Abstract
This systematic review examines whether negative affect symptoms (i.e., anxiety, depression, and internalizing symptoms more broadly) predict subsequent adolescent substance use after controlling for co-occurring externalizing symptoms. Following PRISMA procedures, we identified 61 studies that tested the association of interest. Findings varied depending on the type of negative affect symptom and to some extent on the substance use outcome. The most consistent associations were evident for depressive symptoms, particularly as predictors of substance use composite scores. No clear association between anxiety and substance use or between internalizing symptoms and substance use was evident, and indeed these associations were as often negative as positive. Mixed findings regarding the depression-substance use association, however, also call for greater attention to potential moderating factors that may help define who, when, and in what context depression serves as an important risk factor for later substance use above and beyond risk associated with externalizing symptoms.
Keywords: Adolescent Substance Use, Internalizing Symptoms, Depression, Anxiety, Systematic Review
The literature on developmental pathways to substance use/abuse among youth implicates externalizing symptoms, such as aggression, delinquency, and deviant behaviors, as precursors (Chassin, Sher, Hussong, & Curran, 2013; Hussong, Rothenberg, Smith, & Haroon, in press; King et al., 2004; Steele, et al., 1995). More recently, attention is being given to an internalizing pathway to substance use outcomes whereby substance use is motivated by a desire to reduce distress and negative affect (Hussong, Jones, Stein, Baucom, & Boeding, 2011; Kassel et al., 2010). Evidence in support of the etiologic role of internalizing – or negative affect – symptoms as predictors of substance use is less consistent and weaker than is evidence for the role of externalizing systems (Hussong et al., 2011). Even so, there is a common reliance in the literature on an assumed link between negative affect symptoms and youth substance use (Kaplan, 1980; Khantzian, 1997; McCarty, Curtin, Piper, & Baker, 2010). The purpose of this systematic review is to examine the extent to which negative affect predicts substance use in adolescence, a time when both substance use and many negative affect symptoms are on the rise (Chassin, Sher, Colder & Hussong, 2016; Graber & Sontag, 2009).
The review is challenging because of at least three factors. First, because of co-morbidity of externalizing and internalizing symptoms among youth (Hussong et al., 2011), any effort to detect the unique contributions of internalizing symptoms to substance use must control for the contribution of externalizing symptoms. Otherwise, there is the possibility that any association between negative affect symptoms and adolescent substance use is actually attributable to externalizing symptoms (Angold, Costello, & Erkanli, 1999).
Second, there are differing forms of internalizing symptoms (depression, anxiety, or global indices) and different approaches to measurement (diagnostic interviews versus symptom checklists). Third, substance use outcomes differ both by type of substance, whether distinct by substance or pooled across substances, as well as by the type of use, such as onset or maintenance. These last two challenges potentially obscure conclusions that can be drawn from the literature about the contributions of negative affect to youth substance use. For example, proponents of the internalizing model argue that negative affect symptoms may be a substance-specific predictor, such that negative affect symptoms are more strongly associated with more deviant forms of substance use (i.e., ‘harder’ drugs of abuse versus alcohol, tobacco and marijuana or indicators of problem use rather than consumption alone) or that some forms of negative affect symptoms are more strongly related to substance use (i.e., depression) than are others (i.e., anxiety; Colder, Chassin, Lee, & Villalta, 2010; Hussong et al., 2011). Such variability by type of substance use and type of negative affect may in part account for the inconsistent findings regarding the association between negative affect symptoms and substance use.
We thus examine whether negative affect uniquely predicts substance use when accounting for the contribution of externalizing symptoms and when considered by (1) type of negative affect (anxiety, depression, or composite internalizing symptoms and, where possible, by measurement of symptoms or diagnosis), (2) type of substance use outcome (alcohol, tobacco, marijuana, illicit drugs and composite substance use), and (3) where possible, along potential points of substance use involvement. We include studies with youth covering the broad span of adolescence, ages 11 to 19, with the intent of examining whether relations differ for younger versus older adolescents. In addition, because research links internalizing processes to alcohol use and abuse in girls more so than boys (Federman et al., 1997), where possible, we examine gender as a moderating variable. By parsing studies along these multiple dimensions, our aim is to identify particularly problematic subsets of negative affect – substance use linkages and particularly vulnerable subgroups of individuals. Summarizing the evidence for which youth and for which forms of negative affect and substance use there are unique prospective associations is needed for progress on development of theoretical or organizing frameworks on the internalizing pathway to substance use.
Methods
Search Strategy
We screened the literature for empirical studies that assessed the association between negative affect symptoms and substance use during adolescence after controlling for co-occurring externalizing symptoms. A core search strategy using Boolean operators was developed and used in all searches. The main keywords included: [adolescent OR youth OR teen OR student) AND [(alcohol OR drug OR substance OR tobacco OR marijuana) AND (use OR misuse OR abuse)] AND [internalizing symptom OR anxiety OR depression OR panic disorder OR phobia] AND [externalizing symptom OR aggression OR conduct disorder OR aggressive OR problem behavior OR deviant behavior]. We searched databases appropriate for clinical and behavioral studies of substance use, including PubMed, PsycINFO, Academic Search Premiere, Scopus, Web of Science, CINAHL, Global Health, ERIC, Sociological Abstracts, Education Full Text and Science Direct. We also searched the bibliographies of retained articles to identify additional studies. Our search included any publication date prior to September 14th, 2015. This review was part of a study that receive Institutional Review Board approval.
Inclusion and Exclusion Criteria
Population
Studies were restricted to those that examined substance use during adolescence, defined as ages 11 to 19. (Studies that combined adolescent and young adult samples were excluded.) General community population samples as well as clinical and high-risk samples (e.g., children of alcoholics) were included.
Predictor variables: Negative affect and externalizing symptoms
Because this is the first study to systematically examine the unique effects of negative affect symptoms on substance use net of externalizing symptoms, we defined negative affect symptoms broadly and included both diagnostic and symptom indicators. We included studies of depression, anxiety, panic disorders, and phobias. Studies that measured symptoms separately or constructed an overall negative affect symptom variable were included. Externalizing symptoms were also defined broadly to include aggression, conduct disorders, oppositional defiant disorders, and deviant and/or problem behaviors. Note that symptom measures may include a full-range of severity (from above to below thresholds - though this distribution was rarely reported) but diagnostic measures distinguish severity above versus below thresholds.
Outcome variables: Substance use
Studies included an assessment of alcohol, tobacco, marijuana, other illicit drugs, and/or composite scores of substance use that combined these drug classes.
Type of study
Empirical studies reporting quantitative results in peer-reviewed journals were included. Only longitudinal studies for which negative affect symptoms served as predictors of substance use at a later time point were retained. Clinical trials and reviews (e.g., theoretical reviews or meta-analyses) were excluded. To ensure the most accurate measurement of the time-dependent relation between negative affect symptoms and substance use, we excluded studies with retrospective reporting of variables of interest. Furthermore, studies utilizing analysis methods for which the effect of negative affect symptoms net of externalizing symptoms on substance use could not be isolated (e.g., mixture models) were excluded. Studies were limited to those published in the English language.
Screening and Data Extraction
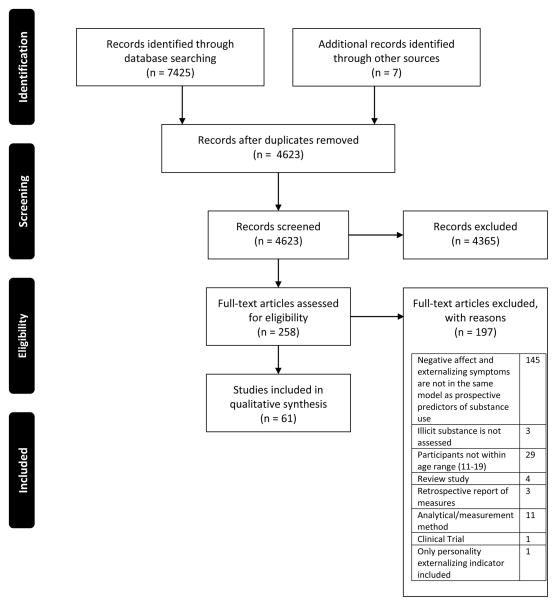
Guidelines set forth by the PRISMA Statement to ensure transparency in the process of identifying, selecting and reporting findings of systematic reviews were followed (Moher, Liberati, Ttzlass, Altman, & PRISMA Group, 2009). Two members of the study team screened 4,623 identified article abstracts for relevance and a third team member helped to resolve discrepancies. A total of 258 articles were retained for full-text review. Two team members reviewed each article to assess inclusion and exclusion criteria in detail with discrepancies resolved by the four member study team. A total of 61 articles were retained for qualitative synthesis. A flow chart detailing inclusion and exclusion decisions at each stage is presented in Figure 1. (A summary table of included studies is available as an online supplement.)
Figure 1.
PRISMA report of search strategy
Review Structure
A meta-analysis of the results was deemed inappropriate given the heterogeneity of articles with regard to population, study design, measurement, and analysis. Given inconsistency in findings, we believe that a summary effect estimate, as offered by meta-analyses, would not reflect the impact of this heterogeneity on conclusions. Thus, a narrative summary of the results is presented below.
We organized the results by three types of negative affect: anxiety, depression, and internalizing symptoms. Within each of these types, we further structure our narrative around type of substance use because associations may vary by substance. As available, we reported findings for alcohol, tobacco, marijuana, illicit drugs, and composite measures of substance use. Illicit drugs included in identified studies were solvents, ecstasy, amphetamines, LSD, tranquilizers, cocaine or crack, heroin/methadone/opioids, barbiturates/sedatives, inhalants, hallucinogens, LSD, PCP, psilocybin; six of the studies had undefined hard/illicit drug use. Across articles, externalizing symptoms most often included disruptive behavior disorders (as an aggregate or separated by Conduct, Oppositional Defiant or Attention Deficit Hyperactivity Disorders), delinquency and aggression, or personality indicators such as impulsivity or sensation seeking (in addition to symptom measures). Symptoms were primarily based on self-reports but a few articles included teacher-report (5 in total), parent-report (14 in total), or peer report (1 in total). All articles had to report tests of the relation between negative affect symptoms and future substance use, controlling for externalizing symptoms, in the same model. All studies used prospective designs but varied in the time lag between assessments, reflecting a range from 3 months to 19 years (with a mode of one year). A total of 16 of the 61 articles identified contained clinical or high-risk samples and the remainder were community samples.
Each section summarizes individual tests of the associations of interest rather than single article findings. The limitation of this approach is that any given article could contribute more than one test and indeed a few articles used the same sample to test the association in slightly different ways. We considered the impact of this approach to summarizing the literature where appropriate in our results and discussion.
Results
Anxiety and Substance Use
Overview of Articles
Our review identified 63 tests of the association between anxiety and substance use controlling for externalizing behavior as reported in 16 studies. Of these tests, five (as reported in two articles) indicated that a positive unique association between anxiety and substance use was present, six (as reported in four articles) found a negative association, and the remaining 52 produced null findings (as reported in all but one article).
Alcohol
A total of 18 tests of the unique association between indicators of anxiety and alcohol use were identified in nine articles. Only one test found a positive association (Marmorstein, White, Loeber, & Stouthamer-Loeber, 2010) and four tests in three articles showed a negative anxiety-alcohol use association (Cerda et al., 2013; McCarty, Rhew, et al., 2012; Peeters et al., 2014).
The positive effect was reported by Marmorstein et al. (2010), who showed that generalized anxiety predicted greater risk for subsequent alcohol use in a male sample of 13–20 year olds, though generalized anxiety did not predict problem use and social anxiety did not predict use or problem use. Reporting tests showing a negative association, Cerda et al. (2010) found that greater anxiety symptoms and neuroticism were associated with a reduced likelihood of initiating alcohol use in males and Peeters et al. (2014) showed that higher anxiety sensitivity scores predicted a reduced likelihood of persistent alcohol use in a young adolescent sample of boys and girls. McCarty, Rhew et al. (2012) showed that greater separation and panic symptoms each predicted a reduced likelihood of initiating alcohol use in a young adolescent sample but social anxiety and somatization were unrelated to alcohol use, and none of these anxiety indicators predicted age of drinking onset.
The remaining tests reported null effects regarding the prediction of alcohol use disorders (Biederman, 1996) or alcohol use involvement as a function of anxiety disorders (Costello, Erkanli, Federman, & Angold, 1999; King, Iacono, & McGue, 2004) or anxiety symptoms (Dobkin, Tremblay, & McDuff, 1997; Little et al, 2013).
Tobacco
A total of 21 tests of the unique association between anxiety and tobacco use were identified in nine articles. One test reported a positive association (Marmorstein et al., 2010), two a negative association (both in Costello et al., 1999), and the remainder reported null findings (Brown, Lewinsohn, Seeley, & Wagner, 1996; Cornelius, Leech, Goldschmidt, & Day, 2005; Dieker, Avenevoli, Merikangas, Flaherty, & Stolar, 2001; Dobkin et al., 1997; Griesler, Hu, Schaffran, & Kandel, 2008; King et al., 2004; Marmorstein et al., 2010; Pederson & Von Soest, 2009).
Reporting a positive association, Marmorstein et al. (2010) showed that generalized but not social anxiety predicted greater risk for smoking behavior but not smoking-related problems. Reporting a negative association, Costello et al. (1999) showed that having an anxiety disorder was associated with a later age of smoking onset in both boys and girls but not with lifetime smoking.
Marijuana
A total of 12 tests of the unique association between anxiety and marijuana use were identified in five articles. Only one reported a positive association (Marmorstein et al., 2010) and the remainder reported null effects (Aseltine, Gore, & Gordon, 2000; Cerda et al., 2013; Costello et al., 1999; King et al., 2004). Contrasting with their findings for tobacco, Marmorstein et al. (2010) found that social but not generalized anxiety predicted greater risk for marijuana-related problems but not age of onset.
Illicit Drugs
A total of six tests of the unique association between anxiety and illicit drug use were identified in four articles; all reported null findings (Biederman, 1996; Costello et al., 1999; Dobkin et al., 1997; McCarty et al., 2012).
Composite Substance Use Scores
Six tests of the unique association between anxiety and composite scores of substance use were identified in two articles that both used the Great Smoky Mountain Study. One study reported two tests showing a positive association (Sung, Erkanli, Angold, & Costello, 2004) and the other reported null effects for four tests of this association (Costello et al., 1999). Sung et al. (2004) showed that anxiety disorders predicted substance use at age 16 but not earlier (ages 13–15), more so in girls than boys; Costello et al. (1999) did not examine the effect as a function of adolescent age and found no anxiety-substance use association.
Summary
A total of 16 articles provided 63 unique tests of the association between anxiety and substance use in adolescents after controlling for indicators of externalizing symptoms. Only two articles found a positive anxiety-use association (Marmorstein et al., 2010; Sung et al., 2004) and both articles used samples that also found no evidence of this association in other tests reported either in the same publication (Marmorstein et al., 2010) or in other publications with the same data set (e.g., Costello et al., 1999 and Sung et al., 2004). A negative association was found in four articles, each showing that anxiety indicators predicted lower risk for later drinking outcomes after controlling for externalizing symptoms. Articles reporting tests of anxiety as a predictor of drug use (n=4) found no evidence of an association. Overall, there was weak support for a main effect association between anxiety and substance use in adolescents, with as many effects suggesting that anxiety may be a protective factor as well as a risk factor for future substance use after controlling for externalizing symptoms.
Depression and Substance Use
Overview of Articles
Our review identified 113 tests of the unique association between depression and substance use as reported in 41 articles. Of these tests, 36 reported a positive association (as reported in 20 articles), one reported a negative association (reported in one article), and the remaining 78 reported null effects (in all but nine articles).
Alcohol
A total of 32 tests of the unique association between depression and alcohol use were identified in 22 articles. Ten effects found a positive association (Cerda et al., 2013; Costello et al., 1999; King et al., 2004; Kumpulainen, 2000; Leve, Harold, Van Ryzin, Elam, & Chamberlain, 2012; Pesola et al., 2015; Wu, et al., 2006; Wu et al., 2008) and the remaining effects were null. Regarding studies that examined depressive symptoms (rather than disorder) as a predictor, positive associations were found for a variety of alcohol use indicators. For example, in their sample of boys aged 7–19, Cerda et al. (2013) showed that depressive symptoms predicted earlier age of drinking onset; Wu et al. (2006) showed that depressive symptoms predicted alcohol initiation over two years among Puerto Rican youth who were abstainers at baseline; and Pesola et al. (2015) found that depressive symptoms predicted harmful drinking for both boys and girls in the United Kingdom. Two studies reported a positive association between depressive disorder and alcohol use (King et al, 2004; Costello et al, 1999). King et al. (2004) showed that adolescents with a depressive disorder had an earlier age of onset and regular use than their peers. Costello et al. (1999) found mixed effects of this association based on gender such that depressive disorders predicted later age of onset in 9–13 year-old girls but not boys as well as alcohol use in boys but not girls.
Other studies also showed mixed effects. Two articles by Kumpulainen and colleagues provide somewhat contradictory findings. Kumpulainen (2000) found that both parent- and teacher-reported depressive symptoms predicted heavy alcohol use at age 15 among Finnish youth after controlling for hyperactivity, relationship difficulties, and more general indicators of externalizing behavior, though the association between teacher-reported depressive symptoms and heavy alcohol use was stronger in boys than in girls. Using the same sample, Kumpulainen and Roine (2002) did not find a depression-alcohol use association using five factors derived from the Child’s Depression Inventory as predictors of heavy alcohol use after controlling for interpersonal problems and aggression. Only one factor (defined by ineffectiveness and low self-esteem) was associated with later heavy alcohol use and only in girls. Leve et al. (2012) found that girls in foster care with greater depressive symptoms at age 11 and faster increases in depression over two years drank more alcohol by age 13 but not in a second sample reported in the same article.
In addition to these mixed findings, several articles reported no association between depressive symptoms and alcohol use (Capaldi & Stoolmiller, 1999; Cortes, Fleming, Mason, & Catalano, 2008; Dishion, Capaldi, &Yoerger, 1999; Little et al., 2013; Maslowsky, Schulenberg, & Zucker, 2014; McCarty et al., 2012; McCarty, Wymbs, et al., 2012; Pardini, Lochman, & Wells, 2004; Saraceno, Heron, Munafo, Carddock, & van den Bree, 2012) and no articles found an association between depressive symptoms and alcohol use disorders (Adrian, McCarty, King, McCauley, & Vander Stoep, 2014; Biederman, 1996; Fergusson & Woodward, 2002; Miller-Johnson, Lochman, Coie, & Hyman, 1998; Tartter, Hammen, & Brennan, 2014) when controlling for externalizing symptoms.
Tobacco
A total of 37 tests of the unique association between depression and tobacco use were identified in 19 articles. Of these, 12 tests reported a positive association and all predicted tobacco use patterns rather than nicotine disorder (Brown et al., 1996; Cornelius et al., 2005; Costello et al., 1999; King et al., 2004; Leve et al., 2012; Maslowsky et al., 2014; Niemela et al., 2009; Park, Weaver, & Romer, 2009; Prinstein & La Greca, 2009; Weiss, Mouttapa, Cen, Johnson, & Unger, 2011).
Regarding articles that examined depressive symptoms as a predictor, positive associations were found for a variety of tobacco use indicators. For example, Weiss et al. (2011) showed that depressive symptoms predicted smoking initiation; Prinstein and La Greca (2009) and Niemela et al. (2009) both showed that depressive symptoms predicted more frequent smoking; and Leve et al. (2012) found that adolescents with greater depressive symptoms at age 11 and steeper increases in depressive symptoms over two years were more likely to engage in lifetime smoking.
In addition to these effects regarding depressive symptoms and tobacco use, three articles found positive associations between depressive disorders and tobacco use. Brown et al. (1996) found that adolescents with depressive disorders had an earlier age of smoking onset and Costello et al. (1999) showed that boys, but not girls, engaged in more frequent smoking. King et al. (2004) showed that adolescents with a depressive disorder had a greater chance of lifetime smoking than their peers but not a greater chance of engaging in regular or everyday smoking.
Other studies that found positive associations between depressive symptoms and tobacco use produced mixed effects. Park et al. (2009) found that depressive symptoms predicted increased risk for progression to temporary daily smoking but not to continued daily smoking. Cornelius et al. (2005) found that depressive symptoms increased risk for level of smoking in 14 year olds but not for lifetime smoking or an earlier age of onset. Maslowsky et al. (2014) found that depressive symptoms in Monitoring the Future eighth graders predicted increased cigarette use in 10th and 12th grade but tenth grade depressive symptoms did not predict 12th grade smoking.
In addition to these mixed results, several articles found no association between depressive symptoms and tobacco use (Capaldi & Stoolmiller, 1999; Dishion et al., 1999; Pedersen and Von Soest, 2009; Hu, Griesler, Schaffran, & Kandel, 2011; Miller-Johnson et al., 1998; Nargiso et al., 2012; Wu et al., 2008) and no articles reported an association between depressive disorders and nicotine disorders (out of three tests, Dierker et al., 2001; Griesler et al., 2008; Fergusson & Woodward, 2002) when controlling for externalizing symptoms.
Marijuana
A total of 16 tests of the unique association between depression and marijuana use were identified out of ten articles. Three tests reported a positive depression-marijuana use association (as reported in Costello et al., 1999 and Maslowsky et al., 2014). Costello et al. (1999) found that boys with a depressive disorder were at greater risk for using marijuana by age 13 and for an earlier age of onset. Maslowsky et al. (2014) showed mixed effects such that depressive symptoms in 10th grade predicted greater marijuana use in 12th grade, but 8th grade depressive symptoms were unrelated to 10th and 12th grade marijuana use after controlling for conduct problems.
In addition to these mixed results, several articles found no association between depressive symptoms and marijuana use after controlling for externalizing symptoms (Adrian et al., 2014; Capaldi & Stoolmiller, 1999; Cerda et al., 2013; Cortes et al., 2008; Dishion et al., 1999; King et al., 2004; Miller-Johnson et al., 1998; Tartter et al., 2014).
Illicit Drugs
A total of nine tests of the unique association between depression and illicit drug use were identified out of six articles. Two reported a positive depression-illicit drug use association. Costello et al. (1999) found that boys with a depressive disorder were at greater risk for using illicit drugs but not for an earlier age of drug use onset. Wu et al. (2008) found that depressive symptoms predicted an increase in illicit drug use among those who had initiated illicit substance use at baseline. Other tests reported null effects regarding the association between depressive symptoms and illicit drug use (Capaldi & Stoolmiller, 1999; McCarty, Rhew, et al., 2012) and the association between depressive disorders and illicit drug use disorders (Biederman, 1996; Tartter et al., 2014).
Composite Substance Use Scores
A total of 19 tests of unique association between depression and substance use scores that pooled across different types of drugs were identified out of ten articles. Nine tests reported a positive depression-substance use association (Costello et al., 1999; Henry et al., 1993; Mason, Hitchings, & Spoth, 2007; Mason, Hitch, Spoth, 2009; Sung et al., 2004), and one reported a negative depression-substance use association (Hersh, Curry, & Becker, 2013).
Analyzing the Dunedin Longitudinal Cohort Study, Henry et al. (1993) showed that depressive symptoms at age 11 predicted greater substance use at age 15 in boys, but not in girls. Studies by Mason and colleagues (Mason et al., 2007; Mason et al., 2009; Mason, Hitchings, & Spoth, 2008) found two positive effects out of three tests that controlled for conduct problems. These articles reported that depressive symptoms predicted overall substance use (Mason et al., 2009), problem use in girls but not in boys (Mason et al., 2007), and had no effect on substance use (Mason et al., 2008) although depressive symptoms interacted with conduct problems such that depression was negatively associated with substance use when conduct problems were high. Analyzing the Great Smoky Mountain Study, Costello et al. (1999) and Sung et al. (2004) also show mixed effects. Costello et al. (1999) reported that depressive disorders were associated with greater substance use but not with an earlier age of use or disorder onset. However, Costello et al. (1999) and Sung et al. (2004) reported that depressive disorders increased risk for later substance use disorder in boys, though not in girls.
In a treatment sample study that found a negative association between depression and substance, Hersh et al. (2013) reported that depressive symptoms predicted lower substance use problems, though not substance use frequency, at six-month follow-up but not at three months. This effect was moderated by conduct problems such that, as reported by Mason et al. (2008), depressive symptoms were negatively associated with substance use at high levels of conduct problems.
In addition to these mixed results, two articles found no association between depressive symptoms and composite measures of substance use after controlling for externalizing symptoms (Adrian et al., 2014; Bailey & McCloskey, 2005; Capaldi & Stoolmiller, 1999).
Summary
Evidence for a positive depression-substance use effect varies somewhat over type of drug. We found that 10 of 32 effects (31%) showed such an association between depression and alcohol use, a rate similar for tobacco use (12 of 37 effects, or 32%); the rate was somewhat higher for composite substance use outcomes (9 of 19 effects, or 47%) and somewhat lower for illicit drug use (2 of 9 effects, or 22%) and marijuana use (3 of 16 effects, or 19%). Negative associations between depression and substance use were isolated and reported in only one article of high-risk youth (Hersh et al., 2013).
Internalizing Symptoms and Substance Use
Overview of articles
Our review identified 51 tests of the unique association between internalizing symptoms (a broader construct encompassing both anxiety and depression) and substance use as reported in 17 articles. Of these tests, eight found a positive association (as reported in five articles), six found a negative association (as reported in five articles), and 39 produced null results (as reported in all but two articles).
Alcohol
A total of 16 tests of the unique association between internalizing symptoms and alcohol use were identified out of 9 articles. One reported a positive internalizing symptom-alcohol use association (Strandheim, Bratberg, Holmen, Coombest, & Betnzen, 2011), two reported a negative association (Niemala, 2006; Scalco et al., 2014), and the remaining eight found no association.
The only positive association was reported by Strandheim et al. (2011), who found that internalizing symptoms in 13–15 year olds predicted more frequent alcohol use four years later among females but not males, and only for those females who began drinking before the age of sixteen.
In contrast, Niemala (2006) found that greater internalizing symptoms predicted lower rates of drunkenness in a sample of 8–18 year-old boys. In addition, Scalco et al. (2014) found that internalizing symptoms in 11–12-year-old boys and girls predicted less alcohol involvement one year but not two years later. Using the same sample and a novel structural equation modeling analysis, Colder et al. (2013) showed that internalizing symptoms at ages 11–12 were not associated with alcohol use two years later after controlling for externalizing symptoms; however, co-occurring symptoms (high levels of both internalizing and externalizing symptoms) did predict later alcohol use.
Largely, these tests found internalizing symptoms to be a non-significant predictor of a variety of alcohol use outcomes (Englund & Siebenbrunner, 2012; Goodman, 2010; Kumpulainen, 2000; Schlauch et al., 2013; Stice, Barrera, & Chassin, 1998; Vitulano et al., 2014).
Tobacco
A total of ten tests of the unique association between internalizing symptoms and tobacco use were identified in seven articles. Three reported a positive internalizing symptom-tobacco use association (Goodman, 2010 and two from Vitulano et al., 2014), two reported a negative association (Colder et al., 2013; Fischer, Najman, Williams, & Clavarino, 2012), and five reported null effects (Goodman, 2010; Leff et al., 2003; Niemala et al., 2006; Schlauch et al., 2013).
Vitulano et al. (2014) found that internalizing symptoms predicted higher risk of initiation by ninth grade and a faster acceleration in smoking from fourth to ninth grade in a sample of children with elevated aggression who comprised the control group in an intervention study. Goodman (2010) also found that boys and girls elevated above diagnostic cut-offs for internalizing symptoms engaged in greater subsequent smoking behavior after controlling for externalizing symptoms.
In contrast, Fischer et al. (2012) used a community sample to show that greater internalizing symptoms at age 5 predicted lower risk for smoking at age 14 though not at age 21. Moreover, Colder et al. (2013) showed that internalizing symptoms at ages 11–12 predicted lower later risk for past year smoking frequency after controlling for externalizing symptoms, but co-occurring symptoms predicted higher risk for smoking. These findings suggest that externalizing symptoms moderate the association between internalizing symptoms and smoking behavior, serving to exacerbate risk for tobacco involvement. Adding to this complexity, in a clinical sample of adolescents, Schlauch et al. (2013) found no unique effect of internalizing symptoms on tobacco use overall but did find that internalizing symptoms were a risk factor for increased tobacco use over the period of a year for a subset of youth. Moderation analysis showed that this effect held only for those with low externalizing symptoms and low family involvement (compared to those with low externalizing symptoms and high family involvement) as well as for those with high externalizing symptoms and low family involvement. Thus, even in the absence of high externalizing symptoms, other moderators may exist that exacerbate the risk for tobacco involvement among youth high in internalizing symptoms.
Marijuana
A total of 13 tests of the unique association between internalizing symptoms and marijuana use were identified out of seven articles. One test reported a positive association (Fox, Towe, Stephens, Walker, & Roffman, 2011), two reported a negative association (Colder et al., 2013; Rogosch, Oshri, & Cichetti, 2010), and the remainder reported null effects (Englund et al., 2012; Goodman, 2010; Schlauch et al., 2013; Vitulano et al., 2014).
Fox et al. (2011) reported that internalizing symptoms predicted increased risk for problems with marijuana use three months after baseline in a sample of high school students participating in a brief intervention study; however, internalizing symptoms did not predict these problematic marijuana use outcomes one year later, nor did they predict marijuana use at either three or 12 months post-baseline.
In contrast, Rogosch et al. (2010) reported that a latent variable comprised of internalizing symptoms assessed at ages 13–15 predicted lower risk for symptoms of marijuana abuse/dependence at ages 15–18. Colder et al. (2013) also reported that internalizing symptoms predicted lower rates of marijuana use after controlling for externalizing and co-occurring symptoms; co-occurring symptoms were unrelated to marijuana use.
Illicit Drugs
Only one article tested the association between internalizing symptoms and illicit drug use while controlling for externalizing behaviors. Goodman (2010) extended the measurement of internalizing behaviors to include probability bands for diagnosis as well as clinical diagnoses but found no relationship between these diagnostic or traditional scale measures of internalizing behaviors and marijuana use.
Composite Substance Use Scores
A total of ten tests of the unique association between internalizing symptoms and substance use scores that pooled across different types of drugs were identified out of six articles. Three tests reported a positive internalizing symptom-substance use association (Loeber, Stouthamer-Loeber, & White, 1999; Strandheim et al., 2011) and the remainder reported null effects (Kaplow, Curran, Dodge & the Conduct Problems Prevention Resarch Group, 2002; Scalco et al., 2014; Schlauch et al., 2013; Skeer at al., 2011).
In a study of boys, Loeber et al. (1999) found that elevated internalizing behaviors in both middle and late childhood (but not adolescence) positively predicted adolescent substance use. Strandheim et al. (2011) also found a positive association between internalizing symptoms and lifetime substance use in boys, but not in girls; however, this finding only held for boys who had not initiated alcohol use by the age of sixteen as compared to their early drinking counterparts.
Summary
Across drugs, evidence for an association between internalizing symptoms and substance use was weak. Out of 51 effects tested, nine found a positive association and six a negative association. Two articles also found conditional effects of internalizing symptoms on substance use, although these articles used different methodologies and found different effects. Colder et al. (2013) reported that co-occurring internalizing and externalizing symptoms predicted greater risk for using alcohol and tobacco, but not marijuana, two years later. Schlauch et al. (2013) reported that internalizing symptoms were a stronger predictor of later alcohol use and tobacco use when family involvement was low.
Discussion
The key finding of this systematic review regarding the unique association between negative affect symptoms and substance use after controlling for externalizing symptoms is that a clear and consistent association is not evident across the multiple associations examined. This finding is not unexpected given the differing forms and measures of both negative affect symptoms and substance use and the multiple associations therein. Our review of 61 studies suggests variation in relations according to the type of negative affect symptoms and type of substance use, but even within particular associations, findings from the studies are mixed. Overall, however, we find that depression is a more consistent unique predictor of adolescent substance use after controlling for co-occurring externalizing symptoms than either anxiety or internalizing symptoms; findings regarding prediction of substance use by anxiety and internalizing symptoms are not compelling. We structure our discussion to highlight seven areas reflecting some coherence of findings and offer potential implications for future research.
First, as noted, evidence for a positive association between negative affect symptoms and substance use is considerably stronger for depression (considering all types of substance use, 36 of 113 effects; 32%) than it is for anxiety (5 of 63 effects; 8%) or internalizing symptoms (9 of 51 effects; 18%). Negative associations were rarely found, but were more common for anxiety (6 of 63 effects; 10%) and internalizing symptoms (6 of 51 effects; 12%) than for depression (1 of 113 effects; < 1%). One interpretation of these findings is that prediction of substance use is most consistently positive for depression but is either absent or equally positive and negative for anxiety and, therefore, for internalizing symptoms, which combine indicators of depression and anxiety symptoms. In addition, anxiety and internalizing symptoms may show less association with substance use outcomes than depression because anxiety may convey different forms of risk, owing to the target of distress. For example, Marmorstein et al. (2010) found that generalized, rather than social, anxiety was associated with greater risk for alcohol and tobacco use in boys (though social anxiety, and not generalized anxiety, predicted problems with marijuana). Thus, we recommend that future studies focus on depression and specific indices of anxiety as unique predictors of subsequent substance use rather than on aggregated indicators of negative affect symptoms
Second, the severity and not just the form of negative affect symptoms may impact the strength of this unique association. A critical mass of articles for examining this question was only available for depression-substance use associations. In these articles, 16 of 43 effects (37%, as reported in nine studies) reported a positive association whereas 20 of 70 effects (28%, as reported in 32 studies) reported no association. Although more severe indicators of depression may be more strongly associated with substance use, these effects may be harder to detect in high-risk and clinical samples that have a more restricted range of depression symptomatology as well as higher rates of comorbid disorders. Of nine studies that examined high-risk of clinical samples in the current review, only two found a positive depression-use association (22%) whereas 18 of 43 articles (43%) that examined community associations did so. Future studies would benefit from using designs and measures that capture the full range of symptom severity.
Third, although not a clear pattern, findings indicated that the unique association between negative affect symptoms and substance use after controlling for externalizing symptoms may also vary as a function of the type of drug use. Positive associations between negative affect symptoms and substance use were most consistent for composite substance use scores (14 of 35 effects; 40%), followed by tobacco (16 of 68 effects; 24%), alcohol (12 of 66 effects; 18%), marijuana use (6 of 41 effects; 15%), and illicit drug use (2 of 17 effects; 12%). One interpretation of the stronger effects of negative affect symptoms on composite substance use scores is that adolescents may use drugs to address negative affect symptoms largely as a function of availability. Specific types of drugs used by adolescents may be selected less for mood-enhancement or dampening effects per se as for availability at a given opportunity to use. In other words, perhaps adolescents use whichever substance they can access, and because they use for a variety of reasons, drug-specific patterns of use as related to negative affect symptoms may have yet to emerge. However, we should note that much less is known about the unique associations between negative affect symptoms and illicit drug use after controlling for externalizing symptoms due to a paucity of studies – this remains a fruitful area for exploration to determine whether there is drug specificity in this association.
Fourth, in addition to distinguishing across type of drug for understanding variation in the negative affect symptom-use association, we also examined articles in our review for differences in findings regarding extent of substance use engagement. Again turning to our largest group of studies that examined depression-alcohol use associations, we found greater support for this association in studies that predicted earlier onset (3 of 5 articles), followed by indicators of problem drinking (1 of 2 articles), indicators of overall use (3 of 10 articles), and then diagnostic outcomes (4 of 19 articles). Although there was an insufficient number of articles representing these potential points along a drinking continuum or drinking trajectories more broadly (such as McCarty et al., 2013) to draw conclusions at this point, future studies should consider variation in the negative affect symptom-use association over not just type of drugs used but also progression of drug involvement.
Fifth, moderation of relations between negative affect and substance use was reported in several studies; gender was of particular interest in this review. When present, gender differences appeared to be more complex than simple moderation hypotheses would predict. Focusing on our largest pool of studies testing the depression-use association, we found nineteen studies that tested gender differences or tested the association separately by gender. Six of these studies did not find a depression-substance use association regardless of gender. The remaining thirteen all found a positive depression-use association but gender differences were only evident in four of these studies with some studies finding stronger associations in boys (Costello et al., 1999; Sung et al., 2004; Kumpulainen, 2000) and others in girls (Mason et al., 2007). More nuanced models are needed to guide the study of how gender differences might emerge in this association over development.
Sixth, whether age functions as moderator was also of interest, with the findings suggesting a clear need for future research on the role of development in the negative affect symptom- substance use association over adolescence. For example, Miller-Johnson et al. (1998) showed that eighth graders who were above the mean on depression and conduct problems had higher rates of alcohol use than their peers who were elevated in conduct problems only, though this association did not hold for sixth or tenth graders. Maslowsky et al. (2014) also found that these associations were stronger in older than in younger teens. However, most studies included broad age ranges and did not test for age effects. Importantly, although a few studies indicated that depression-substance use associations were evident in younger and not older cohorts, the wide age bands used in most studies and lack of age moderation tests did not permit conclusions regarding developmental trends in this association.
Seventh, comorbid externalizing symptoms emerged from the review as a potential moderator. The risk for substance use associated with negative affect symptoms may only occur in the presence of comorbid externalizing symptoms, suggesting that these two symptom clusters interact to exacerbate risk for substance use. Or, perhaps risk for substance use is present only in the absence of externalizing symptoms, when coping may be more dominant among the potential motives for using and thus strengthen the association between negative affect symptoms and substance use (Hussong et al., 2011). Some evidence for each of these interactions were evident in articles included in this review. Tests that pit mechanisms that may underlie these opposing patterns of risk for comorbid internalizing and externalizing symptoms (e.g., the dual failure model and negative affect impulsivity models that involve negative urgency versus pure self-medication models) are clearly needed.
There are some limitations to the current review. First, we considered individual tests of the associations of interest as our level of analysis rather than study-level associations, although we made connections between the two throughout. In addition, the review lacks the inferential power of a meta-analysis despite the large number of studies, though we assert that due to the small number of studies within any given combination of negative affect symptoms and type of substance use, a qualitative review is more appropriate.
In conclusion, the review suggests that the association between negative affect symptoms and adolescent substance use after controlling for co-occurring externalizing symptoms is not invariant across the specific associations falling under this umbrella. Depression emerged as the most consistent unique predictor of substance use—particularly of alcohol, tobacco, and composite measures of substance use.
Even so, the findings regarding the depression-substance use association are mixed and call for greater attention to the potential moderating factors that may help define who, when, and in what context depression serves as an important risk factor for later substance use above and beyond risk associated with externalizing symptoms. The current review offers a number of directions for future research that could clarify this association.
Supplementary Material
Acknowledgments
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health through grant funding awarded to Dr. Hussong (R01 DA037215) and Dr. Ennett (R01 DA13459).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Contents of this manuscript have not presented or submitted elsewhere.
References
- Adrian M, McCarty C, King K, McCauley E, Stoep A Vander. The internalizing pathway to adolescent substance use disorders: Mediation by ruminative reflection and ruminative brooding. Journal of Adolescence. 2014;37(7):983–991. doi: 10.1016/j.adolescence.2014.07.010. http://doi.org/10.1016/j.adolescence.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):S0021963098003448. http://doi.org/10.1017/S0021963098003448. [PubMed] [Google Scholar]
- Aseltine RH, Gore S, Gordon J. Life stress, anger and anxiety, and delinquency: an empirical test of general strain theory. Journal of Health and Social Behavior. 2000;41(3):256–275. http://doi.org/10.2307/2676320. [PubMed] [Google Scholar]
- Bailey JA, McCloskey LA. Pathways to Adolescent Substance Use Among Sexually Abused Girls. Journal of Abnormal Child Psychology. 2005;33(1):39–53. doi: 10.1007/s10802-005-0933-0. http://doi.org/10.1007/s10802-005-0933-0. [DOI] [PubMed] [Google Scholar]
- Biederman J. A Prospective 4-Year Follow-up Study of Attention-Deficit Hyperactivity and Related Disorders. Archives of General Psychiatry. 1996;53(5):437. doi: 10.1001/archpsyc.1996.01830050073012. http://doi.org/10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(12):1602–1610. doi: 10.1097/00004583-199612000-00011. http://doi.org/10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Development and Psychopathology. 1999;11(1):S0954579499001959. doi: 10.1017/s0954579499001959. http://doi.org/10.1017/S0954579499001959. [DOI] [PubMed] [Google Scholar]
- Cerdá M, Bordelois PM, Keyes KM, Galea S, Koenen KC, Pardini D. Cumulative and recent psychiatric symptoms as predictors of substance use onset: does timing matter? Addiction. 2013;108(12):2119–2128. doi: 10.1111/add.12323. http://doi.org/10.1111/add.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Sher KA, Hussong AM, Curran PJ. The developmental psychopathology of alcohol use and alcohol disorders: Research achievements and future directions. Development and Psychopathology. 2013;25(4 Pt 2):1567–1584. doi: 10.1017/S0954579413000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Sher KA, Colder CR, Hussong AM. Substance use and substance use disorder. In: Cicchetti D, editor. Developmental Psychopathology, Volume III: Maladaptation and psychopathology. Hoboken, NJ: Wiley and Sons, Inc; 2016. pp. 833–897. [DOI] [Google Scholar]
- Colder CR, Chassin L, Lee MR, Villalta IK. Developmental perspectives: Affect and adolescent substance use. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 109–135. http://doi.org/10.1037/12067-005. [Google Scholar]
- Colder CR, Scalco M, Trucco EM, Read JP, Lengua LJ, Wieczorek WF, Hawk LW. Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. Journal of Abnormal Child Psychology. 2013;41(4):667–677. doi: 10.1007/s10802-012-9701-0. http://doi.org/10.1007/s10802-012-9701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Cornelius MD, Leech SL, Goldschmidt L, Day NL. Is prenatal tobacco exposure a risk factor for early adolescent smoking? A follow-up study. Neurotoxicology and Teratology. 2005;27(4):667–676. doi: 10.1016/j.ntt.2005.05.006. http://doi.org/10.1016/j.ntt.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Cortes RC, Fleming CB, Mason WA, Catalano RF. Risk Factors Linking Maternal Depressed Mood to Growth in Adolescent Substance Use. Journal of Emotional and Behavioral Disorders. 2008;17(1):49–64. doi: 10.1177/1063426608321690. http://doi.org/10.1177/1063426608321690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of Psychiatric Comorbidity With Substance Abuse in Adolescents: Effects of Timing and Sex. Journal of Clinical Child Psychology. 1999;28(3):298–311. doi: 10.1207/S15374424jccp280302. http://doi.org/10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Dierker LC, Avenevoli S, Merikangas KR, Flaherty BP, Stolar M. Association Between Psychiatric Disorders and the Progression of Tobacco Use Behaviors. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(10):1159–1167. doi: 10.1097/00004583-200110000-00009. http://doi.org/10.1097/00004583-200110000-00009. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Capaldi DM, Yoerger K. Middle Childhood Antecedents to Progressions in Male Adolescent Substance Use: An Ecological Analysis of Risk and Protection. Journal of Adolescent Research. 1999;14(2):175–205. http://doi.org/10.1177/0743558499142003. [Google Scholar]
- Dobkin PL, Tremblay RE, Mcduff P. Can Childhood Behavioural Characteristics Predict Adolescent Boys’ Health? Journal of Health Psychology. 1997;2(4):445–456. doi: 10.1177/135910539700200402. http://doi.org/10.1177/135910539700200402. [DOI] [PubMed] [Google Scholar]
- Englund MM, Siebenbruner J. Developmental pathways linking externalizing symptoms, internalizing symptoms, and academic competence to adolescent substance use. Journal of Adolescence. 2012;35(5):1123–1140. doi: 10.1016/j.adolescence.2012.03.004. http://doi.org/10.1016/j.adolescence.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. http://doi.org/10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Fischer JA, Najman JM, Williams GM, Clavarino AM. Childhood and adolescent psychopathology and subsequent tobacco smoking in young adults: findings from an Australian birth cohort. Addiction. 2012;107(9):1669–1676. doi: 10.1111/j.1360-0443.2012.03846.x. http://doi.org/10.1111/j.1360-0443.2012.03846.x. [DOI] [PubMed] [Google Scholar]
- Fox CL, Towe SL, Stephens RS, Walker DD, Roffman RA. Motives for cannabis use in high-risk adolescent users. Psychology of Addictive Behaviors. 2011;25(3):492–500. doi: 10.1037/a0024331. http://doi.org/10.1037/a0024331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman A. Substance use and common child mental health problems: Examining longitudinal associations in a British sample. Addiction. 2010;105(8):1484–1496. doi: 10.1111/j.1360-0443.2010.02981.x. http://doi.org/10.1111/j.1360-0443.2010.02981.x. [DOI] [PubMed] [Google Scholar]
- Graber JA, Sontag LM. Internalizing problems in adolescence. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology: Vol. 1, Individual bases of adolescent development. 3. Hoboken, NJ: Wiley; 2009. pp. 642–682. [Google Scholar]
- Griesler P, Hu MC, Schaffran C, Kandel D. Comorbidity of psychiatric disorders and nicotine dependence among adolescents: findings from a prospective, longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(11):1340–1350. doi: 10.1097/CHI.0b013e318185d2ad. http://doi.org/10.1097/CHI.0b013e318185d2ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry B, Feehan M, McGee R, Stanton W, Moffitt TE, Silva P. The importance of conduct problems and depressive symptoms in predicting adolescent substance use. Journal of Abnormal Child Psychology. 1993;21(5):469–480. doi: 10.1007/BF00916314. http://doi.org/10.1007/BF00916314. [DOI] [PubMed] [Google Scholar]
- Hersh J, Curry JF, Becker SJ. The Influence of Comorbid Depression and Conduct Disorder on MET/CBT Treatment Outcome for Adolescent Substance Use Disorders. International Journal of Cognitive Therapy. 2013;6(4):325–341. doi: 10.1521/ijct.2013.6.4.325. http://doi.org/10.1521/ijct.2013.6.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu MC, Griesler P, Schaffran C, Kandel D. Risk and protective factors for nicotine dependence in adolescence. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2011;52(10):1063–72. doi: 10.1111/j.1469-7610.2010.02362.x. http://doi.org/10.1111/j.1469-7610.2010.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25(3):390–404. doi: 10.1037/a0024519. http://doi.org/10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Rothenberg WA, Smith RK, Haroon M. Implications of heterogeneity in alcohol use disorders for understanding developmental pathways and prevention programming. To appear. In: Fitzgerald HE, Puttler LI, editors. Developmental perspectives on alcohol and other addictions over the life course. Oxford Press; (in press) [Google Scholar]
- Kaplan HB. Deviant Behavior in Defense of Self. New York: Academic Press; 1980. [Google Scholar]
- Kaplow JB, Curran PJ, Dodge KA Conduct Problems Prevention Research Group. Child, Parent, and Peer Predictors of Early-Onset Substance Use: A Multisite Longitudinal Study. Journal of Abnormal Child Psychology. 2002;30(3):199–216. doi: 10.1023/a:1015183927979. http://doi.org/10.1023/A:1015183927979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel JD, Hussong AM, Wardle MC, Veilleux JC, Heinz A, Greenstein JE, Evatt DP. Affective influences in drug use etiology. In: Scheier L, editor. Handbook of drug use etiology: Theory, methods, and empirical findings. Washington, DC: American Psychological Association; 2010. pp. 183–205. [Google Scholar]
- Khantzian EJ. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harvard Review of Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. http://doi.org/10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99(12):1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. http://doi.org/10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Kumpulainen K. Psychiatric symptoms and deviance in early adolescence predict heavy alcohol use 3 years later. Addiction. 2000;95(12):1847–1857. doi: 10.1046/j.1360-0443.2000.9512184713.x. http://doi.org/10.1080/09652140020011144. [DOI] [PubMed] [Google Scholar]
- Kumpulainen K, Roine S. Depressive symptoms at the age of 12 years and future heavy alcohol use. Addictive Behaviors. 2002;27(3):425–436. doi: 10.1016/s0306-4603(01)00182-4. http://doi.org/10.1016/S0306-4603(01)00182-4. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25(7):841–861. doi: 10.1016/j.cpr.2005.06.002. http://doi.org/10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Leff MK, Moolchan ET, Cookus BA, Spurgeon L, Evans LA, London ED, … Ernst M. Predictors of smoking initiation among at risk youth: A controlled study. Journal of Child & Adolescent Substance Abuse. 2003;1(1):59–75. http://doi.org/10.1300/J029v13n01_04. [Google Scholar]
- Leve LD, Harold GT, Van Ryzin MJ, Elam K, Chamberlain P. Girls’ tobacco and alcohol use during early adolescence: prediction from trajectories of depressive symptoms across two studies. Journal of Child & Adolescent Substance Abuse. 2012;21(3):254–272. doi: 10.1080/1067828X.2012.700853. http://doi.org/10.1080/1067828X.2012.700853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little K, Hawkins MT, Sanson A, O’Connor M, Toumbourou JW, Smart D, Vassallo S. Longitudinal predictors of alcohol-related harms during the transition to adulthood. Australian Psychologist. 2013;48(4):270–280. http://doi.org/10.1111/j.1742-9544.2012.00095.x. [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999;28(3):322–332. doi: 10.1207/S15374424jccp280304. http://doi.org/10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, White HR, Loeber R, Stouthamer-Loeber M. Anxiety as a predictor of age at first use of substances and progression to substance use problems among boys. Journal of Abnormal Child Psychology. 2010;38(2):211–224. doi: 10.1007/s10802-009-9360-y. http://doi.org/10.1007/s10802-009-9360-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslowsky J, Schulenberg JE, Zucker RA. Influence of conduct problems and depressive symptomatology on adolescent substance use: developmentally proximal versus distal effects. Developmental Psychology. 2014;50(4):1179–1189. doi: 10.1037/a0035085. http://doi.org/10.1037/a0035085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitch JE, Spoth RL. Longitudinal relations among negative affect, substance use, and peer deviance during the transition from middle to late adolescence. Substance Use & Misuse. 2009;44:1142–1159. doi: 10.1080/10826080802495211. http://doi.org/10.1080/10826080802495211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. Emergence of delinquency and depressed mood throughout adolescence as predictors of late adolescent problem substance use. Psychology of Addictive Behaviors. 2007;21(1):13–24. doi: 10.1037/0893-164X.21.1.13. http://doi.org/10.1037/0893-164X.21.1.13. [DOI] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. The interaction of conduct problems and depressed mood in relation to adolescent substance involvement and peer substance use. Drug and Alcohol Dependence. 2008;96(3):233–248. doi: 10.1016/j.drugalcdep.2008.03.012. http://doi.org/10.1016/j.drugalcdep.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DE, Curtin JJ, Piper ME, Baker TB. Negative reinforcement: Possible clinical implications of an integrative model. In: Kassel JD, editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 15–42. http://doi.org/10.1037/12067-001. [Google Scholar]
- McCarty CA, Rhew IC, Murowchick E, McCauley E, Vander Stoep A. Emotional health predictors of substance use initiation during middle school. Psychology of Addictive Behaviors. 2012;26(2):351–357. doi: 10.1037/a0025630. http://doi.org/10.1037/a0025630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73(3):444–53. doi: 10.15288/jsad.2012.73.444. http://dx.doi.org/10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, Mason WA, King KM, McCauley E, Baer J, Vander Stoep A. Early adolescent growth in depression and conduct problem symptoms as predictors of later substance use impairment. Journal of Child Psychology. 2013;41:1041–1051. doi: 10.1007/s10802-013-9752-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: Substance use outcomes across adolescence. Journal of Abnormal Child Psychology. 1998;26(3):221–232. doi: 10.1023/a:1022676302865. http://doi.org/10.1023/A:1022676302865. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberatti A, Tetzlaff J, Altman D PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Nargiso JE, Becker SJ, Wolff JC, Uhl KM, Simon V, Spirito A, Prinstein MJ. Psychological, peer, and family influences on smoking among an adolescent psychiatric sample. Journal of Substance Abuse Treatment. 2012;42(3):310–318. doi: 10.1016/j.jsat.2011.07.010. http://doi.org/10.1016/j.jsat.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann CS, Vitacco M, Robertson A, Sewell K. Longitudinal Assessment of Callous/Impulsive Traits, Substance Abuse, and Symptoms of Depression in Adolescents. Annals of the New York Academy of Sciences. 2003;1008(1):276–280. doi: 10.1196/annals.1301.031. http://doi.org/10.1196/annals.1301.031. [DOI] [PubMed] [Google Scholar]
- Niemela S, Sourander A, Pilowsky DJ, Susser E, Helenius H, Piha J, … Almqvist F. Childhood antecedents of being a cigarette smoker in early adulthood. The Finnish “From a Boy to a Man” Study. Journal of Child Psychology and Psychiatry. 2009;50(3):343–351. doi: 10.1111/j.1469-7610.2008.01968.x. http://doi.org/10.1111/j.1469-7610.2008.01968.x. [DOI] [PubMed] [Google Scholar]
- Niemela S, Sourander A, Poikolainen K, Helenius H, Sillanmaki L, Parkkola K, … Moilanen I. Childhood predictors of drunkenness in late adolescence among males: a 10-year population-based follow-up study. Addiction. 2006;101(4):512–521. doi: 10.1111/j.1360-0443.2006.01381.x. http://doi.org/10.1111/j.1360-0443.2006.01381.x. [DOI] [PubMed] [Google Scholar]
- Pardini D, Lochman J, Wells K. Negative emotions and alcohol use initiation in high-risk boys: The moderating effect of good inhibitory control. Journal of Abnormal Child Psychology. 2004;32(5):505–518. doi: 10.1023/b:jacp.0000037780.22849.23. http://doi.org/10.1023/B:JACP.0000037780.22849.23. [DOI] [PubMed] [Google Scholar]
- Park S, Weaver TE, Romer D. Predictors of the transition from experimental to daily smoking among adolescents in the United States. Journal for Specialists in Pediatric Nursing. 2009;14(2):102–111. doi: 10.1111/j.1744-6155.2009.00183.x. http://doi.org/10.1111/j.1744-6155.2009.00183.x. [DOI] [PubMed] [Google Scholar]
- Pedersen W, Von Soest T. Smoking, nicotine dependence and mental health among young adults: A 13-year population-based longitudinal study. Addiction. 2009;104(1):129–137. doi: 10.1111/j.1360-0443.2008.02395.x. http://doi.org/10.1111/j.1360-0443.2008.02395.x. [DOI] [PubMed] [Google Scholar]
- Peeters M, Monshouwer K, van de Schoot R, Janssen T, Vollebergh WA, Wiers RW. Personality and the prediction of high-risk trajectories of alcohol use during adolescence. Journal of studies on alcohol and drugs. 2014;75(5):790–798. doi: 10.15288/jsad.2014.75.790. http://doi.org/10.15288/jsad.2014.75.790. [DOI] [PubMed] [Google Scholar]
- Pesola F, Shelton KH, Heron J, Munafò M, Maughan B, Hickman M, van den Bree MB. The mediating role of deviant peers on the link between depressed mood and harmful drinking. Journal of Adolescent Health. 2015;56(2):153–159. doi: 10.1016/j.jadohealth.2014.10.268. http://doi.org/10.1016/j.jadohealth.2014.10.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, La Greca AM. Childhood depressive symptoms and adolescent cigarette use: a six-year longitudinal study controlling for peer relations correlates. Health Psychology. 2009;28(3):283–291. doi: 10.1037/a0013949. http://doi.org/10.1037/a0013949. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology. 2010;22(04):883–897. doi: 10.1017/S0954579410000520. http://doi.org/10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraceno L, Heron J, Munafò M, Craddock N, van den Bree M. The relationship between childhood depressive symptoms and problem alcohol use in early adolescence: findings from a large longitudinal population-based study. Addiction. 2012;107(3):567–577. doi: 10.1111/j.1360-0443.2011.03662.x. http://doi.org/10.1111/j.1360-0443.2011.03662.x. [DOI] [PubMed] [Google Scholar]
- Scalco MD, Colder CR, Hawk LW, Read JP, Wieczorek WF, Lengua LJ. Internalizing and externalizing problem behavior and early adolescent substance use: a test of a latent variable interaction and conditional indirect effects. Psychology of Addictive Behaviors. 2014;28(3):828–40. doi: 10.1037/a0035805. http://doi.org/10.1037/a0035805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlauch RC, Levitt A, Connell CM, Kaufman JS. The moderating effect of family involvement on substance use risk factors in adolescents with severe emotional and behavioral challenges. Addictive Behaviors. 2013;38(7):2333–2342. doi: 10.1016/j.addbeh.2013.02.010. http://doi.org/10.1016/j.addbeh.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer MR, McCormick MC, Normand SLT, Mimiaga MJ, Buka SL, Gilman SE. Gender differences in the association between family conflict and adolescent substance use disorders. Journal of Adolescent Health. 2011;49(2):187–192. doi: 10.1016/j.jadohealth.2010.12.003. http://doi.org/10.1016/j.jadohealth.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Barrera M, Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: examining the mechanisms of effect. Journal of Abnormal Psychology. 1998;107(4):616–628. doi: 10.1037//0021-843x.107.4.616. http://doi.org/10.1037/0021-843X.107.4.616. [DOI] [PubMed] [Google Scholar]
- Strandheim A, Bratberg GH, Holmen TL, Coombes L, Bentzen N. The influence of behavioural and health problems on alcohol and drug use in late adolescence - a follow up study of 2 399 young Norwegians. Child and Adolescent Psychiatry and Mental Health. 2011;5(1):17. doi: 10.1186/1753-2000-5-17. http://doi.org/10.1186/1753-2000-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug and Alcohol Dependence. 2004;75(3):287–299. doi: 10.1016/j.drugalcdep.2004.03.013. http://doi.org/10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tartter M, Hammen C, Brennan P. Externalizing disorders in adolescence mediate the effects of maternal depression on substance use disorders. Journal of Abnormal Child Psychology. 2014;42(2):185–194. doi: 10.1007/s10802-013-9786-0. http://doi.org/10.1007/s10802-013-9786-0. [DOI] [PubMed] [Google Scholar]
- Vitulano ML, Fite PJ, Hopko DR, Lochman J, Wells K, Asif I. Evaluation of underlying mechanisms in the link between childhood ADHD symptoms and risk for early initiation of substance use. Psychology of Addictive Behaviors. 2014;28(3):816–827. doi: 10.1037/a0037504. http://doi.org/10.1037/a0037504. [DOI] [PubMed] [Google Scholar]
- Weiss JW, Mouttapa M, Cen S, Johnson CA, Unger J. Longitudinal effects of hostility, depression, and bullying on adolescent smoking initiation. Journal of Adolescent Health. 2011;48(6):591–596. doi: 10.1016/j.jadohealth.2010.09.012. http://doi.org/10.1016/j.jadohealth.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Bird HR, Liu X, Fan B, Fuller C, Shen S, … Canino GJ. Childhood depressive symptoms and early onset of alcohol use. Pediatrics. 2006;118(5):1907–1915. doi: 10.1542/peds.2006-1221. http://doi.org/10.1542/peds.2006-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Liu X, Fuller CJ, Fan B, Musa G, … Cook JA. The relationship between depressive symptom levels and subsequent increases in substance use among youth with severe emotional disturbance. Journal of Studies on Alcohol and Drugs. 2008;69(4):520–7. doi: 10.15288/jsad.2008.69.520. http://dx.doi.org/10.15288/jsad.2008.69.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.