Abstract
Although it is well established that HIV-related stigma, depression, and lack of social support are negatively associated with health-related quality of life (HRQoL) among people living with HIV (PLH), no studies to date have examined how these psychosocial factors interact with each other and affect HRQoL among incarcerated PLH. We, therefore, incorporated a moderated mediation model (MMM) to explore whether depression mediates the effect of HIV-related stigma on HRQoL as a function of the underlying level of social support. Incarcerated HIV-infected men with opioid dependence (N=301) were recruited from the HIV units in Kajang prison in Malaysia. Participants completed surveys assessing demographic characteristics, HIV-related stigma, depression, social support, and HRQoL. Results showed that the effect of HIV-related stigma on HRQoL was mediated via depression (a1:β=0.1463, p<0.001; b1:β=−0.8392, p<0.001), as demonstrated by the two-tailed significance test (Sobel z=−3.8762, p<0.001). Furthermore, the association between social support and HRQoL was positive (β=0.4352, p=0.0433), whereas the interaction between HIV-related stigma and depression was negatively associated with HRQOL (β=−0.0317, p=0.0133). This indicated that the predicted influence of HIV-related stigma on HRQoL via depression had negative effect on HRQoL for individuals with low social support. The results suggest that social support can buffer the negative impact of depression on HRQoL and highlights the need for future interventions to target these psychosocial factors in order to improve HRQoL among incarcerated PLH.
Keywords: Prisoners, HIV-related stigma, depression, social support, health-related quality of life
Background
HIV continues to be a major global public health issue, with more than 36 million people living with HIV (PLH) at the end of 2015 [1]. The HIV epidemic in Malaysia remains volatile and one of only a few countries in the world where mortality continues to increase [2], primarily related to inadequate access to harm reduction services and antiretroviral therapy (ART). With over 100,000 cumulative HIV cases [3], Malaysia’s rapidly expanding HIV epidemic is the fifth largest in the Asia-Pacific region and concentrated within the most-at-risk populations, especially among people who inject drugs (PWID). The epidemics of HIV and injection drug use are intertwined in Malaysia [4, 5], with an estimated HIV prevalence of 12.5%–19.2% among PWID [6, 7], who are disproportionally concentrated within the criminal justice system (CJS) due to harsh criminalization for drug use. Results from mandatory HIV testing of the approximately 40,000 prisoners in Malaysia documents HIV prevalence to be 10–15 times greater (4.6% vs. 0.40%) than in the general population [8, 9].
Alongside challenges in medically managing their disease, PLH face other issues, such as HIV-related stigma, depression, and lack of social support. In Malaysia, as in many countries, HIV-related stigma is both a cause and consequence of limited access to HIV prevention and treatment [10]. Incarcerated PLH, the majority of whom are PWID [11], may face stigma and discrimination due to the ‘triple burden’ of HIV-infection, drug use, and incarceration [12]. Moreover, Malaysian physicians are unlikely to prescribe ART to several key populations, including PWID and recently released prisoners [13], which undermines HIV treatment as prevention strategies. Although attitudes toward PLH have improved in recent years [14], the insidious effects of stigma are still prevalent in Malaysia, and in most of the world [8, 15].
Prior research has shown that HIV-related stigma can severely compromise the health-related quality of life (HRQoL) of PLH, particularly among incarcerated individuals, by reducing access to quality care [16–19]. Furthermore, HIV-related stigma has been associated with poor medication adherence, contributing to high morbidity and high mortality [18, 19]. It is possible that HIV stigma isolates PLH from family and community support, and creates cultural barriers that inhibit integration into social networks [20]. As a result, PLH are more likely to be depressed and anxious, and report feelings of loss of interest, feelings of worthlessness and hopelessness, and recurrent suicidal ideation [14, 21]. In addition, depression is common among PLH, with the global prevalence ranging from 30% to 79% [22–25]. In Malaysia, notably high rates of depressive symptoms were observed among HIV-seropositive male prisoners [26]. Thus, the cumulative impact of depressive symptoms may disrupt the daily life and self-management activities of PLH, particularly among prisoners, significantly affecting their HRQoL [16, 18, 19, 26–29].
For many PLH, coping with HIV may be facilitated by their social support networks [30]. Previous studies on the impact of social support among PLH, mostly incarcerated individuals, suggest that it is an important resource that buffers and allows people to manage stress-related crises, such as depression, and thus, potentially improves HRQoL [17, 31–36]. Research has established that better social support from family members, friends, and healthcare providers predicts higher HRQoL [37, 38]. In addition, prior studies have shown that perceived social support is inversely associated with levels of perceived stigma [39–41]. Taken together, the social support of PLH has critical public health implications because it has a significant impact on health outcomes, including reducing depression, improving coping with their disease, increasing positive health behaviors, and slowing disease progression [30, 42]. It is, however, important to note that changes in social network during incarceration may reflect upon individuals’ strength of support, network characteristics, and the types of support offered or gained [35]. These factors may play different roles in an incarcerated PLH’s depression course, substance use recovery, overall treatment outcomes, and reentry efforts [35, 36, 43–45].
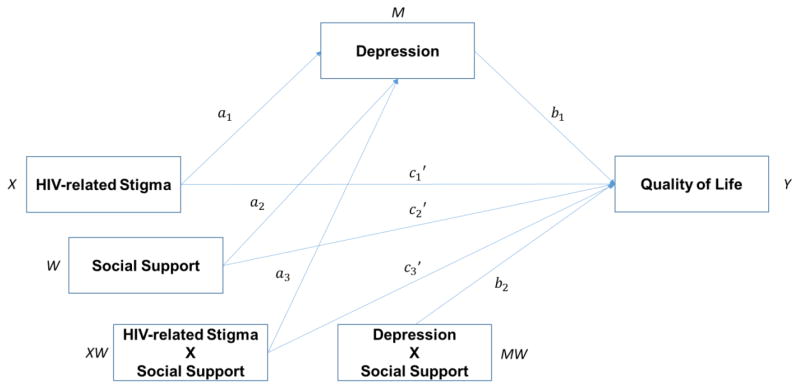
Though we recognize that HIV-related stigma, depression, and social support are significantly associated with HRQoL among PLH, little is known regarding the extent to which these psychosocial factors play a role among incarcerated PLH in Malaysia. Furthermore, no studies have explored precisely how these psychosocial factors interact with HRQoL when considered together among incarcerated PLH. A better understanding of the possible mechanism of how these factors function is critical to develop future programs designed to improve HRQoL of incarcerated PLH. In the present study, we therefore sought to explore whether depression mediates the effect of HIV-related stigma on HRQoL as a function of the underlying level of social support among incarcerated HIV-positive men transitioning to the community (see Figure 1). The hypotheses tested in the study include: 1) HIV-related stigma will be inversely associated with HRQoL; 2) HIV-related stigma will be positively associated with depression; 3) Depression will be inversely associated with HRQoL; 4) Depression will mediate the relationship between HIV-related stigma and HRQoL; and 5) Social support will moderate the mediation effect of depression on the relationship between HIV-related stigma and HRQoL.
Figure 1.
The proposed conceptual diagram of moderated mediation model in the study
Methods
Baseline data from Project Harapan (collected January 2010 – December 2014) was used to perform secondary data analysis in order to examine the relationships between HIV-related stigma, depression, social support, and HRQoL in the study population. Project Harapan was a 2×2 multi-factorial randomized controlled trial designed to evaluate and compare the relative effectiveness of a pre-release methadone maintenance program and an evidence-based behavioral intervention (Holistic Health Recovery Program, HHRP+) in terms of reducing HIV-related risk behaviors and illicit drug use for HIV-infected, opioid dependent prisoners in Malaysia [46].
The protocol for the parent study was approved by institutional review boards at the University Malaya Medical Centre and Yale University. The protocol was also reviewed and approved by the Office of Human Research Protection at the US Department of Health and Human Services (DHHS) as it involved federally-funded research with prisoners. The study is registered at www.clinicaltrials.gov (NCT02396979).
Participants
This analysis includes 301 incarcerated HIV-positive men with opioid dependence who were recruited at Kajang prison located in Greater Kuala Lumpur. Study eligibility criteria included i) age ≥ 18 years; ii) HIV-infected; iii) pre-incarceration opioid dependence using DSM-IV criteria; iv) Malaysian citizen; and v) due to be released in the Greater Kuala Lumpur area within three – six months.
Settings and procedures
Malaysia’s incarceration rate is 171 per 100,000 people, with approximately 39,000 sentenced prisoners located in 35 prisons nationwide [47]. All sentenced prisoners undergo mandatory HIV testing upon entry and all PLH are segregated into a dedicated HIV unit. HIV prevalence in the prison system is approximately 2%, 5-fold higher than in the general population, and prevalence in the Kajang prison is even higher at 5% [48–50]. At the time of this study, Kajang Prison, the country’s largest prison, had an average daily census of 4,435 prisoners, of which 412 (9.3%) were HIV-seropositive. Additionally, prior research has shown high rates of lifetime psychiatric disorders among both HIV-seropositive (44.0%) and HIV-seronegative (38.5%) prisoners [26].
The prison has an inpatient and outpatient medical unit. HIV care was initially provided by Ministry of Health clinicians in the prison clinic and later also by study clinicians [51]. All PLH, regardless of study participation, received CD4 and viral load testing and a comprehensive clinical assessment and medical record review. Despite high prevalence of mental illness, no psychiatric services were available onsite. Severely ill patients are transferred to a local hospital for treatment. Upon release, study participants were provided written referrals to their choice of one of Kuala Lumpur’s few public or private HIV specialty clinics. All first-line ART medications are fully subsidized by the Ministry of Health.
The prison officials assigned to the HIV unit referred HIV-positive men who were listed as 90–180 days pre-release to study personnel. All interested individuals were screened in a private room for eligibility. Patients who met inclusion criteria, and who were willing to participate as subjects, were provided a description of the study and invited to provide informed consent, followed by a baseline assessment. All interviews were completed face-to-face in a private room without prison personnel by research assistants using standardized instruments that were translated to Bahasa Malaysia, back-translated and adapted to the Malaysian context [52]. Prisoners were not compensated for their time within prison, but were for all post-release interviews.
Measures
Demographic variables
Data collected included characteristics of the participants, such as age, sex, ethnicity, religion, marital status, educational status, employment status, sex- and drug-related practices, type of offence for current incarceration, length of current incarceration, visit to psychiatrist prior to incarceration, duration since HIV diagnosis, and currently on ART, and CD4+ count.
HIV-related stigma
Participants’ perceived HIV-related stigma was assessed using the Berger HIV Stigma Scale [53], which is a 40-item instrument developed to measure the stigma perceived by PLH in the United States, and has been widely used in other cultural contexts [54, 55]. Responses were measured on a 4-point Likert-type scale and were scored from 1–4 giving total stigma score of 40–160, with higher scores indicating greater stigma. Internal consistency has been reported at .96, and 2–3 week test–retest correlation ranges from .89 to .92 [53]. The reliability of the scale in our sample was 0.90 as measured by Cronbach’s α.
Depression
Patients’ depressive symptoms over the previous week were assessed using the Center for Epidemiological Studies Depression Scale (CES-D) [56]. The CES-D is a 20-item self-report screening measure for depressive symptoms that has demonstrated excellent reliability and validity, and has been widely used in studies of HIV-positive individuals [57–60]. The 20 items are rated on a 4-point Likert scale with 0 = rarely or none of the time (less than 1 day); 1 = some or little of the time (1–2 days); 2 = occasionally or a moderate amount of the time (3–4 days); 3 = most or all of the time (5–7 days). Total sum scores range from 0 to 60, with higher scores indicating increased levels of depression. The overall internal consistency (Cronbach’s alpha) for the entire 20-item scale was 0.74.
Social support
The Medical Outcomes Study Social Support Survey (MOS-SSS) [61] was used to measure the perceived availability of different types of social support. The 19 items in the scale were rated on a 5-point response format ranging from none of the time (1) to all of the time (5) as to the perceived availability of different types of support that an individual can turn to, if needed. A total social support score was obtained by summing responses to all items and transformed to a 0–100 scale. Higher scores reflected higher levels of perceived availability of social support. The scale’s reliability for the study sample was 0.96.
Health-Related Quality of life (HRQoL)
HRQoL was assessed using the RAND 36-Item Health Survey (SF-36) [62]. It is comprised of 36 items that assess eight health concepts: physical functioning, role limitations caused by physical health problems, role limitations caused by emotional problems, social functioning, emotional wellbeing, energy/fatigue, pain, and general health perceptions. Participants were asked to describe how they felt and how able they were to carry out their usual activities over the past month. Scores for individual items were recoded and mean total score was calculated to create a HRQoL index. HRQoL index ranged from 0 to 100, with a higher score indicating a higher HRQoL. Cronbach’s alpha value for the SF-36 survey was found to be 0.93.
Data analysis
All data analyses were performed using SPSS v. 22 [63]. We present descriptive statistics, including frequencies for categorical variables and means, standard deviations, and ranges for continuous variables. We tested our hypotheses in two interlinked steps. First, we examined a simple mediation model (Hypotheses 1–4). Collectively, Hypotheses 1, 2, 3, and 4 indicate an indirect effects model, whereby the relationship between HIV-related stigma and HRQoL is mediated by depression. This test of the mediation hypothesis was guided by the approach proposed by Baron and Kenny [64], the Sobel test [65], and the bootstrap method [66, 67]. Second, we integrated the proposed moderator variable into the mediation model and empirically tested the overall moderated mediation model (Hypothesis 5). Both analyses controlled for covariates (age, educational status, employment status, length of current incarceration, length of HIV diagnosis, currently taking ART, and current CD4+ count). Two variables, namely “currently taking ART” and “current CD4+ count”, were included in the moderated mediation model because both of them have been shown to have significant influence on HRQoL [68–71]. They were, however, excluded from the final model because of their non-significant association with HRQoL among our sample.
Hypotheses were tested using the SPSS PROCESS macro developed by Hayes (2013) [72]. The PROCESS macro uses an ordinary least squares (OLS) regression-based path analytic framework to test the proposed conditional direct and indirect effects. This macro facilitates implementation of the recommended bootstrapping methods and provides a method for probing the significance of conditional indirect effects at different values of the moderator variable.
Results
Sample characteristics
Table 1 and 2 represent characteristics of study participants and summary statistics for variables of interest, respectively. Using a conventional definition of depression (CES-D ≥ 16) [56], 36.9% were classified as having moderate to severe depressive symptoms.
Table 1.
Characteristics of the participants (N = 301)
| Variable | Frequency | % |
|---|---|---|
| Age | ||
| Mean (±SD) | 38.9 (6.8) | |
| Range | 21–58 | |
| Ethnicity | ||
| Malay | 216 | 71.8 |
| Chinese | 28 | 9.3 |
| Indian | 50 | 16.6 |
| Other | 7 | 2.3 |
| Religion | ||
| Muslim | 228 | 75.7 |
| Othera | 73 | 24.3 |
| Marital status | ||
| Single | 192 | 63.8 |
| Married | 34 | 11.3 |
| Widowed | 58 | 19.3 |
| Divorced | 17 | 5.6 |
| Employed full-time before incarceration | ||
| No | 111 | 36.9 |
| Yes | 190 | 63.1 |
| Highest level of education | ||
| Primary or belowb | 58 | 19.4 |
| Incomplete secondaryc | 197 | 65.9 |
| Secondary or higherd | 46 | 14.7 |
| Unprotected sexual risk prior to incarceration | ||
| No | 44 | 14.6 |
| Yes | 257 | 85.4 |
| History of injection drug use prior to incarceration | ||
| No | 17 | 5.6 |
| Yes | 284 | 94.4 |
| Type of offence(s) for current incarceration | ||
| Homicide | 1 | 0.3 |
| Violent-related crime | 23 | 7.7 |
| Property-related crime | 50 | 16.7 |
| Substance-related offence | 204 | 68.2 |
| Sexual-related crime | 1 | 0.3 |
| Others | 18 | 6.0 |
| Ever visited psychiatrist prior to incarceration | ||
| No | 283 | 94.0 |
| Yes | 18 | 6.0 |
| Months of incarceratione | ||
| Mean (±SD) | 34.0 (49.4) | |
| Range | 4–290 | |
| Time since HIV diagnosis (years) | ||
| Mean (±SD) | 8.3 (5.3) | |
| Range | 0.02–24 | |
| Currently on ARTf | ||
| No | 264 | 87.7 |
| Yes | 37 | 12.3 |
| CD4+ count | ||
| Mean (±SD) | 445.04 (286.54) | |
| Range | 8–1752 | |
Notes:
Includes Christian, Buddhist, Hindu, and other
Includes participants without any formal education and those with primary education
Includes Form 1 – 5
includes participants holding SPM, STPM/Diploma, and higher level of education
Months of incarceration at the time of interview
ART: Antiretroviral therapy
Table 2.
Summary statistics for variables of interest among the participants
| Variable | Scale (Range) | Meana | SDb | Minimum | Maximum |
|---|---|---|---|---|---|
| HIV-related stigma | 40 – 160 | 100.4 | 12.2 | 56.0 | 136 |
| Depression | 0 – 60 | 14.9 | 6.0 | 0.0 | 39 |
| Social support | 0 – 100 | 50.3 | 19.5 | 3.9 | 100 |
| HRQoLc | 0 – 100 | 77.7 | 14.9 | 22.2 | 100 |
Notes:
Higher scores indicate higher levels of HIV-related stigma, depression, social support, and HRQoL
SD: Standard deviation
HRQoL: Health-related quality of life
Tests of mediation
Table 3 presents the results of the OLS regression analyses for simple mediation. As hypothesized, HIV-related stigma was positively associated with depression (B = .1463, p <.001), however, the direct association between HIV-related stigma and HRQoL was not significant (B = −.0974, p = .1646). Similarly, depression was negatively associated with HRQoL (B = −.8392, p < .001). And finally, the strength of negative association between HIV-related stigma and HRQoL decreased after controlling for depression (B = −.0254). This supports our fourth hypothesis of an indirect or mediation effect (i.e., inconsistent mediation or suppressor effect) of HIV-related stigma on HRQoL via depression (Effect = −.1228). The formal two-tailed significance test (assuming a normal distribution) demonstrated that the indirect effect was significant (Sobel z = −3.8762 p < .001). Bootstrap results confirmed the Sobel test (Table 3), with a bootstrapped 95% confidence interval around the indirect effect not containing zero (−.2034, −.0648).
Table 3.
Regression results for simple mediation
| Variable | Coeff. | SE | t | p |
|---|---|---|---|---|
| HRQoLb regressed on HIV stigma | −0.0974 | 0.0699 | −1.3934 | .1646 |
| Depression regressed on HIV stigma | .1463 | 0.0276 | 5.3093 | <.001 |
| HRQoL regressed on depression | −0.8392 | 0.1454 | −5.7718 | <.001 |
| HRQoL regression on HIV stigma controlling for depression | 0.0254 | 0.0694 | 0.3658 | .7148 |
|
| ||||
| Indirect Effect of HIV stigma on HRQoL | ||||
|
| ||||
| Depression | Effect | Boot SE | BootLLCI | BootULCI |
|
| ||||
| −0.1228 | 0.0349 | −0.2034 | −0.0648 | |
|
| ||||
| Sobel test |
Tests for Indirect
Effect
|
|||
| Effect | SE | z | p | |
|
| ||||
| −0.1228 | 0.0317 | −3.8762 | 0.0001 | |
Notes:
Controlling for age, educational status, employment status, length of current incarceration, length of HIV diagnosis, currently taking ART, and current CD4+ count
HRQoL: Health-related quality of life
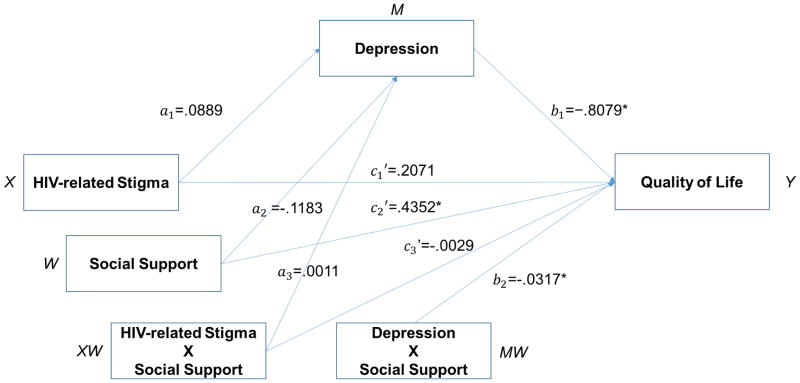
Tests of moderated mediation
Table 4 and Figure 2 present the results for the conditional indirect effect (i.e., moderated mediation model). With regard to our fifth hypothesis, we hypothesized that the inverse relationship between HIV-related and HRQoL via depression would be lower for individuals with higher level of social support than for their counterparts with lower level of social support. The results indicated that the interaction effect between depression and social support on HRQoL was significant (B = −.0317, p = .0133). In addition, we examined the conditional indirect effect of HIV-related stigma on HRQoL (through depression) at various levels of social support. Normal-theory tests indicated the conditional indirect effect (based on moderator: increasing level of social support) decreased and were all significant. Bootstrap confidence intervals and index of moderated mediation corroborated these results (Table 4). Thus, our fifth hypothesis was supported, such that the higher degree of indirect and negative effect of HIV-related stigma on HRQoL through depression was observed among individuals with lower level of social support, whereas this effect was lower (but significant) for those with higher levels of social support.
Table 4.
Regression results for the conditional indirect effect (moderated mediation model)
| Explanatory Variablea | Consequent |
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
M
(Depression) |
Y
(HRQoLc) |
||||||||
| Coeff. | SEb | p | w | SE | p | ||||
| HIV stigma | a1 | 0.0889 | 0.0709 | .2109 | c1 | 0.2071 | 0.1721 | .2298 | |
| Depression | - | - | - | - | b1 | −0.8079 | 0.3550 | .0237 | |
| Social support | a2 | -−0.1183 | 0.1289 | .3596 | c2 | 0.4352 | 0.7546 | .0433 | |
| HIV stigma × Social support | a3 | 0.0011 | 0.0013 | .3978 | c3 | −0.0029 | 0.0031 | .3538 | |
| Depression × Social support | - | - | - | - | b2 | −0.0317 | 0.0012 | .0133 | |
| Constant | i1 | 13.0461 | 7.6204 | .0880 | i2 | 94.6678 | 5.6492 | <.0001 | |
| R2 = 13.99% | R2 = 23.25% | ||||||||
| F(10,270) = 4.3912, p <0.001 | F(12,268) = 6.7667, p < .001 | ||||||||
|
| |||||||||
|
Conditional indirect
effect of HIV stigma on HRQoL at values of the moderator
| |||||||||
| Mediator | Moderator | Coeff. | Boot SE | BootLLCI | BootULCI | ||||
|
| |||||||||
| Depression | 30.6889 | −0.0987 | 0.0419 | −0.2016 | −0.0336 | ||||
| 50.5479 | −0.1162 | 0.0341 | −0.1975 | −0.0552 | |||||
| 70.4069 | −0.1336 | 0.0544 | −0.2623 | −0.0466 | |||||
Note:
Controlling for age, educational status, employment status, length of current incarceration, length of HIV diagnosis, currently taking ART, and current CD4+ count
SE: Standard error
HRQoL: Health-related quality of life
Figure 2.
Statistical diagram of moderated mediation model in the study
Note: Controlling for age, educational status, employment status, length of current incarceration, length of HIV diagnosis, currently taking ART, and current CD4 count
Discussion
In our sample, approximately two-fifths of the sample met screening criteria for moderate to severe depression, which is similar with finding from a previous study by Zahari et al. (2010) among HIV seropositive prisoners in Malaysia [26]. Similar to prior findings, the magnitude of depression in our sample is impressively high and higher than reported among general PLH in most international settings. This high rate of depressive symptoms among our sample may be due to higher levels of perceived HIV-related stigma [73, 74], incarceration itself [75–77], and/or HIV sero-status [75]. More importantly, it was concerning to find that though nearly half of the prisoners screened positive for depression, very few had ever seen a psychiatrist (6%) and even fewer had been seen by one during their incarceration (3%). These findings suggest the need for increased screening and treatment of mental illnesses in this population in order to improve HIV treatment outcomes and curb the transmission of HIV upon their transition to community.
Furthermore, our results emphasize the significance of psychosocial variables (e.g., HIV-related stigma, depression and HRQoL). The present finding of inconsistent mediation help clarify the complex inter-relationships between these psychosocial variables. That is, greater HIV-related stigma was associated with worse depressive symptoms. Worse depressive symptoms, in turn, was associated with poorer HRQoL. This finding confirms those of previous studies among PLH [16, 17] where HIV-related stigma may increase depressive symptoms, and subsequently, have a negative impact on HRQoL.
The potential mechanism for this may be that perceived HIV-related stigma and being in prison may lead to low self-esteem and negative self-image and thereby contribute to worsening depressive symptoms [12, 16]. More importantly, early symptoms of depression are largely untreated in Malaysia, particularly among incarcerated PLH, due to unavailability of trained psychiatrists and treatment facilities [78]. Furthermore, depression, like all psychiatric disorders, is highly stigmatized in the region and the use of mental health services is relatively low, as suggested by a low proportion of our sample who visited psychiatrists prior to incarceration. As a result, HRQoL of an individual can deteriorate [16, 27, 28]. Our preliminary exploration suggests important implications for prison-based care and pre-release planning of HIV-infected inmates. Management of depression, reduction of HIV-related stigma, and enhancing coping skills prior to release may be essential to improve the HRQoL among incarcerated individuals transitioning to the community.
As an extension of previous research, we also found the influence of the moderating effect of social support on the translation of HIV-related stigma into HRQoL via depressive symptoms. That is, the presence of depressive symptoms reinforces the negative influence of HIV-related stigma on HRQoL, particularly among individuals with lower social support. This is consistent with findings that social support helps to buffer the negative impact of depression on HRQoL [17, 31]. By taking moderated mediation into account, we acknowledge that this conditional process works differently in subgroups of individuals: those with a higher degree of social support are more able to buffer the negative indirect effect of depression, and thus are less likely to experience a negative impact on HRQoL. This evidence of the protective role of social support in buffering the negative effect of depression highlights that interventions to improve the HRQoL among incarcerated individuals living with HIV should integrate components to enhance social support.
Implications and future studies
Findings here have important implications for prison-based care and pre-release planning of incarcerated PLH. Consistent with prior results, the results from the current study highlight that prisoners often experience multiple psychosocial issues, such as low social support, HIV-related stigma, and depression [30, 42], which may serve as a barrier to maintaining HRQoL after release. To address these issues and improve the HRQoL, programs for incarcerated PLH should embrace a restorative approach whereby family members or trusted others who are willing to provide social support should be incorporated into pre-release planning. Such strategies, however, will also require assistance with HIV disclosure and family strengthening since many prisoners with HIV have not shared such information with trusted others. Other restorative strategies should incorporate post-release economic opportunities (e.g., income support, work, training, housing, employment) and social networking and community building – from the moment of incarceration to well beyond the initial period of release back into the community. Overall, the findings of this study highlight the importance of precisely targeting perceived HIV-related stigma, depression, and social support, while developing interventions for PLH with a history of incarceration and opioid dependence. Indeed, since nearly all (94%) PLH met pre-incarceration criteria for opioid dependence and be at high risk for relapse, a restorative approach would include enrollment in methadone treatment, which has documented stabilization benefits for patients and assist with transition back to the community [79, 80]. Such strategies in Malaysia, however, will need to overcome negative attitudes about prison-based methadone treatment where only 45% would accept it [81].
Additionally, the present analyses suggest some interesting directions for future research. For example, future research that expands the proposed model to include other relevant variables (e.g., neurocognitive impairment, alcohol use disorder) would make for an interesting contribution. Furthermore, future studies need to investigate the HRQoL among this high-risk population as they transition through prison and back to the community. Adding to that, future studies should use prospective data and longitudinal analyses to test this moderated mediation model that would allow researchers to examine causality and bi-directional causation in this relationships.
Limitations
While this study advances the current state of knowledge on how psychosocial factors (i.e., HIV-related stigma, depression, and social support) interact with each other and affect HRQoL, it must be considered in light of a few study limitations. First, the study’s use of self-report may have reduced the ability to accurately detect some measures (i.e., psychosocial factors) due to participants’ reluctance to self-report socially undesirable behaviors [82]. Second, social support among participants was measured while they were still in prison. This may have underestimated the level of social support among the participants due to the change in their social network. Third, this study made use of baseline data to examine the moderated mediation model. Thus, we are unable to infer cause-and-effect and directionality of relationships. Fourth, certain characteristics of the sample limit the generalizability of the findings. The results are specific to incarcerated men infected with HIV, and may not be generalizable to the entire population. Fifth, some of the items in the SF-36 scale (e.g., have you felt so down in the dumps that nothing could cheer you up?; have you felt downhearted and blue?) may be indicative of depressive symptoms as reported on the CES-D scale. This may have some influence in the overall moderated mediation model tested in this study. Despite these limitations, our findings have several clinical and research implications and add to our understanding of the processes by which psychosocial variables impact on different dimensions of HRQoL.
Conclusion
The current study adds to the growing body of literature that HIV-related stigma and depression are the key psychosocial factors associated with HRQoL among incarcerated, HIV-positive men with opioid dependence in Malaysia. Furthermore, the results found preliminary evidence of interactions between depression and social support, such that depressive symptoms had lesser negative effect on HRQoL for individuals with greater degree of social support. The results of our study, therefore, make an important contribution to our understanding of the applicability of moderated mediation framework of the psychosocial factors for improving HRQoL among PLH with a history of incarceration and opioid dependence. Particularly when taken in the context of limited mental health services and social support available for this high-risk population, future interventions seeking to improve HRQoL among PLH in Malaysia and elsewhere should include alleviating depressive symptoms and increasing social support as primary goals.
Acknowledgments
Source of Funding: This work was supported by grants from the National Institute on Drug Abuse for research (R01 DA025943 and R01 DA041271 to FLA), for career development (NIDA K24 DA017072 to FLA; K02 DA033139 to MMC), and for training (T32GM07205, F30DA039716 to ARB).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Compliance with Ethical Standards
Ethical approval
The protocol for the parent study was approved by institutional review boards at the University Malaya Medical Centre and Yale University. The protocol was also reviewed and approved by the Office of Human Research Protection at the US Department of Health and Human Services (DHHS) as it involved federally-funded research with prisoners. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Joint United Nations Programme on HIV/AIDS. How AIDS changed everything? Geneva, Switzerland: 2015. [Google Scholar]
- 2.UNAIDS. The Gap Report. Switzerland: 2014. [Google Scholar]
- 3.Ministry of Health Malaysia. Global AIDS response progress report 2014: Malaysia. Malaysia: 2014. [Google Scholar]
- 4.Kamarulzaman A. Impact of HIV prevention programs on drug users in Malaysia. J Acquir Immune Defic Syndr. 2009;52(Suppl 1):S17–19. doi: 10.1097/QAI.0b013e3181bbc9af. [DOI] [PubMed] [Google Scholar]
- 5.Todd C, Nassiramanesh B, Stanekzai M, Kamarulzaman A. Emerging HIV epidemics in muslim countries: Assessment of different cultural responses to harm reduction and implications for HIV control. Current HIV/AIDS Reports. 2007;4(4):151–157. doi: 10.1007/s11904-007-0022-9. [DOI] [PubMed] [Google Scholar]
- 6.Ngadiman S, Suleiman A, Taib SM, Yuswan F. Malaysia 2014: Country responses to HIV/AIDS. Malaysia: Ministry of Health Malaysia; 2014. [Google Scholar]
- 7.Bazazi A, Crawford F, Zelenev A, Heimer R, Kamarulzaman A, Altice FL. HIV Prevalence Among People Who Inject Drugs in Greater Kuala Lumpur Recruited Using Respondent-Driven Sampling. AIDS Behav. 2015;19(12):2347–2357. doi: 10.1007/s10461-015-1191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi P, Kavasery R, Desai MM, Govindasamy S, Kamarulzaman A, Altice FL. Prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Int J STD AIDS. 2010;21(6):416–423. doi: 10.1258/ijsa.2009.009180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372(9651):1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 10.Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–59. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bachireddy C, Bazazi AR, Kavasery R, Govindasamy S, Kamarulzaman A, Altice FL. Attitudes toward opioid substitution therapy and pre-incarceration HIV transmission behaviors among HIV-infected prisoners in Malaysia: implications for secondary prevention. Drug Alcohol Depend. 2011;116(1–3):151–157. doi: 10.1016/j.drugalcdep.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Wang H, He G, Fennie K, Williams AB. Shadow on My Heart: A Culturally Grounded Concept of HIV Stigma Among Chinese Injection Drug Users. The Journal of the Association of Nurses in AIDS Care. 2012;23(1):52–62. doi: 10.1016/j.jana.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferro E, Wickersham JA, Marcus R, Lee CK, Westergaard RP, Kamarulzaman A, et al. ID Week. San Francisco, CA: Infectious Diseases Society of America; 2013. Lack of Prescription of Antiretroviral Therapy to Vulnerable Populations by Malaysian Physicians. pp. [Abstract WE-1206] [Google Scholar]
- 14.Lee R, Kochman A, Sikkema K. Internalized Stigma Among People Living with HIV-AIDS. AIDS and Behavior. 2002;6(4):309–319. [Google Scholar]
- 15.Ferro E, Wickersham J, Marcus R, Kamarulzaman A, Altice F. Infectious Diseases Society of America Meeting. San Francisco, CA: Infectious Diseases Society of America; 2013. Lack of prescription of Antiretroviral Therapy to vulnerable population by Malaysian physicians. [Google Scholar]
- 16.Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India – a community based cross sectional study. BMC Public Health. 2012;12:463–463. doi: 10.1186/1471-2458-12-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X, Li L, Wang H, Fennie KP, Chen J, Williams AB. Mediation analysis of health-related quality of life among people living with HIV infection in China. Nursing & health sciences. 2015;17(2):250–256. doi: 10.1111/nhs.12181. [DOI] [PubMed] [Google Scholar]
- 18.Westergaard RP, Spaulding AC, Flanigan TP. HIV among persons incarcerated in the US: a review of evolving concepts in testing, treatment and linkage to community care. Current opinion in infectious diseases. 2013;26(1):10–16. doi: 10.1097/QCO.0b013e32835c1dd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Small W, Wood E, Betteridge G, Montaner J, Kerr T. The impact of incarceration upon adherence to HIV treatment among HIV-positive injection drug users: a qualitative study. AIDS Care. 2009;21(6):708–714. doi: 10.1080/09540120802511869. [DOI] [PubMed] [Google Scholar]
- 20.Briongos Figuero LS, Bachiller Luque P, Palacios Martin T, Gonzalez Sagrado M, Eiros Bouza JM. Assessment of factors influencing health-related quality of life in HIV-infected patients. HIV medicine. 2011;12(1):22–30. doi: 10.1111/j.1468-1293.2010.00844.x. [DOI] [PubMed] [Google Scholar]
- 21.Duffy L. Suffering, shame, and silence: the stigma of HIV/AIDS. J Assoc Nurses AIDS Care. 2005;16(1):13–20. doi: 10.1016/j.jana.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 23.Jin H, Hampton Atkinson J, Yu X, Heaton RK, Shi C, Marcotte TP, et al. Depression and suicidality in HIV/AIDS in China. Journal of affective disorders. 2006;94(1–3):269–275. doi: 10.1016/j.jad.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Kagee A, Martin L. Symptoms of depression and anxiety among a sample of South African patients living with HIV. AIDS Care. 2010;22(2):159–165. doi: 10.1080/09540120903111445. [DOI] [PubMed] [Google Scholar]
- 25.Dal-Bo MJ, Manoel AL, Filho AO, Silva BQ, Cardoso YS, Cortez J, et al. Depressive Symptoms and Associated Factors among People Living with HIV/AIDS. Journal of the International Association of Providers of AIDS Care. 2015;14(2):136–140. doi: 10.1177/2325957413494829. [DOI] [PubMed] [Google Scholar]
- 26.Zahari MM, Hwan Bae W, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36(1):31–38. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tate D, Paul RH, Flanigan TP, Tashima K, Nash J, Adair C, et al. The impact of apathy and depression on quality of life in patients infected with HIV. AIDS Patient Care STDS. 2003;17(3):115–120. doi: 10.1089/108729103763807936. [DOI] [PubMed] [Google Scholar]
- 28.Jia H, Uphold CR, Wu S, Chen GJ, Duncan PW. Predictors of changes in health-related quality of life among men with HIV infection in the HAART era. AIDS Patient Care STDS. 2005;19(6):395–405. doi: 10.1089/apc.2005.19.395. [DOI] [PubMed] [Google Scholar]
- 29.Shrestha R, Weikum D, Copenhaver M, Altice FL. The Influence of Neurocognitive Impairment, Depression, and Alcohol Use Disorders on Health-Related Quality of Life among Incarcerated, HIV-Infected, Opioid Dependent Malaysian Men: A Moderated Mediation Analysis. AIDS and Behavior. 2016:1–12. doi: 10.1007/s10461-016-1526-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19(10):1223–1229. doi: 10.1080/09540120701402830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson J, Alloy LB, Panzarella C, Metalsky GI, Rabkin JG, Williams JB, et al. Hopelessness as a mediator of the association between social support and depressive symptoms: findings of a study of men with HIV. J Consult Clin Psychol. 2001;69(6):1056–1060. doi: 10.1037//0022-006x.69.6.1056. [DOI] [PubMed] [Google Scholar]
- 32.Silver EJ, Bauman LJ, Camacho S, Hudis J. Factors associated with psychological distress in urban mothers with late-stage HIV/AIDS. AIDS Behav. 2003;7(4):421–431. doi: 10.1023/b:aibe.0000004734.21864.25. [DOI] [PubMed] [Google Scholar]
- 33.Mkangara OB, Wang C, Xiang H, Xu Y, Nie S, Liu L, et al. The univariate and bivariate impact of HIV/AIDS on the quality of life: a cross sectional study in the Hubei Province-Central China. Journal of Huazhong University of Science and Technology Medical sciences = Hua zhong ke ji da xue xue bao Yi xue Ying De wen ban = Huazhong keji daxue xuebao Yixue Yingdewen ban. 2009;29(2):260–264. doi: 10.1007/s11596-009-0226-x. [DOI] [PubMed] [Google Scholar]
- 34.Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol. 2007;26(4):488–495. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nargiso JE, Kuo CC, Zlotnick C, Johnson JE. Social support network characteristics of incarcerated women with co-occurring major depressive and substance use disorders. Journal of psychoactive drugs. 2014;46(2):93–105. doi: 10.1080/02791072.2014.890766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson JE, Esposito-Smythers C, Miranda R, Jr, Rizzo CJ, Justus AN, Clum G. Gender, social support, and depression in criminal justice-involved adolescents. Int J Offender Ther Comp Criminol. 2011;55(7):1096–1109. doi: 10.1177/0306624X10382637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bajunirwe F, Tisch DJ, King CH, Arts EJ, Debanne SM, Sethi AK. Quality of life and social support among patients receiving antiretroviral therapy in Western Uganda. AIDS Care. 2009;21(3):271–279. doi: 10.1080/09540120802241863. [DOI] [PubMed] [Google Scholar]
- 38.Bekele T, Rourke SB, Tucker R, Greene S, Sobota M, Koornstra J, et al. Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care. 2013;25(3):337–346. doi: 10.1080/09540121.2012.701716. [DOI] [PubMed] [Google Scholar]
- 39.Galvan FH, Davis EM, Banks D, Bing EG. HIV stigma and social support among African Americans. AIDS Patient Care STDS. 2008;22(5):423–436. doi: 10.1089/apc.2007.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care. 2008;20(10):1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 41.Mak WW, Cheung RY, Law RW, Woo J, Li PC, Chung RW. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc Sci Med. 2007;64(8):1549–1559. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 42.Leslie MB, Stein JA, Rotheram-Borus MJ. The Impact of Coping Strategies, Personal Relationships, and Emotional Distress on Health-Related Outcomes of Parents Living with Hiv or Aids. Journal of Social and Personal Relationships. 2002;19(1):45–66. [Google Scholar]
- 43.Bui HN, Morash M. The Impact of Network Relationships, Prison Experiences, and Internal Transformation on Women’s Success After Prison Release. Journal of Offender Rehabilitation. 2010;49(1):1–22. [Google Scholar]
- 44.Harp KL, Oser C, Leukefeld C. Social support and crack/cocaine use among incarcerated mothers and nonmothers. Substance use & misuse. 2012;47(6):686–694. doi: 10.3109/10826084.2012.659367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Staton-Tindall M, Royse D, Leukfeld C. Substance use criminality, and social support: an exploratory analysis with incarcerated women. Am J Drug Alcohol Abuse. 2007;33(2):237–243. doi: 10.1080/00952990601174865. [DOI] [PubMed] [Google Scholar]
- 46.Bazazi A, Wickersham J, Wegman M, Pillai V, Culbert G, Shrestha R, et al. Design and implementation of a factorial randomized controlled trial of methadone maintenance therapy and an evidence-based behavioral intervention for incarcerated people living with HIV and opioid dependence in Malaysia. Contemp Clin Trials. 2016 doi: 10.1016/j.cct.2017.05.006. (Under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Walmsley R. World Prison Population List. 11. London: International Centre for Prison Studies; 2015. [Google Scholar]
- 48.HIV/STI Section, Disease Control Division, Ministry of Health Malaysia. Global AIDS Response Progress Report Malaysia 2015: Reporting period January 2014 to December 2014. 2015. [Google Scholar]
- 49.Personal Communication: Malaysian Prison Department. 2016.
- 50.Bick J, Culbert GJ, Al-Darraji HA, Koh C, Pillai V, Kamarulzaman A, et al. Healthcare resources are inadequate to address the burden of illness among HIV-infected male prisoners in Malaysia. 2016 doi: 10.1108/IJPH-06-2016-0017. [Under Review] [DOI] [PubMed] [Google Scholar]
- 51.Culbert GJ, Pillai V, Bick J, Al-Darraji HA, Wickersham JA, Wegman MP, et al. Confronting the HIV, Tuberculosis, Addiction, and Incarceration Syndemic in Southeast Asia: Lessons Learned from Malaysia. Journal of neuroimmune pharmacology : the official journal of the Society on NeuroImmune Pharmacology. 2016;11(3):446–455. doi: 10.1007/s11481-016-9676-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Brislin RW. Back-Translation for Cross-Cultural Research. J Cross-Cultural Psych. 1970;1:185–216. [Google Scholar]
- 53.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Research in nursing & health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 54.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 55.Holzemer WL, Human S, Arudo J, Rosa ME, Hamilton MJ, Corless I, et al. Exploring HIV Stigma and Quality of Life for Persons Living With HIV Infection. Journal of the Association of Nurses in AIDS Care. 2009;20(3):161–168. doi: 10.1016/j.jana.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 56.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 57.Cook JA, Cohen MH, Burke J, Grey D, Anastos K, Kirstein L, et al. Effects of depressive symptoms and mental health quality of life on use of highly active antiretroviral therapy among HIV-seropositive women. J Acquir Immune Defic Syndr. 2002;30(4):401–409. doi: 10.1097/00042560-200208010-00005. [DOI] [PubMed] [Google Scholar]
- 58.Low-Beer S, Chan K, Yip B, Wood E, Montaner JS, O’Shaughnessy MV, et al. Depressive symptoms decline among persons on HIV protease inhibitors. J Acquir Immune Defic Syndr. 2000;23(4):295–301. doi: 10.1097/00126334-200004010-00003. [DOI] [PubMed] [Google Scholar]
- 59.Jeyaseelan L, Kumar S, Mohanraj R, Rebekah G, Rao D, Manhart LE. Assessing HIV/AIDS Stigma in South India: Validation and Abridgement of the Berger HIV Stigma Scale. AIDS and Behavior. 2013;17(1):434–443. doi: 10.1007/s10461-011-0128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Franke MF, Muñoz M, Finnegan K, Zeladita J, Sebastian JL, Bayona JN, et al. Validation and Abbreviation of an HIV Stigma Scale in an Adult Spanish-Speaking Population in Urban Peru. AIDS and Behavior. 2010;14(1):189–199. doi: 10.1007/s10461-008-9474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 62.Hays RD, Sherbourne CD, Mazel RM. The rand 36-item health survey 1.0. Health Economics. 1993;2(3):217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 63.IBM Corp. IBM SPSS Statistics for Windows, Version 23. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 64.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 65.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological methodology. 1982;13(1982):290–312. [Google Scholar]
- 66.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 67.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 68.Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV/AIDS (Auckland, NZ) 2012;4:117–124. doi: 10.2147/HIV.S32321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McInerney PA, Ncama BP, Wantland D, Bhengu BR, McGibbon C, Davis SM, et al. Quality of life and physical functioning in HIV-infected individuals receiving antiretroviral therapy in KwaZulu-Natal, South Africa. Nursing & health sciences. 2008;10(4):266–272. doi: 10.1111/j.1442-2018.2008.00410.x. [DOI] [PubMed] [Google Scholar]
- 70.Safren SA, Hendriksen ES, Smeaton L, Celentano DD, Hosseinipour MC, Barnett R, et al. Quality of life among individuals with HIV starting antiretroviral therapy in diverse resource-limited areas of the world. AIDS Behav. 2012;16(2):266–277. doi: 10.1007/s10461-011-9947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Igumbor J, Stewart A, Holzemer W. Comparison of the health-related quality of life, CD4 count and viral load of AIDS patients and people with HIV who have been on treatment for 12 months in rural South Africa. SAHARA J. 2013;10(1):25–31. doi: 10.1080/17290376.2013.807070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- 73.Grov C, Golub SA, Parsons JT, Brennan M, Karpiak SE. Loneliness and HIV-related stigma explain depression among older HIV-positive adults. AIDS Care. 2010;22(5):630–639. doi: 10.1080/09540120903280901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nachega JB, Morroni C, Zuniga JM, Sherer R, Beyrer C, Solomon S, et al. HIV-related stigma, isolation, discrimination, and serostatus disclosure: a global survey of 2035 HIV-infected adults. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill : 2002) 2012;11(3):172–178. doi: 10.1177/1545109712436723. [DOI] [PubMed] [Google Scholar]
- 75.Scheyett A, Parker S, Golin C, White B, Davis C, Wohl D. HIV-Infected Prison Inmates: Depression and Implications for Release Back to Communities. AIDS and Behavior. 2010;14(2):300–307. doi: 10.1007/s10461-008-9443-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fazel S, Seewald K. Severe mental illness in 33 588 prisoners worldwide: systematic review and meta-regression analysis. The British Journal of Psychiatry. 2012;200(5):364–373. doi: 10.1192/bjp.bp.111.096370. [DOI] [PubMed] [Google Scholar]
- 77.Ciesla JA, Roberts JE. Meta-Analysis of the Relationship Between HIV Infection and Risk for Depressive Disorders. American Journal of Psychiatry. 2001;158(5):725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- 78.Chong ST, Mohamad M, Er A. The Mental Health Development in Malaysia: History, Current Issue and Future Development. Asian Social Science. 2013;9(6):1–8. [Google Scholar]
- 79.Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: Implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013;132(1–2):378–382. doi: 10.1016/j.drugalcdep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rich JD, McKenzie M, Larney S, Wong JB, Tran L, Clarke J, et al. Methadone continuation versus forced withdrawal on incarceration in a combined US prison and jail: a randomised, open-label trial. Lancet. 2015 doi: 10.1016/S0140-6736(14)62338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mukherjee TI, Wickersham JA, Desai MM, Pillai V, Kamarulzaman A, Altice FL. Factors Associated with Interest in Receiving Prison-based Methadone Maintenance Therapy in Malaysia. Drug Alcohol Depend. 2016 doi: 10.1016/j.drugalcdep.2016.04.037. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Turner CF, Rogers SM, Hendershot TP, Miller HG, Thornberry JP. Improving representation of linguistic minorities in health surveys. Public Health Reports. 1996;111(3):276–279. [PMC free article] [PubMed] [Google Scholar]