Place the participant's head into the Frankfort Plane (Figure 2).
- Determine the Frankfort Plane by doing the following: Looking at the side of the participant's head, draw an imaginary line from the lowest margin of the eye orbit to the highest margin at the opening of the ear canal. Position the head so that the imaginary line is parallel to the floor and perpendicular to the stadiometer.
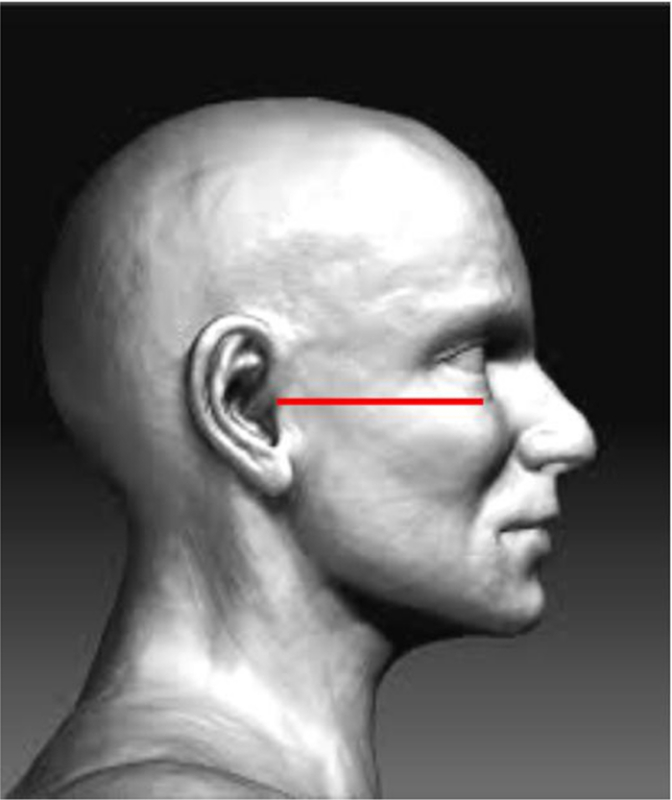 Figure 2:The Frankfort Plane. A horizontal plane that passes through the inferior margin of the orbit and the tragion (notch above the tragus of the ear)16. Please click here to view a larger version of this figure.
Figure 2:The Frankfort Plane. A horizontal plane that passes through the inferior margin of the orbit and the tragion (notch above the tragus of the ear)16. Please click here to view a larger version of this figure.
Remind the participant to stand straight and tall, and position the headpiece firmly on top of his/her head with sufficient pressure to compress the hair and make contact with the skull. With the headpiece at eye level, take the measurement to the nearest tenth of a centimeter.
4. Sitting Height
Place the stadiometer on top of a sturdy stool tall enough to allow the participant's legs to form a 90° angle with the ground. Alternatively, if the stadiometer is wall-mounted, place a stool of known height in front of the stadiometer.
Ask the participant to sit on the stadiometer or on top of the stool so that the buttocks are touching the back of the board.
Have the participant sit as erect as possible, with buttocks, shoulders and/or head touching the back of the board. Ensure that the mid-axillary line (as described in 3.6) is perpendicular to the stool and parallel to the stadiometer.
Guide the participant's knees directly in front of his/her body, and place his/her hands on the thighs.
Place the participant's head into the Frankfort Plane. Refer to 3.8.
Position the headpiece firmly on top of the participant's head with sufficient pressure to compress the hair and make contact with the skull.
While directly facing the measuring index with the headpiece at eye level, take measurement to the nearest tenth of a centimeter.
5. Weight
Instruct the participant to wear either light clothing or the standard clothing provided at the onset of the anthropometric measurements, to empty his/her bladder, and to remove his/her shoes before attempting the weight measurement.
Ask the participant, to stand on the scale. Record the measurement to the nearest tenth of a kilogram.
6. Waist Circumference
Instruct the participant to stand erect, still, and lateral to a chair, ideally in front of a mirror. Sit facing the mirror, with the participant's right or left hip bone at eye level. Instruct the participant to cross his/her arms in front while holding up his/her shirt.
Sitting to the side of the participant, locate the anterior part of the hip bone, which is usually the portion of the hip bone that is most easily identified through dense adipose tissue. Palpate upward along the hip bone to locate the iliac crest, the superior ridge of the hip bone. Continue to palpate the iliac crest until reaching the intersection between the uppermost point of the iliac crest and the mid-axillary line (refer to section 3.6 to locate mid-axillary line). Identify site with a self-adhesive sticker.
Repeat 6.2 on the other side of the participant's body.
While the participant stands perpendicular to the mirror, gently place the measuring tape around the waist on top of the two stickers with the zero side (or base) of the tape measure below. Using the mirror as a guide, adjust the tape so that it is on a level, horizontal plane across the front, back, and both sides.
Tighten the tape, without pulling the skin. As this is a fine balance, start with the tape measure pinching the skin slightly. Then slowly loosen the tape measure to form a smooth line along the skin, so that the skin is no longer constricted. Place the tape measure firmly on skin without cinching the participant's waist, so that there are neither gaps in the tape measure nor pinched skin.
At the end of the participant's natural exhalation, read the tape to the nearest tenth of a centimeter. NOTE: This measurement is most effectively performed in the presence of mirrors or two research assistants. One researcher, alone, cannot observe proper placement of the tape measure on all sides of the body. The mirrors and/or additional staff member compensate for obstructed areas, informing proper tape measure placement.
7. Hip Circumference
Instruct the participant to stand erect next to a chair, perpendicular to the mirror. Ask the participant to fold his/her arms in front of the body with feet pressed together.
Sit to the side of the participant and face the mirror, so that eyes are level with the participant's hips.
Place the measuring tape around the hips over lightweight, tight-fighting clothing. Anchor the tape measure at the maximum protuberance of the buttocks. Adjust the tape so that it is on a horizontal plane around the body. Hold the tape measure firmly. Similarly to the waist measurement, tighten the tape measure so that skin is pinched. Release the tape measure slowly until there is a smooth line around the tape measure.
Holding the tape measure firmly and flatly, read the measurement to the nearest tenth of a cm.
8. Mid-Upper Arm Circumference (MUAC)
Instruct the participant to lift his/her shirtsleeve to shoulder height, to ensure that measurement is conducted directly on skin. While the participant is standing, position his/her right arm so that it is flexed at a 90° angle at the elbow with the palm facing up and fingertips pointing straight ahead.
Stand behind the participant. Locate the posterior lateral shoulder bone that connects the participant's shoulder blade and clavicle bone (Figure 3). This bony structure, known as the acromion process, will serve as initial point zero on the tape measure.
 Figure 3:Anatomy of the Shoulder. Shoulder anatomy includes the acromion process, identified in red17. Please click here to view a larger version of this figure.
Figure 3:Anatomy of the Shoulder. Shoulder anatomy includes the acromion process, identified in red17. Please click here to view a larger version of this figure.
Extend the tape down the midline of the back of the arm, past the bony tip of the elbow, known as the olecranon. Using a tape measure the distance between the acromion process and the olecranon to the nearest tenth of a centimeter and place a self-adhesive sticker halfway between the olecranon and the acromion process over the posterior center of the humorous.
Hold the participant's arm slightly away from body, to ensure that muscles are relaxed.
Standing to the right and slightly behind the participant, wrap the MUAC Tape (small, flip tape) around the upper arm so that it covers the self-adhesive sticker. Ensure that the tape measure is perpendicular to the arm length.
Pull the tape so that there are no gaps in tape or areas of skin constriction. As with the hip and arm circumferences, this is a fine balance. Use greater tension and slowly release the tape until there are no further areas of pinched skin.
Read the measurement and record to the nearest tenth of a centimeter.
9. Triceps Skin Fold Thickness
Use the sticker placement at the posterior midpoint of the participant's arm (as determined by steps 8.1 - 8.3). Instruct the participant to stand upright, with shoulders relaxed and arms hanging loosely.
Standing behind the participant, identify a location approximately 2 cm above the sticker at the upper arm midpoint. Grasp a sizable fold of skin between the thumb and index finger about 1 - 2 cm into the skin. Roll the skin between fingers. NOTE: If the skinfold rolls easily between the fingers, it likely contains only skin and subcutaneous fat. If the skinfold does not roll easily or the grasp is particularly painful for the participant, it may contain muscle.
Shake the skin and/or roll fingers slowly to adjust the fold so that it contains only skin and subcutaneous fat, not muscle. Measure all subcutaneous fat above the muscle.
Hold the skinfold parallel to the arm. Place the skinfold caliper jaw perpendicular to the length of the fold and on either side of the marked midpoint.
While holding the skinfold, completely release grip on the caliper lever. The caliper dial will continue to decrease as the skin is compressed by the caliper jaws. Hold the skin between the caliper jaws for 4 full s, after which time the skin should be fully compressed. After 4 s, record the measurement to the nearest two tenths of a centimeter. NOTE: If it is the correct amount of skin and subcutaneous tissue, the measurement (as read on the caliper dial) will decrease less rapidly or will not decrease at all after 4 s. If the measurement value on the caliper dial continues to decrease rapidly, the skinfold did not contain enough subcutaneous fat. Should this be the case, wait two minutes for the compressed skin to return to normal. Retry the measurement by grasping a thicker fold.
10. Subscapular Skinfold Thickness
Instruct the participant to stand upright, with shoulders relaxed and arms hanging loosely.
Standing behind the participant, palpate the lowermost tip of the scapula. Locate the measurement site, two centimeters below the lower tip of the scapula, and place the calipers there.
Grasp a sizable fold of skin between the thumb and index finger on a diagonal approximately 2 cm above and to the left of the measurement site. The skin should roll easily between fingers if it contains only skin and subcutaneous fat. Adjust the skinfold, so that the measurement contains only skin and subcutaneous fat.
Place the caliper jaws perpendicular to the measurement site, so that the measurement is taken parallel to the medial, inferior bone of the scapula. While holding the skinfold, completely release grip on the caliper lever. Record measurement to the nearest two tenths of a cm after 4 s.
Ensure that the caliper dial remains consistent or decreases only minimally after 4 s. A rapidly decreasing measure on the caliper dial indicates that not enough subcutaneous fat has been obtained. If this is the case, wait 2 min for the compressed skin to return to normal. Retry the measurement by grasping a thicker fold.
11. Quality Control (QC) Procedures
Require all staff members, including experienced and new research staff members, to measure volunteers during the QC sessions. Obtain an equal number of volunteers and staff members to maximize efficiency. If the study staff consists of 1-3 people, request at least four volunteers to ensure that reliability is properly assessed.
Designate one individual to be the gold standard rater for the QC session, either a quality rater from the research staff or an outside expert. Ensure that he/she has a proven record of reliability (both intra-rater reliability and reliability when compared to either a skilled auxologist or a gold standard, such as DXA).
Have all study staff members conduct each manual anthropometric measure two or more times on each volunteer.
Calculate intra-rater and inter-rater reliability after the QC session, using technical error of measurement (TEM). NOTE: TEM is used to assess the difference between two measurements that is attributable to measurement error12. TEM is the square root of measurement error variance: TEM=
 , where d2 is either the difference between repeated measurements by each research assistant (intra-rater reliability) or the difference between the sum of the anthropometry expert's replicates minus the sum of a research assistant's replicates (inter-rater reliability)12.
, where d2 is either the difference between repeated measurements by each research assistant (intra-rater reliability) or the difference between the sum of the anthropometry expert's replicates minus the sum of a research assistant's replicates (inter-rater reliability)12.Identify staff members whose inter- or intra-rater TEM values fall outside of the predetermined TEM range of acceptability14. Provide more training for staff members whose anthropometric measures fall outside of the acceptable range, prior to allowing field data collection from study participants.
Representative Results
This analysis addresses precision of the manual anthropometric measurements using data generated from quality control (QC) procedures, and evaluates intra-rater measurement error by Technical Error of Measurement (TEM)12. TEM ranges of acceptability are based on calculations of repeated intra-rater anthropometric measures, where 95% of measurement discrepancy is due to factors other than rater imprecision12,14. A higher TEM indicates greater variability among measurements. Acceptable measurements, as analyzed in relation to TEM ranges of acceptability, fall below or within TEM ranges of acceptability. Large TEM values, that is TEM values above the range, indicate unreliability and indicate need for additional training. In this analysis, we present TEM values both in native units and in percent TEM, calculated by (average TEM/mean of the measure)*100, to compare across multiple anthropometric measures with different units.
Table 1 shows intra-rater TEM values from a QC session the Project Viva research team conducted on five healthy adult female volunteers. Six research assistants measured the volunteers repeatedly for a maximum of 60 times per anthropometric component. Each woman provided 55 measures, on average. TEM values fell within the range of acceptability for each measure, indicating low variability between measurements and thus accurate technique12,14. Research assistants most precisely measured height (% TEM = 0.2) followed by hip circumference (% TEM = 0.7). Research assistants were least precise at measuring subscapular skinfold thickness (% TEM = 7.4) and triceps skinfold thickness (% TEM = 6.9). Two members of the research staff achieved TEM values for waist circumference that were above the range of acceptability (TEM = 2.1; TEM = 3.0), signaling need for further training.
Data used to calculate TEM values are presented in Figure 4 and Figure 5. Figure 4 shows all height measurements obtained at the QC session described above. Each volunteer provided an average of 11 height measurements. Height measurements ranged from 151.4 cm to 166.4 cm amongst the five volunteers. Individual volunteer variation ranged from 1.3 cm (for the volunteer represented in red) to 4.1 cm (for the volunteer represented in orange) across all six raters. Most height measurements were within 1.0 cm of each other. The research assistant represented by circles was least accurate in measuring height, with several outlying measurements. This signals need for more training. Figure 5 shows all subscapular skinfold thickness measurements obtained at the QC session. Skinfold thickness measurements ranged from 8.6 cm to 33.8 cm amongst the five volunteers. Volunteer variation ranged from 1.6 cm (for the volunteer represented in blue) to 9.6 cm (for the volunteer represented in green). Research staff members experienced greater inter-rater reliability for subscapular skinfold thickness measurements than for height measurements.
Table 2 is adapted from a previous analysis by Boeke et al.1 on 1,110 Project Viva participants measured during mid-childhood (age 6.5 - 10.9 years). This table addresses accuracy of manual anthropometric measures of body fat, expressed as Spearman correlations with gold standard DXA measures. DXA fat was highly correlated with all manual anthropometric measures including weight (rs= 0.80), waist circumference (rs= 0.81), and sum of triceps + subscapular skinfold thickness (rs= 0.90) but was less strongly correlated with height (rs= 0.47).
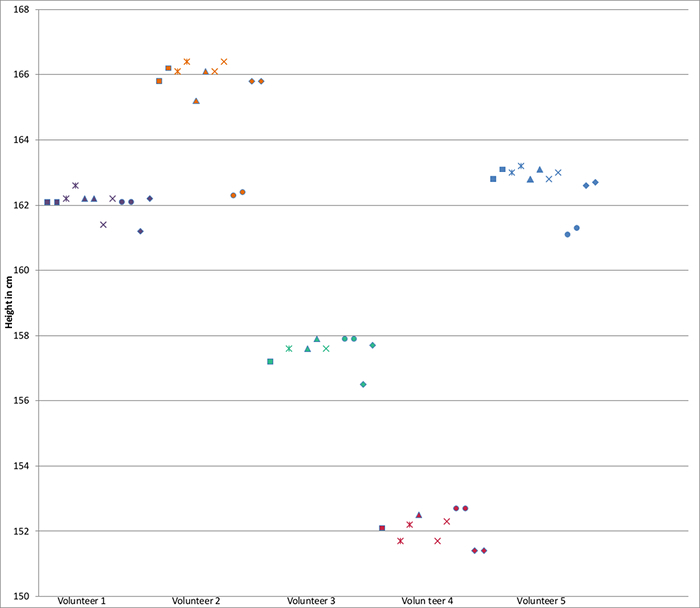 Figure 4:Scatterplot of Height Measurements. Height measurements (cm) taken by six research assistants during QC session on five adult female volunteers. Each volunteer is represented by a different color. Each research assistant is represented by a different shape. Please click here to view a larger version of this figure.
Figure 4:Scatterplot of Height Measurements. Height measurements (cm) taken by six research assistants during QC session on five adult female volunteers. Each volunteer is represented by a different color. Each research assistant is represented by a different shape. Please click here to view a larger version of this figure.
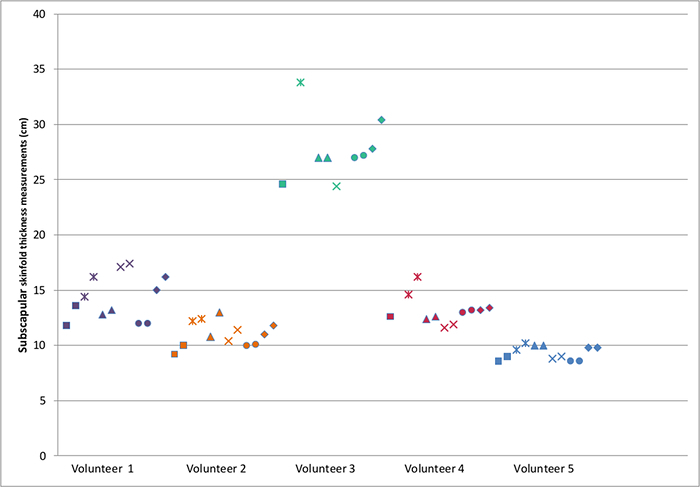 Figure 5:Scatterplot of Subscapular Skinfold Thickness Measurements. Subscapular skinfold thickness measurements (cm) taken by six research assistants during QC session on five adult female volunteers. Each volunteer is represented by a different color. Each research assistant is represented by a different shape. Please click here to view a larger version of this figure.
Figure 5:Scatterplot of Subscapular Skinfold Thickness Measurements. Subscapular skinfold thickness measurements (cm) taken by six research assistants during QC session on five adult female volunteers. Each volunteer is represented by a different color. Each research assistant is represented by a different shape. Please click here to view a larger version of this figure.
| No. of measures | Mean | TEM for each of the 6 research staff | Mean TEM | Acceptable | % TEM | ||||||
| TEM range[1] | |||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | ||||||
| Height (cm) | 55 | 160.4 | 0.2 | 0.3 | 0.4 | 0.4 | 0.1 | 0.5 | 0.3 | 0.1 - 1.3 | 0.2 |
| Waist circumference (cm) | 54 | 77.1 | 2.1 | 3.0 | 0.4 | 0.4 | 0.4 | 1.5 | 1.3 | 1.0 - 1.6 | 1.9 |
| Hip circumference (cm) | 54 | 99.2 | 0.5 | 1.1 | 0.8 | 0.2 | 0.6 | 0.6 | 0.6 | 1.2 - 1.4 | 0.7 |
| Mid upper arm circumference (cm) | 56 | 27.9 | 0.3 | 0.4 | 0.4 | 0.2 | 0.2 | 0.3 | 0.3 | 0.1 - 0.6 | 1.1 |
| Subscapular skinfold thickness (mm) | 56 | 14.5 | 0.8 | 0.9 | 0.7 | 0.4 | 0.1 | 0.9 | 0.6 | 0.1 - 7.4 | 7.4 |
| Triceps skinfold thickness (mm) | 55 | 16.7 | 0.7 | 0.7 | 1.2 | 0.9 | 0.1 | 1.9 | 0.9 | 0.1 - 3.7 | 6.9 |
Table 1: Intra-rater Reliability (within Measurer). Technical error of measurement (TEM) for each of the anthropometric measures, within each individual measurer. Data from six Project Viva research assistants performing repeated measures on five adult women. TEM calculated as ![]() , where d2 is the difference between repeated measurements by each research staff member (intra-rater reliability)12. A higher TEM indicates greater variability within the repeat measurements collected by each individual. %TEM calculated as (average TEM/mean of the measure)*100.
, where d2 is the difference between repeated measurements by each research staff member (intra-rater reliability)12. A higher TEM indicates greater variability within the repeat measurements collected by each individual. %TEM calculated as (average TEM/mean of the measure)*100.
| Height | Weight | Weight: | BMI | Waist circ | SS+TR | DXA fat | |
| (cm) | (kg) | Height | (kg/m2) | (cm) | (mm) | (kg) | |
| N | 1110 | 1110 | 1110 | 1110 | 1106 | 1103 | 875 |
| Mean (SD) | 128.8 (7.8) | 29.0 (7.9) | 0.22 (0.05) | 17.2 (3.1) | 60.0 (8.3) | 19.9 (9.8) | 7.5 (3.9) |
| Spearman correlation coefficient | |||||||
| Height | 1.00 | 0.80 | 0.66 | 0.38 | 0.56 | 0.33 | 0.47 |
| Weight | 1.00 | 0.98 | 0.84 | 0.87 | 0.69 | 0.80 | |
| Weight: Height | 1.00 | 0.93 | 0.90 | 0.75 | 0.84 | ||
| BMI | 1.00 | 0.86 | 0.79 | 0.83 | |||
| Waist circumference | 1.00 | 0.73 | 0.81 | ||||
| SS+TR | 1.00 | 0.90 | |||||
| DXA fat | 1.00 |
Table 2:Correlations between Each of Several Anthropometric Measures and with DXA Body Fat among 1110 Project Viva Children at 6.5 - 10.9 Years. Adapted from Boeke et al1. BMI = body mass index; SS = subscapular skinfold; TR = triceps skinfold; DXA = dual X-ray absorptiometry.
Discussion
Accurate body composition measures are critical for properly assessing childhood growth in research studies. Researchers widely accept DXA as a gold standard method, and many criticize manual anthropometric measures as being imprecise and inaccurate. However, this analysis of anthropometric techniques to estimate body fat suggests that well-trained research assistants who follow a standardized protocol can conduct manual anthropometric measures with excellent accuracy, yielding adiposity estimates that are highly correlated with DXA1. In addition to individual measures, combinations of manual anthropometric measures, such as the sum of skinfold thickness and weight to height ratio, are highly correlated with measures of DXA body fat. The purpose of this protocol is to standardize processes for eight commonly used anthropometric measures, to improve accuracy and allow comparison between research studies and pooling of results.
Critical Steps within the Protocol
Accurate assessment of body composition with manual anthropometry requires sufficient time for training and the conduct of quality control procedures to ensure precision and accuracy. Given the lead time required, research assistants optimally should be available for a minimum of 24 months. Equipment should be sturdy and regularly checked for calibration. To achieve high levels of reliability, raters must follow all steps of the anthropometric protocol precisely, as even minor alterations affect accuracy. Anecdotal evidence suggests that improper identification of anatomical measurement sites, hand placement, and tautness of measurement equipment cause the greatest variation between measures. With attention to detail, the enclosed protocol provides a clear method of collecting precise measurements yet it also shows that protocol alone is insufficient to achieve universally accurate results in the field.
Modifications and Troubleshooting
Low intra-rater TEM values achieved by research staff members who completed brief but rigorous training suggest a high level of repeatability. Trainers should provide additional training, however, to research assistants with TEM values outside of the range of acceptability for any measurement. To ensure that research assistants achieve precise measures in the field, all trainees undergo a certification process. Trainees must pass two field QC assessments in order to be fully certified as anthropometric raters. In this analysis, two raters achieved waist circumference measures outside of the TEM range of acceptability (as shown in Table 1), thus did not pass the certification process. These trainees received additional supervision and training prior to repeating their QC assessments and independent field data collection. While the outlined QC procedures provide overall confidence in a research assistant's ability, they do not produce immediate feedback at the time of the field measurement. One approach to overcoming this limitation is to have two observers each perform the measurement on the same subject. If numbers differ, the research assistants can take additional measurements; data analysts may use the mean of the two research assistants' measures.
Limitations of the Technique
Manual anthropometric assessment requires time and training, with ongoing monitoring of quality. However, other methods also may require substantial training or other start-up costs in addition to the costs of the equipment. For example, Massachusetts (where Project Viva is conducted) requires that anyone conducting a DXA scan be certified as a radiologic technologist or licensed physician. Project Viva research assistants studied for an average of 60 h for the 3-h long test, for which registration cost $425. Additionally, manual anthropometry cannot directly assess visceral fat, in contrast to some imaging techniques.
Significance of the Technique with Respect to Existing/Alternative Methods
All approaches to measuring body composition have advantages and disadvantages. Manual anthropometry can be used at all ages, confers no risks, and has minimal costs. However, the success of these methods depends on the availability of a stable staff able to spend weeks or months completing the training procedures and to follow protocols precisely.
Future Applications or Directions
With minor alterations, these techniques can also be adapted for other anthropometric measures, such as recumbent length, and chest and thigh skinfolds. In summary, this paper demonstrates that with training and QC, research assistants can perform manual anthropometric methods for assessment of adiposity in children with precision and accuracy. These methods are safe, low-cost, and require minimal, portable equipment and are therefore suitable for field studies among children.
Disclosures
The authors have nothing to disclose.
Acknowledgments
We greatly appreciate the contributions of our expert anthropometry trainers Irwin Shorr and Jorge Chavarro; the many volunteers who have allowed themselves to be pinched and measured in our anthropometry workshops, and the Project Viva mothers and children for their invaluable contributions. We'd like to extend a special thanks to members of the Project Viva research staff, past and present, especially to Nicole Witham and Marleny Ortega, for their contribution to the video accompanying this manuscript. Funding from the National Institutes of Health supported this work (R01 HD 034568, K24 HD069408).
References
- Boeke CE, Oken E, Kleinman KP, Rifas-Shiman SL, Taveras EM, Gillman MW. Correlations among adiposity measures in school-aged children. BMC Pediatrics. 2013;13(99) doi: 10.1186/1471-2431-13-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erermis S, Cetin N, Tamar M, Bukusoglu N, Akdeniz F, Goksen D. Is obesity a risk factor for psychopathology among adolescents. Pediatr Int. 2004;46(3):296–301. doi: 10.1111/j.1442-200x.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- Gunnell D, Frankel S, Nachahal K, Peters T, Smith G. Childhood obesity and adult cardiovascular mortality: A 57-y follow-up study based on the boyd orr cohort. AJCN. 1998;67(6):1111–1118. doi: 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- Vanhala M, Vanhala P, Kumpusalo E, Halonen P, Takala J. Relation between obesity from childhood to adulthood and the metabolic syndrome: Population based study. Brit Med J. 1998;317(7154):319. doi: 10.1136/bmj.317.7154.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papoutsakis C, Priftis KN, Drakouli M, Prifti S, Konstantaki E, Chondronikola M, Antonogeorgos G, Matziou V. Childhood overweight/obesity and asthma: is there a link? A systematic review of recent epidemiologic evidence. J Acad Nutr Diet. 2013;113(1):77–105. doi: 10.1016/j.jand.2012.08.025. [DOI] [PubMed] [Google Scholar]
- Rifas-Shiman SL, Rich-Edwards JW, Scanlon KS, Kleinman KP, Gillman MW. Misdiagnosis of overweight and underweight children younger than 2 years of age due to length measurement bias. MedGenMed. 2005;7(4):56. [PMC free article] [PubMed] [Google Scholar]
- Horan M, Gibney E, Molloy E, McAuliffe F. Methodologies to assess paediatric adiposity. Ir J Med Sci. 2014;814(1):1–16. doi: 10.1007/s11845-014-1124-1. [DOI] [PubMed] [Google Scholar]
- Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child. 2006;91(7):612–617. doi: 10.1136/adc.2005.085522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells JC, Fuller NJ, Dewit O, Fewtrell MS, Elia M, Cole TJ. Four-component model of body composition in children: Density and hydration of fat-free mass and comparison with simpler models. Am J Clin Nutr. 1999;69(5):904–912. doi: 10.1093/ajcn/69.5.904. [DOI] [PubMed] [Google Scholar]
- Damilakis J, Adams JE, Guglielmi G, Link TM. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur J Radiol. 2010;20(11):2707–2714. doi: 10.1007/s00330-010-1845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulijaszek SJ, Kerr DA. Anthropometric measurement error and the assessment of nutritional status. Brit J Nutr. 1999;82(3):165–177. doi: 10.1017/s0007114599001348. [DOI] [PubMed] [Google Scholar]
- Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, DeMeo D, Gillman MW. Cohort profile: Project Viva. Int J Epidemiol. 2015;44(1):37–48. doi: 10.1093/ije/dyu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulijaszek SJ, Lourie JA. Anthropometry: the Individual and the Population. Cambridge University Press; 1994. Intra- and inter-observer error in anthropometric measurement; pp. 30–55. [Google Scholar]
- Häggström M. Medical gallery of Mikael Häggström 2014. Wikiversity Journal of. Medicine. 2014;1(2) [Google Scholar]
- Meredith D. Male anatomy study face side. Flickr. 2007. Available from: http://www.flickr.com.
- DBCLS. Japan: BodyParts3D; 2013. Acromion of Scapula05. [Google Scholar]


