Abstract
Purpose of review
While hand injuries occur frequently in the athletic population, sagittal band ruptures, boutonniere deformities, and pulley ruptures are infrequently encountered. These injuries represent diagnostic challenges and can result in significant impairment. Early recognition with appropriate treatment is necessary to maximize recovery and minimize return to athletic competition. This review will focus on the underlying mechanism, pathophysiology of injury, diagnosis, and treatment of each of these injuries.
Recent findings
With respect to sagittal band ruptures, boutonniere deformities, and pulley ruptures, the recent literature has been limited in scope. For sagittal band injuries, current efforts have focused on alternative techniques for sagittal band reconstruction. Little progress has been made in recent years with respect to boutonniere injuries in the athletic population; prevention of fixed deformities remains the backbone of treatment. The exact contribution from individual and combined pulley injuries in the creation of bowstringing remains controversial. Recent anatomical studies have failed to definitively answer the question of what degree of rupture is necessary to create symptomatic bowstringing. Favorable outcomes, with respect to both preventing bowstringing and returning to full athletic participation, have been newly reported following pulley reconstruction in rock climbers.
Summary
Due to the infrequent nature of sagittal band ruptures, boutonniere deformities, and pulley ruptures, current treatment is mostly guided by historically established methods, limited case series, and case reports. Nonsurgical treatment remains the mainstay for most injuries and, if employed early, often precludes the need for surgery. Further anatomical and clinical research, including outcome studies, is necessary in guiding treatment algorithms.
Keywords: Sagittal band, Pulley injuries, Boutonniere deformity, Central slip disruption, Extensor tendon injuries, Athletic hand injuries
Introduction
Hand injuries are common in the professional and recreational athletic population. Sagittal band ruptures, boutonniere deformities, and pulley ruptures are infrequently encountered. All three injuries, however, represent diagnostic challenges and can result in significant functional loss. Early recognition with appropriate treatment can often preclude the need for surgery and prevent unnecessary morbidity. This review will focus on the underlying mechanism, pathophysiology of injury, diagnosis, and treatment of each of these injuries.
Sagittal band injuries
Sagittal band injuries represent zone 5 extensor tendon injuries. The sagittal band attaches dorsally to the extensor hood, runs palmar to insert on the volar plate, and serves as the primary lateral stabilizer to the tendon over the metacarpophalangeal (MCP) joint [1].
Controversy exists regarding the exact mechanism of sagittal band injury. A direct blow to a flexed MCP joint can result in rupture and has been termed a “boxers knuckle” [2•]. Others have theorized that the injury results from forced digital flexion with the wrist in a position of flexion and ulnar deviation [3]. With this injury, a radial-sided rupture of the sagittal band typically occurs. Rupture results in pain, swelling, and ulnar subluxation of the extensor tendon with MCP flexion. The long finger is most frequently injured due to its greater length and the relative weakness of its fibrous attachments to the extensor hood in comparison to the other digits [4]. Tendon subluxation can result in localized pain and mechanical symptoms of triggering or snapping with digital flexion.
Rayan and Murray proposed a classification system for sagittal band injuries: injury without instability of the extensor tendon (type 1), injury with subluxation of the extensor tendon (type 2), and injury with dislocation of the extensor tendon (type 3) [5]. The diagnosis is made with a thorough history and physical examination of the affected MCP joint. Tendon subluxation or dislocation is demonstrated with active or passive digital motion, reproducing the patient’s pain (Fig. 1). Imaging studies are rarely necessary; however, in cases of incomplete injury, magnetic resonance imaging (MRI) or dynamic ultrasound (US) can provide confirmation. Comparison sequences performed with the MCP joint in positions of both maximum flexion and full extension can be useful in evaluating the degree of tendon subluxation or dislocation.
Fig. 1.
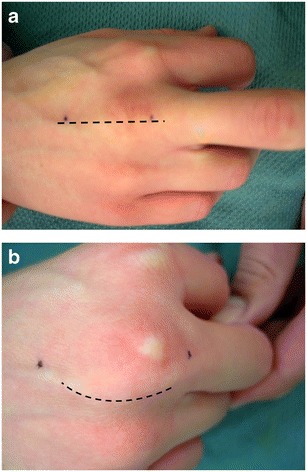
a Long finger MCP joint in an injured volleyball player; MCP in extension. The dashed line indicates the course of the tendon. b Tendon dislocation with MCP flexion. The dashed line indicates the course of the tendon
Quite often, sagittal band injuries are underappreciated with a delay in presentation common. In the absence of tendon subluxation or in cases with subluxation diagnosed early (within 4–6 weeks of injury), nonoperative management is indicated. While some advocate acute operative intervention with subluxation or dislocation, we reserve this for athletes with type 3 injuries. The injured digit is treated with a custom orthosis which maintains the affected MCP joint in hyperextension or slight flexion for 4–6 weeks [5, 6•, 7]. For patients presenting in a delayed fashion, a trial course of conservative treatment is often still indicated.
When painful tendon subluxation persists in spite of conservative treatment or for injuries presenting in a markedly delayed interval, surgical intervention is indicated. Direct repair of the sagittal band is typically only possible in cases of acute diagnosis (Fig. 2). Multiple reconstruction techniques have been advocated. The goal of reconstructive efforts is to stabilize the extensor tendon against ulnar subluxation or dislocation. Adjacent juncturae, anomalous tendons (such as the extensor medius proprius of the long finger), and distally based slips of the injured tendon have been successfully utilized to provide a pulley which restrains the tendon [8–11] (Fig. 3). Patients are immobilized with the MCP joints in slight flexion using a custom orthosis for 4–6 weeks with early protected motion initiated within 1–2 weeks.
Fig. 2.
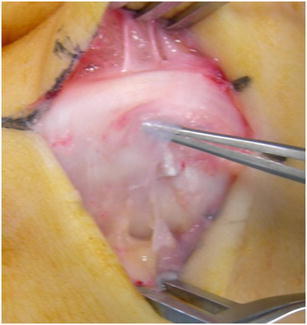
Patulous remnants of sagittal band in a case of chronic injury
Fig. 3.

Repaired sagittal band injury with distally based “lasso”
The results of both operative and nonoperative management are limited to case reports and small case series which are not specific to the athletic population. As these injuries are common in the rheumatoid patient, it is important to avoid comparison with results in this patient population. In general, favorable results have been reported for incomplete injuries treated early. In a series involving a nonrheumatoid patient population of 11 digits with acute injuries treated nonoperatively, Catalano et al. reported 8 digits free from pain and with little or no discernable tendon subluxation. All patients achieved full range of motion [6•]. Surgical intervention for complete injuries has been reported to be successful in returning athletes to return to play [2•, 12].
Boutonniere injuries
Boutonniere injuries represent zone 3 extensor mechanism disruptions over the proximal interphalangeal (PIP) joint (Fig. 4). During athletic participation, common injury mechanisms include hyperflexion injuries, direct blunt or sharp trauma to the dorsum of the finger, and volar dislocations of the PIP joint. Basketball and volleyball players may be at particular risk for these injuries [13]. Injury to the central slip in isolation will not result in boutonniere deformity. Concomitant injury or attenuation of the triangular ligament and subsequent volar subluxation of the lateral bands will result in the characteristic PIP joint extensor lag and DIP joint hyperextension seen in this condition (Fig. 5). With increased pull from the intrinsic muscles, the lateral bands also migrate proximally resulting in increased terminal extensor mechanism tension and DIP joint extension [14].
Fig. 4.

Boutonniere deformity
Fig. 5.
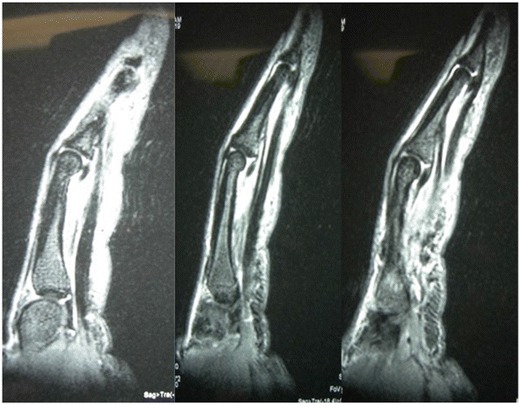
MRI demonstrating A2 pulley rupture
Athletes with central slip injuries may present with seemingly innocuous injury mechanisms such as a “jammed finger” and can be easily missed. Careful history and physical examination are required for a prompt and accurate diagnosis. Pictures of any initial deformity and knowledge of whether an on-field reduction was performed can aid in the diagnosis. As these can be subtle injuries, the clinician should have a low threshold for close follow-up and repeat examination if the diagnosis is in question [15]. For athletes with suspected boutonniere injuries, the Elson test should be performed [16, 17•]. The examiner places the PIP joint in 90° of flexion while the patient attempts to actively extend the DIP joint. With a central slip disruption, patient will demonstrate rigid DIP hyperextension. In the acute setting, some authors recommend administering a digital block prior to performing the Elson test [14, 18]. With a detailed physical examination, advanced imaging is rarely required.
It is important to distinguish a true boutonniere injury from a hyperextension injury to the PIP joint that results in PIP flexion contracture with an intact central slip [19, 20]. This PIP joint flexion contracture secondary to scarring of the volar plate has been described as a “pseudo-boutonniere” injury, and it lacks the pathognomonic rigid DIP joint hyperextension seen in traditional boutonniere injuries. Inappropriate prolonged immobilization of a pseudo-boutonniere deformity would result in increased stiffness and functional loss.
Orthogonal radiographs of the involved digit are utilized to assess for bony avulsion at the dorsal base of P2, volar subluxation or dislocation, and any degenerative changes at the PIP joint. While there is no universally accepted classification system, there are a number of injury characteristics that should be determined. The chronicity of the injury, bony involvement, presence of an open injury, and whether the deformity is passively correctable can all guide treatment decisions. Burton proposed a four-stage classification system, highlighting the importance of determining whether the PIP deformity was fixed or passively correctable [18]. Stage I injuries are passively correctable, stage II are fixed without joint involvement, and stage III have both volar plate and collateral ligament contractures with intra-articular fibrosis. Stage IV includes all the findings in stage III with the additional presence of PIP joint arthritis.
Most acute central slip ruptures can be managed nonsurgically. For athletes with acute, closed central slip ruptures without substantial bony involvement, full-time PIP joint extension splinting for 4–6 weeks is recommended with the goal of preventing boutonniere deformity. It is important to encourage active DIP flexion which will help to keep the lateral bands dorsally located. After this period, the athlete can be transitioned to night splinting for an additional 4 weeks. Nonsurgical treatment can also be attempted in some chronic injuries where either dynamic splints, progressive static splinting, or serial static casting can be utilized to correct fixed PIP flexion contractures [21].
Operative management includes acute central slip repair, open reduction internal fixation, reconstruction procedures, and arthrodesis. For acute open injuries, irrigation and debridement with central slip repair are recommended followed by the PIP extension splinting protocol described above. Open reduction internal fixation is recommended in the setting of a central slip avulsion with a large osseous fragment.
For patients with functionally limiting chronic boutonniere deformities, a variety of reconstructive procedures have been described [8, 22–31]. Unfortunately, there is a paucity of literature describing the outcomes of these procedures in younger athletic populations. It is critical to understand the particular skills and activities required of each athlete for participation in their sport before proceeding with operative intervention. Reconstruction procedures can be performed as single or staged procedures with a goal of achieving full passive PIP extension and tendon rebalancing. Extensor tenolysis and PIP joint contracture releases may also be necessary. Arthrodesis is reserved for patients with fixed PIP contractures and painful degenerative changes.
One of the biggest challenges when treating athletes with boutonniere injuries involves return-to-play criteria. While there are no universally accepted guidelines, Lourie describes a helpful mnemonic to guide decision-making [32]. The components of “APPLES” include the following: age (A), position and hand dominance (P), performance level (PL), history of enhancement drugs (E), and in-season versus out-of-season injury (S). While a distance runner may be able to tolerate a PIP extension splint for an acute closed injury, the same may not be true for a high-level soccer goalkeeper or professional pitcher with an injury to the index finger of their throwing hand.
Pulley injuries
Closed pulley injuries can occur in athletes, most commonly in rock climbers. In a series of 600 injured rock climbers, pulley injuries accounted for 20% of all injuries [33]. Pulley ruptures are most common in the ring and long fingers [33, 34]. Loss of pulley integrity can lead to bowstringing with subsequent losses of both motion and grip strength. While substantial anatomic variability can be present, the pulley system is commonly described as having five annular pulleys and three cruciate pulleys.
Vigouroux et al. studied eight human subjects and found that fingertip forces were highest in the ring and long fingers and that these forces were close to their rupture thresholds [34]. Schoffl et al. described two finger positions frequently used in rock climbing and their relationship to pulley rupture [33]. In the hanging position, the MCP, PIP, and DIP joints are all flexed. In the crimp position, the carpus both supinates and ulnarly deviates with the DIP and MCP joints extending while the PIP joint flexes. This position places increased stress on the ring finger.
While the function between each of the annular pulleys continues to be defined, the A2 and A4 pulleys have classically been described to prevent bowstringing. In a recent cadaveric study, Leeflang et al. demonstrated that a 30% excision of A2 resulted in bowstringing and that distal A2 rupture caused more bowstringing than a proximal A2 rupture [35]. Furthermore, they noted that complete A3 excision did not result in bowstringing. In contrast to these findings, Moriya et al. released the entire A2 pulley in seven patients who underwent zone 2 flexor tendon repair and noted an absence of bowstringing in all patients [36]. Moriya et al. also noted an absence of bowstringing after excising A3, C2, and A4 in their series of patients undergoing flexor tendon repair [37].
History, physical examination, and imaging can aid in the diagnosis of closed pulley injuries. Climbers will often report an acute onset of pain during climbing and may recall hearing a “pop.” In a series of four professional pitchers, three reported prodromal pain over the middle phalanx prior to sustaining an A4 pulley rupture [38]. Swelling, and occasionally a volar hematoma, will be present in the digit along with tenderness to palpation elicited over the injured pulley. Bowstringing may be present on examination when multiple pulleys are ruptured but may not be present with an isolated rupture [39].
AP and lateral radiographs of the injured digit should be obtained to evaluate for fracture, which should be in the differential diagnosis. At our institution, we utilize dynamic ultrasound when the diagnosis of pulley rupture is suspected. Ultrasound has a sensitivity and specificity of 98 and 100%, respectively [40]. MRI demonstrates similar diagnostic accuracy and can also be utilized in skeletally immature patients where the differential diagnosis includes a non-displaced epiphyseal injury (Fig. 6) [41]. However, it is more expensive and may not be as readily available.
Fig. 6.
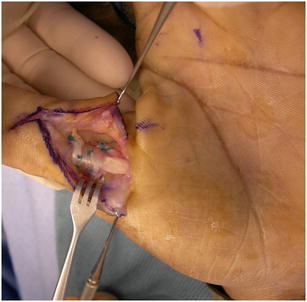
Pulley repair using palmaris longus tendon graft
Schoffl proposed a classification system that aids in treatment decision-making: pulley strain (grade I), complete A4 or partial A2 or A3 rupture (grade II), complete rupture of A2 or A3 (grade III), and multiple ruptures or A2 or A3 rupture combined with lumbrical or ligament injury (grade IV) [42].
For partial or isolated complete pulley ruptures (grades I–III), nonsurgical treatment is indicated with rest, taping, edema control, splinting, and functional sport-specific therapy. Multiple complete ruptures (grade IV) are treated surgically. Recent authors have presented their results using a variety of reconstruction techniques. Schoffl et al. reported excellent sport-specific outcomes in five of six climbers who underwent reconstruction of multiple pulley ruptures with a palmaris longus graft [43] (Fig. 6). Bouyer performed 38 reconstructions with extensor retinaculum, noting that 30 patients returned to their previous climbing level and found an association between bowstringing correction and climbing level recovery [44•]. For athletes with multiple pulley ruptures, reconstructive procedures can allow for the return to climbing.
Conclusions
Due to the infrequent nature of sagittal band ruptures, boutonniere deformities, and pulley ruptures, current treatment is mostly guided by historically established methods, limited case series, and case reports. Nonsurgical treatment remains the mainstay for most injuries and, if employed early, often precludes the need for surgery. Further anatomical and clinical research, including outcome studies, is necessary in guiding treatment algorithms.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Hand and Wrist Sports Medicine
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Wheeldon FT. Recurrent dislocation of extensor tendons in the hand. J Bone Joint Surg Br. 1954;36B:612–617. doi: 10.1302/0301-620X.36B4.612. [DOI] [PubMed] [Google Scholar]
- 2.Hame SL, Melone CP. Boxer’s knuckle in the professional athlete. Am J Sports Med. 2000;28:879–882. doi: 10.1177/03635465000280061701. [DOI] [PubMed] [Google Scholar]
- 3.Boyes J. Bunnell’s surgery of the hand. 4th ed. Boyes J, editor. Philadelphia: Lippincott; 1984.
- 4.Kettelkamp DB, Flatt AE, Moulds R. Traumatic dislocation of the long-finger extensor tendon. A clinical, anatomical, and biomechanical study. J Bone Joint Surg Am. 1971;53:229–240. doi: 10.2106/00004623-197153020-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rayan GM, Murray D. Classification and treatment of closed sagittal band injuries. J Hand Surg. 1994;19:590–594. doi: 10.1016/0363-5023(94)90261-5. [DOI] [PubMed] [Google Scholar]
- 6.• Catalano LW, Gupta S, Ragland R, Glickel SZ, Johnson C, Barron OA. Closed treatment of nonrheumatoid extensor tendon dislocations at the metacarpophalangeal joint. J Hand Surg. 2006. 242–5. Retrospective series illustrating the results of non-operative treatment of acute sagittal band injuries for patients without rheumatoid arthritis. [DOI] [PubMed]
- 7.Inoue G, Tamura Y. Dislocation of the extensor tendons over the metacarpophalangeal joints. J Hand Surg. 1996;21:464–469. doi: 10.1016/S0363-5023(96)80364-9. [DOI] [PubMed] [Google Scholar]
- 8.Carroll C, Moore JR, Weiland AJ. Posttraumatic ulnar subluxation of the extensor tendons: a reconstructive technique. J Hand Surg. 1987;12:227–231. doi: 10.1016/S0363-5023(87)80276-9. [DOI] [PubMed] [Google Scholar]
- 9.Andruss RJ, Herndon JH. Ulnar subluxation of the extensor digitorum communis tendon: a case report and review of the literature. Iowa Orthop J. 1993;13:208–213. [PMC free article] [PubMed] [Google Scholar]
- 10.Beck JD, Riehl JT, Klena JC. Anomalous tendon to the middle finger for sagittal band reconstruction: report of 2 cases. J Hand Surg. 2012;37:1646–1649. doi: 10.1016/j.jhsa.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 11.Watson HK, Weinzweig J, Guidera PM. Sagittal band reconstruction. J Hand Surg. 1997;22:452–456. doi: 10.1016/S0363-5023(97)80012-3. [DOI] [PubMed] [Google Scholar]
- 12.Posner MA, Ambrose L. Boxer’s knuckle-dorsal capsular rupture of the metacarpophalangeal joint of a finger. J Hand Surg. 1989;14:229–236. doi: 10.1016/0363-5023(89)90011-7. [DOI] [PubMed] [Google Scholar]
- 13.Weiland AJ. Boutonnière and pulley rupture in elite baseball players. Hand Clin. 2012;28:447. doi: 10.1016/j.hcl.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 14.McKeon K, Lee D. Posttraumatic boutonniere and swan neck deformities. J Am Acad Orthop Surg. 2015;23:623–632. doi: 10.5435/JAAOS-D-14-00272. [DOI] [PubMed] [Google Scholar]
- 15.Smith DW. Boutonnière and pulley rupture in elite basketball. Hand Clin. 2012;28:449–450. doi: 10.1016/j.hcl.2012.05.046. [DOI] [PubMed] [Google Scholar]
- 16.Elson RA. Rupture of the central slip of the extensor hood of the finger: a test for early diagnosis. J Bone Joint Surg Br. 1986;68:229–231. doi: 10.1302/0301-620X.68B2.3958008. [DOI] [PubMed] [Google Scholar]
- 17.Rubin J, Bozentka DJ, Bora FW. Diagnosis of closed central slip injuries: a cadaveric analysis of non-invasive tests. J Hand Surg Eur. 1996;21:614–616. doi: 10.1016/S0266-7681(96)80142-2. [DOI] [PubMed] [Google Scholar]
- 18.Green D, Wolfe S. In: Green’s operative hand surgery. 6th. Green D, Wolfe S, editors. Philadelphia: Elsevier/Churchill Livingstone; 2011. [Google Scholar]
- 19.McCue FC, Honner R, Gieck JH, Andrews J, Hakala M. A pseudo-boutonniere deformity. Hand. 1975;7:171–174. doi: 10.1016/0072-968X(75)90014-5. [DOI] [PubMed] [Google Scholar]
- 20.Rothwell AG. The pseudo-boutonniere deformity. NZ Med J. 1979;89:51–54. [PubMed] [Google Scholar]
- 21.Chauhan A, Jacobs B, Andoga A, Baratz ME. Extensor tendon injuries in athletes. Sports Med Arthrosc. 2014;22:45–55. doi: 10.1097/JSA.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 22.Ahmad F, Pickford M. Reconstruction of the extensor central slip using a distally based flexor digitorum superficialis slip. J Hand Surg. 2009;34:930–932. doi: 10.1016/j.jhsa.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 23.Curtis RM, Reid RL, Provost JM. A staged technique for the repair of the traumatic boutonniere deformity. J Hand Surg. 1983;8:167–171. doi: 10.1016/S0363-5023(83)80009-4. [DOI] [PubMed] [Google Scholar]
- 24.Dolphin J. Extensor tenotomy for chronic boutonniere deformity of the finger: a report of two cases. J Bone Joint Surg Am. 1965;47:161–164. doi: 10.2106/00004623-196547010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Gama C. Results of the Matev operation for correction of boutonniere deformity. Plast Reconstr Surg. 1979;64:319–324. doi: 10.1097/00006534-197909000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Grundberg AB. Anatomic repair of boutonniere deformity. Clin Orthop Relat Res. 1980;153:226–229. [PubMed] [Google Scholar]
- 27.Meadows SE, Schneider LH, Sherwyn JH. Treatment of the chronic boutonniere deformity by extensor tenotomy. Hand Clin. 1995;11:441–447. [PubMed] [Google Scholar]
- 28.Snow J. A method for reconstruction of the central slip of the extensor. Plast Reconstr Surg. 1976;57:455–459. doi: 10.1097/00006534-197604000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Stern PJ. Extensor tenotomy: a technique for correction of posttraumatic distal interphalangeal joint hyperextension deformity. J Hand Surg. 1989;14:546–549. doi: 10.1016/S0363-5023(89)80022-X. [DOI] [PubMed] [Google Scholar]
- 30.Terrill RQ, John GR. Correction of the severe nonrheumatoid chronic boutonniere deformity with a modified Matev procedure. J Hand Surg. 1992;17:874–880. doi: 10.1016/0363-5023(92)90459-3. [DOI] [PubMed] [Google Scholar]
- 31.Urbaniak JR, Hayes MG. Chronic boutonniere deformity—an anatomic reconstruction. J Hand Surg. 1981;6:379–383. doi: 10.1016/S0363-5023(81)80048-2. [DOI] [PubMed] [Google Scholar]
- 32.Lourie GM. Boutonnière and pulley rupture football commentary. Hand Clin. 2012;28:451–452. doi: 10.1016/j.hcl.2012.05.047. [DOI] [PubMed] [Google Scholar]
- 33.Schöffl V, Hochholzer T, Winkelmann HP, Strecker W. Pulley injuries in rock climbers. Wilderness Environ Med. 2003;14:94–100. doi: 10.1580/1080-6032(2003)014[0094:PIIRC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Vigouroux L, Quaine F, Paclet F, Colloud F, Moutet F. Middle and ring fingers are more exposed to pulley rupture than index and little during sport-climbing: a biomechanical explanation. Clin Biomech. 2008;23:562–570. doi: 10.1016/j.clinbiomech.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Leeflang S, Coert JH. The role of proximal pulleys in preventing tendon bowstringing: pulley rupture and tendon bowstringing. J Plast Reconstr Aesthetic Surg. 2014;67:822–827. doi: 10.1016/j.bjps.2014.01.041. [DOI] [PubMed] [Google Scholar]
- 36.Moriya K, Yoshizu T, Tsubokawa N, Narisawa H, Hara K, Maki Y. Clinical results of releasing the entire A2 pulley after flexor tendon repair in zone 2C. J Hand Surg Eur. 2016;41(4):400–405. doi: 10.1177/1753193415619082. [DOI] [PubMed] [Google Scholar]
- 37.Moriya K, Yoshizu T, Tsubokawa N, Narisawa H, Hara K, Maki Y. Outcomes of release of the entire A4 pulley after flexor tendon repairs in zone 2A followed by early active mobilization. J Hand Surg Eur. 2016;41:400–405. doi: 10.1177/1753193415619082. [DOI] [PubMed] [Google Scholar]
- 38.Lourie GM, Hamby Z, Raasch WG, Chandler JB, Porter JL. Annular flexor pulley injuries in professional baseball pitchers: a case series. Am J Sports Med. 2011;39:421–424. doi: 10.1177/0363546510387506. [DOI] [PubMed] [Google Scholar]
- 39.Marco R, Sharkey N, Smith T, Zissimos A. Pathomechanics of closed rupture of the flexor tendon pulleys in rock climbers. J Bone Joint Surg. 1998;80:1012–1019. doi: 10.2106/00004623-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 40.Klauser A, Frauscher F, Bodner G, Halpern EJ, Schocke MF, Springer P, et al. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222:755–761. doi: 10.1148/radiol.2223010752. [DOI] [PubMed] [Google Scholar]
- 41.Hauger O, Chung CB, Lektrakul N, Botte MJ, Trudell D, Boutin RD, et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000;217:201–212. doi: 10.1148/radiology.217.1.r00oc40201. [DOI] [PubMed] [Google Scholar]
- 42.Schoffl V, Schoffl I. Injuries to the finger flexor pulley system in rock climbers: current concepts. J Hand Surg Am. 2006;31:647–654. doi: 10.1016/j.jhsa.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 43.Schöffl V, Küpper T, Hartmann J, Schöffl I. Surgical repair of multiple pulley injuries: evaluation of a new combined pulley repair. J Hand Surg Am. 2012;37:224–230. doi: 10.1016/j.jhsa.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 44.Bouyer M, Forli A, Semere A, Chedal Bornu BJ, Corcella D, Moutet F. Recovery of rock climbing performance after surgical reconstruction of finger pulleys. J Hand Surg Eur. 2016;41(4):406–412. doi: 10.1177/1753193415623914. [DOI] [PubMed] [Google Scholar]


