Abstract
Background
Preventable medical harm is a leading cause of death in the United States. Incident reporting systems have been identified as the primary method to capture medical error and harm. Incident underreporting remains common, particularly among physician trainees.
Methods
We conducted a single-center, quasi-experimental study to examine how incident reporting education and weekly Patient Safety Rounds would affect incident reporting among trainees.
Results
Over 6 months, 73 resident physicians participated in the study. Median incident reports entered by trainees increased from 1 report per month during the pre-intervention period to 10 reports per month after the intervention, p=0.005. Residents reported not knowing how and why to file incident reports, which improved with the intervention.
Conclusion
Real-time education and regular reinforcement increased incident reporting among resident physicians. This educational approach may increase incidence reporting in other institutions.
Introduction
In 1999, the Institute of Medicine (IOM) reported that over 1 million injuries and 100,000 deaths annually in the United States were attributable to medical errors.1 This estimate has now increased to 400,000 deaths each year from preventable medical harm, comprising the third leading cause of death in the United States.2
One approach to improving patient safety is through incident reporting, which provides the opportunity of learning from medical errors and near misses, and thereby correcting hospital systems to minimize the likelihood of recurrence of similar events. Institutions with higher rates of incident reporting have better staff perceptions of safety culture.3,4
While incident reporting systems are standard at hospitals, incident reporting is rare. And, although the majority of healthcare workers know an incident reporting system exists, only a fraction have filed reports.5,6 Incident reporting is especially low among physicians, as compared to nurses. In one study 93.6% of physicians knew that an incident reporting system existed, but only 49.7% of these physicians knew how to complete and submit an incident report compared to 81.9% of nurses.6 Another study reported that approximately half of physician trainees had ever reported an incident.7 Commonly cited barriers to reporting include fear of retribution, lack of time, and unclear outcomes or feedback.8–10
To improve trainee incident reporting in our institution, we investigated the perception, attitudes, and barriers of incident reporting among Internal Medicine resident physicians, and provided small group education sessions on filing incident reports. We reinforced education with Patient Safety Rounds.
Methods
Study Design
We conducted a quasi-experimental study from July 1 to December 31, 2015 of an educational intervention to improve rates of incident reporting among Internal Medicine resident physicians at an academic medical institution. The primary outcome of rates of reporting were compared to the proceeding 6 months, January 1–June 30, 2015. Resident trainees completed 4-week rotations on one of 6 medical teams at our institution. During the first week of their rotation, trainees completed a 5 question pre-education survey of existing knowledge of incident reports including what an incident report is and how to file one, assessing if patient safety events have occurred during their rotation and if they reported the event, and identifying any barriers to reporting. After completion of the survey, education was conducted by a member of the study team and included what an incident report is, when it is appropriate to complete an incident report, demonstration of how to file a report electronically, and what happens to reports that are filed. At the time of education, residents also received a laminated pocket-card of instructions of how to file an incident report.
After education was completed, weekly Patient Safety Rounds were conducted by a member of the study team who inquired about patient safety events that occurred, reinforced the education they had received on filing incident reports, and provided follow up on incident reports that were filed. Patient Safety Rounds occurred after traditional attending rounds, lasting approximately 5–10 minutes with each medical team. At the end of the 4-week rotation, the resident trainees filled out a post-education survey again assessing their knowledge of incident reports, rate of reporting, and any barriers to reporting. All surveys were anonymous and voluntary. The number and category of incident reports filed by resident physicians during the intervention were compared to 6 months prior to intervention through review of reports in the electronic incident reporting system. This study was approved by the Institutional Review Board for the University of Maryland School of Medicine and VA Maryland Healthcare System R&D committee.
Statistical Methods
Bivariate associations between categorical outcome frequencies and intervention were assessed using a chi-square or Fisher’s exact test, as appropriate. The primary outcome of number of resident incident reports filed, was analyzed by comparing the pre-intervention median number of incident reports by residents to post-intervention median number of incident reports using the Wilcoxon Mann Whitney non-parametric test. All statistical tests were two-sided. Data were analyzed using SAS, version 9.3 (SAS Corporation, Cary, NC).
Results
During the 6 months of intervention, 95 trainees were eligible for the study of which, 73 completed the pre-intervention survey (response rate 76.8%) and received education about incident reports. Among them, 63 residents completed the post-intervention survey at the end of their 4-week rotation (response rate 86.3%). Response rates did not differ pre and post-intervention, p=0.12. Residents who had multiple rotations at our institution during the intervention period were only eligible to complete the survey once, but could participate in multiple Patient Safety Rounds.
In the pre-intervention period, 65 (89.0%) of residents knew what an incident report was and 13 (17.8%) knew how to file an incident report. Following education, all of the residents reported knowing what an incident report was, p=0.007, and how to file an incident report, p<0.0001. The most common barriers to reporting prior to intervention were lack of knowledge on how to report (72.6%), lack of knowledge on what needs to be reported (56.2%), and lack of time (42.5%). Additional survey results are listed in Table 1.
Table 1.
Resident trainee responses to surveys before and after the educational intervention.
| Post-intervention period n=63 |
Post-intervention period n=63 |
p- value |
|
|---|---|---|---|
| Response rate | 73/95 (76.8%) | 63/73 (86.3%) | |
| Reports knowing what an incident report is | 65 (89.0%) | 63 (100.0%) | 0.007 |
| Knows how to file an incident report | 13 (17.8%) | 63 (100.0%) | <0.0001 |
| Had situation in which an incident report was indicated |
50 (68.5%) | 39 (61.9%) | 0.42 |
| Perceived Barriers to Reporting*: | |||
| Lack of knowledge on how to report | 53 (72.6%) | 0 (0.0%) | <0.0001 |
| Lack of knowledge on what needs to be reported | 41 (56.2%) | 8 (12.7%) | 0.001 |
| Incident perceived as minor | 30 (41.1%) | 13 (20.6%) | 0.01 |
| Fear of punishment | 10 (13.7%) | 7 (11.1%) | 0.65 |
| Unclear outcomes after reporting | 22 (30.1%) | 12 (19.1%) | 0.14 |
| Lack of time | 31 (42.5%) | 27 (42.9%) | 0.96 |
| Self-reported frequency of filing incident reports | Total responses n=57 |
Total responses n=42 |
0.01 |
| Always | 6 (10.5%) | 10 (23.8%) | |
| Sometimes | 15 (26.3%) | 15 (35.7%) | |
| Rarely | 7 (12.3%) | 9 (21.4%) | |
| Never | 29 (50.9%) | 8 (19.1%) | |
Note that multiple barriers could be selected.
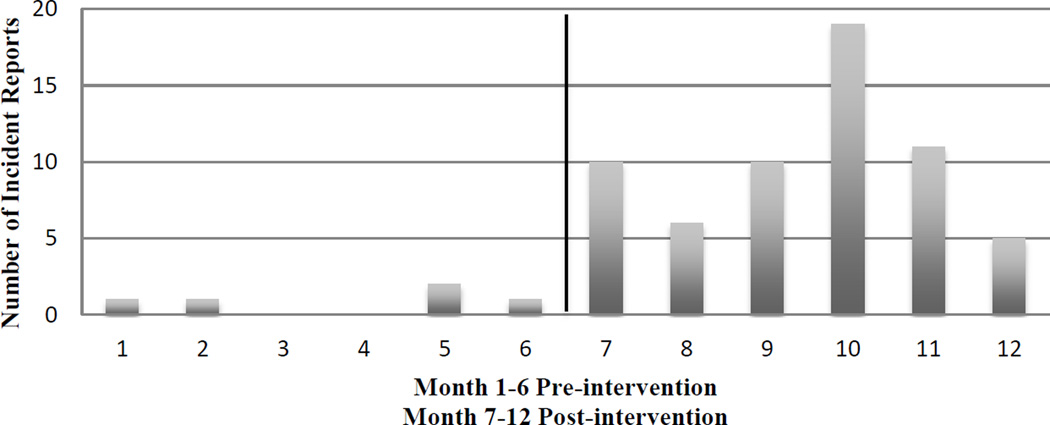
On review of the electronic incident reporting system, 5 incident reports were filed by trainees in the 6 months prior to intervention with a median of 1 incident report per month (IQR, 0.0–1.0). During the 6 months of the intervention period, a total of 61 incidents were reported for the 6 teams, a median of 10 incident reports per month (IQR, 6.0–11.0), p=0.005 (Figure 1). Of all the incidents reported, 22 (33.3%) were near misses (Table 2). The majority of incidents reported were due to delay in patient care (40.9%), followed by medication errors (33.3%). Of note, there were no reports filed on either misdiagnosis or delay in diagnosis.
Figure 1.
Total number of incident reports filed by trainees pre and post-intervention
Table 2.
Characteristics of incident reports filed
| Characteristic | Total (across study periods) |
|---|---|
| Number of incidents reported (by residents) |
66 |
| Number of near misses | 22 (33.3%) |
| Training level of residents | |
| Postgraduate Year 1 | 26 (39.4%) |
| Postgraduate Year 2 | 24 (36.4%) |
| Postgraduate Year 3, 4, 5 | 16 (24.2%) |
| Type of incident | |
| Medication | 22 (33.3%) |
| Laboratory | 5 (7.6%) |
| Delay in Care | 27 (40.9%) |
| Equipment | 3 (4.6%) |
| Fall | 1 (1.5%) |
| Other | 8 (12.1%) |
| Unit Location | |
| General Medical Ward | 56 |
| Intensive Care Unit | 8 |
| Emergency Room | 1 |
Discussion
Our study demonstrates that through the implementation of small-group education and reinforcement of education through Patient Safety Rounds, rates of incident reports among trainees significantly rose. Additionally, several barriers to incident reporting were eliminated through addressing them directly during education.
We believe the increase in reporting was largely attributed to the novel concept of Patient Safety Rounds. Many studies have shown that incident report systems alone will not capture the majority of adverse events and suggest intensive chart review captures more patient safety events.12,13 The limitation of chart review is that some types of errors may not be documented in the medical record.
In order to prevent medical errors in the future, we must be aware of problematic systematic issues, and act on the knowledge gained from incident reports. As a result of the incident reports filed in this study, several quality and patient safety initiatives were created in our institution. Engaging trainees in filing incident reports is critical in propelling forward a patient safety culture. This concept has recently gathered more national attention as the Accreditation Council for Graduate Medical Education (ACGME) under its Clinical Learning Environment Review (CLER) program conducted residency training site visits to improve the education of physicians and the quality of healthcare provided to patients. The 1st pathway in the CLER program is reporting of adverse events and close calls.11
Limitations to our study include being a single-center study. Replication of this intervention in other institutions, would strengthen our results. Other limitations include trainees generally not reporting on misdiagnosis or delay in diagnosis. The IOM recently released a report focusing on improving diagnosis, and encouraged reporting of diagnostic error.14
Conclusion
In conclusion, we found a simple educational intervention that included weekly patient safety rounds was able to increase incidence reporting tenfold. Weekly patient safety rounds should be considered by hospitals attempting to increase reporting of adverse events.
Acknowledgments
Source of support: N/A
References
- 1.Kohn L, Corrigan J, Donaldson M. To Err is Human, Institute of Medicine Report. Washington DC: National Academy Press; 2000. [Google Scholar]
- 2.James JT. A new, evidence based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9(3):122–128. doi: 10.1097/PTS.0b013e3182948a69. [DOI] [PubMed] [Google Scholar]
- 3.Howell AM, Burns EM, Bouras G, et al. Can Patient Safety Incident Reports Be Used to Compare Hospital Safety? Results from a Quantitative Analysis of the English National Reporting and Learning System Data. PLoS One. 2015 Dec 9;10(12):e0144107. doi: 10.1371/journal.pone.0144107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hutchinson A, Young TA, Cooper KL, et al. Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and Learning System. Qual Saf Health Care. 2009;18:5–10. doi: 10.1136/qshc.2007.022400. [DOI] [PubMed] [Google Scholar]
- 5.AbuAlRub RF, Al-Akour NA, Alatari NH. Perceptions of reporting practices and barriers to reporting incidents among registered nurses and physicians in accredited and nonaccredited Jordanian hospitals. J Clin Nurs. 2015 Oct;24(19–20):2973–2982. doi: 10.1111/jocn.12934. [DOI] [PubMed] [Google Scholar]
- 6.Evans SM, Berry JG, Smith BJ, et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care. 2006 Feb;15(1):39–43. doi: 10.1136/qshc.2004.012559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagenal J, Sahnan K, Shantikumar S. Comparing the Attitudes and Knowledge Toward Incident Reporting in Junior Physicians and Nurses in a District General Hospital. J Patient Saf. 2016;12:51–53. doi: 10.1097/PTS.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 8.Rea D, Griffiths S. Patient safety in primary care: incident reporting and significant event reviews in British general practice. Health Soc Care Community. 2015 Mar 25; doi: 10.1111/hsc.12221. (ahead of print) [DOI] [PubMed] [Google Scholar]
- 9.Winsvold Prang I, Jelsness-Jørgensen LP. Should I report? A qualitative study of barriers to incident reporting among nurses working in nursing homes. Geriatr Nurs. 2014;35(6):441–447. doi: 10.1016/j.gerinurse.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Hewitt T, Chreim S, Forster A. Sociocultural Factors Influencing Incident Reporting Among Physicians and Nurses: Understanding Frames Underlying Self- and Peer-Reporting Practices. J Patient Saf. 2014;00:00–00. doi: 10.1097/PTS.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 11.Accreditation Council for Graduate Medical Education Clinical Learning Environment Review (CLER) Program. CLER Pathways to Excellence. [Accessed December 8, 2015]; https://www.acgme.org/acgmeweb/Portals/0/PDFs/CLER/CLER_Brochure.pdf. [Google Scholar]
- 12.Olsen S, Neale G, Schwab K, et al. Hospital staff should use more than one method to detect adverse events and potential adverse events: incident reporting, pharmacist surveillance, and local real-time record review may all have a place. Qual Saf Health Care. 2007;16:40–44. doi: 10.1136/qshc.2005.017616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Westbrook J, Li L, Lehnbom EC, et al. What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported in an incident system. International Journal for Quality in Health Care. 2015:1–9. doi: 10.1093/intqhc/mzu098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balogh EP, Miller BT, Ball JR, editors. Improving Diagnosis in Health Care. 2015. Sep, Committee on Diagnostic Error in Health Care; Board of Health Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine. [PubMed] [Google Scholar]