Abstract
Most clinicians approach the objective fitting of hearing aids with three goals in mind: audibility, comfort, and tolerance. When these three amplification goals have been met, the hearing aid user is more likely to adapt to and perceive benefit from hearing aid use. However, problems related to the loudness of sounds and reduced sound tolerance, which may or may not be reported by the aided user, can adversely impact adaptation to amplification and the individual's quality of life. Although there are several standardized questionnaires available to evaluate hearing aid benefit and satisfaction, there is no standardized questionnaire or interview tool for evaluating reduced sound tolerance and the related impact on hearing aid use. We describe a 36-item tool, the Sound Tolerance Questionnaire (STQ), consisting of six sections, including experience with hearing aids, sound sensitivity/intolerance, medical and noise exposure histories, coexisting tinnitus problems, and a final question to differentiate the primary and secondary problems related to sound intolerance, tinnitus, and hearing loss. In its current format as a research tool, the STQ was sensitive in pinpointing vague sound tolerance complaints not reported by the study participants in eligibility screening by Formby et al. A refined version of the STQ, the Sound Tolerance Interview and Questionnaire Instrument (STIQI), structured as a two-part tool, is presented in the appendix for prospective clinical use. The STIQI has potential utility to delineate factors contributing to loudness complaints and/or reduced sound tolerance in individuals considering hearing aid use, as well as those who have been unsuccessful hearing aid users secondary to loudness complaints or sound intolerance. The STIQI, when validated and refined, also may hold promise for predicting hearing aid benefit and/or assessing treatment-related change over time of hearing aid use or interventions designed to remediate problems of loudness and/or sound intolerance among hearing aid candidates or users.
Keywords: Hearing aid benefit, hyperacusis, sound tolerance
Learning Outcomes: As a result of this activity, the participant will be able to: (1) describe how reduced sound tolerance affects activity avoidance and (2) describe differences in sound tolerance.
Most clinicians approach the objective fitting of modern nonlinear hearing aids with three goals in mind: ensuring user audibility, comfort, and tolerance. When these three amplification goals have been met, the hearing aid user is more likely to adapt to hearing aid use and perceive benefit. The starting point for reaching these goals is the use of prescriptive methods to achieve hearing aid gain targets that provide audibility for soft sounds, comfort for moderately loud sounds, and tolerance for loud sounds.
Since 1935, several hearing aid fitting prescriptive methods have been developed to adjust hearing aid gain; these may be referred to as fitting rationales. For some methods, prescribed gain is determined using threshold data, with the underlying assumption that the hearing-impaired patient who is being fitted has average sound tolerance. These threshold-based methods are the most popular clinically. For other methods, gain is determined using some measure of loudness. A couple of methods use a combination of threshold and loudness data to prescribe gain.1 Current methods using audiometric thresholds to generate gain targets include the National Acoustic Laboratories NL2 procedure (NAL-NL2) and the Desired Sensation Level 5.0 procedure (DSL 5.0).2 3 Less commonly used methods using loudness data such as most comfortable levels (MCLs) or loudness discomfort levels (LDLs) include the Independent Hearing Aid Fitting Forum/Contour and DSL[i/o].4 5 Methods using both threshold and loudness data include DSL[i/o] and Memphis State University (MSU).6
In contrast to a fitting rationale, a fitting protocol is a specified procedure. In the context of fitting hearing aids, the protocol typically includes a process for determining final hearing aid gain settings. The ultimate goal of the fitting protocol is to achieve audibility, comfort, and tolerance and typically involves transitioning patients from their preferred gain settings to prescribed gain settings. It is not unusual for new hearing aid users to complain about the volume and/or sound quality of hearing aids during an initial fitting session. Clinicians are familiar with patient complaints related to amplified sounds being tinny, too loud, or too sharp. When hearing aid output is adjusted and verified with probe-microphone measurements to approximate the prescribed gain for a given input level, new users often complain about the sound quality or volume. In turn, they may indicate an unwillingness to use the hearing aids.7
The fitting protocol can be audiologist-driven or patient-driven. In an audiologist-driven protocol, hearing aid output is typically adjusted to maximize speech understanding. The patients who complain that output is too loud are often advised they will get used to it. In a patient-driven protocol, adjustments are made to output to accommodate patients' concerns for sound quality and loudness, with the underlying assumption that they may not adapt to hearing aid settings that are intended to maximize speech understanding. There is evidence to suggest that new hearing aid users may not adapt to prescribed gain provided in an audiologist-driven protocol, even after 8 weeks of hearing aid use, because of the perception that amplified sounds are too loud.8 Other evidence suggests that outcomes are essentially the same, as measured by objective and subjective measures of hearing aid benefit, over a period of 5 months, regardless of fitting protocol.9 10
Reduced sound tolerance can adversely impact adjustment to amplification. The new user who complains that the hearing aids are uncomfortably loud for several listening situations, even when maximum output has been set below the patient's LDLs, presents a challenge to the audiologist. Results from a survey by Kochkin indicate that overamplification of environmental sounds is the third most common reason for hearing aid dissatisfaction.11 Furthermore, 58% of those surveyed reported reduction in the pain caused by aided loud sounds as a highly desirable improvement in hearing aid technology. A discrepancy between objective measures of sound tolerance (e.g., measurement of LDLs for pure tones, narrowband noise, speech) and subjective real-world sound tolerance is a vexing problem for patients and their audiologists.12 13
Suprathreshold sensitivity to the loudness of sounds is dependent on the auditory dynamic range (DR). The DR is defined as the difference between one's threshold for sound and the loudest level at which sound can be tolerated. The DR for those with normal hearing is ∼95 dB.14 Individuals with sensorineural hearing loss have a reduced DR as a result of their elevated hearing thresholds; their LDLs are often similar for those with normal-hearing sensitivity, with slight increases as audiometric threshold exceeds 50- to 60-dB hearing loss (HL).15 16 17 18 These individuals are typical hearing-impaired listeners with sensorineural hearing losses who are diagnosed with loudness recruitment. Goldstein and Shulman have offered a classification scheme for sound tolerance problems of individuals with sensorineural hearing loss based on their DRs, owing primarily to their reduced DRs.19 They describe varying degrees of problems for DRs less than 60 dB, with severe problems designated for DRs < 40 dB. Some individuals with hearing loss also may have a reduced DR due to discomfort for sound levels that would not bother the typical listener. Estimates vary widely from ∼12 to 40% of individuals who have LDLs at least 5 dB below typical values.15 17 20 Those with LDL values ≤ 90-dB HL, with associated reports of distress for moderately intense sounds, may be diagnosed with some degree of loudness-based hyperacusis.19
Reduced sound tolerance can have a substantial impact on quality of life by limiting occupational and/or social activities. Individuals with reduced sound tolerance often report they avoid activities that may be uncomfortable, such as going to restaurants, movie theaters, and sporting events. One patient, for example, reported that she called in sick to work frequently because the noise level from an overhead paging system outside of her office caused her to feel physically ill.
The combination of reduced sound tolerance and hearing loss resulting in a narrow DR presents an obstacle to achieving successful hearing aid fitting for a large segment of the hearing-impaired population. For example, threshold-based fitting methods such as NAL-NL2 would provide the same prescriptive fit for two listeners with the same audiometric thresholds; however, their LDLs might differ by 40 dB or more! The one with lower LDLs almost certainly would reject amplification, whereas the other with average LDLs would likely be a satisfied user and successfully fitted patient.
Several questionnaires exist to establish prefitting expectations, such as the Client Oriented Scale of Improvement, the Expected Consequences of Hearing Aid Ownership, and the Hearing Aid Selection Profile.21 22 23 There also are questionnaires to evaluate postfitting outcomes regarding use, benefit, and satisfaction, including the Client Oriented Scale of Improvement, the Glasgow Profile of Hearing Aid Benefit, the Abbreviated Profile of Hearing Aid Benefit, and the Satisfaction with Amplification in Daily Life.24 25 26 The Abbreviated Profile of Hearing Aid Benefit has loudness-based questions that may be useful for anticipating or screening for loudness problems prior to fitting hearing aids; however, typically these questions are not routinely used in the clinical environment for this purpose. Other questionnaires also may have specific items related to tolerating loud sounds. Nonetheless, there currently is no standardized questionnaire for evaluating loudness complaints or problems related to reduced sound tolerance typically associated with abnormally low LDLs or the potential impact of these conditions on adaptation to hearing aid use.
Below we describe the item content and responses to an interview and questionnaire instrument, the Sound Tolerance Questionnaire (STQ), which may eventually lead to a standardized tool of the kind we highlight at the end of this report and share in Appendices B and C. We refer to this latter two-part interview and questionnaire tool as the Sound Tolerance Interview and Questionnaire Instrument (STIQI).
Appendix B: Sound Tolerance Interview The purpose of this interview is to find out if your patient has more trouble with sound than others. For each affirmative response, have your patient describe in more detail. Instruct the patient to consider moderate and moderately loud sounds, not loud sounds, when answering the questions. Examples of moderate sounds include an electric razor and a microwave buzzer sounding. Examples of moderately loud sounds include a speaker at a motivational talk or traffic noise on a moderately busy street. Examples of loud sounds include a door slamming, listening to a marching band, a barking dog and a lawn mower.
| 1. Have you ever used hearing aids? |
| If the answer is yes, ask questions 2–7. If the answer is no, skip to question 8. |
| 2. As of today, do you wear hearing aids? |
| 3. How long did you/have you used hearing aids? |
| 4. How often did you/do you use your hearing aids? |
| 5. How many hours per day did/do you wear your hearing aids? |
| 6. When you are not wearing your hearing aids, are moderate or moderately loud sound(s) ever uncomfortably loud? |
| 7. When you were/are wearing your hearing aids, are moderate or moderately loud sound(s) ever uncomfortably loud? |
| 8. How long have you been sensitive to sound? |
| 9. Was the onset of your sound sensitivity sudden or gradual? |
| 10. Do you associate the onset of your sound sensitivity with a particular event? |
| 11. If yes, describe the event. |
| 12. Is your sound tolerance problem in one ear or both ears? |
| 13. To your knowledge, have you ever taken any mycin or other ototoxic drugs (such as gentamycin or vancomycin)? |
| 14. Do you have any allergies to specific medications, foods, or other chemicals or products? |
| 15. Have you received any treatment for your sound tolerance problem, such as sound therapy, medication (e.g., antianxiety medication), cognitive behavioral therapy? |
| 16. Since you first noticed difficulty tolerating sound, has there been a change? If yes, is it better or worse? |
| 17. Do you experience any pain in your ears during exposure to moderate to moderately loud sounds? |
| If yes, does the pain occur during and/or after the exposure? |
| How long does the pain last? |
| 18. Do you have a history of occupational noise exposure (e.g., truck driving, factory work)? |
| 19. Do you have a history of military noise exposure? |
| 20. Do you have a history of recreational noise exposure (e.g., live concerts, bars/nightclubs, power tools, lawn mowers)? |
| 21. Do you use hearing protection devices, such as earplugs or earmuffs, during exposure to loud noise? |
| 22. Do you have tinnitus (ringing, roaring, buzzing)? If yes, is it constant or intermittent? |
| 23. Where is your tinnitus (e.g., right ear, left ear, both ears, head)? |
| 24. How long have you had tinnitus? |
| 25. Was the onset of your tinnitus sudden or gradual? |
| 26. What does your tinnitus sound like? |
| 27. Does noise have any effect on your tinnitus? If yes, does it make your tinnitus softer or louder? |
| 28. If noise does affect your tinnitus, how long does the effect last (e.g., minutes, hours, days)? |
| 29. Please rank the problems of reduced sound tolerance, hearing and tinnitus (1 = biggest problem, 2 = next biggest problem and 3 = last biggest problem). |
| Sound tolerance 1 2 3 |
| Hearing 1 2 3 |
| Tinnitus 1 2 3 |
| 30. Do you have any other information you would like to share about your tolerance problem? |
Appendix C: A Scorable Sound Tolerance Questionnaire Name: ______________________________The purpose of this questionnaire is to determine the extent of your sound sensitivity problem. Please circle the answers that come closest to your everyday experience.
|
How frequently do you experience tolerance problems in the following situations?
1 = never; 2 = seldom; 3 = about half the time; 4 = usually; 5 = always | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| When I am not wearing hearing aids | When I am wearing hearing aids | ||||||||||||
| 1. | Dining at restaurants, shopping (grocery, retail) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 2. | Sports events, concerts, movie theaters | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 3. | At work | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 4. | While in a car (driver or passenger) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 5. | Social events (family, friends) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 6. | When I'm around children | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 7. | When I leave my house | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 8. | While doing housework | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 9. | When water is running (e.g., shower, toilet flushing, water running from faucet) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 10. | While watching television | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
|
Which of the following activities do you avoid because of your sound tolerance problem? If you avoid certain activities for reasons
other
than your sound tolerance problem (e.g., you do not like going to movies), the appropriate answer is “rarely or never.”
1 = never; 2 = seldom; 3 = about half the time; 4 = usually; 5 = always | |||||||||||||
| When I am not wearing hearing aids | When I am wearing hearing aids | ||||||||||||
| 11. | Dining at restaurants, shopping (grocery, retail) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 12. | Sports events, concerts, movie theaters | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 13. | Going to work (e.g., you call out sick) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 14. | While in a car (driver or passenger) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 15. | Social events (family, friends) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 16. | Being around children | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 17. | Leaving the house | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 18. | Doing housework | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 19. | Running water (e.g., shower, flushing toilet, water running from faucet) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 20. | While watching television | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
|
When you are exposed to bothersome sounds, do you experience any of the following?
1 = never; 2 = seldom; 3 = about half the time; 4 = usually; 5 = always | |||||||||||||
| When I am not wearing aids | When I am wearing hearing aids | ||||||||||||
| 21. | Headaches | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 22. | Pain in your ears | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 23. | Anger, depression, and/or frustration | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| How often do any of the following occur? | |||||||||||||
| 24. | Sensitivity to light | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 25. | Sensitivity to touch | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 26. | I use earplugs or earmuffs) to avoid moderate or moderately loud* sounds | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
|
Please indicate how much the following sounds bother you, using the scale described below.
1 = a great deal; 2 = much; 3 = somewhat; 4 = a little; 5 = not much | |||||||||||||
| When I am not wearing aids | When I am wearing hearing aids | ||||||||||||
| 27. | Loud music | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 28. | Other people talking when I am trying to listen to someone | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 29. | The sound of paper rustling or rattling | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 30. | Repetitive sounds | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 31. | The sound of other people chewing and/or swallowing | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 32. | The sound of birds and/or crickets | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 33. | The sound of children talking and playing | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 34. | Mechanical noises (e.g., fans, air-conditioning units, computer fans) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 35. | Clattering noises (e.g., utensils on dishes) | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 36. | Lots of noise (e.g., people talking, dishes clattering, doors closing, footsteps) at the same time | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 37. | The sound of the toilet flushing | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 38. | The sound of water running from a faucet | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 39. | Please rate the severity of your sound tolerance problem as of today: 1 = none; 10 = as bad as you can imagine | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| 40. | Please rate how much your sound tolerance problem causes you distress: 1 = none; 10 = as much as you can imagine | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| 41. | Please rate the effect your sound tolerance problem has on your life: 1 = none; 10 = as much as you can imagine | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
*Examples of moderate sounds include an electric razor and a microwave buzzer sounding. Examples of moderately loud sounds include a speaker at a motivational talk or traffic noise on a moderately busy street. Do not answer this question for loud sounds, such as a door slamming, listening to a marching band, a barking dog or a lawn mower.
Sound Tolerance Questionnaire
In the context of conducting a randomized double-blind placebo-controlled trial of a sound therapy-based treatment for expanding the auditory DR, we devised a questionnaire instrument, the STQ, for the purpose of elucidating complaints related to problems of loudness and/or reduced sound tolerance experienced by sound-challenged or intolerant difficult-to-fit hearing aid candidates.27 In Goldstein and Shulman's classification schemes for hyperacusis/sound sensitivity, these individuals are labeled as mildly hyperacusic on the basis of their reduced LDLs, and severely hyperacusic based on their reduced DRs.19 The participants completed the questionnaires, without guidance or additional questioning by the research assistants.
The resulting STQ included a mix of open-ended interview-type questions, Likert 10-point scale rankings of the perceived problem or complaints, and yes-or-no questions selected based on clinical experience with patients who report reduced sound tolerance and/or related loudness complaints. The questions used in the STQ were phrased to avoid the use of technical terms and leading questions and were grouped on the basis of experience with hearing aids, sound sensitivity/intolerance, medical and noise exposure histories, coexisting tinnitus problems, and a final question ranking their primary problem in terms of sound intolerance, tinnitus, and/or hearing loss. The aim of the STQ was to characterize the often poorly ascribed loudness and sound tolerance complaints for this population of potential hearing aid users as part of the process of evaluating and assessing the sound therapy intervention under study. The study participants were recruited on the basis of their self-reported unaided or aided sound intolerance but were not recruited based on a diagnosis of hyperacusis. Although hyperacusis has no consensus definition,19 for the purposes of this report it is defined as an increased sensitivity to everyday sounds that are not troublesome for the typical listener. Jastreboff has suggested that loudness-based hyperacusis arises as a consequence of an abnormally strong reaction to sound occurring within the auditory pathways.28 This presumably is not the primary problem for the majority of hearing aid candidates seen clinically, who typically reject amplification on the basis of some complaint of excessive loudness other than primary loudness-based hyperacusis.
Results from 44 completed questionnaires were analyzed and are reported here. A total of 31 study participants who completed the STQ also completed the sound therapy trial.27 An additional group of 13 participants completed the STQ, but either did not elect to participate in the trial or withdrew at some point from the study. The original intent of the trial was to recruit people who were not wearing their hearing aids because of sound intolerance; however, due to difficulty recruiting this target group, the inclusion criteria were modified to include people who had not pursued hearing aids because they anticipated amplification might be too loud for them. The majority of the respondents did not have experience with hearing aids.
The average age of the respondents was 66 (standard deviation = 10.41; range 37 to 84) years. There were 24 men and 20 women. Pure tone thresholds were measured at 250, 500, 1,000, 2,000, 3,000, 4,000, 6,000, and 8,000 Hz. LDLs were measured at 500, 1,000, 2,000, and 4,000 Hz. The participants' average pure tone thresholds and LDLs are shown in Fig. 1. Hearing sensitivity, on average, was characterized by a mild sloping to moderately severe sensorineural hearing loss. LDLs were generally reduced across the participants; on average, LDLs were in the range of 85- to 90-dB HL and DRs at higher frequencies were less than 40 dB pretreatment.
Figure 1.
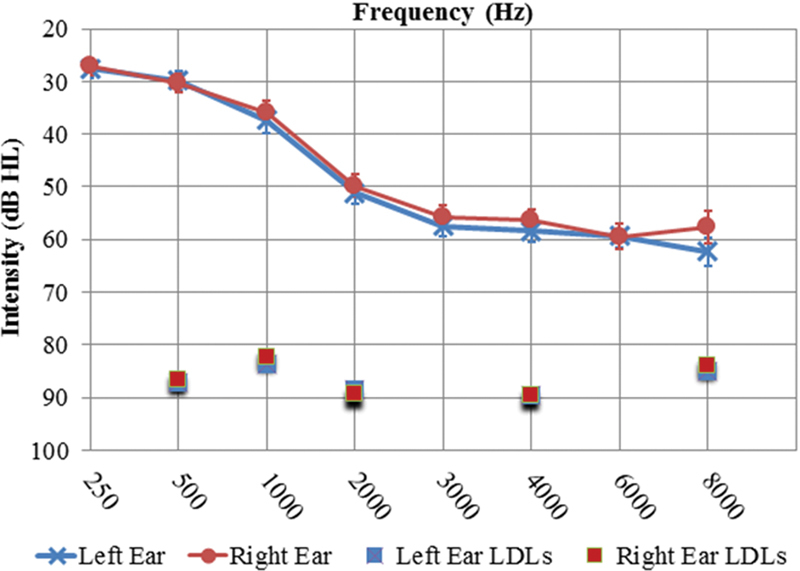
Average pure tone thresholds and LDLs, plotted with standard error of the mean bars. Abbreviations: dB HL, decibels of hearing loss; LDL, loudness discomfort level.
Experience with Hearing Aids (Questions 1 to 5)
In the introductory section of the STQ, we evaluated current or prior experience with amplification with five questions. Our objective was to determine that the individual complaining of sound intolerance demonstrated difficulty adjusting to hearing aid use. We also sought to distinguish between sound intolerance for aided versus unaided listening.
Respondents were asked about current and previous hearing aid use (question 1). The majority of respondents, 77%, were not currently using hearing aids (n = 34). Of those, eight indicated prior hearing aid use. Acquisition of current hearing aids was queried in question 2; a small percentage of respondents (n = 10) reported current sporadic hearing aid use (monaural or binaural). Respondents were asked to describe their hearing aid use as daily or occasionally (question 3). Hearing aid use varied considerably across the 10 current hearing aid users. Several of the respondents who indicated they were currently not using hearing aids reported use time; however, it is unclear if they were indicating use time from prior hearing aid use. Respondents were asked to indicate whether or not sounds were ever uncomfortably loud when they used their hearing aids (question 4). Of the 44 respondents, 13 indicated loudness discomfort for aided listening. One individual responded no to current or prior hearing aid use, but then indicated sounds are uncomfortably loud when wearing hearing aids. Respondents were asked to indicate whether or not they experience similar loudness discomfort even when not wearing hearing aids (question 5). Only nine responded affirmatively and nine responded negatively. The majority of respondents (n = 26) did not answer this question. Of the 26 respondents who did not answer question 5, regarding unaided loudness discomfort, 19 answered the questions in the following section regarding sound sensitivity.
Sound Sensitivity/Intolerance (Questions 6 to 18)
This section contains 13 items probing onset and lateralization of self-perceived sound sensitivity (questions 6 to 9), prior treatment and use of hearing protection devices (HPDs) to avoid sound exposures (questions 10 to 12), changes in sound tolerance over time (question 13), associated pain or discomfort (question 14), ratings of severity of distress caused by reduced sound tolerance and the associated overall effect on life (question 15), activities affected by reduced sound tolerance (question 16), situations that affect sound tolerance (question 17), and specific sounds to which the respondent is sensitive (question 18).
Onset of sound sensitivity (question 6) varied considerably among the respondents, ranging from 2 months (n = 1) to more than 20 years (n = 3). Onset was reported as gradual by 18 respondents. No one reported sudden onset, and 11 reported they were uncertain regarding the rate of onset (i.e., sudden versus gradual onset).
The majority of the respondents indicated sound sensitivity onset was not associated with anything in particular. One person reported onset with menopause, one associated onset with attending a loud basketball game, and one reported that onset occurred while driving a car.
In response to question 9, sound sensitivity was reported as being bilateral for the majority of the respondents who reported unaided sound sensitivity (n = 24). There was no trend toward right or left ear when sound sensitivity was reported as unilateral.
Respondents were asked about prior treatment for sound sensitivity (question 10), with the intent of determining whether or not the respondent had undergone any kind of therapy that might involve sound (e.g., Tinnitus Retraining Therapy, listening to neutral noise on a regular basis). All of the respondents denied prior treatment. This was not surprising in view of the poorly defined problems and the little-known impact of low-level sound for expanding the auditory DR.27
The use of HPDs to minimize loud sound exposures was addressed (question 11). Clinically, many patients who self-report reduced sound tolerance also report using some type of HPDs (e.g., earplugs, swim plugs, or earmuffs) to limit their exposure to sound. In some cases, this practice may result in overprotecting their ears, which may be counterproductive when otherwise healthy sound exposure is diminished. The resulting adverse effects may manifest as increased perceived loudness and enhanced sensitivity to suprathreshold sound.29 30 The majority of respondents denied use of HPDs for this purpose; however, a few respondents indicated use of HPDs to protect their hearing, rather than for sound avoidance. For example, respondents commented they used HPDs when doing yard work (n = 1) or when they knew they would be exposed to loud sound (n = 2).
Respondents were asked to indicate whether or not they had noticed any change in their sound tolerance problem (question 13). Specifically, they were to indicate if their sound tolerance problem was better, worse, or the same since the initial onset. Of those who described a sound tolerance problem (n = 27), more of them reported a change (n = 16) since the onset of their sound intolerance than those who reported no change (n = 11). The direction of change was predominantly worse (n = 15), with only one respondent reporting their sound tolerance was better.
To evaluate the physical correlate of pain associated with sound sensitivity, respondents were queried (question 14) about the presence of pain and/or discomfort during exposure to moderate or loud sounds. Question 14 was worded such that if the answer was yes, respondents had the option to mark pain and/or discomfort as well. Not all respondents who responded with yes indicated pain versus discomfort. A total of 18 responded that they do experience pain or discomfort for moderate or loud sounds, and 11 responded they do not experience pain or discomfort. Most people who indicated pain or discomfort reported the duration of the pain/discomfort (question 14) corresponded to the actual exposure time (n = 8), with a few reporting the pain/discomfort persisted anywhere from 1 to 2 minutes up to 15 hours after the exposure (n = 4).
A rating system was included in this section to evaluate the severity of the sound tolerance problem, the distress caused by the sound tolerance problem, and the effect of the sound tolerance problem on the respondent's life (question 15). Respondents used an 11-point scale, for which 0 indicated low severity/distress/effect and 10 indicated the worst. The average severity rating was 4.72, with a range of 1 to 10. The average rating for the distress caused by their sound tolerance problem was 4.42, with a range of 1 to 10. Finally, the average rating for effect on life was 4.72, with a range of 1 to 10.
Activity avoidance due to sound tolerance problems was addressed (question 16). The response choices included concerts, church, social events, driving, sports events, restaurants, sports, shopping, work, child care, housekeeping, movies, music and other. These options, which were included based on reports by patients with hyperacusis and tinnitus seen in the University of Maryland Tinnitus and Hyperacusis Center, were some of the most frequently mentioned sources of sound discomfort. The activity most avoided was concerts (n = 13), followed by social events (n = 12), movies (n = 12), and sporting events (n = 10). The other activities were checked as being avoided by four or fewer respondents. No one selected driving as an activity he or she avoided because of sound intolerance.
An attempt was made to probe factors that might affect sound tolerance problems (question 17). The response options included stress, hormonal cycle, early in the day, late in the day, barometric pressure, weather, and other. Again, these response options were selected based on patient report. Not surprisingly, the factor most often associated with affecting sound tolerance was stress (n = 11). Several respondents (n = 11) did not indicate any factors that affect their sound tolerance. Other factors were selected by three or fewer respondents.
An evaluation of specific sounds to which one might be sensitive was addressed in question 18. Possible responses included noise, music, talking, paper noises, clatter, mechanical/monotonous sounds, and other. The sample sounds listed encompassed high-pitched sounds, low-pitched sounds, and voices. Specific examples of universally loud sounds such as sirens and slamming doors were not included in the list. The intent was to identify sounds that are generally tolerable to everyone so as to distinguish sensitivity to “regular” sounds as opposed to sensitivity to sounds that are usually judged to be loud by the general population. These also are the types of sounds that new hearing aid users often complain are too loud when they are using their hearing aids. Noise was the number one response (n = 15) followed closely by mechanical/monotonous sounds (n = 13). Talking (n = 9) and music (n = 8) were the next most prevalent bothersome sounds.
Medical History (Questions 19 to 25)
There are some known medical conditions associated with increased sensory sensitivity. These known conditions were included in this section. The occurrence of headache in conjunction with reduced sound tolerance was evaluated (question 19). The majority of the respondents (n = 35) replied no; seven indicated they were uncertain and two reported headaches associated with their sound tolerance problem. One respondent reported the headaches occur daily, but did not characterize the headaches (e.g., migraine, tension, sinus, other), and the other indicated the headaches occur a few times and are characterized as tension and sinus headaches. Other typical auditory-related problems (e.g., dizziness, vertigo) and associated sensory hypersensitivities (e.g., light, touch, smell) were addressed (question 20). About half of the respondents (n = 24) reported problems with speech understanding. Very likely this was related to the presence of hearing loss. Thirteen of the participants reported balance problems, eight reported dizziness, five reported vertigo, and four reported balance sensitivity. Hypersensitivity to light was indicated by seven respondents, to touch by one, and to smell by one, with no one reporting hypersensitivity to taste.
Ototoxic medications have been associated with sensory hypersensitivity, secondary to damage to the auditory system, which can lead to hyperactivity in the neural system and to an associated sound tolerance problem.31 Treatment with ototoxic medications was addressed (question 21). The majority of the respondents (n = 37) indicated they had never taken, to their knowledge, any mycin or other ototoxic drugs. Only one respondent indicated he or she had taken an ototoxic medication (but did not specify which one, how long ago, or the duration of usage), and six indicated they were uncertain.
Respondents were instructed to list current medications (question 22). Nearly all respondents were taking some kind of medication. Only five of the respondents indicated they were not currently taking any medications. Among the current medications were many in use for reducing cholesterol and controlling blood pressure. A few respondents were on antidepressants and/or antianxiety medication; several individuals reported use of aspirin (but dosage not indicated), and others were on hormone therapy. This open-ended question is typical in the context of diagnostic evaluations and may shed light on a possible source of sound sensitivity, hyperacusis, or tinnitus in the individual patient.
Allergies to medications, foods, chemicals, or products were queried (question 23). About half of the respondents (n = 22) indicated no known allergies and half (n = 18) indicated they had allergies. Only one respondent was uncertain. Listed allergens included bee stings; foods such as peanuts, shellfish, and pineapple; medications such as codeine, penicillin, and sulfa drugs; and outdoor sources such as grass. Respondents also were instructed to list any illnesses or surgical procedures they had undergone. Certain illnesses and conditions have been associated with hyperacusis, such as Lyme disease, chronic fatigue syndrome, Bell palsy, head injury, and epilepsy.32 Only one respondent reported Lyme disease; none of the other commonly associated conditions were reported. The inclusion of this question was intended to facilitate the recognition of patterns, but no consistent response pattern or profile was identified.
Noise Exposure (Questions 26 to 28)
Noise exposure history and use of HPDs were evaluated in this set of questions. Specifically, in question 26, respondents were asked if they had any history of occupational, military, or recreational noise exposure. Sixteen respondents indicated they had a history of noise exposure, 15 indicated they did not, and 5 indicated they were uncertain. In view of the fact that sound sensitivity is often associated with noise exposure, typically traumatic noise exposure, and the fact that occupational noise exposure tends to differ from recreational noise exposure in terms of duration, frequency spectrum, and intensity, questions querying the nature of the noise exposure could shed light on the individual's exposure. Of the 16 respondents who reported a history of noise exposure, most described their noise exposure as occupational or military, with a couple of respondents noting recreational noise exposures.
Use of HPDs (question 28) was indicated by 15 of the respondents. Not all of those who reported a history of noise exposure reported use of HPDs, and some who reported no history of noise exposure indicated use of HPDs. Of those who reported use of HPDs, the majority reported using sound-attenuating earplugs. Only four reported using earmuffs and one reported using both. Respondents were asked to estimate the percentage of time they use HPDs. The estimates ranged from 1 to 100% of the time.
Tinnitus (Questions 29 to 35)
Although sound tolerance problems and hearing loss each can exist in isolation, very often both are accompanied by tinnitus.33 Indeed, estimates indicate that almost 90% of persons with hyperacusis experience tinnitus and up to 55% of those with tinnitus have some degree of hyperacusis.34 35 At least one study suggests virtually all tinnitus patients have some degree of hearing loss.36 Questions in the tinnitus subsection probed presence/absence of tinnitus, laterality, onset and sound quality of tinnitus, and the effect of noise on tinnitus. The majority of the respondents (n = 33) reported they had tinnitus (question 29). Only 10 reported they did not have tinnitus and no one indicated uncertainty about having tinnitus. Of those reporting tinnitus, 88% reported their tinnitus was in both ears (question 30). Only two indicated unilateral tinnitus, specifically in the right ear. No one indicated unilateral tinnitus in the left ear. Of those reporting tinnitus in both ears, seven reported right ear worse than left ear and five reported left ear worse than right ear (question 31). For question 31, about half of the respondents with tinnitus described their tinnitus as constant (n = 17) and half as intermittent (n = 16).
Tinnitus duration since onset varied from 7 months to over 60 years (question 32). Tinnitus onset (question 33) was described as gradual by 14 respondents (42%), sudden by 3 (9%), and 15 (45%) were uncertain. One person who reported tinnitus did not respond to the nature of onset. Tinnitus sound quality (question 34) was described as ringing/high-pitched by the majority of the respondents. Twelve described their tinnitus sound quality as buzzing, often in conjunction with high-pitched and ringing.
Some people with tinnitus experience exacerbation of their tinnitus during or after exposure to noise.37 Of the respondents reporting tinnitus, eight reported noise exposure had no effect on their tinnitus and 10 reported noise masks their tinnitus. Two respondents reported tinnitus got louder and one reported tinnitus became softer after noise exposure. The effect of noise on tinnitus generally lasted only while the person was exposed to noise, with one person indicating that noise made their tinnitus louder for hours after the noise exposure.
Question 36
The final questionnaire item asked the respondent to rank sound tolerance, hearing, and tinnitus as they relate to each other in terms of problem areas. Specifically, respondents were instructed as follows: “Please rank the following issues as they relate to each other (e.g., sound tolerance problems are worse than hearing problems, tinnitus is worse than hearing problems, etc.).” The goal of this item was to determine which problem is perceived as being the most significant for the respondent. Clinically, this information can be very useful for guiding treatment. For example, if a patient ranks sound tolerance problems greater than hearing problems, then a treatment protocol addressing sound sensitivity would be indicated, which then could facilitate adjustment to hearing aids after the respondent's sound tolerance issues were resolved. An individual reporting tinnitus is a worse problem than the hearing problem would potentially benefit from the use of counseling together with sound therapy from sound generators alone, or in conjunction with amplification.37
The majority of respondents in our sample ranked hearing problems as the primary problem (n = 14). Sound tolerance was ranked as the primary problem by seven respondents and tinnitus was ranked as the primary problem by five participants. In a few cases, respondents ranked two problems as equally bothersome (sound tolerance and hearing problem for 3 respondents, sound tolerance and tinnitus for 2 respondents).
Discussion
We have described the preliminary design and responses to a 36-item interview and questionnaire instrument that has potential utility for understanding loudness complaints and reduced sound tolerance among individuals considering hearing aid use, as well as those who have been unsuccessful hearing aid users secondary to complaints of excessive loudness or sound intolerance. Currently, there are several questionnaires available to evaluate hearing aid expectations,21 22 23 to establish treatment goals,21 to evaluate subjective hearing handicap and disability,21 24 25 and to assess aided benefit and satisfaction.21 24 25 To date, however, a clinical questionnaire is lacking to facilitate identification of self-perceived problems of loudness and/or reduced sound intolerance. Such problems may present as nebulous, poorly described, and/or delineated complaints from a broad range of potential and unsuccessful hearing aid users. The Profile of Aided Loudness represents yet another self-report instrument that may have potential to identify reduced sound tolerance indirectly, but its original intent was primarily to identify whether or not satisfactory loudness has been achieved in fitting nonlinear hearing aids.38
Perhaps the paucity of validated questionnaires for addressing problems related to decreased sound tolerance and related complaints stems from the challenges of distinguishing the effects of reduced sound tolerance from recruitment. More aptly worded, the distinction of interest is the perceived effect of reduced sound tolerance, as quantified by lower than normal LDLs (<90-dB HL), from that resulting from a reduced DR for loudness, owing primarily to elevated hearing thresholds due to sensorineural hearing loss.19 This is potentially a critical clinical distinction that may have real utility for understanding, delineating, and managing loudness and sound tolerance complaints of hearing aid candidates. Indeed, this is a distinction that ultimately may lead to improved strategies for fitting amplification. All but one of our 44 respondents met Goldstein and Shulman's criteria for hyperacusis based on a reduced DR (<60 dB for at least one audiometric frequency) and 39 of the 44 respondents met the criteria for hyperacusis on the basis of LDLs (<95 dB at 2 or more audiometric frequencies).19 Of the five respondents who were not hyperacusic, regarding LDLs, only one indicated subjective hyperacusis by responding affirmatively to the question, “Do you have similar loudness discomfort even when you are not wearing your hearing aids?” Two of the five respondents responded negatively, but responded positively to the question about sounds being too loud when using hearing aids. The final two respondents did not answer either question. Further complicating this distinction is the lack of consensus regarding the various types of reduced sound tolerance or excessive sound sensitivity to suprathreshold sounds that can arise from reduced sound tolerance related to physical sensitivity to sound (i.e., loudness hyperacusis) compared with reduced sound tolerance related to the emotional reaction to sound (i.e., misophonia or annoyance hyperacusis and phonophobia or fear hyperacusis).39 40 It could well be that potential hearing aid users, or unsuccessful hearing aid users, are reacting with discomfort to a given sound or sound quality (rather than to a given sound level or volume), which would be consistent with misophonia and/or phonophobia rather than hyperacusis.
Several existing questionnaires potentially could be used by clinicians to identify or delineate the impact of reduced sound tolerance on successful hearing aid use.34 41 42 43 44 45 Although these questionnaires differ in approach and intent, there are similarities. Nearly all evaluate the role of reduced sound tolerance on activity avoidance and overprotection of the ears to avoid sound.34 42 44 45 Some also evaluate the types of sounds that cause discomfort, such as high-pitched sounds and repetitive sounds.34 41 42 These questions are useful in evaluating an individual's behavioral response to reduced sound tolerance and may more clearly distinguish hyperacusis, misophonia, and phonophobia from one another. Some questionnaires evaluate the presence of aural discomfort or pain in conjunction with sound exposure.34 43 Individuals who report inordinate pain to sound exposures likely have a different underlying neurophysiological processes contributing to their hyperacusis condition.46 47 We are aware of only two questionnaires, not including the STQ described here, that probe other sensory hypersensitivities such as sensitivity to light and touch.34 43 As mentioned earlier, some health conditions are associated with increases in sensitivity across multiple sensory systems. Individuals reporting concurrent sensory hypersensitivities should be considered for referral for neurologic consultation. Similarly, no other questionnaire to our knowledge probes physical factors that might affect sound sensitivity, such as time of day or weather, or physiologic factors such as hormonal cycle and menopause. Onset of sound sensitivity is rarely probed34; this piece of information may make a significant contribution to identifying the etiology of the reduced sound tolerance. Self-perceived ratings of severity, distress, annoyance, and effect on life are helpful for monitoring treatment progress and are included in some of the questionnaires.41 43 45
The majority of the respondents in our study reported gradual onset of their loudness condition or reduced sound tolerance, followed by a significant number being uncertain regarding rate of onset. This contrasts with the findings of the American Tinnitus Association, who surveyed their members and found that 50% of those who reported sound sensitivity described sudden onset, 47% described gradual onset, and 3% were unsure of onset.48 Anecdotally, onset of suprathreshold sound hypersensitivity is typically associated with traumatic noise exposure, use of medications, and head injury.
Comparison of the responses regarding tinnitus onset in the Tinnitus Archive database reveals striking differences to the onset dynamics we documented for sudden onset tinnitus (9% for our population compared with 39% in the Tinnitus Archive database), and greater uncertainty regarding sudden versus gradual onset (45% for our population compared with less than 3% in the Tinnitus Archive).49 With respect to tinnitus sound quality, our population was comparable in that ringing was described by the majority of patients in the Tinnitus Archive database.
It is worth restating here that the STQ was developed as a research tool as part of an effort to understand and evaluate the efficacy of a sound therapy intervention for DR expansion. The STQ therefore was not specifically designed as a clinical tool. The future goal is to modify the STQ to eliminate or refine questions that: (1) respondents frequently left blank; (2) did not contribute toward an understanding of the individual's sound tolerance complaints or loudness concerns (see Appendix B); or (3) were often vague or nebulous for some of the study respondents. In view of the fact that new hearing aid users frequently report loudness-related complaints when initiating amplification, refinements of this interview and questionnaire instrument (see Appendices B and C), leading to a validated clinical self-report tool, may have potential utility in the absence of clinical indices for differentiating patients with respect to their suprathreshold sound sensitivity complaints. Ideally, such a tool would guide clinicians toward selection of a loudness-based fitting rationale, the provision of optimal counseling, and would promote successful fitting and use of hearing aids among individuals with sound tolerance challenges that otherwise restrict their abilities to benefit from amplification.
Some STQ items require clarification or refinement to improve their utility. Such items include those dealing with unaided sound sensitivity, the use of HPDs to overprotect hearing, type and duration of noise exposure, and ranking the problems of sound tolerance, tinnitus, and hearing. Based on the responses to questions 4 and 5, the need for a question regarding unaided sound sensitivity without reference to hearing aid use is indicated, especially if a questionnaire like this is to be used as a tool in the hearing aid selection process. Question 11, regarding use of HPDs to minimize sound exposure, could be clarified by distinguishing between protection and avoidance, and by providing a reference for loud. Most people would judge the sound of an airplane taking off nearby or going to a live music concert as loud. The question might elicit more accurate responses if phrased as, “Do you use earplugs or earmuffs to protect your hearing against loud sounds such as those encountered at rock concerts or during use of lawnmowers?”; a related additional question might also be included such as, “Do you use earplugs or earmuffs to avoid the possibility of being exposed to sounds louder than conversational speech?” By anchoring loud to examples like this, respondents might have better understood the difference between protection and avoidance in the STQ. Respondents were asked to describe the type and frequency (daily, monthly, and so on) of exposure (question 27); this question was perhaps too open-ended and may benefit in future use from specific categories (e.g., <8 hours per week, >8 hours per day) per type of noise. Finally, the direction to “rank” the problems relative to each other, using a 10-point scale for each of the three problems, may have confused the respondents. That is, it may have been unclear what was being ranked; the severity of each problem itself, rather than the relative severity of each problem. Although this question has a high degree of utility for differentiating and prioritizing treatment, the question could be clarified either by giving patients the option to rank their respective tinnitus, hearing, and sound tolerance problems numerically as 1, 2, and 3 in order of their relative perception of each problem and/or by asking patients to rank the severity of each problem, which would also enable patients to indicate the relative importance of each problem.
Ultimately, these and other refinements will be needed before the STQ is clinically ready for roll out as a validated tool. The STQ mix of open-ended interview questions, Likert-scale ranking questions, and yes-or-no questions in Appendix A does not now offer a format for standardized scoring and validation of this tool. A step toward such a tool is presented in the Appendices B and C. The first part of the tool is an interview (Sound Tolerance Interview in Appendix B) to be administered by the clinician. The second part is a reformatted and scorable STQ, designed as a self-report questionnaire (Appendix C), to be completed by the patient, to quantify the impact of sound tolerance on the individual. The combined instruments together are designated here as the STIQI. That this reformatted version of the interview and questionnaire components of the STQ (or some other relevant formalized questionnaire) is needed now, both for research and clinical applications, is highlighted by within-subject respondent conflicts in the individual participant's written STQ responses (reported here) and his or her verbal reports to screening intake and history questions used in determining initial eligibility for the sound therapy-based DR expansion trial.27 These conflicts are most evident in the rankings of the respondents' primary problems (e.g., sound tolerance versus tinnitus) and the relative severity of each problem. Thus, the STQ, or our reformatted version of it in a formal scorable structured format akin to that presented in Appendix C, appears to have potential utility for parsing and delineating the subjective perception of loudness concerns and related sound tolerance complaints, which may be vague, but of real clinical relevance.
Appendix A: Original Sound Tolerance Questionnaire.
| Hearing Aids |
|---|
| 1. Do you wear hearing aids now? Yes / no / one / two |
| If the answer is no, have you worn hearing aid(s) in the past? Yes / no |
| 2. When did you get your present hearing aid(s)? |
| 3. Describe your hearing aid use (circle all that apply): |
| Daily / occasionally / less than 4 hours a day, 5–10 hours a day, more than 10 hours a day |
| 4. When you are wearing your hearing aid(s), are sounds ever uncomfortably loud? Yes / no |
| 5. Do you have similar loudness discomfort even when you are not wearing your hearing aid(s)? Yes / no |
| If you have problems tolerating loud sounds without hearing aid(s), please go on to question #6. If you only have trouble when using hearing aids, please skip to item #19. |
| Sound Sensitivity/Intolerance |
| 6. Write the approximate date when you began to be sensitive to moderate and / or loud sounds. |
| 7. Please indicate if the onset was: gradual / sudden / uncertain. |
| 8. Was the onset associated with any particular event? Yes / no |
| If yes, please describe: |
| 9. Is your sound tolerance problem usually right / left / both? |
| 10. Have you received any treatment for your sound tolerance problem? Yes / no |
| If yes, please describe: |
| 11. Do you use hearing protection devices to avoid loud sounds? Yes / no |
| 12. If yes, what percentage of the time (___%) and what type? Earplugs / earmuffs / both |
| 13. Since you first noticed a problem with sound tolerance, has there been any change? Yes / no |
| Is it better / worse / same? |
| 14. Do you experience any pain and / or discomfort for moderate or loud sounds? Yes / no |
| If yes, indicate the duration of the pain or discomfort by checking one of the boxes below. |
| During exposure to the sound / for__ minutes / for __ hours / for ___ days |
| 15. There are three rating scales below for you to describe, as of today, the severity of your sound tolerance problem, the distress this problem causes you, and its overall effect on your life: |
| a. Severity: 0 to 10 (the worst) |
| b. Distress: 0 to 10 (the worst) |
| c. Effect on life: 0 to 10 (the worst) |
| 16. Please check below the activities that you avoid or limit due to your sound tolerance problem: concerts / church / social events / driving / sports events / restaurants / sports / shopping / work / child care / housekeeping / movies / music / other. |
| 17. Please check below any of the following situations that affect your sound tolerance: stress / hormonal cycle / early in the day / late in the day / barometric pressure / weather / other. |
| 18. Please check below any sounds that you are sensitive to: noise / music / talking / paper noises / clatter / mechanical, monotonous sounds / none of the above / other (please describe below). |
| Medical History |
| 19. Do you have problems with headaches associated with your sound tolerance problem? Yes / no / uncertain |
| Frequency of headaches |
| Type of headache: migraine / tension / sinus / other |
| 20. Do you have problems with any of the following? Dizziness / vertigo / balance problems / speech understanding (distorted speech) / other hypersensitivity to light / touch / smell / taste / balance / pain |
| 21. To your knowledge, have you ever taken any mycin or other ototoxic drugs (such as gentamycin or vancomycin)? Yes / no / uncertain |
| 22. Please list any medications you are currently taking. |
| 23. Do you have any allergies to specific medications, foods, or other chemicals or products? Yes / no / uncertain |
| 24. If yes, please list: |
| 25. Please list any illnesses and surgical procedures that you have had. |
| Noise Exposure History |
| 26. Do you have any history of occupational / military / recreational noise exposure? Yes / no / uncertain |
| 27. If yes, please describe the type and degree (e.g., every day for x many years, or about once a month) of exposure. |
| 28. Do you use hearing protection devices during exposure to loud noise? In noise: yes / no |
| What type do you wear? earplugs / earmuffs / both |
| What percent of time do you wear noise protection devices? ___% |
| Tinnitus |
| 29. Do you experience tinnitus (ringing in your ears)? Yes / no |
| 30. If yes, is the ringing right / left / both? |
| If both, is one ear worse than the other? Yes / no / right / left |
| 31. Is your tinnitus constant / intermittent? |
| 32. How long have you had tinnitus? |
| 33. Was the onset gradual / sudden / uncertain? |
| 34. Please indicate what kind of sound your tinnitus is (check all that apply): ringing / buzzing / humming / clicking / other (please describe). |
| 35. What effect does noise exposure have on your tinnitus? None / it is masked (or covered) / it gets louder / it gets softer |
| Does this effect last only while you are in noise? Yes / no |
| If no, how long does the tinnitus last? __minutes / __hours / __days |
| Primary Problem |
| 36. Please rank the following issues as they relate to each other (e.g., sound tolerance problems are worse than hearing problems, tinnitus is worse than hearing problems): |
| Tolerance: 0 to 10 |
| Hearing: 0 to 10 |
| Tinnitus: 0 to 10 |
A combined interview and self-assessment instrument, in conjunction with measurement of frequency-specific LDLs, offers promise as a sensible approach to facilitate the identification of patients with sound tolerance problems that interfere with successful adjustment to amplification. Together, the resulting responses could, in turn, inform the rehabilitative process. The STIQI, as a combined structured clinician interview and self-report questionnaire instrument, is more likely to assess with greater specificity problem aspects of sound tolerance that cannot be captured by LDL measurements alone. The STIQI should have good face validity based on our clinical experience, but validation of the two-component instrument is essential and remains to be conducted in future research.50
Summary
Differentiating self-perceived loudness and sound tolerance problems related to loudness recruitment and a reduced DR as a consequence of sensorineural hearing loss versus primary hyperacusis is complicated by the poorly defined nature of loudness-based hyperacusis and related conditions, including misophonia, and associated conditions such as tinnitus. However, recognition of the fundamental differences between these two conditions and the above confounding problems can affect aided outcome. The STQ described here represents a preliminary effort to assess the potential utility of a self-report tool to facilitate the identification and differentiation of subjectively significant loudness and sound tolerance complaints that may negatively impact the successful use of amplification or negatively affect the process of adapting to hearing aid use. Our future efforts will focus on realization of a two-component interview instrument and standardized, scorable, validated questionnaire toward this end goal.
Acknowledgments
This research was supported by a Public Health Service research award (parent grant NIDCD R01DC04678) from the National Institutes of Health to Craig Formby and by a pair of companion supplement awards. Work was started while LaGuinn Sherlock and Craig Formby were at the University of Maryland, Baltimore. We gratefully acknowledge assistance from Susan Gold in identifying content for the STQ, and from Sue Ann Erdman for assistance in selecting the content and structure of the questionnaire and for constructive criticism of the manuscript. We would like to acknowledge also the assistance provided by Monica Hawley in entering the handwritten responses on the STQ to electronic format. Karen Tucker prepared the final draft of this manuscript. We are grateful to the students who provided assistance in conducting this study: Justine Cannavo, Allyson Segar, and Christine Gmitter Masuicca.
Notes
The views expressed in this article are those of the authors and do not reflect the official policy of the Department of the Army, the Department of the Navy, the Department of the Air Force, the Department of Defense, or the U.S. Government.
References
- 1.Dillon H Prescribing hearing aid amplification In: Dillon H, ed. Hearing Aids, New York, NY: Thieme; 2012286–353. [Google Scholar]
- 2.Keidser G, Dillon H, Flax M, Ching T, Brewer S. The NAL-NL2 prescription procedure. Audiology Res. 2011;1(1):e24. doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scollie S, Seewald R, Cornelisse L. et al. The Desired Sensation Level multistage input/output algorithm. Trends Amplif. 2005;9(4):159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valente M, Van Vliet D. The Independent Hearing Aid Fitting Forum (IHAFF) protocol. Trends Amplif. 1997;2(1):6–35. doi: 10.1177/108471389700200102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornelisse L E, Seewald R C, Jamieson D G. The input/output formula: a theoretical approach to the fitting of personal amplification devices. J Acoust Soc Am. 1995;97(3):1854–1864. doi: 10.1121/1.412980. [DOI] [PubMed] [Google Scholar]
- 6.Cox R. The MSU hearing instrument prescription procedure. Hear Instrum. 1988;39(1):6–10. [Google Scholar]
- 7.Franks J R, Beckmann N J. Rejection of hearing aids: attitudes of a geriatric sample. Ear Hear. 1985;6(3):161–166. doi: 10.1097/00003446-198505000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Lindley G A, Palmer C V, Durrant J, Pratt S. Audiologist- versus patient-driven hearing aid fitting protocols. Semin Hear. 2001;22:139–159. [Google Scholar]
- 9.Cunningham D R, Williams K J, Goldsmith L J. Effects of providing and withholding postfitting fine-tuning adjustments on outcome measures in novice hearing aid users: a pilot study. Am J Audiol. 2001;10(1):13–23. doi: 10.1044/1059-0889(2001/001). [DOI] [PubMed] [Google Scholar]
- 10.Reber M B, Kompis M. Acclimatization in first-time hearing aid users using three different fitting protocols. Auris Nasus Larynx. 2005;32(4):345–351. doi: 10.1016/j.anl.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Kochkin S. Customer satisfaction with single and multiple microphone digital hearing aids. Hear Rev. 2000;7:24–29. [Google Scholar]
- 12.Filion P R, Margolis R H. Comparison of clinical and real-life judgments of loudness discomfort. J Am Acad Audiol. 1992;3(3):193–199. [PubMed] [Google Scholar]
- 13.Munro K J, Blount J. Adaptive plasticity in brainstem of adult listeners following earplug-induced deprivation. J Acoust Soc Am. 2009;126(2):568–571. doi: 10.1121/1.3161829. [DOI] [PubMed] [Google Scholar]
- 14.Sherlock L P, Formby C. Estimates of loudness, loudness discomfort, and the auditory dynamic range: normative estimates, comparison of procedures, and test-retest reliability. J Am Acad Audiol. 2005;16(2):85–100. doi: 10.3766/jaaa.16.2.4. [DOI] [PubMed] [Google Scholar]
- 15.Bentler R A, Cooley L J. An examination of several characteristics that affect the prediction of OSPL90 in hearing aids. Ear Hear. 2001;22(1):58–64. doi: 10.1097/00003446-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Kamm C, Dirks D D, Mickey M R. Effect of sensorineural hearing loss on loudness discomfort level and most comfortable loudness judgments. J Speech Hear Res. 1978;21(4):668–681. doi: 10.1044/jshr.2104.668. [DOI] [PubMed] [Google Scholar]
- 17.Keller J N Loudness discomfort levels: a retrospective study comparing data from Pascoe (1988) and Washington University School of Medicine. Independent Studies and Capstones Paper 83. Program in Audiology and Communication Sciences, Washington University School of Medicine. 2006. Available at: http://digitalcommons.wustl.edu/. Accessed January 27, 2016
- 18.Pascoe D P Clinical measurements of the auditory dynamic range and their relationship to formulas for hearing aid gain In: Jensen J H, ed. Hearing Aid Fitting: Theoretical and Practical Views. 13th Danavox Symposium Copenhagen, Denmark: Stougaard Jensen; 1988129–151. [Google Scholar]
- 19.Goldstein B, Shulman A. Tinnitus—hyperacusis and the loudness discomfort level test—a preliminary report. Int Tinnitus J. 1996;2:83–89. [PubMed] [Google Scholar]
- 20.Elberling C. Loudness scaling revisited. J Am Acad Audiol. 1999;10(5):248–260. [PubMed] [Google Scholar]
- 21.Dillon H, James A, Ginis J. Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. J Am Acad Audiol. 1997;8(1):27–43. [PubMed] [Google Scholar]
- 22.Cox R M Alexander G C Expectations about hearing aids and their relationship to fitting outcome J Am Acad Audiol 2000117368–382., quiz 407 [PubMed] [Google Scholar]
- 23.Jacobson G P Newman C W Fabry D A Sandridge S A Development of the three-clinic hearing aid selection profile (HASP) J Am Acad Audiol 2001123128–141., quiz 165–166 [PubMed] [Google Scholar]
- 24.Gatehouse S. Glasgow hearing aid benefit profile: derivation and validation of a client-centered outcome measure for hearing aid services. J Academy of Audiology. 1999;10:80–103. [Google Scholar]
- 25.Cox R M, Alexander G C. The abbreviated profile of hearing aid benefit. Ear Hear. 1995;16(2):176–186. doi: 10.1097/00003446-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Cox R M, Alexander G C. Measuring satisfaction with amplification in daily life: the SADL. Ear Hear. 1999;20(4):306–320. doi: 10.1097/00003446-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Formby C, Hawley M L, Sherlock L P. et al. A sound therapy-based intervention to expand the auditory dynamic range for loudness among persons with sensorineural hearing losses: a randomized placebo-controlled clinical trial. Semin Hear. 2015;36(2):77–110. doi: 10.1055/s-0035-1546958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jastreboff P J. San Diego, CA: Singular, Thomson Learning; 2000. Tinnitus habituation therapy (THT) and tinnitus retraining therapy (TRT) pp. 357–376. [Google Scholar]
- 29.Formby C, Sherlock L P, Gold S L. Adaptive plasticity of loudness induced by chronic attenuation and enhancement of the acoustic background. J Acoust Soc Am. 2003;114(1):55–58. doi: 10.1121/1.1582860. [DOI] [PubMed] [Google Scholar]
- 30.Formby C, Sherlock L P, Gold S L, Hawley M L. Adaptive recalibration of chronic auditory gain. Semin Hear. 2007;28:295–302. [Google Scholar]
- 31.Salvi R J, Wang J, Lockwood A H, Burkard R, Ding D. Noise and drug induced cochlear damage leads to functional reorganization in the central auditory system. Noise Health. 1999;1(2):28–42. [PubMed] [Google Scholar]
- 32.Vernon J A, Sanders B T. Boston, MA: Allyn and Bacon; 2001. Tinnitus—Questions and Answers. [Google Scholar]
- 33.Andersson G, Lindvall N, Hursti T, Carlbring P. Hypersensitivity to sound (hyperacusis): a prevalence study conducted via the Internet and post. Int J Audiol. 2002;41(8):545–554. doi: 10.3109/14992020209056075. [DOI] [PubMed] [Google Scholar]
- 34.Anari M, Axelsson A, Eliasson A, Magnusson L. Hypersensitivity to sound—questionnaire data, audiometry and classification. Scand Audiol. 1999;28(4):219–230. doi: 10.1080/010503999424653. [DOI] [PubMed] [Google Scholar]
- 35.Schecklmann M Landgrebe M Langguth B; TRI Database Study Group. Phenotypic characteristics of hyperacusis in tinnitus PLoS One 201491e86944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicolas-Puel C, Faulconbridge R L, Guitton M, Puel J-L, Mondain M, Uziel A. Characteristics of tinnitus and etiology of associated hearing loss: a study of 123 patients. Int Tinnitus J. 2002;8(1):37–44. [PubMed] [Google Scholar]
- 37.Jastreboff P J, Hazell J. Cambridge, UK: Cambridge University Press; 2004. Tinnitus Retraining Therapy. Implementing the Neurophysiological Model. [Google Scholar]
- 38.Palmer C V, Mueller H G, Moriarty M. Profile of aided loudness: a validation procedure. Hear J. 1999;52(6):34–42. [Google Scholar]
- 39.Tyler R S, Pienkowski M, Roncancio E R. et al. A review of hyperacusis and future directions: part I. Definitions and manifestations. Am J Audiol. 2014;23(4):402–419. doi: 10.1044/2014_AJA-14-0010. [DOI] [PubMed] [Google Scholar]
- 40.Jastreboff P J, Jastreboff M M. Treatments for decreased sound tolerance (hyperacusis and misophonia) Semin Hear. 2014;35:105–120. [Google Scholar]
- 41.Dauman R, Bouscau-Faure F. Assessment and amelioration of hyperacusis in tinnitus patients. Acta Otolaryngol. 2005;125(5):503–509. doi: 10.1080/00016480510027565. [DOI] [PubMed] [Google Scholar]
- 42.Henry J A Zaugg T L Myers P J Kendall C J Progressive Tinnitus Management Clinical Handbook for Audiologists 1st ed. San Diego, CA: Plural Publishing; 2010117–119. [Google Scholar]
- 43.Jastreboff M M Jastreboff P J Questionnaires for assessment of the patients and treatment outcomeSixth International Tinnitus Seminar; September 5–9, 1999, Cambridge, UK; 487–490
- 44.Khalfa S, Dubal S, Veuillet E, Perez-Diaz F, Jouvent R, Collet L. Psychometric normalization of a hyperacusis questionnaire. ORL J Otorhinolaryngol Relat Spec. 2002;64(6):436–442. doi: 10.1159/000067570. [DOI] [PubMed] [Google Scholar]
- 45.Tyler R S, Bergan C, Preece J, Nagase S. Stuttgart, Germany: Georg Thieme Verlag; 2003. Audiologische messmethoden de hyperakusis; pp. 39–46. [Google Scholar]
- 46.Flores E N, Duggan A, Madathany T. et al. A non-canonical pathway from cochlea to brain signals tissue-damaging noise. Curr Biol. 2015;25(5):606–612. doi: 10.1016/j.cub.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu C, Glowatzki E, Fuchs P A. Unmyelinated type II afferent neurons report cochlear damage. Proc Natl Acad Sci U S A. 2015;112(47):14723–14727. doi: 10.1073/pnas.1515228112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tabachnick B. Sound sensitivity. Tinnitus Today. 1998;23:14–16. [Google Scholar]
- 49.Meikle M B Creedon T A Griest S E Tinnitus Archive 2nd ed. 2004. Available at: http://www.tinnitusArchive.org/. Accessed January 27, 2016 [Google Scholar]
- 50.Erdman S A Self-assessment: From research focus to research toolInGagné J-P Tye-Murray N, eds. Research in audiological rehabilitation: Current trends and future directionsJournal of the Academy of Rehabilitative Audiology 1994; 27(Mongr. suppl.):67–90 [Google Scholar]


